Abstract
Adopting sun exposure as a low-cost sustainable strategy in tropical countries needs critical analysis for its feasibility and inclusion in national policy. This review explores the opportunities and challenges associated with sun exposure in tropical countries and discusses potential strategies that may be adopted for promoting sun exposure. For this, two strands of evidence were reviewed; trials on sun exposure, analysed for risk of bias and, the environmental factors that influence acquisition of vitamin D from sun exposure in the context of on-going ecological and nutritional transition. Compilation of data from available databases in terms of deficiency, per cent rural population, status of fortification, air pollution, ultraviolet index, skin reflectance and skin cancer prevalence were done. In the context of environmental and lifestyle-related challenges, opportunities go hand-in-hand in terms of built environment, variability in air pollution and personal factors such as skin pigmentation, precursor availability and general nutritional status. Contextual policy decisions should consider urban and rural development planning, control of air pollution, targeted guidelines for indigenous and immigrant population and use of space technology in educating general population for balanced sun exposure as essential components for a sustainable strategy. Important opportunities exist for tropical countries to develop sun exposure as a strategy for acquiring vitamin D and these need to be explored.
Keywords: Challenges and opportunities, sun exposure, tropical countries, vitamin D
Vitamin D deficiency is now known to be a global public health problem, irrespective of sunlight availability1. This has challenged the concept that natural sun exposure and the downstream events would fulfil the bodily demands. While rapid correction of the current deficiency requires short-term strategies such as supplementation or fortification, there needs to be a sustainable solution to the problem in the years to come.
Sun exposure is so far the most sustainable solution to the problem of widespread vitamin D deficiency especially in case of tropical countries. Moreover, vitamin D-independent benefits of sun exposure have also been indicated, and therefore, sun exposure cannot be completely replaced by fortification or supplementation. For example, ultraviolet (UV) exposure is postulated to promote the synthesis of opioid beta-endorphins which are mood elevators, and UVA-generated nitric oxide can improve cardiovascular health2. Higher sun-seeking behaviour has been linked to reduce all-cause mortality in a dose-dependent manner in Sweden3. Further, a latitude dependency has been observed in the case of carotid artery atheroma and cardiovascular mortality3. There is therefore a need to explore the possibilities of a balanced sun exposure in the population groups residing in tropical countries. The aim of the present review was to examine the scientific evidence related to the challenges and opportunities for using sun exposure as a sustainable strategy for combating vitamin D deficiency by reviewing trials that used sun exposure as an intervention. Studies which used artificial sources of UVB as an intervention were not considered. Environmental and other factors (precursor, skin colour, calcium status, safety, and other micronutrient deficiencies) that influence acquisition of vitamin D from sun exposure in the context of ongoing ecological and nutrition transition were also reviewed. Although the global evidence was considered for this review, for specific analysis of environmental factors, India was taken as a case study.
Exploring sun exposure as a strategy to enhance vitamin D status: Inadequacy of vitamin D in tropical countries is thought to be a paradox. Table I presents the reported data on vitamin D inadequacy in tropical countries. The inadequacies reported were variable with a lower prevalence of 11 per cent in Fiji to >70 per cent in Bangladesh4,5,6. The environmental and personal factors such as air pollution and dress code could be the major factors underlying these differences. Even though there are Nation wide efforts to fortify vitamin D in commonly consumed foods, the major source of vitamin D remains to be sun exposure7 (Table I).
Table I.
Vitamin D inadequacy in developing countries lying partially between the Tropic of Cancer and Capricorn
| Country | Latitude | Percentage <50 nmol/l4 | Rural population5 | PM2.559 Weighted annual concentration | Status of fortification6 |
|---|---|---|---|---|---|
| Malaysia | 4°21 | 70 | 25 | 13.2 | Mandatory |
| Tanzania | 6°37 | 23 | 68 | 23 | Mandatory |
| Sri Lanka | 7°87 | 49.5 | 82 | 28 | Voluntary |
| Nigeria | 9°08 | 19.5 | 52 | 30 | Mandatory |
| Vietnam | 14°06 | 35 | 66 | 29 | Nil |
| Fiji | 17°71 | 11 | 46 | 7 | Nil |
| Brazil | 23°6 | 77 | 14 | 21.7 | Nil |
| Bangladesh | 23°68 | 80 | 66 | 83.3 | Nil |
| India | 26° | 66 | 67 | 60.6 | Voluntary |
| Pakistan | 30°37 | 58 | 61 | 115.7 | Voluntary |
| Chile | 35°67 | 40 | 10 | 26.8 | Voluntary |
Metabolic fate of vitamin D (synthesis storage and longer biological half-life): The precursor for vitamin D in human skin is 7-dehydrocholesterol (DHC). The main source of 7-DHC is the Malpighian layer of the epidermis8. The circulating 7-DHC is not considered to have a significant role in the formation of vitamin D9. Some studies have shown a relationship between systemic high-density and low-density lipoprotein cholesterol levels and DHC reductase-7 activities in keratinocytes10. An increase in 25-hydroxyvitamin D [25(OH)D] level after UVB exposure has also been positively correlated with baseline total cholesterol level (P<0.005)11. Ecological studies on the association between latitude, sunlight and cholesterol have also shown some interesting findings12. Blood cholesterol increased with distance from the Equator (4.14 nmol/L at 33° N to 6.86 nmol/L at 63° N), and there was an increase in age-adjusted death rates with decreasing hours of sunshine exposure per annum. This was however, attributed to the progression of squalene metabolism to cholesterol synthesis rather than to vitamin D synthesis.
Following sun exposure, the peak concentrations of circulating cholecalciferol (vitamin D3) are achieved between 24 and 48 h. In liver, cholecalciferol is hydroxylated to 25-hydroxyvitamin D3 [25(OH)D3], which is the major circulating form of vitamin D. Production of 1,25(OH)2D3 is effected by the enzyme 25(OH)D-1α-hydroxylase and is tightly regulated by serum phosphorus, parathyroid hormone (PTH) levels and a number of other factors10. Unaltered vitamin D (cholecalciferol) is the major storage form in the adipose tissue13. Storage in the adipose tissue forms the largest exchangeable pool for vitamin D, increasing its half-life to 2-4 months. The serum half-life of 25(OH)D3 is approximately 15 days14.
