Abstract
BACKGROUND:
Type 2 myocardial infarction (MI) is increasingly diagnosed in patients with heart failure (HF). A paucity of data exists pertinent to the contemporary prevalence and impact of type 2 MI in patients with HF. We studied the patient profiles and the prognostic impact of type 2 MI on outcomes of HF hospitalizations.
METHODS:
The Nationwide Readmission Database 2018 was queried for patients with HF hospitalizations with and without type 2 MI. Baseline characteristics, inpatient outcomes, and 30-day all-cause readmissions between both cohorts were compared.
RESULTS:
Of 1,072,674 primary HF hospitalizations included in the study, 28,813 (2.7%) had type 2 MI. Patients with type 2 MI were more likely to be males (56.5% vs 51.6%; P < .001) and had a higher prevalence of hypertension (94% vs 92.2%; P < .001), prior myocardial infarction (17.1% vs 14.9%; P < .001), anemia (9.1% vs 8.1%; P < .001), chronic kidney disease (55.7% vs 49.4%; P < .001), neurological disorders (9.4% vs 7.3%; P < .001), and weight loss (7.3% vs 5.6%; P < .001). Compared with their counterparts without type 2 MI, patients with HF with type 2 MI had significantly higher in-hospital mortality (adjusted odds ratio [aOR], 1.53; 95% confidence interval [CI], 1.37–1.72), hospital costs (adjusted parameter estimate, $1785; 95% CI, 1388–2182), discharge to nursing facility (aOR, 1.22; 95% CI, 1.15–1.29), longer length of stay (adjusted parameter estimate, 0.53; 95% CI, 0.42–0.64), and rate of 30-day all-cause readmissions (aOR, 1.06; 95% CI, 1.01–1.12).
CONCLUSION:
Type 2 MI in patients hospitalized with HF is associated with higher mortality and resource utilization in the United States.
Keywords: Heart failure, Outcomes research, Readmissions, Type 2 myocardial infarction
Graphical Abstract
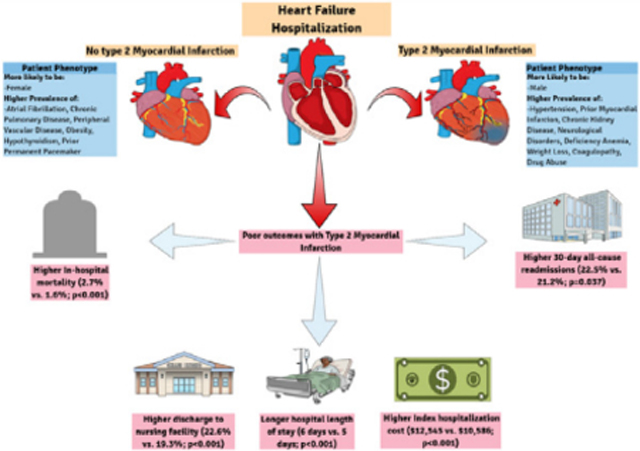
Differences in clinical characteristics and outcomes between patients with heart failure with type 2 myocardial infarction compared with those without type 2 myocardial infarction.
INTRODUCTION
Heart failure is associated with high mortality and morbidity and a significant economic burden in the United States.1,2 For the approximately 6 million patients currently affected by heart failure, the average in-hospital mortality is 3%, and unplanned readmissions within 30-days of discharge occur in more than 20% of patients, resulting in costs amounting to $10,000 per patient.3,4 Although heart failure already imposes substantial costs, these costs are expected to rise dramatically due to the aging population.2 The total annual expenditures are expected to rise to $70 billion by 2030 in the United States.5 Through the Hospital Readmissions Reduction Program (HRRP), the Centers for Medicare and Medicaid Services (CMS) has attempted to control costs associated with heart failure hospitalizations with limited success.6,7 Because health care costs of heart failure are largely driven by rehospitalization costs, tremendous efforts have been made to better understand the risk factors leading to rehospitalizations.
Although type 1 myocardial infarction is characterized by coronary atherothrombosis resulting in acute interruption of coronary blood flow and myocardial necrosis, type 2 myocardial infarction is characterized by myocardial necrosis caused by a mismatch between myocardial oxygen supply and demand.8–10 Patients with heart failure have a higher prevalence of coronary artery disease and a high burden of associated comorbidities, which may predispose them to an increased risk of myocardial oxygen demand-supply mismatch. In contemporary clinical practice, type 2 myocardial infarction is more common than type 1 myocardial infarction and is similarly associated with poor outcomes.11,12 However, the contemporary impact of type 2 myocardial infarction on outcomes in real-world patients with heart failure remains largely unknown. The purpose of the current report is to examine the patient profiles, in-hospital mortality, resource utilization, and 30-day all-cause readmissions among patients with heart failure with type 2 myocardial infarction using a large nationally representative database.
METHODS
Data Source and Study Population
The Nationwide Readmission Database (NRD) was used to extract relevant patient information from January 1, 2018, to December 31, 2018. The NRD is a nationally representative sample of all-payer discharges from US nonfederal hospitals (excluding rehabilitation and long-term acute care facilities) developed by the Agency for Health Care Research and Quality (AHRQ) as part of the Health Care Cost and Utilization Project (HCUP).13 The NRD is drawn from the State Inpatient Databases that contain verified patient linkage numbers that can be used to track individual patients across hospitals within a state while adhering to strict privacy guidelines. The 2018 NRD includes data from 28 geographically dispersed states, accounting for ~60% of all US hospitalizations. Individual patient records in the NRD contain information on the patients’ diagnoses and procedures performed during the hospitalization, based on the International Classification of Diseases, Tenth Revision-Clinical Modification (ICD-10-CM) codes. The institutional review board exempted the study because it uses public deidentified data.
We used the ICD-10-CM diagnosis codes I09.81, I11.0, I13.0, I13.2, and I50.x to identify all primary heart failure hospitalizations (weighted national estimate = 1,268,576). These codes have been found to have excellent sensitivity and specificity in several studies for the identification of heart failure.14,15 A primary heart failure diagnosis refers to hospitalizations mainly attributable to heart failure, whereas a secondary diagnosis refers to hospitalizations in patients with heart failure who were admitted for reasons other than heart failure. We excluded patients younger than 18 years of age, those with missing information on death, end-stage renal disease (ESRD), type 1 (ST-elevation myocardial infarction, non-ST-elevation myocardial infarction) and types 3, 4, and 5 myocardial infarction, cardiogenic shock, cardiac arrest, takotsubo syndrome, acute/chronic myocarditis, pulmonary embolism, severe sepsis, septic shock, and those who underwent any of the following cardiac procedures during the index hospitalization: percutaneous coronary intervention, transcatheter aortic valve replacement, transcatheter edge-to-edge mitral valve repair, transcatheter mitral valve replacement, left atrial appendage occlusion, coronary artery bypass grafting, valvular surgery [aortic, mitral, tricuspid, and pulmonic]. The final study sample included 1,072,951 primary heart failure hospitalizations (Figure 1). Patients with type 2 myocardial infarction were identified using ICD-10-CM code I21.A1. This code has been used by previous studies using the HCUP databases to identify patients with type 2 myocardial infarction.16–18
Figure 1.
