Abstract
Purpose
Telepractice was extensively utilized during the COVID-19 pandemic. Little is known about issues experienced during the wide-scale rollout of a service delivery model that was novel to many. Social media research is a way to unobtrusively analyze public communication, including during a health crisis. We investigated the characteristics of tweets about telepractice through the lens of an established health technology implementation framework. Results can help guide efforts to support and sustain telehealth beyond the pandemic context.
Method
We retrieved a historical Twitter data set containing tweets about telepractice from the early months of the pandemic. Tweets were analyzed using a concurrent mixed-methods content analysis design informed by the nonadoption, abandonment, scale-up, spread, and sustainability (NASSS) framework.
Results
Approximately 2,200 Twitter posts were retrieved, and 820 original tweets were analyzed qualitatively. Volume of tweets about telepractice increased in the early months of the pandemic. The largest group of Twitter users tweeting about telepractice was a group of clinical professionals. Tweet content reflected many, but not all, domains of the NASSS framework.
Conclusions
Twitter posting about telepractice increased during the pandemic. Although many tweets represented topics expected in technology implementation, some represented phenomena were potentially unique to speech-language pathology. Certain technology implementation topics, notably sustainability, were not found in the data. Implications for future telepractice implementation and further research are discussed.
In early 2020, telepractice was thrust to the forefront of clinical practice globally as the COVID-19 pandemic unfolded. As typical service delivery settings were closed to avoid the community spread of the virus, clinical services transitioned online. Delivery of direct patient care remotely through telecommunications technology has long been a key service delivery model for disaster response (Bashshur & Shannon, 2009; Institute of Medicine, 2012; Lurie & Carr, 2018). Telerehabilitation specifically was suggested as a measure to avoid COVID-19 infection risk and/or continue rehabilitation for quarantined individuals (Koh & Hoenig, 2020). The pandemic necessitated sudden, unexpected, and widespread adoption and scale-up in the use of telepractice—the term adopted by the American Speech-Language-Hearing Association (ASHA, 2021b). Many speech-language pathologists (SLPs) found themselves delivering services via telehealth for the first time. Similarly, clients, their families, and organizations often faced expectations of rapid adjustment to the new service delivery model.
Little is currently known about how members of the public, clinicians, scientists, and organizations responded in real-time to the wide-scale adoption of telepractice during COVID-19. The abrupt and nationwide shift in service delivery presented a unique learning opportunity for researchers to discover the challenges and successes of implementing technology such as telepractice on a previously unseen scale (Bashshur et al., 2020). Telepractice is recognized by ASHA (2021b) as an appropriate service delivery model for SLPs, and systematic reviews continue to find promising evidence of efficacy in various disorder populations (Akemoglu et al., 2020; Sanchez et al., 2019; Weidner & Lowman, 2020). Prior to the pandemic, telepractice faced persistent barriers, such as lack of reimbursement, state licensure issues, lack of clinician training or training standards, clinician attitudes, technology access, and cost, all of which can affect telepractice program sustainability (Theodoros, 2011). It is uncertain whether gains in the field of telepractice in these areas will last beyond the pandemic. Insights from experiences gained during the pandemic may be used to clarify telepractice implementation barriers and prevent telepractice abandonment in the future. Exploring public opinions, attitudes, and experiences during a widespread telepractice deployment can be achieved through qualitative investigation. However, some traditional techniques, such as interviews or surveys, particularly those conducted in person, could put participants at risk during a pandemic. Even when conducted with safety precautions, traditional methods involving time-consuming interaction (e.g., in-depth interviewing) may place undue burden on clinicians in already strained health and educational settings.
As the pandemic evolved, individuals and organizations used social media as a method to ask questions, share experiences, and offer information or resources on health care topics. Many clients, families, clinicians, and researchers use social media to discuss topics related to communication sciences and disorders (Finn, 2019). Informal observation of social media platforms during the pandemic (browsing platforms such as Facebook and Twitter by the first and second authors) revealed organizations posting updates on telepractice reimbursement status, rehabilitation clinics advertising telepractice availability, and clinician groups offering suggestions on therapeutic activity ideas for the telepractice environment. ASHA and the National Foundation of Swallowing Disorders (NFOSD) started regularly tweeting resources for clinicians using telepractice; for example, the NFOSD provided a link to resources addressing telehealth dysphagia management during COVID-19 (NFOSD, 2020). During an unprecedented global event, a public conversation about telepractice occurred in the relatively natural environment of social media.
Social media posts can be a valuable source of data when monitoring the response to a significant, worldwide clinical situation. For example, researchers used Twitter during a past pandemic to monitor public conversation during major health events. During the 2009 H1N1 influenza pandemic, Chew and Eysenbach (2010) used Twitter data mining, a method they called “infoveillance,” to examine longitudinal patterns in knowledge translation and public attitudes about the virus. Specific to communication disorders, researchers have also used Twitter as a data source when examining public conversation about traumatic brain injury (Brunner et al., 2018), aphasia (Bryant et al., 2020), amyotrophic lateral sclerosis (Hemsley & Palmer, 2016), tinnitus (Deshpande et al., 2018; Ni et al., 2020), and language functioning in epilepsy (Dutta et al., 2018). Beyond using Twitter to monitor public conversation, communication disorders researchers may also explore how specific populations perceive Twitter and interact with the platform (Hemsley et al., 2018). Related disorders have also been examined in the Twitter environment, such as autism (Bellon-Harn et al., 2020) and dementia (Talbot et al., 2020). Researchers choose the Twitter platform due to the relatively public nature of tweets (Twitter, 2020) and Twitter's longstanding openness to the use of tweet data by academic researchers (van Dijck, 2013). Given this foundation, it is reasonable to assume a methodology similar to that of previous studies may be used to monitor the response of the communication sciences and disorders community to the implementation of telepractice during COVID-19.
The aim of this study was to evaluate the content of Twitter posts relevant to SLP telepractice during the beginning of the COVID-19 pandemic. Specifically, we were interested in how many tweets about telepractice were posted over time, which Twitter users were posting about telepractice (e.g., health care professionals, organizations, clients, or caregivers), and which components of health technology implementation were being discussed. We wished to determine how many tweets were about telepractice, who tweeted about telepractice, and what the relevant tweets contained.