Skin-fold thickness, a measure of adiposity, has shown a positive association with Body Mass Index (BMI) and a negative association with 25(OH)D in normal weight post-menopausal women. An age-related decline in 25(OH)D was also observed15. However, in case of obese subjects, this relationship seems to be different. A meta-analysis on the association between vitamin D deficiency and obesity among Asians and European-Americans has reported higher odds of deficiency in obese as compared to healthy controls16. Several reasons have been proposed for this association including low sun exposure and physical inactivity17, volumetric dilution or sequestration of vitamin D in subcutaneous fat depots18 and decreased bioavailability of vitamin D because of its deposition in body fat compartments19. Therefore, the role of the precursor availability as a determinant of vitamin D deficiency is a research area, which is in the nascent stage and needs to be understood further.
Cutaneous vitamin D and skin colour: Darker skin absorbs more UVB in the melanin than the skin of White people and, therefore, to acquire the same amount of vitamin D, they may require a higher amount of sun exposure20,21,22. The amount of vitamin D production based on skin type can be optimized using minimal erythemal dose (MED, a measure of redness of skin with UV radiation). Studies using artificial UV sources, which have equalized the dose of sun exposure based on MED, have reported a similar capacity of producing vitamin D by Asian skin types as compared to Caucasians23. Since MEDs are higher for Asian/African skin types, the sun exposure time required may be more, but the insolation is also abundant in the tropical countries24,25. Immigrant Asian population, in temperate countries where the intensity and duration of sunshine are less, show higher incidence of vitamin D inadequacy and therefore result in higher incidence of inadequacy21. One study from the UK reported that an optimized sun exposure that equals to holiday sunshine in the UK did not produce sufficient vitamin D in immigrants with darker skin type21.
Experiences from the African continent (Tanzania, 2-4°S of Equator) among indigenous population also support the above evidence24,25. The participants from different African five ethnic groups were found to have high concentrations of 25(OH)D in their blood (115 nmol/L), irrespective of the fish consumption and their darkest complexion (skin type VI)24,25. Therefore, available evidence from Asia and Africa suggests that despite the darker skin type of people, sun exposure may be an effective strategy to prevent vitamin D deficiency.
Global evidence for sun exposure meeting daily requirements of vitamin D: The controlled trials which utilized sun exposure as a strategy for enhancing vitamin D status are summarized in Table II. The studies found a positive effect in enhancing 25(OH)D3 status, with increment ranging from 0.6 to 13.9 nmol/L. However, two of these studies were not randomized and were pilot studies26,27,28,29,30,31.
Table II.
Intervention studies using sun exposure as a source for vitamin D
| Country/latitude | Type of study | Group | Duration | Time | Change in 25(OH)D status/baseline and end-line | Conclusion | Risk of bias analysis |
|---|---|---|---|---|---|---|---|
| Al Ain, UAE, 34.0° N26 | Pilot parallel group trial | RCT, 8 women | Four weeks | 15 min, face, arms and hands | Mean increase of 5.4 nmol/l | Deficiency related to sun exposure behaviours and supplements | Pilot study |
| Sydney, Australia, 33.87° S27 | Cluster RCT | 602 elderly aged 70 or more from 51 aged care facilities | 12 months | 30-40 min/day, early morning, with or without calcium | Increment of 5.9 nmol/l in status. Risk of falls decreased with increase in number of sun exposure sessions attended (IRR, 0.52; 95% CI, 0.31-0.88; P=0.01) | Sun exposure strategy is in effective most likely due to poor adherence to intervention | Concerns with respect to start and adherence to intervention, missing outcome data |
| Abu Dhabi, UAE, 24° N30 | Pilot parallel group trial, Natural sun exposure | 20 female students | 12 wk | Face, arms and hands for 60 min per week | Mean increment of 3.6 nmol/l compared to a drop in control group | Sunlight exposure could be an effective way to improve the vitamin D status among females | Pilot study |
| Delhi, India, 28.61° N28 | Parallel group trial | 36 boys, 35 girls | Four weeks | 30 min between 11:15 and 11:45 AM in summer | Increase of 0.6 nmol/l | Significant increase in serum 25(OH)D | Risk with respect to deviation from intended intervention, selection of reported result |
| Delhi, India, 28.61° N31 | Pre-post trial | School children aged 10-15 yr 50 boys and 155 girls | Four weeks in winter | 30 min/day with 10 per cent exposure between 11:00 AM and 12 noon in winter | Decrease of 0.48 nmol/l predominant decrease in girls | Supplementation required in winter | Elements of RCT missing for RoB analysis |
| Pune, India, 18.52° N29 | Prospective, randomized (1:1), open-label, parallel group | Adult men 40-60 yr | Six months | 20 min daily on face and forearms between 11:00 AM and 3:00 PM over and above current exposure | Mean increment of 13.9 nmol/l | Significant increment in 25(OH)D with exposure between June and December | Concerns with respect to missing outcome data and measurement of outcome data |
RoB, risk of bias; RCT, randomized controlled trials; IRR, incidence rate ratio; CI, confidence interval; 25(OH)D, 25-hydroxy vitamin D
Cross-sectional studies have also been conducted to understand the association between sun exposure and vitamin D. One study from Delhi, India, has examined the role of sun exposure in acquiring daily requirement of vitamin D32. Men with varying degrees of outdoor sun exposure were studied during August-September 2015. Outdoor workers with prolonged sun exposure had sufficient vitamin D based on blood markers. Sun exposure was the only significant determinant of vitamin D status, increasing serum 25(OH)D by about 2 ng/ml/h of sun exposure per day [95% confidence interval (CI) 1.8-2.3; P<0.001] after adjusting for serum vitamin D-binding protein levels32. Outdoor workers with an average exposure of 4.4 h daily have been reported to have higher serum 25(OH)D compared to indoor workers with an exposure of 0.9 h per day from Israel33. Rural women in Malaysia who spent more hours in sun had mean 25(OH)D levels almost double than that of urban women34. This is despite a lower body surface area exposure among rural women.
