Abstract
Introduction: the Er,Cr:YSGG laser has a suitable wavelength for the ablation of both hard and soft tissues of the periodontium and can be considered as a potential tool in periodontal surgeries. The current study aimed at evaluating the application of this laser versus conventional instruments in periodontal pocket reduction flap surgery.
Methods: Eight patients (16 dental arches) requiring periodontal surgery were included (Trial registration number: IRCT201711129014N199). Using a split-mouth study design, two posterior sextants of a dental arch were randomly allocated into either a test group, open flap debridement periodontal surgery using the Er,Cr:YSGG laser or a control group using the conventional method. Laser parameter settings of a 2780 nm wavelength, H mode (60 µs pulse duration), 25-50 Hz, 2-3.5 W output powers and Air-20%, Water-60-80% were applied and adjusted individually for each step of the flap surgery procedure. Baseline, 1 and 3-month measurements of plaque index (PI), Gingival Index (GI), gingival recession (GR), probing depth (PD) and clinical attachment level (CAL) were recorded for comparisons. Data were analyzed by a linear model for correlated data using the generalized estimating equations (GEE) method and the least significant difference (LSD).
Results: In both treatment groups, reductions in PI and GI were observed in the 3-month follow-up period. These indices were significantly lower in the laser-treated sides compared to the conventional group (P<0.05). The Mean PD and CAL were lower at 1 month and 3 months compared to the baseline in both groups (P<0.05). However, these parameters were not statistically different in the treatment groups during these follow-up timelines. An increase in GR was observed from the baseline to 1 month and 3 months with less recession in the laser-treated sides (P=0.016).
Conclusion: Based on the results of the present study, the Er,Cr:YSGG laser assisted periodontal flap surgery resulted in similar treatment outcomes to the conventional method and may be considered as a safe and effective treatment modality.
Keywords: Laser, Surgical flap, Periodontitis, Randomized controlled trial
Introduction
Periodontal diseases (periodontoclasia) include a diverse array of inflammatory conditions affecting the attachment apparatus and leading to tooth loss or even systemic inflammation in severe and chronic cases. 1
Periodontal therapy is aimed to halt disease progression or promote regeneration of lost periodontal tissues. 2-4 Treatment approaches to periodontitis vary from non-surgical debridement (scaling and root planning) and sub/supragingival curettage to gingivectomy and full or split-thickness periodontal flap procedures which may involve osseous recontouring or regeneration procedures. 5-9
Recent research on laser-assisted periodontal procedures has been seeking to use the less invasive and more favorable decontamination effects of lasers to assist in treating periodontitis. Different laser types, including diodes, Nd:YAG, CO2 and erbium (Er:YAG, Er,Cr:YSGG), have been suggested as devices with the potential to be used as adjunctive or alternative tools in periodontal treatment procedures. 10-12
The Erbium, chromium-doped: yttrium, scandium, gallium, garnet laser (Er,Cr:YSGG) with a wavelength of 2780 nm is one of the erbium lasers that is currently being used in dentistry for the removal of soft tissues such as gingiva and hard tissues such as bone, dentin and even the enamel. It has high absorption in hydroxyapatite and water, and with its water-mediated thermomechanical mechanism of action, it can result in ablation of these tissues with minimal thermal side effects. 13-15
The erbium laser has been shown to be effectively used as an adjunctive in non-surgical periodontal therapy and removal of plaque, calculus, and diseased cementum and enhance access to complex anatomical structures such as furcation areas. 16-18 Its application has also been reported to result in higher patient comfort and satisfaction, and other beneficial effects such as reduction in the bacterial load, the enhancement of healing and less postoperative pain have been reported. 17,19,20
Many studies have been conducted on the application of the Er,Cr:YSGG laser in the debridement and non-surgical phase of periodontal treatments resulting in the reduction of inflammation in periodontal tissues. A recent systematic review with meta-analysis in 2021 by Li et al has reported its additional benefits in probing depth (PD) reduction and clinical attachment level (CAL) gain in the short term. 17,21-23
The Er,Cr:YSGG laser is a suitable device for performing periodontal surgical procedures as it is capable of cutting and recontouring both hard and soft periodontal structures with negligible heat or damage to the adjacent tissue. 13,15,19,24-29 Its effectiveness in root debridement and bactericidal effects combined with the water spray and irrigation provide convenient management and debridement of periodontal defects. However, its clinical application for the entire procedure of surgical periodontal treatment of needs further well-designed clinical studies.
A recent multicenter study has indicated a similar clinical outcome for applying the Er,Cr:YSGG laser in closed pocket debridement compared with the minimally invasive surgical technique (MIST) to treat intrabony defects. They also reported more favorable patient-reported outcomes of the laser treatment. 30
Previously, the clinical effectiveness of a different wavelength of Erbium lasers, the Er:YAG (2940 nm), has been studied for performing a surgical periodontal flap treatment, and its superiority in long-term reduction of PD and gain in attachment compared to the conventional surgery has been reported. 7
However, to our knowledge, this is the first study using an Er,Cr:YSGG laser as a tool for the entire procedure of periodontal flap surgery and comparing it to a conventional open flap debridement procedure. The positive potentials of this device made us eager to conduct a split-mouth study to propose a step-by-step laser surgical procedure and assess its clinical outcomes in the treatment of periodontitis.
Materials and Methods
This study was designed as a single-blinded, split-mouth, randomized controlled trial. The trial has been registered in the registry of clinical trials (identifier: IRCT201711129014N199) and the design has been ethically approved by the university ethical committee (IR.UMSHA.REC.1396.525). Sixteen dental arches in eight systemically healthy patients aged 18-45 years of either gender were referred to the department of periodontics with a diagnosis of generalized periodontitis. Stage II- III, Grade B were considered for the study after obtaining informed consent from each patient. Patients with at least 20 teeth with bilateral sextants with similar horizontal bone loss with pockets of ≥ 5 mm PD at a minimum of two sites, in the sextants, remaining after initial nonsurgical periodontal treatment were included for the split-mouth study. The patients had been followed up 4 weeks after initial therapy. They were selected for surgical treatment if their full mouth plaque index (O’Leary) was below 20%. The patients also received oral hygiene instructions on each visit. The exclusion criteria were areas with deep angular bone loss, patients with systemic diseases and conditions affecting the periodontium, including diabetes, pregnancy and lactation, tobacco use, or antibiotic treatments in the previous 6 months. Simple randomization using a coin was used for allocating the sextant to the two groups by a person not aware of the treatment procedures.
