Abstract
Gastrostomy tube placement is a procedure that achieves enteral access for nutrition, decompression, and medication administration. Preprocedural evaluation and selection of patients is necessary to provide optimal benefit and reduce the risk of adverse events (AEs). Appropriate indications, contraindications, ethical considerations, and comorbidities of patients referred for gastrostomy placement should be weighed and balanced. Additionally, endoscopist should consider either a transoral or transabdominal approach is appropriate, and radiologic or surgical gastrostomy tube placement is needed. However, medical history, physical examination, and imaging prior to the procedure should be considered to tailor the appropriate approach and reduce the risk of AEs.
Keywords: Gastrostomy, Gastropexy, Enterostomy, Decompression, Enteral nutrition, Endoscopy
Core Tip: We reviewed 179 articles and compiled suggested considerations, especially for endoscopists, in the preprocedural evaluation of gastrostomy candidates. Patients referred to for gastrostomy tube placement should be evaluated for indications, contraindications, ethical considerations, and comorbidities. Additionally, the proceduralist should consider whether radiologic or surgical tube placement may be more appropriate, and whether a transoral or transabdominal approach is appropriate. Prior to the procedure, physical examination, imaging, and other interventions should be performed to reduce adverse events.
INTRODUCTION
Percutaneous gastrostomy is a method of inserting a tube transabdominally into the stomach to provide nutrition, decompress, and/or administer medication. The first of these is the most common indication for gastrostomy tube placement and is critical to preserve nutritional status and improve prognosis for a wide spectrum of conditions and illnesses[1]. Minimally invasive methods of gastrostomy placement have been developed and include, but are not limited to, percutaneous endoscopic gastrostomy (PEG). Since this is an invasive procedure associated with a number of potential adverse events (AEs), appropriate patients and technique selection is essential.
Over the past decade, all-cause mortality from PEG placement has decreased approximately 40% despite AE rates, time to placement, indications, and comorbidities of patients having generally remained the same[2]. This could be attributable to better patient selection and optimization of placement technique. However, there is still a considerable patient cohort that is exposed to PEG and/or other gastrostomy tube placement without adequate preprocedural planning[3].
In this review, we discuss gastrostomy tube indications, contraindications, optimal gastrostomy technique, informed consent, physical exam tenets, and imaging considerations as well as management of anticoagulation and antibiotic prophylaxis. We also provide practical pearls to decrease the risk of various AEs and equip the proceduralist with a comprehensive preprocedural approach, as summarized in Table 1.
Table 1.
Periprocedural pearls for gastrostomy tube placement
| Recognize indications, relative contraindications, and absolute contraindications for gastrostomy tube placement |
| Ensure appropriate informed consent and discussion of the benefits of gastrostomy tubes |
| Ensure correct selection of gastrostomy technique: |
| Transoral techniques should be first line except in select indications where transabdominal techniques maybe more appropriate |
| Placement by radiology is appropriate when the endoscopist is not trained in the transoral or transabdominal technique necessary or lacks availability of materials |
| Laparoscopic tube placement should be utilized when endoscopic or radiographic gastrostomy fails or is contraindicated |
| Perform certain periprocedural interventions to reduce adverse events: |
| Physical exam for oropharyngeal and abdominal wall abnormalities, ascites, and obesity |
| Hold anticoagulation and antiplatelet therapy appropriately and correct coagulopathy to avoid bleeding |
| Administer antibiotic prophylaxis targeting skin flora thirty minutes prior to procedure to prevent infection |
| Drain ascites beforehand and avoid gastrostomy tube placement if fluid reaccumulation is expected to occur within 7-10 d |
| Obtain cross-sectional imaging (e.g., computed tomography) if colonic interposition and other suspected anatomical abnormalities are suspected |
| Use reverse Trendelenburg patient positioning, proper transillumination and palpation of anterior gastric wall, and use of safe track maneuver during initial needle puncture to prevent inadvertent liver or colonic puncture |
| Minimize external bumper traction and ensure tube is rotatable to prevent buried bumper syndrome and ulceration |
| Consider abdominal binders to restrict access, gastropexy devices, and low-profile gastrostomy button with detachable tubing to prevent patient tube dislodgement |
GASTROSTOMY TUBE INDICATIONS
Regardless of clinical context, gastrostomy tube placement is mostly indicated to provide nutrition and bypass obstruction. In certain conditions such as gastric volvulus, gastrostomy tube can be utilized for gastropexy procedure, though these are beyond the scope of the discussion.
It is appropriate to place the gastrostomy tube in patients with underlying conditions that require more than four weeks of artificial enteral nutrition. Such conditions include Guillain-Barre syndrome, acute stroke, intracranial trauma, anorexia nervosa, hyperemesis gravidarum, severe burns, facial trauma, esophageal disease, malnutrition especially in patients prior to transplantation, and head and neck tumors undergoing treatment[4]. Moreover, it may also be appropriate to place gastrostomy tubes permanently in certain conditions with poor prognosis to improve quality of life. Such conditions include neurological diseases like multiple sclerosis and amyotrophic lateral sclerosis, advanced head and neck tumors, oropharyngeal malformations, advanced esophageal or gastric malignancy, rheumatologic disorders associated with esophageal dysfunction such as scleroderma, cystic fibrosis, and amyloidosis[5] (Table 2).
Table 2.
Select Indications for gastrostomy placement
| Palliative venting for malignant obstruction and peritoneal carcinomatosis[20,46,120-124] | Can reduce symptoms of nausea and vomiting without a cumbersome NG tube |
| Head and neck malignancy[20,125-130] | Reactive rather than prophylactic gastrostomy can reduce treatment related critical weight loss |
| Esophageal malignancy[131-136] | Achieves adequate nutritional status better than self-expandable metal stent insertion |
| Ventilator-dependent respiratory failure including COVID-19[137-144] | Early enteral nutrition can decrease complication rates and length of stay due to a catabolic state in prolonged ventilation |
| Stroke with dysphagia[145-147] | Can be placed after 28 d if prolonged enteral nutrition is needed |
| Non-stroke neurologic disease[148-155] | Supported in amyotrophic lateral sclerosis. No guideline specific recommendations in Parkinson’s disease, multiple sclerosis complicated by dysphagia, cerebral palsy, or trauma patients with severe cerebral injury but has been effective |
| Pregnancy complicated by severe hyperemesis gravidarum[156-159] | Successfully performed in up to a 29 wk gestation with favorable maternal and fetal outcomes |
| Gastric bypass | Can be performed in concurrence with surgery to avoid reoperation in patients who are at higher risk for an anastomotic leak or gastro-enteric obstruction[20,160,161] |
CONTRAINDICATIONS
Relative contraindications include recent gastrointestinal (GI) bleeding, hemodynamic instability, ascites, respiratory failure, peritoneal carcinomatosis, and anatomical alterations[2]. Absolute contraindications include mechanical obstruction of the GI tract unless procedure is indicated for decompression, active peritonitis, uncorrectable coagulopathy, and bowel ischemia[5] (Table 3).
Table 3.
Select relative contraindications to gastrostomy placement
|
|
Comments
|
| Certain alterations in abdominal anatomy and motility[2,5] | Open abdomen, ostomy sites, drain tubes, and surgical scars can alter or preclude location for gastrostomy tube placement |
| Altered oropharyngeal anatomy[2] | Vocal cord paralysis, active radiation, head/neck tumors, facial and skull fractures, and high cervical fractures can obstruct the gastrostomy tube and create an airway emergency |
| Massive refractory ascites[2,162,163] | Increased risk for bacterial peritonitis, impairment of stoma tract maturation, and tube dislodgement if ascites rapidly reaccumulates over 7-10 d despite paracentesis or PleurX catheter placement; gastropexy devices can increase success |
| Upper GI bleeding from ulcer or varices[2] | Bleeding peptic ulcers and esophageal varices can have high rates of recurrent bleeding; bleeding from stress gastropathy, gastritis, or angiodysplasia are less likely to recur, and do not need a delay in enteral access |
| Obesity[2] | Shifting of panniculus increases the risk of tube dislodgement from the stomach into the peritoneal space |
| Early feeding in stroke with dysphagia[20,29,164-166] | Enteral tubes prior to 28 d rather than temporary NG tubes had greater development of pressure ulcers, sepsis, pneumonia, and GI bleeding over 2 yr |
| Nutrition in terminal metastatic malignancy[2,167,168] | Administration of nutrition beyond specific patient request plays a minimal role in comfort and does not improve complication rate, survival, or functionality in terminal malignancy |
| VP shunts[20,46,169,170] | May increase risk of ascending meningitis |
| Irreversible dementias[171-179] | Does not improve mortality or rehospitalization rate |
METHODS OF MINIMALLY INVASIVE GASTROSTOMY TUBE PLACEMENT
Percutaneous gastrostomy has supplanted open gastrostomy and can be performed with tube introduction transorally or transabdominally, using endoscopic (Figure 1), imaging (Figure 2), or laparoscopic guidance (Figure 3)[2].
Figure 1.
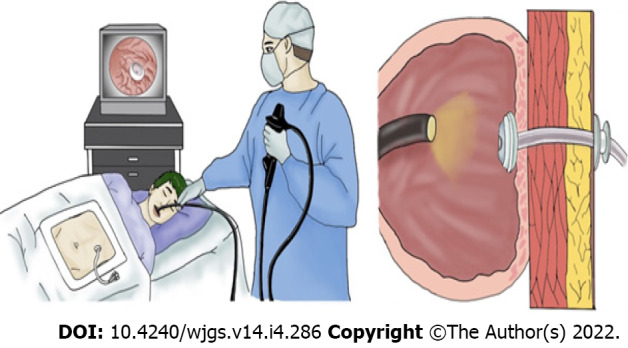
Endoscopic gastrostomy tube placement.
Figure 2.
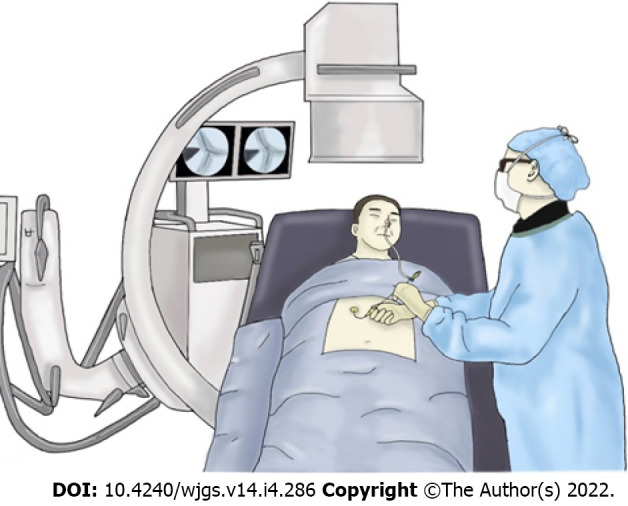
Radiologic gastrostomy tube placement.
Figure 3.
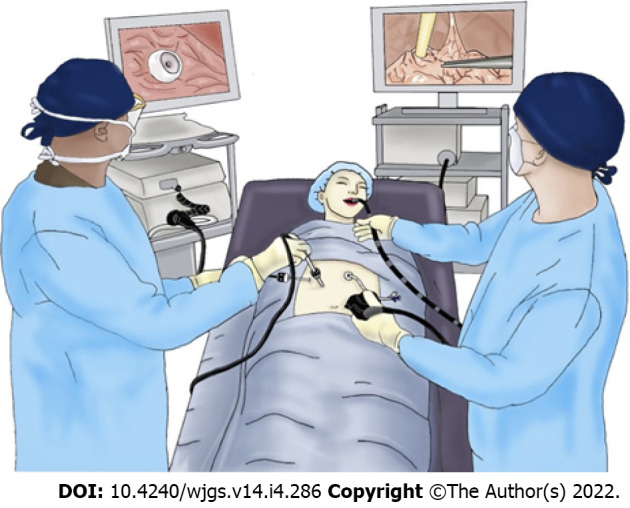
Laparoscopic-assisted endoscopic gastrostomy tube placement.
Endoscopic placement: Brief overview of technique
With endoscopic guidance for PEG, the “pull” (Ponsky-Gauderer) technique[6,7], “push-over-wire” (Sacks-Vine) technique[8,9], and “introducer” (Russell)[10,11] technique can be used depending on training or operator preference. The introducer method is the only true transabdominal method that can be used to avoid transoral passage of the PEG tube. For patients with near-obstructing head and neck malignancy, the “SLiC” technique can be performed with a small-bore endoscopy if fluoroscopy cannot be used[12].