A systematic review including 71 studies across the globe with representations from tropical developing countries, such Bangladesh, Pakistan, Malaysia, India and China, assessed the relationship between occupation and vitamin D deficiency. Compared to outdoor workers, indoor workers had a significantly lower 25(OH)D (40.6±13.3 vs. 66.7±16.7 nmol/l), indicating the influence of lifestyle factors including sun exposure on vitamin D. Shift-workers, healthcare workers and other indoor workers were at the highest risk of deficiency35.
Other host-related factors: The most important factors that regulate the production of 1,25(OH)2D3 are serum calcium, phosphorus and PTH levels. The wide individual differences in vitamin D status may also be related to the differences in calcium status36. Previous studies done in this area had proposed two mechanisms to explain the role of low calcium intakes as a determinant of vitamin D deficiency37,38. A shorter half-life of serum 25(OH)D on account of an increased conversion to 1,25(OH)D to enhance calcium absorption to compensate for the low calcium intake is one such mechanism. An increase in hepatic conversion of vitamin D to polar inactivation products in conditions of calcium deprivation is another mechanism, but it has been demonstrated only in animals37. Hypotheses on similar lines have been proposed regarding the possibility of a secondary vitamin D deficiency with low calcium intakes based on two studies among outdoor workers with different calcium intakes38. More research is, however, needed to shed light on these mechanisms.
Genetic predisposition has also been associated with vitamin D insufficiency39. However, since it is a non-modifiable factor and conclusive evidence has not been generated in this area.
Methodology for assessment of 25(OH)D: The reported prevalence of vitamin D deficiency in a given population depends on the method used40. It is also known that optimum levels of vitamin D are also not established with lack of dose-response studies and studies on calcium absorption and vitamin D.
The reporting on the prevalence of deficiencies needs to be supported by standardized methodologies considered as gold standard41. Often, the methodology used is immunoassays42, which have wide variances compared to methods such as high-performance liquid chromatography. Standardized methodologies with more specific biomarkers are required to define deficiency in the population43.
Co-existence of vitamin D deficiency with other micronutrient deficiencies: Unlike developed countries where single nutrient deficiency is common, in developing countries, the manifestations of vitamin D deficiency are quite complex with concurrent deficiencies of several nutrients44, the cumulative effect of which is not known. As in the case of other micronutrients such as iron or vitamin A, a situation where multiple nutrient deficiencies would be leading to exacerbation of vitamin D deficiency cannot be ruled out.
Safety of cutaneous versus supplemental vitamin D: The UV radiation-induced production of vitamin D precursors is counter balanced by degradation of vitamin D and its precursors to photo end-products45. During prolonged exposure to UV radiation, a steady state is attained with a 10-15 per cent cutaneous conversion of 7-DHC to pre-vitamin D3. It is postulated that this process of photo-regulation ensures that under conditions of excessive sun exposure, toxicity does not occur46. On the other hand, for vitamin D supplementation, counter-regulatory mechanisms are reported to operate at a dose range of 800-20,000 IU by maintaining the serum 25(OH)D concentration at a range of <75-220 nmol/l. However, at doses higher than that mentioned above, a sharp rise in dose–response curve has been reported probably exceeding the capabilities of various mechanisms regulating 25(OH)D47. High doses of >50,000 IU ingested weekly from one to four months have reported to cause adverse effects48,49. The cautions that need to be followed for a successful supplementation regimen and the varying bioavailability reported for different forms of supplements50,51 add on to the desirability of sun exposure as a source of vitamin D.
Nutrition–ecological transition
Transition from adequacy to inadequacy (the urban–rural differences in prevalence of vitamin D deficiency): Urbanization and lifestyle changes over the past few decades have affected the vitamin D status globally52,53. Non-agricultural activity, consequent migration and resultant overcrowding, pollution of air, water and noise in cities due to industrial development are major problems associated with urbanization. In addition, on account of the known adverse effects of extreme sun exposure such as skin cancer, people tend to spend more time indoors in several countries.
In contrast to Europe and the United States, where only <20 per cent population is rural, in several developing countries, about 40 per cent of the population5 lives in rural areas. The rural–urban differences in vitamin D status are significant with urban residents having a higher prevalence of vitamin D deficiency as reported in South-East Asian nutrition surveys54 and surveys in tropical countries, such as Malaysia, Ethiopia and Thailand34,55,56. However, even among rural agricultural labourers who spend around eight hours per day outdoors and have a considerable body surface area exposed, a higher prevalence of vitamin D deficiency has been reported to the order of 44-70 per cent57. Therefore, it appears that the determinants of vitamin D deficiency in rural and urban contexts need to be understood separately before developing strategies for tackling vitamin D deficiency.
How vitamin D status is affected by air pollution [trends in aerosol optical density (AOD) and particulate matter (PM)]: Particulate matter (PM) is made up of a number of components, including acids (such as nitrates and sulphates), organic chemicals, metals and soil or dust particles and is a derived parameter from AOD58. As per the standards set by the WHO58, the annual mean PM2.5 value should be around 10 µg/m3, while all the cities in India have been reported to have an average above this59.
The extent of solar UVB that reaches earth surface is negatively affected by the level of air pollution60. In two cities of Iran with high and low air pollution (Tehran and Ghazvin), a study was undertaken in 200 free living women aged 20-55 yr, to understand the effect of air pollution and vitamin D status. The ground-level UVB was measured to be almost double in the less polluted area compared to the area with higher pollution. Although the altitude differences between the two places accounted for around 12 per cent of the difference in ground-level UVB, the influence of air pollution had a significant effect. The odds of vitamin D deficiency was five times (OR, 5.22; 95% CI, 2.2-12.2; P<0.001) in the higher polluted area compared to the area with lower pollution60.
