Abstract
Background
Pulmonary hypertension (PH) is an important cause of morbidity and mortality, which leads to a substantial loss of exercise capacity. PH ultimately leads to right ventricular overload and subsequent heart failure and early death. Although early detection and treatment of PH are recommended, due to the limited responsiveness to therapy at late disease stages, many patients are diagnosed at a later stage of the disease because symptoms and signs of PH are nonspecific at earlier stages. While direct pressure measurement with right‐heart catheterisation is the clinical reference standard for PH, it is not routinely used due to its invasiveness and complications. Trans‐thoracic Doppler echocardiography is less invasive, less expensive, and widely available compared to right‐heart catheterisation; it is therefore recommended that echocardiography be used as an initial diagnosis method in guidelines. However, several studies have questioned the accuracy of noninvasively measured pulmonary artery pressure. There is substantial uncertainty about the diagnostic accuracy of echocardiography for the diagnosis of PH.
Objectives
To determine the diagnostic accuracy of trans‐thoracic Doppler echocardiography for detecting PH.
Search methods
We searched MEDLINE, Embase, Web of Science Core Collection, ClinicalTrials.gov, World Health Organization International Clinical Trials Registry Platform from database inception to August 2021, reference lists of articles, and contacted study authors. We applied no restrictions on language or type of publication.
Selection criteria
We included studies that evaluated the diagnostic accuracy of trans‐thoracic Doppler echocardiography for detecting PH, where right‐heart catheterisation was the reference standard. We excluded diagnostic case‐control studies (two‐gate design), studies where right‐heart catheterisation was not the reference standard, and those in which the reference standard threshold differed from 25 mmHg. We also excluded studies that did not provide sufficient diagnostic test accuracy data (true‐positive [TP], false‐positive [FP], true‐negative [TN], and false‐negative [FN] values, based on the reference standard). We included studies that provided data from which we could extract TP, FP, TN, and FN values, based on the reference standard. Two authors independently screened and assessed the eligibility based on the titles and abstracts of records identified by the search. After the title and abstract screening, the full‐text reports of all potentially eligible studies were obtained, and two authors independently assessed the eligibility of the full‐text reports.
Data collection and analysis
Two review authors independently assessed the risk of bias and extracted data from each of the included studies. We contacted the authors of the included studies to obtain missing data. We assessed the methodological quality of studies using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS‐2) tool. We estimated a summary receiver operating characteristic (SROC) curve by fitting a hierarchical summary ROC (HSROC) non‐linear mixed model. We explored sources of heterogeneity regarding types of PH, methods to estimate the right atrial pressure, and threshold of index test to diagnose PH. All analyses were performed using the Review Manager 5, SAS and STATA statistical software.
Main results
We included 17 studies (comprising 3656 adult patients) assessing the diagnostic accuracy of Doppler trans‐thoracic echocardiography for the diagnosis of PH. The included studies were heterogeneous in terms of patient distribution of age, sex, WHO classification, setting, country, positivity threshold, and year of publication. The prevalence of PH reported in the included studies varied widely (from 6% to 88%). The threshold of index test for PH diagnosis varied widely (from 30 mmHg to 47 mmHg) and was not always prespecified. No study was assigned low risk of bias or low concern in each QUADAS‐2 domain assessed. Poor reporting, especially in the index test and reference standard domains, hampered conclusive judgement about the risk of bias. There was little consistency in the thresholds used in the included studies; therefore, common thresholds contained very sparse data, which prevented us from calculating summary points of accuracy estimates. With a fixed specificity of 86% (the median specificity), the estimated sensitivity derived from the median value of specificity using HSROC model was 87% (95% confidence interval [CI]: 78% to 96%). Using a prevalence of PH of 68%, which was the median among the included studies conducted mainly in tertiary hospitals, diagnosing a cohort of 1000 adult patients under suspicion of PH would result in 88 patients being undiagnosed with PH (false negatives) and 275 patients would avoid unnecessary referral for a right‐heart catheterisation (true negatives). In addition, 592 of 1000 patients would receive an appropriate and timely referral for a right‐heart catheterisation (true positives), while 45 patients would be wrongly considered to have PH (false positives). Conversely, when we assumed low prevalence of PH (10%), as in the case of preoperative examinations for liver transplantation, the number of false negatives and false positives would be 13 and 126, respectively.
Authors' conclusions
Our evidence assessment of echocardiography for the diagnosis of PH in adult patients revealed several limitations. We were unable to determine the average sensitivity and specificity at any particular index test threshold and to explain the observed variability in results. The high heterogeneity of the collected data and the poor methodological quality would constrain the implementation of this result into clinical practice. Further studies relative to the accuracy of Doppler trans‐thoracic echocardiography for the diagnosis of PH in adults, that apply a rigorous methodology for conducting diagnostic test accuracy studies, are needed.
Keywords: Adult; Humans; Echocardiography; Echocardiography, Doppler; Hypertension, Pulmonary; Hypertension, Pulmonary/diagnostic imaging; Physical Examination; Physical Examination/methods; Sensitivity and Specificity
Plain language summary
Doppler trans‐thoracic echocardiography for detection of pulmonary hypertension in adults
What was studied in this review?
Pulmonary hypertension is high blood pressure in the blood vessels that supply blood from the right half of the heart to the lungs. It is a serious condition that can damage the right side of the heart. The walls in the blood vessels become thick and stiff which makes it harder for the blood to flow. This can lead to heart failure. Symptoms can include shortness of breath, tiredness, chest pain, a racing heartbeat or swelling in the lower limbs and abdomen.
The symptoms can be similar to other heart and lung diseases, so diagnosis can take time. Early diagnosis is beneficial because treatment can start early. Starting treatment early is better because people respond better to treatment in the early stages of the disease. Not being diagnosed early can have severe consequences such as disability in daily life or death.
The most accurate way to diagnose pulmonary hypertension is using a pressure measurement called right‐heart catheterisation. However, this is invasive and can cause complications. Another technique, called Doppler echocardiography is noninvasive, cheaper and more widely available in hospitals. Therefore, many guidelines recommend the use of echocardiography as an initial diagnosis method. We wanted to do this review because several studies have questioned the accuracy of echocardiography. We wanted to find out how good echocardiography is compared to right‐heart catheterisation for the diagnosis of pulmonary hypertension.
What was the aim of this review?
To evaluate evidence on the ability of echocardiography to identify pulmonary hypertension in adults compared to right‐heart catheterisation.
What were the main results of the review?
We found 17 studies involving 3656 people who had suspected pulmonary hypertension.
There was a lot of variation in the studies. We found the characteristics of participants varied in terms of age, sex, cause of pulmonary hypertension, setting and country. The cut‐off values for the echocardiography readings chosen to diagnose pulmonary hypertension also varied. We used the available data to estimate how well the echocardiography performed compared to right‐heart catheterisation. In tertiary care hospitals, where most of the included studies were conducted, it is assumed that 680 of 1000 patients have pulmonary hypertension. We found that 592 people of 1000 would be correctly diagnosed with pulmonary hypertension using echocardiography. But 45 of 1000 patients would be wrongly considered as having pulmonary hypertension (false positive), while 88 of 1000 patients might be incorrectly considered as not having pulmonary hypertension (false negative) and 275 of 1000 patients would avoid unnecessary referral for a right‐heart catheterisation. In a scenario where the preoperative examination for liver transplantation is conducted, 100 of 1000 are assumed to have pulmonary hypertension. We found the number of false negatives and false positives would be 13 and 126, respectively.
How reliable were the results of the studies?
We judged the included studies to have important limitations in their validity, which means that they were at high risk of providing distorted results. Therefore, we cannot be certain if the number of false negatives is correct (i.e. it could be even higher).
Who do the results of this review apply to?
These results apply to adults who are suspected of having pulmonary hypertension. However, the diagnostic accuracy of echocardiography varied considerably among studies and it is yet unclear what causes this diversity of test accuracy. Of note, the results are from studies conducted in relatively high prevalence settings. Therefore, care should be taken when applying this result to individual situations.
How up‐to‐date was the review?
This review is current to August 2021.
Summary of findings
Summary of findings 1. Summary of Findings: Doppler trans‐thoracic echocardiography for detection of pulmonary hypertension in adults.
| Patients/population | Adults with suspected pulmonary hypertension | ||||||
| Settings | High‐prevalence settings: tertiary care hospitals including university hospitals or cardiopulmonary centres Low‐prevalence settings: preoperative examinations for liver transplantation |
||||||
| Index test | Systolic pulmonary arterial pressure calculated from the maximum tricuspid regurgitation jet velocity by using the modified Bernoulli equation and adding right atrial pressure by Doppler trans‐thoracic echocardiography | ||||||
| Reference standard | Mean of pulmonary arterial pressure of 25 mmHg or greater assessed by right‐heart catheterisation | ||||||
| Study designs | Prospective or retrospective cohorts and cross‐sectional studies. We excluded case reports and studies of case‐control design. | ||||||
| .Findings | |||||||
| Evaluations (studies) |
No. of participants | Comfirmed PH participants | Median sensitivity (IQR) [range] |
Median specificity (IQR) [range] |
|||
| 17 | 3656 | 1342 | 87% (81 to 92%) [40 to 98%] |
86% (79% to 91%) [33 to 100%] |
|||
| Index test | Prevalence1 | No. of participants (studies) | Sensitivity (under fixed specificity of 86%)2 | Specificity (fixed) 3 | Numbers of false positives out of 1000 patients | Numbers of false negatives out of 1000 patients | Quality and Comments |
| Systolic pulmonary arterial pressure by echocardiography | 10% | 3656 (17) | 87% (95% CI 78% to 96%) | 86% | 126 | 13 | No study was assigned low risk of bias or low concern in all QUADAS‐2 domains. Poor reporting, especially in the WHO classification of PH, the index test and reference standard domains, hampered conclusive judgements about the risk of bias. |
| 58% | 59 | 75 | |||||
| 68% | 45 | 88 | |||||
| 77% | 32 | 100 | |||||
| 88% | 17 | 114 | |||||
|
1Minimum, 25 percentile, 50 percentile, 75 percentile, maximum of prevalence among included studies 2HSROC (hierarchical summary receiver operating characteristic) parameters were used to illustrate sensitivity for a fixed specificity of 86% (median specificity of the included studies) 3Median specificity estimated from included studies. Abbreviations: CI: confidence interval IQR: interquartile range PH: pulmonary hypertension QUADAS‐2: a revised tool for the quality assessment of diagnostic accuracy studies WHO: World Health Organization | |||||||
Background
Target condition being diagnosed
Pulmonary hypertension (PH) is an important cause of morbidity and mortality. Although the exact prevalence of PH is not known because of various possible aetiologies, a previous study reported that PH affects up to 100 million people worldwide (Schermuly 2011). PH leads to a substantial loss of exercise capacity and can cause right ventricular overload, resulting in heart failure and early mortality. A recently published study reported that three‐year survival ranges from 58.2% to 73.3% (Ling 2012). PH is diagnosed when resting mean pulmonary arterial pressure is 25 mmHg or more at right‐heart catheterisation. It is a progressive disease that, if left untreated, can be fatal although the rate of progression is highly variable.
PH is divided into five aetiological categories according to the World Health Organization (WHO) criteria (Simonneau 2013).
Group 1 comprises patients with pulmonary arterial hypertension (PAH). This group consists of sporadic idiopathic PH (IPAH), heritable IPAH, and PAH due to diseases that localise to small pulmonary muscular arterioles. These diseases include connective tissue disease, HIV infection, portal hypertension, congenital heart disease, schistosomiasis, chronic haemolytic anaemia, persistent PH of the newborn, pulmonary veno‐occlusive disease, and pulmonary capillary hemangiomatosis. Drug‐induced PAH (including anorexigenic) and toxin‐induced PAH are also considered to belong to group 1 PAH.
Group 2 PH comprises patients with PH due to left heart disease and is the most common form of PH worldwide. PH due to systolic dysfunction, diastolic dysfunction, or valvular heart disease is included in this group.
Group 3 PH includes patients with PH due to lung disease or hypoxaemia. This includes PH caused by chronic obstructive pulmonary disease (COPD), interstitial lung disease, pulmonary disease with a mixed restrictive and obstructive pattern, sleep‐disordered breathing, and alveolar hypoventilation disorders.
Group 4 PH comprises patients with chronic thromboembolic PH due to chronic thromboembolic occlusion of the proximal or distal pulmonary vasculature.
Group 5 PH includes patients with PH with unclear, multifactorial mechanisms.
Although the epidemiology of PH varies among the five groups, most of the available evidence relates to group 1 PAH. The prevalence of group 1 PAH in the general population is estimated to be 5 to 15 cases per 1 million adults (Humbert 2006; Ling 2012). The prevalence of PH in groups 2 to 5 is unknown due to the broad classification and multiple aetiologies. One cohort study reported that the proportion of each group among individuals with PH was 0.18, 0.35, 0.17, 0.09, and 0.21 (Meredith 2014).
The prognosis of PH depends on various factors. The Registry to Evaluate Early and Long‐term PAH Disease Management (REVEAL) risk score is used to predict disease progression (Benza 2010). Poor prognostic indicators include age at initial presentation > 50 years (Peacock 2007), male sex and ≥ 60 years (Marcus 2008), persistent (WHO) functional class III or IV (Appendix 1), pericardial effusion, and elevated right atrial pressure (Paulus 2007; Torbicki 2007). The natural history and prognosis of group 1 PAH are better studied than those of groups 2 through 5. In general, in the absence of therapy, those with group 1 PAH have worse survival than groups 2 through 5. Symptomatic patients with IPAH who do not receive treatment have a median survival of approximately three years. Data from the REVEAL registry reported that, from the time of diagnostic right‐heart catheterisation, people with PAH had one‐, three‐, five‐, and seven‐year survival rates of 85%, 68%, 57%, and 49%, respectively (Benza 2010).
Early detection and treatment of PH is recommended as advanced disease may be less responsive to therapy (Galie 2013). Primary therapy of PH is directed at the underlying cause of the PH. People with persistent PH with WHO functional class II, III, or IV, despite treatment of the underlying cause of the PH, should be referred to a specialised centre to be evaluated for advanced therapy. Advanced therapy is directed at the PH itself, rather than the underlying cause of the PH. It includes treatment with prostacyclin pathway agonists, endothelin receptor antagonists, phosphodiesterase 5 inhibitors, and soluble guanylate cyclase stimulants. Although PH is divided into five aetiological categories, the first diagnosis test for PH is echocardiography. Therefore, we defined the target condition as PH regardless of the WHO classification group 1 to 5.
Index test(s)
Estimated systolic pulmonary artery pressure determination by Doppler trans‐thoracic echocardiography was the Index test. The Doppler echocardiography is a noninvasive test that can be used to estimate the blood flow through blood vessels or cardiac chamber by using high‐frequency sound waves. The tricuspid regurgitation jet velocity, which is the velocity of regurgitated blood flow through tricuspid valve from right ventricular to right atrium, is also estimated by Doppler echocardiography. The systolic pulmonary arterial pressure can be estimated from the maximum tricuspid regurgitation jet velocity by using the modified Bernoulli equation and adding the right atrial pressure (systolic pulmonary arterial pressure = 4 (v)2 + right atrial pressure, where v is the peak velocity of the tricuspid regurgitation jet) (Berger 1985). The majority of people have some degree of tricuspid regurgitation, and the utilisation of tricuspid regurgitation to estimate systolic pulmonary arterial pressure is the most common practice in echocardiography (Kaplan 2010). Right atrial pressure can be estimated by the diameter and collapse of the inferior vena cava (IVC) during spontaneous respiration(Galie 2016; Rudski 2010). An IVC diameter of < 2.1 cm that collapses > 50% with a sniff suggests a normal right atrial pressure of 3 mmHg (range 0–5 mmHg), whereas an IVC diameter of > 2.1 cm that collapses < 50% with a sniff or < 20% on quiet inspiration suggests a high right atrial pressure of 15 mmHg (range 10–20 mmHg) (Galie 2016; Rudski 2010). Several studies have demonstrated an adequate correlation between the estimated systolic pulmonary arterial pressure by Doppler trans‐thoracic echocardiography and the direct measurement of mean pulmonary artery pressure with right‐heart catheterisation (Zhang 2010). If the estimated systolic pulmonary arterial pressure is higher than 35 to 40 mmHg or if tricuspid regurgitation velocity is more than 2.8 m/s, further evaluation is recommended by guidelines to determine if PH is present (Galie 2016; Rudski 2010). Although several studies have demonstrated an adequate correlation between the estimated systolic pulmonary arterial pressure by echocardiography and by the direct measurement of right‐heart catheterisation, several studies have reported that the overinflated lung lowered the diagnostic accuracy of echocardiography (Fisher 2007). In patients with overinflated lungs such as in COPD, the heart may rotate toward the right, which makes it difficult to visualise the tricuspid valve and pulmonary artery. In patients with severe tricuspid regurgitation, pulmonary arterial pressure may also be underestimated (Galie 2016). Another problem of Doppler echocardiography is the overestimation of systolic pulmonary arterial pressure mainly due to the overestimation of right atrial pressure (Fisher 2009;Testani 2010). The size of the IVC, and its variation with respiration may affect this overestimation. Due to the risk of underestimation or overestimation, the current European Society of Cardiology guidelines reported that the estimation of pulmonary arterial pressure based solely on Doppler transthoracic echocardiography measurements could not be suitable for triage for mild and asymptomatic PH (Galie 2016).