Transoral approach is usually performed in both push-over-wire and pull techniques. Upper endoscopy is performed to insufflate and transilluminate the stomach. A site for placement is chosen via endoscopic visualization combined with manual palpation of the stomach. After local anesthesia is given through the chosen site and a small cutaneous incision is performed to the fascia. A catheter over needle is passed percutaneously into the stomach. A snare is passed through the endoscope.
Subsequently with the pull method, the needle is removed and a silk suture loop (“string”) is passed through the remaining catheter into the stomach. The snare that passed through the endoscope grasps the string. The string is pulled out via endoscope through the mouth. The wire loop of the string is then tied to the wire loop of the PEG tube. The tube is then “pulled” via string back through the mouth to the stomach, and then out the abdominal wall. The endoscope is then reinserted to confirm placement.
With the push-over-wire technique, a guidewire instead is placed into the stomach after needle removal. Similarly, the endoscope pulls the wire through the mouth via snare. The PEG tube is placed over guidewire exiting the mouth and pushed out through the stomach and abdominal wall. To accomplish this, a long plastic tapered dilator is fused to the tip of the PEG tube to facilitate passage[13].
Unlike the push-over-wire and pull methods, the introducer method avoids PEG tube contact with the oropharyngeal cavity[13,14]. This technique is more employed in fluoroscopic placement by radiology, though can be performed by the endoscopist as well. The initial steps are similar wherein a trocar is placed into the stomach with endoscopic visualization, and guidewire is passed into the stomach. The wire is held by endoscopic snare to secure it. Two to four T-fasteners are then deployed into the stomach via cannula around the trocar for gastropexy. The tract through which the guidewire passes is then dilated serially, and a peel-away sheath is passed over the wire[13]. There are other variations in which other gastropexy methods are used such as a double-lumen gastropexy device[11]. The PEG tube is passed through the sheath over wire and sheath removed, with balloon tip inflation to secure the tube in the stomach[13].
The SLiC technique is similar to the introducer technique but avoids the need for T-fasteners which are not widely available[12]. After a blunt 7-8 mm AutoSuture Mini Step Trocar is placed into the stomach with endoscopic visualization, the blunt needle within is withdrawn leaving the radially expandable sleeve in place. A tapered blunt dilater with cannula is inserted to expand the trocar sleeve radially. The dilator is then removed from the cannula, leaving a self-anchoring 7-8 mm working port through the cannula. A metal stylet is passed through a 20 french Malecot catheter (the PEG tube) and together they are inserted into the port. The port surrounding the PEG tube is then removed while the tube is held in place with endoscopic verification.
Radiologic placement: Brief overview
With fluoroscopy, computed tomography (CT), or ultrasound guidance, percutaneous radiological gastrostomy (PRG) can be performed transabdominally with push type A technique (Seldinger) and push type B technique (Peel-away sheath). If desired, PRG can achieve gastropexy similar to the introducer technique with T-fasteners or other devices[15-17]. Similar to the PEG “push-over-wire” technique, hybrid per-oral image guided gastrostomy technique (PIG) has also been used for transoral placement[18,19]. Alternatively, percutaneous transesophageal gastrotubing (PTEG) with image guidance can be used to place esophagostomy when gastrostomy is contraindicated such as massive refractory ascites, hostile abdomen, or massive peritoneal carcinomatosis[20-25].
Laparoscopic placement: Brief overview
Gastrostomy tube placement can be performed with laparoscopic guidance. Percutaneous laparoscopic assisted gastrostomy (PLAG) requires two midline trocars to perform gastropexy with sutures and place the tube[20,26-29]. A novel hybrid laparoscopic-assisted PEG (LAPEG) is a combination of endoscopy with laparoscopic visualization[30-34], as shown in Figure 3.
Comparison of endoscopic gastrostomy methods
Although the use of each technique depends on institution and clinical scenario, transoral PEG placement is often first-line, though variation exists across institutions. The pull technique may have lower rates of AEs in non-oropharyngeal cancer patients, especially for palliative decompression[35]. Additionally, a larger and more robust tube can be placed with transoral technique. The smaller diameter of available introducer trocars limits transabdominal technique. This may lead to higher rate of tube blockage and occlusions[36,37]. Transoral technique also allows placement of mushroom type catheters without need for gastropexy. Lastly, transoral technique can present a lower minor bleeding rate (0.6% vs 6.6%) likely due to the additional needle punctures needed for gastropexy and use of a larger trocar[38].
Though technically more complicated for the endoscopist, the introducer technique could provide a stronger gastropexy with T-fasteners and avoid tube dislodgement[39], especially in patients with neurologic impairment[40,41]. Furthermore, this method is associated with a lower rate of mild peristomal wound infection[42]. The introducer method is more effective than the transoral method in patients with oropharynx or esophageal stricture from radiation, inflammation, or malignancy. Recent studies showed that the introducer technique is widely used in patients with advanced head and neck malignancy due to lower rates of AEs and PEG site metastases related to possible contact with malignant cells with the pull technique[43-47]. However, some institutions continue to use the transoral technique given the low incidence of abdominal wall metastases and the need for large randomized controlled trials comparing the procedural vs metastatic risk[48].
Overall, the pull technique has a higher rate of infection but a lower rate of bleeding compared to the introducer technique[38]. Therefore, the type of technique for gastrostomy tube placement should be chosen based on patient characteristics and operator’s skill. The introducer technique should be considered in patients with head and neck malignancy. However, further studies are warranted.
The Russell introducer technique is inferior to the SLiC technique described in the prior section, and may also be technically harder for the endoscopist. First, the size of the PEG tube is limited by the extent of dilation that can be achieved and using larger dilators without T-fasteners increases the likelihood of the stomach being pushed away from the abdominal wall. Second, T-fasteners may not be readily available at all institutions. The Mini Step Trocar used in the SLiC technique dilates axially in one step without the need of T-fasteners[12]. Third, the balloon catheter used in the introducer technique has a greater chance of rupture and dislodgement than mushroom catheters including the Malecot catheter used in the SLiC technique[49]. Thus, in selected patients in whom the conventional push-over-wire or pull techniques cannot be performed, the SLiC technique should be considered over the introducer technique where larger PEG tube are preferred and T-fasteners are not available. Other modified introducer methods involving direct placement of bumper-button-type catheters have been described[50,51] and can also be considered over the Russell technique if preferred.
Comparison of endoscopic, radiologic, and laparoscopic gastrostomy tube placement methods
There is a large confusion of nomenclature in the surgical, radiological, and gastroenterological literatures. For endoscopic placement, the pull and push-over-wire methods are performed transorally. There are no differences in the success and AE rate between both methods. Thus, either method can be used depending on operator’s experience, though the pull method is more widely employed[13,52,53]. Several studies comparing the “pull” vs “push” method are referring to a comparison between the transoral and transabdominal introducer methods or other “push” trocar methods. Multidisciplinary guidelines describe transoral gastrostomy as the pull PEG technique and transabdominal gastrostomy as type A or B push PRG techniques[2].
If the less common PIG technique is readily available, the choice of transoral PEG vs PIG technique depends on institutional preference and operator capability due to similar AE rates[18,19]. PRG vs transoral PEG placement parallels the choice of transoral vs transabdominal PEG technique in the previous section. Only a large meta-analysis study reported a higher success rate but lower morbidity rate in PRG technique[54], but other previous studies showed lower rates of AEs, mortality, and readmission in PEG technique especially in those with head and neck malignancy[20,55,56]. In contrast, several studies demonstrated a similar AE rate between PRG and PEG technique[42,57-61]. However, the AE profile of each study may be different. Despite lower rates of bleeding and pain, PEG pull technique could cause more superficial wound infection and buried bumpers than PRG technique[60]. PRG may be considered if transabdominal PEG cannot be performed due to lack of endoscopic training or resources.
Endoscopic feeding tube placement has the advantage of placement at bedside as opposed to the radiology suite for PIG/PRG or operating room for PLAG[13]. This may be particularly useful in critically-ill patients. Transabdominal PEG should be favored over transoral PEG in patients with obstruction or stricture due to oropharyngeal mass and those with head and neck malignancy who are at risk of tumor seeding from the PEG site. However, if the endoscopist lacks experience or resources are unavailable, the gastrostomy tube placement by interventional radiology is more appropriate.
PLAG is a safe and preferred method of placement if PEG or PRG cannot be performed due to unsuccessful endoscopic trans-illumination and finger palpation, inadequate imaging window, or inability to insufflate the stomach[28,62]. It does not preclude PEG placement, as it can be used when PEG is contraindicated to ensure that there is no obstruction or blood vessels at the site of tube placement. Such conditions include morbid obesity, need for lysis of adhesions, organ interposition, gastric varices, large hiatal hernia, ileus, intraabdominal mass, gravid uterus, ascites, use of peritoneal dialysis, or altered anatomy due to gastric bypass[30,63]. Though PEG technique has been utilized in altered Roux-en-Y anatomy with double balloon enteroscopy, it requires fluoroscopy and is not widely used[20]. In pediatric patients, PLAG is more preferred in to avoid serious AEs such as intestinal fistula formation[64-66]. Laparoscopic placement should also be considered when jejunostomy is needed for more durable long-term enteral access compared to jejunal extension tubing[67].
LAPEG is a hybrid approach for gastrostomy tube placement as it allows direct visualization of all cavities. If available, it can be considered over PLAG due to the advantage of luminal visualization. It also allows transoral tube placement, conferring the advantages described in prior sections over transabdominal method. However, this technique requires physicians with advanced expertise in laparoscopy with PLAG, increased peritoneal insufflation, and placement of multiple ports[30-34].
APPROPRIATE INFORMED CONSENT AND MANAGING EXPECTATIONS
Gastrostomy tube placement should involve the informed and educated consent of the patient in order to respect patient autonomy over perceived beneficence. Informed consent for gastrostomy tube placement is often inadequate[42,68,69]. Legal precedence over the past thirty years has determined that artificial nutrition should not be thought of as different from any other medical therapy, and that there is no obligation to provide it if it is unwanted[2,70]. If the patient cannot provide consent, the consent of the health care proxy from an advanced directive should be obtained. The living will should be followed if the patient is considered terminally ill[2,70].
Appropriate expectations must be set about what benefit the gastrostomy tube can provide for the patient. Clinical indications can start the decision-making process but are rarely adequate alone[20]. Social support should also be evaluated, as it plays a significant role at reducing gastrostomy tube dependence[71]. In conditions such as anorexia from advanced malignancy, it has been suggested that gastrostomy tube not even be offered due to an inability to utilize nutrients from feeding[72]. In conditions such as a permanent vegetative state, gastrostomy tube can be offered but should be recommended against due to inability of the patient to experience any quality of life. In contrast, if the patient has uncomplicated dysphagia with preserved quality of life otherwise, gastrostomy tube should be offered and recommended due to unequivocal nutritional benefit[73]. Furthermore, in malignant gastrointestinal obstruction, gastrostomy tube venting provides clear symptomatic benefit.
Decision-making is most difficult in equivocal indications such as recurrent strokes, and can lead to decision regret among surrogate decisionmakers[74]. Gastrostomy tubes that are frequently placed into elderly or neurological impaired patients have a significant financial burden on the healthcare system associated with dislodgement[75]. Gastrostomy insertion in such patients provides a greater health-related quality of life improvement for caregivers than patients[20,76], purportedly due to greater ease of medication administration and greater sense of accomplishment by the caregiver[70]. The intervention can provide physiologic benefit in prolonged life but may not actually improve quality of life. Given that data on long term functional outcomes are often lacking, decision-makers focus on short-term procedural safety and potential for improved nutrition[77]. A limited feeding trial can be discussed, but strict criteria on what constitutes a successful response to feeding should be defined in discussion with the patient or health care proxy[20].
PRE-PROCEDURAL PHYSICAL EXAM AND IMAGING CONSIDERATIONS
Physical examination may help identify certain contraindications to gastrostomy tube placement and prevent occurrence of AEs. The oropharynx and head should be inspected for features that preclude endoscopic approach such as facial fractures or complete obstruction. An anesthesia or sedation team should additionally look for features that may impact sedation such as stridor, large neck circumference, or presence of obstructive sleep apnea to reduce procedure-related cardiopulmonary AEs[78].
The abdomen should be examined for ascites and obesity, which can increase the risk of tube dislodgement, failed transillumination, or failed gastropexy. To avoid puncture of liver, the caudal and lower edge of the liver should be identified with percussion before gastrostomy placement[78]. Any devices such as VP shunts should be noted as well so that the endoscopist can be aware of any infection risk. The patient’s mental status should be examined to determine ability to consent.