Objectives
Analyze time-related patterns in telepractice tweets during the evolution of the COVID-19 pandemic and patterns across different user groups. We expect there will be an increase in Twitter post activity related to telepractice in the early stages of the COVID-19 pandemic.
Characterize tweets using pertinent telepractice hashtags and key words during the COVID-19 pandemic according to an established framework of health care technology implementation and scale-up.
Method
This study was approved as exempt human subjects research by the University of Kentucky Institutional Review Board. General ethical recommendations for social media research were followed, such as de-identification of user information and detailed consideration and compliance with social media platform terms and conditions (Ahmed et al., 2017; Beninger et al., 2014; Eysenbach & Till, 2001; Fiesler & Proferes, 2018).
The study applied a constructivist paradigm using content analysis to answer the research questions. We used the standards for reporting qualitative research tool to guide this report (O'Brien et al., 2014).
Keywords and Hashtag Determination
Tweets were retrieved via collaboration with faculty at the University of Kentucky Division of Biomedical Informatics. Faculty provided input into the technical methodology required to retrieve a comprehensive, yet relevant, sample of telepractice tweets and on the appropriate interpretation of tweet data and metadata. Prior to extracting tweets, hashtags and key words were determined through consensus among authors and initial manual searches on Twitter.com using the NVivo 12 NCapture plug-in (QSR International, n.d.). These initial searches were a modification of previously employed tweet retrieval methods in communication sciences and disorders research (Brunner et al., 2018). Researchers tested strings of key words and hashtags on the Twitter site until the largest set of tweets subjectively relevant to SLP telepractice were retrieved. Test searches on Twitter.com and application programming interface (API) queries suggested terms performed similarly in the search function whether entered as key words or hashtags. The final search query is listed in Table 1. The search was conducted by the sixth author under the supervision of the seventh author. We ensured comprehensiveness across search dates of interest by extracting data based on these terms through the Twitter historical search API (Twitter, 2021).
Table 1.
Query terms.
| (telehealth OR telepractice) AND (slp OR slpeeps OR speechtherapy OR “speech therapy”) |
Tweet Collection Method
Tweets were collected for a 4-month period (January 11, 2020, to May 11, 2020), corresponding to 2 months prior to and 2 months following March 11, the date at which COVID-19 was declared a pandemic (World Health Organization [WHO], 2020). We included all English language tweets that were relevant to the delivery of speech-language pathology services via telepractice. Tweets were extracted in JSON file format from the Twitter API, converted to CSV format, and stored in password-protected Excel files for analysis. Retweets and quote tweets were not included in the analysis. Chew and Eysenbach (2010), as an example, did not complete manual qualitative content analysis of retweets in efforts to avoid spam and popular posts saturating their sample.
We split and separately analyzed the 2 months prior to the pandemic (January 11, 2020, to March 10, 2020) and the 2 months following (March 11, 2020, to May 11, 2020) for patterns in tweet volume. Tweets were sorted into categories by the nonadoption, abandonment, scale-up, spread, and sustainability (NASSS) framework (Greenhalgh et al., 2017) and Twitter user types. Results were described by proportion of tweets in each category.
Qualitative Content Analysis
Deductive Content Analysis
Content analysis was chosen as a qualitative method to distill large amounts of information into predetermined, mutually exclusive, theory- and data-driven categories, known as deductive coding, to describe the body of data (Schreier, 2012). Categorizing large amounts of data is a reductive method. Our analysis was based on previously used qualitative content analysis methods to describe health-related tweets (Lee et al., 2014). However, our study is distinguished by the use of directed content analysis, in which the data are compared against an existing theoretical framework, in this case, the NASSS framework, to explore “supporting and nonsupporting evidence for a theory” (Hsieh & Shannon, 2005, p. 1282). Deductive content analysis is appropriate for testing existing theory, including whether existing theory adequately captures content in a situation distinct from its original context and comparing results across time (Elo & Kyngäs, 2008). In our study, our analysis is focused on testing whether tweets about telepractice are adequately captured by the NASSS framework, which was originally developed for health technology implementation in general.
NASSS Framework
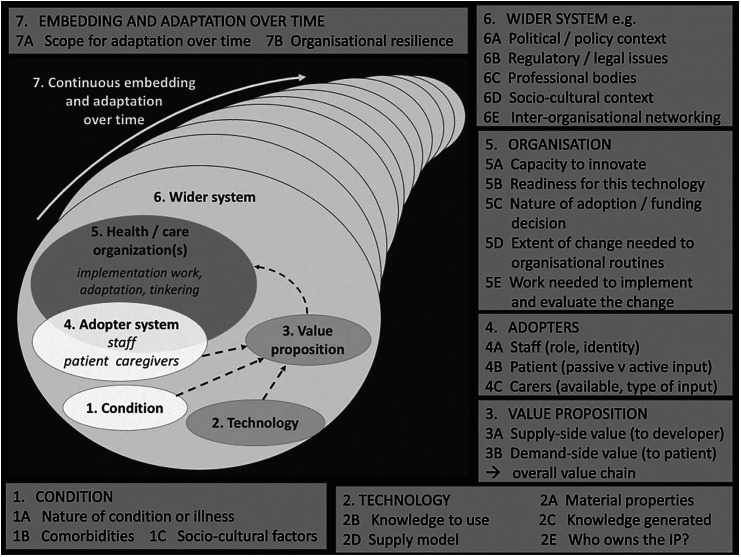
We chose the NASSS framework to compare how the content of telepractice conversations before and after the declaration of the COVID-19 pandemic may fit into an established health care technology implementation model. The NASSS framework considers the initial use and acceptance of health care technology, such as telepractice, and examines scale-up or more wide-scale use of the technology. Scale-up and spread were relevant considering the sudden nationwide use of telehealth during the pandemic. The NASSS framework also focuses on sustainability; it is unknown whether telepractice growth in the pandemic context will be sustained long term. Widespread adoption and sustainability of remote patient care initiatives in medicine historically have been problematic (Bashshur & Shannon, 2009; Bashshur et al., 2013; Wells & Lemak, 1996). An illustration of NASSS framework domains is provided in Figure 1.
Figure 1.
The nonadoption, abandonment, scale-up, spread, and sustainability framework (NASS). From Greenhalgh et al. (2018), used under Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/legalcode). Modified to black and white.
