Abstract
Background & objectives:
Ultrasound BI-RADS categories 3 and 4 constitute those breast masses which cannot be confidently classified as benign or malignant, owing to their morphological characteristics. These masses are further managed by follow up and biopsy, respectively. This study aims to evaluate the role of strain elastography and Doppler in better characterization of these sonographically indeterminate breast masses as benign or malignant.
Methods:
Fifty female patients with ultrasound BI-RADS 3 or 4 were evaluated with strain elastography and color Doppler including spectral analysis. Eight variables were assessed by elastography and Doppler, including a new phenomenon called bidirectional arterial flow (BAF). The findings were correlated with the gold standard diagnostic method of histopathology/cytology. Based on findings of combined elastography and Doppler method, the initial ultrasound BI-RADS categories of masses were re-categorized by up-gradation or down-gradation. Sensitivity, specificity, accuracy, positive predictive value, negative predictive value and receiver operating characteristic (ROC) curves were used to estimate the diagnostic performance of the combination method.
Results:
Using ROC analysis, the positivity of ≥3 among the total eight variables correlated with malignancy on histopathology. Sensitivity, specificity and accuracy of the combination method using cut-off score ≥3 (i.e. at least three out of the eight parameters in the combination method being positive) for the prediction of malignancy was 100, 76.47 and 92 per cent, respectively, with the area under curve being 0.967. In addition, BAF was found predictive of malignancy with a diagnostic accuracy of 70 per cent.
Interpretation & conclusions:
This non-invasive, cheaper and readily accessible combination method of strain elastography and Doppler imaging can improve the diagnostic characterization of sonographically indeterminate breast masses and may obviate the need of magnetic resonance imaging and unnecessary biopsies, thus proving helpful in resource-poor countries.
Keywords: Bidirectional arterial flow, BI-RADS, breast, Doppler, elastography, size ratio, strain ratio, Tsukuba score
Breast cancer is the most commonly diagnosed cancer and the leading cause of cancer-related mortality in women globally1. Death rates for female breast and cervical cancers are considerably higher in developing versus developed countries1. This has led to more work on new cost-effective, non-invasive diagnostic techniques and their combinations, which can help increase the specificity of current imaging modalities such as mammography and ultrasound.
Mammography is the baseline screening imaging modality in suspected breast lesions but has false-positive rate of six per cent2. It is a good screening tool, especially in females older than 40 yr and those without dense breast tissue. Magnetic resonance imaging (MRI) is useful in detecting multiquadrant, bilateral and small (2-3 mm) lesions and for detailing the architectural abnormalities in the breast with lymphatic spread. However, MRI has its inherent limitations like contraindications in patients with metallic implants and claustrophobia and has low specificity in differentiating breast lesions, leading to an increasingly high number of unnecessary biopsies in benign breast masses3.
Sonography is among the most imperative and widely practiced imaging methods for differentiating benign from malignant breast masses owing to its easy accessibility, low cost, real-time imaging, high spatial resolution and sensitivity, with no contraindication in patients with implants in situ. However, sonography has the limitation of lack of specificity and high rates of false-positive outcomes4. ACR BI-RADS (American College of Radiology Breast Imaging-Reporting and Data System) categories 3 and 4 constitute indeterminate breast lesions; category 3 being probably benign lesions (≤2% chance of malignancy) and category 4 being suspicious lesions (>2 to ≤94% chance of malignancy). The course of further management of category 3 is short-term follow up and of category 4 is further evaluation in the form of biopsy. As BI-RADS categorization focuses primarily on the qualitative assessment of anatomical features, subjective factors from the examiner may influence categorization of lesions5. To prevent excessive biopsies in benign lesions labelled as BI-RADS 4 and furthermore to provide the highest level of patient safety by not branding a benign-looking malignant lesion as follow up category (BI-RADS 3), additional diagnostic methods of sonoelastography and Doppler may be added to further increase the specificity of conventional ultrasound.
Although conventional mammography is a good screening tool, features like stiffness or vascularity of breast masses cannot be assessed. Breast MR elastography is an evolving technique with the potential of assessing tissue stiffness6 while dynamic contrast MR mammography is a good to assess neoangiogenesis7. Sonoelastography is a novel technique and has developed considerably over the last few years. The technique grounds itself on the principle that soft tissue deforms readily as compared to hard tissue and hence malignant lesions with increased hardness deform less and display larger dimensions on elastography in contrast to benign lesions8. Two major strain elastography parameters have been described, size ratio and strain ratio or stiffness criteria9. Size ratio denotes the difference in the extent of the longest diameter of lesion on the corresponding B-mode image and the elastographic image9. Barr et al9 evaluated 635 breast lesions and concluded that a size ratio of more than one is suggestive of a malignant breast lesion with sensitivity and specificity of 98.6 and 87.4 per cent respectively. Strain ratio is a semi-quantitative assessment of differences in strain between two operator-defined areas in an elastographic image9. In 2006, Itoh et al10 described a scoring system to classify elastographic findings called the Tsukuba score, in which lesions with score 1 and 2 are considered benign, those with scores 4 and 5 are considered malignant and score 3 is given for probably benign lesions.
Different Doppler modalities such as colour Doppler, power Doppler, spectral Doppler with or without contrast medium injection are used as an adjunct to B-mode ultrasound in the evaluation of breast masses11. Spectral Doppler assessment of blood flow also hypothetically helps in the characterization of breast masses; literature suggests a high peak systolic velocity (PSV), pulsatility index (PI) and resistivity index (RI) in malignant masses than in benign lesions12. Hypervascularisation (two or more circumferential or central vessels or penetrating vessel in mass), a penetrating vessel in the mass, branching and disordered course of vessels and RI >0.85 were considered as probable malignant criteria by Elkharbotly and Farouk13. A novel Doppler sign-bidirectional arterial flow (BAF) was evaluated by Liu et al14 in 2015 for differentiating BI-RADS category 4 masses. It is defined as the occurrence of two vessels with different arterial blood flow directions within the same breast mass, as indicated by red and blue colours on colour and spectral Doppler study. The lesions exhibiting this phenomenon were identified as suspicious for malignancy and this feature was proposed to help distinguish breast cancers from fibroadenomas and other benign lesions.
This study aimed to appraise the role of strain elastography combined with Doppler studies in indeterminate breast masses (BI-RADS 3, 4 on conventional ultrasound), helping in a more specific upgradation or downgradation of the BI-RADS category of the lesions after the combined assessment.