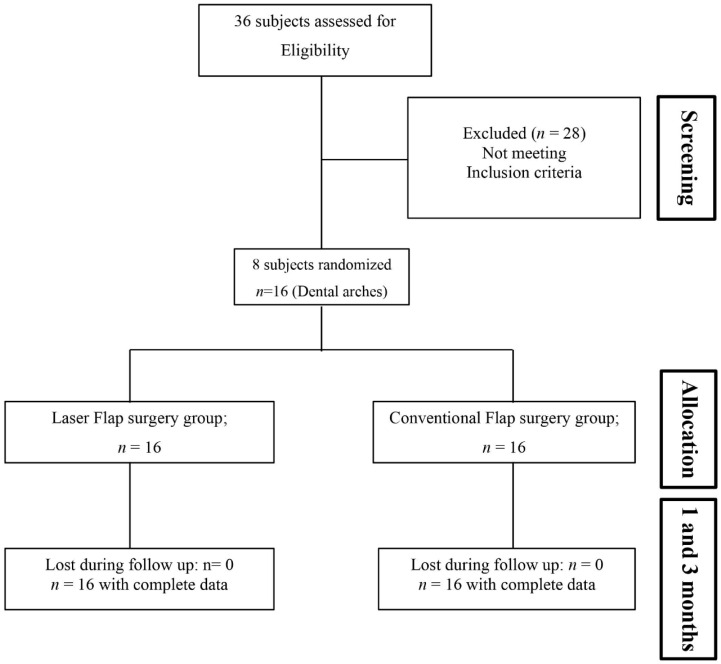
Six areas around each tooth were carefully probed by a single periodontist who was blinded to the surgical intervention assigned to each side. Plaque index (PI), Gingival Index (GI), probing depth (PD), clinical attachment level (CAL) and gingival recession (GR) were recorded at baseline and re-evaluated after 1 month and 3 months (Figure 1).
Figure 1.
Flowchart of the Study Design and Conduct.
Surgical Procedures
One side of each arch was randomly assigned to receiving the flap surgery by the Er,Cr:YSGG laser as the test group and the control side was treated by conventional open flap surgery. Local anesthesia was achieved using 2% lidocaine hydrochloride solution with epinephrine (1:80 000) (Darou Pakhsh Pharmaceutical, Tehran, Iran) prior to surgeries.
Conventional Flap Debridement Surgery Treatment Group
In the Control group (open flap debridement), a periodontal flap incision was made with a No. 15 blade (Swann-Morton, Sheffield, England) with 0.5 mm from the margin just removing the epithelial lining of the pockets. Reflections were performed by a periosteal elevator. After the removal of fibrous and granulomatous tissues, complete scaling and root planning on root surfaces was performed by an ultrasonic device (UDS-k, Guilin Woodpecker Medical Instrument Co, China). Then minimal bone recontouring was completed as needed using bur and hand instruments (Hu-Friedy, Chicago, IL, USA). The flap was re-adapted and sutured with 3.0 silk (Supa Medical, Tehran, Iran) in simple interrupted sutures.
Er,Cr:YSGG Laser Flap Surgery Group
On the contralateral side, the complete surgical procedure was performed using a 2780 nm wavelength laser (Water Lase iPlus, BIOLASE, CA, USA) and its gold handpiece with suitable laser tips. Detailed laser parameters are presented in Table 1. The procedure consisted of the following steps (Figure 2).
Table 1. Laser parameters for each step of the surgical procedure .
| Stage | Tip/Setting |
| Flap incisions | MZ6 tip/2 W, 50 Hz, 20% A/60% W, H-mode (60 µs pulse duration) |
| Root debridement, calculus removal and tissue degranulation | MZ6 tip/3.5 W, 30 Hz, 20% A/80% W, H-mode |
| Root planning | Sapphire chisel MC3/3.5 W, 75 Hz, 20% A/80% W, H-mode |
| Osseous recontouring | MZ8 tip/2.5 W, 25 Hz, 20% A/80% W |
| De-epithelialization | Sapphire chisel MC3 tip / 2 W, 50 Hz, 20% A/60% W, H-mode |
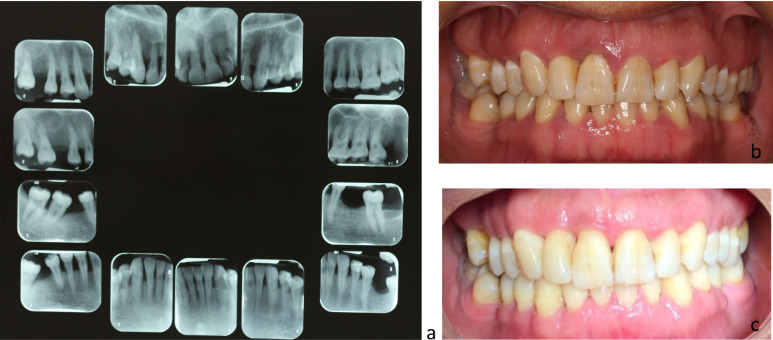
Figure 2.
(a) Baseline full-mouth periapical radiograph, (b) Pretreatment intraoral photo of a patient who was treated with the laser technique in the right maxillary sextant and the conventional flap surgery in the left side, (c) 3-month follow-up intraoral photograph.
1- Horizontal incisions and flap elevation:The incision was performed by adjusting the settings to 2 W, 50 Hz, 40 mJ with Air-20%, water-60% with H-mode (pulse duration of 60 µm), resulting in an energy density of 111 J/cm2 (Calculations based on irradiating a surface covered by the laser tip at a speed of 2 mm/s in 30 seconds). The MZ6 tip (BIOLASE, CA, USA) was inserted to the base of the pocket circumferentially and used to perform horizontal incisions of the flap like the conventional flap and remove the epithelial pocket lining.
2- Granulation Tissue removal:The flap was elevated with a periosteal elevator and the same laser irradiation was used to remove the granulation tissues remaining in interproximal areas.
3- Root debridement: In the first stage, any remaining calculus was removed with laser irradiation with a settings of air-20%, water-80%, MC3 Chisel tip, 3.5 W, 30 Hz, H mode, 116 mJ, 161 J/cm2. Then, the setting was changed to a higher frequency of 75 Hz, 47 mJ, 65 J/cm2 for root planning.
4- Osseous recontouring: This procedure was performed as needed with an MZ8 tip that is wider and makes bone contouring easier. A power of 2.5 W, 25 Hz, Air-40%, Water-80% with H-mode, 100 mJ, 208 J/cm2 was used.
5- De-epithelialization of the gingival at the flap margins: Two to three mm from the margin on the outer epithelium of the flap was de-epithelialized to prevent early proliferation and migration of the epithelial cells towards the sulcus and assist in better healing and attachment gain. 31,32 Irradiation parameters and laser tips were identical to step 1 for this final step.