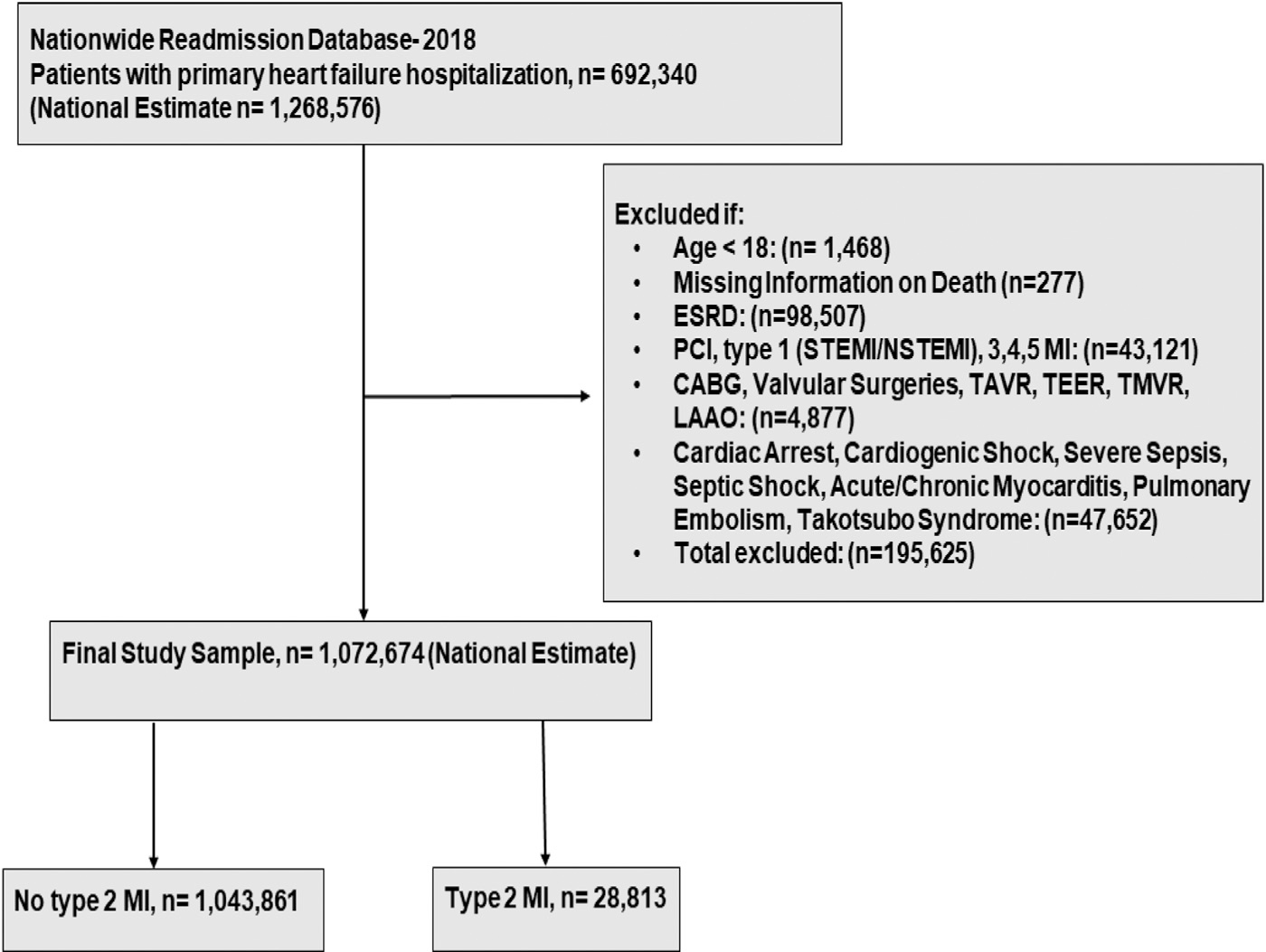
Study population selection flowchart. CABG = coronary artery bypass grafting; ESRD = end-stage renal disease; LAAO = left atrial appendage occlusion; MI = myocardial infarction; NSTEMI = non-ST elevation myocardial infarction; PCI = percutaneous coronary intervention; STEMI = ST-elevation myocardial infarction; TAVR = transcatheter aortic valve replacement; TEER = transcatheter edge-to-edge repair of the mitral valve; TMVR = transcatheter mitral valve replacement.
Patient and Hospital Characteristics
Baseline data included patient demographics (age, sex), admission status (elective vs nonelective, weekend vs weekday), comorbidities (diabetes mellitus, dyslipidemia, hypertension, smoking, obesity, weight loss, hypothyroidism, deficiency anemia, coagulopathy, peripheral vascular disease, prior cerebrovascular accident, prior myocardial infarction, prior percutaneous coronary intervention, prior coronary artery bypass grafting, atrial fibrillation, neurological disorders, alcohol abuse, drug abuse, prior permanent pacemaker, liver disease, chronic kidney disease, chronic lung disease), hospital characteristics (bed size and location/teaching status), and expected primary payer (Medicare, Medicaid, private insurance, self-pay/no charge/other). The ICD-10-CM codes used to define these variables were extracted from the Elixhauser comorbidity index as defined in the HCUP database and additional covariates that are listed in Supplementary Table 1, available online.
Measures and Outcomes
The primary outcome of interest was in-hospital mortality. Secondary outcomes included length of stay, hospital costs, discharge to a nursing facility, and 30-day all-cause readmissions. We also examined the independent predictors of in-hospital mortality and 30-day all-cause readmissions in patients with heart failure with type 2 myocardial infarction. Readmissions were identified according to the methodology outlined by HCUP.13 For the readmission analysis, we excluded records of patients discharged in December 2018 (because of unavailability of 30-day follow-up data on these cases), those who died during hospitalization, and those who left against medical advice during the index hospitalization. For patients who had multiple readmissions within 30 days after index discharge, only the first readmission was included.
