SUMMARY
Objective
The prognostic significance of the resection margins is still subject of conflicting opinions. The purpose of this paper is to report the results of a study on the margins in carcinoma of the oral cavity, oro-hypopharynx and larynx.
Methods
A multicentre prospective study was carried out between 2015 and 2018 with the participation of 10 Italian reference hospitals. The primary objective was to evaluate local control in patients with well-defined clinical characteristics and comprehensive histopathological information.
Results
During the study period, 455 patients were enrolled; the minimum follow-up was 2 years. Previous treatment, grading and fresh specimen examination were identified as risk factors for local control in multivariate analysis. On the basis of these results, it seems possible to delineate “risk profiles” for different oncological outcomes.
Discussion
The prognostic significance of the margins is reduced, and other risk factors emerge, which require diversified treatment and follow-up.
Conclusions
Multidisciplinary treatment with adjuvant therapy, if indicated, reduces the prognostic importance of margins. Collaboration with a pathologist is an additional favourable prognostic factor and quality indicator.
An appendix with literature review is present in the online version.
KEY WORDS: resection margins, oral-pharyngeal-laryngeal cancer
RIASSUNTO
Obiettivo
Il significato prognostico dei margini di resezione è ancora oggetto di pareri discordanti. Scopo di questo scritto è riportare i risultati di uno studio sui margini nel carcinoma del cavo orale, oro-ipofaringe e laringe.
Metodi
È stato condotto uno studio prospettico multicentrico con la partecipazione di 10 Centri italiani, nel periodo 2015-2018, con l’obiettivo primario di valutare il controllo locale in pazienti con ben determinate caratteristiche cliniche e con disponibilità di esaurienti informazioni istopatologiche.
Risultati
Nel periodo in studio sono stati arruolati 455 pazienti con un follow-up minimo di 2 anni. All’analisi multivariata per il controllo locale sono risultati fattori di rischio il trattamento precedente, il grading e l’esame a fresco dello specimen. Sulla base dei risultati ottenuti è possibile delineare un “profilo di rischio” per tutti i diversi outcomes oncologici.
Discussione
Il significato prognostico dei margini è ridotto, altri fattori emergono come profili di rischio, che richiederebbero trattamento e follow-up diversificati.
Conclusioni
Il trattamento multidisciplinare con la terapia adiuvante se indicata, può aver ridimensionato l’importanza prognostica dei margini. La collaborazione con l’anatomopatologo è fattore prognostico favorevole supplementare ed indicatore di qualità.
Appendice con revisione della letteratura nella versione online.
PAROLE CHIAVE: margini resezione, carcinoma cavo orale-faringe-laringe
Introduction
In head and neck squamous cell carcinoma, the variable “surgical margins” is often recognised to have a good prognostic relevance 1-3, which involves the indication for therapeutic intensification 4. However, there are some conflicting opinions, albeit on selected series 5, and reports on the difficulties in standardising data. Namely, quantification of margins and subdivision into “free”, “close” and “infiltrated” do not always have shared values and studies comparing margin width with relapses have yielded conflicting results. The importance not only of millimeters, but of the margin type and many other factors are recognised 6-9. Although margins < 5 mm appear to be associated with a significantly higher relapse rate and would therefore require adjuvant treatment 10, data for 20% of local relapses with margins ≥ 5 mm 11 and for 9% of relapses with margins ≥ 10 mm 12 suggest the presence of subsets of patients who should be adequately identified. Only some studies present multivariate analysis of prognostic factors without confounding effects and the interrelation between margins and other histopathological and clinical factors is still unclear. There is also a need for reliable reassessment of the prognostic impact of variable “margins” in relation to other parameters and for accurate identification of patients at risk of relapse even with free margins. A verification of the relationships between all tumour pathologies and size of margins and, therefore, of the efficacy of surgery as initial or only treatment 13,14 is also needed. A prospective multicentre study on resection margins and other factors in squamous cell carcinoma of the oral cavity, oro-hypopharynx and larynx was conducted in order to contribute to the clarification of some of the current issues. This paper aims to present the collected data, with a minimum follow-up of 2 years, and review of literature on this topic in the online version.
Methods
After a series of preliminary meetings of the Directors of the Otolaryngology Departments (the invitation was initially extended to the geographical area of Triveneto, North-Eastern Italy, within the network of the Scuola Triveneta di Discipline Otorinolaringoiatriche), with the participation of Pathologists, Radiotherapists, Medical Oncologists and Biostatistic experts, a protocol of “Multicentre prospective observational study on resection margins and other histopathological factors in squamous cell carcinoma of the oral cavity, oro-hypopharynx, larynx” was shared and formalised. The primary objective was evaluation of margins and other factors in local control (LC), measured by the absence of relapses at the primary tumour site (T).
Inclusion criteria were: female and male patients who had signed an informed consent, age > 18 years with squamous cell carcinoma of the oral cavity-oropharynx-larynx-hypopharynx (diagnosis on the surgical specimen) even pretreated, surgery performed for radical purposes, ECOG (Eastern Cooperative Oncology Group) performance status < 4 and complete staging with adequate imaging.
The exclusion criteria were: distant metastatic disease, palliative surgery, surgical specimen without a correct, definite identification of its anatomical relationships and margins, comorbidity so as to discourage the use of adjuvant-concomitant chemotherapy with radiotherapy if indicated, pregnancy, lactation, other synchronous tumours (excluding cutaneous basal cell carcinoma and cervical Tis) and primary and secondary immunosuppression.
Consecutively treated patients who had given their consent participated in the study. Type of surgery and any adjuvant treatment were left to the decisions of the individual centres, which all had an operative Multidisciplinary Head & Neck Board.
Surgery
The practice of removing margins and sending them separately was avoided, unless the surgeon saw the need, after initial resection, for further radicalisation in one or more directions, with correct identification of the side opposite to the one of the tumour. If logistically possible, the surgical specimen was sent intact and fresh to be macroscopically and microscopically evaluated. Alternatively, various measures were taken to make orientation and margins (even of N in the case of massive lymph node metastasis) identifiable. The surgeon reported the instrument mainly used for the resection of T, any additional radicalisations, if she/he decided to stop near an anatomical barrier. If N surgery was performed, it was specified if it was done in monobloc with T, discontinuous or deferred.