Abdominal imaging with CT or radiography can be obtained prior to the procedure if abnormal anatomy is suspected or known due to prior surgery. Certain patients requiring gastrostomy tubes may have structural deformities of the spine, previous abdominal surgery, or chronic constipation, which predispose transposition of the transverse colon in front of the anterior gastric wall. Preprocedural abdominal radiographs can be obtained and subsequent enema administration can be performed to decompress the colon if interposed on imaging[79,80]. Furthermore, use of abdominal x-ray after insufflation of 500 cc of air may help identify an optimal gastric puncture point[81]. Concordance between pre-procedural CT scan and abdominal radiography was reported to be approximately 73%[82]. CT scan increased the success rate of gastrostomy tube placement from 77% to 98% due to high sensitivity of adequate window identification[82].
ANTIBIOTIC PROPHYLAXIS
Patients undergoing PEG tube placement are more prone to infection due to poor nutrition, advanced age, immunocompromise, age, and comorbidities (diabetes, obesity, malnutrition). Infection may occur more frequently with transoral technique due to exposure to oral flora and is one of the most common AEs of external bolster traction[48,71-80]. Major peristomal infection is rare, seen in less than 1.6% of cases. The incidence of minor infection ranges from 5.4%-30%[20,83,84].
Pre-procedural antibiotic prophylaxis is recommended to reduce infectious AEs. Pooled analysis of thirteen randomized control trials evaluating use of prophylactic antibiotics during PEG tube placement showed a significant reduction in incidence of peristomal infection[85]. The introducer technique can be used to avoid oral flora contamination with the pull method to confer lower infection risk[64,86] especially in head and neck cancer patients with overgrowth of oral flora related to tumor[44]. However, there are some reports of increased intraperitoneal abscess and leakage with the introducer method[87]. Prophylactic antibiotics may still be needed regardless of technique[88].
The choice of antibiotic does not necessarily seem to matter if appropriate cutaneous flora is covered. According to the ASGE guideline, antibiotic prophylaxis with IV cefazolin 1 g or equivalent antibiotic thirty minutes before gastrostomy tube placement is recommended to cover cutaneous organisms if patient has not already received appropriate antibiotics[89]. One clinical trial found that administering a single dose of oral Bactrim through PEG tube after insertion is not inferior to a single dose of intravenous 1.5 g cefuroxime before insertion[90]. Another study showed that three doses of IV cefuroxime prior to the procedure with post-procedural betadine spray modestly decreased the rate of stomal infection during the first week[20]. In contrast, a clinical trial found no significant differences between 2 g of cefotaxime and 0.5-4 g of piperacillin-tazobactam prior to the procedure as normal skin flora was mostly considered as a cause of topical wound infection[84].
MANAGEMENT OF ANTIPLATELET AND ANTICOAGULANT AGENTS AND COAGULOPATHY
Gastrostomy placement is a high-risk procedure according to consensus GI society guidelines and moderate risk procedure according to SIR guidelines in patients receiving anticoagulant or antiplatelet therapy[20,83,91-94]. The risk of bleeding should be weighed against thromboembolic event risk after stopping medication. Additionally, resumption of medication is dependent on achieving proper hemostasis[2].
Patients on antiplatelet agents do not necessarily need to have low-dose aspirin withheld. Thienopyridines such as clopidogrel, prasugrel, ticagrelor, and ticlopidine should be withheld 5-7 d before gastrostomy placement. They can be resumed one day after the procedure with the exception of the non-loading dose of clopidogrel, which can be resumed as early as six hours after. Aspirin should additionally be started in the interim if the patient is not already taking it when temporarily discontinuing these antiplatelet agents. There have been certain studies that have had findings in opposition to these consensus statements. Even with use of uninterrupted antithrombotic therapy with clopidogrel and aspirin, risk of significant bleeding was found to be minimal or nonsignificant as compared to holding therapy[95-97]. A risk/benefit discussion should be held with patients who have a higher risk of thromboembolism such as those with coronary artery disease and drug eluting stent placement within the past twelve months or bare stent placement within the past month. A loading dose of thienopyridine can be considered on recontinuation in these patients as well[2,20,83,91-94].
For patients on anticoagulation, patients with higher risk of thromboembolism are those with thrombophilia conditions, deep venous thrombosis within past three months, atrial fibrillation with mitral valve stenosis or prosthetic valve, and metal mitral valve. Warfarin should be discontinued five days before gastrostomy placement. In high risk patients, low molecular weight heparin (LMWH) can be substituted to bridge the patient, with a dose withheld on the morning of the procedure. In low risk patients, INR should be checked to ensure it is less than 1.8 pre-procedure. Warfarin can then be resumed the evening of the procedure. DOACs such as apixaban should be discontinued in high risk patients for the appropriate drug-specific interval[20] and be resumed one to three days after. For heparin products prior to procedure, unfractionated heparin should be withheld six hours before, prophylactic LMWH should be held one dose before, and therapeutic LMWH should be held two doses before[2,20,83,91-94]. Use of uninterrupted heparin products were shown to be independent predictors of bleeding[96,97].
Prior to procedure, platelets, INR, aPTT should the checked. INR should be corrected to a range of 1.5-1.8 and platelets should be corrected to at least 50 x 109/L. There is no consensus on correcting aPTT, though there is a trend towards correcting for values 1.5 x above normal limits. In chronic liver disease patients, fibrinogen levels should be checked as well. INR should be corrected to below 2.5, platelets should be corrected to above 30x10^9/L, and fibrinogen should be corrected to above 100 mg/dL[92,93].
AES AND APPROACH TO PREVENTION AND MANAGEMENT
Gastrostomy tubes are associated with various potential AEs. There are various measures which can be taken to mitigate these, as discussed hereinafter.
Aspiration
Aspiration related to the gastrostomy tube procedure occurs in about 0.3%-1% of cases, and was associated with supine position, deeper sedation, advanced age, and neurologic impairment[20,46,98]. The endoscopist should avoid excessive sedation, have prior evaluation by a sedation team, aspirate all gastric contents before gastrostomy tube placement, suction all insufflated air after gastrostomy tube is placed, and minimize procedural time[78].
Bleeding
Acute bleeding is a rare AE, which occurs roughly 1%. Of these, less than 0.5% requires blood transfusion and laparotomy due to bleeding[87,99-101]. The endoscopist should consider blood transfusion and temporarily holding anticoagulation per guidelines mentioned in prior section. Additionally, if the patient is particularly prone to bleeding, the pull technique should be considered over the introducer technique[38]. Cutaneous puncture should be performed lateral to the rectus muscle. Puncture of anterior gastric wall should be performed at the mid to distal body of the stomach and equidistant from the lesser and greater curvatures to avoid arterial injury[102,103]. Underlying lesions that can cause bleeding (i.e. ulcer, erosion, or angioma) should also be assessed.
Perforation and pneumoperitoneum
Inadvertent perforation of the intestines is a rare but potentially fatal AE. The endoscopist can minimize this, among other means, by performing a safe track maneuver to ensure no intervening loops of the bowel[2]. With high intragastric insufflation pressure during endoscopy, air may escape during gastrostomy tube insertion or needle puncture leading to pneumoperitoneum. Transient subclinical pneumoperitoneum is a common benign finding that is usually asymptomatic, but a minority of patients can have signs and symptoms of peritonitis. Carbon dioxide rather than ambient air may be used for insufflation to significantly reduce the severity of pneumoperitoneum[78,104]. Internal bolster placement below the upper body of the stomach can be used to prevent pneumoperitoneum[102].
Peristomal infection
Infection of the peristomal site can be prevented with appropriate pre-procedural antibiotic prophylaxis as described prior. Patients who have comorbid diabetes, obesity, poor nutritional status, or long-term corticosteroid administration have not only a higher incidence of mortality[105] but also infection risk[106]. Additionally, patients with diabetes, chronic kidney disease, pulmonary tuberculosis, or alcoholism could be at risk for the rare development of necrotizing fasciitis around the ostomy site[107-109]. Particular attention should be paid to patients with such comorbid conditions to prevent infection. Standard infection control measures such as aseptic surgical field preparation and preprocedural hand disinfection[78]. As expanded upon in the next sections, introducer technique has been associated with reports of intraperitoneal abscess[87]. The transoral approach has risks as well since it can drag oropharyngeal flora along with the tube, leading to increased peristomal infection rate[42]. If transoral technique is used in high risk chronically hospitalized patients, nasopharyngeal decolonization of MRSA and mouthwash with oral chlorhexidine solution can be considered to reduce peristomal infection[20,78].
Fungal tube degradation
Degradation of PEG tube by fungal colonization has been shown to cause PEG tube failure up to 37% of the time by 250 d and 70% of the time up to 450 d[110]. Fungal growth leads to brittleness, cracking, and obstruction of tube. Though there is no definitive management, the endoscopist should consider polyurethane tubing over silicone tubing to increase resistance to degradation[111,112].
Buried bumper syndrome
Buried bumper syndrome is a partial or complete growth of gastric mucosa over the internal bumper in the stomach. This could lead to migration of the bumper through the gastric wall and gastrostomy tract, which can cause abscess formation, leakage around the gastrostomy site, immobile gastrostomy tube, abdominal pain, and possible resistance to formula infusion. Risk factors include poor wound healing, malnutrition, significant weight gain due to successful nutrition, placement of internal bumper in the upper gastric body, and excess tension between the internal and external bumpers[2,102].
To reduce the risk of buried bumper, the endoscopist should place the outer bumper tight enough to ensure proper gastropexy but loose enough to allow room for post-procedural tissue swelling. The external bumper should be subjected to a very low traction without tension. The next day, the outer bumper should be loosened and rotated to allow back and forth movement at least 1 cm with minimum resistance. The tube should also be covered to prevent inadvertent tugging. The tube needs to be rotated daily and moved inward from 2 to 10 cm once the gastrostomy tract is healed around 7-10 d. Subsequent restricted movement, pain or leakage around the site should be evaluated for buried bumper as early endoscopic intervention can preserve the feeding tube[78,113,114]. The most common signs of buried bumper syndrome is an inability to move the PEG tube inward[78].
Ulceration
Ulceration or erosion from PEG tube can be found up to 1.2% of all cases. This is usually caused by friction of the gastric wall opposite to or underneath the internal bumper[20,87,100,115]. Similar to preventing buried bumper syndrome, the endoscopist should avoid excess tension between the internal and external bumpers, rotate the tube daily, and move the tube inward after the gastrostomy tract is healed[78]. The mucosa under the internal bumper should be visualized after placement, and excess lateral traction on the tube should be avoided[2].
Colonic injury and fistulae
Excessive gastric and small bowel insufflation can lead to bowel transposition and gastric rotation[80]. If the colon is accidentally punctured or cannulated, fistulous tracts can later form between stomach, colon, and skin. Many patients are asymptomatic but can develop severe diarrhea after feeding, fecal discharge around the tube, and even peritonitis and sepsis[78]. If the gastrostomy tube is replaced into a gastrocolocutaneous fistula, the tube could miss the gastrostomy and enter the colon creating a new colocutaneous fistula. The proceduralist can mitigate such AEs with safe track technique to avoid initial puncture of colon. Reverse Trendelenburg positioning, proper transillumination, and finger imprinting may help. If misplaced gastrostomy tube is suspected, radiographic imaging (CT) should be performed with subsequent removal of the misplaced tube[2,116].
Liver injury
Similar to colonic interposition, the lateral segment of the liver can interpose between the abdominal wall and stomach, leading to possible injury during gastrostomy placement. Injuries may be associated with bleeding but could be asymptomatic. As mentioned previously, caudal edge of the liver should be identified with physical exam before puncture[78].
Gastric outlet obstruction
Gastric outlet obstruction is usually seen in pediatric patients due to migration of the internal bumper and obstruction of the pyloric channel. It can occur in adults if catheter with internal balloon is used, and the balloon migrates into the pylorus or proximal small bowel. This can be prevented by reducing the length of tube inserted into the gastric lumen, though caution must be taken to avoid excess tension at the gastrostomy tube site[80].
Tube dislodgement and removal
Maturation of the gastrostomy tract usually occurs within the first seven to ten days after placement but can take weeks longer if there is concurrent malnutrition, ascites, or steroid treatment. If gastrostomy tube is removed during this period, it should be replaced endoscopically or radiographically as an immature tract can result in free perforation. Altered mental status including delirium and dementia increase the risk for accidental tube removal. Additionally, internal bolster placement in the upper body of the stomach increases risk of dislodgement[102]. Measures should be taken to reduce such events, such as using abdominal binders or elastic bandage to restrict access, gastropexy devices at time of tube placement, proper gastrostomy site choice, and use of low-profile gastrostomy button with detachable extension tubing. The latter is already used in the pediatric population to reduce risk of dislodgement[78,117].
