Abstract
Pre-exposure prophylaxis (PrEP) is highly effective in preventing new HIV infection, but uptake remains challenging among Black and Hispanic/Latino persons. The purpose of this review was to understand how studies have used electronic telecommunication technology to increase awareness, uptake, adherence, and persistence in PrEP care among Black and Hispanic/Latino persons and how it can reduce social and structural barriers that contribute to disparities in HIV infection. Of the 1114 articles identified, 10 studies were eligible. Forty percent (40%) of studies focused on Black or Hispanic/Latino persons and 80% addressed social and structural barriers related to PrEP use such as navigation or access to PrEP. Mobile health designs were more commonly used (50%) compared to telehealth (30%) and e-health (20%) designs. There is a need to increase the development of telecommunications interventions that address the needs of Black and Hispanic/Latino persons often challenged with uptake and adherent use of PrEP.
Keywords: PrEP, HIV, Disparities, mHealth, Telehealth
Introduction
A crucial need exists for reducing new HIV infections among Black or African American (hereafter referred to as Black) and Hispanic/Latino persons in the United States (U.S.), who accounted for 41% and 29% of new HIV diagnoses in 2019, respectively [1]. Antiretroviral pre-exposure prophylaxis (PrEP) is a key element of the Ending the HIV Epidemic in the U.S. initiative effort to prevent new HIV infections [2]. PrEP is highly effective when taken as prescribed [3], but uptake and adherent use among Black and Hispanic/Latino persons with indications for PrEP use remain a challenge [4]. In addition, social and structural barriers (e.g., out-of-pocket cost of PrEP medication and clinical care, access and proximity to healthcare providers, transportation to distal PrEP delivery sites, lack of support from family/friends, stigma related to taking PrEP medication) affecting some Black and Hispanic/Latino populations contribute to the reduced use [5, 6]. Overcoming the many challenges that decrease the uptake, adherent use and persistence in PrEP care is needed to reduce new infections in this population.
Electronic telecommunication technology uses interactive websites, mobile apps, telephones, and videoconferencing, as alternative ways of educating and providing health information and care to clients. Use of these technologies (e.g., eHealth, mHealth, telehealth) in the delivery of HIV treatment services throughout the continuum of care has increased in recent years because of their potential effectiveness in outreach, ease of use, and cost savings [7]. The use of telecommunication technology also has the potential to facilitate patient awareness and education about PrEP and support medication adherence and persistence in PrEP care. Prior to the COVID-19 pandemic, the use of telehealth in HIV care was less common [8]. However, recent use of these practices in HIV services has proved promising in improving and ensuring the consistent delivery of healthcare, especially among Black and Hispanic/Latino persons [9].
Using telecommunication technology in the stages of PrEP patient awareness and use can also help reduce barriers and challenges to accessing these services. For example, telehealth may reduce privacy concerns and anticipated stigma (e.g., being seen in a clinic waiting room), a concern reported by some patients when accessing healthcare providers for PrEP in-person [10–12]. Additionally, telehealth alleviates the need for transportation to meet providers in-person by providing patients with streamlined and remote access to health navigators, providers, and required laboratory testing.
Some earlier research suggested that Black and Hispanic/Latino persons who experience challenges accessing PrEP due to social and structural barriers could most benefit from the use of these technologies [13]. On the other hand, use of such technology may have its own barriers and challenges (e.g., lack of access to reliable Internet or required bandwidth, lack of access to computers, cell phones, or smartphones needed to access these services) [14]. To understand how this technology may or may not reduce disparities, we conducted a systematic review of published literature to assess how telecommunication technology is being used to increase awareness, uptake, adherence, and persistence in PrEP care among Black and Hispanic/Latino persons. We also sought to understand whether use of this technology can reduce social and structural barriers that often prevent or delay the use of PrEP and contribute to disparities in HIV infection.
Methods
Study Selection
We conducted a systematic literature review search of studies published between January 1, 2015 and December 31, 2020 using the following databases: PubMed, EMBASE, Cochrane Library, CINAHL (EbscoHost), and Scopus. Studies were identified using varying combinations of keywords: telemedicine, telehealth, mHealth, eHealth, text messages, mobile app, social media, HIV, PrEP, chemoprevention, chemoprophylaxis, iPREX, Truvada, Descovy, tenofovir, or emtricitabine.
All study citations identified were exported to Endnote and the article citations were deduplicated. We then exported the studies to a spreadsheet and reviewed all titles and abstracts for inclusion criteria. Study titles had to: (1) contain PrEP or HIV and telehealth, telemedicine, mobile health, text messaging, or social media (or known variations/acronyms), AND (2) enroll participants for an intervention study, AND (3) use telecommunication technology modalities (e.g., live videoconferencing, cell phone, text message) to deliver the study intervention. The primary outcome had to focus on at least one of the following in the stages of PrEP use (1) increasing patient awareness of PrEP (i.e., education), OR (2) uptake of PrEP (i.e., study participant linked or prescribed), OR (3) adherence to PrEP (i.e., taking PrEP as prescribed daily or near daily), OR (4) persistence (i.e., retention) in PrEP care (i.e., prescribed and taking PrEP for a certain amount of months/years). Both qualitative and quantitative studies were included. Studies not written in English, review articles, clinical trials, modeling studies, conference abstracts, not containing published data (i.e., commentary, news articles) or not conducted in the U.S. were excluded.