Pathology
The modalities of treatment of the specimen, margin mapping, histopathologic examination and reporting, followed the guidelines of the Royal College of Pathologists 15, and were reviewed by the Board of Pathologists participating in the study. The evaluation of margins for both intraoperative and definitive examination was performed with perpendicular samples (no shave sections) that included T and each margin of interest. Each edge was examined at least on 3 floors/levels. In the final evaluation of margin distance, which was microscopically measured in mm on glass, the specimen’s margins were considered. If further immediate or deferred radicalisations were performed, in the final assessment of margis status (free or infiltrated) the state of the ultimate definitive margin was assessed. In the final report, the pathologist, in addition to the macroscopic and microscopic description of the specimen, explained all the items listed in Table III.
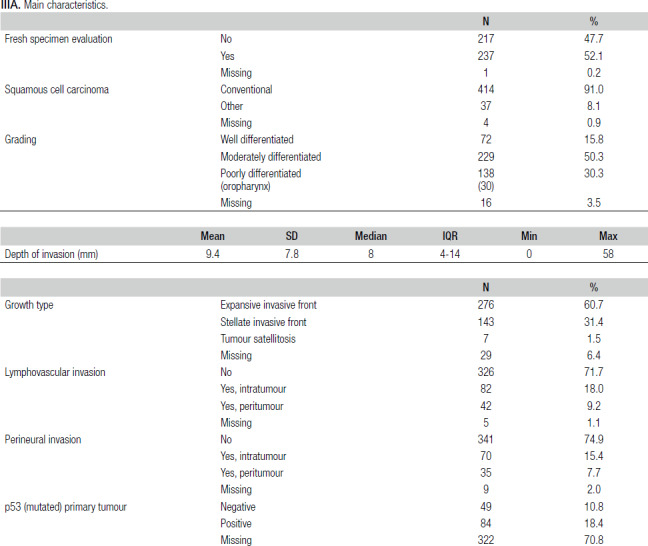
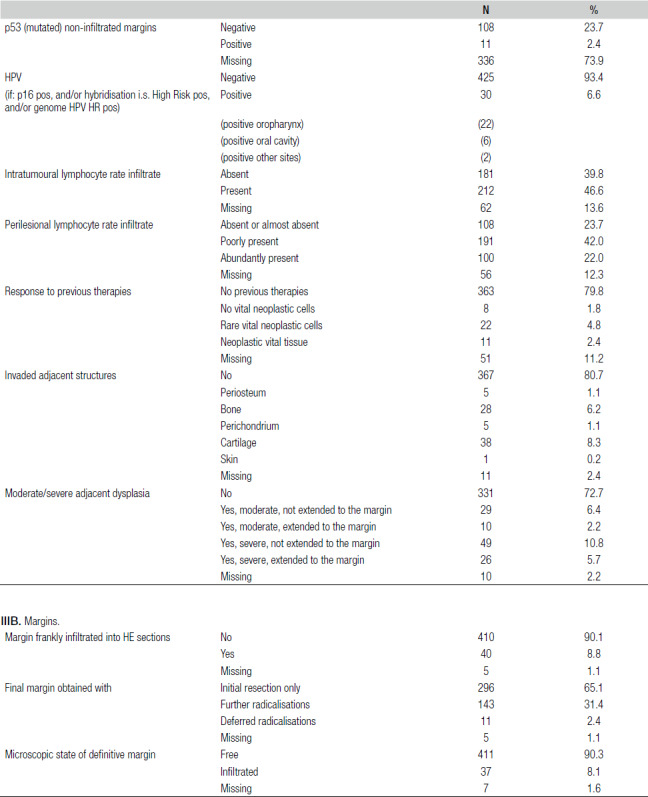
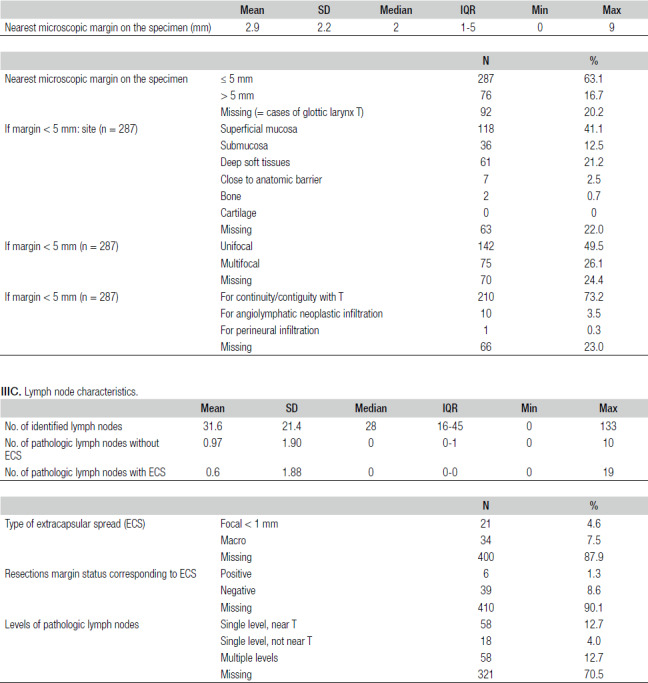
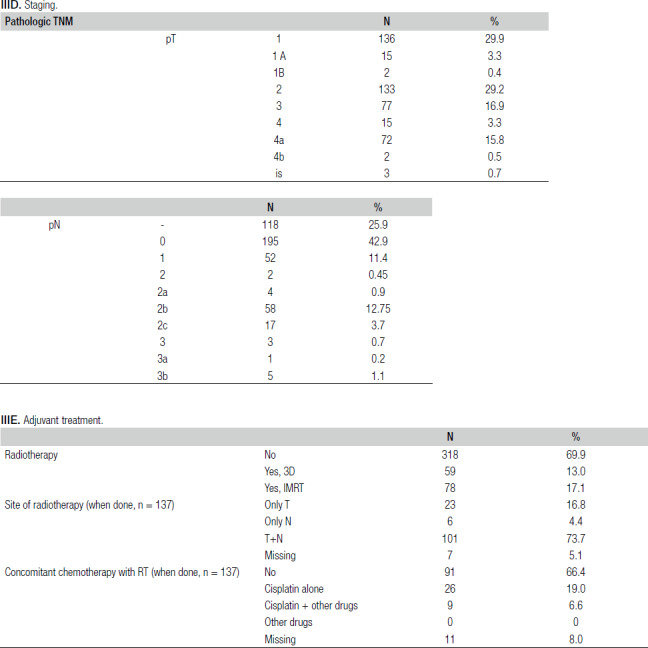
Table III.