Statistical Analyses
All statistical analyses were performed using discharge weights provided by the AHRQ to obtain national estimates. We used complex survey methods to account for stratification and clustering of data in the NRD as recommended by the AHRQ.19 Baseline comorbidities and hospital characteristics were compared between patients with and without type 2 myocardial infarction using the Rao-Scott χ2 test for categorical variables and linear regression for continuous variables. Categorical variables are expressed as frequencies and percentages and continuous variables as mean ± standard error (SE). Multivariable logistic and linear regression models were used to determine the association of type 2 myocardial infarction with outcomes in the overall study cohort and predefined subgroups by heart failure type (systolic vs diastolic), gender (men vs women), and age (<75 vs ≥75 years). These models were adjusted for age, sex, admission status, and all baseline comorbidities/hospital characteristics listed in Table 1. In cases with missing covariates, multivariable regression analyses were performed on complete cases. For the predictors of in-hospital mortality and 30-day readmission, the following covariates were selected a priori and entered in the regression model: age, sex, admission status, and all baseline comorbidities listed in Table 1. Variables with a P < .1 on univariable analysis were entered into a multivariable regression model to identify independent predictors of in-hospital mortality and 30-day readmissions. Hospital charges were converted to costs using the HCUP cost-to-charge ratio files. Effect sizes were expressed using odds ratios (ORs) and 95% confidence intervals (CIs). Associations were considered significant if the P value was <.05. All statistical analyses were performed using Stata 16.0 (StataCorp).
Table 1.
Baseline Characteristics of Heart Failure Patients with and Without Type 2 MI
| Characteristics | Overall (n = 1,072,951) | Type II MI |
P Value | |
|---|---|---|---|---|
| No (n = 1,044,128) | Yes (n = 28,823) | |||
|
| ||||
| Demographics | ||||
| Age, years (mean ± SE) | 72.3(0.13) | 72.3(0.13) | 72.9(0.41) | .12 |
| Female | 518,320(48.3) | 505,790(48.4) | 12,529(43.5) | <.001 |
| Weekend Admission | 253,054(23.6) | 245,851(23.5) | 7202(25) | <.001 |
| Elective Admission | 39,059(3.6) | 38,645(3.7) | 413(1.4) | <.001 |
| Comorbidities | ||||
| Chronic pulmonary disease | 452,668(42.2) | 441,201(42.2) | 11,467(39.8) | <.001 |
| Atrial fibrillation | 506,058(47.1) | 494,140(47.3) | 11,918(41.3) | <.001 |
| Dyslipidemia | 584,038(54.4) | 568,193(54.4) | 15,844(54.9) | .48 |
| Diabetes mellitus | 516,640(48.1) | 502,970(48.1) | 13,670(47.4) | .15 |
| Hypertension | 990,631(92.3) | 963,551(92.2) | 27,080(93.9) | <.001 |
| Obesity | 290,338(27) | 284,112(27.2) | 6226(21.6) | <.001 |
| Peripheral vascular disease | 201,969(18.8) | 196,783(18.8) | 5185(17.9) | .04 |
| Chronic kidney disease | 531,989(49.5) | 515,926(49.4) | 16,062(55.7) | <.001 |
| Liver disease | 49,407(4.6) | 47,982(4.6) | 1425(4.9) | .14 |
| Neurological disorders | 78,801(7.3) | 76,082(7.3) | 2719(9.4) | <.001 |
| Deficiency anemias | 87,096(8.1) | 84,477(8.1) | 2618(9.1) | <.001 |
| Hypothyroidism | 200,165(18.6) | 195,408(18.7) | 4756(16.5) | <.001 |
| Weight loss | 60,958(5.6) | 58,844(5.6) | 2113(7.3) | <.001 |
| Coagulopathy | 67,097(6.2) | 65,022(6.2) | 2074(7.2) | <.001 |
| History of smoking | 469,551(43.7) | 456,709(43.7) | 12,842(44.5) | .34 |
| Alcohol abuse | 41,109(3.8) | 39,880(3.8) | 1229(4.2) | .08 |
| Drug abuse | 54,618(5.1) | 52,620(5.1) | 1997(6.9) | <.001 |
| Previous myocardial infarction | 161,135(15.) | 156,198(14.9) | 4936(17.1) | <.001 |
| Previous CABG | 158,619(14.7) | 154,229(14.7) | 4389(15.2) | .28 |
| Previous PCI | 146,109(13.6) | 142,106(13.6) | 4002(13.9) | .52 |
| Prior ICD or PPM | 105,454(9.8) | 103,166(9.8) | 2288(7.9) | <.001 |
| Prior CVA | 146,764(13.6) | 142,828(13.6) | 3936(13.6) | .94 |
| Hospital Location | .05 | |||
| Metropolitan non-teaching | 241,035(22.4) | 235,483(22.5) | 5551(19.2) | |
| Metropolitan teaching | 706,323(65.8) | 685,825(65.6) | 20,497(71.1) | |
| Nonmetropolitan hospital | 125,591(11.7) | 122,818(11.7) | 2772(9.6) | |
| Hospital Bed-Size | .11 | |||
| Small | 213,705(19.9) | 208,302(19.9) | 5402(18.7) | |
| Medium | 302,860(28.2) | 295,861(28.3) | 6998(24.2) | |
| Large | 556,385(51.8) | 539,963(51.7) | 16,421(56.9) | |
| Primary Expected Payer | .2 | |||
| Medicare | 808,182(75.4) | 786,640(75.4) | 21,542(74.8) | |
| Medicaid | 108,346(10.1) | 105,130(10.1) | 3216(11.1) | |
| Private insurance | 105,804(9.8) | 103,144(9.9) | 2660(9.2) | |
| Self-pay, no charge, or other | 49,098(4.5) | 47,733(4.5) | 1365(4.7) | |
CABG = coronary artery bypass grafting; CVA = cerebrovascular accident; ICD = implantable cardioverter defibrillator; MI = myocardial infarction; PCI = percutaneous coronary intervention; PPM = permanent pacemaker; SE = standard error.
Numbers are frequency (%) unless specified otherwise.
RESULTS
Baseline Characteristics
A total of 1,072,674 primary heart failure hospitalizations were included in this study. Of these, 28,813 (2.7%) had heart failure with type 2 myocardial infarction. Compared to patients without type 2 myocardial infarction, those with type 2 myocardial infarction were less likely to be females and had a higher prevalence of hypertension, previous myocardial infarction, chronic kidney disease, neurological disorders, deficiency anemia, weight loss, coagulopathy, and drug abuse (Table 1, Graphical Abstract, available online). Patients with type 2 myocardial infarction were also more likely to have weekend and nonelective admission. Atrial fibrillation, chronic pulmonary disease, peripheral vascular disease, obesity, hypothyroidism, and prior permanent pacemaker were more prevalent in patients without compared to those with type 2 myocardial infarction.