Coding Framework
We began the analysis of the Twitter data by sorting the tweets as those made before the declaration of the COVID-19 pandemic and afterward. Each of these groups of tweets were sorted by categories found within the NASSS framework and by user type. Tweets were coded with the use of a codebook according to qualitative content analysis procedures (Saldaña, 2016; Schreier, 2012). NASSS domain codes were pulled from the existing NASSS framework, and types of user codes were developed based on Lee et al. (2014). Where these codes were insufficient, the first author added data-driven categories to reflect the data set (e.g., “none” when content did not fit into a NASSS category, or modifications of Lee et al., 2014, user types to fit communication sciences and disorders populations vs. broad health-related populations).
Coding tweets. To be consistent in sorting tweets into the NASSS framework categories, we developed operational definitions. Table 2 provides the definitions and an example tweet. After the tweets were sorted, we identified themes within each category. We did not code for subcategories of NASSS domains, as we felt units of analysis (tweet content) typically did not provide enough detail to justify the level of granularity and demonstrated overlap between subcategories.
Table 2.
Nonadoption, abandonment, scale-up, spread, and sustainability (NASSS) framework domain definitions and example tweets.
| NASSS domain | Example | Example tweet content |
|---|---|---|
| 1. Condition | Focus on use of telepractice for a specific communication disorder, such as aphasia, social communication disorder, or Parkinson's disease | Check out this video demonstrating effective telepractice with individuals with motor speech disorders. |
| 2. Technology | General telehealth hardware or software, such as webcams, monitors, or videoconferencing programs | Does anyone use a wireless webcam for telepractice? Which one works best? |
| 3. Value proposition | Focus on the value of telepractice for patients, providers or clinics; evidence for the efficacy, effectiveness, and/or cost-effectiveness of telepractice | Here is a link to a summary of the research evidence on using telepractice in the school setting. |
| 4. Adopters | Experiences, adjustments, needs, and opinions of clinicians, patients, or caregivers; experience of or resistance to trying telehealth; clinician training needs or resources | We had our first day of delivering services via telepractice at work today. I'm exhausted but learned a lot. |
| 5. Organization | Organizational capacity for telepractice, workflow, routines and logistical concerns; developing private practice telepractice procedures | This webinar will help you adapt your private practice business routines to the new online format. |
| 6. Wider system | Reimbursement or policy change, regulatory issues (e.g., privacy and licensure), and professional bodies' (e.g., ASHA) response to telepractice | Call your state representative and ask them for support legislature to reimburse emergency telepractice services for kids. |
| 7. Adaptation/embedding over time | Sustainability of telepractice long term or postpandemic | (No tweets were found, but this category would involve addressing how current telepractice systems can be reinforced to continue into the future.) |
Note. ASHA = American Speech-Language-Hearing Association.
Twitter Users
We inserted each username associated with the extracted tweets to search each Twitter user's public biographical information manually and then sorted users into categories. User categories were defined by the Twitter categories developed in Lee et al. (2014), with modifications reflecting our data set; for example, the user category “health advocates” in their study of health professionals was unnecessary given our specific tweet sample. See Table 3 for the operational definitions of user types.
Table 3.
Twitter user types.
| User type | Description |
|---|---|
| Organization | Nonprofit organizations such as international, national, state or local associations, government, public schools, or universities |
| Public | Personal account and/or health care consumer |
| Business | Commercially oriented, typically for-profit groups or companies, including groups providing care such as private practices, hospitals, or clinics |
| Clinical professionals/personnel | Speech-language pathologists and related clinical or educational professionals or providers closely related to patient care |
| Unknown | No information in public bio or inadequate information to determine user type |
Coding of Data
The initial codebook was developed by the first author and tested on samples of about 100–200 tweets. During initial codebook development, the first author recorded category development procedures and reflexivity notes in a research journal. Category development decisions, which typically involved modification of NASSS categories to reflect SLP-specific content, were discussed between the first and second authors. Samples of tweets were coded with the codebook by two or more researchers independently, and the results were compared. To strengthen the coding frame, the research team engaged in discussion and consensus for their coding decisions. In the event of disagreement, coders provided their rationale and agreed upon a final code. When possible, based on coding decisions, further detail was added to the codebook to improve the consistency of subsequent ratings. “Double coding,” or multiple researchers independently coding the same information and comparing results to refine the coding frame, can help develop “an approximation of objectivity” (Schreier, 2012). A sample of 50 tweets was coded independently for user type by the first and fifth authors. A sample of 50 tweets was coded independently for NASSS domains by the first, fourth, and fifth authors. The final coding of tweets was completed for user type and NASSS domain by the fifth and first authors, respectively. Final analysis postcoding was completed by the first, second, and third authors and discussed with all authors.
Quantitative Content Analysis
We used the tweets posted prior to and after the COVID-19 pandemic was declared that were sorted by the NASSS framework and Twitter user type to quantitatively describe the data. Using these data, we calculated the proportion of tweets that fit into each of the NASSS framework before and after the pandemic and proportion of tweets by user type before and after the pandemic.
Results
A total of 2,276 tweets were retrieved using the Twitter historical API. Of these, 13.36% (304) were quote tweets (in which a user reposts another user's tweet with an added comment), 50.62% (1,152) were retweets, and 36.03% (820) were original tweets. All tweets were analyzed for general tweet volume patterns across time. In the content analysis, only original tweets were analyzed. Retweets and quote tweets were not analyzed. Six irrelevant tweets were removed; for example, irrelevant tweets referenced physical or occupational therapy services delivered via telehealth and did not mention speech-language pathology. When looking up user types, some users no longer had active profiles. Following Twitter developer terms and conditions, these data, a total of 21 tweets, were also removed. In total, 795 original tweets were used for content analysis.