The flaps were readapted and sutured in the same manner as the conventional OFD side. A periodontal dressing was placed on both sides (Coe-Pak, GC America. Inc, Illinois, USA). Post-surgical instructions were given, and acetaminophen as an analgesic, in case of pain, and a mouth rinse (Chlorhexidine, Shahre Darou Pharmaceutical, Tehran, Iran), twice daily, were prescribed for one week. Sutures were removed after a week and the patient was instructed on starting tooth brushing.
Re-evaluation Phase and Data Collection
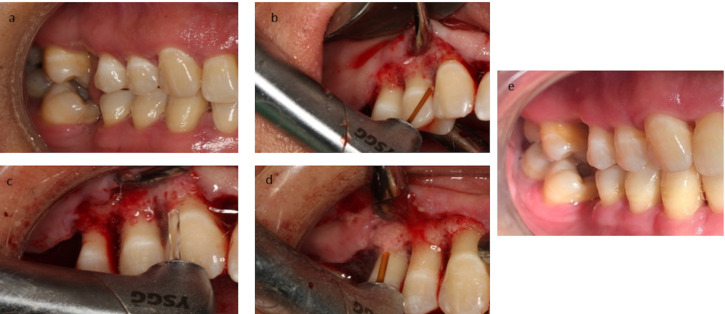
A calibrated and blinded clinician measured the baseline clinical parameters and re-evaluated them one month and three months after the treatments. Clinical evaluations consisted of Sillness & Loe PI, GI, GR, PD, and CAL. A manually calibrated Periodontal probe (UNC15, Hu-Friedy, Chicago, IL, USA) was used for the measurements (Figure 3).
Figure 3.
Laser Flap Surgery Treatment Stages. (a) Before treatment, (b) Flap incision using MZ6 laser tip and elevation using a periosteal elevator and removal of granulation tissues, (c) Removal of calculus and root planning with a MC3 tip, (d) Bone recontouring using a MZ8 tip, (e) 3 months after treatment.
Statistical Analysis
The collected data were analyzed by SPSS statistical software (Version 25.0, SPSS Inc. Chicago, IL, USA). Mean and standard deviation for the description of outcomes and a linear plot for the visualization of quantitative data were used. To investigate the trend of different features over time for the two groups, a linear model for correlated data using the generalized estimating equations (GEE) method was applied. Also, pairwise comparisons within each treatment group in 1 month and 3 months versus the baseline were performed by the least significant difference (LSD) method. The level of significance was set at less than 0.05.
Results
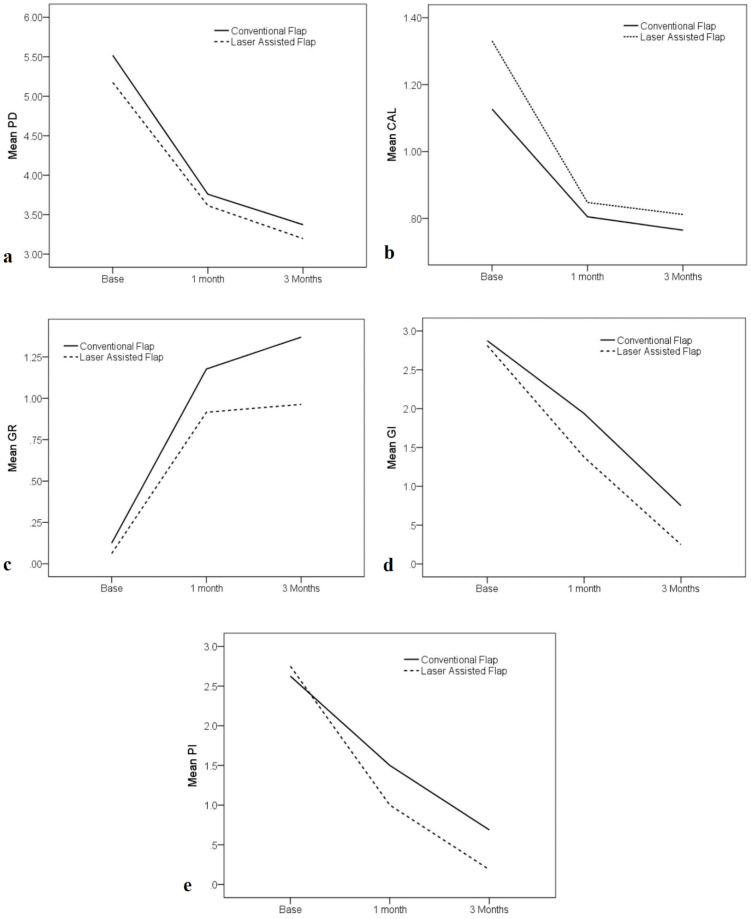
All patients (16 dental arches) were treated without any side effects, and clinical treatment outcome measurements were evaluated at one- and three-month recalls (Figure 4).
Figure 4.
Means (± SD) of Periodontal Indices From the Baseline and 1- and 3-Month Follow-ups.
Plaque Index
A full mouth plaque score (O’Leary) was used for the inclusion of patients in the study and for evaluating patients’ overall oral hygiene during the study. PIs were less than 20% for all participants during this period. PI of Sillness & Loe was used for comparison between the two treated sextants in patients. No statistical difference existed between the baseline measurements of the treatment groups (Table 1). PI reduced significantly 1 month and 3 months after the treatment, and the PI values were lower in the laser group at both time points of 1 month and 3 months (P < 0.05). However, there were no significant differences in comparing the mean amounts of PI in the treatment groups (P = 0.19). The mean amounts of changes were also not considered statistically significant (P = 1.0) (Tables 2 and 3).
Table 2. Means (± SD) of the Periodontal Indexes by Treatment Groups at Baseline and Follow-up Periods of 1 and 3 Months in 16 Quadrants .
| Baseline | 1-Month | 3-Month | P Value | ||
| PD | Conventional flap n = 16 | 5.51 (0.72) | 3.75(0.48)a | 3.37(0.35)a | 0.575 |
| Laser flap n = 16 | 5.17(0.19) | 3.61(0.41)a | 3.19(0.41) a | ||
| GR | Conventional flap n = 16 | 0.12(0.34) | 1.17(0.68)a | 1.36(0.64) a,b | 0.350 |
| Laser flap n = 16 | 0.06(0.25) | 0.91(0.61) a | 0.96(0.63)a,b | ||
| CAL | Conventional flap n = 16 | 1.12 (0.20) | 0.80 (0.21) a | 0.76 (0.14)a | 0.398 |
| Laser flap n = 16 | 1.32(0.16) | 0.84 (0.20) a | 0.80 (0.16) a | ||
| PI | Conventional flap n = 16 | 2.62 (0.50) | 1.50 (0.51)a,b | 0.69 (0.47) a,b | 0.19 |
| Laser flap n = 16 | 2.75 (0.44) | 1.00 (0.63) a,b | 0.19 (0.40) a,b | ||
| GI | Conventional flap n = 16 | 2.87 (0.34) | 1.94 (0.44)a,b | 0.75 (0.44)a,b | 0.039 |
| Laser flap n = 16 | 2.81 (0.40) | 1.38 (0.50)a,b | 0.25 (0.44)a,b |
Abbreviations: PD, probing depth; GR, Gingival Recession; CAL, clinical attachment level; PI, plaque index; GI, Gingival Index.