Tube occlusion
Tube occlusion when feeding can be caused by obstruction of the internal lumen or mechanical tube failure. Smaller bore feeding tubes (less than 10-12 French) are more prone to occlusion with repeated gastric residual aspiration[118]. The endoscopist should consider placing larger bore tubes if possible[119].
Gastrostomy tract tumor seeding
Transoral approach of PEG tube placement may increase risk of tumor seeding in patients with head and neck malignancy due to contact with malignant cells during tube insertion[43-47]. Thus, transabdominal methods such as the introducer, SLiC, PRG, and LAPEG techniques should be highly considered in these patients.
CONCLUSION
PEG has gained increasing acceptance as a safe and effective technique to provide enteral nutrition for a wide variety of indications. However, the preprocedural evaluation and selection of patients remains paramount to provide optimal benefit while reducing risk of AEs. The endoscopist should examine indications, contraindications, ethical considerations, and comorbidities of patients referred for gastrostomy placement. Additionally, the endoscopist should consider whether radiologic or surgical tube placement may be more appropriate, and whether a transoral or transabdominal technique is best. If gastrostomy placement appears indicated, physical exam, imaging, and other interventions should be performed to reduce procedure-related AEs.
Footnotes
Conflict-of-interest statement: All the Authors have no conflict of interest related to the manuscript.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: December 18, 2021
First decision: January 27, 2022
Article in press: April 3, 2022
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Balakrishnan DS, India; Masaki S, Japan S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
Contributor Information
Anand Rajan, Department ofGastroenterology, Olive View-UCLA Medical Center, Sylmar, CA 91342, United States; Department ofGastroenterology, City of Hope Medical Center, Duarte, CA 91010, United States.
Peerapol Wangrattanapranee, Department ofMedicine, Keck School of Medicine of USC, Los Angeles, CA 90033, United States.
Jonathan Kessler, Department ofInterventional Radiology, City of Hope Medical Center, Duarte, CA 91010, United States.
Trilokesh Dey Kidambi, Department ofGastroenterology, City of Hope Medical Center, Duarte, CA 91010, United States.
James H Tabibian, Department ofGastroenterology, UCLA-Olive View Medical Center, Sylmar, CA 91342, United States. jtabibian@dhs.lacounty.gov.
References
- 1.Westaby D, Young A, O'Toole P, Smith G, Sanders DS. The provision of a percutaneously placed enteral tube feeding service. Gut. 2010;59:1592–1605. doi: 10.1136/gut.2009.204982. [DOI] [PubMed] [Google Scholar]
- 2.Itkin M, DeLegge MH, Fang JC, McClave SA, Kundu S, d'Othee BJ, Martinez-Salazar GM, Sacks D, Swan TL, Towbin RB, Walker TG, Wojak JC, Zuckerman DA, Cardella JF Society of Interventional Radiology; American Gastroenterological Association Institute; Canadian Interventional Radiological Association; Cardiovascular and Interventional Radiological Society of Europe. Multidisciplinary practical guidelines for gastrointestinal access for enteral nutrition and decompression from the Society of Interventional Radiology and American Gastroenterological Association (AGA) Institute, with endorsement by Canadian Interventional Radiological Association (CIRA) and Cardiovascular and Interventional Radiological Society of Europe (CIRSE) Gastroenterology. 2011;141:742–765. doi: 10.1053/j.gastro.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 3.ASGE Technology Committee, Kwon RS, Banerjee S, Desilets D, Diehl DL, Farraye FA, Kaul V, Mamula P, Pedrosa MC, Rodriguez SA, Varadarajulu S, Song LM, Tierney WM. Enteral nutrition access devices. Gastrointest Endosc. 2010;72:236–248. doi: 10.1016/j.gie.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Stein DJ, Moore MB, Hoffman G, Feuerstein JD. Improving All-Cause Inpatient Mortality After Percutaneous Endoscopic Gastrostomy. Dig Dis Sci. 2021;66:1593–1599. doi: 10.1007/s10620-020-06396-y. [DOI] [PubMed] [Google Scholar]
- 5.Lucendo AJ, Friginal-Ruiz AB. Percutaneous endoscopic gastrostomy: An update on its indications, management, complications, and care. Rev Esp Enferm Dig. 2014;106:529–539. [PubMed] [Google Scholar]
- 6.Ponsky JL, Gauderer MW. Percutaneous endoscopic gastrostomy: a nonoperative technique for feeding gastrostomy. Gastrointest Endosc. 1981;27:9–11. doi: 10.1016/s0016-5107(81)73133-x. [DOI] [PubMed] [Google Scholar]
- 7.Gauderer MW, Ponsky JL, Izant RJ Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15:872–875. doi: 10.1016/s0022-3468(80)80296-x. [DOI] [PubMed] [Google Scholar]
- 8.Sacks BA, Vine HS, Palestrant AM, Ellison HP, Shropshire D, Lowe R. A nonoperative technique for establishment of a gastrostomy in the dog. Invest Radiol. 1983;18:485–487. doi: 10.1097/00004424-198309000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Hogan RB, DeMarco DC, Hamilton JK, Walker CO, Polter DE. Percutaneous endoscopic gastrostomy--to push or pull. A prospective randomized trial. Gastrointest Endosc. 1986;32:253–258. doi: 10.1016/s0016-5107(86)71841-5. [DOI] [PubMed] [Google Scholar]
- 10.Russell TR, Brotman M, Norris F. Percutaneous gastrostomy. A new simplified and cost-effective technique. Am J Surg. 1984;148:132–137. doi: 10.1016/0002-9610(84)90300-3. [DOI] [PubMed] [Google Scholar]
- 11.Dormann AJ, Wejda B, Kahl S, Huchzermeyer H, Ebert MP, Malfertheiner P. Long-term results with a new introducer method with gastropexy for percutaneous endoscopic gastrostomy. Am J Gastroenterol. 2006;101:1229–1234. doi: 10.1111/j.1572-0241.2006.00541.x. [DOI] [PubMed] [Google Scholar]
- 12.Sabnis A, Liu R, Chand B, Ponsky J. SLiC technique. A novel approach to percutaneous gastrostomy. Surg Endosc. 2006;20:256–262. doi: 10.1007/s00464-005-0383-3. [DOI] [PubMed] [Google Scholar]
- 13.McClave SA. Techniques in Enteral Access. In: Clinical Gastrointestinal Endoscopy. Elsevier; 2019: 467-487.e2. [Google Scholar]
- 14.Bosco JJ, Barkun AN, Isenberg GA, Nguyen CC, Petersen BT, Silverman WB, Slivka A, Taitelbaum G, Ginsberg GG ASGE Technology Assessment Committee. Endoscopic enteral nutritional access devices. Gastrointest Endosc. 2002;56:796–802. doi: 10.1016/s0016-5107(02)70350-7. [DOI] [PubMed] [Google Scholar]
- 15.Preshaw RM. A percutaneous method for inserting a feeding gastrostomy tube. Surg Gynecol Obstet. 1981;152:658–660. [PubMed] [Google Scholar]
- 16.Brown AS, Mueller PR, Ferrucci JT Jr. Controlled percutaneous gastrostomy: nylon T-fastener for fixation of the anterior gastric wall. Radiology. 1986;158:543–545. doi: 10.1148/radiology.158.2.2934763. [DOI] [PubMed] [Google Scholar]
- 17.Coleman CC, Coons HG, Cope C, Derauf BJ, Krenzel C, Epstein DH, Schlam BW, Castaneda F, Hough JP, Moradian GP. Percutaneous enterostomy with the Cope suture anchor. Radiology. 1990;174:889–891. doi: 10.1148/radiology.174.3.2406788. [DOI] [PubMed] [Google Scholar]
- 18.Laasch HU, Wilbraham L, Bullen K, Marriott A, Lawrance JA, Johnson RJ, Lee SH, England RE, Gamble GE, Martin DF. Gastrostomy insertion: comparing the options--PEG, RIG or PIG? Clin Radiol. 2003;58:398–405. doi: 10.1016/s0009-9260(03)00058-8. [DOI] [PubMed] [Google Scholar]
- 19.Ahmed O, Jilani D, Sheth S, Giger M, Funaki B. Radiologically Guided Placement of Mushroom-retained Gastrostomy Catheters: Long-term Outcomes of Use in 300 Patients at a Single Center. Radiology. 2015;276:588–596. doi: 10.1148/radiol.15141327. [DOI] [PubMed] [Google Scholar]
- 20.Selby D, Nolen A, Sittambalam C, Johansen K, Pugash R. Percutaneous Transesophageal Gastrostomy (PTEG): A Safe and Well-Tolerated Procedure for Palliation of End-Stage Malignant Bowel Obstruction. J Pain Symptom Manage. 2019;58:306–310. doi: 10.1016/j.jpainsymman.2019.04.031. [DOI] [PubMed] [Google Scholar]
- 21.Oishi H, Shindo H, Shirotani N, Kameoka S. A nonsurgical technique to create an esophagostomy for difficult cases of percutaneous endoscopic gastrostomy. Surg Endosc. 2003;17:1224–1227. doi: 10.1007/s00464-002-8948-x. [DOI] [PubMed] [Google Scholar]
- 22.Mackey R, Chand B, Oishi H, Kameoka S, Ponsky JL. Percutaneous transesophageal gastrostomy tube for decompression of malignant obstruction: report of the first case and our series in the US. J Am Coll Surg. 2005;201:695–700. doi: 10.1016/j.jamcollsurg.2005.05.036. [DOI] [PubMed] [Google Scholar]
- 23.Udomsawaengsup S, Brethauer S, Kroh M, Chand B. Percutaneous transesophageal gastrostomy (PTEG): a safe and effective technique for gastrointestinal decompression in malignant obstruction and massive ascites. Surg Endosc. 2008;22:2314–2318. doi: 10.1007/s00464-008-9984-y. [DOI] [PubMed] [Google Scholar]
- 24.Murakami M, Nishino K, Takaoka Y, Murakami S, Mori K, Murakami B, Azuma M, Tanabe S, Kida M, Koizumi W. Endoscopically assisted percutaneous transesophageal gastrotubing: a retrospective pilot study. Eur J Gastroenterol Hepatol. 2013;25:989–995. doi: 10.1097/MEG.0b013e3283614ae1. [DOI] [PubMed] [Google Scholar]
- 25.Singal AK, Dekovich AA, Tam AL, Wallace MJ. Percutaneous transesophageal gastrostomy tube placement: an alternative to percutaneous endoscopic gastrostomy in patients with intra-abdominal metastasis. Gastrointest Endosc. 2010;71:402–406. doi: 10.1016/j.gie.2009.10.037. [DOI] [PubMed] [Google Scholar]
- 26.Murayama KM, Schneider PD, Thompson JS. Laparoscopic gastrostomy: a safe method for obtaining enteral access. J Surg Res. 1995;58:1–5. doi: 10.1006/jsre.1995.1001. [DOI] [PubMed] [Google Scholar]
- 27.Bolder U, Scherer MN, Schmidt T, Hornung M, Schlitt HJ, Vogel P. Percutaneous laparoscopic assisted gastrostomy (PLAG)--a new technique for cases of pharyngoesophageal obstruction. Langenbecks Arch Surg. 2010;395:1107–1113. doi: 10.1007/s00423-010-0612-7. [DOI] [PubMed] [Google Scholar]
- 28.Serrano Aguayo P, Gros Herguido N, Parejo Campos J, Barranco Moreno A, Tous Romero MDC, Pereira Cunill JL, Alarcón Del Agua I, Socas Macias M, García Luna PP, Morales Conde S. New laparoscopic assisted percutaneous gastrostomy. Description and comparison with others gastrostomy types. Clin Nutr ESPEN. 2016;16:24–29. doi: 10.1016/j.clnesp.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Ha L, Hauge T. Percutaneous endoscopic gastrostomy (PEG) for enteral nutrition in patients with stroke. Scand J Gastroenterol. 2003;38:962–966. doi: 10.1080/00365520310005190. [DOI] [PubMed] [Google Scholar]
- 30.Thaker AM, Sedarat A. Laparoscopic-Assisted Percutaneous Endoscopic Gastrostomy. Curr Gastroenterol Rep. 2016;18:46. doi: 10.1007/s11894-016-0520-2. [DOI] [PubMed] [Google Scholar]