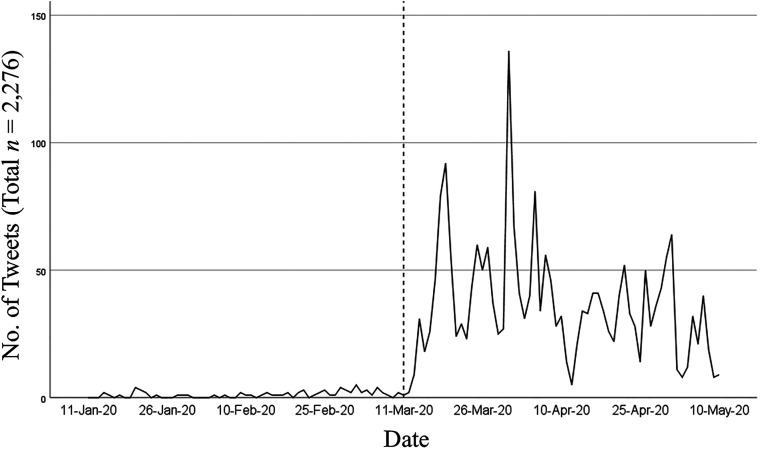
Tweet Volume
The 2,276 total tweets were distributed along the 4-month time sample as illustrated in Figure 2. March 11, 2020, the declaration of COVID-19 as a global pandemic, is demarcated with a dashed line in the graph's center. A marked increase in tweet volume is noted shortly after the public declaration of the pandemic, as was expected in our hypothesis. Of the 2,276 total tweets, 73 (3.21%) were posted in the 2 months prior to the declaration, and 2,203 (96.79%) were posted in the 2 months after. In our results, in addition to the increase in volume associated with the pandemic declaration, a relative spike in tweet volume can be noted on March 31, 2020. On this day, 136 relevant tweets were posted. This was the highest daily volume over the 4-month period. The spike appeared to be associated with (a) the release of new resources for clinicians and (b) a change in U.S. federal health policy on telehealth services provided by rehabilitation clinicians. Many tweets on March 31 referenced a Centers for Medicare & Medicaid Services' interim final rule release, which allowed rehabilitation codes to be billed for telehealth services in the setting of COVID-19 but excluded SLPs, physical therapists, and occupational therapists as eligible telehealth providers (American Occupational Therapy Association, 2020; American Physical Therapy Association, 2020; ASHA, 2020).
Figure 2.
Volume of tweets by time.
NASSS Framework Domain
The number and proportion of tweets by NASSS framework domain are provided in Table 4. Most of the tweets fit into one of the defined domains of the NASSS framework domains; however, nearly 20% of original tweets did not fall into any of the domains, as represented by the “none” category. Within the “none” category, clinicians repeatedly tweeted about the use of therapy materials in the online environment. Treatment materials include manipulatives, such as toys or books, or online activities, such as digital game boards or worksheets. These included sharing what worked and soliciting for ideas. “None” tweets also included tweets that generally promoted telehealth services, such as tweets encouraging the reader to take advantage of a discount, purchase a particular program, or schedule services at a particular clinic. About 6% of the tweets were coded as “unknown” due to inadequate information to make a category judgment. Tweets coded as “unknown” typically had text content of only a few words and a hyperlink.
Table 4.
Proportions of tweets by the nonadoption, abandonment, scale-up, spread, and sustainability framework domain.
| User type | Overall |
Pre–COVID-19 declaration
a
|
Post–COVID-19 declaration
b
|
|||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| 1. Condition | 24 | 3.02 | 0 | 0.0 | 24 | 3.25 |
| 2. Technology | 20 | 2.52 | 6 | 10.71 | 14 | 1.89 |
| 3. Value proposition | 39 | 4.91 | 2 | 3.57 | 37 | 5.01 |
| 4. Adopters | 263 | 33.08 | 15 | 26.79 | 248 | 33.56 |
| 5. Organization | 34 | 4.28 | 4 | 7.14 | 30 | 4.06 |
| 6. Wider system | 214 | 26.92 | 4 | 7.14 | 210 | 28.42 |
| 7. Adaptation/embedding over time | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| None | 152 | 19.12 | 14 | 25.00 | 138 | 18.67 |
| Unknown | 49 | 6.16 | 11 | 19.64 | 38 | 5.14 |
| Total | 795 | 56 | 739 | |||
January 11, 2020, to March 10, 2020.
March 11, 2020, to May 11, 2020.
Across the entire 4-month time period, no original tweets were found and eligible for analysis regarding “adaptation/embedding over time.” Although not a comparatively large proportion of tweets overall, we noted the emergence of tweets relevant to the condition NASSS domain after the pandemic declaration. These tweets referenced telepractice use with specific communication disorders or populations.
Tweets addressing “adopters”—the clients, family members, and clinicians adjusting to telepractice—remained relatively constant over time. Overall, the adopters domain was the most represented NASSS domain in our tweet sample. In our study, this referred to tweets detailing the experiences and needs of SLPs and families adjusting to remote service delivery. These individuals are considered the “adopters” of a new technology, such as telepractice, as they are the end users. Many tweets addressed training needs for clinicians transitioning to the digital environment, including webinars and online resources. Others described clients' and families' reactions to telepractice or suggested ways to ease the transition for them. Twitter users shared experiences managing barriers, such as distractions during sessions, scheduling changes, and the effort required to adapt to a new delivery method.
An increase was noted in “wider system”–related tweets. Content of these tweets appeared to revolve around reimbursement for remote rehabilitation services, whether requesting information, sharing information, or advocating for policy changes. About a quarter of tweets overall related to the wider system domain of the NASSS framework, which includes reimbursement and regulatory issues. Telepractice issues such as funding, privacy, and licensure have long existed but became critical as in-person facilities shut down in an effort to slow the spread of the virus. SLPs and related professionals, members of the public, and organizations all tweeted about this topic. Twitter users shared news about reimbursement changes or calls to advocacy at the federal or state level to improve reimbursement coverage.
Interestingly, we did not find a large percentage of tweets addressing the actual technology used to deliver telepractice services (second NASSS domain). Within NASSS framework categories, there did not appear to be consistent differences in text content before and after the pandemic declaration. For example, tweets detailing the features of a given telepractice technology were similar before and after March 11. Examples included features of common videoconferencing platforms or apps and computer hardware. As could be expected, COVID-19 was not frequently mentioned in tweets prior to March 11; coronavirus-related terminology began appearing in tweets a few days before the declaration. Additionally, postdeclaration tweets more often referred to the initiation of telepractice services (e.g., the idea of a “learning curve”).