Vitamin D status and sun exposure index (SEI) among rural and urban residents were examined by a group of researchers from Belgium61. SEI was derived from their reported sun exposure times and percentage of body surface area exposed. 25(OH)D serum levels increased linearly as the index of sun exposure increased. For the same 25(OH)D level, the urban inhabitants required about three times more SEI when compared to the rural counterparts. For any given SEI, the vitamin D status was lower when compared to the rural dwellers. This indicated that the amount of UVB reaching the earth may have been significantly altered due to air pollution in case of urban setting61. In Romania, where the prevalence of vitamin D deficiency was about 65 per cent, it was found that the total body bone mineral density was inversely associated with indicators of air pollution62.
Risk of high exposure and skin cancer: The Ultraviolet Index (UVI) is a measure of the amount of skin damaging UV radiation expected to reach earth’s surface at the time when the sun is highest in the sky, i.e. around midday63. The compilation of TEMIS (Tropospheric Emission Monitoring Internet Service) satellite data among tropical countries shows abundant insolation across the year64 almost double than that of a temperate country. This necessitates a guideline on sun exposure which would prevent over exposure but would recommend limits of exposure for synthesis of vitamin D across seasons.
Skin reflectivity also appears to be in favour of tropical countries in protecting against cancer. The latitudinal dependence of skin colour is already well known; farther from Equator, lighter the skin colour65. This evolutionary change is considered to be protective against UV radiation65. An association between darker skin typology and lower DNA damage has been reported which indicates skin cancer protective effects of darker skin types66.
Exposure to intense ambient radiation is a risk factor for cataract67. Therefore, balanced sun exposure avoiding high-intensity radiation or protecting eyes while exposing to the sun should be practised for optimum sun exposure. In tropical countries, UVI, which indicates over exposure would aid in practising appropriate protective measures to prevent sunburn in summer and sun exposure for vitamin D in other seasons.
Way forward in developing sun exposure as a sustainable strategy for vitamin D: The opportunities and challenges that tropical countries need to face for strategizing sun exposure for acquiring vitamin D are summarized in Table III and Figure.
Table III.
Challenges and opportunities associated with utilizing sun exposure as a feasible strategy for tropical developing countries
| Opportunities | Challenges | Way forward |
|---|---|---|
| Longer half-life and safety of 25(OH)D | Balanced seasonal exposure for storage during lean period | Season-specific guidelines using satellite data Popularization of UV index using mobile applications and monitoring |
| Scattered evidence on positive impact of sun exposure under controlled settings | Translating the strategy requires careful analyses of associated factors | Generating high-quality evidence |
| Less prevalence of deficiency in rural areas | Low outdoor activity and low body surface area exposure in urban areas | Policy directions to promote out-door physical activity Facilitative built environment changes conducive for sun exposure especially for females |
| Regional differences in air pollution | Polluted air hindering insolation especially in urban areas | Policy directives to reduce pollution |
| Adaptive darker skin colour in tropics | Immigrant population not adaptive | Native and immigrant populations require separate policy decisions guidelines |
| Multiple strategies to control multiple micronutrient deficiencies | Interactions among micronutrients due to multiple deficiencies | National health policy on holistic approach, establish dose-response relationship with calcium |
| Cutaneous synthesis of vitamin D is not affected by cutaneous precursor availability | Associations with cholesterol/ body weight reported. Also, age-related decline in cutaneous 7-dehydrocholesterol has been reported. | Understand the interactions between precursor and 25(OH)D syntheses in the current scenario of malnutrition. Specific guidelines/strategies for elderly |
Figure.
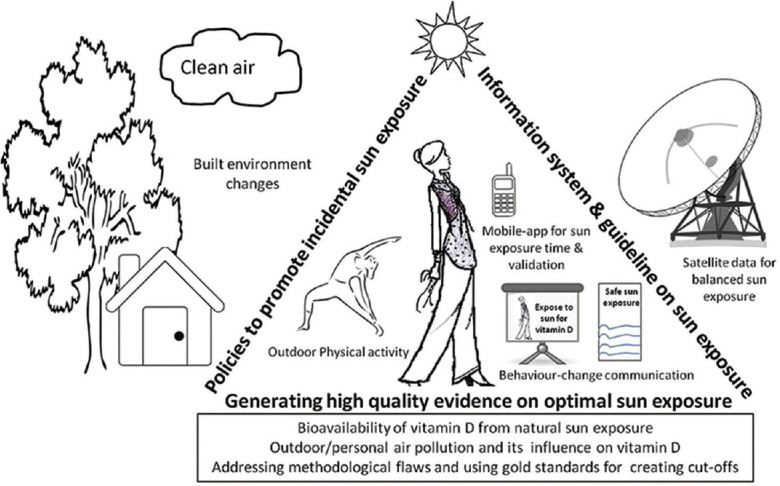
Schematic representation of strategies to be adopted for prioritizing sun exposure in tropical developing countries.
Region-specific guidelines for balanced sun exposure: Detailed guidelines in countries such as the UK and the USA concentrate on preventing skin cancer and safe sun exposure for vitamin D68,69. Such guidelines are, however, lacking in the Asian context and needs to be incorporated in the dietary guidelines to increase awareness on UVI in the general population. It is also necessary to create targeted guidelines for indigenous and immigrant populations since the immigrant population will not have the advantage of latitude-dependent adaptive changes31,32.
Use of space technology for creating guidelines: Space technology can be a powerful tool for estimating the time and duration of sun exposure and thereby help in creating a guideline for promoting balanced sun exposure70,71. This technology can prove to be beneficial in generating database on estimating the sun exposure time required for adequate synthesis of vitamin D at a given place and time on a day-to-day basis. Due to large geographical area coverage and the resolution the technology can provide guidance for promoting sun exposure.