In-Hospital Mortality
In hospitalized patients with heart failure, type 2 myocardial infarction was associated with significantly higher in-hospital mortality compared with their counterparts without type 2 myocardial infarction (2.7% vs 1.6%; adjusted OR, 1.53, 95% CI, 1.37–1.72; P < .001). In the subgroup analyses, type 2 myocardial infarction was associated with an increased risk of in-hospital mortality in patients with heart failure irrespective of heart failure type (systolic vs diastolic) and age (<75 vs ≥75 years) (Pinteraction ≥ .05). Similar results were seen in the subgroups analyses of gender (men vs women), except the magnitude of risk was more pronounced in women patients with heart failure compared with men (Pinteraction = .007) (Figure 2).
Figure 2.
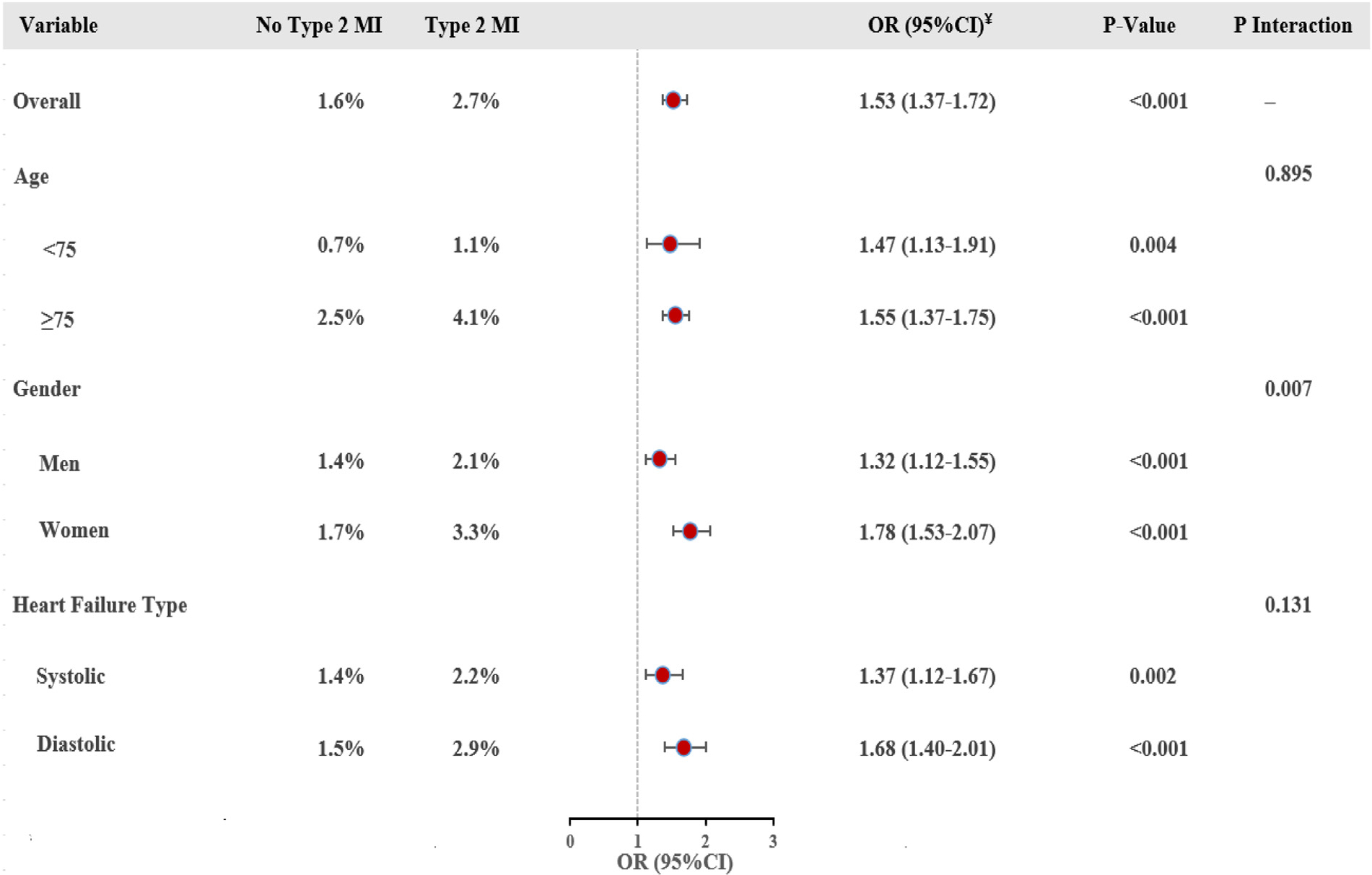
Association between type 2 myocardial infarction and in-hospital mortality among heart failure hospitalizations in the overall cohort and in the prespecified subgroups. ¥ The multivariable logistic regression model included age, sex, and all baseline characteristics listed in Table 1 as covariates. CI = confidence interval; MI = myocardial infarction; OR = odds ratio.
Multivariable analyses identified age, coagulopathy, liver disease, weight loss, and neurological disorders as independently associated with increased risk of in-hospital mortality in heart failure patients with type 2 myocardial infarction (Figure 3). On the other hand, dyslipidemia, smoking, hypertension, and prior percutaneous coronary intervention were identified as negative predictors of in-hospital mortality in patients with heart failure with type 2 myocardial infarction.
Figure 3.
