Abstract
Background and aim
The use of endoluminal flow diversion in bifurcation aneurysms has been questioned due to the potential for complications and lower occlusion rates. In this study we assessed outcomes of endovascular treatment of intracranial sidewall and bifurcation aneurysms with flow diverters
Methods
In July 2020, a literature search for all studies utilizing endoluminal flow diverter treatment for sidewall or bifurcation aneurysms was performed. Data were collected from studies that met our inclusion/exclusion criteria by two independent reviewers and confirmed by a third reviewer. Using random-effects meta-analysis the target outcomes including overall complications (hematoma, ischemic events, minor ischemic stroke, aneurysm rupture, side vessel occlusion, stenosis, thrombosis, transient ischemic stroke, and other complications), perioperative complications, and follow-up (long-term) aneurysm occlusion were intestigated.
Results
Overall, we included 35 studies with 1084 patients with 1208 aneurysms. Of these aneurysms, 654 (54.14%) and 554 (45.86%) were classified as sidewall and bifurcation aneurysm, respectively, based on aneurysm location. Sidewall aneurysms had a similar total complication rate (R) of 27.12% (95% CI, 16.56%–41.09%), compared with bifurcation aneurysms (R, 20.40%, 95% CI, 13.24%–30.08%) (p = 0.3527). Follow-up angiographic outcome showed comparable complete occlusion rates for sidewall aneurysms (R 69.49%; 95%CI, 62.41%–75.75%) and bifurcation aneurysms (R 73.99%; 95% CI, 65.05%–81.31%; p = 0.4328).
Conclusions
This meta-analysis of sidewall and bifurcation aneurysms treated with endoluminal flow diverters demonstrated no significant differences in complications or occlusion rates. These data provide new information that can be used as a benchmark for comparison with emerging devices for the treatment of bifurcation aneurysms.
Keywords: Brain ischemia, stroke, aneurysm, ruptured, thrombosis
Introduction
Intracranial aneurysms affect approximately 2% of the United States population, 1 of which approximately 40% are bifurcation aneurysms. 2 Bifurcation aneurysms are associated with many challenges stemming from aneurysm morphology, location, and adverse hemodynamic environment, as well as the fundamental difficulty of placing a cylindrical device to cover an aneurysmal neck centered at the flow divider of a bifurcation. Several studies have reported that intracranial aneurysm hemodynamics are influenced by aneurysm location and that bifurcation aneurysms have more hemodynamic complexities than sidewall aneurysms.3–6
Endoluminal flow diverters have been introduced to successfully treat intracranial aneurysms, particularly sidewall aneurysms.7–10 However, flow diverters may be associated with serious complications in a bifurcation context since they cover both the aneurysm neck and the side branch. Studies have reported serious complications associated with flow diverter-treated aneurysms such as thromboembolism, side branch occlusion, in-stent thrombosis, and intracranial hemorrhage.11–19 In addition, complete aneurysm occlusion following treatment with flow diverters can take up to 5 years following the procedure, thus leaving the aneurysm unprotected and at risk of rupture.14,15
In this study, we performed a systematic review and meta-analysis of studies reporting complication outcomes, perioperative complications, and complete aneurysm occlusion rates in patients with sidewall or bifurcation aneurysms treated with endoluminal flow diverters. We aimed to 1) compare whether the use of endoluminal flow diverters in bifurcation group is associated with safety and efficacy outcomes than sidewall group, and 2) provide data against which current and future innovative devices for intracranial aneurysms can be compared.
Methods
Literature search
The current study adheres to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. We performed a comprehensive literature search through July 2020. Several databases including PubMed, Ovid MEDLINE, and Ovid EMBASE were used to identify relevant articles we searched for studies presenting baseline characteristics and safety outcomes for treatment of intracranial aneurysms by flow diverters to locate relevant studies using predefined search criteria. Search terms included any of the following keywords alone or in combination: “flow diverter”, “flow diversion”, “aneurysm”, “sidewall”, “bifurcation”, “intracranial”, “FRED”, “Surpass”, “SILK”, “PED”, “p64”.
All studies presenting data regarding treatment of aneurysms by flow diverters were screened. Studies were then filtered down to those presenting outcome data from treatment of intracranial aneurysms occurring in “sidewall” or “bifurcation” locations.
Study eligibility
The inclusion criteria for studies in the analysis were: all studies including human subjects, regardless of age or sex; studies including at least 5 patients; studies that were classified as retrospective, prospective, and randomized clinical trials; and studies reporting complications of sidewall aneurysms and bifurcation aneurysms treated with flow diverters separately and without using coils. The exclusion criteria were: studies classified as abstracts, reviews, secondary publications, letters, and editorials; studies that did not differentiate outcomes based on bifurcation or sidewall locations; studies that reported intrasaccular flow diversion only; studies that combined the locations of interest of this study and other locations; in vivo animal studies or in vitro studies; case reports; and studies not reported in the English language.
Data collection and outcome
Two researchers independently scanned all manuscripts and performed data extraction. All retrieved studies were examined, and any overlapping data were omitted. A third experienced reviewer examined all the data and recon ciliated any events of discrepancies of data extraction after further extensive review of the full text articles. We used previously reported definition to discriminate between sidewall and bifurcation aneurysms. In brief, bifurcation aneurysyms were defined as aneurysms which were located at a major bifurcation in cerebral vasculture. Sidewall aneurysms were defined as aneurysms which originate from only one parent vessel or from the origin of a branch that was much smaller than the parent artery. 6 In a case of duplication or overlapping study population (studies published on the same registry), studies with the largest patients’ population or the most amount of data relevant to our outcome were selected. The following data were collected for each eligible investigation: authors, year of publication; nature of study (retrospective or prospective); device used; aneurysm type (sidewall or bifurcation); number of patients, number of aneurysms; patients demographics, perioperative complications; and other complications, complete aneurysm occlusion rates, and device placement success.