Pairwise comparisons of estimated marginal means based on the original scale of dependent variables were also made between Baseline values and 1 and 3 months follow up periods. a: The mean difference from baseline in each treatment group is significant at the 0.05 level. b: indicates significant difference between the treatment groups at each time point. *Significant difference Compared to baseline.
Table 3. Means (± SD) of Changes Compared to Baseline in Periodontal Indexes in the Two Treatment Groups .
| 1-Month | 3-Month | P Value | ||
|
PD changes |
Conventional flap n = 16 | -1.75 (0.63) | -2.14 (0.61) | 0.898 |
| Laser flap n = 16 | -1.55 (0.41) | -1.97 (0.45) | ||
|
GR changes |
Conventional flap n = 16 | 1.05 (0.68) | 1.24 (0.68) | 0.598 |
| Laser flap n = 16 | 0.85 (0.60) | 0.90 (.62) | ||
|
CAL changes (Gain) |
Conventional flap n = 16 | -0.97 (0.88) | -1.43 (1.00) | 0.952 |
| Laser flap n = 16 | -.90 (0.72) | -1.34 (0.62) | ||
| PI changes | Conventional flapn = 16 | -1.12 (0.80) | -1.93 (0.68) | 1.00 |
| Laser flap n = 16 | -1.75 (0.85) | -2.56 (0.62) | ||
| GI changes | Conventional flap n = 16 | -0.93 (0.57) | -2.12 (0.50) | 0.831 |
| Laser flap n = 16 | -1.43 (0.63) | -2.56 (0.63) |
Abbreviations: PD, probing depth; GR, Gingival Recession; CAL, clinical attachment level; PI, plaque index; GI, Gingival Index.
Gingival Index
GI showed a significant decrease compared to the baseline in both groups (Table 4). No statistically significant difference was found for mean changes in GI when comparing the two groups at 1 month and 3 months (P = 0.831) (Tables 3 and 4). However, GI levels were lower in the laser-treated areas at each re-evaluation time point (P < 0.05).
Table 4. Means (± SD) Levels of the Periodontal Indexes at Baseline .
| Periodontal index |
Conventional Flap
Mean (SD) |
Laser Flap
Mean (SD) |
P Value |
| PD | 5.51 (0.72) | 5.17(0.19) | 0.016 |
| GR | 0.12(0.34) | 0.06(0.25) | 0.711 |
| CAL | 1.12(0.20) | 1.32(0.16) | 0.055 |
| PI | 2.62 (0.50) | 2.75 (0.44) | 0.489 |
| GI | 2.87 (0.34) | 2.81 (0.40) | 0.679 |
Abbreviations: PD, probing depth; GR, Gingival Recession; CAL, clinical attachment level; PI, plaque index; GI, Gingival Index.
Probing Depth and Clinical attachment levels
The Mean PD and CAL measurements decreased from the baseline to 1 month and 3 months in the study groups. However, the differences between the groups were not statistically significant at any follow-ups (Table 4 and Figure 4). There was a difference observed in baseline measurements between the two groups; therefore, changes in these amounts were reported and compared for further evaluation and analysis of the data (Tables 3, 5 and 6)
Table 5. Percentage of Sites With ≥ 5 mm Initial Probing Depths and the Changes in PD Between Baseline and Follow up Periods of 1 and 3 Months .
| PD Changes | 1-Month vs Baseline | 3-Month vs Baseline | |||
| Laser, No. (%) | Conventional Flap, No. (%) | Laser, No. (%) | Conventional Flap, No. (%) | ||
| Gain | ≤ -2 | 73 (62.4) | 57 (55.9) | 99 (84.7) | 77 (75.5) |
| Gain | -1 | 40 (34.2) | 36 (35.3) | 17 (14.5) | 22 (21.6) |
| No change | 0 | 4 (3.4) | 9 (8.8) | 1 (0.9) | 3 (2.9) |
| Loss | 1 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Total (initial PD ≥ 5) | 117 (100) | 102 (100) | 117 (100) | 102 (100) | |
Table 6. Percentage of Sites With ≥ 5 mm Initial Probing Depths and the Changes in CAL Between Baseline and Follow‐up Periods at 1- and 3-Month Time Points .
| CAL Changes (mm) | 1-Month vs Baseline | 3-Month vs Baseline | |||
| Laser, No. (%) | Conventional Flap, No. (%) | Laser, No. (%) | Conventional Flap, No. (%) | ||
| Gain | ≤ -2 | 53 (45.3) | 48 (47.1) | 55 (47.1) | 52 (51.1) |
| Gain | -1 | 49 (41.9) | 37 (36.3) | 51 (43.6) | 35 (34.3) |
| No change | 0 | 15 (12.8) | 16 (15.7) | 11 (9.4) | 14 (13.7) |
| Loss | 1 | 0 (0.0) | 1 (1.0) | 0 (0.0) | 1 (1.0) |
| Total (initial PD ≥ 5) | 117 (100) | 102 (100) | 117 (100) | 102 (100) | |
The mean PD change (reduction) at one month was -1.55 (0.41) in the laser group and -1.75 (0.63) for the conventional treatment method. The changes in PD at 3 months were -1.97(0.45) in the laser treatment group and -2.14 (0.61) in the control group with no statistically significant difference between the groups (P = 0.898). Comparison of CAL changes (gain) in the two groups revealed no statistically significant difference (P = 0.952) (Table 3).
To further evaluate the clinical outcomes of these treatment modalities, the reduction of PD and gain in CAL in deep pockets, the percentage of sites with PDs of ≥ 5 mm showing different amounts of PD reduction and CAL gain were investigated (Tables 5 and 6).
In terms of changes in PD and CAL in sites with pockets of 5 mm or more, similar trends of changes in PD and CAL were observed in the two treatment groups. At 3 months, 84.7% of sites in the laser-treated group and 75.5% in the conventional flap group showed a 2 mm or more reduction in PD (Table 5), and a 2 mm or more gain in CAL was observed in 47.1% and 51.1% of laser and conventional treatment methods respectively after 3 months. Overall, there were only 5 (1.3%) sites in the laser flap group and 6 (1.4%) sites in the conventional flap group with 5 mm or greater PD remaining. Positive changes and treatment results were observed in most of these sites in both groups, and no statistically meaningful difference was observed between the groups regarding these changes (P > 0.05) (Table 5 and 6).