Clinical pathway
Symptoms and signs of PH are nonspecific, which frequently result in a delay in diagnosis (Brown 2011). The initial symptoms of PH are exertional dyspnoea, fatigue, chest pain, syncope, palpitations, and peripheral oedema. Many people with PH visit hospitals complaining of these nonspecific symptoms and physicians suspect the presence of PH in the presence of these nonspecific symptoms or following initial evaluation by chest radiograph or electrocardiogram. The classic chest radiograph of an individual with PH shows enlargement of the central pulmonary arteries, right ventricular enlargement, and right atrial dilatation. An electrocardiogram of an individual with PH may show signs of right ventricular disease, which includes right axis deviation, an R wave/S wave ratio greater than one in the lead V1, incomplete or complete right bundle branch block, or increased P wave amplitude in lead II.
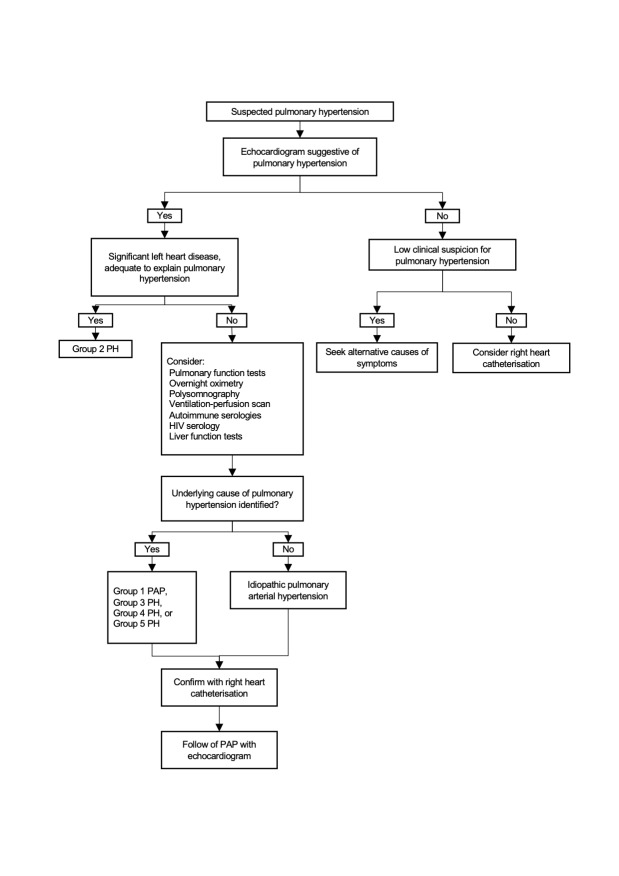
When PH is suspected by these signs or initial diagnosis tests, diagnostic evaluation is performed to confirm that PH exists, to determine its severity, and to identify its cause (Figure 1) (Rubin 2016).
1.
Clinical pathway of diagnostic evaluation for pulmonary hypertension among adults, adolescents, and children
Abbreviations: PAH: pulmonary arterial hypertension; PH: pulmonary hypertension (Rubin 2016).
The first step of diagnostic testing is evaluation by echocardiogram. Pulmonary arterial pressure can be estimated by this noninvasive method. When the echocardiogram does not suggest PH, further evaluation depends on clinical suspicion. If clinical suspicion of PH is still high, right‐heart catheterisation should be considered. When the echocardiogram is suggestive of PH, clinicians should evaluate whether left heart disease exists to adequately explain the degree of estimated PH. Patients with substantial left heart disease revealed by the echocardiogram to explain the degree of estimated PH do not require further evaluation to determine the aetiology of PH.
Patients who have no left heart disease should undergo additional diagnostic testing to determine the aetiology of PH other than left heart diseases and appropriate treatment. Such additional tests may include a pulmonary function test, ventilation‐perfusion scanning, overnight oximetry, polysomnography, or laboratory testing (e.g. autoimmune serologies, HIV serology, and liver function tests) based on the history and physical examination.
Right‐heart catheterisation is indicated to confirm PH and its severity. Direct pressure measurement of pulmonary arterial pressure with right‐heart catheterisation is the clinical reference standard to confirm PH (Lewis 2016).
Alternative test(s)
Some additional tests (e.g. chest radiograph, magnetic resonance, computed tomography) may also be considered to confirm the aetiology of PH, however Doppler echocardiography plays a central role in the diagnosis and management of PH (Freed 2016).
Rationale
Many patients are diagnosed at a late stage of the disease because symptoms and signs of PH are nonspecific at the beginning of the disease (Brown 2011). Early and accurate detection of PH would therefore be of great benefit. While direct pressure measurement with right‐heart catheterisation is the clinical reference standard for PH, it is not routinely used in clinical practice due to its invasiveness and potential complications (Connors 1996).
Trans‐thoracic Doppler echocardiography is less invasive, less expensive, and widely available compared with right‐heart catheterisation. The guidelines from the European Society of Cardiology and the European Respiratory Society (Galie 2016) and the expert consensus document from the American Heart Association and the American College of Cardiology Foundation (McLaughlin 2009) suggested that echocardiography should be performed as an initial diagnosis method and as a method for monitoring disease progression for both patients suspected with PH and those diagnosed with PH. However, the guidelines also documented the insufficient test accuracy of Doppler echocardiography. Several studies have questioned the accuracy of noninvasively measured pulmonary arterial pressure (Arcasoy 2003; Fisher 2009; Rich 2011). They reported that Doppler echocardiography underestimated pulmonary arterial pressure, which could lead to missed diagnosis of PH. To avoid diagnosis in later stages of the disease, accurate triage of PH is necessary. We will therefore evaluate the diagnostic accuracy of echocardiography to diagnose patients suspected of PH.
We hypothesise that Doppler echocardiography could be a beneficial test to triage PH since ultrasound devices have become more commonly available in a variety of clinical settings.
Objectives
To determine the diagnostic accuracy of Doppler trans‐thoracic echocardiography for detecting PH in people with suspected pulmonary hypertension.
Secondary objectives
To investigate several possible sources of heterogeneity as indicated below.
Types of PH defined by WHO classification (Group 3, not Group 3, or classification not reported).
Mechanical ventilation (including noninvasive positive pressure ventilation) or not.
Estimation of right atrial pressure (whether estimated by using the diameter and collapse of the IVC during spontaneous respiration or by any other methods).
Methods
Criteria for considering studies for this review
Types of studies
We included studies that evaluated the diagnostic accuracy of trans‐thoracic Doppler echocardiography for detecting PH, where right‐heart catheterisation was the reference standard. We excluded diagnostic case‐control studies (two‐gate design) (Rutjes 2005). We excluded studies where right‐heart catheterisation was not the reference standard or the reference standard threshold differed from 25 mmHg. We excluded studies with an interval of more than one week between the index test and the reference standard because interventions may be implemented soon after the initial examination and medical conditions could differ due to different times (e.g. > 1 week apart) (Delcroix 2010; Lewis 2016). We excluded studies that did not provide sufficient diagnostic test accuracy data (true positive [TP], false positive [FP], true negative [TN], and false negative [FN] values, based on the reference standard) such as case series studies. We included studies that provided data from which we could extract TP, FP, TN, and FN values, based on the reference standard. We contacted study authors for missing data. We did not exclude studies based on the publication type (e.g. full articles, letters to the editor, conference abstracts, or unpublished data).
Participants
We included all adults (16 years of age or older) with suspected PH. We excluded any participant with a prior diagnosis of PH. We did not exclude participants based on sex or cause of PH.
Index tests
Measurement by Doppler trans‐thoracic echocardiography was the index test. We included all studies where systolic pulmonary arterial pressure was calculated from the maximum tricuspid regurgitation jet velocity using the modified Bernoulli equation and adding right atrial pressure (Berger 1985). We included all methods used to measure right atrial pressure (e.g. clinical estimation from jugular venous pressure, using a fixed value from 5 mmHg to 10 mmHg, using the diameter and collapse of the IVC during spontaneous respiration). The threshold of the estimated systolic pulmonary arterial pressure by echocardiography to diagnose PH was defined as the authors defined in the included studies.
Target conditions
The target condition was PH regardless of WHO classification group 1 to 5 (Simonneau 2013).
Reference standards
We included only studies in which PH was defined as a mean pulmonary arterial pressure assessed by right‐heart catheterisation of ≥ 25 mmHg (Hoeper 2013).
Search methods for identification of studies
Electronic searches
We systematically searched the following databases on 21 October 2019 and updated the search on 03 August 2021:
MEDLINE Ovid SP (1946 to 03 August 2021) (Appendix 2);
Embase Ovid SP (1974 to 03 August 2021) (Appendix 3);
Web of Science Core Collection (1970 to 03 August 2021) (Appendix 4).
We searched the following trials registries on 21 October 2019 and updated the search on 03 August 2021:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov/) (Appendix 5).
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch/) (Appendix 5).
We combined search terms describing the target condition and the index text. We did not use search terms to describe diagnostic study designs as this is not currently recommended in the Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy (De Vet 2008). We applied no restrictions on language or type of publication.
Searching other resources
To identify additional published, unpublished, and ongoing studies, we entered included studies identified from the above sources into the Web of Science database and used the ‘Related Articles’ feature. We checked the reference lists of all primary studies and relevant systematic reviews. Furthermore, we also searched for conference proceedings through Embase and the Web of Science.
Data collection and analysis
Selection of studies
We undertook the systematic review using the methods outlined in the Cochrane Handbook for Reviews of Diagnostic Test Accuracy (Deeks 2013). Two authors (from JK and YN, YK, YT, MK, SO, HI, TM) independently reviewed titles and abstracts identified by the search strategy. After the title and abstract screening, the full‐text reports of all potentially eligible studies were obtained and two authors independently assessed the eligibility of the full‐text reports. Differences were resolved by discussion between the review authors. We provided details of both included and excluded studies in the Characteristics of included studies and Characteristics of excluded studies tables.
Data extraction and management
Two authors (from JK and YN, YK, YT, MK, SO, HI, TM) independently extracted data on study characteristics, participant demographics, sample size, test methods, methodological quality, sensitivity, and specificity. Two review authors then extracted data to construct a 2 × 2 contingency table. Disagreements were resolved by consensus.
Assessment of methodological quality
We used the QUADAS‐2 tool to assess the quality of studies (Whiting 2011). The qualities to be assessed are described in detail in (Appendix 6). For each item in the quality assessment form, we included a description of how the study addressed the issue and entered a judgement of 'low', 'high', or 'unclear' for the overall risk of bias for each of the four domains. In addition, we added a judgement of 'low', 'high', or 'unclear' for the overall concern of applicability to the review question for domains 1, 2, and 3. The assessment of methodological quality is reported in Assessment of methodological quality table which lists all judgements made for each included study. Two authors (from JK and YN, YK, YT, MK, SO, HI, TM) independently assessed methodological quality. Disagreements were resolved by discussion among the review authors.
Statistical analysis and data synthesis
We performed data synthesis using the methods recommended by the Working Group of the Cochrane Collaboration on Systematic Reviews of Diagnostic Test Accuracy (Deeks 2013). We extracted accuracy data for all thresholds used in the primary studies. We represented individual study sensitivities and specificities in forest plots in order to inspect between‐study variability. These individual study accuracy estimates were also represented in a Receiver Operating Characteristic (ROC) plot of sensitivity versus 1‐specificity to visually assess the correlation between both indices. Given the considerable variation of cut‐off values in the collected data, we did not use the bivariate model and avoided providing the summary point of sensitivity and specificity (Deeks 2013). Instead, we estimated a summary ROC (SROC) curve by fitting a hierarchical summary ROC (HSROC) model (Rutter 2001). Using HSROC parameter estimates, we derived sensitivity at the median value of specificity along with corresponding 95% confidence intervals (CI)s. We set the fixed specificity as median specificity among the included studies and calculated the sensitivity with the corresponding 95% CIs or vice versa in a manner similar to a previous Cochrane review (Molano 2019). This is because diagnostic accuracy studies typically contain fewer patients with the target condition than without, and estimates of sensitivities are often made with less certainty than estimates of specificity. (Best 2018; Heazell 2019). Since we observed a large variability in specificity, we added a post hoc analysis to present the summary of specificity and 95% CI at median sensitivity among the included studies. The potential numerical consequences, given a positive and negative index test result using different prevalence, were calculated. We performed all analyses using Review Manager 5 (Review Manager 2014), STATA software, version 13.0 (Stata 2013), or SAS studio (SAS/STAT®, SAS Institute Inc. NC, USA).
Investigations of heterogeneity
To test whether sensitivity or specificity, or both, differed in subgroups of studies, we tabulated the median and range of sensitivity and specificity for the following subgroups:
Types of PH defined by WHO classification (Group 3 (PH due to lung diseases or hypoxaemia), not Group 3, or classification not reported). We expected that measuring tricuspid regurgitation would be more difficult in patients with lung disease, especially COPD, than in patients without lung disease, which could decrease the sensitivity and specificity of echocardiography to detect PH.
Mechanical ventilation (including non‐invasive positive pressure ventilation) or not.
Estimation of right atrial pressure (using the diameter of IVC, any other methods, or not reported).
Since we observed considerable heterogeneity, we performed a post hoc subgroup analysis using the bivariate model (Macaskill 2021; Reitsma 2005) stratified by the threshold of the index test that was categorised according to the guidelines (Rudski 2010) as follows: < 36 mmHg, ≥ 36 and < 40 mmHg, and ≤ 40 mmHg for clinical implementation.
Sensitivity analyses
We examined the robustness of the meta‐analysis by conducting the following sensitivity analysis where possible.
Repeating the analysis excluding studies at high risk of bias in domains 1 or 4 of the QUADAS‐2 assessment: We anticipated that studies at high risk of bias in domains 1 and 4 would have a great impact on meta‐analysis because these domains would cause selection bias.
Repeating the analysis for each quartile of prevalence: due to the invasiveness of the reference standard, less severe cases would not be verified by right‐heart catheterisation, which would lead to partial verification bias. We therefore performed additional sensitivity analysis by using prevalence as a surrogate of partial verification. We used the quartiles of prevalence among included studies and checked the robustness of the results.
Repeating the analysis by including uninterpretable results as both test negative and positive: although uninterpretable results would be likely to occur among patients with overinflated lung, which is associated with the severity of pulmonary hypertension and causes a difficulty of visualisation, they are not always considered test positive.
Assessment of reporting bias
We did not plan to explore reporting bias due to a lack of suitable statistical methods (Deeks 2013).
Results
Results of the search
We identified 11,999 references through electronic searches of MEDLINE, Embase, Web of Science, Clinicaltrial.gov, the International Clinical Trials Registry Platform (ICTRP), and additional references through other searches (citation search of previous systematic reviews). The flow of studies through the diagnosis process is shown in Figure 2. After removing 3816 duplicates, 8183 references remained. Of these, we excluded 8012 references by analysis of the title and abstracts. We assessed the full text of the remaining 171 references. We excluded 154 references for reasons listed in the Characteristics of excluded studies table. The remaining 17 references (of 17 studies) met our inclusion criteria.
2.