Histopathological characteristics.
Radiotherapy
Any adjuvant treatment followed the standards of the 2015 NCCN guidelines 16. High risk: infiltrated margins, extracapsular lymph nodal spread (ECS), advanced class of T or N, lymph nodes at levels IV-V and perineural or angiolymphatic spread. Radiation therapy, when possible, started within 6 (max 8) weeks after surgery. The IMRT with a dose range between 60 and 66 Gy at the volume of 95% was used when possible.
Chemotherapy
Only infiltrated margins or ECS indicated concomitant adjuvant chemotherapy.
Statistical analysis
Descriptive statistics were used to summarise data (mean and standard deviation, median and interquartile range (IQR) for quantitative variables and frequencies and percentages for qualitative ones). Qualitative variables were analysed using Pearson’s Chi-square test, while a t-test was employed to analyse continuous variables.
Univariate [crude ORs and corresponding 95% confidence intervals (CI)] and multivariate (adjusted ORs and corresponding 95% CI) logistic analyses were used to identify independent risk factors for local control (LC) and loco-regional control (LRC).
A receiving operating curve (ROC) was plotted for margin distance against LC status to define a cut-off to maximise sensitivity and specificity.
Kaplan-Meier curves and log-rank test were used for survival analysis of local recurrence-free survival (LRFS), overall survival (OS), disease-specific survival (DSS) and disease-free survival (DFS). Multivariate Cox proportional hazard models were used to determine the independent effect of variables on LRFS, OS, DSS and DFS. For each outcome, a multivariate Cox model was fitted, including only those variables significant at univariate analysis as independent variables. In all analyses, p-values < 0.05 were considered significant. Stata/IC 15 was used for statistical analysis (Stata Corp LP, College Station, TX, USA).
All paper documents, enrollment and follow-up forms were collected and are available for consultation at the Aviano Oncological Referral Centre. Data were transferred to an Excel sheet and regularly updated as the follow-up proceeded.
Results
Patient enrollment, which began in December 2015, was completed in December 2018; all patients had follow-up data. The allocation of the 455 patients in the participating centers was as follows:
University of Padua: 103;
Hospital of Cittadella: 77;
Hospital of Pordenone: 71;
University of Trieste: 55;
Hospital of Mestre-Venezia: 38;
University of Padua-Treviso: 38;
Hospital of Legnago: 27;
University of Pavia: 26;
Hospital of Trento: 11;
Oncology Referral Centre of Aviano: 9.
General characteristics
Table I shows the main clinical characteristics of the study population. The mean age at diagnosis was 66.5 (± 12.4) years, with a minimum age of 23 and a maximum of 95 years. Table II shows the distribution of smoking status by sex and by T site. There was a significant association between smoking habit and gender (p < 0.0001) and between smoking habit and tumour site (p < 0.0001): for the most frequent site of T, the oral cavity, the number of never smokers was very high compared to smokers and former smokers.
Table I.
Clinical characteristics.
| N | % | ||
|---|---|---|---|
| Sex | Male | 318 | 69.9 |
| Female | 137 | 30.1 | |
| Site of T | Oral cavity | 232 | 51.0 |
| Oropharynx | 62 | 13.6 | |
| Supraglottic larynx | 40 | 8.8 | |
| Glottic larynx | 92 | 20.2 | |
| Hypopharynx | 29 | 6.4 | |
| cT (clinical class of T) | 1 | 134 | 29.5 |
| 2 | 144 | 31.6 | |
| 3 | 88 | 19.3 | |
| 4 | 89 | 19.6 | |
| cN (clinical class of N) | 0 | 340 | 74.7 |
| 1 | 34 | 7.5 | |
| 2 | 1 | 0.2 | |
| 2a | 20 | 4.4 | |
| 2b | 46 | 10.1 | |
| 2c | 14 | 3.1 | |
| TNM stage | I | 125 | 27.5 |
| II | 116 | 25.5 | |
| III | 84 | 18.4 | |
| IV | 130 | 28.6 | |
| Previous treatment | No | 354 | 77.8 |
| Yes | 101 | 22.2 | |
| Surgery of glottic larynx | Transoral | 33 | 35.9 |
| Partial laryngectomy | 16 | 17.4 | |
| Total laryngectomy | 43 | 46.7 | |
| Main instrument (for all T sites) | Cold | 114 | 25.1 |
| Electrosurgical blade | 159 | 34.9 | |
| Laser | 112 | 24.6 | |
| Radiofrequencies | 10 | 2.2 | |
| Energy-based technology* | 49 | 10.8 | |
| Other | 2 | 0.4 | |
| Missing | 9 | 2.0 | |
| Surgery of N | No | 126 | 27.7 |
| Yes selective | 253 | 55.6 | |
| Yes all levels | 76 | 16.7 | |
| Type of N surgery | En bloc with T | 117 | 25.71 |
| Discontinuous | 205 | 45.05 | |
| Deferred | 5 | 1.10 | |
| Missing | 128 | 28.13 |
* Harmonic, Ligasure, EnSeal, Gyrus PK et al.
Table II.
Smoking distribution by gender and by T site.
| Gender | T site | |||||||
|---|---|---|---|---|---|---|---|---|
| Males | Females | Oral cavity | Oropharynx | Supraglottic larynx | Glottic larynx | Hypopharynx | Total | |
| Smoker | 120 | 33 | 69 | 19 | 18 | 43 | 4 | 153 |
| Former smoker | 136 | 26 | 67 | 24 | 18 | 32 | 21 | 162 |
| Never smoker | 58 | 75 | 94 | 16 | 4 | 15 | 4 | 133 |
| Missing | 4 | 3 | 2 | 3 | - | 2 | - | 7 |
| Total | 318 | 137 | 232 | 62 | 40 | 92 | 29 | 455 |
There was no difference between the average daily number of cigarettes of smokers (18.5 ± 8.8) and the average number of cigarettes smoked by former smokers (20 ± 10.5). The number of years of smoking was significantly higher among smokers vs former smokers (37.8 ± 12.3 vs 31.5 ± 12.4, p < 0.001).