Gingival Recession
The mean (SD) value of GR at baseline was 0.06 (0.25) for the laser group and 0.12 (0.34) for the flap group with no statistically significant difference (P = 0.711). At one month and 3 months, there was an increase in GR in both groups compared to the baseline. The mean amount of recession was lower in the laser-treated sites at each time point and this difference was statistically meaningful at 3 months (P = 0.016) (Table 4). However, there was no significant difference between the mean changes in GR when comparing the two treatment groups at the re-evaluation time points (Table 2).
Discussion
The Er,Cr:YSGG laser was utilized as monotherapy to perform the full procedure of periodontal flap surgery in the present study. To evaluate its clinical efficacy, periodontal parameters were compared with the conventional treatment procedure in a split-mouth design. According to the obtained data, both treatment methods were able to result in the pocket reduction, CAL gain, and elimination of deep pockets with no statistically significant difference between the study groups. The amount of PI and GI reduced with treatment with lower amounts in the laser group (P < 0.05, Table 2). An increase in GR was observed with both treatment modalities; however, GR was lower in the laser-treated sites at 3 months (P < 0.05, Table 2).
The Erbium family of lasers consists of two wavelengths of Er:YAG (2940 nm) and Er,Cr:YGG (2780 nm) with a similar water-mediated thermomechanical mechanism of action. With the correct irradiation settings and sufficient water irrigation, both can be considered tools to produce effective ablation of soft and hard periodontal tissues with good healing. Moreover, these lasers are capable of removing calculus and smear layers from the roots in periodontally involved teeth which make them a suitable device for the treatment of periodontitis. 33 Moreover, laser light irradiation provides better debridement of all root surfaces without having the dimensional limitations of conventional devices.
Favorable healing has been reported for Er,Cr:YSGG laser treatments when used with appropriate settings. 28,34-36 Perussi et al have performed an animal study on soft tissue and bone healing of the Er,Cr:YSGG laser and concluded that in soft tissues healing of a cut produced by 2 W, 20 Hz irradiation of Er,Cr:YSGG was similar to a scalpel. Its use on hard tissue, however, revealed statistically more significant bone formation than bone removal using a diamond bur. 29 Pavone et al have reported a stimulated bone repair for Er,Cr:YSGG performed osteotomies in rats that were exposed to inhalation of cigarette smoke. 27
These lasers have been studied for their application in non-surgical periodontal treatments, showing their effectiveness as adjunctive to non-surgical pocket debridement. 16,37-43 Based on a recent meta-analysis on the results of the application of Er,Cr:YSGG in non-surgical treatments of periodontitis, additional effectiveness was reported for this device in PD reduction and CAL gain and lower pain compared with Scaling and root planing (SRP) alone. 23
Although there exists a specific open flap surgery option on the Er,Cr:YSGG device used in the current study, its efficacy in clinical practice has not been studied in a randomized clinical trial before.
Previously, Gaspirc and Skaleric have conducted a similar study on the Er:YAG laser and its application in periodontal flap surgery. Based on their results, a greater PD reduction and CAL gains could be achieved in Er:YAG treated groups compared to the conventional Widman flap treated group for up to 3 years, which might be as a result of an excellent root debridement obtainable with Er:YAG laser irradiation. Moreover, it was demonstrated that the results of both treatments could be maintained for up to 5 years. 7
Root surface biocompatibility is a significant variable for the creation of new attachment, clinically noted after surgical therapy as a gain in CAL. In vitro, root surface irradiation by the Er,Cr:YSGG laser has shown positive results in terms of PDL cell attachment, spread and orientation. 42,44,45 According to these researchers, the laser exerts its stimulating impact by producing prostaglandin E2 through increased cyclooxygenase-2 expression, a significant regulatory pathway for rapid wound healing. The laser used in our study was similar to the device used in Hakki and colleagues’ 42 study in which an Er,Cr:YSGG laser ( 2.780 nm, short pulse (H mode), 1.5 W, 10 Hz with 65% air and 55% water) was utilized that created high peak powers, resulting in effective ablation and minimum thermal effects.
Improved biocompatibility of root surfaces by Er,Cr:YSGG laser irradiation may have helped in achieving better attachment. Although no statistically significant difference in CAL gain or PD reduction was observed in the current study between the two groups, there was less GR in the laser-treated group, which may result from the favorable root debridement and favorable healing achievable with this laser. This lower amount of recession in laser-treated sites was also reported in the surgical flap application of the Er:YAG by Gaspirc and Skaleric. 7
In a study similar to the present study, Desai and Gutknecht have applied a minimally invasive erbium laser surgery method for the treatment of periodontal pockets using Er:YAG and Er,Cr:YSGG devices. These researchers reported improvements in PD and CAL with both lasers with a comparable range of changes to the results observed in previous studies implementing a conventional modified Widman flap or osseous surgery. They also concluded that in comparison to those traditional techniques, no significant change in terms of recession in patients treated with the minimally invasive erbium flap technique was observed over a six-month period. 46 These researchers had used hand instruments and ultrasonic devices for calculus removal after raising the periodontal flaps and laser only for smear layer removal, However, in the current study we used the laser irradiation for removal of any remaining calculus in hard-to-reach areas with a lower frequency setting of the device and then the setting was adjusted to a higher frequency to achieve a smoother root planing surface and detoxification.
Clem et al. have recently studied the Er,Cr:YSGG laser for treating intrabony defects, using the radial firing tip of this device designed for deep periodontal pocket debridement without raising a flap. According to the reported results, the laser treatment was as effective as the MIST. The differences in comparing the two treatment strategies were not statistically significant for GR or PD reduction or CAL gain, and the authors concluded that this laser treatment procedure is as effective as the MIST. 30
Previous in vitro research has shown bactericidal and detoxifying impacts of laser irradiation on root surfaces, smear layer removal resulting in favorable tissue reattachments that might contribute to better healing and lower recessions observed in laser-treated groups. 19,47-51 Moreover, it has been shown that laser radiation can eliminate endotoxins from roots in a dosage-dependent manner. 52 This may be performed without noticeable morphological changes to the root surface and with effective calculus removal. 18 This antibacterial effect has also been shown on periodontal pathogens with Er,Cr:YSGG in a study by Gutknecht et al. 20
PI and GI results were also lower in laser-treated sites in the present study, which might result from better root debridement and the disinfecting effect of the laser that might have influenced the healing process. Therefore, less pain and good healing may have made oral hygiene of the laser-treated sides easier for patients. Microbial evaluations from the baseline and residual pockets are recommended in future studies to investigate correlations between bacterial loads and clinical parameters. The patient reported satisfaction, and the outcomes are also suggested to be evaluated in future studies.