Material & Methods
A single centre prospective, observational study was carried out in the department of Radiology, Vardhman Mahavir Medical College and Safdarjung Hospital over a span of one year (December 2015 to December 2016) in collaboration with departments of Surgery and Pathology. The study included 50 female patients aged above 20 yr with palpable or suspicious breast lump, who were detected with BI-RADS 3 or 4 lesions on ultrasound (irrespective of whether they had undergone mammography as the sensitivity of mammography is less in young patients with dense breasts). All patients with BI-RADS 3 or 4 lesions then underwent strain elastography, colour and spectral Doppler analysis followed by histopathological/cytological examination. Patients with predominantly cystic lesions were excluded. None of the patients had undergone prior biopsy or treatment for the concerned lesion. The study was conducted after the approval of the Institutional Ethics Committee. A written consent was obtained from all participants after informing regarding the available management options.
Sonographic evaluation: Following clinical evaluation, bilateral whole-breast sonography was performed in each patient in both the transverse and longitudinal planes, in the supine position in all patients and when necessary in the decubitus position for patients with bulky breasts. All the examinations were performed by a Radiology resident (observer 1) with a minimum one year of experience under the supervision of a Radiology Professor (observer 2) with over 30 yr of experience in the field. Data acquisition was performed using ultrasound scanner equipped with linear-array transducers of frequency 5-12 and 7-12 MHz respectively. BI-RADS categories were assigned to the masses based on descriptors in the ultrasound lexicon after assessing shape and size, orientation, margin, echo pattern, posterior acoustic features and axillary nodes. Lesions satisfying BI- RADS US criteria 3 and 4A, 4B, 4C were further recruited into study for strain elastography and Doppler imaging. Well circumscribed, non-calcified, hypoechoic lesions with parallel orientation were labelled BI-RADS 3. Similar morphology lesions with minor atypical features such as small cystic spaces or lobulated margins were assigned under BI-RADS 4A category. Lesions with microlobulated margins and/or non-parallel orientation were labelled as BI-RADS 4B and those with angulated margins, non-parallel orientation and with mild surrounding architectural distortion were labelled as 4C categories, respectively. Masses with obvious invasion into the skin, subcutaneous tissue or underlying pectoralis major muscle and those causing nipple retraction were excluded as such masses befit BI-RADS 5 categorization.
Combination method of elastography & Doppler: Strain elastography image of each mass was obtained by defining ROI (region of interest) encompassing the majority of the tumour area, with sufficient area of surrounding normal tissue. To avoid stress decay and to standardize the technique, ROI was placed in glandular tissue at a depth similar to or as adjacent to the target mass as possible. The size of the ROIs was kept constant throughout the study for a given patient. Red colour was selected as depictive of hardness and blue colour as softness, with green colour depicting intermediate stiffness. The effort was made to keep the pressure constant (around 50% of the pressure bar on the side of the screen) in all patients to achieve a standardized, reproducible examination protocol.
After placing an ROI in the focal lesion, reference ROI was kept in the surrounding normal tissue, preferably at the same depth as the lesion. The elastography software yielded the ratio of the average strain in the reference (normal) area to the average strain in the lesion as strain ratio. Size ratio of the mass lesion was calculated as the ratio of the longest diameter of lesion on elastography to the longest diameter on B-mode ultrasound. The target lesion was also scored from 1 to 5 rendering to the scoring system as proposed earlier10 (Tsukuba elastography score) (Fig. 1).
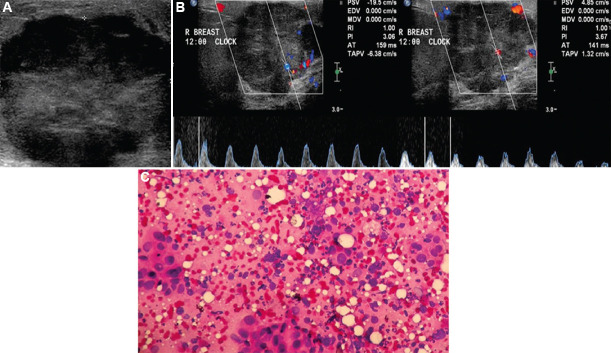
Fig. 1.
Ultrasound BI-RADS 4C lesion visualized in the right breast of a 40 yr old patient. Strain elastography showed target lesion with Tsukuba score 4 and strain ratio 6.82.
Colour Doppler and spectral Doppler modes were performed on each mass. The masses were first assessed using colour Doppler to determine whether internal or peripheral vascularity was present. In masses with only peripheral vascularity, spectral Doppler analysis was done from the peripheral vessels and the maximum values obtained were recorded. In cases of lesions with internal vascularity, spectral Doppler analysis was done to determine which of the vessels indicated arterial or venous flow. Spectral analysis of all the arteries within the field of view was done and the values of PSV, RI and PI obtained from the artery with maximum values were recorded. The presence of BAF was documented as well (Fig. 2).
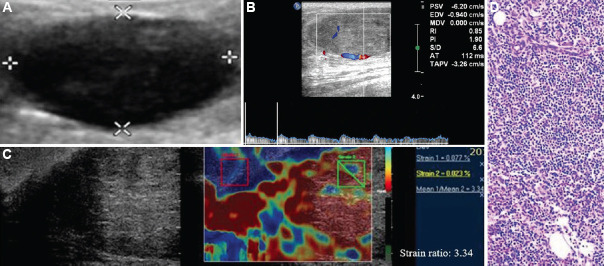
Fig 2.
(A) Grey scale ultrasound depicts a BI-RADS 4C lesion. (B) Doppler analysis of a BI-RADS 4C lesion revealed internal vascularity with bidirectional arterial color flow. (C) Cytology diagnosis: infiltrating ductal carcinoma.
Ultrasound-guided core needle biopsy/FNAC (Fine Needle Aspiration Cytology) was performed in all the patients with BI-RADS 3 and 4 category lesions under complete aseptic precautions, with informed consent from the patients (and permission from the referring clinician for BI-RADS 3 masses, which are usually managed by short-term follow up/biopsies based on clinician’s suspicion). Tissue diagnosis was made by the pathologist and this was used as the gold standard for comparison of results of imaging studies.