Table III lists the histopathological characteristics.
For all T sites, as depth increased by 1 mm, the probability of pN + increased by approximately 5% (OR = 1.05, p = 0.0004, 95% CI 1.02-1.09). If the glottic larynx site is excluded, increasing by 1 mm in depth, this increased the probability of pN + by 5% (OR = 1.06, p = 0.0005, 95% CI 1.02-1.09).
The mean values of margins in mm were not modified within the classes of T (all sites of T, excluding the glottic larynx): more advanced T did not result in wider margins on average.
Given the anatomical peculiarities and the different significance of the margins in mm usually recognised in the literature, it was decided to keep the analysis of the glottic larynx separate from the other anatomical sites.
LC
LC FOR T SITES OTHER THAN THE GLOTTIC LARYNX
The number of patients was 363, 300 (83%) with LC and 63 (17%) without. Univariate (crude ORs) and multivariate (adjusted ORs) logistic analyses were performed to identify independent risk factors for LC. All variables were analysed, but only those that were significant at univariate analysis are reported in Table IV. Namely, at univariate analysis we can state that:
Table IV.
Local control for T site other than glottic larynx.
| Crude | Adjusted | |||||
|---|---|---|---|---|---|---|
| OR | p | 95% CI | OR | p | 95% CI | |
| Previous treatment (No vs Yes) | 0.36 | 0.0005 | 0.20-0.66 | 0.40 | 0.006 | 0.21-0.76 |
| Fresh specimen evaluation (Yes vs No) | 1.9 | 0.022 | 1.09-3.35 | 1.85 | 0.05 | 0.99-3.46 |
| Nearest microscopic margin on the specimen (mm) as continuous | 1.2 | 0.010 | 1.04-1.32 | 1.14 | 0.084 | 0.98-1.33 |
| Grading (continuous) | 0.50 | 0.0013 | 0.32-0.76 | 0.55 | 0.021 | 0.33-0.91 |
| Lymphovascular Invasion (Yes vs No) | 0.49 | 0.013 | 0.28-0.87 | 0.85 | 0.636 | 0.42-1.69 |
| Perineural invasion (Yes vs No) | 0.52 | 0.032 | 0.29-0.95 | 0.73 | 0.384 | 0.36-1.49 |
the probability of LC decreased by about 60% if the patient is pretreated, and more specifically it decreased by 70% if she/he was previously treated by surgery with/without other therapy, and by about 60% if she/he was previously treated by radiotherapy with/without other therapy (data not shown);
the probability of LC is roughly doubled if the specimen was fresh when it was evaluated;
the probability of LC did not change if the definitive margin was microscopically infiltrated or free. In order to have a significant probability of LC, it is not only sufficient that the margin is free but it must also be a few mm. The cut-off was 2.3 mm (see forward);
the probability of LC increased by 20% with a 1 mm increase in margins;
when passing from one category of grading to the next, the probability of LC was halved;
the likelihood of LC decreased by 50% if lymphovascular invasion was present;
the likelihood of LC decreased by approximately 50% if perineural invasion was present.
The minimum effective margin in mm for LC at univariate analysis was calculated by using a logistic model containing the nearest microscopic margin on the specimen (mm) as an independent variable and at ROC analysis a value of 2.3 mm was identified as the LC cut-off (AUC = 0.60, 95% CI 0.53-0.68, sensitivity 48.33%, specificity 69.84%).
The number of positive HPV oropharynx samples (n = 22) was too small to determine if the statement is valid even in this subgroup: “the probability of LC increased by 20% as the margin increases by 1 mm”.
At multivariate analysis (Tab. IV), margins (in mm), lymphovascular and perineural invasion lose statistical significance, whereas the following variables were independent factors for LC:
previous treatment: the probability of LC decreased by about 60% if the subject was pretreated, more specifically it decreased by 70% if she/he was previously treated by surgery with/without other treatments (different previous treatments are not significant, data not shown);
grading: when passing from one grade to the next, the probability of LC decreased by 45%;
evaluation of fresh specimens: the probability of LC increased by 85% if the specimen was evaluated when fresh.
LC FOR GLOTTIC LARYNX AS T SITE
92 patients were analysed, among whom 77 (84%) with LC and 15 (16%) without. No variables were significantly associated with LC.
LRC
LRC FOR T SITES OTHER THAN GLOTTIC LARYNX
363 patients were analysed, among whom 266 (73%) with LRC and 97 (27%) without. At multivariate analysis, only grade (OR 0.39; p 0.031; 95% CI 0.16-0.91) and p53 status of the primary tumour (pos vs neg) (OR 0.32; p 0.046; 95% CI 0.11-0.98) remained significant. This means that moving from one grade to the next, the likelihood of LRC decreases by approximately 40%, regardless of other variables in the model. Moreover, the probability of LRC decreased by 68% if the primary tumour was p53-positive, regardless of other variables in the model.
LRC FOR GLOTTIC LARYNX AS THE T SITE
In the sample of 92 patients, 75 (81.5%) with LRC and 17 (18.5%) without, none of the variables were significant.
LRFS
LRFS FOR T SITES OTHER THAN GLOTTIC LARYNX
Median follow-up time was 30.8 (mean 29.4) months. Kaplan-Meier curves are reported in Figure 1. Previous treatment, grading, evaluation of the fresh specimen, microscopic state of definitive margin, lymphovascular invasion, perineural invasion, TNM stage, pT and pathologic nodes with ECS were found to be prognostic factors for LRFS.
Figure 1.