Statistical analysis
Total, perioperative, and individual complication rates were separated into a sidewall and a bifurcation aneurysm sample. When individual complication rates were too sparse to analyze individually, they were pooled into a single group called “other complications.” These “other complications” included increased mass effect, transient deficit, asymptomatic internal carotid artery (ICA) dissection, monocular blindness, transient numbness, edema, bleeding complications, device occlusion, headache, gastrointestinal (GI) bleed, extravasation in the subarachnoid space, facial palsy, dissection flap, gum bleeding, hemiparesis, neurologic complications, generalized tonic-clonic seizure, lower extremity thrombus, injury to the profunda, femoris, hemiplegia, transient monopoiesis of right upper limb, diminished flow in side vessel, transient left face weakness/left arm drift, transient worsening of opthalmoparesis, aneurysm recurrence, left eye blindness, easy bruising, aphasia, permanent visual complications, vasospasm, extremity weakness, epistaxis, persistent hydrocephalus, retroperitoneal bleeding, hypotension, superficial, and skin abscess at the femoral puncture site.
Sidewall aneurysm- and bifurcation aneurysm-specific complications were compared using a random effects meta-analysis. We applied meta-regression using a restricted effects maximum-likelihood estimator to identify moderators that significantly impacted study complication rates. The following moderators were considered: 1) number of aneurysms per study population, 2) mean aneurysm diameter, 3) mean follow-up period, 4) nature of study (retrospective or prospective), 5) device placement success rate, 6) device used, and 7) complete occlusion rates according to Raymond-Roy occlusion classification (class I), 20 or O'Kelly-Marotta grading scale (Grade D). 21 The impact of small study bias was depicted visually using funnel plots and testing their symmetry and analyzed using Egger’s regression. 22 Raw event rates for each complication type were also computed. The percentage of heterogeneity that was unattributable due to sampling error was evaluated by I2 statistics. 23 For the evaluation of occlusion rates, a random effects model without moderators was performed. In all cases, p-values <0.05 were considered significant. Statistics were performed using RStudio (Version 1.2.5033) and using the metafor package.
Results
Literature search
A systematic search resulted in 3,629 studies. After excluding 1,783 duplicates, non- English studies, case reports, and meta-analyses/reviews, 1,846 studies were screened by abstracts, resulting in the exclusion of 1,455 studies. The full texts of the remaining 391 studies were assessed to identify the presence of any exclusion criteria and evaluation of aneurysm location. The final meta-analysis included 35 eligible studies with 1,084 patients. Supplementary Figure 1 represents a PRISMA flow chart of the search and selection process of the articles.
The 35 included studies and baseline patient demographics are shown in supplementary Table 1. Of these, 30 were retrospective and 5 were prospective studies. The mean patient age across the studies ranged from 42 years 24 to 63.4 years. 25 The largest study had 97 patients, 26 while the smallest study had 6 patients. 27
Table 1 shows baseline characteristics of aneurysms. Among the 1,084-patient population, 597 (55%) patients were treated for sidewall aneurysms and 487 (44.93%) were treated for bifurcation aneurysms. The total number of aneurysms treated was 1,208, of which 654 (54%) were sidewall aneurysms and 554 (46%) were bifurcation aneurysms.
Table 1.
Baseline characteristics of sidewall and bifurcation aneurysms.
| References | Flow diverter | Aneurysms (n) | Aneurysm morphology (n) | Mean/median aneurysm diameter (mm) | Aneurysm location (n) |
|---|---|---|---|---|---|
| Sidewall aneurysms | |||||
| Enriquez-Marulanda et al. 28 | PED | 21 | Fusiform (2), Saccular (19) | 4.9 | ICA: C7 (communicating/terminal) (21) |
| Brinjikji et al. 29 | PED | 15 | – | 13 | ICA (1), Paraclinoid (3), Anterior choroidal (1), Posterior Communicating (8), ICA terminus (2) |
| Mazur et al. 30 | PED | 11 | Fusiform (9), Saccular (2) | 8.5 | V4 segment (11) |
| Chalouhi et al. 26 | PED | 95 | Fusiform (7), Saccular (88) | 8 | ICA: C4 segment (cavernous) (7), ICA: C6 (ophthalmic) (54), Paraclinoid (29), Posterior Communicating (4) |
| Corley et al. 31 | PED | 9 | Dissecting (9) | 10.6 | V4 segment (9) |