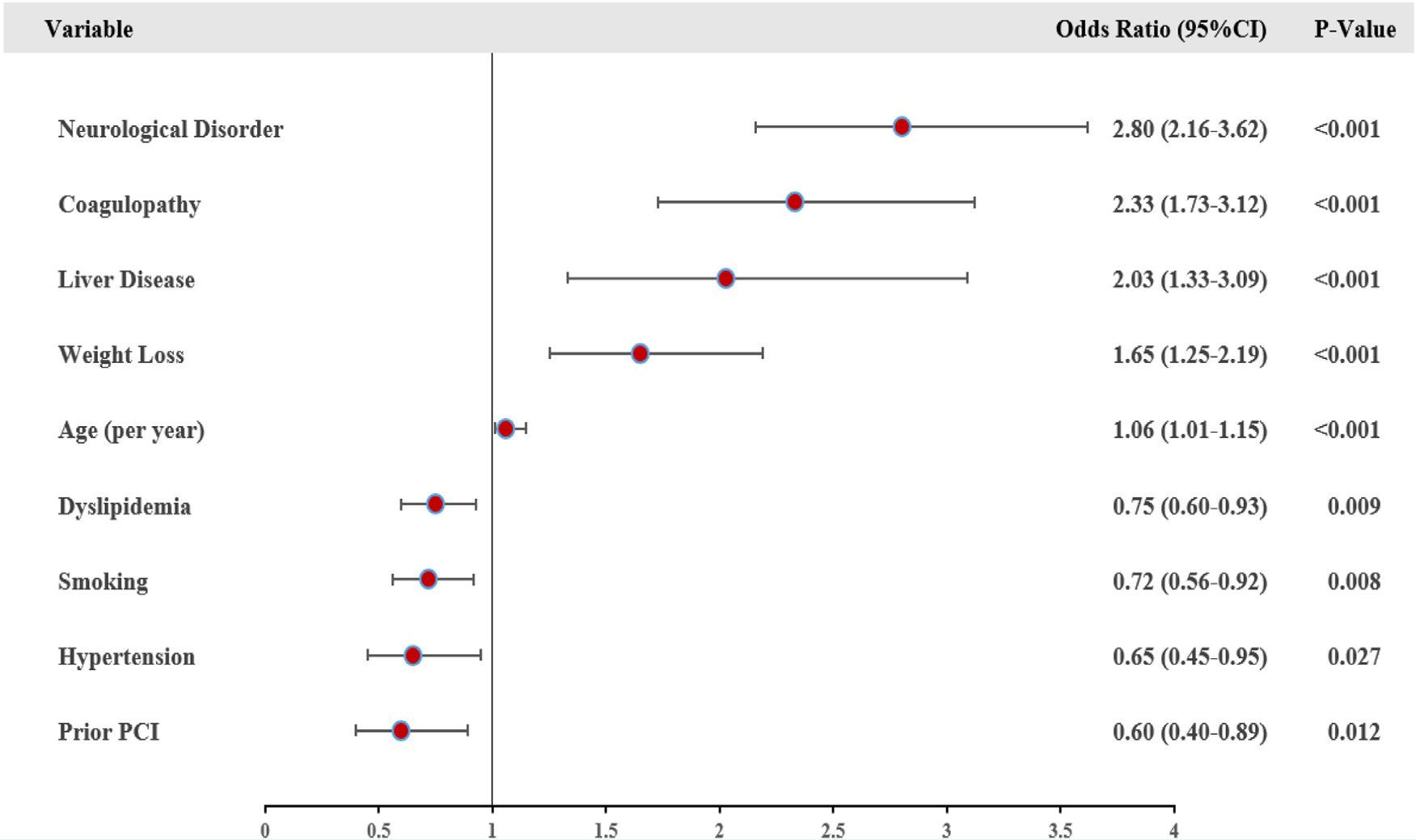
Variables associated with in-hospital mortality in patients with heart failure patients with type 2 myocardial infarction. The multivariable logistic regression model included age, sex, and clinically important baseline characteristics listed in Table 1 as covariates. PCI = percutaneous coronary intervention.
Length of Stay, Costs, and Discharge to Nursing Facility
Patients with heart failure with type 2 myocardial infarction were more likely to be discharged to a nursing facility, had longer length of stay, and higher hospital costs compared with patients without type 2 myocardial infarction (Table 2).
Table 2.
Outcomes and Resource Utilization of Heart Failure Hospitalizations with and Without Type 2 MI
| Outcomes | Type II MI |
OR (95% CI) |
P Value | ||
|---|---|---|---|---|---|
| No (n = 1,044,128) | Yes (n = 28,823) | Unadjusted | Adjusted* | ||
|
| |||||
| In-Hospital Mortality | 16,614(1.6) | 768(2.7) | 1.69(1.50–1.91) | 1.53(1.37–1.72) | <.001 |
| LOS, Days (mean [SE]) | 5(0.02) | 6(0.07) | 0.63(0.5–0.75)† | 0.53(0.42–0.64)† | <.001 |
| Hospital Costs, (mean [SE]) US$ | 10,586(96.9) | 12,545(237.1) | 1959(1538–2379)† | 1785(1388–2182)† | <.001 |
| Discharge to Nursing Facility | 201,669(19.3) | 6530(22.6) | 1.22(1.14–1.31) | 1.22(1.15–1.29) | <.001 |
| 30-day All-Cause Readmission‡ | 179,678(21.2) | 5187(22.5) | 1.08(1.03–1.14) | 1.06(1.01–1.12) | .037 |
CI = confidence interval; LOS = length of stay; MI = myocardial infarction; OR = odds ratio; SE = standard error.
Multivariate model adjusted for age, sex, admission status, and all baseline/hospital characteristics listed in Table 1.
β coefficient and corresponding 95% CI.
Among patients discharged alive.Numbers are frequency (%) unless specified otherwise.
In the subgroup analyses, predominantly similar findings were seen in patients with heart failure with type 2 myocardial infarction compared with patients without type 2 myocardial infarction irrespective of heart failure type (systolic vs diastolic), age (<75 vs ≥75 years), and gender (men v. women) (Supplementary Tables 2–4, available online).
30-Day All-Cause Readmissions
Patients with heart failure with type 2 myocardial infarction had higher a rate of 30-day readmissions compared with those without type 2 myocardial infarction (22.5% vs 21.2%; adjusted OR, 1.05; 95% CI 1.04–1.11; P = .037).
In the subgroup analysis, heart failure with type 2 myocardial infarction was associated with higher rate of 30-day readmissions irrespective of heart failure type (systolic vs diastolic, and age (<75 vs ≥75 years) (Supplementary Table 5, available online). However, in the subgroup analysis based on gender (women vs men), only women with heart failure with type 2 myocardial infarction had higher rate of 30-day readmissions compared to men (Pinteraction = .025).
After multivariable adjustment, liver disease, chronic kidney disease, chronic pulmonary disease, peripheral vascular disease, diabetes mellitus, and atrial fibrillation were independently associated with increased 30-day readmission rates among patients with heart failure with type 2 myocardial infarction (Figure 4).
Figure 4.