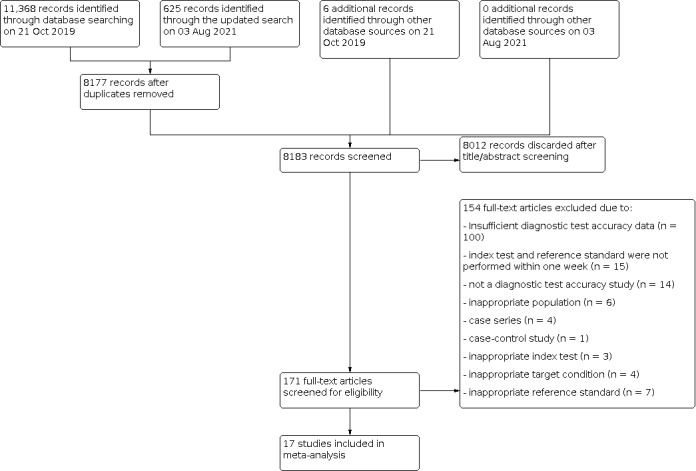
Flow diagram
Included studies
We summarised the characteristics of the 17 included studies in the Characteristics of included studies table and Table 2. The studies included 3656 participants, of which 1342 participants (37%) had PH. The prevalence of PH ranged from 10% to 88% with a median of 68% (interquartile range (IQR): 58% to 77%). The included studies were conducted in various departments from university or tertiary hospitals; three studies were from lung or liver transplantation centres (Balci 2016; Colle 2003; Wainstein 2017), nine studies were from the cardiology or pulmonary department of university or tertiary hospitals (Amsallem 2016; Er 2010; Greiner 2014; Hellenkamp 2018; Lafitte 2013; Nowak 2018; Sawada 2019; Schneider 2017; Venkateshvaran 2021), and the others were from unclear settings (Hsu 2008; Kyranis 2018; Mazhar 2011; Mo 2015; Mo 2015a).
1. Summary of characteristics of included studies.
| Study ID | Number of participants (included in analysis/included in study) | Prevalence of PH (%) | Age | Sex, male (%) | Classification of PH defined by WHO | Threshold of index test (mmHg) | RAP estimation | The interval between the index test and reference standard | How to handle the uninterpretable results of the index test | Sensitivity | Specificity |
| Amsallem 2016 | 199/307 | 77 | 50 ± (13)* | 46 | NR | 40 | using the diameter of IVC | 2 days | excluded from analysis | 92% | 89% |
| Balci 2016 | 103/103 | 57 | 48 (18 to 70)*** | 65 | Group 3 | 35 | NR | 3 days | NA | 85% | 66% |
| Colle 2003 | 165/165 | 10 | 48 ± (8)* | 70 | Group 1 | 30 | using the diameter of IVC | 7 days | NA | 76% | 95% |
| Er 2010 | 50/50 | 86 | 66.9 ± (14.5)* | 28 | NR | 38 | using the diameter of IVC | 2 hours | NA | 98% | 100% |
| Greiner 2014 | 1695/3920 | 72 | 63 ± (15)* | 67 | NR | 36 | using the diameter of IVC | 5 days | excluded from analysis | 87% | 79% |
| Hellenkamp 2018 | 90/90 | 76 | 64.8 [55 to 79]**** | 48 | NR | 31 | using the diameter of IVC | 1 days | NA | 81% | 55% |
| Hsu 2008 | 49/55 | 33 | 55 (20 to 80)** | 18 | Group 1 | 47 | not using the diameter of IVC | 4 hours | excluded from analysis | 75% | 91% |
| Kyranis 2018 | 96/100 | 68 | 58 ± (14)* | 43 | NR | 31 | using the diameter of IVC | 1 days | excluded from analysis | 92% | 87% |
| Lafitte 2013 | 155/310 | 67 | 64.8 ± (15.9)* | 52 | NR | 38 | using the diameter of IVC | 5 days | excluded from analysis | 88% | 83% |
| Mazhar 2011 | 99/159 | 58 | NR | NR | NR | 31 | NR | 3 days | excluded from analysis | 67% | 83% |
| Mo 2015 | 24/30 | 88 | NR | NR | NR | 35 | NR | 7 days | excluded from analysis | 95% | 33% |
| Mo 2015a | 87/87 | 68 | NR | NR | NR | 45 | NR | 7 days | excluded from analysis | 81% | 86% |
| Nowak 2018 | 37/65 | 70 | 53.3 ± (9.5)* | 75 | NR | 43 | NR | 5 days | excluded from analysis | 92% | 82% |
| Sawada 2019 | 189 /189 | 26 | 58 ± (17)* | 56 | NR | 41 | using the diameter of IVC | 1 days | NA | 92% | 91% |
| Schneider 2017 | 65/65 | 83 | 67.2 (19 to 89)** | 43 | mixture of Group 1, 2, 3, and 4 | 34 | not using the diameter of IVC | 1 days | NA | 87% | 91% |
| Venkateshvaran 2021 | 419/480 | 62 | NR | NR | NR | 31 | using the diameter of IVC | 3 hours | excluded from analysis | 40% | 88% |
| Wainstein 2017 | 134/134 | 62 | 47 ± (14.7)* | 47 | Group 3 | 36 | NR | 3 days | NA | 89% | 60% |
* mean ± (SD), ** mean (range), *** median (range), **** mean [interquartile]
Abbreviations: IVC: inferior vena cava NA: not applicable NR: not reported PH: pulmonary hypertension RAP, right atrial pressure WHO: World Health Organization
Of the 17 studies, six studies were prospective (Balci 2016; Colle 2003; Er 2010; Hsu 2008; Kyranis 2018; Schneider 2017); 11 studies were retrospective (Amsallem 2016; Greiner 2014; Hellenkamp 2018; Lafitte 2013; Mazhar 2011; Mo 2015; Mo 2015a; Nowak 2018; Sawada 2019; Venkateshvaran 2021; Wainstein 2017). Four studies were published as abstracts only (Mazhar 2011; Mo 2015; Mo 2015a; Wainstein 2017), and the remaining 13 studies were full‐text publications. We considered Mo 2015 and Mo 2015a to be separate studies because they had different numbers of participants and a different prevalence of PH. However, there is still a potential overlap among the patients included in the two studies.
Four studies enrolled participants with a single WHO classification of PH, two studies enrolled participants with group 1 PH (Colle 2003; Hsu 2008); two studies enrolled participants with group 3 PH (Balci 2016; Wainstein 2017); two studies enrolled participants with group 1, 2, 3 and 4 PH (Er 2010; Schneider 2017); one study enrolled participants with group 2, 3, and 4 PH (Nowak 2018); and the remaining 10 studies did not report the WHO classification. Four studies reported the proportion of mild or asymptomatic participants (Er 2010; Greiner 2014; Hellenkamp 2018; Nowak 2018), but others did not. The reported proportion ranged from 2% to 16%.
The cut‐off value of the index test (systolic pulmonary arterial pressure) ranged from 30 to 47 mmHg with a median of 36 mmHg (IQR: 31 to 40 mmHg). In nine studies, right atrial pressure was measured using the diameter and collapse of the inferior vena cava during spontaneous respiration (Amsallem 2016; Colle 2003; Er 2010; Greiner 2014; Hellenkamp 2018; Kyranis 2018; Lafitte 2013; Sawada 2019; Venkateshvaran 2021); in another study, right atrial pressure was defined as 10 mmHg (Hsu 2008); and the remaining seven studies did not report the methods used to measure right atrial pressure.
The interval between the index test and reference standard was less than one day in seven of the 17 studies (Er 2010; Hellenkamp 2018; Hsu 2008; Kyranis 2018; Sawada 2019; Schneider 2017; Venkateshvaran 2021) and was between two and seven days in the remaining 10 studies.
We contacted trial authors for missing data, but none were provided except for one study (Amsallem 2016).
Excluded studies
We excluded 154 references (154 studies). The reason for exclusion is stated for each study in the Characteristics of excluded studies table and summarised below.
insufficient diagnostic test accuracy data: 100
index test and reference standard were not performed within one week: 15
not a diagnostic test accuracy study: 14
inappropriate population: 6
case series: 4
case‐control study: 1
inappropriate index test: 3
inappropriate target condition: 4
inappropriate reference standard: 7
Methodological quality of included studies
The methodological quality of the included studies is reported in the Characteristics of included studies, Figure 3 and Figure 4. Poor reporting, especially in the index test and reference standard domains, hampered conclusive judgement relative to the risk of bias. Only one study had a low risk of bias in all four domains (Hellenkamp 2018).
3.
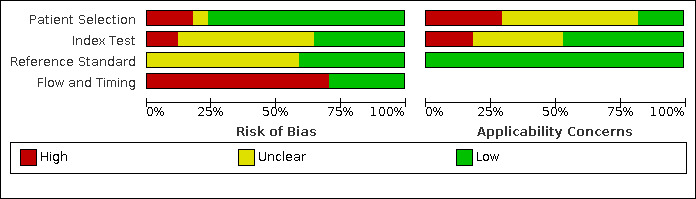
Risk of bias and applicability concerns graph: review authors' judgements about each domain presented as percentages across included studies
4.
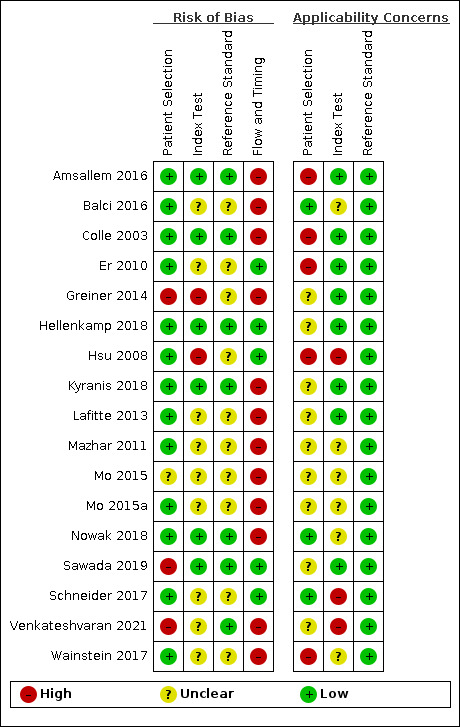
Risk of bias and applicability concerns summary: review authors' judgements about each domain for each included study
Patients selection domain
Three studies had a high risk of bias with regard to patient selection due to inappropriate exclusion (Greiner 2014; Sawada 2019; Venkateshvaran 2021). For these studies, patients whose index test results were not explicitly documented were excluded. One study had unclear risk of bias because the inclusion procedures were not reported (Mo 2015). For the remaining 13 studies, we rated patient selection as having low risk of bias. We judged applicability as being of high concern. The prevalence from the included studies was high as the included studies were often conducted in tertiary care settings. The classification of PH in the patients included in our review was mainly unclear.
Index test domain
Two studies had a high risk of bias because the threshold of index test was not prespecified ((Greiner 2014; Hsu 2008); in Greiner 2014, the threshold that had the highest accuracy was reported and in Hsu 2008, the threshold that had the highest positive likelihood ratio was reported), seven studies had a low risk of bias (Amsallem 2016; Colle 2003; Hellenkamp 2018; Kyranis 2018; Nowak 2018; Sawada 2019; Venkateshvaran 2021), and we rated the remaining eight studies as having an unclear risk of bias because it was unclear whether the index test results were interpreted without the knowledge of the results of the reference standard (Balci 2016; Er 2010; Lafitte 2013; Mazhar 2011; Mo 2015; Mo 2015a; Schneider 2017; Wainstein 2017) and/or it was unclear whether a threshold was prespecified (Balci 2016; Lafitte 2013; Mazhar 2011; Mo 2015; Mo 2015a; Venkateshvaran 2021; Wainstein 2017). Applicability was judged as of high concern in two studies because right atrial pressure was not measured using the diameter and collapse of the inferior vena cava during spontaneous respiration (Hsu 2008; Schneider 2017), of unclear concern in six studies because the methods used to measure right atrial pressure were unclear (Balci 2016; Mazhar 2011; Mo 2015; Mo 2015a; Nowak 2018; Wainstein 2017), and of low concern in the remaining nine studies.
Reference standard domain
Seven studies were at low risk of bias in the reference standard domain (Amsallem 2016; Colle 2003; Hellenkamp 2018; Kyranis 2018; Nowak 2018; Sawada 2019; Venkateshvaran 2021). For the remaining 10 studies, the risk of bias was unclear because it was not specified whether reference standard results were interpreted without knowledge of the results of the index tests (Balci 2016; Er 2010; Greiner 2014; Hsu 2008; Lafitte 2013; Mazhar 2011; Mo 2015; Mo 2015a; Schneider 2017; Wainstein 2017). It was not clear whether a threshold was prespecified in 13 studies (Balci 2016; Colle 2003; Er 2010; Greiner 2014; Hellenkamp 2018; Hsu 2008; Kyranis 2018; Lafitte 2013; Mazhar 2011; Mo 2015; Mo 2015a; Nowak 2018; Wainstein 2017). Applicability was of low concern in all the studies.
Flow and timing domain
Five studies were at low risk of bias in the flow and timing domain (Er 2010; Hellenkamp 2018; Hsu 2008; Sawada 2019; Schneider 2017). The remaining 12 studies were at high risk of bias. Eight studies excluded some participants from the analysis due to the uninterpretable results of the index test (Amsallem 2016; Greiner 2014; Kyranis 2018; Lafitte 2013; Mazhar 2011; Mo 2015; Mo 2015a; Venkateshvaran 2021) and in 10 studies the interval between the index test and reference standard was not less than one day (Amsallem 2016; Balci 2016; Colle 2003; Greiner 2014; Lafitte 2013; Mazhar 2011; Mo 2015; Mo 2015a; Nowak 2018; Wainstein 2017).
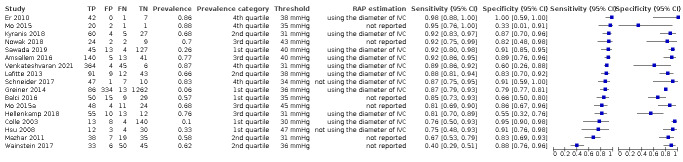
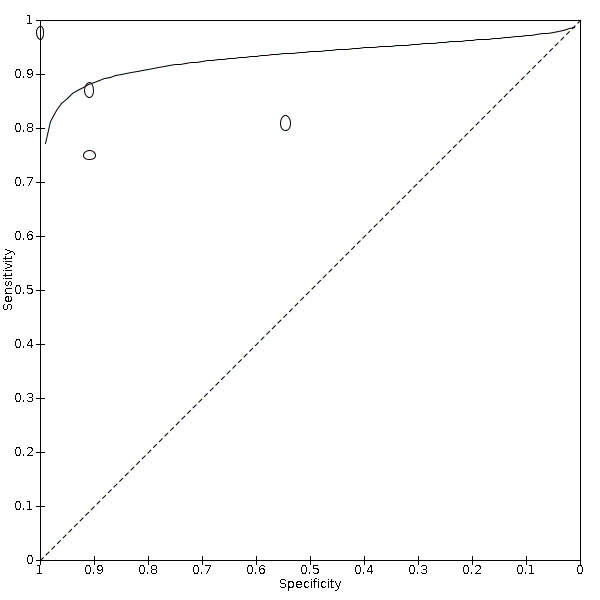
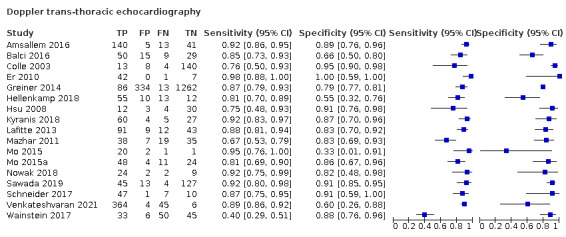
Findings
The sensitivity of the index test ranged from 40% to 98% with a median of 87% and the specificity of the index test ranged from 33% to 100% with a median of 86%. The range of sensitivity and specificity estimated by the studies, as well as the different thresholds for echocardiography positive findings, the prevalence of PH, and the methods to estimate the right atrial pressure (RAP) are shown in Figure 5. There was a large variability between the studies and uncertainty in the results. The SROC curve under the HSROC model, representing the accuracy of echocardiography thresholds used across studies, as well as individual study accuracy estimates, are shown in Figure 6. Given the considerable variation of cut‐off values in the collected data, we refrained from calculating the summary diagnostic accuracy using the bivariate model.
5.
Forest plots: sensitivity and specificity of Doppler trans‐thoracic echocardiography for detecting PH
Abbreviations: CI: confidence interval; FN: false negative; FP: false positive; IVC: inferior vena cava; RAP: right atrial pressure; TN: true negative; TP: true positive.
6.
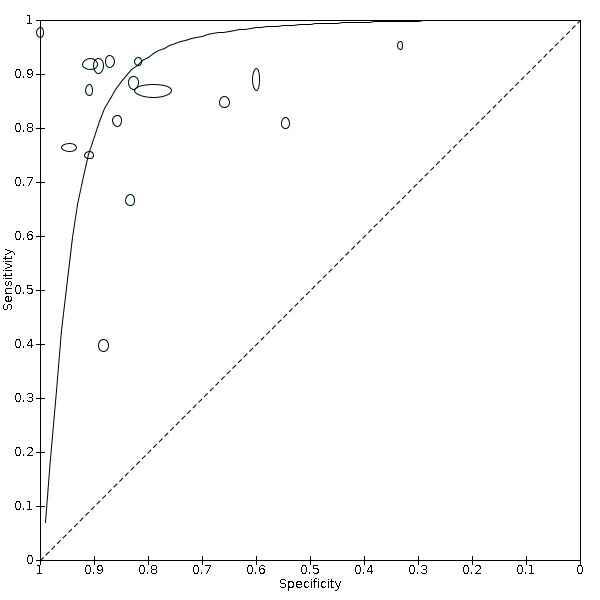
Main analysis: Summary ROC plot and curve of Doppler trans‐thoracic echocardiography for PH under the HSROC model
Abbreviations: HSROC: hierarchical summary receiver operating characteristic; PH: pulmonary hypertension; ROC: receiver operating characteristic.