| Dmytriw et al. 32 | PED, FRED | 16 | Saccular (15), Blister (1) | 20.2 | Basilar apex (16) |
| Nossek et al. 33 | PED | 11 | – | – | ICA bifurcation (4), Anterior choroidal (3), Posterior Communicating (3) |
| Cerejo et al. 34 | PED/PFLEX | 8 | Blister (8) | 2.6 | ICA: Supraclinoid (7), ACA: A1 segment (1) |
| Oishi et al. 25 | PED | 100 | – | 16.9 | ICA: C1 segment (cervical) (51), ICA: C2 segment (petrous) (4), ICA: C3 segment (lacerum) (45) |
| Chalouhi et al. 35 | PED | 8 | Blister (8) | 2.5 | ICA (7), Basilar (1) |
| Mokin et al. 36 | PED/multiple devices | 45 | Blister (45) | 2.4 | ICA: Supraclinoid (45) |
| Cinar et al. 37 | PED | 7 | Blister (7) | – | ICA (7), ICA: Supraclinoid (7) |
| Adeeb et al. 38 | PED | 106 | – | 6.4 | ICA: C4 segment (cavernous) (4), ICA: C6 (ophthalmic) (81), Superior hypophyseal (21) |
| Roy et al. 39 | PED | 73 | – | – | ICA (23), Posterior Communicating (50) |
| Tanweer et al. 40 | PED | 43 | – | 24.3 | ICA (43), ICA: C4 segment (cavernous) (43) |
| Puffer et al. 10 | PED/SILK/Surpass/multiple devices | 44 | – | 20.9 | ICA: C4 segment (cavernous) (44), |
| Lanzino et al. 41 | PED | 22 | – | 14.9 | ICA (22), ICA: C4 segment (cavernous) (9), ICA: C6 (ophthalmic) (12), Superior hypophyseal (1) |
| Puffer et al. 42 | PED | 20 | – | – | ICA (20), ICA: C4 segment (cavernous) (2), ICA: C6 (ophthalmic) (7), Paraclinoid (6), Superior hypophyseal (1) |
| Bifurcation aneurysms | |||||
| Brasiliense et al. 43 | PED | 117 | – | 7.8 | ICA (117), ICA: C4 segment (cavernous) (26), ICA: C6 (ophthalmic) (37), Paraclinoid (8), Superior hypophyseal (25), Anterior choroidal (3), Posterior Communicating (15) |
| Colby et al. 44 | PED | 50 | – | 4.5 | A1-A2 (15), Anterior communicating (26) |
| Lin et al. 27 | PED | 6 | – | 5.1 | Posterior Communicating (2), Anterior communicating (4) |
| Zanaty et al. 45 | PED | 10 | Fusiform (7), Saccular (3) | – | MCA (10) |
| Caroff et al. 46 | PED/SILK/FRED | 15 | – | 6.1 | MCA bifurcation (15) |
| Gawlitza et al. 47 | PED/SILK/FRED | 18 | – | 6.9 | MCA bifurcation (13), Anterior communicating (5) |
| Pujari et al. 48 | PED | 10 | Fusiform (5), Saccular (5) | 14.7 | ICA terminus (10) |
| Yavuz et al. 49 | PED | 25 | – | – | MCA (25), MCA bifurcation (21) |
| Dabus et al. 50 | PED | 20 | Fusiform (5), Saccular (15) | 7.3 | ACA: A1 segment (1), ACA: A2 segment (4), Pericallosal (2) |
| Ravindran et al. 51 | PED/FRED | 46 | Fusiform (19), Saccular (27) | 10.9 | PCA (12), P1-P2 PCA (1), MCA (26), MCA: M1 segment (14), ACA (8), A2 (2), A1-A2 junction (1), ACA: A1 segment (2), Pericallosal (3) |
| Primiani et al. 52 | PED | 65 | Fusiform (19), Saccular (38), Dissecting (8) | 7.8 | PCA (12), MCA (29), ACA (24), A2 (8), A3 (16) |
| Lin et al. 53 | PED | 28 | Fusiform (15), Saccular (8), Dissecting (5) | 12.3 | MCA (20), MCA: M1 segment (12), ACA (6), A2 (2), A3 (2), A1-A2 junction (1), ACA: A1 segment (1), Anterior communicating (2) |
| Lin et al. 54 | PED | 9 | Fusiform (3), Saccular (5), Dissecting (1) | 8.3 | ICA (2), Posterior Communicating (3), ICA terminus (2), ACA (5), ACA: A1 segment (4) |
| Daou et al. 55 | PED | 30 | Fusiform (4), Saccular (26) | 7.2 | Posterior Communicating (30) |
| Pistocchi et al. 9 | PED/SILK | 30 | Fusiform (7), Saccular (21), Blister (2) | 6.8 | PCA (1), MCA (8), MCA: M1 segment (2), ACA: A1 segment (1), ACA: A2 segment (1), Pericallosal (3), Anterior communicating (16) |
| Saleme et al. 56 | PED | 37 | Saccular (31), Dissecting (6) | 5.1 | MCA (19), ICA (4), ACA: A1 segment (2), Pericallosal-callosomarginal junction (3), Communicating artery complex (11) |
| Primiani et al. 57 | PED | 38 | – | 6.8 | ICA (38), ICA: C6 (ophthalmic) (38) |
Heterogeneity
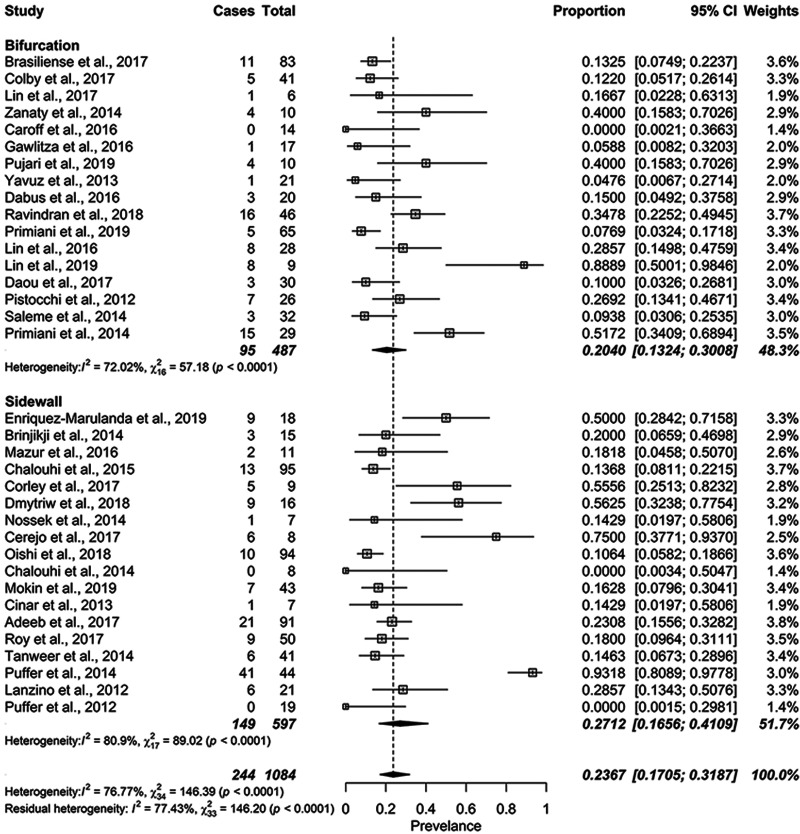
Overall complication rates had substantial heterogeneity that was unattributable to sampling error (I2=81.69%, p < 0.0001). For complication subgroup analyses, I2 values were 81.90% (p < 0.0001) for the sidewall aneurysm group and 72.02% (p < 0.0001) for the bifurcation aneurysm group (Figure 1). For perioperative complication rates, I2 values were 48.37% (p = 0.08) for the sidewall aneurysm group and 19.53% (p = 0.2692) for the bifurcation aneurysm group (Figure 2). For overall complete occlusion rate, the I2 value was 52.41% (p = 0.0025). The P-values for publication bias using Egger’s regression were higher than 0.05 suggesting no bias.
Figure 1.
Forest plot for total complication rates by aneurysm type.
Figure 2.