Twitter Users
Number and proportion of tweets relevant to telepractice posted by Twitter user types prior to and after the declaration of the COVID-19 pandemic are listed in Table 5. Our results suggest that clinical professionals or personnel were the largest group of Twitter users tweeting about telepractice. SLPs and related professionals produced most tweets about telepractice prior to the declaration of the pandemic and just under half of tweets after. Increases in tweets from organizations and members of the public are noted. It should be noted that only 56 original tweets were retrieved and eligible for analysis in the 60-day period prior to the pandemic declaration, compared to 739 after.
Table 5.
Proportions of tweets by user types.
| User type | Overall |
Pre–COVID-19 declaration
a
|
Post–COVID-19 declaration
b
|
|||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Clinical professionals/personnel | 361 | 45.54 | 36 | 64.29 | 325 | 43.98 |
| Business | 210 | 26.42 | 15 | 26.79 | 195 | 26.39 |
| Organization | 128 | 16.10 | 4 | 7.14 | 124 | 16.78 |
| Unknown | 52 | 6.54 | 1 | 1.79 | 51 | 6.90 |
| Public | 44 | 5.53 | 0 | 0.00 | 44 | 5.95 |
| Total | 795 | 56 | 739 | |||
January 11, 2020, to March 10, 2020.
March 11, 2020, to May 11, 2020.
Discussion
Our hypothesis regarding tweet volume was supported. More Twitter activity surrounding SLP telepractice was found following the WHO declaration of the COVID-19 pandemic. We found a clear increase in overall tweets about telepractice in the early stages of the pandemic. We expected relevant tweets may increase after the pandemic declaration based on extrapolation from non–speech-language pathology results during a previous pandemic. During the 2009 H1N1 influenza pandemic, researchers investigating more general health-related topics noted a tweet volume increase in response to the WHO declaration of a pandemic (Chew & Eysenbach, 2010; WHO, 2009). Twitter discussion of telepractice also followed this trend. We also observed an increase in tweets associated with a reimbursement-related news release in late March. Although detailed analysis of tweet text is beyond this article's scope, Twitter users tweeting about telepractice, the largest group of whom were clinical professionals, appeared to use the platform most to discuss the experiences, management, and training of themselves and clients and communicate regarding reimbursement and regulatory concerns. The relative abundance of tweets by clinical professionals reflects findings of previous research. In our study, clinical professionals were the largest group of tweeters, similar to that of Bryant et al. (2020).
Given that social media highlights the voice of the individual, it is perhaps unsurprising that so many tweets involved telepractice end users, that is, the clients, families, and clinicians, as opposed to NASSS domains focused on changes in business routine or organizational procedures. The clinician experience is important to wide-scale telepractice implementation. Researchers in Australia found clinician acceptance to be the most important component in sustainable remote service delivery, although application of this finding to telepractice and to the U.S. health care system is yet to be seen (Wade et al., 2014).
Many tweets shared news or reactions to the multiple relevant policy changes enacted by the U.S. Centers for Medicare & Medicaid Services during this time period. Interestingly, only about 7% of tweets addressed this domain prior to the pandemic declaration, increasing to about 28% postdeclaration. It is unknown if and how reimbursement and regulatory changes enacted during the pandemic will be reversed as it recedes or continue to be a major barrier toward telepractice adoption. Given Twitter's public nature, hashtags' suitability for facilitating message spread and engagement, and the many political leaders and organizations utilizing Twitter, this platform may be an important venue for advocacy by clinicians and individuals with communication disorders (Hemsley et al., 2015; Parmelee & Bichard, 2012; Saxton et al., 2015).
Original tweets about telepractice and specific conditions began to appear only after the declaration of the pandemic. Telepractice research evidence often focuses on specific population groups or communication disorders (Regina Molini-Avejonas et al., 2015). Existing expert telerehabilitation guidelines suggest clinicians determine each client's candidacy for remote service delivery individually (Brennan et al., 2011). Different communication disorders and associated impairments affect candidacy for telepractice or modification of telepractice delivery (Cason & Cohn, 2014). It is largely unknown how clinicians determined candidacy or managed the variety of communication disorders in the pandemic environment. In the future of telepractice, it will be crucial to consider differences among disorders and client characteristics in determining whether telepractice can be an effective and ethical service delivery option for the individual.
Unclassified tweets about the use of therapy materials and manipulatives in the online environment, such as toys and books, or digital game boards and worksheets were common. Users often tweeted about what activities worked and clients enjoyed, or tweeted to elicit recommendations for telepractice treatment materials. It is unknown whether an equivalent counterpart to this topic exists in other fields of remote direct service delivery, such as medicine or counseling. The need to take treatment materials and manipulatives into account could be a unique component of telepractice and telerehabilitation, which could translate into an uninvestigated barrier/facilitator. Tweets coded as “none” also included promotions and marketing of services. We did not feel that promotional content was included in NASSS domains. It was, however, important to reflect this content in order to portray the reality of commercial interests found among the resources and information shared on social media platforms. Consumers of social media content, such as clinicians or individuals with communication disorders, may not always be able to distinguish between free or paid resources or between evidence-based and unreliable information. Conflicts of interest, potentially present in such tweets, may not be easily identifiable for clinicians or clients using Twitter (Lee et al., 2014). Deshpande et al. (2018) raised similar concerns specific to misinformation about products curing tinnitus on Twitter.
None of our retrieved original tweets were interpreted as addressing sustainability issues per the NASSS framework. In the NASSS framework, this domain is “adaptation/embedding over time.” This absence may be related to the pandemic's emergent nature, as clinicians and organizations manage immediate telehealth implementation needs. However, the NASSS model suggests that successful implementation of any health care technology requires planning for sustainability and technology adaptation over time. Telehealth projects historically have faced barriers to sustainability beyond initial pilot programs (Bashshur & Shannon, 2009). Our results may have been different had we analyzed a time period later in the pandemic's development, but the need for sustainability planning is no less important. Postpandemic telehealth sustainability is beginning to be addressed in the literature (Bashshur et al., 2020; Thomas et al., 2020). By discussing potential issues now, SLPs can help lead a successful transition to the long-term implementation of telepractice. This highlights a potential area of inquiry in our profession.