According to the available literature the Er,Cr:YSGG laser seems to offer many advantages such as minimal invasiveness, reduction of inflammation, favorable healing and lower amounts of recession, probably through its reported stimulation of human gingival fibroblast cell proliferation and better root debridement and antibacterial effects. 53-55
The step-by-step laser surgery procedure described in the present study was demonstrated to be safe with clinical results comparable to a conventional approach and may be considered as an alternative treatment modality. However, laser treatments may not be currently regarded as cost-effective and additional education and knowledge of the clinician and implementation of laser safety protocols are needed for laser treatment procedures.
The present study had a limitation of the number of patients and we suggest further well-controlled studies with a greater number of patients and longer follow-up periods. Moreover, it would be interesting to evaluate the surgeon’s preference, amount of pain, and chair time to better elucidate its clinical application potential.
Conclusion
According to the results, the proposed Er,Cr:YSGG laser flap surgical method was as effective as the conventional open flap technique in the surgical treatment of periodontitis patients. There was no significant difference between the groups regarding clinical treatment outcomes of PD and CAL. PI and GI levels were lower in laser-treated sides at 1- and 3-month follow-ups, and GR was lower in the laser-treated sites at 3 months.
Conflict of interests
The authors certify that they have no kind of conflict of interest.
Ethical Considerations
The current research was approved by the university’s ethical committee (Code: IR.UMSHA.REC.1396.525).
Funding
The study was funded by a university grant and there were no other sources of funding (Grant number: 9608305392).
Informed Consent
All patients provided written informed consent prior to the surgery.
Please cite this article as follows: Torkzaban P, Barati I, Faradmal J, Ansari-moghadam S, Gholami L. Efficacy of the er,cr:ysgg laser application versus the conventional method in periodontal flap surgery: a split-mouth randomized control trial. J Lasers Med Sci. 2022;13:e4. doi:10.34172/jlms.2022.04.
References
- 1.Kinane DF, Stathopoulou PG, Papapanou PN. Periodontal diseases. Nat Rev Dis Primers. 2017;3:17038. doi: 10.1038/nrdp.2017.38. [DOI] [PubMed] [Google Scholar]
- 2.Taniguchi Y, Aoki A, Mizutani K, Izumi Y. Application of the Characteristics of Er: YAG Laser in Periodontal Therapy. Nippon Laser Igakkaishi. 2016;37(1):43–51. doi: 10.2530/jslsm.jslsm-37_0006. [DOI] [Google Scholar]
- 3.Aoki A, Mizutani K, Taniguchi Y, Komaki M, Ejiri K, Mikami R. et al. Periodontal pocket therapy using Er:YAG laser: systematic review of literature and introduction of a new treatment procedure. Nippon Laser Igakkaishi. 2017;38(2):167–178. doi: 10.2530/jslsm.jslsm-38_0025. [DOI] [Google Scholar]
- 4.Cobb CM. Clinical significance of non-surgical periodontal therapy: an evidence-based perspective of scaling and root planing. J Clin Periodontol. 2002;29(s2):22–32. doi: 10.1034/j.1600-051X.29.s2.4.x. [DOI] [PubMed] [Google Scholar]
- 5.Ramfjord SP. Present status of the modified widman flap procedure. J Periodontol. 1977;48(9):558–565. doi: 10.1902/jop.1977.48.9.558. [DOI] [PubMed] [Google Scholar]
- 6.Ramfjord SP, Nissle RR. The Modified Widman Flap. J Periodontol. 1974;45(8):601–607. doi: 10.1902/jop.1974.45.8.2.601. [DOI] [PubMed] [Google Scholar]
- 7.Gaspirc B, Skaleric U. Clinical evaluation of periodontal surgical treatment with an Er:YAG laser: 5-year results. J Periodontol. 2007;78(10):1864–71. doi: 10.1902/jop.2007.070054. [DOI] [PubMed] [Google Scholar]
- 8.Stavropoulos A, Bertl K, Spineli LM, Sculean A, Cortellini P, Tonetti M. Medium- and long-term clinical benefits of periodontal regenerative/reconstructive procedures in intrabony defects: Systematic review and network meta-analysis of randomized controlled clinical studies. J Clin Periodontol. 2021;48(3):410–430. doi: 10.1111/jcpe.13409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mailoa J, Lin GH, Khoshkam V, MacEachern M, Chan HL, Wang HL. Long-Term Effect of Four Surgical Periodontal Therapies and One Non-Surgical Therapy: A Systematic Review and Meta-Analysis. J Periodontol. Oct 2015;86(10):1150–8. doi: 10.1902/jop.2015.150159. [DOI] [PubMed] [Google Scholar]
- 10.Aoki A, Sasaki KM, Watanabe H, Ishikawa I. Lasers in nonsurgical periodontal therapy. Periodontol 2000. 2004;36:59–97. doi: 10.1111/j.1600-0757.2004.03679.x. [DOI] [PubMed] [Google Scholar]
- 11.Schwarz F, Sculean A, Berakdar M, Georg T, Reich E, Becker J. Clinical evaluation of an Er:YAG laser combined with scaling and root planing for non-surgical periodontal treatment: A controlled, prospective clinical study. J Clin Periodontol. 2003;30(1):26–34. doi: 10.1034/j.1600-051x.2003.300105.x. [DOI] [PubMed] [Google Scholar]
- 12.Cobb CM. Lasers and the treatment of periodontitis: the essence and the noise. Periodontol 2000. 2017;75(1):205–295. doi: 10.1111/prd.12137. [DOI] [PubMed] [Google Scholar]
- 13.Harashima T, Kinoshita JI, Kimura Y, Brugnera Jr A, Zanin F, Pecora JD. et al. Morphological comparative study on ablation of dental hard tissues at cavity preparation by Er:YAG and Er,Cr:YSGG lasers. Photomed Laser Surg. 2005;23(1):52–55. doi: 10.1089/pho.2005.23.52. [DOI] [PubMed] [Google Scholar]