Forest plot for perioperative complication rates by aneurysm type.
Safety outcomes
Of the included studies, there was sufficient data for the comparison between sidewall and bifurcation aneurysms groups for the following complications; frequencies of hematomas, ischemic events, minor ischemic stroke, rupture, side vessel occlusion, stenosis, thrombosis, TIA-stroke, and hemorrhagic events. All other individual complications were aggregated as “other complications” and compared between the sidewall and bifurcation aneurysm groups.
We then determined whether there were any moderators that could predict the overall complication rates. Based on our meta-regression analysis, none of the moderators we evaluated (aneurysms per study population, complete occlusion rates, device type, mean aneurysm diameter, mean follow-up, placement success rates, and study type) showed to be significant independent predictors of overall complication rates. These data are summarized in Table 2. As such, we proceeded with a random effects model with aneurysm type (sidewall or bifurcation) as the only subgroup analysis.
Table 2.
Potential moderators of complication rates.
| Variable | Log Odds | Standard Error | z-value | p-value |
|---|---|---|---|---|
| Aneurysms per patient | –1.4540 | 1.4717 | –0.9980 | 0.3232 |
| Complete occlusion rate | –0.6648 | 1.5738 | –0.4224 | 0.6732 |
| PED vs. multiple devices | –0.4394 | 0.4139 | –1.0617 | 0.2884 |
| Mean aneurysm diameter | 0.0633 | 0.0409 | 1.5459 | 0.1221 |
| Mean follow-up | 0.0510 | 0.6650 | 0.7667 | 0.4433 |
| Placement success rate | 5.4133 | 8.6956 | 0.6225 | 0.5336 |
| Study type | –0.8198 | 0.5813 | –1.4103 | 0.1584 |
The overall total complication rate (R) for flow diverter treatment of sidewall and bifurcation aneurysms was 24%. The sidewall aneurysm group had an overall total complication rate of 27, which was similar to the rate recorded for bifurcation aneurysm group (R, 20.40%, 95% CI, 13.24%–30.08%; p = 0.3527) (Figure 1 and supplementary Table 2). It is important to note, however, that we identified one highly influential study within the sidewall aneurysm group by Puffer and colleagues that significantly impacted the total complication rate based on our outlier analysis (external standardized residual = 3.6797). 10 This study reported a high complication rate in sidewall aneurysms compared to other studies in the same group, and compared with studies included in bifurcation aneurysm studies (Figure 1).
The overall perioperative complication rate for flow diverter treatment of sidewall and bifurcation aneurysms was 15.91%. The overall perioperative complication rate for the sidewall aneurysm group (R, 22.27%; 95% CI, 11.89%–37.81%) was not significantly different from the rate of bifurcation aneurysm group (R, 13.08%; 95% CI, 8.98%–18.66%) (p = 0.0884) (Figure 2 and supplementary Table 2).
Pooled complication rates for each of the individual complications collected are presented in supplementary Figure 2 and supplementary Table 2. There was no significant difference between the sidewall and bifurcation aneurysm groups for any of the individual complications (p > 0.05).
Efficacy outcomes
Data regarding complete occlusion rate were available for 750/1,208 (62%) aneurysms. The sidewall aneurysm group had data regarding complete occlusion for 409/654 (62%) aneurysms while the bifurcation aneurysm group had data for 341/554 (62%) aneurysms. Data regarding near complete occlusion rate was available for 411/1,208 (34%). The sidewall aneurysm group had data regarding near complete occlusion for 191/654 (29%) aneurysms. while the bifurcation aneurysm group had data for 220/554 (40%) aneurysms. Data regarding incomplete occlusion rate was available for 542/1,208 (45%) aneurysms treated. The sidewall aneurysm group had data regarding incomplete occlusion for 322/654 (49%) aneurysms while the bifurcation aneurysm group had data for 220/554 (40%) aneurysms.
The overall complete occlusion rate for flow diverter treatment of sidewall and bifurcation aneurysms was 71.91% .The overall complete occlusion rates were similar in the sidewall aneurysm group (R 69.49%; 95%CI, 62.41%–75.75%) and bifurcation aneurysm group (R 73.99%; 95% CI, 65.05%–81.31%; p = 0.4328). Similarly, there was no significant difference between the two aneurysm groups for near complete occlusion rates (p = 0.87) and incomplete occlusion rates (p = 0.68). Details about occlusion rates are summarized in supplementary Figure 3, supplementary Table 2, and supplementary Table 3.
Discussion
Our meta-analysis including 35 studies and 1,208 aneurysms (654 sidewall aneurysm group and 554 bifurcation aneurysm group) treated with flow diverters illustrated that treatment with flow diverters have comparable complications and occlusion rates in bifurcation and sidewall aneurysms. In addition, both groups of aneurysms had relatively high long-term complete occlusion rates of 69.49% (95% CI: 62.41–75.75%) for the sidewall group and 73.99% (95% CI: 65.05–81.31%) for the bifurcation group). Our findings show that, despite concerns that flow diverters would produce higher complications in bifurcation contexts, the treatment outcomes across indicate no differences in complication rates.
Several studies have reported that intracranial aneurysm hemodynamics are influenced by aneurysm location and that bifurcation aneurysms have more hemodynamic complexities than sidewall aneurysms.3–6 For instance, by using computational fluid dynamics (CFD), bifurcation aneurysms were found to be associated with rupture status of very small intracranial aneurysm and that there was a significant difference in hemodynamic measurements between ruptured and unruptured aneurysms. 4 Valen-Sendstad & Steinman used high-and normal-resolution CFD simulations in a sample of 12 anatomically realistic MCA aneurysms (4 sidewall and 12 bifurcation aneurysms). The results showed a high-frequency velocity fluctuation on bifurcation aneurysms, but not sidewall aneurysms. 5 Furthermore, Baharoglu and colleagues used CFD in sidewall and bifurcation generic aneurysm models and showed a remarkable differences in morphologic and hemodynamic dichotomy between sidewall aneurysms and bifurcation aneurysms. 6 As hemodynamics influence both occlusion and complications, we aimed to evaluate whether treatment with flow diverters of bifurcation aneurysms would be less safe and less effective than treatment of side wall aneurysms. However, our results did not support a presence of any significant difference between the two aneurysm groups in the development of complications or aneurysm occlusion.