Qualitative research is contextual. SLPs and other groups or individuals likely communicate differently about telepractice in settings other than social media. Compared to the U.S. population in general, Twitter users are younger, are more educated, and have higher incomes (Pew Research Center, 2019). Social media, as a channel, serves a different purpose than other communication contexts. Telepractice discussions held in an academic setting, a private professional forum, an outpatient clinic, or a professional development course likely look different. The NASSS model may be represented differently across these settings. Furthermore, multiple contexts are present within social media, as communication behaviors and communication purposes differ across platforms and users (Beninger et al., 2014; McCay-Peet & Quan-Haase, 2017). This is not indicative of a weakness of qualitative study, but rather of a phenomenon separate from telepractice implementation: how clinician communication differs contextually. We chose social media as an accessible, relatively naturalistic context. Each qualitative researcher brings personal characteristics to their interpretation of data; the author who developed the codebook is a Twitter user with research interests in telepractice. Further studies on telepractice implementation communication behavior or the differences between SLP or public communication across contexts are encouraged by multiple researchers with different perspectives. Studies on social media platforms paired with other qualitative methodology, such as interviewing, focus groups, or surveys, may allow for more in-depth analysis of implementation phenomena.
The NASSS framework, which we used to organize our analysis, was developed for health technology in health care settings. Only about 40% of SLPs work in health care (ASHA, 2021a). This could affect the utility and validity of using such a framework to examine SLP implementation of telepractice in educational, private practice, or other settings. We did not differentiate Twitter users by educational or health care practice setting status (see Table 3), so we are unable to complete subgroup analysis, which could identify whether this affected framework applicability. However, the NASSS framework has good face validity for clinicians working in educational settings, as many identical implementation issues likely apply. Further research may clarify whether a different framework could better capture the diverse environments of SLP practice.
Future research may address a variety of issues and questions raised in our study. However, technical methodology can be extended or may require adaptation for researchers wishing to replicate or expand the project. This project utilized the Twitter historical API to retrieve tweets during a defined time period. Although this ultimately provided a comprehensive sample and we conducted preliminary key word searches before querying the API, we could have missed relevant hashtags or key words. As we coded tweets individually by hand, researcher time limitations restricted the time period (and consequently the number of tweets), which was searched and analyzed. A few months after data were retrieved, Twitter began to launch a new API version (Cairns & Shetty, 2020). This relates to one of the inherent issues with replicability in social media research; researchers intending to replicate our data set with an identical search strategy may retrieve different results given posts and/or profiles may be hidden or deleted at any time (Wheeler, 2018). We did not qualitatively analyze quote tweets and retweets. Future research may more comprehensively analyze tweet content; expand the content analysis to include quote tweets, retweets, likes, or other metrics of tweet reach and impact; extend the time frame analyzed to examine patterns beyond the initial months of the pandemic; or explore groups of Twitter users discussing telepractice through social network analysis.
Conclusions
Twitter is a platform that can be used to observe public and health care professional behavior during the pandemic. Overall, tweet activity about telepractice increased in response to the declaration of the global COVID-19 pandemic. Examination of SLP telepractice tweets during the early COVID-19 pandemic revealed posts by SLPs, related professionals, organizations, businesses, and members of the public. Tweet content covered many topics expected when considered in the perspective of a general health technology implementation framework, particularly in policy issues, such as reimbursement or regulation, but lacked content addressing telepractice sustainability over time. Telepractice program sustainability may be an important area of focus in future research and practice. Tweet content also revealed some potentially meaningful patterns not addressed by the existing theoretical framework, such as issues generating or adapting speech-language pathology treatment materials for the online environment. Further research is needed to examine discussions of telepractice over time in communities or contexts beyond social media.
Acknowledgments
R. Kavuluru's involvement in this project was supported by U.S. National Cancer Institute through Grant R21CA218231. The remaining authors received no financial support for the research, authorship, and/or publication of this article.
Funding Statement
R. Kavuluru's involvement in this project was supported by U.S. National Cancer Institute through Grant R21CA218231.
References
- Ahmed, W. , Bath, P. A. , & Demartini, G. (2017). Chapter 4: Using Twitter as a data source: An overview of ethical, legal and methodological challenges. In Woodfield K. (Ed.), The ethics of online research (Vol. 2, pp. 79–107). Emerald. https://doi.org/10.1108/S2398-601820180000002004 [Google Scholar]
- Akemoglu, Y. , Muharib, R. , & Meadan, H. (2020). A systematic and quality review of parent-implemented language and communication interventions conducted via telepractice. Journal of Behavioral Education, 29(2), 282–316. https://doi.org/10.1007/s10864-019-09356-3 [Google Scholar]
- American Occupational Therapy Association. (2020). Sweeping CMS coronavirus regulatory notice: CMS expands telephone assessments and virtual check-ins to therapy, AOTA fights for telehealth reimbursement. https://www.aota.org/Advocacy-Policy/Federal-Reg-Affairs/News/2020/CMS-Interim-Final-Rule-Analysis.aspx