Data Abstraction and Analysis
Three coders (K.E., R.H., and A.T.) reviewed and abstracted key data. All articles had two reviewers assigned and each reviewer abstracted information related to the following measures: PrEP outcomes (i.e., patient awareness, uptake, adherence, persistence); rural or urban study location as defined by the U.S. Census Bureau [15]; study modality used as an intervention (e.g., live videoconferencing, phone calls, text messaging, or Internet/intranet sites); sample size; race/ethnicities (i.e., Black/African American persons, Hispanic/Latino persons) enrolled; sex/gender identity (i.e., cisgender women, transgender women, cisgender men); HIV transmission risk group (i.e., men who have sex with men [MSM], persons who inject drugs [PWID], Heterosexual), age group (i.e., youth, young adults, all age groups, or only adults); and social and structural factors that contribute to PrEP related disparities (e.g., PrEP care out-of-pocket costs, health care access, PrEP-related stigma, transportation, insurance status and type, provider unawareness of PrEP or unwillingness to prescribe, and anticipated or experienced family/partner/friend objection). We further classified studies as eHealth (e.g., use of e-videos), mHealth (e.g., use of mobile or smart-phones), or telehealth (e.g., use of telephone or videoconferencing with prescribing providers) based on the primary study design.
Any discrepancies were either reconciled by the lead coder or discussed as a study team for final determination. Findings from secondary analysis studies were included in the summaries; however, the primary study and any resulting secondary analyses counted as one study. Additional studies identified through the references list in accepted articles and met inclusion criteria were allowed into the study, as per established systematic reviews methodology [16].
Results
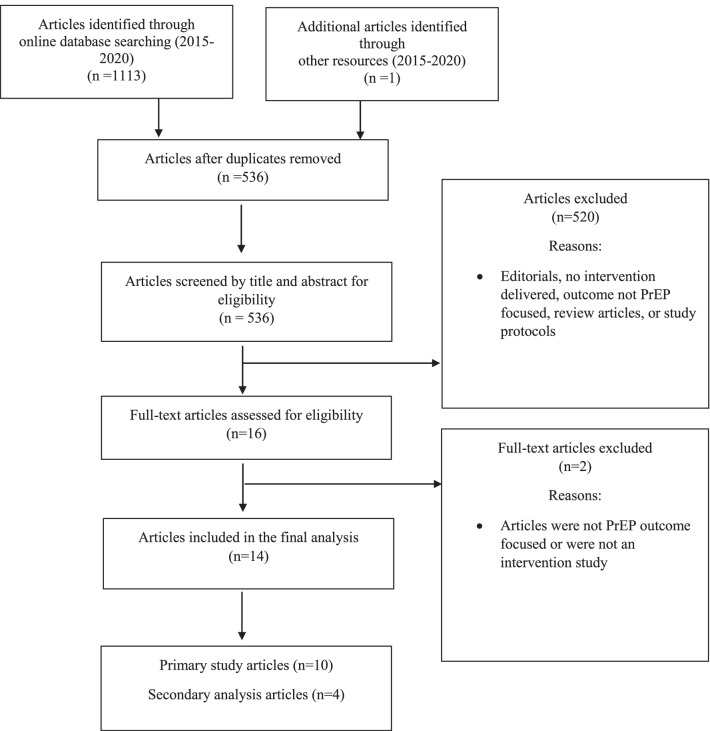
A total of 10 studies met inclusion criteria (Fig. 1). Results from each primary study are summarized in Table 1 [17–31]. Findings from four additional secondary analyses of the Moore et al. primary study [17, 18, 22, 27, 28] are summarized in Table 1. Two studies [19, 20] (20%) used e-health platforms and focused on patient awareness and acceptability of PrEP, three studies [23, 29, 31] (30%) used telehealth and focused on uptake, adherence and persistence in PrEP, and five studies [21, 24–27] (50%) were mHealth primarily focused on adherence to PrEP. Across all technologies, two studies [19, 20] (20%) focused on patient PrEP awareness/acceptability, three studies [23, 29, 31] (30%) focused on PrEP uptake, seven studies [21, 24–27, 29, 31] (70%) focused on adherence to PrEP, and two studies [23, 24] (20%) focused on persistence in PrEP. Seven studies [20, 21, 24, 25, 27, 29, 31] (70%) were in large urban population settings and one study [23] (10%) focused on rural populations, although small urban area residents also participated. Only four studies [19, 20, 24, 25] (40%) had a population of at least 50% or more of Black and/or Hispanic/Latino participants. Seven studies [21, 24–27, 29, 31] (70%) addressed only MSM and eight studies [19, 20, 23–25, 29, 31] (80%) included social and structural barriers by either collecting data on, or intervening to reduce identified barriers (e.g., providing access or navigation to PrEP, access to technology).
Fig. 1.
Selection of study articles for systematic review: telecommunication technology interventional studies focusing on PrEP awareness, uptake, adherence, and persistence in care
Table 1.