Several endovascular treatments are now available to treat bifurcation aneurysms including stent-assisted coiling (SAC), endoluminal flow diverters, intrasaccular flow diverters such as Woven EndoBridge (WEB), and new neck bridging devices such as PulseRider and pCONUS. Endovascular treatment of bifurcation aneurysms, especially those with wide necks, requires the use of adjunctive devices along with coiling to decrease the possibility of coil herniation into the parent artery, which might decrease the rates of complete aneurysm occlusion. 58
Our results corroborate the safety and efficacy findings of endoluminal flow diverter studies outside of our meta-analysis. In a study that included 14 patients with bifurcation in the middle cerebral artery, the morbidity rate was over 20% and complete occlusion rate was 62%. 46 In the Pipeline for Uncoilable or Failed Aneurysms (PUFS) clinical trial including over 100 patients with large and giant wide-neck internal carotid artery aneurysm, the complete occlusion rate was 87% at 12-months. 59 A systematic review and meta-analysis containing 29 studies that described 3–6 months of follow-up data for flow diverter treatment of various kinds of intracranial aneurysms in 1,524 patients, reported an overall technical failure and complication rate of 9.3%, with a 14% rate of procedure-related complication and 6.6% rate of morbidity and mortality. 60
SAC has been used over the past two decades to treat bifurcation aneurysms due to the continuous advent of improved stents. Recently, a systematic review that evaluated the outcome of SAC treatment of 702 wide-neck aneurysms reported a long-term complete occlusion rate of 72%. 58 A recent retrospective study of 659 patients with 670 brain aneurysms (88.8% wide-neck aneurysms) evaluated the efficacy and safety of the Neuroform, Enterprise, and Low-profile Visualized Intraluminal Support (LVIS) stents. 61 Long-term (mean 10.5 months) complete occlusion rate ranged from 78% to 84%, while intra-procedural complications and post-procedural-related complication rates were 7% and 11.5%, respectively. In many instances with wide-neck bifurcation aneurysms, multiple-stent reconstruction such as Y-stenting techniques, which provides support for coil and protection of parent and branch arteries,62,63 might be required. A meta-analysis of 27 studies and 750 aneurysms reported overall treatment-related complications and periprocedural/early complication rates of 8.9% and 6.7%, respectively, and long-term adequate occlusion rate (complete and near-complete) of 95.4%. 64 The same study reported thromboembolic complications of 6.9%. The high rate of thromboembolic complications might be related to the large amount of metal in the otherwise healthy parent artery. Overall, the results with SAC is better than what we found in this study however higher rate of complication in FD might be due to the fact FD is chosen in more complex cases. larger studies are required to draw a definitive conclusion regarding complications of technique and devices.
Over the past several years, intrasaccular flow diverters such as the WEB have emerged to address the short comings of intraluminal flow diverters. In the WEB-IT trial, a multicenter, single-arm study, the rate of complete occlusion of aneurysm was only 53.8% (77/143) at 12-month follow-up and no primary safety events, which is better than our safety results. 65 In accordance with the WEB-IT, a recent systemic analysis of the cumulative population of three studies (the French Observatory, 66 WEBCAST, 67 and WEBCAST-2 68 ) comprised of 168 patients, showed that the rate of complete aneurysm occlusion was 52.9% (81/153) at 12-month follow-up. 69 The same study reported a morbidity rate of 3.0% (5/167); however, a high rate of thromboembolic complications of 14.4% (24/167) was recorded at 1-month follow-up, 69 which corroborates our results.
Finally, PulseRider and pCONUS devices are new neck bridging technologies intended to treat wide-neck bifurcation aneurysms in conjunction with coils. These devices have less metal than conventional stents and are designed to protect the 3 branches of bifurcation aneurysms since they mainly brace against the parent vessel wall. A systematic review and meta-analysis containing 3 studies (2 multicenter case series and 1 single-arm clinical trial) described safety and efficacy outcomes of the PulseRider device in the treatment of bifurcation aneurysms in 63 patients: complete occlusion was achieved in 66.7% of patients at 6-month follow-up, while the intraoperative complication rate was 7.9%. 70 The Adjunctive Neurovascular Support of Wide-Neck Aneurysm Embolization and Reconstruction (ANSWER) trial reported complete occlusion rate in 67% (20/30) of patients and posttreatment ischemic event rate in 3.3% (1/30) of patients at 1-year follow-up. 71 A recent systematic review and meta-analysis of studies reporting the treatment of 203 intracranial aneurysms with pCONUS showed a long-term complete occlusion rate of 60%, perioperative morbidity rate of 7%, perioperative hemorrhage rate of 0%, and treatment-related long term neurological deficit in 2% of patients. 72 While the complete occlusion rates are similar between our results and PulseRider and pCONUS studies, both are associated with lower complication rates compared to our study. However, more studies are still needed for better comparison between the flow diverters and these neck bridging devices.
Overall, comparing published safety data from SAC, WEB, or new neck bridging devices with our results is difficult since many studies do not report complications outside of their established criteria of primary or secondary safety events, precluding us from estimating morbidity or mortality rates. However, treatment with endoluminal flow diverters seems to be relatively less safe, albeit effective, when compared with WEB and new neck bridging devices. In addition, although the complete occlusion rate is in line with rates for SAC, WEB, PulseRider, and pCONUS, the rate is suboptimal with all devices, highlighting the pressing need for endovascular therapies with improved occlusion rates for intracranial aneurysms.
Conclusions
Our study of complications and occlusion rates for patients with sidewall vs. bifurcation aneurysms treated with flow diverters suggests that there are no significant differences in the rate of complications, and that complete occlusion rates are suboptimal for both groups.
Supplemental Material
Supplemental material, sj-pdf-1-ine-10.1177_15910199211026713 for Endoluminal flow diverters in the treatment of sidewall and bifurcation aneurysm: A systematic review and meta-analysis of complications and angiographic outcomes by Mehdi Abbasi, Luis E Savasatano, Waleed Brinjikji, Kevin M Kallmes, Nick Mikoff, Natalie Reierson, Mohamed Abdelmegeed, John Pederson, Beth Warren, Jillienne C Touchette, Sarah Khan, Shelby Kamrowski, Averi Barrett, David F Kallmes and Ramanathan Kadirvel in Interventional Neuroradiology
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by a grant from the National institutes of Health (NS076491).