Creating built environment conducive for vitamin D and synergizing sun exposure with other lifestyle interventions: Built environment has a significant impact on the health of people residing in an urban environment. Planners need to be innovative on constructing built environment which would facilitate natural vitamin D synthesis by designing open spaces conducive for sun exposure72. Building models which would optimize sun exposure during different seasons and utilization of sun control and shade devices wherever appropriate need to be thought about. For instance, when UV radiation transmitted through different types of glass was studied, it was found that all glasses (laminated, ordinary, coloured) blocked UVB radiation totally while smooth ordinary glass (4 mm thick) transmitted 66.6-74.3 per cent of UVA, depending upon the distance from the source and intensity of radiation falling on the surface73.
Built environment changes in schools and neighbourhood, such as ‘walking school bus’, where children move in groups to school, sidewalks and bicycle routes for safe commutation to school in order to prevent overweight would help in enhancing sun exposure too74.
Utilizing shade: Shaded environments may also be utilized for sun exposure without experiencing the high levels of UVA of full sun75,76. At 27.6° S (Australia), diffuse UV under shade has been proved to be capable of providing the human body with adequate levels of UVD3 (290-315 nm) radiation77,78.
Utilizing sun of less intensity in summer and possibility of storage for winter: Tropical areas receive a relatively high UVB to UVA ratio which requires less exposure per day for acquiring vitamin D. Based on in vitro studies, vitamin D effective radiation is also high, ranging with conversions from 3.4 per cent at 9:00 AM to a maximum of 16.1 per cent at 1:00 PM and drop there on (latitude 13.40° N)79.
The ideal time of sun exposure for maximum conversion of 7DHC to 25(OH) D is therefore during 11:00 AM to 2:00 PM80. However, photo-conversion occurs from 9:00 AM onwards. These early hours may be utilized for vitamin D synthesis during summer when UVI is maximum in India. At 6° South (Jakarta), exposure to sunlight at 9:00 AM which contained about 0.6 MED/h, exposing to sunlight for 25 min with 25 per cent BSA exposure, three times a week for six weeks led to an increase of mean 25(OH)D levels of participants from 59 nmol/l at the baseline to 84 nmol/l in elderly81.
Overall, it appears that sun exposure can be effective for tropical countries in enhancing vitamin D status, but excessive sun exposure needs to be avoided due to associated risks of skin cancers. Robust research needs to be taken up in the area of sun exposure for vitamin D synthesis. Outdoor physical activity and suitable modifications in built environment need to be included in national guidelines for promoting a balanced sun exposure for vitamin D. The policy level initiatives are required globally for changes in environment with respect to air pollution, in addition to individual efforts in designing and creating an enabling environment. Implementation of guidelines and applying recommended methods of monitoring vitamin D status also lead to creating evidence for sustainability of this approach.
Acknowledgment
We acknowledge Indian Council of Medical Research (ICMR), New Delhi, India, for the ICMR Centenary post-doctoral fellowship to LA and Mr. Srikanth Apsingaker for the artwork used for the info graphic presented in this article.
Footnotes
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- 1. Cashman KD. Vitamin D deficiency: A public health issue in high- and low-income countries or just hype? World Rev Nutr Diet. 2017;118:206–14. doi: 10.1159/000484391. [DOI] [PubMed] [Google Scholar]
- 2. Juzeniene A, Moan J. Beneficial effects of UV radiation other than via vitamin D production. Dermatoendocrinol. 2012;4:109–17. doi: 10.4161/derm.20013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lindqvist PG, Epstein E, Nielsen K, Landin-Olsson M, Ingvar C, Olsson K. Avoidance of sun exposure as a risk factor for major causes of death: a competing risk analysis of the Melanoma in Southern Sweden cohort. J Intern Med. 2016;280:375–87. doi: 10.1111/joim.12496. [DOI] [PubMed] [Google Scholar]
- 4. Palacios C, Gonzalez L. Is vitamin D deficiency a major global public health problem? J Steroid Biochem Mol Biol. 2014;144(Pt A):138–45. doi: 10.1016/j.jsbmb.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The World Bank. World development Indicator tables. Washington, USA: World Bank Group; 2015. [Google Scholar]
- 6.Food fortification Initiative. Global progress. [accessed on October 29, 2019]. Available from: https://www.ffinetwork.org/globalprogress .
- 7. Whiting SJ, Calvo MS. Vitamin D: Nutrition information brief. Adv Nutr (Bethesda, Md) 2021;12:2037–39. doi: 10.1093/advances/nmab051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Reinertson RP, Wheatley VR. Studies on the chemical composition of human epidermal lipids. J Invest Dermatol. 1959;32:49–59. [PubMed] [Google Scholar]
- 9. Glossmann HH. Origin of 7-dehydrocholesterol (provitamin D) in the skin. J Invest Dermatol. 2010;130:2139–41. doi: 10.1038/jid.2010.118. [DOI] [PubMed] [Google Scholar]