- 31.Raaf JH, Manney M, Okafor E, Gray L, Chari V. Laparoscopic placement of a percutaneous endoscopic gastrostomy (PEG) feeding tube. J Laparoendosc Surg. 1993;3:411–414. doi: 10.1089/lps.1993.3.411. [DOI] [PubMed] [Google Scholar]
- 32.Smitherman S, Pimpalwar A. Laparoendoscopic gastrostomy tube placement: our all-in-one technique. J Laparoendosc Adv Surg Tech A. 2009;19:119–123. doi: 10.1089/lap.2007.0210. [DOI] [PubMed] [Google Scholar]
- 33.Lopes G, Salcone M, Neff M. Laparoscopic-assisted percutaneous endoscopic gastrostomy tube placement. JSLS. 2010;14:66–69. doi: 10.4293/108680810X12674612014662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Croshaw RL, Nottingham JM. Laparoscopic-assisted percutaneous endoscopic gastrostomy: its role in providing enteric access when percutaneous endoscopic gastrostomy is not possible. Am Surg. 2006;72:1222–1224. [PubMed] [Google Scholar]
- 35.Currie BM, Getrajdman GI, Covey AM, Alago W Jr, Erinjeri JP, Maybody M, Boas FE. Push versus pull gastrostomy in cancer patients: A single center retrospective analysis of complications and technical success rates. Diagn Interv Imaging. 2018;99:547–553. doi: 10.1016/j.diii.2018.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sutcliffe J, Wigham A, Mceniff N, Dvorak P, Crocetti L, Uberoi R. CIRSE Standards of Practice Guidelines on Gastrostomy. Cardiovasc Intervent Radiol. 2016;39:973–987. doi: 10.1007/s00270-016-1344-z. [DOI] [PubMed] [Google Scholar]
- 37.Köhler G, Kalcher V, Koch OO, Luketina RR, Emmanuel K, Spaun G. Comparison of 231 patients receiving either "pull-through" or "push" percutaneous endoscopic gastrostomy. Surg Endosc. 2015;29:170–175. doi: 10.1007/s00464-014-3673-9. [DOI] [PubMed] [Google Scholar]
- 38.Retes FA, Kawaguti FS, de Lima MS, da Costa Martins B, Uemura RS, de Paulo GA, Pennacchi CM, Gusmon C, Ribeiro AV, Baba ER, Geiger SN, Sorbello MP, Kulcsar MA, Ribeiro U Jr, Maluf-Filho F. Comparison of the pull and introducer percutaneous endoscopic gastrostomy techniques in patients with head and neck cancer. United European Gastroenterol J. 2017;5:365–373. doi: 10.1177/2050640616662160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kulvatunyou N, Zimmerman SA, Sadoun M, Joseph BA, Friese RS, Gries LM, O'Keeffe T, Tang AL. Comparing Outcomes Between "Pull" Versus "Push" Percutaneous Endoscopic Gastrostomy in Acute Care Surgery: Under-Reported Pull Percutaneous Endoscopic Gastrostomy Incidence of Tube Dislodgement. J Surg Res. 2018;232:56–62. doi: 10.1016/j.jss.2018.06.011. [DOI] [PubMed] [Google Scholar]
- 40.Timratana P, El-Hayek K, Shimizu H, Kroh M, Chand B. Percutaneous endoscopic gastrostomy (PEG) with T-fasteners obviates the need for emergent replacement after early tube dislodgement. Surg Endosc. 2012;26:3541–3547. doi: 10.1007/s00464-012-2348-7. [DOI] [PubMed] [Google Scholar]
- 41.Prathanvanich P, Chand B. Novel methods of enteral access. Tech Gastrointest Endosc. 2013;15:216–223. [Google Scholar]
- 42.Maetani I, Tada T, Ukita T, Inoue H, Sakai Y, Yoshikawa M. PEG with introducer or pull method: a prospective randomized comparison. Gastrointest Endosc. 2003;57:837–841. doi: 10.1016/s0016-5107(03)70017-0. [DOI] [PubMed] [Google Scholar]
- 43.Tucker AT, Gourin CG, Ghegan MD, Porubsky ES, Martindale RG, Terris DJ. 'Push' versus 'pull' percutaneous endoscopic gastrostomy tube placement in patients with advanced head and neck cancer. Laryngoscope. 2003;113:1898–1902. doi: 10.1097/00005537-200311000-00007. [DOI] [PubMed] [Google Scholar]
- 44.Foster JM, Filocamo P, Nava H, Schiff M, Hicks W, Rigual N, Smith J, Loree T, Gibbs JF. The introducer technique is the optimal method for placing percutaneous endoscopic gastrostomy tubes in head and neck cancer patients. Surg Endosc. 2007;21:897–901. doi: 10.1007/s00464-006-9068-9. [DOI] [PubMed] [Google Scholar]
- 45.Cappell MS. Risk factors and risk reduction of malignant seeding of the percutaneous endoscopic gastrostomy track from pharyngoesophageal malignancy: a review of all 44 known reported cases. Am J Gastroenterol. 2007;102:1307–1311. doi: 10.1111/j.1572-0241.2007.01227.x. [DOI] [PubMed] [Google Scholar]
- 46.Teriaky A, Gregor J, Chande N. Percutaneous endoscopic gastrostomy tube placement for end-stage palliation of malignant gastrointestinal obstructions. Saudi J Gastroenterol. 2012;18:95–98. doi: 10.4103/1319-3767.93808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fung E, Strosberg DS, Jones EL, Dettorre R, Suzo A, Meara MP, Narula VK, Hazey JW. Incidence of abdominal wall metastases following percutaneous endoscopic gastrostomy placement in patients with head and neck cancer. Surg Endosc. 2017;31:3623–3627. doi: 10.1007/s00464-016-5394-8. [DOI] [PubMed] [Google Scholar]
- 48.Oakley RJ, Donnelly R, Freeman L, Wong T, McCarthy M, Calman F, O'Connell M, Jeannon JP, Simo R. An audit of percutaneous endoscopic gastrostomy insertion in patients undergoing treatment for head and neck cancer: reducing the incidence of peri-operative airway events by the introduction of a tumour assessment protocol. Ann R Coll Surg Engl. 2009;91:249–254. doi: 10.1308/003588409X391857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yip D, Vanasco M, Funaki B. Complication rates and patency of radiologically guided mushroom gastrostomy, balloon gastrostomy, and gastrojejunostomy: a review of 250 procedures. Cardiovasc Intervent Radiol. 2004;27:3–8. doi: 10.1007/s00270-003-0108-8. [DOI] [PubMed] [Google Scholar]
- 50.Horiuchi A, Nakayama Y, Tanaka N, Fujii H, Kajiyama M. Prospective randomized trial comparing the direct method using a 24 Fr bumper-button-type device with the pull method for percutaneous endoscopic gastrostomy. Endoscopy. 2008;40:722–726. doi: 10.1055/s-2008-1077490. [DOI] [PubMed] [Google Scholar]
- 51.Ogino H, Akiho H. Usefulness of percutaneous endoscopic gastrostomy for supportive therapy of advanced aerodigestive cancer. World J Gastrointest Pathophysiol. 2013;4:119–125. doi: 10.4291/wjgp.v4.i4.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kozarek RA, Ball TJ, Ryan JA Jr. When push comes to shove: a comparison between two methods of percutaneous endoscopic gastrostomy. Am J Gastroenterol. 1986;81:642–646. [PubMed] [Google Scholar]
- 53.Akkersdijk WL, van Bergeijk JD, van Egmond T, Mulder CJ, van Berge Henegouwen GP, van der Werken C, van Erpecum KJ. Percutaneous endoscopic gastrostomy (PEG): comparison of push and pull methods and evaluation of antibiotic prophylaxis. Endoscopy. 1995;27:313–316. doi: 10.1055/s-2007-1005699. [DOI] [PubMed] [Google Scholar]
- 54.Wollman B, D'Agostino HB, Walus-Wigle JR, Easter DW, Beale A. Radiologic, endoscopic, and surgical gastrostomy: an institutional evaluation and meta-analysis of the literature. Radiology. 1995;197:699–704. doi: 10.1148/radiology.197.3.7480742. [DOI] [PubMed] [Google Scholar]
- 55.Neeff M, Crowder VL, McIvor NP, Chaplin JM, Morton RP. Comparison of the use of endoscopic and radiologic gastrostomy in a single head and neck cancer unit. ANZ J Surg. 2003;73:590–593. doi: 10.1046/j.1445-2197.2003.t01-1-02695.x. [DOI] [PubMed] [Google Scholar]
- 56.Kohli DR, Kennedy KF, Desai M, Sharma P. Safety of endoscopic gastrostomy tube placement compared with radiologic or surgical gastrostomy: nationwide inpatient assessment. Gastrointest Endosc. 2021;93:1077–1085.e1. doi: 10.1016/j.gie.2020.09.012. [DOI] [PubMed] [Google Scholar]
- 57.Galaski A, Peng WW, Ellis M, Darling P, Common A, Tucker E. Gastrostomy tube placement by radiological versus endoscopic methods in an acute care setting: a retrospective review of frequency, indications, complications and outcomes. Can J Gastroenterol. 2009;23:109–114. doi: 10.1155/2009/801925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Silas AM, Pearce LF, Lestina LS, Grove MR, Tosteson A, Manganiello WD, Bettmann MA, Gordon SR. Percutaneous radiologic gastrostomy versus percutaneous endoscopic gastrostomy: a comparison of indications, complications and outcomes in 370 patients. Eur J Radiol. 2005;56:84–90. doi: 10.1016/j.ejrad.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 59.Yang B, Shi X. Percutaneous endoscopic gastrostomy versus fluoroscopic gastrostomy in amyotrophic lateral sclerosis (ALS) sufferers with nutritional impairment: A meta-analysis of current studies. Oncotarget. 2017;8:102244–102253. doi: 10.18632/oncotarget.22288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Clayton S, DeClue C, Lewis T, Rodriguez A, Kolkhorst K, Syed R, Kumar A, Davis C, Brady P. Radiologic versus Endoscopic Placement of Gastrostomy Tube: Comparison of Indications and Outcomes at a Tertiary Referral Center. South Med J. 2019;112:39–44. doi: 10.14423/SMJ.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 61.Park SK, Kim JY, Koh SJ, Lee YJ, Jang HJ, Park SJ Small Intestine and Nutrition Research Group of the Korean Association for the Study of Intestinal Diseases (KASID) Complications of percutaneous endoscopic and radiologic gastrostomy tube insertion: a KASID (Korean Association for the Study of Intestinal Diseases) study. Surg Endosc. 2019;33:750–756. doi: 10.1007/s00464-018-6339-1. [DOI] [PubMed] [Google Scholar]
- 62.Bankhead RR, Fisher CA, Rolandelli RH. Gastrostomy tube placement outcomes: comparison of surgical, endoscopic, and laparoscopic methods. Nutr Clin Pract. 2005;20:607–612. doi: 10.1177/0115426505020006607. [DOI] [PubMed] [Google Scholar]
- 63.Hermanowicz A, Matuszczak E, Komarowska M, Jarocka-Cyrta E, Wojnar J, Debek W, Matysiak K, Klek S. Laparoscopy-assisted percutaneous endoscopic gastrostomy enables enteral nutrition even in patients with distorted anatomy. World J Gastroenterol. 2013;19:7696–7700. doi: 10.3748/wjg.v19.i43.7696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chang WK, McClave SA, Yu CY, Huang HH, Chao YC. Positioning a safe gastric puncture point before percutaneous endoscopic gastrostomy. Int J Clin Pract. 2007;61:1121–1125. doi: 10.1111/j.1742-1241.2006.01106.x. [DOI] [PubMed] [Google Scholar]
- 65.Petrosyan M, Khalafallah AM, Franklin AL, Doan T, Kane TD. Laparoscopic Gastrostomy Is Superior to Percutaneous Endoscopic Gastrostomy Tube Placement in Children Less Than 5 years of Age. J Laparoendosc Adv Surg Tech A. 2016;26:570–573. doi: 10.1089/lap.2016.0099. [DOI] [PubMed] [Google Scholar]