Statistical analysis: The study included 50 female patients suspected to have breast lump, who were detected with BI-RADS 3 or 4 lesions on ultrasound. Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± standard deviation and median. Normality of data was tested using Kolmogorov–Smirnov test. If the normality was rejected then non-parametric test was used. Quantitative variables were compared using unpaired t test/Mann–Whitney U test (when the data sets were not normally distributed) between the two groups. Qualitative variables (pattern of vascularity, presence of BAF) were compared using the Chi-square test and Fisher’s exact test. Receiver operating characteristic (ROC) curve was used to assess the cut-off values for strain ratio, PSV, RI and PI for predicting malignancy. A combination method considering all the eight variables used in elastography and Doppler assessment, was used by attributing score of one for each variable positive for malignancy, based on the result of the gold standard. The ultrasound BI-RADS categories of lesions were re-categorized by upgradation or downgradation based on the combination method of elastography and Doppler.
Diagnostic test was used to calculate sensitivity, specificity, negative predictive value (NPV), positive predictive value (PPV) and accuracy of each modality and combination of elastography with Doppler. Inter-rater Kappa agreement was used to find out the strength of agreement between two methods for prediction of malignancy, with P value of <0.05 being statistically significant. Using the ROC curve, the optimal cut-off value for predicting malignancy with the combination method was obtained. Data analysis was done using Statistical Package for the Social Sciences (SPSS) version 21.0 (IBM Corp., Chicago, USA).
Results
The study included 50 female patients aged above 20 yr, with palpable breast lump, detected with BI-RADS 3 or 4 lesions on B-mode ultrasound. Majority of the patients belonged to the age group 31-40 yr. No patients had bilateral breast lumps, making 50 patients with 50 mass lesions. Pathologic examination detected 17 benign lesions (34%) and 33 malignant lesions (66%) (Table I). The mean age of patients with benign lesions was 33.35±10.74, while that of benign lesions was 47.27±12.5 (Table II). Ten patients had ultrasound BI-RADS 3 category mass of which one (10%) proved malignant. One (11.11%) out of nine patients with BI-RADS 4A, 12 (92.3%) out of 13 patients with BI-RADS 4B and 17 (94.4%) out of 18 masses with BI-RADS 4C masses respectively had malignancy, clearly demonstrating an association of malignancy with increasing BI-RADS score and an accuracy of 74.73 per cent for B-mode ultrasound categorization.
Table I.
Histolopathological diagnosis of the masses
| Diagnosis | Number of lesions (n=50) |
|---|---|
| Benign | 17 |
| Fibroadenoma | 14 |
| Benign phyllodes tumor | 2 |
| Papilloma | 1 |
| Malignant | 33 |
| Infiltrating ductal carcinoma | 30 |
| Mucinous/colloid carcinoma | 1 |
| Medullary carcinoma | 1 |
| Lymphoma | 1 |
Table II.
Mean values of continuous variables with their statistical significance
| Parameter | Mean±SD | |
|---|---|---|
|
| ||
| Benign (n=17) | Malignant (n=33) | |
| Age | 33.35±10.74 | 47.27±12.5** |
| Strain ratio | 3.75±2.13 | 6.9±1.55*** |
| Size ratio | 1.01±0.07 | 1.13±0.1*** |
| PSV | 13.71±6 | 15.57±11.19* |
| RI | 0.69±0.19 | 0.93±0.12*** |
| PI | 1.49±0.77 | 2.62±0.93*** |
PSV, peak systolic velocity; RI, resistive index; PI, pulsatility index; SD, standard deviation. P*<0.05, **<0.01, ***<0.001
Masses with Tsukuba score >3 and those with size ratio >1 were taken as malignant and this assessment proved statistically significant in the current study (Table II). We obtained strain ratio cut-off value of >3.78 as indicative of malignancy, by plotting the ROC curve (area under curve (AUC) 0.8752). Lesion sizes varied from 2 to 3 cm in the longest dimension. Out of the three strain elastography parameters used, strain ratio showed the highest sensitivity (100%), specificity (76.47%) and accuracy (92%) for distinguishing benign vs. malignant breast masses in this study. Size ratio had an accuracy of 80 per cent and value above one is a good indicator of adjacent desmoplastic reaction/invasion in small infiltrating ductal carcinomas of size below 3 cm. The final ROC curve was prepared for elastography technique using the three parameters and >0 (i.e. at least 1 positive parameter) was found to be significant [AUC, 0.8601; 95% confidence interval (CI): 0.73 to 0.94].
The internal pattern of vascularity within the lesions was indicative of malignancy with sensitivity of 96.9 per cent with P value of 0.004. The presence of BAF was found to have sensitivity of 72.73 per cent and specificity of 64.71 per cent in the detection of malignancy with P value of 0.010. By plotting ROC curve, predictive cut-off values for PSV, RI and PI for malignancy were obtained as 24.9 cm/s, 0.84 and 1.94, respectively, with significant P value (Table III). Out of the five Doppler parameters used, RI showed the greatest sensitivity (81.82%) and specificity (82.35%) for differentiating benign vs malignant breast masses in our study. The final ROC curve was obtained for the Doppler technique using the above-mentioned parameters and >1 parameter was found to be significant (AUC, 0.9037; 95% CI: 0.78 to 0.96).
Table III.
Diagnostic results of the eight parameters used in the study
| Variables | Benign | Malignant | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | AUC (95% CI) | F-1 score |
|---|---|---|---|---|---|---|---|---|
| Pattern of vascularity | Peripheral | Internal** | 96.9 | 35.3 | 74.4 | 85.7 | - | 0.842 |
| BDAF | Absent | Present* | 72.73 | 64.71 | 80 | 55 | - | 0.762 |
| PSV | ≤23.9 cm/s | >23.9 cm/s | 18.18 | 100 | 100 | 38.64 | 0.516 (0.37-0.66) | 0.308 |
| RI | ≤0.84 | >0.84*** | 81.82 | 82.35 | 90 | 70 | 0.8467 (0.71-0.93) | 0.857 |
| PI | ≤1.94 | >1.94*** | 81.82 | 76.47 | 87.1 | 68.42 | 0.8378 (0.70-0.92) | 0.844 |
| Tsukuba score | ≤3 | >3** | 96.9 | 41.1 | 76.2 | 87.5 | - | 0.853 |
| Size ratio | ≤1 | >1*** | 84.85 | 70.5 | 84.85 | 70.5 | - | 0.849 |
| Strain ratio | ≤3.78 | >3.78*** | 100 | 76.47 | 89.19 | 100 | 0.875 (0.75-0.95) | 0.943 |
NPV, negative predictive value; PPV, positive predictive value, AUC, area under the curve; CI, confidence interval; BDAF, bidirectional arterial flow. P* <0.05, **<0.01, ***<0.001
To calculate the diagnostic performance of combined elastography and Doppler technique, a score of one was given for each positive variable out of the eight variables under consideration. ROC curve was used to estimate the diagnostic performance and optimal cut-off of combination method of strain elastography and Doppler was determined using the Youden index. A cut-off value of >2 total scores (i.e. at least three positive variables out of eight variables under consideration) was obtained with significant discriminating power as predictive of malignancy. Hence, lesions with at least three positive variables were upgraded (Figs 3 and 4), while others were downgraded (Figs 5, 6 and Table IV). The discriminating power of the combined method for recognition of malignancy (AUC, 0.9670; 95% CI: 0.87-0.99) was significantly greater than that of Doppler (AUC, 0.9037; 95% CI: 0.78-0.96) or elastography (AUC, 0.8601; 95% CI: 0.73-0.94) separately with a sensitivity of 100 per cent, specificity of 76.47 per cent and accuracy of 92 per cent (Fig. 7). P value was used to compare the AUC-ROC curves of three techniques (Table V).