Summary of findings: interventional U.S. studies using technology to increase PrEP awareness, uptake, adherence, and persistence in care
| Primary study modality | First author and publication year | Study focus: patient awareness/acceptability, uptake, adherence, or persistence in PrEP | Study population location/ geographic location of study: urban or rural | Study sample size and race/ethnicities (e.g., Black/African American, Hispanic/Latino) enrolled | Sex/gender identity/sexual orientation—cisgender women, cisgender men, transgender women | HIV transmission risk factor/risky behavior targeted (i.e., MSM, PWID, Heterosexual) | Age group—youth, young adults, only adults, all age groups, | Social and structural barriers discussed or addressed during study | Summary of study/findings |
|---|---|---|---|---|---|---|---|---|---|
| E-Health Platform | Bond et al. (2016) [19] | Patient Awareness/Acceptability of PrEP | Unknown |
N = 119 Black/African American = 119 (100%) |
Female | Heterosexual | Adults: ≥ 18 years | Stigma; burden of use; long-term use | Study used pre-recorded e-health videos to deliver the intervention. Found 53.9% of women perceived only advantages to using PrEP; 16.4% reported both advantages and disadvantages to using PrEP; 18.7% reported only disadvantages to using PrEP |
| Chandler et al. (2020) [20] | Patient Awareness/Acceptability of PrEP | Urban |
N = 43 Black/African American = 43 (100%) |
Cisgender Women, Bisexual female | Heterosexual | Young Adults: 18–24 years old | PrEP cost; insurance status and type; provider unawareness or unwillingness to prescribe PrEP | Investigators used an e-learning online platform vs. in-person comparison group to deliver the intervention. Among Black women in college, 67% were unaware of PrEP and 72% were apprehensive about initiating PrEP. Results post-intervention found the in-person group had higher scores in learning about PrEP and were likely to use PrEP in the future (72.0%) compared to the online group (62.6%) | |
| Telehealth | Hoth et al. (2019) [23] | Uptake of PrEP, Persistence in PrEP care |
Urban Rural |
N = 127 White = 103 (81%); Black = 9 (7%); Hispanic/Latinx = 7 (6%); Asian = 2 (3%); Multiracial = 2 (2%); Native American = 1 (1%) |
Cisgender Men, Cisgender Women, Gender Fluid/nonbinary | MSM; Heterosexual | Adults: ≥ 18 years | Insurance status and type; PrEP cost | Investigators used live videoconferencing with physicians to prescribe PrEP. Of the 127 participants who completed an initial visit, 91% started PrEP within 7 days. The median number of follow-up days after starting PrEP was 214 days (range 3–609 days). Among participants starting PrEP, retention was 60% at 180 days |
| Refugio et al. (2019) [29] | Uptake of PrEP; Adherence of PrEP | Urban |
N = 25 Hispanic = 10 (40%); Asian = 8 (32%); White = 4 (16%); Black = 2 (8%); Middle Eastern = 1 (4%) |
Cisgender Men | MSM | Young Adults: 18–25 years and older | Access to PrEP home-delivered; transportation; stigma; privacy; health care access to providers; insurance status and type; provider unawares or wiliness to prescribe | Intervention used telehealth visits via telephone to prescribe PrEP. The median time to PrEP initiation was 46 days. Majority of participants (≥ 85%) agreed that PrEPTECH is a better way to receive PrEP at 90 and 180 days. 100% of participants reported that PrEPTECH was very or extremely fast and convenient compared with other forms of getting on PrEP and would continue to use PrEPTECH even if the services were not free | |
| Stekler et al. (2018) [31] | Uptake of PrEP, Adherence to PrEP | Urban |
N = 48 White = 18 (37.5%); Asian = 4 (8.3%); Hispanic = 14 (29.2%); Black = 3 (6.3%); Other/multiracial = 9 (18.7) |
Cisgender Men, Transgender Women | MSM | Not specified: 19–46 years old enrolled | Insurance status and type; access to technology; PrEP cost | Intervention used live videoconferencing with a provider to improve PrEP uptake and adherence. Compared with standard-of-care group participants, there were no significant differences in proportions of telehealth participants prescribed PrEP (70% vs. 79%), who attended the first follow-up visit (83% vs. 85%), or adherence at 1-month | |
| mHealth | Fuchs et al. (2018) [21] | Adherence to PrEP | Urban |
N = 56 Hispanic = 6 (10.7%); White = 38 (67.9%), Black = 7 (12.5%); Other = 5 (8.9%) |
Cisgender men | MSM | Not specified: age summarized as ≤ 30 years old or > 30 years old | No | Intervention used a smartphone mobile app. Mean number of days when medication was not taken was reduced by 50% (95% CI 16–71; p = 0.008), and when comparing missed doses to specific visits before and after iText intervention, the proportion of missed doses was reduced by 77% (95% CI 33–92; p = 0.007) |
| Liu et al. (2018) [24] | Adherence to PrEP; Persistence in PrEP | Urban |
N = 121 Hispanic/Latino = 43 (36%); Black = 33, (27%;); White = 30 (25%); Asian = 8 (7%); Other = 5 (4%) |
Cisgender men, transgender women | MSM | Young adults: 18–29 years old | Access to PrEP | Intervention was delivered with a smartphone mobile app via text messages. Participants who received PrEPmate were more likely to have PrEP levels consistent with ≥ 4 doses/week (72% PrEPmate vs. 57% standard-of-care, SOC) (OR 2.05, 95% CI 1.06–3.94, p = 0.03). For retention, greater percentage of visits were completed by PrEPmate (86%) vs. SOC participants (71%) (OR 2.62; 95% CI 1.24–5.54, p = 0.01) | |
| Liu et al. (2020) [25] | Adherence to PrEP | Urban |
N = 20 Black = 15 (75%) Latino = 5 (25%) |
Cisgender Men | MSM | Young Adults: 18–35 years old | Access to PrEP during study and access/navigation to PrEP after study | Use of the directly observed therapy (DOT) app and diary was high, with median PrEP adherence of 91%. Most (84%) participants reported the app helped with PrEP adherence | |
| Mitchell et al. (2018) [26] | Adherence to PrEP | Unknown |
N = 10 White = 7 (70%); Asian = 2 (20%); Multiracial = 1 (10%) |