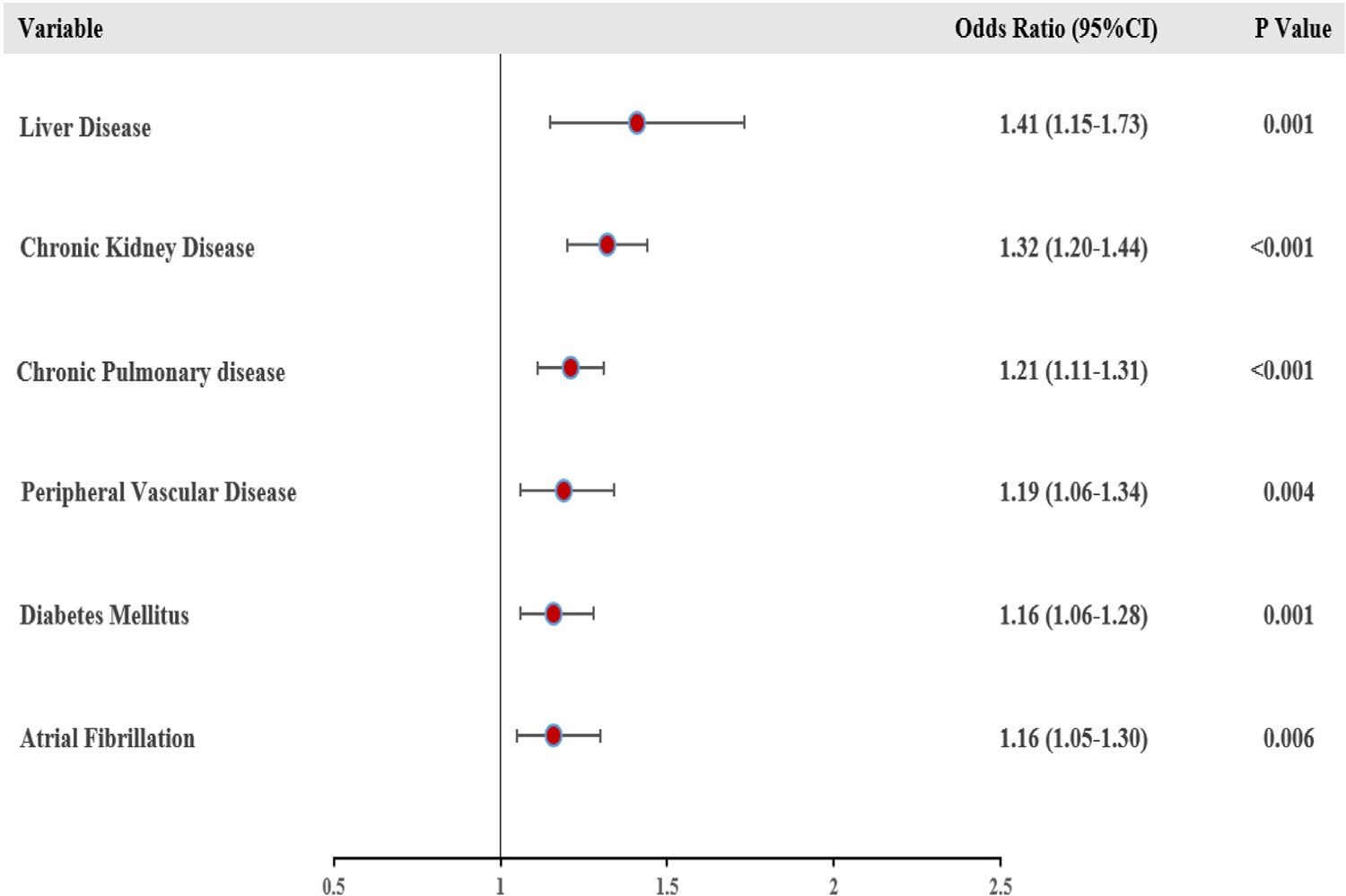
Variables associated with 30-day all-cause readmission in patients with heart failure with type 2 myocardial infarction. The multivariable logistic regression model included age, sex, and clinically important baseline characteristics listed in Table 1 as covariates.
DISCUSSION
The current study has important findings regarding the prevalence and outcomes of heart failure hospitalizations complicated with type 2 myocardial infarction. First, 2.7% of heart failure hospitalizations are associated with a type 2 myocardial infarction, and these patients are more likely to be males with a distinct profile of underlying comorbidities. Second, heart failure with type 2 myocardial infarction is associated with increased in-hospital mortality. Third, heart failure with type 2 myocardial infarction is associated with increased resource utilization (length of stay and hospital costs), and higher rates of discharge to a nursing facility and of 30-day all-cause readmission.
The overall in-hospital mortality for heart failure hospitalizations has been decreasing over the last 2 decades in the United States, from 6.1% in 2000 to 2.9% in 2014.20,21 In this study, the in-hospital mortality for patients with and without type 2 myocardial infarction was lower than previous national estimates, likely due to the exclusion of sicker patients (end-stage renal disease, cardiogenic shock, and cardiac arrest among others [Figure 1]), which are known to carry an increased risk of mortality,22,23 and possibly due to the extension of the declining trend of in-hospital mortality seen over the last 2 decades.
Scarce data exists on the outcomes of type 2 myocardial infarction in the setting of heart failure hospitalizations. In a previous study (preceding the formal introduction of the type 2 myocardial infarction ICD-10 code) from the acute decompensated heart failure national registry (ADHERE), elevated cardiac troponin in the setting of acute heart failure hospitalization was associated with 2.5-fold increased odds of in-hospital mortality.24 Our analysis extends the current literature of poor outcomes with type 2 myocardial infarction to acute heart failure hospitalizations. These findings were consistent across the subgroups analyzed. Comorbid conditions such as neurological disorders, liver disease, and weight loss were identified as independent variables associated with in-hospital mortality among patients with heart failure with type 2 myocardial infarction. Neurological disorders represent a broad category of diseases that have been established to interact with heart failure. For example, lower ejection fraction correlates with decreased gray matter density.24 Prior stroke/transient ischemic attack and confusion/somnolence at heart failure admission is associated with increased mortality among patients with heart failure.25 Similarly, liver disease caused by severe heart failure leading to congestive hepatopathy and elevated bilirubin is independently associated with increased mortality among patients with heart failure.25,26 Finally, in the Candesartan in Heart failure: Reduction in Mortality and morbidity (CHARM) study, patients with 5% or greater weight loss over 6 months had a significantly higher all-cause mortality compared to those with stable weight.27
Resource utilization remains a key aspect of heart failure with both prognostic and economic implications. In the ADHERE registry, elevated cardiac troponin during heart failure hospitalization was associated with longer intensive care unit and hospital stays.24 Longer length of stay during heart failure hospitalization is associated with higher rates of 30-day all-cause readmission and mortality.28,29 In the current study, patients who had type 2 myocardial infarction required longer hospitalization and, therefore, had increased hospital costs. Early identification of patients with type 2 myocardial infarction may allow early implementation of aggressive therapy to minimize health care resources. Nursing home discharge among patients with Medicare is associated with increased risk of readmission/ mortality following heart failure hospitalization and consequently increased economic burden.30 In a single-center study of 633 all-comer patients with type 2 myocardial infarction, the rate of discharge to a nursing facility was higher than the Medicare national average, reflecting the poor outcomes and complexity of this group of patients in accordance with our findings.31 Because heart failure is the leading cause of hospitalization for Medicare beneficiaries,1–4 identification of type 2 myocardial infarction and incorporating it in validated risk prediction models may improve risk stratification and management, such as earlier intensive treatment with diuretics and higher-level monitoring in cardiac care units, as well as allow physicians to better counsel patients regarding prognosis, treatment goals, and options.32–34
Early unplanned readmissions following heart failure are common and represent a significant component of the financial burden of heart failure care.3,4 The Centers for Medicare and Medicaid Services HRRP applies reimbursement penalties to hospitals with increased 30-day all-cause readmission for certain primary discharge diagnoses including heart failure.6,7 Since the implementation of the HRRP, the 30-day all-cause readmission for heart failure has been decreasing; however, approximately ~20% of patients still have 30-day unplanned readmissions following an index hospitalization for heart failure.3,4,35 In this study, we found similar rates of 30-day all-cause readmissions in the overall cohort (~21%) compared with previous studies. Further, patients with heart failure with type 2 myocardial infarction had a higher risk of readmission compared with those without type 2 myocardial infarction. Among patients hospitalized with heart failure, women are known to carry a higher risk of all-cause readmission compared with men.36–38 Our results extend these findings to patients with heart failure with type 2 myocardial infarction, showing higher risk of readmissions in women compared with men with type 2 myocardial infarction. In this study, diabetes mellitus, liver disease, chronic kidney disease, and chronic pulmonary disease were identified as independent predictors of 30-day all-cause readmission. In a previous study from the NRD, diabetes mellitus, chronic kidney disease, and chronic pulmonary disease were associated with a higher risk of 30-day all-cause readmission among patients with heart failure.39