- 10. Carbone LD, Rosenberg EW, Tolley EA, Holick MF, Hughes TA, Watsky MA, et al. 25-Hydroxyvitamin D, cholesterol, and ultraviolet irradiation. Metabolism. 2008;57:741–8. doi: 10.1016/j.metabol.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 11. Bogh MK, Schmedes AV, Philipsen PA, Thieden E, Wulf HC. Vitamin D production after UVB exposure depends on baseline vitamin D and total cholesterol but not on skin pigmentation. J Invest Dermatol. 2010;130:546–53. doi: 10.1038/jid.2009.323. [DOI] [PubMed] [Google Scholar]
- 12. Grimes DS, Hindle E, Dyer T. Sunlight, cholesterol and coronary heart disease. QJM. 1996;89:579–89. doi: 10.1093/qjmed/89.8.579. [DOI] [PubMed] [Google Scholar]
- 13. Rosenstreich SJ, Rich C, Volwiler W. Deposition in and release of vitamin D3 from body fat: Evidence for a storage site in the rat. J Clin Invest. 1971;50:679–87. doi: 10.1172/JCI106538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Clements MR, Davies M, Hayes ME, Hickey CD, Lumb GA, Mawer EB, et al. The role of 1,25-dihydroxy vitamin D in the mechanism of acquired vitamin D deficiency. Clin Endocrinol (Oxf) 1992;37:17–27. doi: 10.1111/j.1365-2265.1992.tb02278.x. [DOI] [PubMed] [Google Scholar]
- 15. Need AG, Morris HA, Horowitz M, Nordin C. Effects of skin thickness, age, body fat, and sunlight on serum 25-hydroxy vitamin D. Am J Clin Nutr. 1993;58:882–5. doi: 10.1093/ajcn/58.6.882. [DOI] [PubMed] [Google Scholar]
- 16. Yao Y, Zhu L, He L, Duan Y, Liang W, Nie Z, et al. A meta-analysis of the relationship between vitamin D deficiency and obesity. Int J Clin Exp Med. 2015;8:14977–84. [PMC free article] [PubMed] [Google Scholar]
- 17. Florez H, Martinez R, Chacra W, Strickman-Stein N, Levis S. Outdoor exercise reduces the risk of hypovitaminosis D in the obese. J Steroid Biochem Mol Biol. 2007;103:679–81. doi: 10.1016/j.jsbmb.2006.12.032. [DOI] [PubMed] [Google Scholar]
- 18. Drincic AT, Armas LA, Van Diest EE, Heaney RP. Volumetric dilution, rather than sequestration best explains the low vitamin D status of obesity. Obesity (Silver Spring) 2012;20:1444–8. doi: 10.1038/oby.2011.404. [DOI] [PubMed] [Google Scholar]
- 19. Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72:690–3. doi: 10.1093/ajcn/72.3.690. [DOI] [PubMed] [Google Scholar]
- 20. Nair R, Maseeh A. Vitamin D: The “sunshine” vitamin. J Pharmacol Pharmacother. 2012;3:118–26. doi: 10.4103/0976-500X.95506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Farrar MD, Kift R, Felton SJ, Berry JL, Durkin MT, Allan D, et al. Recommended summer sunlight exposure amounts fail to produce sufficient vitamin D status in UK adults of South Asian origin. Am J Clin Nutr. 2011;94:1219–24. doi: 10.3945/ajcn.111.019976. [DOI] [PubMed] [Google Scholar]
- 22. Farrar MD, Webb AR, Kift R, Durkin MT, Allan D, Herbert A, et al. Efficacy of a dose range of simulated sunlight exposures in raising vitamin D status in South Asian adults: Implications for targeted guidance on sun exposure. Am J Clin Nutr. 2013;97:1210–6. doi: 10.3945/ajcn.112.052639. [DOI] [PubMed] [Google Scholar]
- 23. Lo CW, Paris PW, Holick MF. Indian and Pakistani immigrants have the same capacity as Caucasians to produce vitamin D in response to ultraviolet irradiation. Am J Clin Nutr. 1986;44:683–5. doi: 10.1093/ajcn/44.5.683. [DOI] [PubMed] [Google Scholar]
- 24. Luxwolda MF, Kuipers RS, Kema IP, Dijck-Brouwer DA, Muskiet FA. Traditionally living populations in East Africa have a mean serum 25-hydroxy vitamin D concentration of 115 nmol/l. Br J Nutr. 2012;108:1557–61. doi: 10.1017/S0007114511007161. [DOI] [PubMed] [Google Scholar]
- 25. Luxwolda MF, Kuipers RS, Kema IP, van der Veer E, Dijck-Brouwer DA, Muskiet FA. Vitamin D status indicators in indigenous populations in East Africa. Eur J Nutr. 2013;52:1115–25. doi: 10.1007/s00394-012-0421-6. [DOI] [PubMed] [Google Scholar]
- 26. Dawodu A, Kochiyil J, Altaye N. Pilot study of sunlight exposure and vitamin D status in Arab women of childbearing age. East Mediterr Health J. 2011;17:570–4. [PubMed] [Google Scholar]
- 27. Sambrook PN, Cameron ID, Chen JS, Cumming RG, Durvasula S, Herrmann M, et al. Does increased sunlight exposure work as a strategy to improve vitamin D status in the elderly: A cluster randomised controlled trial. Osteoporos Int. 2012;23:615–24. doi: 10.1007/s00198-011-1590-5. [DOI] [PubMed] [Google Scholar]
- 28. Marwaha RK, Sreenivas V, Talwar D, Yenamandra VK, Challa A, Lakshmy R, et al. Impact of solar ultraviolet B radiation (290-320 nm) on vitamin D synthesis in children with type IV and V skin. Br J Dermatol. 2015;173:604–6. doi: 10.1111/bjd.13887. [DOI] [PubMed] [Google Scholar]
- 29. Patwardhan VG, Mughal ZM, Padidela R, Chiplonkar SA, Khadilkar VV, Khadilkar AV. Randomized control trial assessing impact of increased sunlight exposure versus vitamin D supplementation on lipid profile in Indian vitamin D deficient men. Indian J Endocrinol Metab. 2017;21:393–8. doi: 10.4103/ijem.IJEM_9_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Al Anouti F, Thomas J, Abdel-Wareth L, Rajah J, Grant WB, Haq A. Vitamin D deficiency and sun avoidance among university students at Abu Dhabi, United Arab Emirates. Dermatoendocrinol. 2011;3:235–9. doi: 10.4161/derm.3.4.16881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Marwaha RK, Yenamandra VK, Sreenivas V, Sahay R, Baruah MP, Desai A, et al. Regional and seasonal variations in ultraviolet B irradiation and vitamin D synthesis in India. Osteoporos Int. 2016;27:1611–7. doi: 10.1007/s00198-015-3427-0. [DOI] [PubMed] [Google Scholar]