We used the HSROC parameters to calculate the sensitivity under fixed specificity. As shown in Table 1, using a prevalence of PH of 68% (the median prevalence) and a fixed specificity of 86% (the median specificity) (Best 2018; Heazell 2019), the estimated sensitivity was 87% (95% CI 78% to 96%). Seven out of 17 studies in this analysis reported sensitivities inferior to this estimation. The estimated specificity at median sensitivity was 86% (95% CI 76% to 94%).
Additional estimations with a prevalence of 10%, 58%, 77% and 88% (minimum, 25 percentile, 75% percentile and maximum values from included studies) showed an increase in the number of false positives or false negatives, respectively (Table 1).
Investigation of heterogeneity
We summarised these results in Table 3. There were many potential sources of variation and too few studies to explain the observed variabilities.
2. Summary of investigations for heterogeneity.
| Covariate | Subgroup | Number of studies | Number of participants | Number of cases | Sensitivity | Specificity |
| Overall | 17 | 3656 | 1342 | Median (range): 87% (40% to 98%) | Median (range): 86% (33% to 100%) | |
| WHO Classification of PH | Not Group 3 | 3 | 279 | 87 | Median (range): 76% (75% to 87%) | Median (range): 91% (91% to 95%) |
| Group 3 | 2 | 237 | 142 | Median (range): 63% (40% to 85%) | Median (range): 77% (66% to 88%) | |
| Not reported | 12 | 3141 | 1113 | Median (range): 92% (67% to 98%) | Median (range): 85% (33% to 100%) | |
| The methods used to estimating RAP | Using the diameter of IVC | 9 | 3057 | 967 | Median (range): 92% (76% to 98%) | Median (range): 89% (55% to 100%) |
| Not using the diameter of IVC | 2 | 114 | 70 | Median (range): 81% (75% to 87%) | Median (range): 91% (91% to 91%) | |
| Not reported | 6 | 485 | 305 | Median (range): 83% (40% to 95%) | Median (range): 83% (33% to 88%) | |
| Threshold groups | < 36 mmHg | 8 | 1061 | 711 | Pooled sensitivity (95% CI): 89% (79% to 94%) |
Pooled specificity (95% CI): 83% (70% to 91%) |
| ≥ 36 mmHg and < 40 mmHg | 4 | 2034 | 328 | Pooled sensitivity* (95% CI): 85% (57% to 96%) |
Pooled specificity* (95% CI): 80% (76% to 84%) |
|
| ≥ 40 mmHg | 5 | 561 | 303 | Pooled sensitivity* (95% CI): 88% (83% to 92%) |
Pooled specificity* (95% CI): 89% (85% to 93%) |
* Pooled sensitivity and specificity estimated by the bivariate random effects model
Abbreviations: CI: confidence interval IVC: inferior vena cava PH: pulmonary hypertension RAP: right atrial pressure WHO: World Health Organization
Types of PH defined by WHO classification (Group 3, not Group 3, or classification not reported)
Due to the limited number of studies in each group, especially for non‐reporting of the classification, we could not apply the HSROC model. Instead, we presented the summary plots of the sensitivity and specificity in each subgroup (Figure 7).
7.
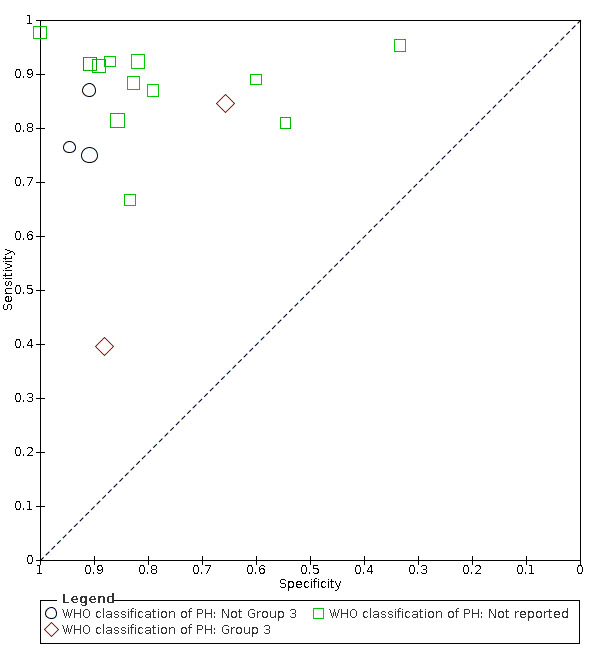
Subgroup analysis: Summary ROC plot and curve of Doppler trans‐thoracic echocardiograph for PH by WHO classifications of pulmonary hypertension
Abbreviations: PH: pulmonary hypertension; ROC: receiver operating characteristic; WHO: World Health Organization.
Mechanical ventilation (including non‐invasive positive pressure ventilation) or not
Since all the included studies did not recruit patients undergoing mechanical ventilation, we could not perform this analysis.
Estimation of right atrial pressure (using the diameter of IVC, any other methods, or not reported)
In 10 studies, right atrial pressure was measured using the diameter and collapse of the inferior vena cava during spontaneous respiration, in two studies, the diameter of the inferior vena cava was not used to measure right atrial pressure, and in the remaining six studies, the method of measuring right atrial pressure was not reported. Due to the limited number of studies in the group using other methods than IVC, we could not apply the HSROC model. Instead, we presented the summary plots of the sensitivity and specificity in each subgroup (Figure 8).
8.
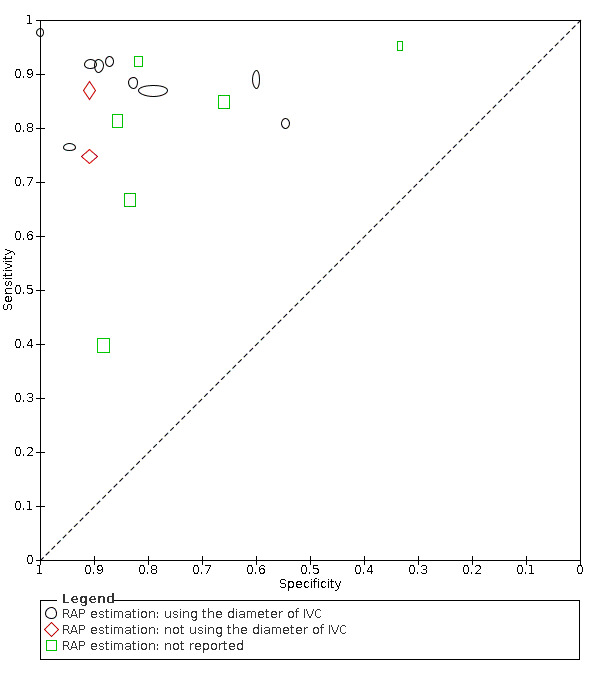
Subgroup analysis: Summary ROC plot and curve of Doppler trans‐thoracic echocardiograph for PH by methods used to estimate RAP
Abbreviations: RAP: right atrial pressure; ROC: receiver operating characteristic.
Threshold of index test (< 36 mmHg, ≥ 36 and < 40 mmHg, and ≤ 40 mmHg)
The pooled sensitivity and specificity of each threshold category are shown in Table 3 and Figure 9. Although we could not observe a clear threshold effect between the categories, there was a large overlap of 95% CIs.
9.
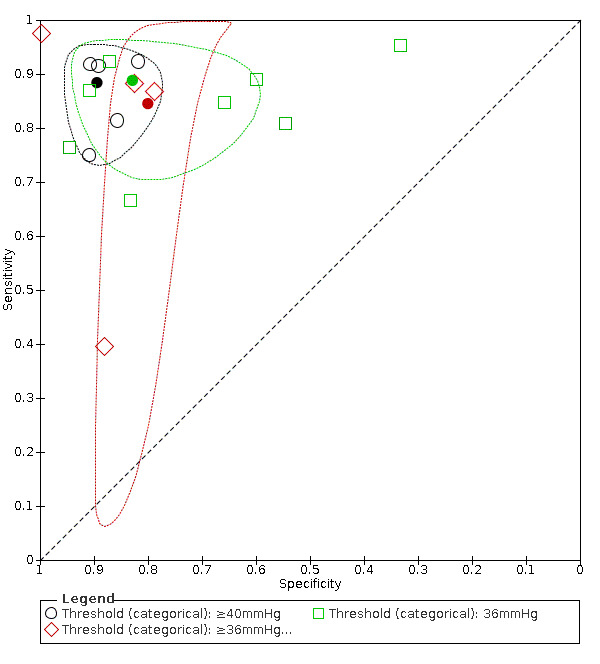
Subgroup analysis: Summary ROC plot of Doppler trans‐thoracic echocardiograph for PH by thresholds under the bivariate model
Abbreviations: RAP: right atrial pressure; ROC: receiver operating characteristic.
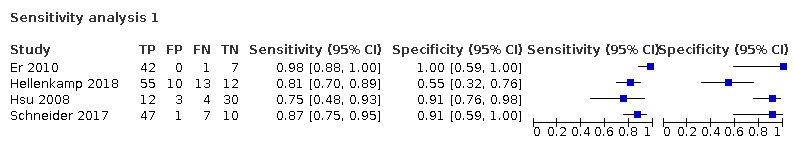
Sensitivity analyses
Table 4 summarised the results from sensitivity analyses. We presented the pooled sensitivity under the fixed specificity of 86% (median of the included studies).
3. Summary of the results from sensitivity analyses.
| Types of sensitivity analysis | Subgroup | Number of studies | Number of participants | Number of cases |
Pooled sensitivity (95% CI) under fixed specificity of 86%* |
| Overall | 17 | 3,656 | 1,342 | 87% (81% to 92%) | |
| Excluding studies at high risk of bias in domains 1 or 4 of the QUADAS‐2 assessment |
Not high risk of bias in domains 1 or 4 | 4 | 254 | 181 | 83% (11% to 100%) |
| Prevalence category | 1st quartile | 4 | 2098 | 181 | 84% (67% to 100%) |
| 2nd quartile | 4 | 491 | 302 | 70% (8% to 100%) | |
| 3rd quartile | 4 | 310 | 218 | 79% (28% to 100%) | |
| 4th quartile | 5 | 757 | 641 | 84% (6% to 100%) |
* Pooled sensitivity and its 95% confidence interval using fixed specificity of 86% (median of the included studies).
Abbreviations: CI: confidence interval QUADAS‐2: a revised tool for the quality assessment of diagnostic accuracy studies
The results were similar to the main results when we excluded studies at high risk of bias in domains 1 and 4 of QUADAS‐2 (Figure 10). The sensitivity varied with the prevalence, but we could not find a clear dose‐response relationship between the accuracy and prevalence (Figure 11).
10.
Sensitivity analysis: Summary ROC plot and curve of Doppler trans‐thoracic echocardiograph for PH, excluding studies at high risk of bias in domain 1 or 4 in QUADAS‐2 assessment under the HSROC model
Abbreviations: HSROC: hierarchical summary receiver operating characteristic; PH: pulmonary hypertension; QUADAS: Quality Assessment of Diagnostic Accuracy Studies; ROC: receiver operating characteristic.
11.
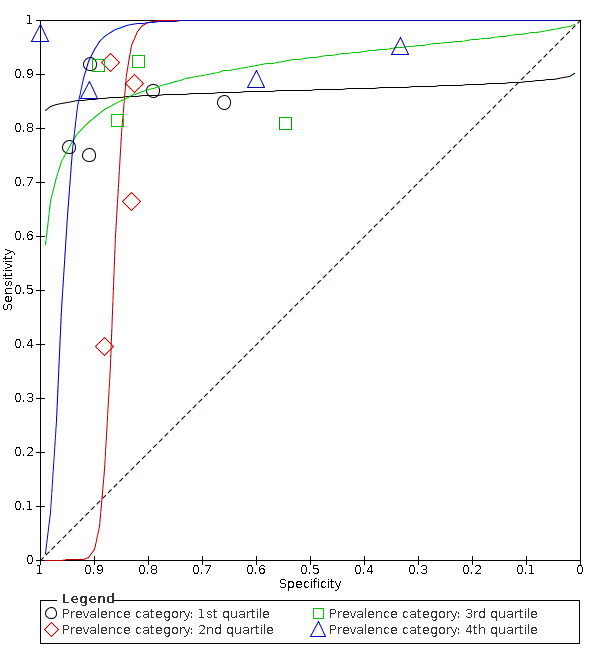
Sensitivity analysis: Summary ROC plot and curve of Doppler trans‐thoracic echocardiograph for PH, repeating the analysis for each quartile of prevalence under the HSROC model
Abbreviations: PH: pulmonary hypertension; ROC: receiver operating characteristic.
We could not perform sensitivity analysis on uninterpretable results it because such patients were excluded from the analysis and the data on whether they had PH was not available (Table 2).
Discussion
Summary of main results
We included 17 studies (3656 adult patients) assessing the diagnostic accuracy of Doppler trans‐thoracic echocardiography for the diagnosis of PH. The included studies enrolled patients suspected of PH. The samples were heterogeneous in terms of their distribution of age, sex, WHO classification, setting, country, positivity threshold, and year of publication. In addition, the prevalence of PH reported in the included studies varied widely (from 6% to 88%). Epidemiological and clinical characteristics of participants are presented in Table 2 and key results in Table 1.
The estimated sensitivity was 87% (95% CI 78 to 96%) when we applied the median specificity of 86% among the included studies. When applying a cohort assuming a 68% prevalence of PH which was the median of the included studies, the result suggested that 275 out of 1000 patients would avoid unnecessary referral for a right‐heart catheterisation but 88 would miss PH diagnosis. The intended role of Doppler echocardiography is as a triage which is used before the reference standard to avoid unnecessary referrals and to minimise false negatives. Given the number of false negatives, the poor prognosis of PH, and the results of our review, a single echocardiography may not be acceptable as a triage test for PH in such a hypothetical cohort. The results of applying the test in other settings with the prevalence of 10%, 58%, 77%, and 88% (minimum, 25% percentile, 75% percentile, and maximum values from included studies) are summarised in the Table 1.
Previous reviews reported that Doppler echocardiography was useful for triage to undergo right‐heart catheterisation (Janda 2011; Taleb 2013; Zhang 2010). However, as shown in Table 1, the diagnostic accuracy of Doppler echocardiography is not likely to be sufficient for clinical use in patients suspected of having PH in settings where the prevalence of PH is high. Such settings include patients with heart failure treated in tertiary care hospitals or patients with end‐stage lung disease who need lung transplantation (Andersen 2012; Bursi 2012; Dzudie 2014). This inaccuracy is likely to partly be due to the problem of overestimation or underestimation of pulmonary arterial pressure, as reported previously (Fisher 2009; Galie 2016; Lang 2015). When the prevalence is low (10%), as is the case for preoperative examinations for liver transplantation (Colle 2003) in the present review, the number of true negatives and false negatives would be 808 and 8 of 1000, respectively. Such low prevalence scenarios can also be apparent in patients with systemic sclerosis or older patients with chronic obstructive pulmonary disease (Avouac 2010; Moreira 2015). In these settings, Doppler echocardiography might be considered as a triage test.
The consequences of applying the test to the hypothetical cohort above used the estimated sensitivity at a fixed specificity. Of note, the reporting sensitivity at a fixed specificity does not indicate how the test would likely perform in practice but represents a point on the HSROC curve that is ideally somewhere near the centre of the observed data. Overall, the methodological quality was low; no study was assigned a low risk of bias or low concern in each QUADAS‐2 domain assessed. Further, there was a high concern regarding applicability due to a variety of settings, characteristics of participants, and prevalence. Poor reporting, especially in the index test and reference standard domains, also raises unclear concerns. Due to the limited amount of data, it was not possible to estimate the cause of heterogeneity in the results of each study. Therefore, the uncertainty of the present results should be noted.