- 14.Ishikawa I, Aoki A, Takasaki AA, Mizutani K, Sasaki KM, Izumi Y. Application of lasers in periodontics: true innovation or myth? Periodontol 2000. 2009;50:90–126. doi: 10.1111/j.1600-0757.2008.00283.x. [DOI] [PubMed] [Google Scholar]
- 15.Mizutani K, Aoki A, Coluzzi D, Yukna R, Wang CY, Pavlic V. et al. Lasers in minimally invasive periodontal and peri-implant therapy. Periodontol 2000. 2016;71(1):185–212. doi: 10.1111/prd.12123. [DOI] [PubMed] [Google Scholar]
- 16.Agoob Alfergany M, Nasher R, Gutknecht N. Calculus Removal and Root Surface Roughness When Using the Er:YAG or Er,Cr:YSGG Laser Compared with Conventional Instrumentation Method: A Literature Review. Photobiomodul Photomed Laser Surg. Apr 2019;37(4):197–226. doi: 10.1089/photob.2018.4465. [DOI] [PubMed] [Google Scholar]
- 17.Ge L, Zhang Y, Shu R. Er,Cr:YSGG Laser Application for the Treatment of Periodontal Furcation Involvements. Photomed Laser Surg. 2017;35(2):92–97. doi: 10.1089/pho.2016.4145. [DOI] [PubMed] [Google Scholar]
- 18.Ting CC, Fukuda M, Watanabe T, Aoki T, Sanaoka A, Noguchi T. Effects of Er,Cr: SGG laser irradiation on the root surface: morphologic analysis and efficiency of calculus removal. J Periodontol. 2007;78(11):2156–2164. doi: 10.1902/jop.2007.070160. [DOI] [PubMed] [Google Scholar]
- 19.Noori ZT, Fekrazad R, Eslami B, Etemadi A, Khosravi S, Mir M. Comparing the effects of root surface scaling with ultrasound instruments and Er,Cr:YSGG laser. Lasers Med Sci. 2008;23(3):283–287. doi: 10.1007/s10103-007-0480-8. [DOI] [PubMed] [Google Scholar]
- 20.Gutknecht N, Van Betteray C, Ozturan S, Vanweersch L, Franzen R. Laser supported reduction of specific microorganisms in the periodontal pocket with the aid of an Er,Cr:YSGG laser: a pilot study. Scie World J. 2015;2015:450258. doi: 10.1155/2015/450258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gupta M, Lamba AK, Verma M, Faraz F, Tandon S, Chawla K. et al. Comparison of periodontal open flap debridement versus closed debridement with Er,Cr:YSGG laser. Aust Dent J. 2013;58(1):41–49. doi: 10.1111/adj.12021. [DOI] [PubMed] [Google Scholar]
- 22.Sezen D, Hatipoğlu M, Üstün K. Evaluation of the clinical and biochemical efficacy of erbium, chromium:ytrium-scandium-gallium-garnet (ER,CR:YSGG) laser treatment in periodontitis. Lasers Med Sci. 2020;35(7):1567–1575. doi: 10.1007/s10103-020-02990-8. [DOI] [PubMed] [Google Scholar]
- 23.Li MM, Jia JH, Wu MX, Zhao CY, Jia LY, Shi H. et al. Clinical effectiveness of Er,Cr:YSGG lasers in non-surgical treatment of chronic periodontitis: a meta-analysis of randomized controlled trials. Lasers Med Sci. Jun 2021;36(4):889–901. doi: 10.1007/s10103-020-03156-2. [DOI] [PubMed] [Google Scholar]
- 24.Ekworapoj P, Sidhu SK, McCabe JF. Effect of different power parameters of Er,Cr:YSGG laser on human dentine. Lasers Med Sci. 2007;22(3):175–182. doi: 10.1007/s10103-006-0426-6. [DOI] [PubMed] [Google Scholar]
- 25.Schwarz F, Aoki A, Becker J, Sculean A. Laser application in non-surgical periodontal therapy: a systematic review. J Clin Periodontol. 2008;35(8 Suppl):29–44. doi: 10.1111/j.1600-051X.2008.01259.x. [DOI] [PubMed] [Google Scholar]
- 26.Almehdi A, Aoki A, Ichinose S, Taniguchi Y, Sasaki KM, Ejiri K. et al. Histological and SEM analysis of root cementum following irradiation with Er:YAG and CO2 lasers. Lasers Med Sci. 2013;28(1):203–213. doi: 10.1007/s10103-012-1110-7. [DOI] [PubMed] [Google Scholar]
- 27.Pavone C, Scardueli CR, De Oliveira GJPL, Cerri PS, Marcantonio Junior E, Marcantonio RAC. Effects of an Er,Cr:YSGG laser on bone regeneration in critical-sized calvarial defects of rats exposed to inhalation of cigarette smoke. Photobiomodul Photomed Laser Surg. 2019;37(8):500–507. doi: 10.1089/photob.2018.4546. [DOI] [PubMed] [Google Scholar]
- 28.Wang X, Zhang C, Matsumoto K. In vivo study of the healing processes that occur in the jaws of rabbits following perforation by an Er,Cr:YSGG laser. Lasers Med Sci. 2005;20(1):21–27. doi: 10.1007/s10103-005-0329-y. [DOI] [PubMed] [Google Scholar]
- 29.Perussi LR, Pavone C, de Oliveira GJPL, Cerri PS, Marcantonio RAC. Effects of the Er,Cr:YSGG laser on bone and soft tissue in a rat model. Lasers Med Sci. 2012;27(1):95–102. doi: 10.1007/s10103-011-0920-3. [DOI] [PubMed] [Google Scholar]
- 30.Clem D, Heard R, McGuire M, Scheyer ET, Richardson C, Toback G. et al. Comparison of Er,Cr:YSGG laser to minimally invasive surgical technique in the treatment of intrabony defects: Six-month results of a multicenter, randomized, controlled study. J Periodontol. 2021;92(4):496–506. doi: 10.1002/jper.20-0028. [DOI] [PubMed] [Google Scholar]
- 31.Rossmann JA, Israel M. Laser de-epithelialization for enhanced guided tissue regeneration. A paradigm shift? Dent Clin North Am. 2000;44(4):793–809. [PubMed] [Google Scholar]
- 32.Romanos G. Current concepts in the use of lasers in periodontal and implant dentistry. J Indian Soc Periodontol. 2015;19(5):490–4. doi: 10.4103/0972-124x.153471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aoki A, Mizutani K, Schwarz F, Sculean A, Yukna RA, Takasaki AA. et al. Periodontal and peri-implant wound healing following laser therapy. Periodontol 2000. 2015;68(1):217–69. doi: 10.1111/prd.12080. [DOI] [PubMed] [Google Scholar]
- 34.Sperandio FF, Meneguzzo DT, Ferreira LS, Da Ana PA, Azevedo LH, de Sousa SC. Different air-water spray regulations affect the healing of Er,Cr:YSGG laser incisions. Lasers Med Sci. 2011;26(2):257–265. doi: 10.1007/s10103-010-0849-y. [DOI] [PubMed] [Google Scholar]