Limitations
Our study has important limitations. First, the ICD-10-CM code for type 2 myocardial infarction was introduced in October 2017. Therefore, clinicians may not be familiar with using the code and miscoding practices could have occurred. In a prior single-center study, only ~60% of the patients were correctly classified as type 2 myocardial infarction based on the fourth-universal definition of myocardial infarction and the rest were mainly classified as myocardial injury.40 Therefore, we excluded potential major causes of acute/chronic myocardial injury (Figure 1). Nevertheless, this code has been previously used in multiple studies of type 2 myocardial infarction from the administrative databases.16–18 Second, the NRD is an administrative database, and hence prone to miscoded/missing dataset, lacks granularity, and robust adjudication of clinical outcomes. Third, since this is a retrospective observational study, we cannot exclude the possibility of unmeasured confounders influencing the results despite our rigorous multivariate adjustment. In addition, the database does not contain information on important variables such as echocardiographic results, biomarkers, laboratory variables, and treatments at discharge. We were therefore unable to adjust for these variables. Fourth, the subgroup analysis is prone to its inherent limitations, such as false-positives due to multiple comparisons and false-negative due to inadequate power. Last, the NRD lacks long-term follow-up data, and thus, we were unable to establish the impact of type 2 myocardial infarction on long-term outcomes.
CONCLUSIONS
The results from this analysis provide clarity regarding the prevalence and risk profile of hospitalized patients with heart failure with type 2 myocardial infarction. Heart failure hospitalizations with type 2 myocardial infarction are associated with increased in-hospital mortality, resource utilization, and 30-day all-cause readmissions compared with heart failure hospitalizations without type 2 myocardial infarction. Currently, there is a lack of consensus regarding treatment for patients with type 2 myocardial infarction. In addition, less than two-thirds of patients with type 2 myocardial infarction are evaluated by a cardiologist in the hospital.41,42 Therefore, there remains an unmet need to improve clinical outcomes for this high-risk group of patients. Further studies are needed to assess the long-term outcomes and management strategies for heart failure with type 2 myocardial infarction.
Supplementary Material
CLINICAL SIGNIFICANCE.
A total of 2.7% of patients with heart failure had type 2 myocardial infarction.
Patients with type 2 myocardial infarction were more likely to be males with a distinct profile of underlying comorbidities.
Patients with heart failure with type 2 myocardial infarction had higher in-hospital mortality and resource utilization compared to their counterparts without type 2 myocardial infarction.
Patients with heart failure with type 2 myocardial infarction had higher rates of 30-day all-cause readmission.
Footnotes
Conflicts of Interest: AN reports serving on the advisory panels of Medtronic, Pfizer, and Myokardia. AN, AMKM, ISK, RWA, GVM, JCPG, SF, BB, and HJ report none.
References
- 1.Chang PP, Wruck LM, Shahar E, et al. Trends in hospitalizations and survival of acute decompensated heart failure in four us communities (2005–2014): ARIC study community surveillance. Circulation 2018;138(1):12–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ziaeian B, Heidenreich PA, Xu H, et al. Medicare Expenditures by race/ethnicity after hospitalization for heart failure with preserved ejection fraction. JACC Heart Fail 2018;6(5):388–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jackson SL, Tong X, King RJ, Loustalot F, Hong Y, Ritchey MD. National burden of heart failure events in the United States, 2006 to 2014. Circ Heart Fail 2018;11(12):e004873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zohrabian A, Kapp JM, Simoes EJ. The economic case for US hospitals to revise their approach to heart failure readmission reduction. Ann Transl Med 2018;6(15); . Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6123214/. [Accessed December 28, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail 2013;6(3):606–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Medicare & Medicaid Services. Hospital Readmissions Reduction Program (HRRP). Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program. Accessed December 28, 2020.
- 7.Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the Hospital Readmissions Reduction Program with mortality among medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. JAMA 2018;320 (24):2542–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation 2018;138(20):e618–51. [DOI] [PubMed] [Google Scholar]
- 9.McCarthy CP, Vaduganathan M, Singh A, et al. Type 2 myocardial infarction and the Hospital Readmission Reduction Program. J Am Coll Cardiol 2018;72(10):1166–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeFilippis AP, Chapman AR, Mills NL, et al. Assessment and treatment of patients with type 2 myocardial infarction and acute nonischemic myocardial injury. Circulation 2019;140(20):1661–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chapman AR, Shah ASV, Lee KK, et al. Long-term outcomes in patients with type 2 myocardial infarction and myocardial injury. Circulation 2018;137(12):1236–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arora S, Strassle PD, Qamar A, et al. Impact of type 2 myocardial infarction (mi) on hospital-level mi outcomes: implications for quality and public reporting. J Am Heart Assoc 2018. Mar 26;7(7):e008661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Healthcare Cost and Utilization Project (HCUP). National Readmissions Database Overview. Available at: https://www.hcup-us.ahrq.gov/nrdoverview.jsp. Accessed December 28, 2020.