Cisgender Men | MSM | Young adults: 18–30 years old | PrEP cost; family/partner/friend objection; health care access to providers | PrEP adherence increased 30% for participants who used the mobile app. For participants who did not indicate any change, PrEP adherence scores were already at a level considered efficacious (i.e., ≥ 4 doses per week) at baseline. 30% reported a decrease in barriers. Participants self-reported mean PrEP adherence rates of 91% through daily entries in the mSMART app | |
| Moore et al. (2017) [27] | Adherence to PrEP | Urban |
N = 398 Asian = 12 (6.2%); Black = 52 (13.1%); White = 295 (74.1%); Multiple = 24 (6.0%); Other = 7 (1.8%) Hispanic Ethnicity = 119 (29.9%) |
Cisgender men, transgender women | MSM | Adults: ≥ 18 years | No |
The text messaging intervention did not significantly improve adequate adherence (≥ 719 fmol/punch) compared to the SOC (72.0% vs 69.2%; p = 0.58), but did improve near-perfect adherence (≥ 1246 fmol/ punch) a secondary outcome, through week 48 (33.5% vs 24.8%, p = 0.06) Secondary analysis studies • Blumenthal et al. (2019) [17]—Analysis found the correlation between self-report measures of adherence were significant associated with quantifiable biomarker collected • Blumenthal et al. (2019) [18]—Study calculated modified calculated risk scores to estimate likelihood of HIV seroconversion based on self -reported risk behaviors. Analysis found participants with moderate or high-risk behaviors had higher PrEP adherence levels compared to lower risk groups • Hoenigl et al. (2018) [22]—No statistical difference was found in PrEP adherence among substance users compared to non substance users • Pasipanodya et al. (2018) [28]—growth mixture modeling to identify 4 trajectories of text-reported adherence. Classes with higher reported adherence had higher drug concentrations. Younger age and minority race were associated with lower adherence. Participants reported adherence on 85.10% of days. Greater adherence responses were associated with a higher PrEP concentration (ρ = 0.36; p < 0.001) |
E-Health Studies
Two studies (20%) used e-health technology to increase the awareness and acceptability of PrEP among Black women. In the Bond & Gunn study [19], Black women (n = 119) watched an online e-video about PrEP and post-exposure prophylaxis (PEP). Afterwards, 53.9% of women perceived only advantages to using PrEP and 18.7% of women reported only disadvantages to using PrEP. Through qualitative methods, women found using PrEP as empowering, a self-controlled prevention method, and providing an option when engaging with risky sex partners. However, perceived social and structural barriers contributing to fears of initiating PrEP were stigma (i.e., taking medication to prevent HIV), burden of use (i.e., taking PrEP daily, in addition to, birth control and using condoms), out of pocket PrEP cost associated with long-term use, and medical mistrust.
In the Chandler et al. study [20], an educational intervention was delivered either through an online platform or in-person among Black college women (n = 43) residing in Atlanta, Georgia. Participants were randomized to one of the delivery modalities (in-person or online) and at baseline there were no statistically significant differences between the two groups. The educational intervention included topics on PrEP knowledge, PrEP dosing and side effects, and PrEP empowerment (e.g., how to initiate a conversation with a healthcare provider about initiating PrEP). Participants who met in-person for the intervention were 70.0% more likely to use PrEP in the future compared with 62.6% who participated in the intervention online. Investigators assessed barriers to using PrEP through semi-structured focus groups. Perceived cost of PrEP medication, burden of use (i.e., already taking enough pills, inconvenience), and concern about its use promoting sexual risk behaviors were the primary barriers raised among participants; however, 67.4% of participants felt the intervention was very helpful in learning about PrEP (85.0% among in-person group vs. 52.2% in online group, p = 0.03).
Telehealth Studies
Three studies (30%) used telehealth to attempt to increase the uptake, adherence, and persistence in PrEP care. The Hoth et al. study [23] focused on increasing PrEP uptake among majority White (81%), 18 years and older participants (n = 127) in 16 rural counties and five small urban communities. This was the only study identified which addressed rural populations. Live videoconferencing at the participant home or a private setting occurred with physicians who prescribed PrEP. Of the 127 participants, the majority (91%) of participants started PrEP within seven days and retention was 60% at 180 days. The investigators addressed social and structural factors by providing navigation to PrEP medication assistance programs and health insurance, and mailing PrEP through participating pharmacies.
Refugio et al. [29] study focused on uptake of and adherence to PrEP among MSM, 18–25 years old residing in the urban San Francisco Bay area. Enrolled participants (n = 25) were Hispanic (40%), Asian (32%) and Black (8%) persons. PrEPTECH was a pilot intervention that used telehealth to initiate and promote PrEP adherence. Telehealth visits were conducted through the telephone at various intervals until the end of the study period. Most participants (≥ 85%) reported that PrEPTECH was a better way to receive PrEP for long term use (i.e., 90 and 180 days) than by in-person clinic visits. The investigators addressed social and structural barriers by providing free, home delivered PrEP and navigated participants to sustainable PrEP providers after study completion to ensure participants had access to providers willing to prescribe PrEP. In addition, the investigators collected cross-sectional data about PrEPTECH related to confidentiality, convenience, and stigma to better address these barriers.