Fig. 3.
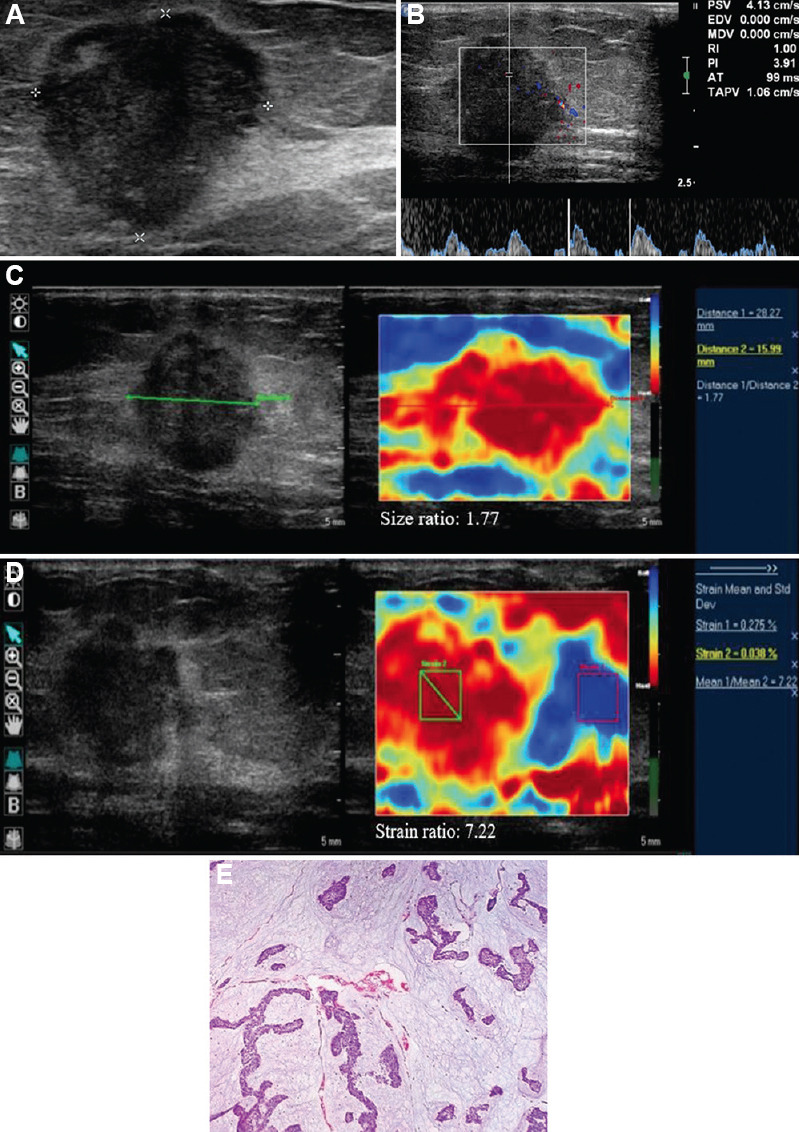
(A) Ultrasound BI-RADS 4B lesion seen in the left breast of a 38 yr old patient. (B) On Doppler analysis, the mass demonstrated internal arterial vascularity, however, without bidirectional arterial flow. Spectral analysis revealed arterial flow with peak systolic velocity of 4.13, but high values of resistivity index of one and pulsatility index of 3.91. Strain elastography assessment demonstrated Tsukuba elastography score of 5, (C) size ratio of 1.77 and (D) strain ratio of 7.22. Lesion was upgraded to BI-RADS 4C following combined method assessment. (E) Histologic diagnosis: colloid carcinoma.
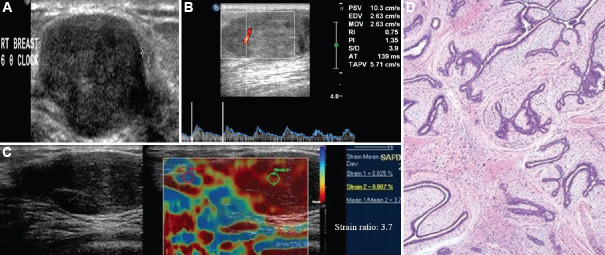
Fig. 4.
(A) Ultrasound demonstrated an oval, hypoechoic lesion with circumscribed margins and parallel orientation (ultrasound BI-RADS 3 lesion) in the left breast of a 5 yr old child with retropositive status. (B) Color Doppler revealed minimal internal and peripheral vascularity with resistive index 0.85, pulsatility index 1.9 and peak systolic velocity 6.2 cm/s. (C) Strain elastography revealed Tsukuba score of 4 and strain ratio of 3.34 (suspicious features). In view of three positive variables (internal vascularity, high resistivity index and Tsukuba score), mass was upgraded to BI-RADS 4A. (D) Histologic diagnosis: lymphoma.
Fig. 5.