- American Physical Therapy Association. (2020). New CMS rule includes therapy codes in telehealth, stops short of allowing PTs to conduct telehealth services. https://www.apta.org/news/2020/03/31/new-cms-rule-includes-therapy-codes-in-telehealth-stops-short-of-allowing-pts-to-conduct-telehealth-services
- American Speech-Language-Hearing Association. (2020). ASHA continues seeking Medicare telepractice authority; Interim final rule insufficient. https://www.asha.org/News/2020/ASHA-Continues-Seeking-Medicare-Telepractice-Authority/
- American Speech-Language-Hearing Association. (2021a). Employment settings for SLPs. https://www.asha.org/students/employment-settings-for-slps/
- American Speech-Language-Hearing Association. (2021b). Telepractice. https://www.asha.org/Practice-Portal/Professional-Issues/Telepractice/
- Bashshur, R. , Doarn, C. R. , Frenk, J. M. , Kvedar, J. C. , & Woolliscroft, J. O. (2020). Telemedicine and the COVID-19 pandemic, lessons for the future. Telemedicine and e-Health, 26(5), 571–573. https://doi.org/10.1089/tmj.2020.29040.rb [DOI] [PubMed] [Google Scholar]
- Bashshur, R. , & Shannon, G. W. (2009). History of telemedicine: Evolution, context, and transformation. Mary Ann Liebert. [Google Scholar]
- Bashshur, R. L. , Shannon, G. , Krupinski, E. A. , & Grigsby, J. (2013). Sustaining and realizing the promise of telemedicine. Telemedicine and e-Health, 19(5), 339–345. https://doi.org/10.1089/tmj.2012.0282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellon-Harn, M. L. , Ni, J. , & Manchaiah, V. (2020). Twitter usage about autism spectrum disorder. Autism, 24(7), 1805–1816. https://doi.org/10.1177/1362361320923173 [DOI] [PubMed] [Google Scholar]
- Beninger, K. , Fry, A. , Jago, N. , Lepps, H. , Nass, L. , & Silvester, H. (2014). Research using social media: User's views. NatCen Social Research, 1–40. http://www.natcen.ac.uk/media/282288/p0639-research-using-social-media-report-final-190214.pdf [Google Scholar]
- Brennan, D. M. , Tindall, L. , Theodoros, D. , Brown, J. , Campbell, M. , Christiana, D. , Smith, D. , Cason, J. , & Lee, A. (2011). A blueprint for telerehabilitation guidelines. Telemedicine and e-Health, 2(2), 31–34. https://doi.org/10.5195/ijt.2010.6063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunner, M. , Hemsley, B. , Dann, S. , Togher, L. , & Palmer, S. (2018). Hashtag #TBI: A content and network data analysis of tweets about traumatic brain injury. Brain Injury, 32(1), 49–63. https://doi.org/10.1080/02699052.2017.1403047 [DOI] [PubMed] [Google Scholar]
- Bryant, L. , Brunner, M. , Power, E. , & Hemsley, B. (2020). Content and network analysis of tweets tagged with #aphasia: An emergent community of practice. Aphasiology, 1–19. https://doi.org/10.1080/02687038.2020.1770195 [Google Scholar]
- Cairns, I. , & Shetty, P. (2020). Introducing a new and improved Twitter API. https://blog.twitter.com/developer/en_us/topics/tools/2020/introducing_new_twitter_api.html
- Cason, J. , & Cohn, E. R. (2014). Telepractice: An overview and best practices. SIG 12 Perspectives on Augmentative and Alternative Communication, 23(1), 4–17. https://doi.org/10.1044/aac23.1.4 [Google Scholar]
- Chew, C. , & Eysenbach, G. (2010). Pandemics in the age of Twitter: Content analysis of tweets during the 2009 H1N1 outbreak. PLOS ONE, 5(11), Article e14118. https://doi.org/10.1371/journal.pone.0014118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deshpande, A. K. , Deshpande, S. B. , & O'Brien, C. (2018). A study of social media utilization by individuals with tinnitus. American Journal of Audiology, 27(4), 559–569. https://doi.org/10.1044/2018_aja-18-0033 [DOI] [PubMed] [Google Scholar]
- Dutta, M. , Murray, L. , Miller, W. , & Groves, D. (2018). Effects of epilepsy on language functions: Scoping review and data mining findings. American Journal of Speech-Language Pathology, 27(1S), 350–378. https://doi.org/10.1044/2017_AJSLP-16-0195 [DOI] [PubMed] [Google Scholar]
- Elo, S. , & Kyngäs, H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. https://doi.org/10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- Eysenbach, G. , & Till, J. E. (2001). Ethical issues in qualitative research on Internet communities. BMJ, 323, 1103–1105. https://doi.org/10.1136/bmj.323.7321.1103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiesler, C. , & Proferes, N. (2018). “Participant” perceptions of Twitter research ethics. Social Media + Society, 4(1), 1–14. https://doi.org/10.1177/2056305118763366 [Google Scholar]
- Finn, P. (2019). The impact of social media on communication sciences and disorders: A need for examination and research. Perspectives of the ASHA Special Interest Groups, 4(2), 224–227. https://doi.org/10.1044/2019_PERS-ST-2019-0001 [Google Scholar]
- Greenhalgh, T. , Wherton, J. , Papoutsi, C. , Lynch, J. , Hughes, G. , Hinder, S. , A'Court, C. , Hinder, H. , Procter, R. , & Shaw, S. (2018). Analysing the role of complexity in explaining the fortunes of technology programmes: Empirical application of the NASSS framework. BMC Medicine, 16(1), 66. https://doi.org/10.1186/s12916-018-1050-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh, T. , Wherton, J. , Papoutsi, C. , Lynch, J. , Hughes, G. , Hinder, S. , Fahy, N. , Procter, R. , & Shaw, S. (2017). Beyond adoption: A new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. Journal of Medical Internet Research, 19(11), Article e367. https://doi.org/10.2196/jmir.8775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemsley, B. , Dann, S. , Palmer, S. , Allan, M. , & Balandin, S. (2015). “We definitely need an audience”: Experiences of Twitter, Twitter networks and tweet content in adults with severe communication disabilities who use augmentative and alternative communication (AAC). Disability and Rehabilitation, 37(17), 1531–1542. https://doi.org/10.3109/09638288.2015.1045990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemsley, B. , Palmer, S. , Dann, S. , & Balandin, S. (2018). Using Twitter to access the human right of communication for people who use augmentative and alternative communication (AAC). International Journal of Speech-Language Pathology, 20(1), 50–58. https://doi.org/10.1080/17549507.2017.1413137 [DOI] [PubMed] [Google Scholar]
- Hemsley, B. , & Palmer, S. R. (2016). Two studies on Twitter networks and tweet content in relation to amyotrophic lateral sclerosis (ALS): Conversation, information, and “diary of a daily life”. In Georgiou A., Schaper L. K., & Whetton S. (Eds.), Digital health innovation for consumers, clinicians, connectivity and community: Selected papers from the 24th Australian National Health Informatics Conference (HIC 2016) (pp. 41–47). IOS Press. https://doi.org/10.3233/978-1-61499-666-8-41 [PubMed] [Google Scholar]