Our meta‐analysis yielded better diagnostic values of Doppler echocardiography as compared with several systematic reviews on the same topic (Janda 2011; Taleb 2013; Zhang 2010). The difference might be due to the discrepancy in reference standards between the previous and current reviews. We used a strict reference standard that is likely to diagnose the target condition with a high degree of accuracy. On the other hand, the three reviews included studies where the interval between the index test and the reference standard was more than one week. Both echocardiography and right‐heart catheterisation are subject to disagreement when performed at different times (e.g. days or weeks apart), which is a major limitation of the studies that compare their accuracy in the diagnosis of PH. For example, any treatment would be performed if the results of echocardiography suggested pulmonary hypertension (Delcroix 2010). This could lead to negative results for a reference standard performed a few weeks or months later, which means that the false positive rate increases and specificity decreases. We therefore excluded studies with an interval of more than a week to obtain unbiased estimates.
The included studies adopted a variety of thresholds to diagnose PH (30 to 47 mmHg). Therefore, we used the HSROC model to take the variation into account. We also performed the post hoc subgroup analysis by the threshold categories. The analysis did not show a clear threshold effect in the range of thresholds. However, higher thresholds ≥ 40 mmHg might be avoided based on the role as a triage test.
Strengths and weaknesses of the review
We conducted a thorough literature search and included full‐text publications and abstracts without any language restrictions. There are currently no reliable search strategies to identify diagnostic test accuracy studies (Beynon 2013). The major strengths of the review are as follows: we did not use any diagnostic filters in our search strategy, which ensured that all studies on the topic were identified. PH was defined when the mean pulmonary arterial pressure assessed by right‐heart catheterisation was ≥ 25 mmHg (Simonneau 2013). This strict reference standard was used as it likely could diagnose the target condition with a high degree of accuracy.
This review has several limitations. First, many studies were excluded due to insufficient diagnostic test accuracy data. Of the 131 studies excluded at full‐text screening, 85 studies were excluded because of lack of diagnostic accuracy data, which matched the inclusion criteria of our review. If some of these studies could have been included in our review, the results of our review might have changed. Second, we attempted to obtain detailed data by contacting the authors of included studies, but most of them were not available, especially for studies that were published as conference abstracts. The space limitations for the publication of a conference abstract would yield unclear risk of bias judgements rather than low or high judgements during the QUADAS‐2 assessment. Furthermore, due to the lack of information, there might be potential patient overlap between Mo 2015 and Mo 2015a. Third, there was a high proportion of studies that were judged at high risk of bias on the flow and timing domain and with high concern regarding applicability in the patient selection domain of the QUADAS‐2 tool.
Applicability of findings to the review question
Although our review collated all available evidence on the diagnostic accuracy of Doppler echocardiography for PH, the applicability of our findings to the review question was limited. PH was highly prevalent among the participants in the included studies. For example, the mean systolic pulmonary arterial pressure was 62.3 mmHg and the prevalence of PH was 86% in Er 2010. It is questionable if the triage test is needed in such a high‐prevalence setting. The care settings were mostly hospitals such as university hospitals, cardiovascular centres, and lung and liver transplant centres. Findings from such settings may be difficult to apply to other settings that play a triage role for assessment of PH. Our sensitivity analysis did not show a dose‐response relationship between prevalence and diagnostic accuracy of Doppler echocardiography; however, it was not conclusive as the CIs were substantially wide due to the limited data. We could not investigate the potential reason for the variety of prevalence due to the poor reporting of patient characteristics including WHO classification of PH. Additionally, there was limited information on the symptoms that the participants had. In the four studies that reported the information on symptoms, the proportion of mild or asymptomatic patients was small.
Authors' conclusions
Implications for practice.
Our evidence assessment of echocardiography for the diagnosis of PH in adult patients revealed several limitations.
Current available data indicate generally poor methodological and reporting quality of the evidence. Due to their heterogeneity, we were unable to determine average sensitivity and specificity at any particular index test threshold and could not explain the observed variability in results.
Implications for research.
To determine if the Doppler echocardiography is a useful triage test, we need more studies with transparent reporting and high methodological quality. There is room for further study on the optimal threshold to diagnose PH by trans‐thoracic Doppler echocardiography. The influence of different types of PH, methods of estimating right atrial pressure, and the use of ventilation on the accuracy of diagnosis needs to be investigated.
What's new
| Date | Event | Description |
|---|---|---|
| 25 May 2022 | Amended | Amended to rectify display of figures. |
History
Protocol first published: Issue 9, 2017 Review first published: Issue 5, 2022
Acknowledgements
We thank Elizabeth Stovold, Information Specialist of the Cochrane Airway Group, for designing our search strategy. We thank Dr. Amsallem for correspondence and sending us unpublished data.
We thank the following translators for data extraction and QUADAS‐2 assessment of various articles:
Anja Lieder, Katja Boehm, Liliya Eugenevna Ziganshina, Pascale Hess and Rachael Kelly.
The Cochrane Diagnostic Test Accuracy Editorial Team helped to edit this manuscript and commented critically on the protocol.
The authors and Cochrane Airways Editorial Team are grateful to the following peer reviewers for their time and comments:
Tim Donovan, University of Cumbria, UK;
Alan L Hinderliter, University of North Carolina, USA; and
Prof Dr Tim Seidler, University of Göttingen, Germany.
This project was supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding to the Cochrane Airways Group. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service (NHS), or the Department of Health and Social Care.
Appendices
Appendix 1. World Health Organization (WHO) functional classification for pulmonary hypertension
| Class | WHO functional classification for pulmonary hypertension |
| I | Patients with pulmonary hypertension but without resulting limitations of physical activity. Ordinary physical activity does not cause undue fatigue or dyspnoea, chest pain, or heart syncope. |
| II | Patients with pulmonary hypertension resulting in slight limitation of physical activity. They are comfortable at rest. Ordinary physical activity results in undue fatigue or dyspnoea, chest pain, or heart syncope. |
| III | Patients with pulmonary hypertension resulting in marked limitation of physical activity. They are comfortable at rest. Less‐than‐ordinary physical activity causes undue fatigue or dyspnoea, chest pain, or heart syncope. |
| IV | Patients with pulmonary hypertension resulting in inability to carry on any physical activity without symptoms. These patients manifest signs of right‐heart failure. Dyspnoea or fatigue, or both, may be present even at rest. Discomfort is increased by physical activity. |
Appendix 2. MEDLINE (Ovid) search strategy
1. exp Hypertension, Pulmonary/ 2. Pulmonary Heart Disease/ 3. (pulmonary adj3 hypertens$).tw. 4. pulmonary vascular disease.tw. 5. or/1‐4 6. exp Echocardiography/ 7. (echocardiogra$ or echo‐cardiogra$).tw. 8. doppler.tw. 9. or/6‐8 10. 5 and 9 11. Animals/ not (Animals/ and Humans/) 12. 10 not 11
Appendix 3. Embase (Ovid) search strategy
1. exp pulmonary hypertension/ 2. pulmonary vascular disease/ 3. (pulmonary adj3 hypertens$).tw. 4. or/1‐3 5. exp Doppler echocardiography/ 6. doppler.tw. 7. 5 or 6 8. 4 and 7 9. (exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/) not ((human/ or normal human/ or human cell/) and (exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/)) 10. 8 not 9
Appendix 4. Web of Science search strategy
#1 TS=(pulmonary NEAR hypertension) OR TS=pulmonary heart disease #2 TS=(doppler* NEAR echocardiograph*) #3 #2 AND #1
Appendix 5. ClinicalTrials.gov and WHO ICTRP search strategy
| Field | Search term |
| condition | pulmonary hypertension |
| intervention | doppler |
Appendix 6. Study quality assessment details
Domain 1: Patient selection
Risk of bias: Could the selection of patients have introduced bias?
Signaling question 1: Was a consecutive or random sample of patients enrolled? Signaling question 2: Did the study avoid inappropriate exclusions?
Studies that make inappropriate exclusions, for example, excluding 'difficult to diagnose' patients, whose image of echocardiography is difficult to detect due to obesity or overinflated lungs, may result in overoptimistic estimates of diagnostic accuracy. We will classify the studies as 'yes' if all patients were included in the study regardless of clinical suspicion following index test, 'no' if they conduct any inappropriate exclusions, for example, excluding patients with low clinical suspicion based on the index test, and 'unclear' if this information is not clear.
Applicability: Are there concerns that the included patients and the setting do not match the review question?
If studies include only a clinically relevant population that would have undergone the index test in real practice and includes a representative form of target condition, we will assess as 'low' concern. If the study population differed from the population defined in the review question in terms of demographic features (e.g. studies include mainly younger patients or specific group of WHO classification), we will assess as 'high' concern. If this information is unclear (e.g. WHO classification was not reported), we will assess as 'unclear'.
Domain 2: Index test
Risk of bias: Could the conduct or interpretation of the index test have introduced bias?
Signaling question 1: Were the index test results interpreted without knowledge of the results of the reference standard? Signaling question 2: If a threshold was used, was it prespecified?
We will classify the study as 'yes' if echocardiography results were interpreted without knowledge of the reference standard, 'no' if the echocardiography tests were interpreted with knowledge of the reference standard results, and 'unclear' if this information is not clear. We will classify the study as 'yes' if a threshold was prespecified, 'no' if authors selected a cut‐off value based on the analysis of data collected, and 'unclear' if insufficient information is provided.
Applicability: Are there concerns that the index test, its conduct, or its interpretation differ from the review question?
We will include studies where systolic pulmonary artery pressure calculated from the maximum tricuspid regurgitation jet velocity by using the modified Bernoulli equation and adding right atrial pressure evaluation of pulmonary artery pressure by echocardiography is an index test regardless of threshold, and we will include index tests using various right atrial pressure estimation methods. However, the most common method is using the diameter and collapse of the inferior vena cava during spontaneous respiration. We will therefore judge studies where the right atrial pressure was estimated by using the diameter and collapse of the inferior vena cava during spontaneous respiration as 'low' concern, those where right atrial pressure was estimated by using any other method as 'high' concern, and 'unclear' concern if this information is not clear.
Domain 3: Reference standard
Risk of bias: Could the reference standard, its conduct, or its interpretation have introduced bias?
Signaling question 1: Were the reference standard results interpreted without knowledge of the results of the index test? Signaling question 2: Were the criteria of reference standard for the target condition prespecified?
We will classify the study as 'yes' if right‐heart catheterisation results were interpreted without knowledge of the index test, 'no' if right‐heart catheterisation was interpreted with knowledge of the index test results, and 'unclear' if this information is not clear. We will classify the study as 'yes' if the criteria of the reference standard for the target condition were prespecified, 'no' if the criteria of the reference standard for the target condition were not prespecified, and 'unclear' if this information is not clear.
Applicability: Are there concerns that the target condition as defined by the reference standard does not match the question?
The target condition is pulmonary hypertension defined as mean pulmonary artery pressure assessed by right‐heart catheterisation of 25 mmHg or higher (Hoeper 2013). Use of right‐heart catheterisation for the reference standard and the threshold of 25 mmHg are inclusion criteria for this review, so we anticipate that all studies will be classified as 'low' concern.
Domain 4: Flow and timing
Risk of bias: Could the patient flow have introduced bias?
Signaling question 1: Was the interval between the index test and reference standard less than one day? Signaling question 2: Did all patients receive the same reference standard? Signaling question 3: Were all patients included in the analysis?
Both echocardiography and right‐heart catheterisation are subject to disagreement when performed at different times (e.g. days or weeks apart), which is a major limitation of the studies that compare their accuracy in the diagnosis of pulmonary hypertension (Lewis 2016). We will classify the study as 'yes' if there is a delay of less than a day, 'no' if there is a delay of more than or equal to a day, and 'unclear' if the information is not clear. We will classify the study as 'yes' if all patients had the same reference standard, 'no' if some included patients did not undergo the same reference standard, and 'unclear' if this information is not clear. Uninterpretable results may be present (e.g. unclear echocardiography or failure to insert right‐heart catheterisation). Additionally, withdrawals from the study may be present. We anticipate that uninterpretable results would occur associated with the severity of pulmonary hypertension (e.g. difficulty in detecting Doppler echocardiography among severe chronic obstructive pulmonary disease patients due to overinflated lung) and not at random. If uninterpretable results are withdrawn from analysis, diagnostic accuracy will be overestimated. We will classify the study as 'yes' if uninterpretable results were reported and the study had no withdrawals or the withdrawals were unlikely to affect the results; 'no' if uninterpretable results were not reported or there were withdrawals that were likely to affect the results, or both; and 'unclear' if this information is not clear.
Data
Presented below are all the data for all of the tests entered into the review.
Tests. Data tables by test.
| Test | No. of studies | No. of participants |
|---|---|---|
| 1 Doppler trans‐thoracic echocardiography | 17 | 3656 |
| 2 Sensitivity analysis 1 | 4 | 254 |
1. Test.
Doppler trans‐thoracic echocardiography
2. Test.
Sensitivity analysis 1
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Amsallem 2016.
| Study characteristics | |||
| Patient Sampling | Retrospective | ||
| Patient characteristics and setting |
Study location: USA Study periods: between 2001 and 2012 Care setting: the Stanford University Advanced Lung Disease centre, Kosuyolu Training Hospital Participants enrolled: 307: 125 males and 182 females Participants included in analysis: 199: gender not reported Age: mean age 50 ± 13 years BMI: not reported Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): not reported Number of patients with asymptomatic or mild symptom: not reported Number of participants with COPD: not reported Number of intubated participants: 0 Inclusion criteria: All participants aged > 18 years referred to the Stanford University Advanced lung disease centre for right‐heart catheterisation and with right‐heart catheterisation and complete echocardiography within 5 days Exclusion criteria: not reported |
||
| Index tests |
Description of index test: Resting trans‐thoracic echocardiography was performed using the Philips 7500 or iE33 system (Philips Medical Systems, Andover, MA) with 5‐MHz transducers by experienced, credentialed cardiac sonographers. Right ventricular systolic pressure was estimated from the maximal right ventricular–right atrial pressure gradient, using the modified Bernoulli equation 5: right ventricular systolic pressure = 4 (maximal tricuspid regurgitation velocity)2 + right atrial pressure, where maximal tricuspid regurgitation velocity was measured using continuous wave Doppler Description of method to estimate right atrial pressure: Right atrial pressure was estimated in the subcostal view according to the inferior vena cava size and collapsibility following a normal sniff: 3 mmHg if IVC < 15 mm and collapse > 50%, 5 mmHg if IVC between 15 and 21 mm and collapse > 50%, 15 mmHg if IVC > 21 mm and collapse between 10% and 50%, 20 mmHg if IVC > 21 mm and collapse < 10%, and 10 mmHg in all other cases. Cut‐off value to declare PH: 40 mmHg Estimated systolic pulmonary arterial pressure: not reported Sonographer qualification: performed by experienced, credentialed cardiac sonographers How to handle the uninterpretable results: excluded from analysis |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: A balloon catheter was introduced through the right femoral vein or internal jugular vein after local anaesthesia. Patients could be premedicated with 1 to 3 mg of diazepam 30 min before the procedure. Mean pulmonary arterial pressure: mean 36.5 ± 17.8 mmHg |
||
| Flow and timing | The interval between the index test and reference standard: within 48 hours Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: not stated |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the criteria of reference standard for target condition prespecified? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | No | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Could the patient flow have introduced bias? | High risk | ||
Balci 2016.
| Study characteristics | |||
| Patient Sampling | Prospective | ||
| Patient characteristics and setting |
Study location: Turkey Study periods: between January 2012 and September 2015 Care setting: the lung transplantation unit of Kartal Kosuyolu Training Hospital Participants enrolled: 103: 67 males and 36 females Participants included in analysis: 103: 67 males and 36 females Age: median age 48 years (range: 18‐70 years) BMI: mean BMI 24 Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): Class I: 0, Class II: 0, Class III: 59, Class IV: 0, Class V: 0 Number of patients with asymptomatic or mild symptom: not reported Number of participants with COPD: 54 Number of intubated participants: 0 Inclusion criteria: We included patients with the diagnosis of end‐stage lung disease who were referred as lung transplantation candidates to the lung transplantation unit of Kartal Kosuyolu Training Hospital Exclusion criteria: not reported |
||
| Index tests |
Description of index test: Doppler echocardiography was implemented with the use of conventional clinical echocardiographic equipment (Philips iE33 xMATRIX ultrasound system, Andover, Mass, United States). Transthoracic Doppler and 2‐dimensional images were gained from parasternal long‐ and short‐axis, apical 4‐chamber, and subcostal 4‐chamber views. Description of method to estimate right atrial pressure: not reported Cut‐off value to declare PH: 35 mmHg Estimated systolic pulmonary arterial pressure: median 45 mmHg (range: 20‐144 mmHg) Sonographer qualification: not reported How to handle the uninterpretable results: not applicable |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: Right‐heart catheterisation was performed with the use of a balloon‐tipped, flow directed pulmonary artery catheter. The catheter was introduced via the right femoral vein or right internal jugular vein, using the Seldinger technique under local anaesthesia. The following measurements were obtained in duplicate: right atrial pressures, pulmonary artery systolic and diastolic pressures, pulmonary artery occlusion pressure, and cardiac output. Mean pulmonary arterial pressure: median 26 mmHg (IQR: 20‐35 mmHg) |
||
| Flow and timing | The interval between the index test and reference standard: within 72 hours Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: 0 (0%) |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the criteria of reference standard for target condition prespecified? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | No | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Could the patient flow have introduced bias? | High risk | ||
Colle 2003.