Lastly, the Stekler et al. [31] study focused on increasing uptake and adherence to PrEP among majority White (37.5%) and Hispanic/Latino (29.2%) MSM (n = 48) residing in urban Seattle area. Patients were seen by providers through live videoconferencing when providers were unavailable in-person (i.e., telehealth patients); the comparison was to standard of care visits with clinic physicians available in-person. No significant differences were found in the proportion of telehealth participants compared to the standard of care group who were prescribed PrEP (70% vs. 79%), who attended the first follow-up visit (83% vs. 85%), or with medication adherence at 1 month (median number of missed doses in the last month: 2 (interquartile range [IQR]: 2–2) vs. 1 (IQR 0–3). The clinic providers addressed social and structural barriers by providing navigation to PrEP and assistance with insurance or medication assistance registration.
m-Health Studies
Five studies (50%) used m-health technology to increase adherence to PrEP. Fuchs et al. study [21] focused on increasing adherence to PrEP among majority White (67.9%) MSM (n = 56) residing in urban San Francisco and Chicago areas. A smartphone mobile app was used to deliver a text-messaging intervention (iText). The iText intervention was effective in reducing the mean number of days of missed doses of PrEP by 50% (95% Confidence Interval [CI] 16–71, p = 0.008), compared to pill counts prior to intervention enrollment. Investigators did not address or alleviate any structural or social barriers related to PrEP use or access during the study.
One study by Liu et al. [24] focused on medication adherence and persistence in PrEP care among majority Black (27%) and Hispanic (36%) MSM (n = 121), 18–29 years old residing in the urban Chicago area. The intervention used a smartphone mobile app called PrEPmate to send bidirectional text messages to participants. Participants who used PrEPmate were 72% more likely to have dried blood spot concentrations of tenofovir diphosphate ≥ 700 fmol/punch (i.e., ≥ 4 doses/week) compared with 57% in the standard of care group (OR 2.05, 95% CI 1.06–3.94, p = 0.03). For persistence in PrEP care, 86% of clinic visits were completed by PrEPmate participants compared to 71% among the standard of care participants (OR 2.62, 95% CI 1.24–5.54, p = 0.01). Study investigators also addressed social and structural barriers by providing free PrEP medication and care for 9 months.
A second study by Liu et al. [25] focused on adherence to PrEP among Black (75%) and Hispanic (25%) MSM (n = 20), 18–35 years old residing in urban San Francisco Bay and Atlanta metropolitan areas. The intervention used a mobile app and e-diary for directly observed therapy (DOT) of PrEP. Visual confirmation of PrEP adherence was captured by the mobile app and the median percentage of doses taken was 91%. Most (84%) participants self-reported that the app helped with PrEP adherence. The study investigators addressed social and structural barriers by providing free access to PrEP during the study and benefits/navigation to PrEP after the study, including an additional 3 months of free PrEP medication to reduce a gap in PrEP coverage until participants could be linked to PrEP providers.
Mitchell et al. [26] study focused on adherence to PrEP among mostly White (70%) young MSM (n = 10), 18–30 years old. Investigators used a mobile app to increase adherence to PrEP and found a 30% increase among participants, compared to their baseline measure. Self-reported mean PrEP adherence was 91% measured through daily entries into the app. The app also supported several adherence strategies to decrease barriers, including providing information about concerns with long term use and financial cost of PrEP, how to communicate with health care workers about PrEP, and how to elicit support from family and friends to support PrEP adherence. Participants who used the app reported a 30% decrease in barriers to PrEP.
Lastly, the Moore et al. [27] study focused on adherence to PrEP among mostly White (74%) adult MSM (n = 398) residing in urban Southern California areas. The text messaging intervention did not significantly improve adequate adherence measured by dried blood spot tenofovir diphosphate levels (≥ 719 fmol/punch, 4–6 doses per week) compared to the standard of care (72.0% vs. 69.2%, p = 0.58), but it did improve near-perfect adherence (≥ 1246 fmol/ punch; 7 doses per week) through week 48 after adjusting for age (33.5% vs 24.8%, p < 0.05). Findings from secondary analyses are also reported in Table 1. The study investigators did not address or alleviate any structural or social barriers related to PrEP use or access.
Discussion
Our systematic review identified 10 studies using telecommunication technology to intervene on patient PrEP awareness and acceptability, uptake, medication adherence, and persistence in PrEP care published between 2015 and 2020. Of the 10 studies, 40% focused on Black or Hispanic/Latino persons and 80% included designs to address social and structural barriers related to PrEP use. Mobile health designs were more commonly used (50%) compared to telehealth and e-health designs, especially when focused on adherence to PrEP.
Our study findings indicate that only four out of 10 (40%) of telecommunications studies prioritized the racial/ethnic populations at highest need, despite the estimated 43.7% of Black persons and 24.7% of Hispanics/Latino persons that have indications for PrEP use [32]. Reducing barriers challenging these populations is vital to ensure adequate access, medication adherence, and persistence in PrEP care to effectively reduce disparities in rates of new HIV infections. Even among MSM populations where PrEP uptake has been the greatest compared to other HIV transmission risk groups, uptake among Black and Hispanic/Latino persons compared to White persons is disproportionally lower [33]. Further intervention studies with telecommunication technology that purposely prioritize Black and Hispanic/Latino persons who could most benefit from HIV prevention through PrEP are urgently needed.
A secondary outcome in our review was to identify how telecommunication technology has addressed social and structural barriers that contribute to disparities in PrEP care among Black and Hispanic/Latino persons. Our study found that 80% of telecommunications intervention studies addressed one or more social and structural barriers often cited as barriers to initiating or adhering to PrEP. Stigma and access and navigation to PrEP were key barriers addressed by studies. Overall, some studies were effective in increasing knowledge or PrEP medication adherence. However, some studies such as the Stekler study [31], found no difference in PrEP uptake or adherence among those participating in telehealth compared to their standard of care patients. Patients who could not attend once weekly appointments when a provider was physically present (i.e., every Tuesday from 3 to 5 pm) utilized live videoconferencing at the clinic with providers (i.e., telehealth patients) on alternative days and times and were compared to standard of care patients who met with clinic providers in-person. All patients were still required to visit the clinic to access health providers (in-person or telehealth); thus, not alleviating potential structural barriers of patients who could have benefited from accessing their provider remotely from home and is possibly why no differences in PrEP uptake and adherence were found. Future development of studies using telehealth should consider how patients access providers and facilitate opportunities for patients to be seen remotely from their homes or private locations when feasible to effectively reduce time and distance barriers to accessing services and support persistence in PrEP care.