ORCID iDs: Mehdi Abbasi https://orcid.org/0000-0001-6978-2563
Waleed Brinjikji https://orcid.org/0000-0001-5271-5524
Kevin M Kallmes https://orcid.org/0000-0001-5439-4074
John Pederson https://orcid.org/0000-0003-2551-4828
David F Kallmes https://orcid.org/0000-0002-8495-0040
Ramanathan Kadirvel https://orcid.org/0000-0002-6786-9953
Supplemental material: Supplemental material for this article is available online.
References
- 1.Brown RD. Unruptured intracranial aneurysms. Semin Neurol 2010; 30: 537–544. [DOI] [PubMed] [Google Scholar]
- 2.Murayama Y, Nien YL, Duckwiler G, et al. Guglielmi detachable coil embolization of cerebral aneurysms: 11 years' experience. J Neurosurg 2003; 98: 959–966. [DOI] [PubMed] [Google Scholar]
- 3.Detmer FJ, Chung BJ, Jimenez C, et al. Associations of hemodynamics, morphology, and patient characteristics with aneurysm rupture stratified by aneurysm location. Neuroradiology 2019; 61: 275–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang Y, Tian Z, Jing L, et al. Bifurcation type and larger low shear area are associated with rupture status of very small intracranial aneurysms. Front Neurol 2016; 7: 169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Valen-Sendstad K, Mardal KA, Steinman DA. High-resolution CFD detects high-frequency velocity fluctuations in bifurcation, but not sidewall, aneurysms. J Biomech 2013; 46: 402–407. [DOI] [PubMed] [Google Scholar]
- 6.Baharoglu MI, Lauric A, Gao BL, et al. Identification of a dichotomy in morphological predictors of rupture status between sidewall- and bifurcation-type intracranial aneurysms. J Neurosurg 2012; 116: 871–881. [DOI] [PubMed] [Google Scholar]
- 7.Kallmes DF, Brinjikji W, Cekirge S, et al. Safety and efficacy of the pipeline embolization device for treatment of intracranial aneurysms: a pooled analysis of 3 large studies. J Neurosurg 2017; 127: 775–780. [DOI] [PubMed] [Google Scholar]
- 8.Marosfoi M, Clarencon F, Langan ET, et al. Acute thrombus formation on phosphorilcholine surface modified flow diverters. J Neurointervent Surg 2018; 10: 406–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pistocchi S, Blanc R, Bartolini B, et al. Flow diverters at and beyond the level of the circle of willis for the treatment of intracranial aneurysms. Stroke 2012; 43: 1032–1038. [DOI] [PubMed] [Google Scholar]
- 10.Puffer RC, Piano M, Lanzino G, et al. Treatment of cavernous sinus aneurysms with flow diversion: results in 44 patients. AJNR Am J Neuroradiol 2014; 35: 948–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fiehler J, Ries T. Prevention and treatment of thromboembolism during endovascular aneurysm therapy. Clin Neuroradiol 2009; 19: 73–81. [DOI] [PubMed] [Google Scholar]
- 12.Kallmes DF, Hanel R, Lopes D, et al. International retrospective study of the pipeline embolization device: a multicenter aneurysm treatment study. AJNR Am J Neuroradiol 2015; 36: 108–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tahtinen OI, Manninen HI, Vanninen RL, et al. The silk flow-diverting stent in the endovascular treatment of complex intracranial aneurysms: technical aspects and midterm results in 24 consecutive patients. Neurosurgery 2012; 70: 617–623. discussion 23–24. [DOI] [PubMed] [Google Scholar]
- 14.Brasiliense LB, Hanel RA. Pipeline embolization device: lessons learned after 1000 aneurysms. World Neurosurg 2014; 82: 248–250. [DOI] [PubMed] [Google Scholar]
- 15.Chiu AH, Cheung AK, Wenderoth JD, et al. Long-term follow-up results following elective treatment of unruptured intracranial aneurysms with the pipeline embolization device. AJNR Am J Neuroradiol 2015; 36: 1728–1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kulcsar Z, Houdart E, Bonafe A, et al. Intra-aneurysmal thrombosis as a possible cause of delayed aneurysm rupture after flow-diversion treatment. AJNR Am J Neuroradiol 2011; 32: 20–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turowski B, Macht S, Kulcsar Z, et al. Early fatal hemorrhage after endovascular cerebral aneurysm treatment with a flow diverter (SILK-Stent): do we need to rethink our concepts? Neuroradiology 2011; 53: 37–41. [DOI] [PubMed] [Google Scholar]
- 18.Cebral JR, Mut F, Raschi M, et al. Aneurysm rupture following treatment with flow-diverting stents: computational hemodynamics analysis of treatment. AJNR Am J Neuroradiol 2011; 32: 27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hampton T, Walsh D, Tolias C, et al. Mural destabilization after aneurysm treatment with a flow-diverting device: a report of two cases. J Neurointerv Surg 2011; 3: 167–171. [DOI] [PubMed] [Google Scholar]
- 20.Mascitelli JR, Moyle H, Oermann EK, et al. An update to the Raymond-Roy occlusion classification of intracranial aneurysms treated with coil embolization. J Neurointervent Surg 2015; 7: 496–502. [DOI] [PubMed] [Google Scholar]
- 21.O'Kelly CJ, Krings T, Fiorella D, et al. A novel grading scale for the angiographic assessment of intracranial aneurysms treated using flow diverting stents. Interv Neuroradiol 2010; 16: 133–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003; 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Makalanda H, Wong K, Bhogal P. Flow-T stenting with the silk vista baby and baby leo stents for bifurcation aneurysms – a novel endovascular technique. Interv Neuroradiol 2020; 26: 68–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oishi H, Teranishi K, Yatomi K, et al. Flow diverter therapy using a pipeline embolization device for 100 unruptured large and giant internal carotid artery aneurysms in a single center in a japanese population. Neurol Med Chir(Tokyo) 2018; 58: 461–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chalouhi N, Daou B, Kung D, et al. Fate of the ophthalmic artery after treatment with the pipeline embolization device. Neurosurgery 2015; 77: 581–584. discussion [DOI] [PubMed] [Google Scholar]