- 32. Goswami R, Saha S, Sreenivas V, Singh N, Lakshmy R. Vitamin D-binding protein, vitamin D status and serum bioavailable 25(OH)D of young Asian Indian males working in outdoor and indoor environments. J Bone Miner Metab. 2017;35:177–84. doi: 10.1007/s00774-016-0739-x. [DOI] [PubMed] [Google Scholar]
- 33. Azizi E, Pavlotsky F, Vered I, Kudish AI. Occupational exposure to solar UVB and seasonal monitoring of serum levels of 25-hydroxy vitamin D3: A case-control study. Photochem Photobiol. 2009;85:1240–4. doi: 10.1111/j.1751-1097.2009.00569.x. [DOI] [PubMed] [Google Scholar]
- 34. Nurbazlin M, Chee WS, Rokiah P, Tan AT, Chew YY, Nusaibah AR, et al. Effects of sun exposure on 25(OH) vitamin D concentration in urban and rural women in Malaysia. Asia Pac J Clin Nutr. 2013;22:391–9. doi: 10.6133/apjcn.2013.22.3.15. [DOI] [PubMed] [Google Scholar]
- 35. Sowah D, Fan X, Dennett L, Hagtvedt R, Straube S. Vitamin D levels and deficiency with different occupations: A systematic review. BMC Public Health. 2017;17:519. doi: 10.1186/s12889-017-4436-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Heaney RP. Vitamin D and calcium interactions: Functional outcomes. Am J Clin Nutr. 2008;88:541S–4S. doi: 10.1093/ajcn/88.2.541S. [DOI] [PubMed] [Google Scholar]
- 37. Clements MR, Johnson L, Fraser DR. A new mechanism for induced vitamin D deficiency in calcium deprivation. Nature. 1987;325:62–5. doi: 10.1038/325062a0. [DOI] [PubMed] [Google Scholar]
- 38. Harinarayan CV. Letter to the editor on “vitamin D-binding protein, vitamin D status and serum bioavailable 25(OH)D of young Asian Indian males working in outdoor and indoor environments”. J Bone Miner Metab. 2017;35:243–4. doi: 10.1007/s00774-016-0776-5. [DOI] [PubMed] [Google Scholar]
- 39. Wang TJ, Zhang F, Richards JB, Kestenbaum B, van Meurs JB, Berry D, et al. Common genetic determinants of vitamin D insufficiency: A genome-wide association study. Lancet. 2010;376:180–8. doi: 10.1016/S0140-6736(10)60588-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Granado Lorencio F, Blanco-Navarro I, Pérez-Sacrsitán B. Critical evaluation of assays for vitamin D status. Curr Opin Clin Nutr Metab Care. 2013;16:734–40. doi: 10.1097/MCO.0b013e328364ca96. [DOI] [PubMed] [Google Scholar]
- 41. Spiro A, Buttriss JL. Vitamin D: An overview of vitamin D status and intake in Europe. Nutr Bull. 2014;39:322–50. doi: 10.1111/nbu.12108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Trilok Kumar G, Chugh R, Eggersdorfer M. Poor vitamin D status in healthy Populations in India: A review of current evidence. Int J Vitam Nutr Res. 2015;85:185–201. doi: 10.1024/0300-9831/a000228. [DOI] [PubMed] [Google Scholar]
- 43. Jukic AMZ, Hoofnagle AN, Lutsey PL. Measurement of vitamin D for epidemiologic and clinical research: Shining light on a complex decision. Am J Epidemiol. 2018;187:879–90. doi: 10.1093/aje/kwx297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Nair MK, Augustine LF, Konapur A. Food-based interventions to modify diet quality and diversity to address multiple micronutrient deficiency. Front Public Health. 2015;3:277. doi: 10.3389/fpubh.2015.00277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wacker M, Holick MF. Sunlight and vitamin D: A global perspective for health. Dermatoendocrinol. 2013;5:51–108. doi: 10.4161/derm.24494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tsiaras WG, Weinstock MA. Factors influencing vitamin D status. Acta Derm Venereol. 2011;91:115–24. doi: 10.2340/00015555-0980. [DOI] [PubMed] [Google Scholar]
- 47. Vieth R. Vitamin D supplementation, 25-hydroxy vitamin D concentrations, and safety. Am J Clin Nutr. 1999;69:842–56. doi: 10.1093/ajcn/69.5.842. [DOI] [PubMed] [Google Scholar]
- 48. Koul PA, Ahmad SH, Ahmad F, Jan RA, Shah SU, Khan UH. Vitamin D toxicity in adults: A case series from an area with endemic hypovitaminosis D. Oman Med J. 2011;26:201–4. doi: 10.5001/omj.2011.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mansuri ZH, Kaji BC, Dumra S, Buch HN. Hypervitaminosis-D, an uncommon reality! J Assoc Physicians India. 2014;62:58–60. [PubMed] [Google Scholar]
- 50. Lehmann U, Hirche F, Stangl GI, Hinz K, Westphal S, Dierkes J. Bioavailability of vitamin D(2) and D(3) in healthy volunteers, a randomized placebo-controlled trial. J Clin Endocrinol Metab. 2013;98:4339–45. doi: 10.1210/jc.2012-4287. [DOI] [PubMed] [Google Scholar]
- 51. Borel P, Caillaud D, Cano NJ. Vitamin D bioavailability: State of the art. Crit Rev Food Sci Nutr. 2015;55:1193–205. doi: 10.1080/10408398.2012.688897. [DOI] [PubMed] [Google Scholar]
- 52. Patel SA, Narayan KM, Cunningham SA. Unhealthy weight among children and adults in India: Urbanicity and the crossover in underweight and overweight. Ann Epidemiol. 2015;25:336–4100. doi: 10.1016/j.annepidem.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 53. Kruger MC, Kruger IM, Wentzel-Viljoen E, Kruger A. Urbanization of Black South African women may increase risk of low bone mass due to low vitamin D status, low calcium intake, and high bone turnover. Nutr Res. 2011;31:748–58. doi: 10.1016/j.nutres.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 54. Poh BK, Rojroongwasinkul N, Nguyen BK, Sandjaja , Ruzita AT, Yamborisut U, et al. 25-hydroxy-vitamin D demography and the risk of vitamin D insufficiency in the South East Asian Nutrition Surveys (SEANUTS) Asia Pac J Clin Nutr. 2016;25:538–48. doi: 10.6133/apjcn.092015.02. [DOI] [PubMed] [Google Scholar]