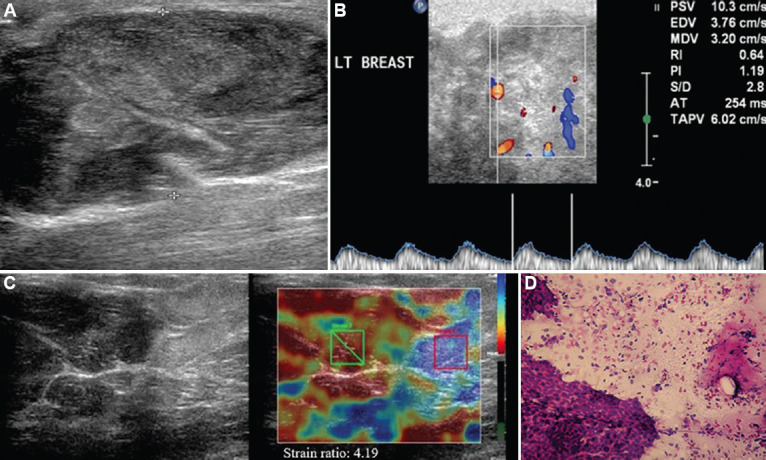
(A) Left breast BI-RADS 4A lesion containing cystic areas and echogenic septations in a 45 yr old patient. (B) Doppler analysis showed increased internal vascularity within the lesion, without bidirectional arterial flow. Spectral analysis revealed peak systolic velocity of 10.3 cm/s, resistivity index of 0.64 and pulsatility index of 1.19. (C) Elastography revealed Tsukuba score of 3, strain ratio of 4.19 size ratio one. On combined method, lesion was downgraded to BI-RADS 3 as only two out of eight variables were positive (strain ratio and presence of internal vascularity). (D) Cytology diagnosis: benign Phyllode’s tumor.
Fig. 6.
(A) Grey scale ultrasound demonstrates an oval, hypoechoic lesion with circumscribed margins and parallel orientation in the right breast of a 20 yr old female, suggestive of BI-RADS 3 lesion. (B) A single artery was noted within the lesion with peak systolic velocity 10.3 cm/s, resistivity index 0.75 and pulsatility index 1.35 on spectral Doppler evaluation. (C) Strain elastography showed Tsukuba score 4 with strain ratio 3.7. On combined method, lesion was downgraded to BI-RADS 2 as only two variables (internal vascularity, Tsukuba score) was positive. (D) Histopathology diagnosis: fibroadenoma.
Table IV.
Re-categorization of masses after combined method evaluation and comparison with pathology diagnosis
| US BI-RADS score | Number of masses (n=50) | Recategorised score | Combined method (n=50) | Histopathologic diagnosis | |
|---|---|---|---|---|---|
|
| |||||
| Benign (n=17) | Malignant (n=33) | ||||
| 3 | 10 | 2 | 8 | 8 | 0 |
| 4A | 2 | 1 | 1 | ||
| 4A | 9 | 3 | 7 | 6 | 1 |
| 4B | 2 | 1 | 1 | ||
| 4B | 13 | 4A | 3 | 1 | 2 |
| 4C | 10 | 0 | 10 | ||
| 4C | 18 | 4B | 1 | 1 | 0 |
| 5 | 17 | 0 | 17 | ||
US BI-RADS, ultrasound breast imaging-reporting and data system
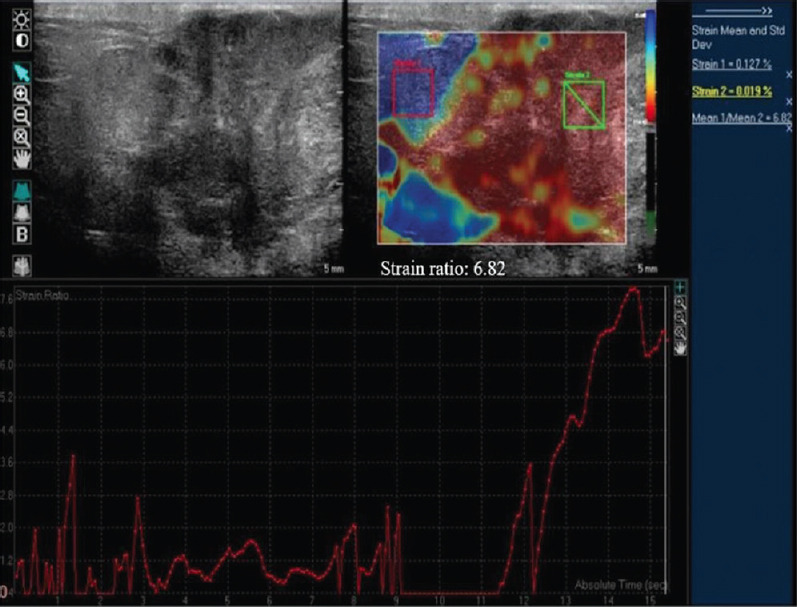
Fig. 7.
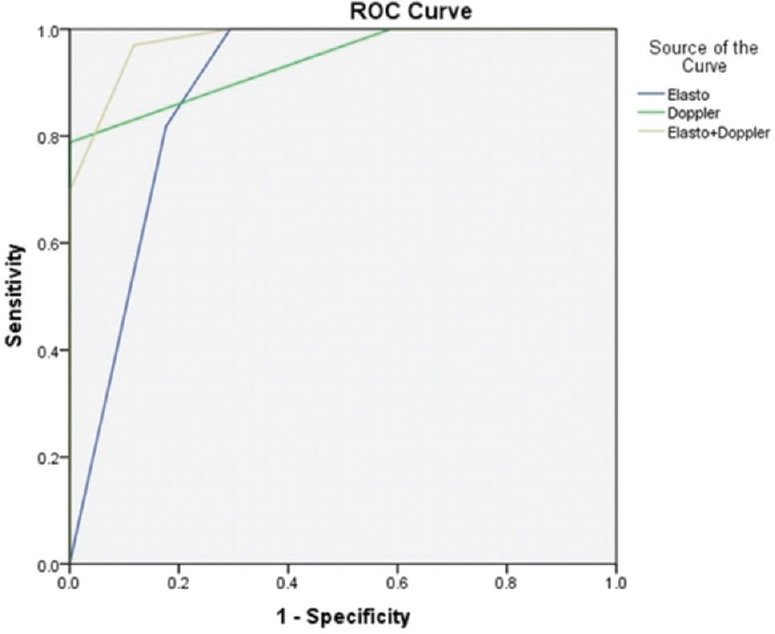
Comparison of receiver operating characteristic curve estimating the diagnostic performance of strain elastography, Doppler and combination method of elastography and Doppler in differentiating benign and malignant lesions. The discriminating power of combined method for detection of malignancy was significantly higher than that of elastography or Doppler alone.
Table V.