- 66.Lantz M, Hultin Larsson H, Arnbjörnsson E. Literature review comparing laparoscopic and percutaneous endoscopic gastrostomies in a pediatric population. Int J Pediatr. 2010;2010:507616. doi: 10.1155/2010/507616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Haskins IN, Strong AT, Baginsky M, Sharma G, Karafa M, Ponsky JL, Rodriguez JH, Kroh MD. Comparison of laparoscopic jejunostomy tube to percutaneous endoscopic gastrostomy tube with jejunal extension: long-term durability and nutritional outcomes. Surg Endosc. 2018;32:2496–2504. doi: 10.1007/s00464-017-5954-6. [DOI] [PubMed] [Google Scholar]
- 68.Van Rosendaal GM, Verhoef MJ, Kinsella TD. How are decisions made about the use of percutaneous endoscopic gastrostomy for long-term nutritional support? Am J Gastroenterol. 1999;94:3225–3228. doi: 10.1111/j.1572-0241.1999.01522.x. [DOI] [PubMed] [Google Scholar]
- 69.Stathopoulos P, Karamanolis G, Papanikolaou IS, Polymeros D, Papadopoulos AA, Triantafyllou K. Percutaneous endoscopic gastrostomy: Patients' outcomes, adequacy and quality of information given to decision-makers and procedure acceptance. Ann Gastroenterol. 2011;24:29–34. [PMC free article] [PubMed] [Google Scholar]
- 70.DeLegge MH, McClave SA, DiSario JA, Baskin WN, Brown RD, Fang JC, Ginsberg GG ASGE Task Force on Enteral Nutrition. Ethical and medicolegal aspects of PEG-tube placement and provision of artificial nutritional therapy. Gastrointest Endosc. 2005;62:952–959. doi: 10.1016/j.gie.2005.08.024. [DOI] [PubMed] [Google Scholar]
- 71.Magnuson JS, Durst J, Rosenthal EL, Carroll WR, Ritchie CS, Kilgore ML, Locher JL. Increased likelihood of long-term gastrostomy tube dependence in head and neck cancer survivors without partners. Head Neck. 2013;35:420–425. doi: 10.1002/hed.22996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Angus F, Burakoff R. The percutaneous endoscopic gastrostomy tube. medical and ethical issues in placement. Am J Gastroenterol. 2003;98:272–277. doi: 10.1111/j.1572-0241.2003.07267.x. [DOI] [PubMed] [Google Scholar]
- 73.Rabeneck L, McCullough LB, Wray NP. Ethically justified, clinically comprehensive guidelines for percutaneous endoscopic gastrostomy tube placement. Lancet. 1997;349:496–498. doi: 10.1016/S0140-6736(96)07369-2. [DOI] [PubMed] [Google Scholar]
- 74.Kuraoka Y, Nakayama K. Factors influencing decision regret regarding placement of a PEG among substitute decision-makers of older persons in Japan: a prospective study. BMC Geriatr. 2017;17:134. doi: 10.1186/s12877-017-0524-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rosenberger LH, Newhook T, Schirmer B, Sawyer RG. Late accidental dislodgement of a percutaneous endoscopic gastrostomy tube: an underestimated burden on patients and the health care system. Surg Endosc. 2011;25:3307–3311. doi: 10.1007/s00464-011-1709-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kurien M, Andrews RE, Tattersall R, McAlindon ME, Wong EF, Johnston AJ, Hoeroldt B, Dear KL, Sanders DS. Gastrostomies Preserve But Do Not Increase Quality of Life for Patients and Caregivers. Clin Gastroenterol Hepatol. 2017;15:1047–1054. doi: 10.1016/j.cgh.2016.10.032. [DOI] [PubMed] [Google Scholar]
- 77.Callahan CM, Haag KM, Buchanan NN, Nisi R. Decision-making for percutaneous endoscopic gastrostomy among older adults in a community setting. J Am Geriatr Soc. 1999;47:1105–1109. doi: 10.1111/j.1532-5415.1999.tb05235.x. [DOI] [PubMed] [Google Scholar]
- 78.Boeykens K, Duysburgh I. Prevention and management of major complications in percutaneous endoscopic gastrostomy. BMJ Open Gastroenterol. 2021;8 doi: 10.1136/bmjgast-2021-000628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pruijsen JM, de Bruin A, Sekema G, Koetse HA, van Rheenen PF. Abdominal plain film before gastrostomy tube placement to predict success of percutaneous endoscopic procedure. J Pediatr Gastroenterol Nutr. 2013;56:186–190. doi: 10.1097/MPG.0b013e31826f750a. [DOI] [PubMed] [Google Scholar]
- 80.Singh A, Gelrud A. Adverse events associated with percutaneous enteral access. Gastrointest Endosc Clin N Am. 2015;25:71–82. doi: 10.1016/j.giec.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 81.Chang WK, Hsieh TY. Safety of percutaneous endoscopic gastrostomy in high-risk patients. J Gastroenterol Hepatol. 2013;28 Suppl 4:118–122. doi: 10.1111/jgh.12300. [DOI] [PubMed] [Google Scholar]
- 82.Gutjahr CJ, Iverson EP, Walker ST, Johnson JD, Shukla UC, Terrell W. Utility of pre-procedural CT and abdominal radiography before percutaneous radiologic gastrostomy placement. Abdom Radiol (NY) 2020;45:571–575. doi: 10.1007/s00261-019-02352-1. [DOI] [PubMed] [Google Scholar]
- 83.Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, Mallery JS, Raddawi HM, Vargo JJ 2nd, Waring JP, Fanelli RD, Wheeler-Harbough J American Society for Gastrointestinal Endoscopy. Guideline on the management of anticoagulation and antiplatelet therapy for endoscopic procedures. Gastrointest Endosc. 2002;55:775–779. doi: 10.1016/s0016-5107(02)70402-1. [DOI] [PubMed] [Google Scholar]
- 84.Gossner L, Keymling J, Hahn EG, Ell C. Antibiotic prophylaxis in percutaneous endoscopic gastrostomy (PEG): a prospective randomized clinical trial. Endoscopy. 1999;31:119–124. doi: 10.1055/s-1999-13658. [DOI] [PubMed] [Google Scholar]
- 85.Lipp A, Lusardi G. Systemic antimicrobial prophylaxis for percutaneous endoscopic gastrostomy. Cochrane Database Syst Rev. 2013:CD005571. doi: 10.1002/14651858.CD005571.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Campoli PM, de Paula AA, Alves LG, Turchi MD. Effect of the introducer technique compared with the pull technique on the peristomal infection rate in PEG: a meta-analysis. Gastrointest Endosc. 2012;75:988–996. doi: 10.1016/j.gie.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 87.Petersen TI, Kruse A. Complications of percutaneous endoscopic gastrostomy. Eur J Surg. 1997;163:351–356. [PubMed] [Google Scholar]
- 88.Adachi Y, Akino K, Mita H, Kikuchi T, Yamashita K, Sasaki Y, Arimura Y, Endo T. Systemic Prophylactic Antibiotics for the Modified Introducer Method for Percutaneous Endoscopic Gastrostomy: A Prospective, Randomized, Double-Blind Study. J Clin Gastroenterol. 2016;50:727–732. doi: 10.1097/MCG.0000000000000470. [DOI] [PubMed] [Google Scholar]
- 89.ASGE Standards of Practice Committee. Banerjee S, Shen B, Baron TH, Nelson DB, Anderson MA, Cash BD, Dominitz JA, Gan SI, Harrison ME, Ikenberry SO, Jagannath SB, Lichtenstein D, Fanelli RD, Lee K, van Guilder T, Stewart LE. Antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc. 2008;67:791–798. doi: 10.1016/j.gie.2008.02.068. [DOI] [PubMed] [Google Scholar]
- 90.Blomberg J, Lagergren P, Martin L, Mattsson F, Lagergren J. Novel approach to antibiotic prophylaxis in percutaneous endoscopic gastrostomy (PEG): randomised controlled trial. BMJ. 2010;341:c3115. doi: 10.1136/bmj.c3115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Malloy PC, Grassi CJ, Kundu S, Gervais DA, Miller DL, Osnis RB, Postoak DW, Rajan DK, Sacks D, Schwartzberg MS, Zuckerman DA, Cardella JF Standards of Practice Committee with Cardiovascular and Interventional Radiological Society of Europe (CIRSE) Endorsement. Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous image-guided interventions. J Vasc Interv Radiol. 2009;20:S240–S249. doi: 10.1016/j.jvir.2008.11.027. [DOI] [PubMed] [Google Scholar]
- 92.Patel IJ, Davidson JC, Nikolic B, Salazar GM, Schwartzberg MS, Walker TG, Saad WE Standards of Practice Committee, with Cardiovascular and Interventional Radiological Society of Europe (CIRSE) Endorsement; Standards of Practice Committee of the Society of Interventional Radiology. Addendum of newer anticoagulants to the SIR consensus guideline. J Vasc Interv Radiol. 2013;24:641–645. doi: 10.1016/j.jvir.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 93.Patel IJ, Rahim S, Davidson JC, Hanks SE, Tam AL, Walker TG, Wilkins LR, Sarode R, Weinberg I. Society of Interventional Radiology Consensus Guidelines for the Periprocedural Management of Thrombotic and Bleeding Risk in Patients Undergoing Percutaneous Image-Guided Interventions-Part II: Recommendations: Endorsed by the Canadian Association for Interventional Radiology and the Cardiovascular and Interventional Radiological Society of Europe. J Vasc Interv Radiol. 2019;30:1168–1184.e1. doi: 10.1016/j.jvir.2019.04.017. [DOI] [PubMed] [Google Scholar]
- 94.Davidson JC, Rahim S, Hanks SE, Patel IJ, Tam AL, Walker TG, Weinberg I, Wilkins LR, Sarode R. Society of Interventional Radiology Consensus Guidelines for the Periprocedural Management of Thrombotic and Bleeding Risk in Patients Undergoing Percutaneous Image-Guided Interventions-Part I: Review of Anticoagulation Agents and Clinical Considerations: Endorsed by the Canadian Association for Interventional Radiology and the Cardiovascular and Interventional Radiological Society of Europe. J Vasc Interv Radiol. 2019;30:1155–1167. doi: 10.1016/j.jvir.2019.04.016. [DOI] [PubMed] [Google Scholar]
- 95.Lucendo AJ, Sánchez-Casanueva T, Redondo O, Tenías JM, Arias Á. Risk of bleeding in patients undergoing percutaneous endoscopic gastrotrostomy (PEG) tube insertion under antiplatelet therapy: a systematic review with a meta-analysis. Rev Esp Enferm Dig. 2015;107:128–136. [PubMed] [Google Scholar]
- 96.Thosani N, Rashtak S, Kannadath BS, Munjal A, Meriwether M, Yoon ED, Hermann A, Ali S, Haddad PG, Patil P, Ramireddy S, Badillo R, DaVee RT, Guha S. Bleeding Risk and Mortality Associated With Uninterrupted Antithrombotic Therapy During Percutaneous Endoscopic Gastrostomy Tube Placement. Am J Gastroenterol. 2021;116:1868–1875. doi: 10.14309/ajg.0000000000001348. [DOI] [PubMed] [Google Scholar]
- 97.Singh D, Laya AS, Vaidya OU, Ahmed SA, Bonham AJ, Clarkston WK. Risk of bleeding after percutaneous endoscopic gastrostomy (PEG) Dig Dis Sci. 2012;57:973–980. doi: 10.1007/s10620-011-1965-7. [DOI] [PubMed] [Google Scholar]
- 98.Grant JP. Percutaneous endoscopic gastrostomy. Initial placement by single endoscopic technique and long-term follow-up. Ann Surg. 1993;217:168–174. doi: 10.1097/00000658-199302000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rabeneck L, Wray NP, Petersen NJ. Long-term outcomes of patients receiving percutaneous endoscopic gastrostomy tubes. J Gen Intern Med. 1996;11:287–293. doi: 10.1007/BF02598270. [DOI] [PubMed] [Google Scholar]
- 100.Amann W, Mischinger HJ, Berger A, Rosanelli G, Schweiger W, Werkgartner G, Fruhwirth J, Hauser H. Percutaneous endoscopic gastrostomy (PEG). 8 years of clinical experience in 232 patients. Surg Endosc. 1997;11:741–744. doi: 10.1007/s004649900440. [DOI] [PubMed] [Google Scholar]
- 101.Mamel JJ. Percutaneous endoscopic gastrostomy. Am J Gastroenterol. 1989;84:703–710. [PubMed] [Google Scholar]