- 55. Wakayo T, Belachew T, Vatanparast H, Whiting SJ. Vitamin D deficiency and its predictors in a country with thirteen months of sunshine: The case of school children in central Ethiopia. PLoS One. 2015;10:E0120963. doi: 10.1371/journal.pone.0120963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Chailurkit LO, Aekplakorn W, Ongphiphadhanakul B. Regional variation and determinants of vitamin D status in sunshine-abundant Thailand. BMC Public Health. 2011;11:853. doi: 10.1186/1471-2458-11-853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Harinarayan CV, Ramalakshmi T, Prasad UV, Sudhakar D, Srinivasarao PV, Sarma KV, et al. High prevalence of low dietary calcium, high phytate consumption, and vitamin D deficiency in healthy South Indians. Am J Clin Nutr. 2007;85:1062–7. doi: 10.1093/ajcn/85.4.1062. [DOI] [PubMed] [Google Scholar]
- 58.World Health Organization. Air quality guidelines: Global update: Particulate matter, ozone, nitrogen dioxide, and sulfur dioxide. Geneva: WHO; 2006. [PubMed] [Google Scholar]
- 59.World Health Organization. Ambient air pollution. Geneva: WHO; 2018. [Google Scholar]
- 60. Hosseinpanah F, Pour SH, Heibatollahi M, Moghbel N, Asefzade S, Azizi F. The effects of air pollution on vitamin D status in healthy women: A cross sectional study. BMC Public Health. 2010;10:519. doi: 10.1186/1471-2458-10-519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Manicourt DH, Devogelaer JP. Urban tropospheric ozone increases the prevalence of vitamin D deficiency among Belgian postmenopausal women with outdoor activities during summer. J Clin Endocrinol Metab. 2008;93:3893–9. doi: 10.1210/jc.2007-2663. [DOI] [PubMed] [Google Scholar]
- 62. Cevei M, Stoicănescu D. Air pollution and genetic influences on bone mineral density and osteoporosis. Analele Univ Oradea Fascicula Biol. 2010;62:84–9. [Google Scholar]
- 63.World Health Organization. Global solar UV index: a practical guide. Geneva, Switzerland: WHO; 2002. [Google Scholar]
- 64.UV station data based on operational TEMIS satellite ozone data: European Space Agency. 2021. [accessed on September 28, 2021]. Available from: https://www.temis.nl/uvradiation/UVarchive/stations_uv.php .
- 65. Jablonski NG. The evolution of human skin and skin color. Annu Rev Anthropol. 2004;33:585–623. [Google Scholar]
- 66. Del Bino S, Bernerd F. Variations in skin colour and the biological consequences of ultraviolet radiation exposure. Br J Dermatol. 2013;169(Suppl 3):33–40. doi: 10.1111/bjd.12529. [DOI] [PubMed] [Google Scholar]
- 67. Roberts JE. Ultraviolet radiation as a risk factor for cataract and macular degeneration. Eye Contact Lens. 2011;37:246–9. doi: 10.1097/ICL.0b013e31821cbcc9. [DOI] [PubMed] [Google Scholar]
- 68. Jerant AF, Johnson JT, Sheridan CD, Caffrey TJ. Early detection and treatment of skin cancer. Am Fam Physician. 2000;62:357–68. 375-6, 381-2. [PubMed] [Google Scholar]
- 69.National Institute for Health Care Excellence. Sunlight exposure: Communicating the benefits and risks to the general public National Institute for Health Care Excellence. United Kingdom: NIHCE; 2011. [Google Scholar]
- 70. Harris TC, Vuilleumier L, Backes C, Nenes A, Vernez D. Satellite-based personal UV dose estimation. Atmosphere. 2021;12:268. [Google Scholar]
- 71. Vuilleumier L, Harris T, Nenes A, Backes C, Vernez D. Developing a UV climatology for public health purposes using satellite data. Environ Int. 2021;146:106177. doi: 10.1016/j.envint.2020.106177. [DOI] [PubMed] [Google Scholar]
- 72. Wai KM, Yu PK, Lam KS. Reduction of solar UV radiation due to Urban high-rise buildings – A coupled modelling study. PLoS One. 2015;10:E0135562. doi: 10.1371/journal.pone.0135562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Duarte I, Rotter A, Malvestiti A, Silva M. The role of glass as a barrier against the transmission of ultraviolet radiation: An experimental study. Photodermatol Photoimmunol Photomed. 2009;25:181–4. doi: 10.1111/j.1600-0781.2009.00434.x. [DOI] [PubMed] [Google Scholar]
- 74. Tester JM. The built environment: designing communities to promote physical activity in children. Pediatrics. 2009;123:1591–98. doi: 10.1542/peds.2009-0750. [DOI] [PubMed] [Google Scholar]
- 75. Lorentzen HF, Weismann K. The shadow rule and appropriate sun behavior. Ugeskr Laeger. 2002;164:3346–50. [PubMed] [Google Scholar]
- 76. Downham TF., 2nd The shadow rule: A simple method for sun protection. South Med J. 1998;91:619–23. [PubMed] [Google Scholar]
- 77. Turnbull DJ, Parisi A. Utilising shade to optimize UV exposure for vitamin D. Atmos Chem Phys. 2008;8:2841–6. [Google Scholar]
- 78. Turnbull DJ, Parisi AV. Latitudinal variations over Australia of the solar UV-radiation exposures for vitamin D3 in shade compared to full sun. Radiat Res. 2010;173:373–9. doi: 10.1667/RR1951.1. [DOI] [PubMed] [Google Scholar]
- 79. Harinarayan CV, Ramalakshmi T, Prasad UV, Sudhakar D. Vitamin D status in Andhra Pradesh: A population based study. Indian J Med Res. 2008;127:211–8. [PubMed] [Google Scholar]
- 80. Harinarayan CV, Holick MF, Prasad UV, Vani PS, Himabindu G. Vitamin D status and sun exposure in India. Dermatoendocrinol. 2013;5:130–41. doi: 10.4161/derm.23873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Setiati S. Vitamin D status among Indonesian elderly women living in institutionalized care units. Acta Med Indones. 2008;40:78–83. [PubMed] [Google Scholar]