- 35.Wang X, Ishizaki NT, Suzuki N, Kimura Y, Matsumoto K. Morphological changes of bovine mandibular bone irradiated by Er,Cr:YSGG laser: an in vitro study. J Clin Laser Med Surg. 2002;20(5):245–250. doi: 10.1089/10445470260420740. [DOI] [PubMed] [Google Scholar]
- 36.Ryu SW, Lee SH, Yoon HJ. A comparative histological and immunohistochemical study of wound healing following incision with a scalpel, CO2 laser or Er,Cr:YSGG laser in the guinea pig oral mucosa. Acta Odontol Scand. 2012;70(6):448–54. doi: 10.3109/00016357.2011.635598. [DOI] [PubMed] [Google Scholar]
- 37.Watanabe H, Ishikawa I, Suzuki M, Hasegawa K. Clinical assessments of the erbium:YAG laser for soft tissue surgery and scaling. J Clin Laser Med Surg. 1996;14(2):67–75. doi: 10.1089/clm.1996.14.67. [DOI] [PubMed] [Google Scholar]
- 38.Schwarz F, Sculean A, Georg T, Reich E. Periodontal treatment with an Er:YAG laser compared to scaling and root planing A controlled clinical study. J Periodontol. 2001;72(3):361–367. doi: 10.1902/jop.2001.72.3.361. [DOI] [PubMed] [Google Scholar]
- 39.Schwarz F, Sculean A, Georg T, Reich E, Becker J. Periodontal treatment with an Er: YAG laser compared to scaling and root planing A controlled clinical study. J Periodontol. 2001;72(3):590–596. doi: 10.1902/jop.2001.72.3.361. [DOI] [PubMed] [Google Scholar]
- 40.Schwarz F, Sculean A, Berakdar M, Georg T, Reich E. Clinical evaluation of an Er:YAG laser combined with scaling and root planing for non-surgical periodontal treatment: A controlled, prospective clinical study. J Clin Periodontol. 2003;30(1):26–34. doi: 10.1034/j.1600-051x.2003.300105.x. [DOI] [PubMed] [Google Scholar]
- 41.Al-Falaki R, Hughes F, Wadia R, Eastman C, Kontogiorgos E, Low S. The effect of an Er,Cr:YSGG laser in the management of intrabony defects associated with chronic periodontitis using minimally invasive closed flap surgery A case series. Laser Ther. 2016;25(2):131–139. doi: 10.5978/islsm.16-OR-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hakki SS, Korkusuz P, Berk G, Dundar N, Saglam M, Bozkurt B. et al. Comparison of Er,Cr:YSGG laser and hand instrumentation on the attachment of periodontal ligament fibroblasts to periodontally diseased root surfaces: an in vitro study. J Periodontol. 2010;81(8):1216–1225. doi: 10.1902/jop.2010.090715. [DOI] [PubMed] [Google Scholar]
- 43.Pourzarandian A, Watanabe H, Ruwanpura S, Aoki A, Noguchi K, Ishikawa I. Er:YAG laser irradiation increases prostaglandin E production via the induction of cyclooxygenase-2 mRNA in human gingival fibroblasts. J Periodontal Res. 2005;40(2):182–186. doi: 10.1111/j.1600-0765.2005.00789.x. [DOI] [PubMed] [Google Scholar]
- 44.Blomlöf JP, Blomlöf LB, Lindskog SF. Smear removal and collagen exposure after none-surgical root planing followed by etching with an EDTA gel preparation. J Periodontol. 1996;67(9):841–845. doi: 10.1902/jop.1996.67.9.841. [DOI] [PubMed] [Google Scholar]
- 45.Blomlöf J, Jansson L, Biomlöf L, Lindskog S. Root surface etching at neutral pH promotes periodontal healing. J Clin Periodontol. 1996;23(1):50–55. doi: 10.1111/j.1600-051x.1996.tb00504.x. [DOI] [PubMed] [Google Scholar]
- 46.Desai P, Gutknecht N. Minimally invasive erbium flap (MINIE TM flap)-a retrospective surgical treatment for chronic periodontitis. AMA Arch Intern Med. 2018;2(1):53–62. doi: 10.1007/s41547-017-0019-7. [DOI] [Google Scholar]
- 47.Ciurescu CE, Cosgarea R, Ciurescu D, Gheorghiu A, Popa D, Franzen R. et al. Adjunctive use of InGaAsP and Er,Cr:YSGG lasers in nonsurgical periodontal therapy: a randomized controlled clinical study. Quintessence Int. 2019;50(6):436–447. doi: 10.3290/j.qi.a42508. [DOI] [PubMed] [Google Scholar]
- 48.Teerakapong A, Chuercharuenwasuchi N, Senarasana P, Chaowaratana S, W W-a. The comparison of morphologic of periodontitis involved root surfaces after radiated in vitro with Er:YAG and ER,Cr:YSGG lasers. Khon Kaen Dent J. 2007;10:80–90. [Google Scholar]
- 49.Qu C, Kang J, Luan Q. Effects of Er,Cr:YSGG laser on the root surface of periodontitis and healthy teeth. Beijing Da Xue Xue Bao Yi Xue Ban. 2016;48(1):71–75. [PubMed] [Google Scholar]
- 50.Ando Y, Aoki A, Watanabe H, Ishikawa I. Bactericidal effect of erbium YAG laser on periodontopathic bacteria. Lasers Surg Med. 1996;19(2):190–200. doi: 10.1002/(SICI)1096-9101(1996)19:2<190::AID-LSM11>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 51.Folwaczny M, Mehl A, Aggstaller H, Hickel R. Antimicrobial effects of 294 microm Er:YAG laser radiation on root surfaces: an in vitro study. J Clin Periodontol. 2002;29(1):73–78. doi: 10.1034/j.1600-051x.2002.290111.x. [DOI] [PubMed] [Google Scholar]
- 52.Folwaczny M, Aggstaller H, Mehl A, Hickel R. Removal of bacterial endotoxin from root surface with Er:YAG laser. Am J Dent. 2003;16(1):3–5. [PubMed] [Google Scholar]
- 53.Pié-Sánchez J, España-Tost AJ, Arnabat-Domínguez J, Gay-Escoda C. Comparative study of upper lip frenectomy with the CO2 laser versus the Er,Cr:YSGG laser. Med Oral Patol Oral Cir Bucal. 2012;17(2):e228–32. doi: 10.4317/medoral.17373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Talebi-Ardakani MR, Torshabi M, Karami E, Arbabi E, Esfahrood ZR. In vitro study of Er:YAG and Er,Cr:YSGG laser irradiation on human gingival fibroblast cell line. Acta Medica Iranica. 2016;54(4):251–255. [PubMed] [Google Scholar]
- 55.Rizoiu IM, Eversole LR, Kimmel AI. Effects of an erbium, chromium: yttrium, scandium, gallium, garnet laser on mucocutanous soft tissues. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82(4):386–395. doi: 10.1016/s1079-2104(96)80302-7. [DOI] [PubMed] [Google Scholar]