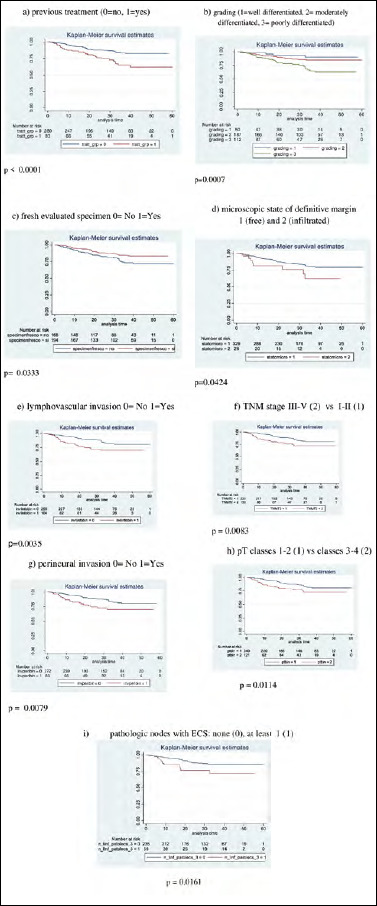
Tumour relapse-free survival (TRFS) for T sites other than glottic larynx. Kaplan-Meier curves based on: (a) previous treatment; (b) grading; (c) fresh specimen evaluation; (d) microscopic state of definitive margin; (e) lymphovascular invasion; (f) TNM stage; (g) perineural invasion; (h) pT; (i) pathologic nodes with ECS.
Table VA shows adjusted HRs for LRFS. Pathological lymph nodes with ECS were the only prognostic factors for LRFS in a multivariate Cox model.
Table V.
Adjusted hazard ratios for different survival outcomes (only significant HR are reported in the Table).
VA.
T site other than glottic larynx.
| LRFS | DSS | OS | DFS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | p | 95% CI | HR | p | 95% CI | HR | p | 95% CI | HR | p | 95% CI | |
| Nearest microscopic margin on the specimen (mm) as continuous | 0.82* | 0.057 | 0.68-1.00 | |||||||||
| Frankly infiltrated margin HE sect | 2.26** | 0.043 | 1.02-4.96 | |||||||||
| Grading (continuous) | 1.65^ | 0.008 | 1.14-2.40 | |||||||||
| TNM stage (III-IV vs I-II) | 2.79^ | 0.009 | 1.29-6.00 | |||||||||
| pT (classes 3-4 vs classes 1-2) | 2.43** | 0.017 | 1.17-5.07 | 1.91^ | 0.035 | 1.05-3.48 | 1.80° | 0.054 | 0.99-3.27 | |||
| Pathologic lymph nodes with ECS (at least 1 vs none) | 2.3* | 0.039 | 1.04-5.08 | 2.07** | 0.046 | 1.01-4.24 | 2.03° | 0.019 | 1.12-3.66 | |||
* Adjusted by: previous treatment, fresh specimen evaluation, nearest microscopic margin on the specimen, grading, lymphovascular invasion, perineural invasion, cT, pT.
** Adjusted by: previous treatment, nearest microscopic margin on the specimen, depth of invasion, grading, lymphovascular invasion, perineural invasion, cT, cN, pN, identified lymph nodes, chemotherapy.
^ Adjusted by: depth of invasion, frankly infiltrated margin HE, nearest microscopic margin on the specimen, lymphovascular invasion, perineural invasion, cT, cN, pN, identified lymph nodes, pathologic lymph nodes with ECS.
° Adjusted by: previous treatment, frankly infiltrated margin HE, nearest microscopic margin on the specimen, grading, lymphovascular invasion, perineural invasion, TNM stage, pN, identified lymph nodes, number of pathological lymph nodes.
VB.
Glottic larynx as T site.
| LRFS | DSS | OS | DFS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | p | 95% CI | HR | p | 95% CI | HR | p | 95% CI | HR | p | 95% CI | |
| Depth of invasion | 0.83& | 0.010 | 0.72-0.96 | |||||||||
| Perineural invasion | 5.76& | 0.025 | 1.24-26.7 | |||||||||
| cN (0 vs remnant) | 7.62§ | 0.007 | 1.74-33.36 | 14.7& | 0.01 | 1.87-115.0 | ||||||
| pT (classes 3-4 vs classes 1-2) | 15.6& | 0.009 | 1.97-123.3 | |||||||||
| pN (0 vs remnant) | 6.96& | 0.015 | 1.46-33.11 | |||||||||
§ Adjusted by: previous treatment, depth of invasion, perineural invasion, pT.
& Adjusted by: previous treatment, depth of invasion, lymph node invasion.
LRFS FOR GLOTTIC LARYNX AS THE T SITE
Median follow-up time was 35 (mean 31.7) months. No variables were significantly associated with LC.
DSS
DSS for T sites other than glottic larynx
Median follow-up time was 29.8 (mean 27.8) months. Kaplan-Meier curves for DSS are reported in Figure 2. Previous treatment, frankly infiltrated margin into hematoxylin & eosin (HE) sections, microscopic state of definitive margins, grade, lymphovascular invasion, cN, perineural invasion, TNM stage, cT, pN, pT, pathological nodes with ECS and number of pathological lymph nodes were found to be prognostic factors for DSS. Table VA shows adjusted HRs for DSS. Frankly infiltrated margins into HE sections, pT and pathological lymph nodes with ECS were prognostic factors for DSS in the multivariate Cox model.
Figure 2.
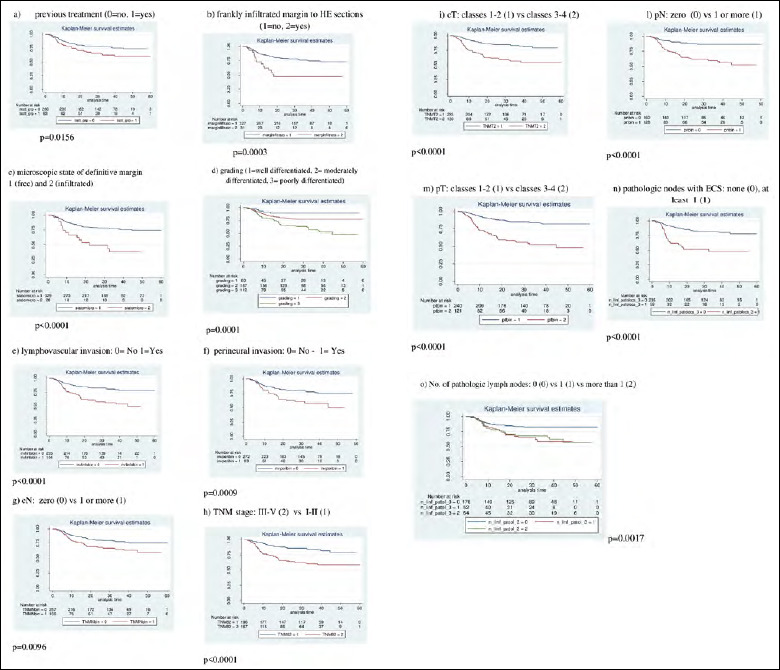
Diseases-pecific survival (DSS) for T site other than glottic larynx. Kaplan-Meier curves based on: (a) previous treatment; (b) frankly infiltrated margin into HE sections; (c) microscopic state of definitive margin; (d) grading; (e) lymphovascular invasion; (f) perineural invasion; (g) cN; (h) TNM stage; (i) cT; (l) pN; (m) pT; (n) pathologic nodes with ECS; (o) No. of pathologic lymph nodes.