- 27.Lin LM, Iyer RR, Bender MT, et al. Rescue treatment with pipeline embolization for postsurgical clipping recurrences of anterior communicating artery region aneurysms. Interv Neurol 2017; 6: 135–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Enriquez-Marulanda A, Salem MM, Ascanio LC, et al. No differences in effectiveness and safety between pipeline embolization device and stent-assisted coiling for the treatment of communicating segment internal carotid artery aneurysms. Neuroradiol J 2019; 32: 344–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brinjikji W, Kallmes DF, Cloft HJ, et al. Patency of the anterior choroidal artery after flow-diversion treatment of internal carotid artery aneurysms. AJNR Am J Neuroradiol 2015; 36: 537–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mazur MD, Kilburg C, Wang V, et al. Pipeline embolization device for the treatment of vertebral artery aneurysms: the fate of covered branch vessels. J Neurointerv Surg 2016; 8: 1041–1047. [DOI] [PubMed] [Google Scholar]
- 31.Corley JA, Zomorodi A, Gonzalez LF. Treatment of dissecting distal vertebral artery (V4) aneurysms with flow diverters. Oper Neurosurg (Hagerstown) 2018; 15: 1–9. [DOI] [PubMed] [Google Scholar]
- 32.Dmytriw AA, Adeeb N, Kumar A, et al. Flow diversion for the treatment of basilar apex aneurysms. Neurosurgery 2018; 83: 1298–1305. [DOI] [PubMed] [Google Scholar]
- 33.Nossek E, Chalif DJ, Chakraborty S, et al. Modifying flow in the Ica bifurcation: pipeline deployment from the supraclinoid Ica extending into the M1 segment-clinical and anatomic results. AJNR Am J Neuroradiol 2014; 35: 2125–2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cerejo R, Bain M, John S, et al. Flow diverter treatment of cerebral blister aneurysms. Neuroradiology 2017; 59: 1285–1290. [DOI] [PubMed] [Google Scholar]
- 35.Chalouhi N, Zanaty M, Tjoumakaris S, et al. Treatment of blister-like aneurysms with the pipeline embolization device. Neurosurgery 2014; 74: 527–532; discussion 32. [DOI] [PubMed] [Google Scholar]
- 36.Mokin M, Chinea A, Primiani CT, et al. Treatment of blood blister aneurysms of the internal carotid artery with flow diversion. J Neurointerv Surg 2018; 10: 1074–1078. [DOI] [PubMed] [Google Scholar]
- 37.Cinar C, Oran I, Bozkaya H, et al. Endovascular treatment of ruptured blister-like aneurysms with special reference to the flow-diverting strategy. Neuroradiology 2013; 55: 441–447. [DOI] [PubMed] [Google Scholar]
- 38.Adeeb N, Griessenauer CJ, Foreman PM, et al. Comparison of stent-assisted coil embolization and the pipeline embolization device for endovascular treatment of ophthalmic segment aneurysms: a multicenter cohort study. World Neurosurg 2017; 105: 206–212. [DOI] [PubMed] [Google Scholar]
- 39.Roy AK, Howard BM, Haussen DC, et al. Reduced efficacy of the pipeline embolization device in the treatment of posterior communicating region aneurysms with fetal posterior cerebral artery configuration. Neurosurgery 2018; 82: 695–700. [DOI] [PubMed] [Google Scholar]
- 40.Tanweer O, Raz E, Brunswick A, et al. Cavernous carotid aneurysms in the era of flow diversion: a need to revisit treatment paradigms. AJNR Am J Neuroradiol 2014; 35: 2334–2340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lanzino G, Crobeddu E, Cloft HJ, et al. Efficacy and safety of flow diversion for paraclinoid aneurysms: a matched-pair analysis compared with standard endovascular approaches. AJNR Am J Neuroradiol 2012; 33: 2158–2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Puffer RC, Kallmes DF, Cloft HJ, et al. Patency of the ophthalmic artery after flow diversion treatment of paraclinoid aneurysms. J Neurosurg 2012; 116: 892–896. [DOI] [PubMed] [Google Scholar]
- 43.Brasiliense LBC, Aguilar-Salinas P, Miller DA, et al. Analysis of predictors and probability of aneurysm occlusion in the internal carotid artery after treatment with pipeline embolization device. World Neurosurg 2017; 107: 641–648. [DOI] [PubMed] [Google Scholar]
- 44.Colby GP, Bender MT, Lin LM, et al. Endovascular flow diversion for treatment of anterior communicating artery region cerebral aneurysms: a single-center cohort of 50 cases. J NeuroIntervent Surg 2017; 9: 679–685. [DOI] [PubMed] [Google Scholar]
- 45.Zanaty M, Chalouhi N, Tjoumakaris SI, et al. Flow diversion for complex middle cerebral artery aneurysms. Neuroradiology 2014; 56: 381–387. [DOI] [PubMed] [Google Scholar]
- 46.Caroff J, Neki H, Mihalea C, et al. Flow-diverter stents for the treatment of saccular middle cerebral artery bifurcation aneurysms. AJNR Am J Neuroradiol 2016; 37: 279–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gawlitza M, Januel AC, Tall P, et al. Flow diversion treatment of complex bifurcation aneurysms beyond the circle of willis: a single-center series with special emphasis on covered cortical branches and perforating arteries. J NeuroIntervent Surg 2016; 8: 481–487. [DOI] [PubMed] [Google Scholar]
- 48.Pujari A, Howard BM, Madaelil TP, et al. Pipeline embolization device treatment of internal carotid artery terminus aneurysms. J NeuroIntervent Surg 2019; 11: 485–488. [DOI] [PubMed] [Google Scholar]
- 49.Yavuz K, Geyik S, Saatci I, et al. Endovascular treatment of middle cerebral artery aneurysms with flow modification with the use of the pipeline embolization device. AJNR Am J Neuroradiol 2014; 35: 529–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dabus G, Grossberg JA, Cawley CM, et al. Treatment of complex anterior cerebral artery aneurysms with pipeline flow diversion: mid-term results. J Neurointerv Surg 2017; 9: 147–151. [DOI] [PubMed] [Google Scholar]