- 102.Lee SP, Lee KN, Lee OY, Lee HL, Jun DW, Yoon BC, Choi HS, Kim SH. Risk factors for complications of percutaneous endoscopic gastrostomy. Dig Dis Sci. 2014;59:117–125. doi: 10.1007/s10620-013-2891-7. [DOI] [PubMed] [Google Scholar]
- 103.Shin JH, Park AW. Updates on percutaneous radiologic gastrostomy/gastrojejunostomy and jejunostomy. Gut Liver. 2010;4 Suppl 1:S25–S31. doi: 10.5009/gnl.2010.4.S1.S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Murphy CJ, Adler DG, Cox K, Sommers DN, Fang JC. Insufflation with carbon dioxide reduces pneumoperitoneum after percutaneous endoscopic gastrostomy (PEG): a randomized controlled trial. Endosc Int Open. 2016;4:E292–E295. doi: 10.1055/s-0042-100192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Calton WC, Martindale RG, Gooden SM. Complications of percutaneous endoscopic gastrostomy. Mil Med. 1992;157:358–360. [PubMed] [Google Scholar]
- 106.Lee JH, Kim JJ, Kim YH, Jang JK, Son HJ, Peck KR, Rhee PL, Paik SW, Rhee JC, Choi KW. Increased risk of peristomal wound infection after percutaneous endoscopic gastrostomy in patients with diabetes mellitus. Dig Liver Dis. 2002;34:857–861. doi: 10.1016/s1590-8658(02)80256-0. [DOI] [PubMed] [Google Scholar]
- 107.Person JL, Brower RA. Necrotizing fasciitis/myositis following percutaneous endoscopic gastrostomy. Gastrointest Endosc. 1986;32:309. doi: 10.1016/s0016-5107(86)71867-1. [DOI] [PubMed] [Google Scholar]
- 108.Korula J, Rice HE. Necrotizing fasciitis and percutaneous endoscopic gastrostomy. Gastrointest Endosc. 1987;33:335–336. doi: 10.1016/s0016-5107(87)71622-8. [DOI] [PubMed] [Google Scholar]
- 109.Cave DR, Robinson WR, Brotschi EA. Necrotizing fasciitis following percutaneous endoscopic gastrostomy. Gastrointest Endosc. 1986;32:294–296. doi: 10.1016/s0016-5107(86)71852-x. [DOI] [PubMed] [Google Scholar]
- 110.Iber FL, Livak A, Patel M. Importance of fungus colonization in failure of silicone rubber percutaneous gastrostomy tubes (PEGs) Dig Dis Sci. 1996;41:226–231. doi: 10.1007/BF02208608. [DOI] [PubMed] [Google Scholar]
- 111.Sartori S, Trevisani L, Nielsen I, Tassinari D, Ceccotti P, Abbasciano V. Longevity of silicone and polyurethane catheters in long-term enteral feeding via percutaneous endoscopic gastrostomy. Aliment Pharmacol Ther. 2003;17:853–856. doi: 10.1046/j.1365-2036.2003.01538.x. [DOI] [PubMed] [Google Scholar]
- 112.Blacka J, Donoghue J, Sutherland M, Martincich I, Mitten-Lewis S, Morris P, Meredith G. Dwell time and functional failure in percutaneous endoscopic gastrostomy tubes: a prospective randomized-controlled comparison between silicon polymer and polyurethane percutaneous endoscopic gastrostomy tubes. Aliment Pharmacol Ther. 2004;20:875–882. doi: 10.1111/j.1365-2036.2004.02191.x. [DOI] [PubMed] [Google Scholar]
- 113.Ma MM, Semlacher EA, Fedorak RN, Lalor EA, Duerksen DR, Sherbaniuk RW, Chalpelsky CE, Sadowski DC. The buried gastrostomy bumper syndrome: prevention and endoscopic approaches to removal. Gastrointest Endosc. 1995;41:505–508. doi: 10.1016/s0016-5107(05)80012-4. [DOI] [PubMed] [Google Scholar]
- 114.McClave SA, Jafri NS. Spectrum of morbidity related to bolster placement at time of percutaneous endoscopic gastrostomy: buried bumper syndrome to leakage and peritonitis. Gastrointest Endosc Clin N Am. 2007;17:731–746. doi: 10.1016/j.giec.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 115.Rimon E. The safety and feasibility of percutaneous endoscopic gastrostomy placement by a single physician. Endoscopy. 2001;33:241–244. doi: 10.1055/s-2001-12800. [DOI] [PubMed] [Google Scholar]
- 116.Foutch PG, Talbert GA, Waring JP, Sanowski RA. Percutaneous endoscopic gastrostomy in patients with prior abdominal surgery: virtues of the safe tract. Am J Gastroenterol. 1988;83:147–150. [PubMed] [Google Scholar]
- 117.Cortez AR, Warren PW, Goddard GR, Jenkins TM, Sauser JA, Gerrein BT, Rymeski BA. Primary Placement of a Low-Profile Gastrostomy Button Is Safe and Associated With Improved Outcomes in Children. J Surg Res. 2020;249:156–162. doi: 10.1016/j.jss.2019.11.027. [DOI] [PubMed] [Google Scholar]
- 118.Powell KS, Marcuard SP, Farrior ES, Gallagher ML. Aspirating gastric residuals causes occlusion of small-bore feeding tubes. JPEN J Parenter Enteral Nutr. 1993;17:243–246. doi: 10.1177/0148607193017003243. [DOI] [PubMed] [Google Scholar]
- 119.Blumenstein I, Shastri YM, Stein J. Gastroenteric tube feeding: techniques, problems and solutions. World J Gastroenterol. 2014;20:8505–8524. doi: 10.3748/wjg.v20.i26.8505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pothuri B, Montemarano M, Gerardi M, Shike M, Ben-Porat L, Sabbatini P, Barakat RR. Percutaneous endoscopic gastrostomy tube placement in patients with malignant bowel obstruction due to ovarian carcinoma. Gynecol Oncol. 2005;96:330–334. doi: 10.1016/j.ygyno.2004.09.058. [DOI] [PubMed] [Google Scholar]
- 121.Kawata N, Kakushima N, Tanaka M, Sawai H, Imai K, Hagiwara T, Takao T, Hotta K, Yamaguchi Y, Takizawa K, Matsubayashi H, Ono H. Percutaneous endoscopic gastrostomy for decompression of malignant bowel obstruction. Dig Endosc. 2014;26:208–213. doi: 10.1111/den.12139. [DOI] [PubMed] [Google Scholar]
- 122.Thampy S, Najran P, Mullan D, Laasch HU. Safety and Efficacy of Venting Gastrostomy in Malignant Bowel Obstruction: A Systematic Review. J Palliat Care. 2020;35:93–102. doi: 10.1177/0825859719864915. [DOI] [PubMed] [Google Scholar]
- 123.Inaba Y, Yamaura H, Sato Y, Kashima M, Kato M, Inoue D, Kurinobu T, Sato T. Percutaneous radiologic gastrostomy in patients with malignant pharyngoesophageal obstruction. Jpn J Clin Oncol. 2013;43:713–718. doi: 10.1093/jjco/hyt069. [DOI] [PubMed] [Google Scholar]
- 124.Laval G, Marcelin-Benazech B, Guirimand F, Chauvenet L, Copel L, Durand A, Francois E, Gabolde M, Mariani P, Rebischung C, Servois V, Terrebonne E, Arvieux C French Society for Palliative Care; French Society for Digestive Surgery; French Society for Gastroenterology; French Association for Supportive Care in Oncology; French Society for Digestive Cancer. Recommendations for bowel obstruction with peritoneal carcinomatosis. J Pain Symptom Manage. 2014;48:75–91. doi: 10.1016/j.jpainsymman.2013.08.022. [DOI] [PubMed] [Google Scholar]
- 125.Kubrak C, Olson K, Jha N, Jensen L, McCargar L, Seikaly H, Harris J, Scrimger R, Parliament M, Baracos VE. Nutrition impact symptoms: key determinants of reduced dietary intake, weight loss, and reduced functional capacity of patients with head and neck cancer before treatment. Head Neck. 2010;32:290–300. doi: 10.1002/hed.21174. [DOI] [PubMed] [Google Scholar]
- 126.Jager-Wittenaar H, Dijkstra PU, Vissink A, van der Laan BF, van Oort RP, Roodenburg JL. Critical weight loss in head and neck cancer--prevalence and risk factors at diagnosis: an explorative study. Support Care Cancer. 2007;15:1045–1050. doi: 10.1007/s00520-006-0212-9. [DOI] [PubMed] [Google Scholar]
- 127.Dawson ER, Morley SE, Robertson AG, Soutar DS. Increasing dietary supervision can reduce weight loss in oral cancer patients. Nutr Cancer. 2001;41:70–74. doi: 10.1080/01635581.2001.9680614. [DOI] [PubMed] [Google Scholar]
- 128.Strom T, Trotti AM, Kish J, Rao NG, McCaffrey J, Padhya TA, Lin HY, Fulp W, Caudell JJ. Risk factors for percutaneous endoscopic gastrostomy tube placement during chemoradiotherapy for oropharyngeal cancer. JAMA Otolaryngol Head Neck Surg. 2013;139:1242–1246. doi: 10.1001/jamaoto.2013.5193. [DOI] [PubMed] [Google Scholar]
- 129.Jack DR, Dawson FR, Reilly JE, Shoaib T. Guideline for prophylactic feeding tube insertion in patients undergoing resection of head and neck cancers. J Plast Reconstr Aesthet Surg. 2012;65:610–615. doi: 10.1016/j.bjps.2011.11.018. [DOI] [PubMed] [Google Scholar]
- 130.Kramer S, Newcomb M, Hessler J, Siddiqui F. Prophylactic versus reactive PEG tube placement in head and neck cancer. Otolaryngol Head Neck Surg. 2014;150:407–412. doi: 10.1177/0194599813517081. [DOI] [PubMed] [Google Scholar]
- 131.Wright GP, Foster SM, Chung MH. Esophagectomy in patients with prior percutaneous endoscopic gastrostomy tube placement. Am J Surg. 2014;207:361–5; discussion 364. doi: 10.1016/j.amjsurg.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 132.Grilo A, Santos CA, Fonseca J. Percutaneous endoscopic gastrostomy for nutritional palliation of upper esophageal cancer unsuitable for esophageal stenting. Arq Gastroenterol. 2012;49:227–231. doi: 10.1590/s0004-28032012000300012. [DOI] [PubMed] [Google Scholar]
- 133.Volkmer K, Meyer T, Sailer M, Fein M. [Metastasis of an esophageal carcinoma at a PEG site--case report and review of the literature] Zentralbl Chir. 2009;134:481–485. doi: 10.1055/s-0028-1098769. [DOI] [PubMed] [Google Scholar]
- 134.Saeed SM, Fontaine JP, Dam AN, Hoffe SE, Cameron M, Frakes J, Mehta R, Gurd E, Pimiento JM. Is Preoperative G-Tube Use Safe for Esophageal Cancer Patients? J Am Coll Nutr. 2020;39:301–306. doi: 10.1080/07315724.2019.1646168. [DOI] [PubMed] [Google Scholar]
- 135.Mahawongkajit P, Techagumpuch A, Limpavitayaporn P, Kanlerd A, Sriussadaporn E, Juntong J, Tongyoo A, Mingmalairak C. Comparison of Introducer Percutaneous Endoscopic Gastrostomy with Open Gastrostomy in Advanced Esophageal Cancer Patients. Dysphagia. 2020;35:117–120. doi: 10.1007/s00455-019-10017-w. [DOI] [PubMed] [Google Scholar]
- 136.Song JH, Ko J, Min YW, Kim K, Lee H, Min BH, Lee JH, Rhee PL, Kim JJ. Comparison between Percutaneous Gastrostomy and Self-Expandable Metal Stent Insertion for the Treatment of Malignant Esophageal Obstruction, after Propensity Score Matching. Nutrients. 2020;12 doi: 10.3390/nu12092756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Allen K, Hoffman L. Enteral Nutrition in the Mechanically Ventilated Patient. Nutr Clin Pract. 2019;34:540–557. doi: 10.1002/ncp.10242. [DOI] [PubMed] [Google Scholar]
- 138.Altintas ND, Aydin K, Türkoğlu MA, Abbasoğlu O, Topeli A. Effect of enteral versus parenteral nutrition on outcome of medical patients requiring mechanical ventilation. Nutr Clin Pract. 2011;26:322–329. doi: 10.1177/0884533611405790. [DOI] [PubMed] [Google Scholar]
- 139.Seron-Arbeloa C, Zamora-Elson M, Labarta-Monzon L, Mallor-Bonet T. Enteral nutrition in critical care. J Clin Med Res. 2013;5:1–11. doi: 10.4021/jocmr1210w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Artinian V, Krayem H, DiGiovine B. Effects of early enteral feeding on the outcome of critically ill mechanically ventilated medical patients. Chest. 2006;129:960–967. doi: 10.1378/chest.129.4.960. [DOI] [PubMed] [Google Scholar]
- 141.Grant JP. Nutrition care of patients with acute and chronic respiratory failure. Nutr Clin Pract. 1994;9:11–17. doi: 10.1177/011542659400900111. [DOI] [PubMed] [Google Scholar]