DSS FOR GLOTTIC LARYNX AS THE T SITE
Median follow-up time was 34.3 (mean 30.7) months. Kaplan–Meier curves for DSS are reported in Figure 3. Previous treatment, cN, tumour growth, pT and perineural invasion were found to be prognostic factors for DSS for glottic larynx tumours.
Figure 3.

Disease-specific survival (DSS) for glottic larynx as T site. Kaplan-Meier curves based on: (a) previous treatment; (b) cN; (c) tumour growth; (d) pT; (e) perineural invasion.
Table VB shows adjusted HRs for DSS: only cN is a prognostic factor for DSS. Due to the small sample size, the 95% CI are wide.
OS
OS FOR T SITES OTHER THAN THE GLOTTIC LARYNX
Median follow-up time was 32.8 (mean 31) months. At multivariate analysis (Tab. VA) grade, TNM stage (III-IV vs I-II) and pT (classes 3-4 vs 1-2) were significant prognostic factors.
OS FOR GLOTTIC LARYNX AS THE T SITE
Median follow-up time was 35.4 (mean 32.8) months. At multivariate analysis (Tab. VB) depth of invasion, perineural invasion, cN (0 vs the remnant), pT (classes 3-4 vs 1-2) and pN (0 vs the remnant) were significant prognostic factors.
DFS
DFS FOR T SITES OTHER THAN THE GLOTTIC LARYNX
Median follow-up time was 30 (mean 28) months. In multivariate analysis (Tab. VA), only the number of pathological lymph nodes with ECS was significant (at least 1 vs none).
DFS FOR GLOTTIC LARYNX AS THE T SITE
Median follow-up time was 34 (mean 30.7) months. At multivariate analysis (Tab. VB), no variables were significantly associated with DFS.
Further results
There was no association between smoking and a microscopic definitive margin. There was no association between smoking and LC and DFS.
The probability that further radicalisations were performed was 4 times greater if the specimen was evaluated when it is fresh (OR = 4.6, 95% CI 2.73-7.73, p < 0.0001).
LC and DFS (all anatomic sites, excluding glottic larynx) do not change whether, with theoretically inadequate surgical radicality (microscopic state of the definitive margin = infiltrate, or margin on the specimen < 5 mm), adjuvant radiotherapy was performed (96 patients) or not (191 patients).
LC and DFS do not change if, with inadequate surgical radicality, adjuvant radiotherapy was done with ≥ 60 Gy or less.
Salvage therapy for T relapse (all T sites) was effective (no further recurrence) in 18 of 81 patients (22.2%).
Discussion
In the recent literature, the prognostic significance of resection margins in carcinomas of the upper airways has been variably evaluated (see Appendix with literature review 2000-2021 in the online version: https://www.actaitalica.it/article/view/1601). Some authors have considered that millimetre distance – albeit with diverse interpretative ranges – is crucial for oncological outcomes 17-19 (among the most recent). Others, while confirming the importance of margins, also suggest that other factors affect prognosis 20,21 (among the most recent). There are also several authors who deny the prognostic significance of margins 22,23 (among the most recent), even in multivariate analyses 24,25.
The present multicentre study, which systematically employed multivariate data analysis, shows some unexpected results, as well as the confirmation of some well-known prognostic factors.
The prognostic significance of resection margins seems decidedly reduced: only the “surgical margin frankly infiltrated into HE sections” for DSS remained significant, whereas all the others “margin items” lost importance, even if they are based on the mm variable of the margin distance. Even carrying out further radicalisations was not significant: if the intervention for some reason was conducted in an inadequate manner with a margin of the specimen that was grossly infiltrated at histology, the prognosis remained difficult to predict.
The variable “fresh specimen evaluation” is not commonly considered in most clinical studies on head and neck cancers, probably because it is not considered to be related to oncological outcomes. In the series presented herein, it was determined if it was linked to other variables. The probability of further radicalisations was four times greater if the specimen was evaluated when it is fresh, but on LC it was irrelevant whether the definitive margin was obtained only with the initial resection or with subsequent radicalisations. The probability of LC was about doubled only when the fresh specimen was evaluated. This is a surprising, unexpected and not easily explainable result. We assume that evaluation of the fresh specimen constitutes a quality indicator of the surgical and pathological procedures and of their effectiveness.
The seriously unfavourable significance of previous treatment for LC is once again documented in this series, especially for patients who had previously undergone surgery. There must be a full awareness of this when preparing a patient for salvage surgery.
T class does not appear to be a prognostic factor for LC. This is probably due to the effect of radiotherapy, which, since it is administered more frequently in more advanced T classes, corrected the theoretically worse prognosis, making it similar to that of the early classes. In fact, patients with more advanced T classes who received adjuvant radiotherapy were 63/121 (52%), while those with early T classes who received radiotherapy were 56/240 (23%) (p < 0.001). A similar consideration on the “leveling” effect of adjuvant treatment can be made for all the variables on resection margins.
The usefulness of adjuvant treatment on inadequate resection margins has long been debated in literature: one recent paper 22, on a series of 1199 patients with head and neck carcinoma aged ≥ 70 years, argued that benefits in OS with adjuvant therapy are only observed for N2-3, and not for margins.