Comparison of area under the receiver operating characteristic curves of Doppler and elastography with the combination method
| AUC-ROC curve comparison | P | Z statistic |
|---|---|---|
| Doppler with combination method | 0.078 | 1.763 |
| Elastography with combination method | 0.0447 | 2.007 |
AUC-ROC, area under the receiver operating characteristic
The final category of eight parameters which yielded the best fit in descending order of accuracy was strain ratio (92%), RI (82%), PI and size ratio (80% each), Tsukuba score (78%), the internal pattern of vascularity (76%), BAF (70%) and PSV (46%).
Interrater kappa agreements of Doppler, elastography and combination method with gold standard tissue diagnosis were 0.65 (good), 0.76 (good) and 0.81 (very good), respectively. Results of Kolmogorov–Smirnov test are enumerated in Table VI, with PSV, RI, PI, size ratio and strain ratio being the variables tested by the non-parametric method.
Table VI.
Results of Kalmogorov-Smirnove test with median and interquartile range (IQR) of non-parametric tests
| Variables | Statistic | df | Significance | Median | IQR |
|---|---|---|---|---|---|
| PSV | |||||
| Benign | 0.168 | 17 | 0.200* | 13.1 | 8.253-18.700 |
| Malignant | 0.177 | 33 | 0.010 | 11.8 | 8.270-19.625 |
| RI | |||||
| Benign | 0.159 | 17 | 0.200* | 0.65 | 0.545-0.840 |
| Malignant | 0.300 | 33 | 0.000 | 1 | 0.890-1 |
| PI | |||||
| Benign | 0.240 | 17 | 0.010 | 1.17 | 0.915-1.980 |
| Malignant | 0.085 | 33 | 0.200* | 2.47 | 2.008-3.110 |
| Size ratio | |||||
| Benign | 0.274 | 17 | 0.001 | 1 | 1-1.018 |
| Malignant | 0.157 | 33 | 0.038 | 1.1 | 1.050-1.200 |
| Strain ratio | |||||
| Benign | 0.259 | 17 | 0.004 | 3.2 | 2.735-3.883 |
| Malignant | 0.110 | 33 | 0.200* | 7.06 | 5.807-8 |
*Indicates is a lower limit of the true significance
Discussion
BI-RADS 3 and 4 category masses, possessing features which are inconsistent to be labelled as definitely benign or malignant, constitute the indeterminate breast masses. ACR BI-RADS recommends short-term follow up for BI-RADS 3 masses while tissue diagnosis is mandatory for category 4. However, according to the latest ACR BI-RADS® atlas fifth edition, BI-RADS 3 masses may be biopsied on clinician’s suspicion. When used properly, the indeterminate categories reduce the number of benign biopsies while allowing the radiologist to maintain a high sensitivity for the detection of early-stage breast cancer15. In a study by Brown et al16 mammography contributed to delineation of disease extent, detection of incidental malignancies, and confirmation of benign diagnoses in women above 30 yr of age. Graziano et al17 observed that ultrasound is a method with good sensitivity (98.1%), but with lower specificity (40.6%) in the evaluation of indeterminate breast masses. Differentiation between BI-RADS 3 and 4 by US elastography had 84 per cent sensitivity and 84 per cent specificity while dynamic contrast-enhanced MRI had 88 per cent sensitivity but only 80 per cent specificity according to a study conducted by ElSaid and Mohamed18. However, Strobel et al19 concluded that MRI is useful for the non-invasive workup of lesions classified as BI-RADS category 4 at mammography or US and can help avoid 92 per cent of unnecessary biopsies. The present study evaluated sonographically indeterminate masses using strain elastography and Doppler, which are simple, easily available, economical and radiation-free techniques which aid in the assessment of stiffness and vascularity of breast masses, unlike MRI and mammography.
In our study, the sensitivity of 41.1 per cent and specificity of 96.9 per cent was thus obtained for the Tsukuba scoring system, which was similar to those obtained by Navarro et al20 in 2011. Using a size ratio cut-off of 1, a sensitivity of 84.85 per cent and specificity of 70.59 per cent in diagnosing malignancy could be reached, which corresponds to the results reported in previously9. By plotting the ROC curve, we obtained a cut-off value of >3.78 as indicative of malignancy with the sensitivity of 100 per cent and specificity of 76.47 per cent, concordant with previous reports21.
On Doppler evaluation, the presence of internal pattern of vascularity was found to be statistically significant for malignancy with sensitivity of 96.9 per cent and specificity of 35.2 per cent. The observations were in concordance with previously published literature22,23,24. The presence of BAF was found to have sensitivity of 72.73 per cent and specificity of 64.71 per cent. Our values were slightly different from the results obtained in the study conducted in 116 BI-RADS category 4 lesions by Liu et al14 who obtained sensitivity of 64.9 per cent, specificity of 98.7 per cent. This disparity could be due to the small sample size used in the present study. By plotting ROC curve, cut-off values as predictive of malignancy for PSV, RI and PI were obtained as >23.9 cm/s, >0.84 and >1.94 in our study with the specificity of 100, 82.35 and 76.47 per cent, respectively. These results were in agreement with previously published studies13,25.
The 50 masses were then further re-categorized by a combination method of elastography and Doppler, where cut-off value (AUC 0.967) obtained by plotting the ROC curve was >2 score (i.e. at least three positive variables out of eight variables). The diagnostic performance of the combined method was found to have high sensitivity (100%), specificity (76.47%), PPV (89.19%), NPV (100%) and accuracy (92%) in tandem with proposing the combined use of elastography and Doppler to increase the diagnostic performance13,14,26,27.
Elastography technique has its own limitations. The softer nature of DCIS (ductal carcinoma in situ), invasive lobular, papillary, mucinous and medullary carcinomas and lesions with areas of central necrosis may lead to false negative results. Involuting/calcified fibroadenoma often leads to false positive elastography findings owing to their excessive stiffness. Other inherent limitations of strain elastography which attribute to misdiagnosis are the deeper location of the lesion and an extremely high or low density of parenchyma, which hinder proper evaluation. In a study from China, elastographic diagnostic sensitivity and specificity in BI-RADS 4 lesions were found to be 90.1 and 85.7 per cent, respectively28.