As HIV continues to disproportionately affect some populations, all groups with indications for PrEP use could benefit from telecommunication technology interventions when they are proven effective to reduce personal, social, and structural factors that are barriers to sustained, adherent PrEP use. Future mobile app and other e-health interventions could be developed and evaluated for their ability to increase patient education about PrEP use [34]; provide effective messages about how to engage in discussions with providers, family, and friends to elicit support; and provide information about how to access navigation services to obtain free or low-cost PrEP. While the use of technology offers many conveniences and has potential to reduce barriers to sustained PrEP use, some persons may benefit from in-person interaction and support offered by study staff. As in the Chandler et al. study [20], participants who met in-person found the intervention more helpful in learning about PrEP compared to those who participated online. Understanding the study population and their preference for engagement will be key to outcome success. The use of telecommunication technology may also present unanticipated barriers to PrEP access and use (e.g., persons lacking access to reliable Internet or required bandwidth, persons lacking access to computers, cell phones, or smartphones, persons lacking experience in operating the technology required) [14] contributing to a digital divide [35, 36] among persons who are already disproportionately affected by social determinants of health (SDOH). To reduce such disparities, interventions should consider incorporating trainings to increase digital literacy, providing access to smartphones or computer tables that can be utilized to facilitate PrEP use and adherence, and only using telecommunication technology when it offers more benefits than barriers for the prioritized population.
In our review, a few telehealth and mHealth studies reported improved PrEP uptake and adherence. Half of the studies (50%) focused on youth and young adults [20, 24–26, 29], with three of the studies using mHealth technology, specifically text messaging and mobile apps features as reminders for PrEP adherence and persistence in care. There is potential to increase the use of mHealth technology among Black and Hispanic/Latino youth and younger adults who are already most comfortable with the technology and frequently early adopters of new technology. However, only two of the five (40%) mHealth studies in our review focused on youth and enrolled Black and Hispanic/Latino persons. More efforts and strategies to enroll young, Black and Hispanic/Latino persons into e-Health, mHealth, and telehealth studies are needed and those proven effective could have substantial impact on reducing HIV disparities.
Of note, seven (70%) of the studies primarily focused on MSM populations. While two studies enrolled Black women identified as heterosexual to increase awareness of PrEP and three studies allowed persons identified as transgender women to enroll, more studies are needed that aim to increase uptake and adherence of PrEP among heterosexual and transgender women. Particularly, more studies are needed among Black heterosexual women and transgender women who experience increased risk for HIV infection [1, 37, 38]. Lastly, no study prioritized PWID despite overlapping injection and sexual risk for HIV transmission. Studies have shown PWID are aware and have interest in taking PrEP, but uptake and adherence remains challenging [39]; thus, there is a need to also prioritize this population for the evaluation of telecommunications and other interventions to increase uptake, adherence, and persistence in PrEP care.
Overall, the use of telecommunication technology to advance patients along the PrEP care continuum is promising. There are still important gaps that exist in our knowledge base about how to effectively use telecommunication technologies among populations who could most benefit, for sustainable impact on PrEP outcomes. Increasing access for rural populations who lack transportation and access to PrEP providers with telehealth technology could substantially increase uptake and sustained use of PrEP. Also, increasing the number of proven effective eHealth, mHealth, and telehealth interventions for Black and Hispanic/Latino persons, especially mHealth interventions among younger persons could also see real benefits. Lastly, increasing our knowledge of effective use of these technologies among PWID, transgender women, and heterosexual cisgender women, specifically in Black and Hispanic/Latino persons who experience increased risk for infection, is an urgent need.
Our study is not without limitations. First, peer-reviewed articles published after December 31, 2020 were not included. Second, we included one study identified outside of the systematic review process when reviewing abstracts although published during our study timeframe. It is possible other studies that were relevant and eligible were not included due to systematic error. Third, purely programmatic clinic and health department efforts (not research studies) and unpublished work are also not captured in this report. Fourth, only 10 published studies were included for this review and the study designs were heterogeneous, not all included a comparison group, and some were small and single-site, yielding results of limited generalizability. Thus, the effectiveness of study designs reporting increased PrEP adherence may not be generalizable beyond the study participants. Last, classifications of certain categories for this review are limited to the methods presented in each study, and thus we could not summarize all aspects for some studies, nor attempt to formally evaluate the strengths of methodology and evidence of the included studies [40].
This is the first review to examine the extent to which telecommunication technology (i.e., telehealth, eHealth, mHealth) interventions have prioritized the enrollment of Black and Hispanic/Latino populations most affected by HIV, and potentially how these technologies could reduce social and structural barriers contributing to disparities in PrEP awareness, uptake, adherence, and persistence in care. Telecommunications interventions can contribute to advancements in Ending the HIV Epidemic in the U.S. goals to reduce new HIV infections by 75% and increase PrEP prescriptions to at least 50% among those with indications for its use by 2025 [2]. This review calls to action the need for engaging more Black and Hispanic/Latino persons in telecommunication and other applied or implementation research to better address social and structural barriers that often challenge Black and Hispanic/Latino persons from engaging in and adhering to PrEP use.