In the present series, radiotherapy did not emerge as a prognostic factor in univariate analyses (and therefore cannot be included in Cox’s models for multivariate ones), because it was not randomly used but linked to specific prognostically unfavourable clinical indications. Even the fact that LC and DFS do not change whether, with theoretically inadequate surgical radicality, adjuvant radiotherapy is performed or not, does not imply that adjuvant therapy was useless, This means that it is difficult to have meaningful data if the guidelines followed do not provide strict indications: the NCCN 16 suggests that “if positive surgical margins are reported, surgical re-resection and/or adjuvant therapy should be considered in selected patients” (not: must be performed in all patients).
Histopathological grading, a significant prognosticator, is often considered to be a partially subjective, operator-dependent parameter. A cumulative series of 10 centres may help eliminate any subjective bias from this variable.
On the basis of the outcomes achieved, it seems possible to delineate “risk profiles” for the various oncological results with the variables found to be significant at multivariate analyses:
for T sites other than glottic larynx: previous treatment (for LC), high grade (for LC, LRC, OS), non-fresh specimen evaluation (for LC), ECS (for LRFS, DFS, DSS), frankly infiltrated surgical margin into HE sections (for DSS), p53 on T (for LRC), advanced stage (for OS), advanced pT (for OS, DSS), all represent clear risk factors;
for glottic larynx as the T site: cN positive class (for DSS and OS), depth of invasion, advanced pT, the pN positive class, perineural invasion (for OS) and advanced TNM stage (for DSS) were documented as risk factors.
All these factors are associated with prognostic risk, which is different depending on the outcome considered, but which would require diversified treatment if possible or, at least, closer and more complete follow-up.
Certainly some aspects of this study could have been improved: although the large number of patients constitutes a key factor for statistical significance of the analysis, it cannot be excluded that the combination of different anatomical sites and sub-sites and the non-stringent common guidelines followed for adjuvant therapy may have produced some weakness. Furthermore, it was not considered that the concept of compartment surgery (oral tongue, lateral oropharynx, supraglottic larynx) may change the connotation of some margins; the prognostic value of specimen-driven or bed-driven frozen sections was not evaluated; molecular margins were not considered. “Margins” are a “world” and dealing with this issue in a complete, exhaustive manner in a single study is perhaps an impossible task. Further prospective well-designed and adequately representative studies are desirable to compensate for the shortcomings of the present analysis and to confirm or not what emerged here.
Conclusions
The treatment administered to patients in this series, with radical surgery and possible adjuvant therapy, significantly reduced the prognostic importance of resection margins. The presence of the Multidisciplinary Board, which is active in all participating centres, helped to standardise treatments, possibly reducing the theoretical significance of resection margins. At multivariate analyses, only surgical margins that frankly infiltrated into the HE sections (for DSS) remained significant, whereas other factors were not. There are many other prognostic factors, however, most of which are well known, which demonstrate that there are “risk profiles” that are worthy of renewed attention. The building of an effective collaboration between the surgeon and pathologist, which also entails the practice of examining the fresh specimen, is documented as a favourable prognostic factor and which can be taken as a quality indicator for the degree of efficiency of a given centre.
Acknowledgements
The authors wish to acknowledge the Scuola Triveneta di Discipline Otorinolaringoiatriche and its President Prof. Roberto Spinato, who made the organisation of this study possible.
Special thanks to Mrs. Daniela Michilin (Radiotherapy, CRO Aviano) for secretarial support and to Manuela Anelli, PhD for external English language revision.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributions
All authors had full access to the data in the study and take responsability for the integrity of the data and the accuracy of the data analysis. Study concept and design: LB, RDC, AM, RA, VG, GT, DP, RS, PBR, MCDM, FF, CG, GF, VC, SS, GM, EV. Acquisition of data: LB, RDC, MB, RC, PN, EG, VL, FBN, LL, DP, AM, FF, IH, MB, ALB, GF. Analysis of data: CM. Drafting the manuscript: LB, CM. Critical revision of the manuscript for intellectual content: LB, CM, GF. Study supervision: LB.
Ethical consideration
This study obtained the approval from the Independent Ethics Committee of the Oncology Referral Centre of Aviano, Pordenone, Italy (19 October 2015, CRO-2015-43) and subsequently from the Ethics Committees of all participating centres.
The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
Written informed consent was obtained from each participant/patient for study participation and data publication.
Figures and tables
References
- 1.Hinni ML, Ferlito A, Brandwein-Gensler M, et al. Surgical margins in head and neck cancer: a contemporary review. Head Neck 2013;35:1362-1370. https://doi.org/10.1002/hed.23110 10.1002/hed.23110 [DOI] [PubMed] [Google Scholar]
- 2.Smits RWH, Koljenovic S, Hardillo JA, et al. Resection margins in oral cancer surgery: room for improvement. Head Neck 2016;38:E197-203. https://doi.org/10.1002/hed.24075 10.1002/hed.24075 [DOI] [PubMed] [Google Scholar]
- 3.Varvares MA, Shannon P, Kenyon B, et al. Surgical margins and primary site resection in achieving local control in oral cancer resections. Laryngoscope 2015;125:2298-2307. https://doi.org/10.1002/lary.25397 10.1002/lary.25397 [DOI] [PubMed] [Google Scholar]