Combining Doppler with elastography was observed to help in overcoming the short comings of elastography alone, by increasing specificity (from 70.59% to 76.47%), accuracy (90% to 92%) and PPV (86.84% to 89.19%) of the technique. In this study, strain ratio alone was found to have the same sensitivity, specificity and accuracy as the combination method. However, soft masses like medullary cancer and mucinous cancer may depict false negative values on elastography and may be downgraded as benign lesions29. Also addition of Doppler technique could demonstrate high spectral flow parameters of vessels within the mass due to the abnormal neo-angiogenesis14. Thus the combination method of elastography and Doppler would help in better characterization of these indeterminate masses, as indicated by the higher AUC (area under the curve) of ROC curve of combination method in the present study as compared to that of strain ratio or elastography alone14. Moreover, the addition of elastography and Doppler to routine ultrasound was found to increase the PPV of screening ultrasound in women with dense breasts, while reducing the number of false-positive findings without missing cancers30. It was observed that addition of elastography in the same session of ultrasound, would take about five minutes more than the conventional ultrasound examination, but improves the accuracy of diagnostic efficiency assessed by the BIRADs scoring system31. The time taken for B mode ultrasound of both breasts and axilla (with targeted Doppler and elastography evaluation of the mass lesion) varies from case to case, depending on the amount of breast parenchyma in each patient. In our experience, ultrasound of bilateral breasts with the combined method takes only around 15-20 min per person on an average.
However, our study had some limitations. The sample size was small and hence needs further work in the field for adequate validation and standardization of the techniques. Furthermore, a larger sample size would allow for the application of binary logistic regression for calculating the predicted probability of the combination method and further application of the ROC curve on the predicted probability. Shear wave elastography technique, which quantifies tissue stiffness accurately, was not performed. Performance of strain elastography and Doppler is operator dependent and depends on myriad factors such as breast size, density, depth and proximity of lesion to nipple/areola, adequate compression and need for avoiding lateral/angulated movements, making it hard to achieve consistent image representation. Certain extent of subjectivity in elastography scoring, neither intra-observer variability nor image acquisition reproducibility has been made allowance for. Furthermore, re-categorization after the combined method did not significantly modify management for the majority of BI-RADS 4B or 4C masses as they remained either BI-RADS 4 or 5, with the result that they had to be biopsied anyhow.
The main target lesions which would benefit from the utilization of combined method would be BI-RADS 3 and 4A lesions, which would undergo a different management plan when upgraded to BI-RADS 4 or downgraded to BI-RADS 3 categories, respectively. Majority of ultrasound BI-RADS 3 lesions (90%) were found to be benign in the present study. Only two cases of BI-RADS 3 were upgraded to 4A category after combined assessment, of which one turned out to be malignant and hence the combined assessment prevented missing cancer.
BI-RADS 4 category masses are managed conventionally based on tissue diagnosis. A favourable result obtained in the study was the downgradation of seven of the nine BI-RADS 4A lesions to 3 category, thus prompting follow up instead of biopsy. Hence, specificity of making decision for biopsy increased from 70.8 to 89.4 per cent when B-mode ultrasound was combined with Doppler and strain elastography, without statistical change in sensitivity. Conversely, our approach also impeaches the risk accompanying false-negative biopsy. Suspicious elastographic or Doppler features in biopsy negative BI-RADS 4 lesions indicate a highly augmented risk for malignancy. Therefore, whenever a BI-RADS US 4 lesion suspicious for malignancy after combined assessment shows no evidence of malignancy on histological evaluation, a re-biopsy may be recommended in view of a possible false-negative scenario. No significant change in management could be hypothesized for 4B and 4C lesions, stressing the fact that BI-RADS categorization based on morphological characters on B – mode ultrasound which evokes suspicion of >10 per cent for malignancy in the radiologist, have no other management consensus other than tissue diagnosis.
In conclusion, the combined use of Doppler and elastography could improve the diagnostic value of B-mode ultrasound that aids in characterizing BI-RADS 3 and 4 masses the aides in decision making for biopsy. According to the BI-RADS classification, downgrading of category 4A lesion to 3 changes the management line from tissue diagnosis to short-term follow up, which could reduce the patient anxiety and discomfort in sampling from a sensitive area like the breast as well as reduce the overall biopsy workload and expenses. Hence, this easily available, simple and economical combination method of strain elastography and Doppler not only overcomes the limitations of individual techniques, but also potentially increases the level of confidence of the astute radiologist in the evaluation of indeterminate breast lesions, with a promising role especially in resource-poor countries.
Footnotes
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- 1. Sung H, Ferlay J, Siegel R, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020:GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2. Houssami N, Lord SJ, Ciatto S. Breast cancer screening:Emerging role of new imaging techniques as adjuncts to mammography. Med J Aust. 2009;190:493–7. doi: 10.5694/j.1326-5377.2009.tb02526.x. [DOI] [PubMed] [Google Scholar]
- 3. Kuhl CK. Current status of breast MR imaging. Part 2. Clinical applications. Radiology. 2007;244:672–91. doi: 10.1148/radiol.2443051661. [DOI] [PubMed] [Google Scholar]
- 4. Zonderland HM, Hermons J. Ultrasound variables and their prognostic value in a population of 1103 patients with 272 breast cancer. Eur Radiol. 2000;10:1562–8. doi: 10.1007/s003300000585. [DOI] [PubMed] [Google Scholar]
- 5.American College of Radiology. ACR BI-RADS®Atlas 5th Edition. [accessed on August 1, 2021]. Available from:https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Bi-Rads .