| Study characteristics | |||
| Patient Sampling | Prospective | ||
| Patient characteristics and setting |
Study location: France Study periods: between April 1993 and August 2001 Care setting: Service d’H ´epatologie and INSERM Participants enrolled: 165: 116 males and 49 females Participants included in analysis: 165: 116 males and 49 females Age: mean age 48 ± 8 years BMI: not reported Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): Class I: 17, Class II: 0, Class III: 0, Class IV: 0, Class V: 0 Number of patients with asymptomatic or mild symptom: not reported Number of participants with COPD: not reported Number of intubated participants: 0 Inclusion criteria: consecutive patients who were evaluated for liver transplantation and for whom transvenous liver biopsy was needed were prospectively included in this study Exclusion criteria: none |
||
| Index tests |
Description of index test: All patients were evaluated with a 2‐dimensional Doppler echocardiography on a Sonos 1500 Hewlett‐Packard or a Supervision 800 Vingmed machine. Continuous wave Doppler of tricuspid regurgitant jet, when present, was used to calculate right ventricular systolic pulmonary artery pressure with the formula: systolic pulmonary artery pressure (4 maximum velocity of the tricuspid regurgitant jet2) mean right atrial pressure. Description of method to estimate right atrial pressure: setting mean right atrial pressure at 5 mmHg, except when the inferior vena cava was collapsed (0 mmHg) or clearly enlarged with no collapse during inspiration (10 mmHg) Cut‐off value to declare PH: 30 mmHg Estimated systolic pulmonary arterial pressure: not reported Sonographer qualification: not reported How to handle the uninterpretable results: not applicable |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: a catheter was inserted into the right or left jugular vein under local anaesthesia. Haemodynamic measurements including pulmonary artery pressure, right atrial pressure, and pulmonary capillary wedge pressure were performed using a Swan‐Ganz catheter. Cardiac output was measured by the thermodilution method (Baxter Healthcare Corporation, Santa Ana, CA). Cardiac output was obtained by the average of 3 consecutive measurements. Arterial pressure was measured using a noninvasive external sphygmomanometer (Dinamap; Critikon, Tampa, FL). Systemic vascular resistance was calculated as follows: systemic vascular resistance (dynes.s.cm 5) (mean arterial pressure‐mean right atrial pressure) 80/cardiac output. Pulmonary vascular resistance (PVR) was calculated as follows: pulmonary vascular resistance (dynes.s.cm 5) (mean pulmonary arterial pressure‐pulmonary capillary wedged pressure) 80/cardiac output. Mean pulmonary arterial pressure: mean 18.8 ± 7.6 mmHg |
||
| Flow and timing | The interval between the index test and reference standard: within the same week Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: 0 (0%) |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the criteria of reference standard for target condition prespecified? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | No | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Could the patient flow have introduced bias? | High risk | ||
Er 2010.
| Study characteristics | |||
| Patient Sampling | Prospective | ||
| Patient characteristics and setting |
Study location: Germany Study periods: from December 2008 to June 2010 Care setting: the Cardiology Department of the University of Cologne Participants enrolled: 50 Participants included in analysis: 50: 14 males and 36 females Age: mean age 66.9 ± 14.5 years BMI: mean 27.1 ± 5.1 Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): not reported Number of patients with asymptomatic or mild symptom: 6 (8%) Number of participants with COPD: not reported Number of intubated participants: 0 Inclusion criteria: Consecutive patients referred to the Cardiology Department of the University of Cologne were included. Exclusion criteria: Patients were excluded when tricuspid regurgitation jet was not available. |
||
| Index tests |
Description of index test: using a Phillips iE33 ultrasound device equipped with a standard transducer operating at 1–5 MHz without using saline contrast. The echocardiography was performed by three different cardiologists. In each patient only one cardiologist performed the examination, randomly. Multiple views were recorded to identify optimal view for analysis as recommended in actual guidelines. Description of method to estimate right atrial pressure: The right atrial pressure was estimated by evaluating IVC diameter and change with respiration: when IVC diameter was less than 20 mm and the collapsibility greater than 50%, right atrial pressure was estimated to be 5 mmHg versus 10 mmHg when the collapsibility was less than 50%. When the IVC diameter was greater than 20 mm, right atrial pressure was estimated to be 15 mmHg when the collapsibility was greater than 50% and to be 20 mmHg when the collapsibility was less than 50%. Cut‐off value to declare PH: 38 mmHg Estimated systolic pulmonary arterial pressure: mean 62.3 ± 25.7 mmHg Sonographer qualification: performed by cardiologists How to handle the uninterpretable results: not applicable |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: Right‐heart catheterisation was performed without sedation at rest in the cardiac catheter laboratory of the Cardiology Department of the University of Cologne. End‐expiratory pressure measurements were taken from the right atrium, right ventricle, pulmonary artery and pulmonary capillary. Mean pulmonary arterial pressure: mean 39.5 ± 14.9 mmHg |
||
| Flow and timing | The interval between the index test and reference standard: within 120 minutes Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: 0 (0%) |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the criteria of reference standard for target condition prespecified? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Greiner 2014.
| Study characteristics | |||
| Patient Sampling | Retrospective | ||
| Patient characteristics and setting |
Study location: Germany Study periods: from July 1, 2007 through June 30, 2013 Care setting: Cardiology Department of the University Hospital of Heidelberg, Germany Participants enrolled: 3920: gender not reported Participants included in analysis: 1695: 1136 males and 559 females Age: mean age 63 ± 15 BMI: mean 26 ± 5 Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): not reported Number of patients with asymptomatic or mild symptom: 85 (5%) Number of participants with COPD: not reported Number of intubated participants: 0 Inclusion criteria: All patients who had a cardiac ultrasound examination performed within 5 days before or after invasive examination Exclusion criteria: Patients whose pulmonary arterial pressure documents were not explicitly documented |
||
| Index tests |
Description of index test: Noninvasive assessment of systolic pulmonary arterial pressure was achieved by measurement of right ventricular systolic pressure and adding right atrial pressure. Right ventricular systolic pressure was derived from the peak systolic velocity of the tricuspid regurgitation obtained with continuous‐wave Doppler using the modified Bernoulli equation: pressure gradient = 49Vmax2. Description of method to estimate right atrial pressure: Right atrial pressure was estimated by the diameter of the inferior vena cava and its variability during inspiration. Cut‐off value to declare PH: 36 mmHg Estimated systolic pulmonary arterial pressure: mean 45.3 ± 15.5 mmHg Sonographer qualification: performed by two independent, experienced examiners How to handle the uninterpretable results: excluded from analysis |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: A femoral or jugular venous approach was used for right‐heart catheterisation. Cardiac output and cardiac index were calculated by saturation measurement according to Fick's method. Pulmonary arterial pressure, pulmonary capillary wedge pressure, and right ventricular and right atrial pressures were measured during breath hold in baseline over at least 3 heart cycles. Mean pulmonary artery pressure was calculated by integration of the pressure curve by Metek software (Metek GmbH, Roetgen, Germany). Mean pulmonary arterial pressure: mean 31.6 ± 10.9 mmHg |
||
| Flow and timing | The interval between the index test and reference standard: within five days Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: not stated |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | No | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the criteria of reference standard for target condition prespecified? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | No | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Could the patient flow have introduced bias? | High risk | ||
Hellenkamp 2018.
| Study characteristics | |||
| Patient Sampling | Retrospective | ||
| Patient characteristics and setting |
Study location: UK and Germany Study periods: between 2011 and 2016 Care setting: the Clinic for Cardiology and Pneumology, University Medical Center Göttingen; King's College Hospital, London; and the Department of Internal Medicine II, University of Regensburg Participants enrolled: 90: 43 males and 47 females Participants included in analysis: 90: 43 males and 47 females Age: mean age 64.8 years (IQR: 55‐79 years) BMI: not reported Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): not reported Number of patients with asymptomatic or mild symptom: 24 (16%) Number of participants with COPD: not reported Number of intubated participants: 0 Inclusion criteria: patients who underwent echocardiography and right‐heart catheterisation within 24 hours Exclusion criteria: not reported |
||
| Index tests |
Description of index test: continuous‐wave Doppler ultrasonography of tricuspid regurgitation in apical four‐chamber and parasternal short‐axis views was applied, and the tricuspid regurgitation time‐velocity tracing was determined to obtain the time‐velocity integral, tricuspid regurgitation max velocity, mean tricuspid regurgitation velocity, maximal right atrial–right ventricular gradient, and TRP mean. Description of method to estimate right atrial pressure: Right atrial pressure was estimated by measuring the diameter of the IVC at end expiration and the inspiratory collapsibility in the subcostal view as follows: when the IVC diameter was #21 mm and the collapsibility with a sniff was > 50%, right atrial pressure was estimated to be 3 mmHg; when the IVC diameter was > 21 mm and the collapsibility was < 50%, right atrial pressure was estimated to be 15 mmHg. In all other cases (either IVC diameter > 21 mm and collapse > 50% or IVC diameter #21 mm and collapse < 50%), right atrial pressure was estimated to be 8 mmHg. Cut‐off value to declare PH: 31 mmHg Estimated systolic pulmonary arterial pressure: not reported Sonographer qualification: not reported How to handle the uninterpretable results: not applicable |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: not reported Mean pulmonary arterial pressure: median 35 mmHg (IQR: 24.7‐46.2 mmHg) |
||
| Flow and timing | The interval between the index test and reference standard: within 24 hours Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: 0 (0%) |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the criteria of reference standard for target condition prespecified? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Hsu 2008.
| Study characteristics | |||
| Patient Sampling | Prospective | ||
| Patient characteristics and setting |
Study location: USA Study periods: between 2002 and 2004 Care setting: not reported Participants enrolled: 55: gender not reported Participants included in analysis: 49: 9 males and 40 females Age: mean age 55 years (range 20‐80 years) BMI: not reported Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): Class I: 16, Class II: 0, Class III: 0, Class IV: 0, Class V: 0 Number of patients with asymptomatic or mild symptom: not reported Number of participants with COPD: not reported Number of intubated participants: 0 Inclusion criteria: We performed a prospective review of established or new patients who presented consecutively to the University of Medicine and Dentistry of New Jersey‐Scleroderma Program between 2002 and 2004 with progressive dyspnoea and/or had clinical features suspicious of PH. Exclusion criteria: Patients were excluded if they had left ventricle dysfunction by echo or right‐heart catheterisation, airway obstruction by pulmonary function tests, thromboembolic pulmonary hypertension (excluded by ventilation/perfusion scan), congenital heart disease, porto‐pulmonary PH, or HIV, and those who refused right‐heart catheterisation or cardiac magnetic resonance imaging. |
||
| Index tests |
Description of index test: Echo images were obtained using a Philips Sonos 7500 model. Tricuspid regurgitant flow velocity was measured by continuous‐wave echo with both an imaging probe and a non‐imaging Pedoff pencil probe. No contrast enhancement was given. RVSP was estimated from the peak tricuspid regurgitant flow velocity (v, in m/s) using a modified Bernoulli equation, P = 4v2 + 10, where P represents the pressure in mmHg. All echo‐Doppler studies were read by a single reader. Description of method to estimate right atrial pressure: 10 mmHg Cut‐off value to declare PH: 47 mmHg Estimated systolic pulmonary arterial pressure: not reported Sonographer qualification: not reported How to handle the uninterpretable results: excluded from analysis |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: Right‐heart catheterisation was performed by percutaneous approach via the femoral vein using a 7‐French Swan‐Ganz catheter (Edwards Lifesciences). Baseline pressures were recorded in the right atrium, right ventricle, PA, and PCW position .Mean pulmonary arterial pressure: mean 25.3 mmHg (range: 11‐58 mmHg) |
||
| Flow and timing | The interval between the index test and reference standard: within 4 hours Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: not stated |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | High | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the criteria of reference standard for target condition prespecified? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Could the patient flow have introduced bias? | Low risk | ||
Kyranis 2018.
| Study characteristics | |||
| Patient Sampling | Prospective | ||
| Patient characteristics and setting |
Study location: Australia Study periods: not reported Care setting: quaternary cardiopulmonary specialist hospital Participants enrolled: 100: 43 males and 57 females Participants included in analysis: 96: gender not reported Age: mean age 58 ± 14 years BMI: mean 28 ± 6 Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): not reported Number of patients with asymptomatic or mild symptom: not reported Number of participants with COPD: not reported Number of intubated participants: 0 Inclusion criteria: patients undergoing clinically indicated right‐heart catheterisation were prospectively enrolled. Exclusion criteria: not reported |
||
| Index tests |
Description of index test: Both sonographers and reporting cardiologists were blinded to the invasive data. Echocardiographic examinations were performed by experienced sonographers using commercially available ultrasound systems (Vivid I, Vivid 7, and Vivid E9, GE Healthcare, Vingmed, Trondheim Norway and iE33, Philips, Eindhoven, The Netherlands) using 1.5–4.0 MHz matrix‐array and phase array transducers according to the guidelines of the American Society of Echocardiography. Description of method to estimate right atrial pressure: Right atrial pressure was estimated to be 3 mmHg when the IVC diameter was < 21 mm with > 50% collapsibility, 8 mmHg when the IVC diameter was < 21 mm with < 50% collapsibility, and 15 mmHg when the IVC diameter was > 21 mm with < 50% collapsibility, as per current American Society of Echocardiography guidelines. Cut‐off value to declare PH: 31 mmHg Estimated systolic pulmonary arterial pressure: mean 54.7± 22.7 mmHg Sonographer qualification: performed by experienced sonographer How to handle the uninterpretable results: excluded from analysis |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: Right‐heart catheterisation via the jugular or femoral venous approach was performed by experienced accredited cardiologists with established skills in right‐heart catheterisation. Mean pulmonary arterial pressure: mean 43.2± 15 mmHg |
||
| Flow and timing | The interval between the index test and reference standard: within 24 hours Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: not stated |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the criteria of reference standard for target condition prespecified? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Could the patient flow have introduced bias? | High risk | ||
Lafitte 2013.
| Study characteristics | |||
| Patient Sampling | Retrospective | ||
| Patient characteristics and setting |
Study location: France Study periods: between June 2011 and March 2012 Care setting: the cardiac catheterisation department, which performs approximately 4500 right‐heart catheterisation procedures every year, and from the echocardiography department, which conducts > 15,000 trans‐thoracic Doppler echocardiographic studies every year Participants enrolled: 310: 162 males and 148 females Participants included in analysis: 155: gender not reported Age: mean age 64.8 ± 15.9 years BMI: mean 26.3± 5.7 Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): not reported Number of patients with asymptomatic or mild symptom: not reported Number of participants with COPD: not reported Number of intubated participants: 0 Inclusion criteria: The inclusion criterion for patient enrolment was having undergone both haemodynamic and echocardiographic investigations (with estimation of pulmonary pressures by Doppler on tricuspid regurgitant flow) between June 2011 and March 2012, irrespective of the causal disease, during a single hospitalisation period. Exclusion criteria: a lack of pulmonary pressures estimation on the basis of tricuspid regurgitant flow using Doppler echocardiography |
||
| Index tests |
Description of index test: All echocardiographic measurements were performed according to American Society of Echocardiography and European Association of Echocardiography recommendations in line with UERD standard operating procedure. Accordingly, tricuspid regurgitant maximum velocities were measured on the basis of adequate acquisitions, and estimated systolic pulmonary arterial pressure levels were determined using the modified Bernoulli equation when tricuspid regurgitant jets were analysable, in conjunction with echocardiographic estimation of right atrial pressure. Description of method to estimate right atrial pressure: Echocardiographic right atrial pressure estimation was performed on the basis of IVC size and collapsibility. Right atrial pressure was estimated to be 3 mmHg when the IVC diameter was < 21 mm with > 50% collapsibility, 8 mmHg when the IVC diameter was < 21 mm with < 50% collapsibility, and 15 mmHg when the IVC diameter was > 21 mm with < 50% collapsibility. Cut‐off value to declare PH: 38 mmHg Estimated systolic pulmonary arterial pressure: mean 49.6 ± 21.7 mmHg Sonographer qualification: underwent systematic validation by one of the senior cardiologists How to handle the uninterpretable results: excluded from analysis |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: Senior physicians specialising in invasive techniques performed the catheterisations according to standard procedures. Fluid‐filled catheters were used for patients not sedated. Systolic, diastolic, and mean PPs were averaged and calculated over five beats. Mean pulmonary arterial pressure: mean 32.7 ± 15.3 mmHg |
||
| Flow and timing | The interval between the index test and reference standard: mean interval 2 days ± 2.9 days Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: not stated |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the criteria of reference standard for target condition prespecified? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | No | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Could the patient flow have introduced bias? | High risk | ||
Mazhar 2011.