Author Contributions
Conception and design: KNE, KB, DKS; Collection and assembly of data: KNE; Data analysis: KNE, RH, AT; Writing-original draft presentation: KNE. Writing- review and editing: KNE, RH, AT, KB, DKS.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data Availability
Not applicable.
Code availability
Not applicable.
Declarations
Conflict of interest
The authors declare they have no conflict of interest.
Ethical Approval
This is a review paper. No ethics approval required.
Disclosure
No financial relationships relevant to this article to disclose.
CDC Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Disease Control and Prevention. HIV Surveillance Report, 2019. 2021. vol 32.
- 2.Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321(9):844–845. doi: 10.1001/jama.2019.1343. [DOI] [PubMed] [Google Scholar]
- 3.Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang YA, Zhu W, Smith DK, Harris N, Hoover KW. HIV preexposure prophylaxis, by race and ethnicity—United States, 2014–2016. MMWR Morb Mortal Wkly Rep. 2018;67(41):1147–1150. doi: 10.15585/mmwr.mm6741a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Golub SA. PrEP stigma: implicit and explicit drivers of disparity. Curr HIV/AIDS Rep. 2018;15(2):190–197. doi: 10.1007/s11904-018-0385-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ojikutu BO, Bogart LM, Higgins-Biddle M, Dale SK, Allen W, Dominique T, et al. Facilitators and barriers to pre-exposure prophylaxis (PrEP) use among black individuals in the United States: results from the National Survey on HIV in the Black Community (NSHBC) AIDS Behav. 2018;22(11):3576–3587. doi: 10.1007/s10461-018-2067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Muessig KE, Nekkanti M, Bauermeister J, Bull S, Hightow-Weidman LB. A systematic review of recent smartphone, Internet and Web 20 interventions to address the HIV continuum of care. Curr HIV/AIDS Rep. 2015;12(1):173–190. doi: 10.1007/s11904-014-0239-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Budak JZ, Scott JD, Dhanireddy S, Wood BR. The impact of COVID-19 on HIV care provided via telemedicine-past, present, and future. Curr HIV/AIDS Rep. 2021;18(2):98–104. doi: 10.1007/s11904-021-00543-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong KYK, Stafylis C, Klausner JD. Telemedicine: a solution to disparities in human immunodeficiency virus prevention and pre-exposure prophylaxis uptake, and a framework to scalability and equity. mHealth. 2020;6:21. [DOI] [PMC free article] [PubMed]
- 10.Calabrese SK, Underhill K. How stigma surrounding the use of HIV preexposure prophylaxis undermines prevention and pleasure: a call to destigmatize “Truvada Whores”. Am J Public Health. 2015;105(10):1960–1964. doi: 10.2105/AJPH.2015.302816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hubach RD, Currin JM, Sanders CA, Durham AR, Kavanaugh KE, Wheeler DL, et al. Barriers to access and adoption of pre-exposure prophylaxis for the prevention of HIV among men who have sex with men (MSM) in a relatively rural state. AIDS Educ Prev. 2017;29(4):315–329. doi: 10.1521/aeap.2017.29.4.315. [DOI] [PubMed] [Google Scholar]
- 12.Mayer KH, Agwu A, Malebranche D. Barriers to the wider use of pre-exposure prophylaxis in the United States: a narrative review. Adv Ther. 2020;37(5):1778–1811. doi: 10.1007/s12325-020-01295-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sullivan PS, Mena L, Elopre L, Siegler AJ. Implementation strategies to increase PrEP uptake in the South. Curr HIV/AIDS Rep. 2019;16(4):259–269. doi: 10.1007/s11904-019-00447-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Philbin MM, Parish C, Pereyra M, Feaster DJ, Cohen M, Wingood G, et al. Health disparities and the digital divide: the relationship between communication inequalities and quality of life among women in a Nationwide Prospective Cohort Study in the United States. J Health Commun. 2019;24(4):405–412. doi: 10.1080/10810730.2019.1630524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.United States Census Bureau. Urban and Rural. 2021. https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural.html.