- 4.Bernier J, Cooper JS, Pajak TF, et al. Defining risk levels in locally advenced head neck cancers: a comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (#22931) and RTOG (#9501). Head Neck 2005;27:843-850. https://doi.org/10.1002/hed.20279 10.1002/hed.20279 [DOI] [PubMed] [Google Scholar]
- 5.Ch’ng S, Corbett-Burns S, Stanton N, et al. Close margin alone does not warrant postoperative adjuvant radiotherapy in oral squamous cell carcinoma. Cancer 2013;119:2427-2437. https://doi.org/10.1002/cncr.28081 10.1002/cncr.28081 [DOI] [PubMed] [Google Scholar]
- 6.Yang TL, Ko JY, Chang YL. Involved margin of tongue cancer: the impact of tumor satellites on prognosis. Head Neck 2008;30:845-851. https://doi.org/10.1002/hed.20789 10.1002/hed.20789 [DOI] [PubMed] [Google Scholar]
- 7.Alicandri-Ciuffelli M, Bonalli M, Piccinini A, et al. Surgical margins in head and neck squamous cell carcinoma: what is “close”? Eur Arch Otorhinolaryngol 2013;270:2603-2609. https://doi.org/10.1007/s00495-012-2317-8 10.1007/s00495-012-2317-8 [DOI] [PubMed] [Google Scholar]
- 8.Almangush A, Bello IO, Keski-Säntti H, et al. Depth of invasion, tumor budding, and worst pattern of invasion: prognostic indicators in early stage oral tongue cancer. Head Neck 2014;36:811-818. https://doi.org/10.1002/hed.23380 10.1002/hed.23380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luryi AL, Chen MM, Mehra S, et al. Treatment factors associated with survival in early stage oral cavity cancer. Analysis of 6830 cases from the National Cancer Data Base. JAMA Otolaryngol Head Neck Surg 2015;141:593-598. https://doi.org/10.1177/0194599814551718 10.1177/0194599814551718 [DOI] [PubMed] [Google Scholar]
- 10.Anderson CR, Sisson K, Moncrieff M. A meta-analysis of margin size and local recurrence in oral squamous cell carcinoma. Oral Oncol 2015;51:464-469. https://doi.org/10.1016/j.oraloncology.2015.01.015 10.1016/j.oraloncology.2015.01.015 [DOI] [PubMed] [Google Scholar]
- 11.Brandwein-Gensler M, Teixeira MS, Lewis CM, et al. Oral squamous cell carcinoma. Histologic risk assessment, but not margin status, is strongly predictive of local disease-free and overall survival. Am J Surg Pathol 2005;29:167-178. https://doi.org/10.1097/01.pas.0000149687.90710.21 10.1097/01.pas.0000149687.90710.21 [DOI] [PubMed] [Google Scholar]
- 12.Hicks WL, North JH, Loree TR, et al. Surgery as a single modality therapy for squamous cell carcinoma of the oral tongue. Am J Otolaryngol 1998;19:24-28. https://doi.org/10.1016/s0196-0709(98)90061-8 10.1016/s0196-0709(98)90061-8 [DOI] [PubMed] [Google Scholar]
- 13.Upile T, Fisher C, Jerjes W, et al. The uncertainty of the surgical margin in the treatment of head and neck cancer. Oral Oncol 2007;43:321-326. https://doi.org/10.1016/j.oraloncology.2006.08.002 10.1016/j.oraloncology.2006.08.002 [DOI] [PubMed] [Google Scholar]
- 14.Dik EA, Willems SM, Ipenburg NA, et al. Resection of early oral squamous cell carcinoma with positive or close marginas: relevance of adjuvant treatment in relation to local recurrence. Margin of 3 mm as safe as 5 mm. Oral Oncol 2014;50:611-615. https://doi.org/10.1016/j.oraloncology.2014.02.014 10.1016/j.oraloncology.2014.02.014 [DOI] [PubMed] [Google Scholar]
- 15.Helliwell T, Woolgar JA. Standard and minimum datasets for reporting cancers. Dataset for histopathology reporting of mucosal malignancies of the head and neck. London: Royal College of Pathologist; 2011. (https://www.rcpath.org/profession/guidelines.html). [Google Scholar]
- 16.NCCN Guidelines, Head Neck Cancers, Version 1.2015 (www.nccn.org/professionals).
- 17.Tasche KK, Buchakjian MR, Pagedar NA, et al. Definition of “close margin” in oral cancer surgery and association of margin distance with local recurrence rate. JAMA Otolaryngol Head Neck Surg 2017;143:1166-1172. https://doi.org/10.1001/jamaoto.2017.0548 10.1001/jamaoto.2017.0548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daniell J, Udovicich C, Rowe D, et al. Impact of histological oral tongue cancer margins on locoregional recurrence: a multi-centre retrospective analysis. Oral Oncol 2020;111:105004. https://doi.org/10.1016/j.oraloncology.2020.105004 10.1016/j.oraloncology.2020.105004 [DOI] [PubMed] [Google Scholar]
- 19.Singh A, Mair M, Singhvi H, et al. Optimim surgical margins in squamous cell carcinoma of the oral tongue: is the current definition adequate? Oral Oncol 2020;111:104938. https://doi.org/10.1016/j.oraloncology.2020.104938 10.1016/j.oraloncology.2020.104938 [DOI] [PubMed] [Google Scholar]
- 20.Huang CY, Lin YS, Kang BH, et al. Log margin-to-thickness ratio improves disease-specific survival prediction in oral cancer: a single cancer centre database. Clin Otolaryngol 2019;44:63-69. https://doi.org/10.1111/coa.13237 10.1111/coa.13237 [DOI] [PubMed] [Google Scholar]
- 21.Brinkman D, Callanan D, O’Shea R, et al. Impact of 3 mm margin on risk of recurrence and survival in oral cancer. Oral Oncol 2020;110:104883. https://doi.org/10.1016/j.oraloncology.2020.104833 10.1016/j.oraloncology.2020.104833 [DOI] [PubMed] [Google Scholar]
- 22.Yoshida EJ, Luu M, David JM, et al. Postoperative chemoradiotherapy in patients with head and neck cancer aged 70 or older with positive margins or extranodal extension and the influence of nodal classification. Head Neck 2018;40:1228-1236. https://doi.org/10.1002/hed.25100 10.1002/hed.25100 [DOI] [PubMed] [Google Scholar]
- 23.Cariati P, Cabello Serrano A, Mosalve Iglesias F, et al. What is the real prognostic value of close margins in oral Oncology? Curr Probl Cancer 2019;43:100500. https://doi.org/10.1016/j.currproblcancer.2019.100500 10.1016/j.currproblcancer.2019.100500 [DOI] [PubMed] [Google Scholar]
- 24.de Almeida JR, Li R, Magnuson JS, et al. Oncologic outcomes after transoral robotic surgery: a multi-institutional study. JAMA Otolaryngol Head Neck Surg 2015;141:1043-1051. https://doi.org/10.1001/jamaoto.2015.1508 10.1001/jamaoto.2015.1508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaczmar JM, Tan KS, Heitjan DF, et al. HPV-related oropharyngeal cancer: risk factors for treatment failure in patients managed with primary transoral robotic surgery. Head Neck 2016;38:59-65. https://doi.org/10.1002/hed.23850 10.1002/hed.23850 [DOI] [PubMed] [Google Scholar]