| Study characteristics | |||
| Patient Sampling | Retrospective | ||
| Patient characteristics and setting |
Study location: New Zealand Study periods: between January 2004 and February 2011 Care setting: not reported Participants enrolled: 159: gender not reported Participants included in analysis: 99: gender not reported Age: not reported BMI: not reported Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): not reported Number of patients with asymptomatic or mild symptom: not reported Number of participants with COPD: not reported Number of intubated participants: not reported Inclusion criteria: Patients having a trans‐thoracic echocardiography and right‐heart catheterisation within three days of each other Exclusion criteria: not reported |
||
| Index tests |
Description of index test: not reported Description of method to estimate right atrial pressure: not reported Cut‐off value to declare PH: 31 mmHg Estimated systolic pulmonary arterial pressure: not reported Sonographer qualification: not reported How to handle the uninterpretable results: excluded from analysis |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: not reported Mean pulmonary arterial pressure: not reported |
||
| Flow and timing | The interval between the index test and reference standard: within 3 days Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: not stated |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the criteria of reference standard for target condition prespecified? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | No | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Could the patient flow have introduced bias? | High risk | ||
Mo 2015.
| Study characteristics | |||
| Patient Sampling | Retrospective | ||
| Patient characteristics and setting |
Study location: USA Study periods: not reported Care setting: not reported Participants enrolled: 30: gender not reported Participants included in analysis: 24: gender not reported Age: not reported BMI: not reported Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): not reported Number of patients with asymptomatic or mild symptom: not reported Number of participants with COPD: not reported Number of intubated participants: not reported Inclusion criteria: Adults with echo and right‐heart catheterisation within one week Exclusion criteria: not reported |
||
| Index tests |
Description of index test: estimable right ventricular systolic pressure by echocardiography Description of method to estimate right atrial pressure: not reported Cut‐off value to declare PH: 35 mmHg Estimated systolic pulmonary arterial pressure: not reported Sonographer qualification: not reported How to handle the uninterpretable results: excluded from analysis |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: right‐heart catheterisation Mean pulmonary arterial pressure: not reported |
||
| Flow and timing | The interval between the index test and reference standard: within one week Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: not stated |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Could the selection of patients have introduced bias? | Unclear risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the criteria of reference standard for target condition prespecified? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | No | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Could the patient flow have introduced bias? | High risk | ||
Mo 2015a.
| Study characteristics | |||
| Patient Sampling | Retrospective | ||
| Patient characteristics and setting |
Study location: USA Study periods: not reported Care setting: not reported Participants enrolled: 87: gender not reported Participants included in analysis: 87: gender not reported Age: not reported BMI: not reported Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): not reported Number of patients with asymptomatic or mild symptom: not reported Number of participants with COPD: not reported Number of intubated participants: not reported Inclusion criteria: We selected adults who underwent echo and right‐heart catheterisation within one week. Exclusion criteria: not reported |
||
| Index tests |
Description of index test: not reported Description of method to estimate right atrial pressure: not reported Cut‐off value to declare PH: 45 mmHg Estimated systolic pulmonary arterial pressure: not reported Sonographer qualification: not reported How to handle the uninterpretable results: excluded from analysis |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: right‐heart catheterisation Mean pulmonary arterial pressure: not reported |
||
| Flow and timing | The interval between the index test and reference standard: within one week Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: 0 (0%) |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the criteria of reference standard for target condition prespecified? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | No | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Could the patient flow have introduced bias? | High risk | ||
Nowak 2018.
| Study characteristics | |||
| Patient Sampling | Retrospective | ||
| Patient characteristics and setting |
Study location: Poland Study periods: between April 2007 and December 2011 Care setting: the Silesian Center of Heart Disease Participants enrolled: 65: 49 males and 16 females Participants included in analysis: 37: males and females Age: mean age 53.3 ± 9.5 years BMI: mean 24.1 ± 4.3 Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): not reported Number of patients with asymptomatic or mild symptom: 2 (3%) Number of participants with COPD: 31 Number of intubated participants: 0 Inclusion criteria: patients with advanced lung disease who underwent right‐heart catheterisation Exclusion criteria: patients with IPH were excluded. |
||
| Index tests |
Description of index test: All patients underwent transthoracic echocardiography, including M‐mode, 2‐dimensional, pulsed, continuous‐wave, and colour‐flow Doppler imaging using the GE VIVID 5 system and a transducer array of 2.5 MHz, according to the guidelines of the American Society of Cardiology. Description of method to estimate right atrial pressure: not reported Cut‐off value to declare PH: 43 mmHg Estimated systolic pulmonary arterial pressure: mean 54.2 ± 21.5 mmHg Sonographer qualification: not reported How to handle the uninterpretable results: excluded from analysis |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: All patients were clinically stable with no changes in medical therapy. This procedure was performed at rest in supine position, using a Swan‐ganz catheter. Measurements were performed using supplemental oxygen, if needed, to achieve saturation over 90%. Mean pulmonary arterial pressure: mean 28.8 ± 11.5 mmHg |
||
| Flow and timing | The interval between the index test and reference standard: mean interval 3 days ± 1.7 days Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: not stated |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the criteria of reference standard for target condition prespecified? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | No | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Could the patient flow have introduced bias? | High risk | ||
Sawada 2019.
| Study characteristics | |||
| Patient Sampling | Retrospective | ||
| Patient characteristics and setting |
Study location: Japan Study periods: between July 2005 and December 2012 Care setting: the University of Tokyo Participants enrolled: 189: 106 males and 83 females Participants included in analysis: 189: 106 males and 83 females Age: mean age 58 ± 17 years BMI: 22 ± 3 Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): not reported Number of patients with asymptomatic or mild symptom: not reported Number of participants with COPD: not reported Number of intubated participants: not reported Inclusion criteria: Patients with heart disease who underwent right‐heart catheterisation were included. Exclusion criteria: Participants whose images of tricuspid regurgitation could not be documented |
||
| Index tests |
Description of index test: The continuous wave Doppler measurement of peak tricuspid regurgitation velocity was recorded according to the guidelines. Description of method to estimate right atrial pressure: The right atrial pressure was categorised into three levels (3, 8, and 15 mmHg) on the basis of inferior vena cava diameter, together with its respiratory variation. Cut‐off value to declare PH: 41 mmHg Estimated systolic pulmonary arterial pressure: median 27 mmHg (IQR: 21‐37.5 mmHg) Sonographer qualification: not reported How to handle the uninterpretable results: not applicable |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: The systolic, diastolic, and mean pulmonary arterial pressure were measured in all participants during the end expiratory period by using a 7F Swan‐Ganz catheter inserted via the femoral or internal jugular vein in the catheter laboratory. Mean pulmonary arterial pressure: median 16 (IQR: 12‐26 mmHg) |
||
| Flow and timing | The interval between the index test and reference standard: within 24 hours Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: 0 (0%) |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | No | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the criteria of reference standard for target condition prespecified? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Schneider 2017.
| Study characteristics | |||
| Patient Sampling | Prospective | ||
| Patient characteristics and setting |
Study location: Austria Study periods: between July 2015 and July 2016 Care setting: Medical University of Vienna Participants enrolled: 65: 28 males and 37 females Participants included in analysis: 65: 28 males and 37 females Age: mean age 67.2 years (range: 19‐89 years) BMI: not reported Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): Class I: 8, Class II: 23, Class III: 10, Class IV: 13, Class V: 0 Number of patients with asymptomatic or mild symptom: not reported Number of participants with COPD: not reported Number of intubated participants: 0 Inclusion criteria: We prospectively included all adult patients with clinically indicated right‐heart catheterisation between July 2015 and July 2016. Exclusion criteria: Patients less than 18 years old were excluded. |
||
| Index tests |
Description of index test: Transthoracic echocardiograms (2D, Doppler) were performed with echocardiography systems equipped with 3.5 MHz transducers (Vivid E9, Vivid S70; General Electric Healthcare) according to the recommendations and guidelines by the American Society of Echocardiography and the European Association of Cardiovascular Imaging. In all patients, peak continuous wave Doppler velocity of the tricuspid regurgitation jet was systematically measured in the parasternal long‐axis view of the right ventricular inflow, the parasternal short axis view of the basal right ventricular, the right ventricular modified apical four chamber view, the apical long axis view of right ventricular inflow, and the subcostal four chamber view. Description of method to estimate right atrial pressure: none Cut‐off value to declare PH: 34 mmHg Estimated systolic pulmonary arterial pressure: not reported Sonographer qualification: performed by experienced physician How to handle the uninterpretable results: not applicable |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: Haemodynamic measurements were performed using a 7F Swan‐Ganz catheter (Edwards Lifesciences GmbH, Austria) via a femoral access. Pressures were documented as average of eight measurements over eight consecutive heart cycles using CathCorLX (Siemens AG, Berlin and Munich, Germany). Mean pulmonary arterial pressure: mean 37.6 ± 14.9 mmHg |
||
| Flow and timing | The interval between the index test and reference standard: within 1 day Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: 0 (0%) |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | High | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the criteria of reference standard for target condition prespecified? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Venkateshvaran 2021.
| Study characteristics | |||
| Patient Sampling | Retrospective | ||
| Patient characteristics and setting |
Study location: Sweden Study periods: between 2010 and 2018 Care setting: Karolinska University Hospital and Norrlands University Hospital Participants enrolled: 480 Participants included in analysis: 419: 199 males and 220 females Age: not reported BMI: not reported Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): not reported Number of patients with asymptomatic or mild symptom: not reported Number of participants with COPD: not reported Number of intubated participants: not reported Inclusion criteria: patients with unexplained dyspnoea referred for right‐heart catheterisation to the pulmonary hypertension referral centres at Karolinska University Hospital (2014–2018) and Norrlands University Hospital (2010–2015) Exclusion criteria: Subjects with absent or poor TR signal quality, in addition to those with a fail tricuspid valve, endocarditis or a coaptation defect resulting in massive, free‐flowing jet |
||
| Index tests |
Description of index test: TRVmax was measured with continuous wave Doppler, considering the most optimal signal obtained from multiple echocardiographic windows. RAPmean was estimated by evaluating inferior vena cava (IVC) size and collapsibility with patients in a supine position, taking care to maximise IVC diameter both during relaxed respiration and with rapid inspiration. All images were subsequently exported and analysed offline (EchoPACPC version 11.0.0.0 GE Ultrasound, Waukesha, Wisconsin). Description of method to estimate right atrial pressure: RAPmean was estimated as 3 mmHg if the IVC diameter was < 2.1 cm and collapsed > 50% during rapid inspiration and 15 mmHg if the IVC diameter was ≥ 2.1 cm and collapsed < 50%. In scenarios where IVC size and dynamics did not ft this paradigm (IVC diameter < 2.1 cm with < 50% collapse and IVC diameter ≥ 2.1 cm with > 50% collapse), RAPmean was estimated as 8 mmHg. Cut‐off value to declare PH: 2.8 m/sec Estimated systolic pulmonary arterial pressure: not reported Sonographer qualification: credentialed echocardiographers with > 15 years’ experience How to handle the uninterpretable results: excluded from analysis |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: 6F Swan Ganz catheter employing jugular or femoral vein access. After suitable calibration with the zero‐level set at the mid‐thoracic line, pressure measurements were taken from the right atrium (RA), right ventricle (RV) and PA during end‐expiration. Five to ten cardiac cycles were acquired and all pressure tracings were stored and analysed offline using a standard haemodynamic software package (WITT Series III, Witt Biomedical Corp., Melbourne, FL). Mean pulmonary arterial pressure: median 32 (IQR: 23‐41 mmHg) |
||
| Flow and timing |
The interval between the index test and reference standard: within 3 hours Number of indeterminates for whom the results of reference standard was available: 0 Number of patients who were excluded from the analysis: 61 |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | No | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | High | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Were the criteria of reference standard for target condition prespecified? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Could the patient flow have introduced bias? | High risk | ||
Wainstein 2017.