- 16.Tawfik GM, Dila KAS, Mohamed MYF, Tam DNH, Kien ND, Ahmed AM, et al. A step by step guide for conducting a systematic review and meta-analysis with simulation data. Trop Med Health. 2019;47(1):46. doi: 10.1186/s41182-019-0165-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blumenthal J, Pasipanodya EC, Jain S, Sun S, Ellorin E, Morris S, et al. Comparing self-report pre-exposure prophylaxis adherence questions to pharmacologic measures of recent and cumulative pre-exposure prophylaxis exposure. Front Pharmacol. 2019;10:721. doi: 10.3389/fphar.2019.00721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blumenthal JM, Jain S, Sun X, Ellorin E, Corado K, Hoenigl M, Dube M, Haubrich R, Morris SR. Recent HIV risk behavior and partnership type predict HIV pre-exposure prophylaxis adherence in men who have sex with men. AIDS Pat Care. 2019;33(5):220–226. doi: 10.1089/apc.2018.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bond KT, Gunn AJ. Perceived advantages and disadvantages of using pre-exposure prophylaxis (PrEP) among sexually active black women: an exploratory study. J Black Sex Relationsh. 2016;3(1):1–24. doi: 10.1353/bsr.2016.0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chandler R, Hull S, Ross H, Guillaume D, Paul S, Dera N, et al. The pre-exposure prophylaxis (PrEP) consciousness of black college women and the perceived hesitancy of public health institutions to curtail HIV in black women. BMC Public Health. 2020;20(1):1172. doi: 10.1186/s12889-020-09248-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fuchs JD, Stojanovski K, Vittinghoff E, McMahan VM, Hosek SG, Amico KR, et al. A mobile health strategy to support adherence to antiretroviral preexposure prophylaxis. AIDS Patient Care STDS. 2018;32(3):104–111. doi: 10.1089/apc.2017.0255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoenigl M, Jain S, Moore DJ, Collins D, Sun X, Anderson PL, et al. Substance-using MSM on HIV preexposure prophylaxis have better adherence. Top Antiviral Med. 2017;25:413s–s414. [Google Scholar]
- 23.Hoth AB, Shafer C, Dillon DB, Mayer R, Walton G, Ohl ME. Iowa TelePrEP: a public-health-partnered telehealth model for HIV pre-exposure prophylaxis (PrEP) delivery in a rural state. Sex Transm Dis. 2019;30:30. doi: 10.1097/OLQ.0000000000001017. [DOI] [PubMed] [Google Scholar]
- 24.Liu AY, Vittinghoff E, von Felten P, Rivet Amico K, Anderson PL, Lester R, et al. Randomized controlled trial of a mobile health intervention to promote retention and adherence to preexposure prophylaxis among young people at risk for human immunodeficiency virus: The EPIC Study. Clin Infect Dis. 2019;68(12):2010–2017. doi: 10.1093/cid/ciy810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu AY, Laborde ND, Coleman K, Vittinghoff E, Gonzalez R, Wilde G, et al. DOT diary: developing a novel mobile app using artificial intelligence and an electronic sexual diary to measure and support PrEP adherence among young men who have sex with men. AIDS Behav. 2021;25(4):1001–1012. doi: 10.1007/s10461-020-03054-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mitchell JT, LeGrand S, Hightow-Weidman LB, McKellar MS, Kashuba AD, Cottrell M, et al. Smartphone-based contingency management intervention to improve pre-exposure prophylaxis adherence: pilot trial. JMIR Mhealth Uhealth. 2018;6(9):e10456. doi: 10.2196/10456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moore DJ, Jain S, Dube MP, Daar ES, Sun X, Young J, et al. Randomized controlled trial of daily text messages to support adherence to preexposure prophylaxis in individuals at risk for human immunodeficiency virus: the TAPIR Study. Clin Infect Dis. 2018;66(10):1566–1572. doi: 10.1093/cid/cix1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pasipanodya EC, Jain S, Sun X, Blumenthal J, Ellorin E, Corado K, et al. Trajectories and predictors of longitudinal preexposure prophylaxis adherence among men who have sex with men. J Infect Dis. 2018;218(10):1551–1559. doi: 10.1093/infdis/jiy368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Refugio ON, Kimble MM, Silva CL, Lykens JE, Bannister C, Klausner JD. Brief Report: PrEPTECH: a telehealth-based initiation program for HIV pre-exposure prophylaxis in young men of color who have sex with men. A pilot study of feasibility. J Acquir Immune Defic Syndr. 2019;80(1):40–45. doi: 10.1097/QAI.0000000000001873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shrestha R, Altice FL, DiDomizio E, Sibilio B, Ranjit YS, Copenhaver MM. Feasibility and acceptability of an mHealth-based approach as an HIV prevention strategy among people who use drugs on pre-exposure prophylaxis. Pat Prefer Adherence. 2020;14:107–118. doi: 10.2147/PPA.S236794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stekler JD, McMahan V, Ballinger L, Viquez L, Swanson F, Stockton J, et al. HIV pre-exposure prophylaxis prescribing through telehealth. J Acquir Immune Defic Syndr JAIDS. 2018;77(5):e40–e42. doi: 10.1097/QAI.0000000000001621. [DOI] [PubMed] [Google Scholar]
- 32.Smith DK, Van Handel M, Grey J. Estimates of adults with indications for HIV pre-exposure prophylaxis by jurisdiction, transmission risk group, and race/ethnicity, United States, 2015. Ann Epidemiol. 2018;28(12):850–7.e9. doi: 10.1016/j.annepidem.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 33.Kanny D, Jeffries WLT, Chapin-Bardales J, Denning P, Cha S, Finlayson T, et al. Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men—23 urban areas, 2017. MMWR Morb Mortal Wkly Rep. 2019;68(37):801–806. doi: 10.15585/mmwr.mm6837a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Commun Health. 2013;38(5):976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramsetty A, Adams C. Impact of the digital divide in the age of COVID-19. J Am Med Inform Assoc. 2020;27(7):1147–1148. doi: 10.1093/jamia/ocaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wood BR, Young JD, Abdel-Massih RC, McCurdy L, Vento TJ, Dhanireddy S, et al. Advancing digital health equity: a policy paper of the Infectious Diseases Society of America and the HIV medicine association. Clin Infect Dis. 2021;72(6):913–919. doi: 10.1093/cid/ciaa1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention. HIV Infection, Risk, Prevention, and Testing Behaviors Among Transgender Women—National HIV Behavioral Surveillance, 7 U.S. Cities, 2019–2020. 2021.
- 38.Centers for Disease Control and Prevention. HIV Surveillance Report, 2018 (Updated). 2020.
- 39.Mistler CB, Copenhaver MM, Shrestha R. The pre-exposure prophylaxis (PrEP) care cascade in people who inject drugs: a systematic review. AIDS Behav. 2021;25(5):1490–1506. doi: 10.1007/s10461-020-02988-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Community Preventative Services Task Force. Methods Manual for Community Guide Systematic Reviews. 2021. https://www.thecommunityguide.org/methods-manual.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.