- 51.Ravindran K, Enriquez-Marulanda A, Kan PTM, et al. Use of flow diversion for the treatment of distal circulation aneurysms: a multicohort study. World Neurosurg 2018; 118: e825–e833. [DOI] [PubMed] [Google Scholar]
- 52.Primiani CT, Ren Z, Kan P, et al. A2, M2, P2 aneurysms and beyond: results of treatment with pipeline embolization device in 65 patients. J Neurointerv Surg 2019; 11: 903–907. [DOI] [PubMed] [Google Scholar]
- 53.Lin N, Lanzino G, Lopes DK, et al. Treatment of distal anterior circulation aneurysms with the pipeline embolization device: a US multicenter experience. Neurosurgery 2016; 79: 14–22. [DOI] [PubMed] [Google Scholar]
- 54.Lin LM, Bender MT, Colby GP, et al. Flow diversion covering the M1 origin as a last resort. Stroke Vasc Neurol 2019; 4: 141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Daou B, Valle-Giler EP, Chalouhi N, et al. Patency of the posterior communicating artery following treatment with the pipeline embolization device. J Neurosurg 2017; 126: 564–569. [DOI] [PubMed] [Google Scholar]
- 56.Saleme S, Iosif C, Ponomarjova S, et al. Flow-diverting stents for intracranial bifurcation aneurysm treatment. Neurosurgery 2014; 75: 623–631; quiz 31. [DOI] [PubMed] [Google Scholar]
- 57.Moon K, Albuquerque FC, Ducruet AF, et al. Treatment of ophthalmic segment carotid aneurysms using the pipeline embolization device: clinical and angiographic follow-up. Neurol Res 2014; 36: 344–350. [DOI] [PubMed] [Google Scholar]
- 58.McLaughlin N, McArthur DL, Martin NA. Use of stent-assisted coil embolization for the treatment of wide-necked aneurysms: a systematic review. Surg Neurol Int 2013; 4: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Becske T, Kallmes DF, Saatci I, et al. Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology 2013; 267: 858–868. [DOI] [PubMed] [Google Scholar]
- 60.Lv X, Yang H, Liu P, et al. Flow-diverter devices in the treatment of intracranial aneurysms: a meta-analysis and systematic review. Neuroradiol J 2016; 29: 66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mokin M, Primiani CT, Ren Z, et al. Stent-assisted coiling of cerebral aneurysms: multi-center analysis of radiographic and clinical outcomes in 659 patients. J Neurointerv Surg 2020; 12: 289–297. [DOI] [PubMed] [Google Scholar]
- 62.Chow MM, Woo HH, Masaryk TJ, et al. A novel endovascular treatment of a wide-necked basilar apex aneurysm by using a Y-configuration, double-stent technique. AJNR Am J Neuroradiol 2004; 25: 509–512. [PMC free article] [PubMed] [Google Scholar]
- 63.Fargen KM, Mocco J, Neal D, et al. A multicenter study of stent-assisted coiling of cerebral aneurysms with a Y configuration. Neurosurgery 2013; 73: 466–472. [DOI] [PubMed] [Google Scholar]
- 64.Cagnazzo F, Limbucci N, Nappini S, et al. Y-stent-assisted coiling of wide-neck bifurcation intracranial aneurysms: a meta-analysis. AJNR Am J Neuroradiol 2019; 40: 122–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Arthur AS, Molyneux A, Coon AL, et al. The safety and effectiveness of the woven EndoBridge (WEB) system for the treatment of wide-necked bifurcation aneurysms: final 12-month results of the pivotal WEB intrasaccular therapy (WEB-IT) study. J Neurointerv Surg 2019; 11: 924–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pierot L, Moret J, Turjman F, et al. WEB treatment of intracranial aneurysms: feasibility, complications, and 1-month safety results with the WEB DL and WEB SL/SLS in the French observatory. AJNR Am J Neuroradiol 2015; 36: 922–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pierot L, Costalat V, Moret J, et al. Safety and efficacy of aneurysm treatment with WEB: results of the WEBCAST study. J Neurosurg 2016; 124: 1250–1256. [DOI] [PubMed] [Google Scholar]
- 68.Pierot L, Gubucz I, Buhk JH, et al. Safety and efficacy of aneurysm treatment with the WEB: results of the WEBCAST 2 study. AJNR Am J Neuroradiol 2017; 38: 1151–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pierot L, Moret J, Barreau X, et al. Safety and efficacy of aneurysm treatment with WEB in the cumulative population of three prospective, multicenter series. J Neurointerv Surg 2018; 10: 553–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Aguilar-Salinas P, Brasiliense LBC, Walter CM, et al. Current status of the PulseRider in the treatment of bifurcation aneurysms: a systematic review. World Neurosurg 2018; 115: 288–294. [DOI] [PubMed] [Google Scholar]
- 71.Spiotta AM, Chaudry MI, Turner RDt, et al. An update on the adjunctive neurovascular support of wide-neck aneurysm embolization and reconstruction trial: 1-year safety and angiographic results. AJNR Am J Neuroradiol 2018; 39: 848–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sorenson TJ, Iacobucci M, Murad MH, et al. The pCONUS bifurcation aneurysm implants for endovascular treatment of adults with intracranial aneurysms: a systematic review and Meta-analysis. Surg Neurol Int 2019; 10: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-ine-10.1177_15910199211026713 for Endoluminal flow diverters in the treatment of sidewall and bifurcation aneurysm: A systematic review and meta-analysis of complications and angiographic outcomes by Mehdi Abbasi, Luis E Savasatano, Waleed Brinjikji, Kevin M Kallmes, Nick Mikoff, Natalie Reierson, Mohamed Abdelmegeed, John Pederson, Beth Warren, Jillienne C Touchette, Sarah Khan, Shelby Kamrowski, Averi Barrett, David F Kallmes and Ramanathan Kadirvel in Interventional Neuroradiology