- 14.Agarwal MA, Fonarow GC, Ziaeian B. National trends in heart failure hospitalizations and readmissions from 2010 to 2017 [e-pub ahead of print]. JAMA Cardiol. doi: 10.1001/jamacardio.2020.7472. Accessed month day, year. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khera R, Wang Y, Bernheim SM, Lin Z, Krumholz HM. Post-discharge acute care and outcomes following readmission reduction initiatives: national retrospective cohort study of Medicare beneficiaries in the United States. BMJ 2020;368:l6831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCarthy CP, Kolte D, Kennedy KF, Vaduganathan M, Wasfy JH, Januzzi JL. Patient characteristics and clinical outcomes of type 1 versus type 2 myocardial infarction. J Am Coll Cardiol 2021;77(7):848–57. [DOI] [PubMed] [Google Scholar]
- 17.Mohamed MO, Contractor T, Abramov D, et al. Sex-based differences in prevalence and outcomes of common acute conditions associated with type 2 myocardial infarction. Am J Cardiol 2021;147:8–15. [DOI] [PubMed] [Google Scholar]
- 18.Nazir S, Hahn J, Minhas AM, et al. Association of Type 2 myocardial infarction with outcomes and resource utilization in patients undergoing endovascular transcatheter aortic valve replacement [e-pub ahead of print]. Cardiovasc Revasc Med. doi: 10.1016/j.carrev.2021.03.006. Accessed month day, year [DOI] [PubMed] [Google Scholar]
- 19.Healthcare Cost and Utilization Project (HCUP). Checklist for Working with the NRD. Available at: https://www.hcup-us.ahrq.gov/db/nation/nrd/nrdchecklist.jsp. Accessed January 6, 2021.
- 20.Krumholz HM, Normand S-LT, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999–2011. Circulation 2014;130(12):966–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akintoye E, Briasoulis A, Egbe A, et al. National trends in admission and in-hospital mortality of patients with heart failure in the United States (2001–2014). J Am Heart Assoc 2017;6(12):e006955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lemor A, Hernandez GA, Lee S, et al. Impact of end stage renal disease on in-hospital outcomes of patients with systolic and diastolic heart failure (insights from the Nationwide Inpatient Sample 2010 to 2014). Int J Cardiol 2018;266:174–9. [DOI] [PubMed] [Google Scholar]
- 23.Yandrapalli S, Sanaani A, Harikrishnan P, et al. Cardiogenic shock during heart failure hospitalizations: age-, sex-, and race-stratified trends in incidence and outcomes. Am Heart J 2019;213:18–29. [DOI] [PubMed] [Google Scholar]
- 24.Peacock WF, De Marco T, Fonarow GC, et al. Cardiac troponin and outcome in acute heart failure. N Engl J Med 2008;358(20):2117–26. [DOI] [PubMed] [Google Scholar]
- 25.Xanthopoulos A, Starling RC, Kitai T, Triposkiadis F. Heart failure and liver disease: cardiohepatic interactions. JACC Heart Fail 2019;7 (2):87–97. [DOI] [PubMed] [Google Scholar]
- 26.Allen LA, Felker GM, Pocock S, et al. Liver function abnormalities and outcome in patients with chronic heart failure: data from the Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity (CHARM) program. Eur J Heart Fail 2009;11(2):170–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pocock SJ, McMurray JJV, Dobson J, et al. Weight loss and mortality risk in patients with chronic heart failure in the candesartan in heart failure: assessment of reduction in mortality and morbidity (CHARM) programme. Eur Heart J 2008;29(21):2641–50. [DOI] [PubMed] [Google Scholar]
- 28.Reynolds K, Butler MG, Kimes TM, Rosales AG, Chan W, Nichols GA. Relation of acute heart failure hospital length of stay to subsequent readmission and all-cause mortality. Am J Cardiol 2015;116 (3):400–5. [DOI] [PubMed] [Google Scholar]
- 29.Sud M, Yu B, Wijeysundera HC, et al. Associations between short or long length of stay and 30-day readmission and mortality in hospitalized patients with heart failure. JACC Heart Fail 2017;5(8):5785–8. [DOI] [PubMed] [Google Scholar]
- 30.Allen LA, Hernandez AF, Peterson ED, et al. Discharge to a skilled nursing facility and subsequent clinical outcomes among older patients hospitalized for heart failure. Circ Heart Fail 2011;4(3):293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCarthy CP, Murphy S, Rehman S, et al. Home-time after discharge among patients with type 2 myocardial infarction. J Am Heart Assoc 2020;9(10):e015978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mueller K, Thiel F, Beutner F, et al. Brain damage with heart failure: cardiac biomarker alterations and gray matter decline. Circ Res 2020;126(6):750–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fonarow GC. Epidemiology and risk stratification in acute heart failure. Am Heart J 2008;155(2):200–7. [DOI] [PubMed] [Google Scholar]
- 34.Matsue Y, Damman K, Voors AA, et al. Time-to-furosemide treatment and mortality in patients hospitalized with acute heart failure. J Am Coll Cardiol 2017;69(25):3042–51. [DOI] [PubMed] [Google Scholar]
- 35.Blecker S, Herrin J, Li L, Yu H, Grady JN, Horwitz LI. Trends in hospital readmission of medicare-covered patients with heart failure. J Am Coll Cardiol 2019;73(9):1004–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O’Brien C, Valsdottir L, Wasfy JH, et al. Comparison of 30-day readmission rates after hospitalization for acute myocardial infarction in men versus women. Am J Cardiol 2017;120(7):1070–6. [DOI] [PubMed] [Google Scholar]
- 37.Shah RU, Tsai V, Klein L, Heidenreich PA. Characteristics and outcomes of very elderly patients after first hospitalization for heart failure. Circ Heart Fail 2011;4(3):301–7. [DOI] [PubMed] [Google Scholar]
- 38.García-Pérez L, Linertova R, Lorenzo-Riera A, Vazquez-Dıaz JR, Duque-Gonzalez B, Sarrıa-Santamera A. Risk factors for hospital readmissions in elderly patients: a systematic review. QJM 2011;104 (8):639–51. [DOI] [PubMed] [Google Scholar]
- 39.Arora S, Patel P, Lahewala S, et al. Etiologies, trends, and predictors of 30-day readmission in patients with heart failure. Am J Cardiol 2017;119(5):760–9. [DOI] [PubMed] [Google Scholar]
- 40.McCarthy C, Murphy S, Cohen JA, et al. Misclassification of myocardial injury as myocardial infarction: implications for assessing outcomes in value-based programs. JAMA Cardiol 2019;4(5):460–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sandoval Y, Jaffe AS. Type 2 myocardial infarction: JACC review topic of the week. J Am Coll Cardiol 2019;73(14):1846–60. [DOI] [PubMed] [Google Scholar]
- 42.McCarthy CP, Olshan DS, Rehman S, et al. Cardiologist evaluation of patients with type 2 myocardial infarction. Circ Cardiovasc Qual Outcomes 2021;14(1):e007440. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