- Hsieh, H. F. , & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. https://doi.org/10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2012). The role of telehealth in an evolving health care environment: Workshop summary. The National Academies Press. https://doi.org/10.17226/13466 [PubMed] [Google Scholar]
- Koh, G. C. , & Hoenig, H. (2020). How should the rehabilitation community prepare for 2019-nCoV? Archives of Physical Medicine and Rehabilitation, 101(6), 1068–1071. https://doi.org/10.1016/j.apmr.2020.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, J. L. , DeCamp, M. , Dredze, M. , Chisolm, M. S. , & Berger, Z. D. (2014). What are health-related users tweeting? A qualitative content analysis of health-related users and their messages on Twitter. Journal of Medical Internet Research, 16(10), Article e237. https://doi.org/10.2196/jmir.3765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie, N. , & Carr, B. G. (2018). The role of telehealth in the medical response to disasters. JAMA Internal Medicine, 178(6), 745–746. https://doi.org/10.1001/jamainternmed.2018.1314 [DOI] [PubMed] [Google Scholar]
- McCay-Peet, L. , & Quan-Haase, A. (2017). What is social media and what questions can social media research help us answer? In Sloan L. & Quan-Haase A. (Eds.), The SAGE handbook of social media research methods (pp. 13–26). Sage. https://doi.org/10.4135/9781473983847 [Google Scholar]
- National Foundation of Swallowing Disorders. (2020). An excellent resource on telehealth recommendations for dysphagia management during COVID-19 from the @PurdueIEaTLab #SLP #MedSLP #telehealth #dysphagia #speechpathology #speechlanguagepathology #acuteSLP #rehabSLP #SNFslp #IPRslp #HHSLP. Twitter. https://twitter.com/NFOSD/status/1255936477676146691 [Google Scholar]
- Ni, J. , Bellon-Harn, M. L. , Zhang, J. , Li, Y. , & Manchaiah, V. (2020). Twitter usage using common reference to tinnitus. American Journal of Audiology, 29(2), 206–217. https://doi.org/10.1044/2020_AJA-19-00055 [DOI] [PubMed] [Google Scholar]
- O'Brien, B. C. , Harris, I. B. , Beckman, T. J. , Reed, D. A. , & Cook, D. A. (2014). Standards for reporting qualitative research: A synthesis of recommendations. Academic Medicine, 89(9), 1245–1251. https://doi.org/10.1097/acm.0000000000000388 [DOI] [PubMed] [Google Scholar]
- Parmelee, J. H. , & Bichard, S. L. (2012). Politics and the Twitter revolution: How tweets influence the relationship between political leaders and the public. Lexington Books. [Google Scholar]
- Pew Research Center. (2019). Sizing up Twitter users. https://www.pewresearch.org/internet/wp-content/uploads/sites/9/2019/04/twitter_opinions_4_18_final_clean.pdf
- QSR International. (n.d.). NCapture. https://help-nv.qsrinternational.com/12/win/v12.1.97-d3ea61/Content/ncapture/ncapture.htm
- Regina Molini-Avejonas, D. , Rondon-Melo, S. , de La Higuera Amato, C. A. , & Samelli, A. G. (2015). A systematic review of the use of telehealth in speech, language and hearing sciences. Journal of Telemedicine and Telecare, 21(7), 367–376. https://doi.org/10.1177/1357633x15583215 [DOI] [PubMed] [Google Scholar]
- Saldaña, J. (2016). The coding manual for qualitative researchers. Sage. [Google Scholar]
- Sanchez, D. , Reiner, J. F. , Sadlon, R. , Price, O. A. , & Long, M. W. (2019). Systematic review of school telehealth evaluations. The Journal of School Nursing, 35(1), 61–76. https://doi.org/10.1177/1059840518817870 [DOI] [PubMed] [Google Scholar]
- Saxton, G. D. , Niyirora, J. N. , Guo, C. , & Waters, R. D. (2015). #AdvocatingForChange: The strategic use of hashtags in social media advocacy. Advances in Social Work, 16(1), 154–169. https://doi.org/10.18060/17952 [Google Scholar]
- Schreier, M. (2012). Qualitative content analysis in practice. Sage. [Google Scholar]
- Talbot, C. , O'Dwyer, S. , Clare, L. , Heaton, J. , & Anderson, J. (2020). Identifying people with dementia on Twitter. Dementia, 19(4), 965–974. https://doi.org/10.1177/1471301218792122 [DOI] [PubMed] [Google Scholar]
- Theodoros, D. (2011). Telepractice in speech-language pathology: The evidence, the challenges, and the future. SIG 18 Perspectives on Telepractice, 1(1), 10–21. https://doi.org/10.1044/tele1.1.10 [Google Scholar]
- Thomas, E. E. , Haydon, H. M. , Mehrotra, A. , Caffery, L. J. , Snoswell, C. L. , Banbury, A. , & Smith, A. C. (2020). Building on the momentum: Sustaining telehealth beyond COVID-19. Journal of Telemedicine and Telecare. Advance online publication. https://doi.org/10.1177/1357633X20960638 [DOI] [PubMed] [Google Scholar]
- Twitter. (2020). Twitter user agreement. https://cdn.cms-twdigitalassets.com/content/dam/legal-twitter/site-assets/tos-oct-14th-2020/Twitter_User_Agreement_EN.pdf
- Twitter. (2021). Twitter's search endpoints. https://developer.twitter.com/en/docs/twitter-api/search-overview
- van Dijck, J. (2013). The culture of connectivity: A critical history of social media. Oxford University Press. https://doi.org/10.1093/acprof:oso/9780199970773.001.0001 [Google Scholar]
- Wade, V. A. , Eliott, J. A. , & Hiller, J. E. (2014). Clinician acceptance is the key factor for sustainable telehealth services. Qualitative Health Research, 24(5), 682–694. https://doi.org/10.1177/1049732314528809 [DOI] [PubMed] [Google Scholar]
- Weidner, K. , & Lowman, J. (2020). Telepractice for adult speech-language pathology services: A systematic review. Perspectives of the ASHA Special Interest Groups, 5(1), 326–338. https://doi.org/10.1044/2019_PERSP-19-00146 [Google Scholar]
- Wells, R. S. , & Lemak, C. H. (1996). Beyond adoption to sustained use: Telemedicine for rural communities. Telemedicine Journal, 2(4), 285–293. https://doi.org/10.1089/tmj.1.1996.2.285 [DOI] [PubMed] [Google Scholar]
- Wheeler, J. (2018). Mining the first 100 days: Human and data ethics in Twitter research. Journal of Librarianship and Scholarly Communication, 6(2), Article eP2235. http://doi.org/10.7710/2162-3309.2235 [Google Scholar]
- World Health Organization. (2009). World now at the start of 2009 influenza pandemic. https://www.who.int/mediacentre/news/statements/2009/h1n1_pandemic_phase6_20090611/en/
- World Health Organization. (2020). WHO Director-General's opening remarks at the media briefing on COVID-19. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020