- 6. Hawley JR, Kalra P, Mo X, Raterman B, Yee LD, Kolipaka A. Quantification of breast stiffness using MR elastography at 3 Tesla with a soft sternal driver:A reproducibility study. J Magn Reson Imaging. 2017;45:1379–84. doi: 10.1002/jmri.25511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sinkus R, Siegmann K, Xydeas T, Tanter M, Claussen C, Fink M. MR elastography of breast lesions:Understanding the solid/liquid duality can improve the specificity of contrast-enhanced MR mammography. Magn Reson Med. 2007;58:1135–44. doi: 10.1002/mrm.21404. [DOI] [PubMed] [Google Scholar]
- 8. Ozturk A, Grajo JR, Dhyani M, Anthony BW, Samir AE. Principles of ultrasound elastography. Abdom Radiol (NY) 2018;43:773–85. doi: 10.1007/s00261-018-1475-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Barr RG, Destounis S, Lackey LB, 2nd, Svensson WE, Balleyguier C, Smith C. Evaluation of breast lesions using sonographic elasticity imaging:A multicenter trial. J Ultrasound Med. 2012;31:281–7. doi: 10.7863/jum.2012.31.2.281. [DOI] [PubMed] [Google Scholar]
- 10. Itoh A, Ueno E, Tohno E, Kamma H, Takahashi H, Shiina T, et al. Breast disease:Clinical application of US elastography for diagnosis. Radiology. 2006;239:341–50. doi: 10.1148/radiol.2391041676. [DOI] [PubMed] [Google Scholar]
- 11. del Cura JL, Elizagaray E, Zabala R, Legórburu A, Grande D. The use of unenhanced Doppler sonography in the evaluation of solid breast lesions. AJR Am J Roentgenol. 2005;184:1788–94. doi: 10.2214/ajr.184.6.01841788. [DOI] [PubMed] [Google Scholar]
- 12. Yang WT, Tse GM, Lam PK, Metreweli C, Chang J. Correlation between color power Doppler sonographic measurement of breast tumor vasculature and immunohistochemical analysis of microvessel density for the quantitation of angiogenesis. J Ultrasound Med. 2002;21:1227–35. doi: 10.7863/jum.2002.21.11.1227. [DOI] [PubMed] [Google Scholar]
- 13. Elkharbotly A, Farouk HM. Ultrasound elastography improves differentiation between benign and malignant breast lumps using B- mode ultrasound and color Doppler. Egypt J Radiol Nucl Med. 2015;10:1231–39. [Google Scholar]
- 14. Liu D, Huang Y, Tian D, Yin J, Deng LJ. Value of sonographic bidirectional arterial flow combined with elastography for diagnosis of breast imaging reporting and data system category 4 breast masses. J Ultrasound Med. 2015;34:759–66. doi: 10.7863/ultra.35.5.759. [DOI] [PubMed] [Google Scholar]
- 15. Lee KA, Talati N, Oudsema R, Steinberger S, Margolies LR. BI-RADS 3:Current and future use of probably benign. Curr Radiol Rep. 2018;6:5. doi: 10.1007/s40134-018-0266-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Brown AL, Phillips J, Slanetz PJ, Fein-Zachary V, Venkataraman S, Dialani V, et al. Clinical value of mammography in the evaluation of palpable breast lumps in women 30 years old and older. AJR Am J Roentgenol. 2017;209:935–42. doi: 10.2214/AJR.16.17088. [DOI] [PubMed] [Google Scholar]
- 17. Graziano L, Bitencourt AG, Cohen MP, Guatelli CS, Poli MR, Souza JA, et al. Elastographic Evaluation of Indeterminate Breast Masses on Ultrasound. Rev Bras Ginecol Obstet. 2017;39:72–9. doi: 10.1055/s-0036-1597753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. ElSaid N, Mohamed H. Sonoelastography versus dynamic magnetic resonance imaging in evaluating BI-RADS III and IV breast masses. Egypt J Radiol Nucl Med. 2012;43:293–300. [Google Scholar]
- 19. Strobel K, Schrading S, Hansen NL, Barabasch A, Kuhl CK. Assessment of BI-RADS category 4 lesions detected with screening mammography and screening US:Utility of MR imaging. Radiology. 2015;274:343–51. doi: 10.1148/radiol.14140645. [DOI] [PubMed] [Google Scholar]
- 20. Navarro B, Ubeda B, Vallespí M, Wolf C, Casas L, Browne JL. Role of elastography in the assessment of breast lesions:Preliminary results. J Ultrasound Med. 2011;30:313–21. doi: 10.7863/jum.2011.30.3.313. [DOI] [PubMed] [Google Scholar]
- 21. Gheonea IA, Stoica Z, Bondari S. Differential diagnosis of breast lesions using ultrasound elastography. Indian J Radiol Imaging. 2011;21:301–5. doi: 10.4103/0971-3026.90697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gokalp G, Topal U, Kizilkaya E. Power Doppler sonography:Anything to add to BI-RADS US in solid breast masses? Eur J Radiol. 2009;70:77–85. doi: 10.1016/j.ejrad.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 23. Madjar H, Prömpeler HJ, Sauerbrei W, Wolfarth R, Pfleiderer A. Color Doppler flow criteria of breast lesions. Ultrasound Med Biol. 1994;20:849–58. doi: 10.1016/0301-5629(94)90045-0. [DOI] [PubMed] [Google Scholar]
- 24. Lee WJ, Chu JS, Huang CS, Chang MF, Chang KJ, Chen KM. Breast cancer vascularity:Color Doppler sonography and histopathology study. Breast Cancer Res Treat. 1996;37:291–8. doi: 10.1007/BF01806510. [DOI] [PubMed] [Google Scholar]
- 25. Bardhan J, Ghosh SK, Sarkar K, Paul S, Nandi D. Color Doppler evaluation of palpable breast lump along with cytological/histopathological correlation. Scholar J of App Med Sci. 2016;4:2553–6. [Google Scholar]
- 26. Cho N, Moon WK, Kim HY, Chang JM, Park SH, Lyou CY, et al. Sonoelastographic strain index for differentiation of benign and malignant non-palpable breast masses. J Ultrasound Med. 2010;29:1–7. doi: 10.7863/jum.2010.29.1.1. [DOI] [PubMed] [Google Scholar]
- 27. Cho N, Jang M, Lyou CY, Park JS, Choi HY, Moon WK. Distinguishing benign from malignant masses at breast US:Combined US elastography and color Doppler US--influence on radiologist accuracy. Radiology. 2012;262:80–90. doi: 10.1148/radiol.11110886. [DOI] [PubMed] [Google Scholar]
- 28. Liu XJ, Zhu Y, Liu PF, Xu YL. Elastography for breast cancer diagnosis:A useful tool for small and BI-RADS 4 lesions. Asian Pac J Cancer Prev. 2014;15:10739–43. doi: 10.7314/apjcp.2014.15.24.10739. [DOI] [PubMed] [Google Scholar]
- 29. Zeinhom F, Abu AA. Real-time tissue elastography combined with BI-RADS US classification system for improving breast lesion evaluation. Egypt J Radiol Nucl Med. 2014;45:1021–8. [Google Scholar]
- 30. Lee SH, Chung J, Choi HY, Choi SH, Ryu EB, Ko KH, et al. Evaluation of screening us-detected breast masses by combined use of elastography and color Doppler US with B-mode US in women with dense breasts:A multicenter prospective study. Radiology. 2017;285:660–9. doi: 10.1148/radiol.2017162424. [DOI] [PubMed] [Google Scholar]
- 31. Zahran MH, El-Shafei M, Emara DM, Eshiba SM. The role of ultrasound elastography in evaluation of breast masses. Acta Sci Med Sci. 2019;3:140–51. [Google Scholar]