- 142.Farina N, Nordbeck S, Montgomery M, Cordwin L, Blair F, Cherry-Bukowiec J, Kraft MD, Pleva MR, Raymond E. Early Enteral Nutrition in Mechanically Ventilated Patients With COVID-19 Infection. Nutr Clin Pract. 2021;36:440–448. doi: 10.1002/ncp.10629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Goyal H, Perisetti A, Tharian B. Percutaneous Endoscopic Gastrostomy tube placement in COVID-19 patients: Multidisciplinary approach. Dig Endosc. 2021;33:209. doi: 10.1111/den.13873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Oberg CL, Keyes C, Panchabhai TS, Sajawal Ali M, Oh SS, Grogan TR, Mojica J, Auchincloss H, Pulido N, Brait K, Folch EE. Combined Percutaneous Tracheostomy and Endoscopic Gastrostomy Tubes in COVID-19: A Prospective Series of Patient Outcomes. J Intensive Care Med. 2021;36:1340–1346. doi: 10.1177/08850666211038875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Volkert D, Berner YN, Berry E, Cederholm T, Coti Bertrand P, Milne A, Palmblad J, Schneider S, Sobotka L, Stanga Z DGEM (German Society for Nutritional Medicine), Lenzen-Grossimlinghaus R, Krys U, Pirlich M, Herbst B, Schütz T, Schröer W, Weinrebe W, Ockenga J, Lochs H; ESPEN (European Society for Parenteral and Enteral Nutrition) ESPEN Guidelines on Enteral Nutrition: Geriatrics. Clin Nutr. 2006;25:330–360. doi: 10.1016/j.clnu.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 146.Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, Khatri P, McMullan PW Jr, Qureshi AI, Rosenfield K, Scott PA, Summers DR, Wang DZ, Wintermark M, Yonas H American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 147.Wirth R, Smoliner C, Jäger M, Warnecke T, Leischker AH, Dziewas R DGEM Steering Committee*. Guideline clinical nutrition in patients with stroke. Exp Transl Stroke Med. 2013;5:14. doi: 10.1186/2040-7378-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Kim DS, Jones RN, Shireman TI, Kluger BM, Friedman JH, Akbar U. Trends and outcomes associated with gastrostomy tube placement in common neurodegenerative disorders. Clin Park Relat Disord. 2021;4:100088. doi: 10.1016/j.prdoa.2020.100088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Lex KM, Kundt FS, Lorenzl S. Using tube feeding and levodopa-carbidopa intestinal gel application in advanced Parkinson's disease. Br J Nurs. 2018;27:259–262. doi: 10.12968/bjon.2018.27.5.259. [DOI] [PubMed] [Google Scholar]
- 150.Ishibashi Y, Shimo Y, Yube Y, Oka S, Egawa H, Kohira Y, Kaji S, Kanda S, Oyama G, Hatano T, Hattori N, Fukunaga T. Technique and outcome of percutaneous endoscopic transgastric jejunostomy for continuous infusion of levodopa-carbidopa intestinal gel for treatment of Parkinson's disease. Scand J Gastroenterol. 2019;54:787–792. doi: 10.1080/00365521.2019.1619830. [DOI] [PubMed] [Google Scholar]
- 151.Epstein M, Johnson DA, Hawes R, Schmulewitz N, Vanagunas AD, Gossen ER, Robieson WZ, Eaton S, Dubow J, Chatamra K, Benesh J. Long-Term PEG-J Tube Safety in Patients With Advanced Parkinson's Disease. Clin Transl Gastroenterol. 2016;7:e159. doi: 10.1038/ctg.2016.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Katzberg HD, Benatar M. Enteral tube feeding for amyotrophic lateral sclerosis/motor neuron disease. Cochrane Database Syst Rev. 2011:CD004030. doi: 10.1002/14651858.CD004030.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Grandidge L, Chotiyarnwong C, White S, Denning J, Nair KPS. Survival following the placement of gastrostomy tube in patients with multiple sclerosis. Mult Scler J Exp Transl Clin. 2020;6:2055217319900907. doi: 10.1177/2055217319900907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Civan HA, Bektas G, Dogan AE, Ozdener F. Percutaneous Endoscopic Gastrostomy Feeding in Children with Cerebral Palsy. Neuropediatrics. 2021;52:326–332. doi: 10.1055/s-0041-1731007. [DOI] [PubMed] [Google Scholar]
- 155.Akkersdijk WL, Roukema JA, van der Werken C. Percutaneous endoscopic gastrostomy for patients with severe cerebral injury. Injury. 1998;29:11–14. doi: 10.1016/s0020-1383(97)00108-3. [DOI] [PubMed] [Google Scholar]
- 156.Godil A, Chen YK. Percutaneous endoscopic gastrostomy for nutrition support in pregnancy associated with hyperemesis gravidarum and anorexia nervosa. JPEN J Parenter Enteral Nutr. 1998;22:238–241. doi: 10.1177/0148607198022004238. [DOI] [PubMed] [Google Scholar]
- 157.Irving PM, Howell RJ, Shidrawi RG. Percutaneous endoscopic gastrostomy with a jejunal port for severe hyperemesis gravidarum. Eur J Gastroenterol Hepatol. 2004;16:937–939. doi: 10.1097/00042737-200409000-00021. [DOI] [PubMed] [Google Scholar]
- 158.Serrano P, Velloso A, García-Luna PP, Pereira JL, Fernádez Z, Ductor MJ, Castro D, Tejero J, Fraile J, Romero H. Enteral nutrition by percutaneous endoscopic gastrojejunostomy in severe hyperemesis gravidarum: a report of two cases. Clin Nutr. 1998;17:135–139. doi: 10.1016/s0261-5614(98)80008-3. [DOI] [PubMed] [Google Scholar]
- 159.Senadhi V, Chaudhary J, Dutta S. Percutaneous endoscopic gastrostomy placement during pregnancy in the critical care setting. Endoscopy. 2010;42 Suppl 2:E358–E359. doi: 10.1055/s-0030-1256052. [DOI] [PubMed] [Google Scholar]
- 160.Wood MF, Sapala JA, Sapala MA, Schuhknecht MP, Flake TM. Micropouch gastric bypass: indications for gastrostomy tube placement in the bypassed stomach. Obes Surg. 2000;10:413–419. doi: 10.1381/096089200321594273. [DOI] [PubMed] [Google Scholar]
- 161.Nosher JL, Bodner LJ, Girgis WS, Brolin R, Siegel RL, Gribbin C. Percutaneous gastrostomy for treating dilatation of the bypassed stomach after bariatric surgery for morbid obesity. AJR Am J Roentgenol. 2004;183:1431–1435. doi: 10.2214/ajr.183.5.1831431. [DOI] [PubMed] [Google Scholar]
- 162.Baltz JG, Argo CK, Al-Osaimi AM, Northup PG. Mortality after percutaneous endoscopic gastrostomy in patients with cirrhosis: a case series. Gastrointest Endosc. 2010;72:1072–1075. doi: 10.1016/j.gie.2010.06.043. [DOI] [PubMed] [Google Scholar]
- 163.Shah I, Bhurwal A, Mehta H, Maas D, Koneru G, Cohen AS, Kadkhodayan KS. Trends and outcomes of percutaneous endoscopic gastrostomy in hospitalized patients with malignant and nonmalignant ascites: a nationwide population study. Ann Gastroenterol. 2020;33:656–660. doi: 10.20524/aog.2020.0531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Wilmskoetter J, Simpson KN, Bonilha HS. Hospital Readmissions of Stroke Patients with Percutaneous Endoscopic Gastrostomy Feeding Tubes. J Stroke Cerebrovasc Dis. 2016;25:2535–2542. doi: 10.1016/j.jstrokecerebrovasdis.2016.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Geeganage C, Beavan J, Ellender S, Bath PM. Interventions for dysphagia and nutritional support in acute and subacute stroke. Cochrane Database Syst Rev. 2012;10:CD000323. doi: 10.1002/14651858.CD000323.pub2. [DOI] [PubMed] [Google Scholar]
- 166.Joundi RA, Saposnik G, Martino R, Fang J, Porter J, Kapral MK. Outcomes among patients with direct enteral vs nasogastric tube placement after acute stroke. Neurology. 2018;90:e544–e552. doi: 10.1212/WNL.0000000000004962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gauvin G, Do-Nguyen CC, Lou J, O'Halloran EA, Selesner LT, Handorf E, Collins ME, Farma JM. Gastrostomy Tube for Nutrition and Malignant Bowel Obstruction in Patients With Cancer. J Natl Compr Canc Netw. 2021;19:48–56. doi: 10.6004/jnccn.2020.7604. [DOI] [PubMed] [Google Scholar]
- 168.McCann RM, Hall WJ, Groth-Juncker A. Comfort care for terminally ill patients. The appropriate use of nutrition and hydration. JAMA. 1994;272:1263–1266. doi: 10.1001/jama.272.16.1263. [DOI] [PubMed] [Google Scholar]
- 169.Oterdoom LH, Marinus Oterdoom DL, Ket JCF, van Dijk JMC, Scholten P. Systematic review of ventricular peritoneal shunt and percutaneous endoscopic gastrostomy: a safe combination. J Neurosurg. 2017;127:899–904. doi: 10.3171/2016.8.JNS152701. [DOI] [PubMed] [Google Scholar]
- 170.Kim JS, Park YW, Kim HK, Cho YS, Kim SS, Youn NR, Chae HS. Is percutaneous endoscopic gastrostomy tube placement safe in patients with ventriculoperitoneal shunts? World J Gastroenterol. 2009;15:3148–3152. doi: 10.3748/wjg.15.3148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Gieniusz M, Sinvani L, Kozikowski A, Patel V, Nouryan C, Williams MS, Kohn N, Pekmezaris R, Wolf-Klein G. Percutaneous Feeding Tubes in Individuals with Advanced Dementia: Are Physicians "Choosing Wisely"? J Am Geriatr Soc. 2018;66:64–69. doi: 10.1111/jgs.15125. [DOI] [PubMed] [Google Scholar]
- 172.Finucane TE, Christmas C, Travis K. Tube feeding in patients with advanced dementia: a review of the evidence. JAMA. 1999;282:1365–1370. doi: 10.1001/jama.282.14.1365. [DOI] [PubMed] [Google Scholar]
- 173.Teno JM, Gozalo P, Mitchell SL, Kuo S, Fulton AT, Mor V. Feeding tubes and the prevention or healing of pressure ulcers. Arch Intern Med. 2012;172:697–701. doi: 10.1001/archinternmed.2012.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Higaki F, Yokota O, Ohishi M. Factors predictive of survival after percutaneous endoscopic gastrostomy in the elderly: is dementia really a risk factor? Am J Gastroenterol. 2008;103:1011–6; quiz 1017. doi: 10.1111/j.1572-0241.2007.01719.x. [DOI] [PubMed] [Google Scholar]
- 175.Finucane TE, Bynum JP. Use of tube feeding to prevent aspiration pneumonia. Lancet. 1996;348:1421–1424. doi: 10.1016/S0140-6736(96)03369-7. [DOI] [PubMed] [Google Scholar]
- 176.Murphy LM, Lipman TO. Percutaneous endoscopic gastrostomy does not prolong survival in patients with dementia. Arch Intern Med. 2003;163:1351–1353. doi: 10.1001/archinte.163.11.1351. [DOI] [PubMed] [Google Scholar]
- 177.Nakanishi M, Hattori K. Percutaneous endoscopic gastrostomy (PEG) tubes are placed in elderly adults in Japan with advanced dementia regardless of expectation of improvement in quality of life. J Nutr Health Aging. 2014;18:503–509. doi: 10.1007/s12603-014-0011-9. [DOI] [PubMed] [Google Scholar]
- 178.Ayman AR, Khoury T, Cohen J, Chen S, Yaari S, Daher S, Benson AA, Mizrahi M. PEG Insertion in Patients With Dementia Does Not Improve Nutritional Status and Has Worse Outcomes as Compared With PEG Insertion for Other Indications. J Clin Gastroenterol. 2017;51:417–420. doi: 10.1097/MCG.0000000000000624. [DOI] [PubMed] [Google Scholar]
- 179.van Bruchem-Visser RL, Mattace-Raso FUS, de Beaufort ID, Kuipers EJ. Percutaneous endoscopic gastrostomy in older patients with and without dementia: Survival and ethical considerations. J Gastroenterol Hepatol. 2019;34:736–741. doi: 10.1111/jgh.14573. [DOI] [PubMed] [Google Scholar]