| Study characteristics | |||
| Patient Sampling | Retrospective | ||
| Patient characteristics and setting |
Study location: Argentina Study periods: between June 2010 and June 2016 Care setting: Transplant Center in Buenos Aires, Argentina Participants enrolled: 134: 63 males and 71 females Participants included in analysis: 134: 63 males and 71 females Age: mean age 47 ± 14.7 years BMI: not reported Classification of PH defined by WHO (diagnosis from right‐heart catheterisation): Class I: 0, Class II: 0, Class III: 83, Class IV: 0, Class V: 0 Number of patients with asymptomatic or mild symptom: not reported Number of participants with COPD: 65 Number of intubated participants: 0 Inclusion criteria: The population included all patients who had Doppler echocardiography and right‐heart catheterisation performed within 3 days of each other. Exclusion criteria: not reported |
||
| Index tests |
Description of index test: not reported Description of method to estimate right atrial pressure: not reported Cut‐off value to declare PH: 36 mmHg Estimated systolic pulmonary arterial pressure: not reported Sonographer qualification: not reported How to handle the uninterpretable results: not applicable |
||
| Target condition and reference standard(s) |
Target condition: pulmonary hypertension Description of reference standard: not reported Mean pulmonary arterial pressure: not reported |
||
| Flow and timing | The interval between the index test and reference standard: within 3 days Number of indeterminates for whom the results of reference standard was available: 0 (0%) Number of patients who were excluded from the analysis: 0 (0%) |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (All tests) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | Unclear | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Were the criteria of reference standard for target condition prespecified? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was the interval between the index test and reference standard less than one day? | No | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Could the patient flow have introduced bias? | High risk | ||
BMI: body mass index COPD: chronic obstructive pulmonary disease HIV: human immunodeficiency virus IQR: interquartile range IPH: idiopathic pulmonary hypertension IVC: inferior vena cava PA: pulmonary artery PCW: pulmonary capillary wedge PH: pulmonary hypertension PP: pulmonary pressure PVR: pulmonary vascular resistance RA: right atrium RAPmean: mean right atrial pressure RVSP: right ventricular systolic pressure RV: right ventricle TR: tricuspid regurgitation TRVmax: tricuspid regurgitation velocity maximum UERD: University echocardiographic regional diploma v: velocity WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aashish 2020 | Insufficient diagnostic test accuracy data |
| Abaci 1998 | Insufficient diagnostic test accuracy data |
| Abbas 2003 | Insufficient diagnostic test accuracy data |
| Abreu 1990 | Insufficient diagnostic test accuracy data |
| Adrian 2016 | Case series |
| Aduen 2009 | Insufficient diagnostic test accuracy data |
| Aduen 2011 | Insufficient diagnostic test accuracy data |
| Agrawal 2019 | Insufficient diagnostic test accuracy data |
| Ahmed 2016 | The index test and reference standard were not performed within one week. |
| Albani 2020 | Insufficient diagnostic test accuracy data |
| Ali 1987 | Not a diagnostic test accuracy study |
| Ali 1988 | Not a diagnostic test accuracy study |
| Alonso 1988 | Insufficient diagnostic test accuracy data |
| Althammer 1994 | Inappropriate target condition |
| Antoun 2009 | Insufficient diagnostic test accuracy data |
| Arcasoy 2003 | Insufficient diagnostic test accuracy data |
| Arellano 2017 | Insufficient diagnostic test accuracy data |
| Artaud‐Macari 2010 | Insufficient diagnostic test accuracy data |
| Ashrith 2015 | Case series |
| Attaran 2009 | Insufficient diagnostic test accuracy data |
| Barbier 2020 | Insufficient diagnostic test accuracy data |
| Bech‐Hanssen 2009 | Insufficient diagnostic test accuracy data |
| Bech‐Hanssen 2013 | Insufficient diagnostic test accuracy data |
| Belfort 1994 | Not a diagnostic test accuracy study |
| Bloch 1989 | Not a diagnostic test accuracy study |
| Boley 2013 | Insufficient diagnostic test accuracy data |
| Bournia 2020 | Insufficient diagnostic test accuracy data |
| Calvin 2011 | The index test and reference standard were not performed within one week. |
| Caravita 2019 | Insufficient diagnostic test accuracy data |
| Castria 2012 | Insufficient diagnostic test accuracy data |
| Cebrian 2010 | Insufficient diagnostic test accuracy data |
| Chan 1987 | Insufficient diagnostic test accuracy data |
| ChiCtr65129 | Inappropriate index test |
| Correale 2019 | Insufficient diagnostic test accuracy data |
| Cottini 2017 | Insufficient diagnostic test accuracy data |
| Cotton 2002 | Insufficient diagnostic test accuracy data |
| D'Alto 2013 | Insufficient diagnostic test accuracy data |
| D'Alto 2018 | Not a diagnostic test accuracy study |
| De Scordilli 2019 | Inappropriate reference standard |
| Denton 1997 | The index test and reference standard were not performed within one week. |
| Dina 2020 | Insufficient diagnostic test accuracy data |
| Doutreleau 2016 | Insufficient diagnostic test accuracy data |
| Etxebeste 1989 | Insufficient diagnostic test accuracy data |
| Fauvel 2020 | Inappropriate reference standard |
| Fei 2017 | Insufficient diagnostic test accuracy data |
| Finkelhor 2014 | The index test and reference standard were not performed within one week. |
| Fisher 2004 | Insufficient diagnostic test accuracy data |
| Fisher 2007 | The index test and reference standard were not performed within one week. |
| Fisher 2009 | Insufficient diagnostic test accuracy data |
| Fitzgerald 2012 | Case series |
| Fontana 2013 | Insufficient diagnostic test accuracy data |
| Gallet 1989 | Insufficient diagnostic test accuracy data |
| Ge 1993 | Inappropriate population |
| Gelape 2011 | Insufficient diagnostic test accuracy data |
| Glinel 2015 | Not a diagnostic test accuracy study |
| Gopal 2014 | Insufficient diagnostic test accuracy data |
| Granstam 2013 | Insufficient diagnostic test accuracy data |
| Guvenc 2020 | Inappropriate population |
| Habash 2017 | Case‐control study |
| Habash 2018 | The index test and reference standard were not performed within one week. |
| Hachulla 2004 | Not a diagnostic test accuracy study |
| Hachulla 2005 | Insufficient diagnostic test accuracy data |
| Held 2014 | Insufficient diagnostic test accuracy data |
| Hilde 2012 | Insufficient diagnostic test accuracy data |
| Hsu 2004 | Insufficient diagnostic test accuracy data |
| Hua 2009 | Inappropriate target condition |
| Jiang 2017 | Insufficient diagnostic test accuracy data |
| Julien 2015 | Case series |
| Junsirimongkol 2019 | Insufficient diagnostic test accuracy data |
| Khanduja 2012 | Insufficient diagnostic test accuracy data. |
| Kim 2000 | Insufficient diagnostic test accuracy data |
| Kim 2013 | Insufficient diagnostic test accuracy data |
| Kooranifar 2021 | Insufficient diagnostic test accuracy data |
| Kovacs 2014 | Inappropriate index test |
| Krowka 1999 | Insufficient diagnostic test accuracy data |
| Laaban 1989 | Inappropriate index test |
| Laaban 1989a | Insufficient diagnostic test accuracy data |
| Lamia 2014 | Insufficient diagnostic test accuracy data |
| Lange 2013 | The index test and reference standard were not performed within one week. |
| Lanzarini 2005 | Insufficient diagnostic test accuracy data |
| Li 1988 | Insufficient diagnostic test accuracy data |
| Lindgren 2009 | Insufficient diagnostic test accuracy data |
| Lindqvist 2011 | Inappropriate population |
| Lindqvist 2012 | Insufficient diagnostic test accuracy data |
| Lindqvist 2013 | Insufficient diagnostic test accuracy data |
| Maeder 2010 | Insufficient diagnostic test accuracy data |
| Maeder 2011 | Insufficient diagnostic test accuracy data |
| Marangoni 1988 | Insufficient diagnostic test accuracy data |
| Matos 1988 | Insufficient diagnostic test accuracy data |
| McClanahan 2011 | Insufficient diagnostic test accuracy data |
| Mercado 2019 | Insufficient diagnostic test accuracy data |
| Metz 1987 | Insufficient diagnostic test accuracy data |
| Metz 1991 | Insufficient diagnostic test accuracy data |
| Minai 2010 | Insufficient diagnostic test accuracy data |
| Miyamoto 1993 | Not a diagnostic test accuracy study |
| Mo 2015b | Inappropriate target condition |
| Modrykamien 2010 | The index test and reference standard were not performed within one week. |
| Mogollon 2008 | Inappropriate reference standard |
| Mukerjee 2004 | The index test and reference standard were not performed within one week. |
| Naeije 1995 | Not a diagnostic test accuracy study |
| Nathan 2008 | The index test and reference standard were not performed within one week. |
| Niederle 1988 | Insufficient diagnostic test accuracy data |
| Niederle 1990 | Insufficient diagnostic test accuracy data |
| Nishimaki 1991 | Insufficient diagnostic test accuracy data |
| Nogami 2009 | Insufficient diagnostic test accuracy data |
| O'Leary 2018 | Insufficient diagnostic test accuracy data |
| Okubo 1988 | Insufficient diagnostic test accuracy data |
| Okubo 1989 | Insufficient diagnostic test accuracy data |
| Oudiz 2003 | Not a diagnostic test accuracy study |
| Pande 2014 | Inappropriate population |
| Parsaee 2016 | Insufficient diagnostic test accuracy data |
| Pasierski 1993 | Not a diagnostic test accuracy study |
| Penning 2001 | Inappropriate reference standard |
| Phetcharat 2019 | Index test and reference standard were not performed within one week |
| Philip 2013 | The index test and reference standard were not performed within one week. |
| Polak‐Slaboszewska 1989 | Insufficient diagnostic test accuracy data |
| Prasanna 2009 | Insufficient diagnostic test accuracy data |
| Raevens 2013 | Insufficient diagnostic test accuracy data |
| Raevens 2013a | Insufficient diagnostic test accuracy data |
| Rajagopalan 2009 | Inappropriate target condition |
| Rallidis 2020 | Inappropriate reference standard |
| Rallidis 2021 | Inappropriate reference standard |
| Refini 2021 | Insufficient diagnostic test accuracy data |
| Rich 2010 | Insufficient diagnostic test accuracy data |
| Rich 2011 | Insufficient diagnostic test accuracy data |
| Roodpeyma 2015 | Insufficient diagnostic test accuracy data |
| Saner 2006 | Insufficient diagnostic test accuracy data |
| Schewel 2020 | Insufficient diagnostic test accuracy data |
| Schiopu 2010 | The index test and reference standard were not performed within one week. |
| Seidova 2020 | Insufficient diagnostic test accuracy data |
| Selby 2012 | Insufficient diagnostic test accuracy data |
| Shen 1989 | Insufficient diagnostic test accuracy data |
| Shim 2018 | Not a diagnostic test accuracy study |
| Skjaerpe 1986 | Insufficient diagnostic test accuracy data |
| Slegg 2021 | Insufficient diagnostic test accuracy data |
| Sohrabi 2016 | Insufficient diagnostic test accuracy data |
| Solik 2013 | Insufficient diagnostic test accuracy data |
| Sonaglioni 2021 | Inappropriate population |
| Torbicki 1987 | Insufficient diagnostic test accuracy data |
| Torbicki 1989 | Insufficient diagnostic test accuracy data |
| Torregrosa 2001 | The index test and reference standard were not performed within one week. |
| Tramarin 1991 | Inappropriate reference standard |
| Wahi 2015 | Insufficient diagnostic test accuracy data |
| Wang 2016 | Inappropriate population |
| Wilansky 1998 | Not a diagnostic test accuracy study |
| Wurtemberger 1992 | Insufficient diagnostic test accuracy data |
| Wylie 2007 | Insufficient diagnostic test accuracy data |
| Yagi 1988 | Insufficient diagnostic test accuracy data. |
| Yamamoto 2013 | Insufficient diagnostic test accuracy data |
| Yamamoto 2013a | Insufficient diagnostic test accuracy data |
| Yock 1984 | Insufficient diagnostic test accuracy data |
| Zenker 1987 | Insufficient diagnostic test accuracy data |
| Zhuravlev 2004 | Not a diagnostic test accuracy study |
| Zompatori 1993 | Insufficient diagnostic test accuracy data |
Differences between protocol and review
We planned to use the HSROC model to perform the prespecified subgroup analyses. However, due to the limited data, we only presented the descriptive statistics as shown in Table 3.
We planned subgroup analysis of the WHO classification to compare group 3 with other group classifications. However, most studies did not report the classification of PH, and we changed the subgroup analysis into: group 3, not group 3, or classification not reported.
We performed the post hoc subgroup analysis using the bivariate model stratified by the threshold of index test (< 36 mmHg, ≥ 36 and < 40 mmHg, and ≥ 40 mmHg).We planned the sensitivity analysis using median‐splitting of the prevalence of PH in each study. However, as the prevalence varied greatly, we split the prevalence into quartiles.
We planned a sensitivity analysis on uninterpretable results, however, we could not perform it because the data on whether the patients with uninterpretable data had PH or not were not available.
For the Summary of Findings table and additional Table 4, we presented the pooled sensitivity under the fixed specificity of 86% (median of the included studies) using the estimated parameters from the HSROC model.
Contributions of authors
JK drafted the protocol and review with contributions from SS, YN, YK, HT, YT, MK, SO, HI and TM. JK and YT devised the study selection criteria. JK, SS, YN, YK, HT, YT, and Elizabeth Stovold undertook the search strategy. JK, SS, YN, and HT developed the study design and research question. JK, HT, YK, and YT developed the statistical analysis/synthesis of the data plan. JK, YN, YK, YT, MK, SO, HI and TM screened search results. JK, YN, YK, YT, MK, SO, HI and TM extracted the data and assessed the methodological quality. All authors contributed to revising the manuscript, reviewed all drafts, and agreed on the final version.
Contributions of editorial team
Chris Cates (Coordinating Editor): checked the data entry prior to the full write‐up of the review, edited the review, advised on methodology, interpretation and content; approved the final review prior to publication.
Mia Schmidt‐Hansen (Contact Editor, Diagnostic Test Accuracy Reviews Group): commented on the review and arranged peer review from DTA specialists; approved the peer reviewed draft prior to publication.
Emma Dennett (Deputy Coordinating Editor): coordinated the editorial process; advised on interpretation and content; edited the review; co‐ordinated sign‐off of the review and completed final checks.
Emma Jackson (Assistant Managing Editor): conducted peer review; obtained translations; edited the plain language summary and reference sections of the protocol and the review.
Elizabeth Stovold (Information Specialist): designed the search strategy; ran the searches; edited the search methods section.
Sources of support
Internal sources
Sakai City Medical Center, Japan
Kyoto University, Japan
Hyogo Prefectural Amagasaki General Medical Center, Japan
External sources
The authors declare that no such funding was received for this systematic review., Japan
Declarations of interest
JK: none known.
SS: none known.
YN: none known.
YK: employed by Kyoto Min‐Iren Asukai Hospital
HT: none known.
YT: employed by Kyoritsu Hospital
MK: none known.
SO: none known.
HI: none known.
TM: none known.
Edited (no change to conclusions)
References
References to studies included in this review
Amsallem 2016 {published and unpublished data}
- Amsallem M, Sternbach JM, Adigopula S, Kobayashi Y, Vu TA, Zamanian R, et al.Addressing the controversy of estimating pulmonary arterial pressure by echocardiography. Journal of the American Society of Echocardiography 2016;29(2):93-102. [DOI] [PubMed] [Google Scholar]
Balci 2016 {published data only}
- Balci MK, Ari E, Vayvada M, Salturk C, Asicioglu E, Kahveci G, et al.Assessment of pulmonary hypertension in lung transplantation candidates: correlation of Doppler echocardiography with right heart catheterization. Transplantation Proceedings 2016;48(8):2797-802. [DOI] [PubMed] [Google Scholar]
Colle 2003 {published data only}
- Colle IO, Moreau R, Godinho E, Belghiti J, Ettori F, Cohen-Solal A, et al.Diagnosis of portopulmonary hypertension in candidates for liver transplantation: a prospective study. Hepatology 2003;37(2):401-9. [DOI] [PubMed] [Google Scholar]
Er 2010 {published data only}
- Er F, Ederer S, Nia AM, Caglayan E, Dahlem KM, Semmo N, et al.Accuracy of doppler-echocardiographic mean pulmonary artery pressure for diagnosis of pulmonary hypertension. PLOS One 2010;5(12):e15670. [DOI] [PMC free article] [PubMed] [Google Scholar]
Greiner 2014 {published data only}
- Greiner S, Jud A, Aurich M, Hess A, Hilbel T, Hardt S, et al.Reliability of noninvasive assessment of systolic pulmonary artery pressure by doppler echocardiography compared to right heart catheterization: analysis in a large patient population. Journal of the American Heart Association 2014;3(4):pii: e001103. [DOI: 10.1161/JAHA.114.001103] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hellenkamp 2018 {published data only}
- Hellenkamp K, Unsold B, Mushemi-Blake S, Shah AM, Friede T, Hasenfuss G, et al.Echocardiographic estimation of mean pulmonary artery pressure: a comparison of different approaches to assign the likelihood of pulmonary hypertension. Journal of the American Society of Echocardiography 2018;31(1):89-98. [DOI] [PubMed] [Google Scholar]
Hsu 2008 {published data only}
- Hsu VM, Moreyra AE, Wilson AC, Shinnar M, Shindler DM, Wilson JE, et al.Assessment of pulmonary arterial hypertension in patients with systemic sclerosis: comparison of noninvasive tests with results of right-heart catheterization. Journal of Rheumatology 2008;35(3):458-65. [PubMed] [Google Scholar]
Kyranis 2018 {published data only}
- Kyranis SJ, Latona J, Platts D, Kelly N, Savage M, Brown M, et al.Improving the echocardiographic assessment of pulmonary pressure using the tricuspid regurgitant signal -The "chin" vs the "beard". Echocardiography 2018;35(8):1085-96. [DOI] [PubMed] [Google Scholar]
Lafitte 2013 {published data only}
- Lafitte S, Pillois X, Reant P, Picard F, Arsac F, Dijos M, et al.Estimation of pulmonary pressures and diagnosis of pulmonary hypertension by Doppler echocardiography: a retrospective comparison of routine echocardiography and invasive hemodynamics. Journal of the American Society of Echocardiography 2013;26(5):457-63. [DOI] [PubMed] [Google Scholar]
Mazhar 2011 {published data only}
- Mazhar J, Pera V, Liang M, Lee E, Tamuno P, Jayabal J, et al.How good is tricuspid regurgitation velocity in excluding pulmonary hypertension in patients with left heart disease. Heart Lung and Circulation 2011;20:S176. [Google Scholar]
Mo 2015 {published data only}
- Mo V, Bellucci B, Fisher J, Balekian A.PAAT and RVET versus RVSP to predict pulmonary hypertension. European Respiratory Journal 2015;46:PA3784. [DOI: 10.1183/13993003.congress-2015.PA3784] [DOI] [Google Scholar]
Mo 2015a {published data only}
- Mo VY, Bellucci BM, Fisher JM, Balekian AA.PAAT, RVET, and Vmax versus RVSP to predict pulmonary hypertension. European Heart Journal Cardiovascular Imaging 2015;16:ii154. [Google Scholar]
Nowak 2018 {published data only}
- Nowak J, Hudzik B, Jastrzebski D, Niedziela JT, Rozentryt P, Wojarski J, et al.Pulmonary hypertension in advanced lung diseases: echocardiography as an important part of patient evaluation for lung transplantation. Clinical Respiratory Journal 2018;12(3):930-8. [DOI] [PubMed] [Google Scholar]
Sawada 2019 {published data only}
- Sawada N, Kawata T, Daimon M, Nakao T, Hatano M, Maki H, et al.Detection of pulmonary hypertension with systolic pressure estimated by doppler echocardiography. International Heart Journal 2019;60(4):836-44. [DOI: doi: 10.1536/ihj.18-453] [DOI] [PubMed] [Google Scholar]
Schneider 2017 {published data only}
- Schneider M, Pistritto AM, Gerges C, Gerges M, Binder C, Lang I, et al.Multi-view approach for the diagnosis of pulmonary hypertension using transthoracic echocardiography. In: Annual Meeting of the OKG-Austrian Cardiology Society; 2017 Jun 7-10; Salzburg. 2017:S73-4.
Venkateshvaran 2021 {published data only}
- Venkateshvaran A, Seidova N, Tureli HO, Kjellstrom B, Lund LH, Tossavainen E, et al.Accuracy of echocardiographic estimates of pulmonary artery pressures in pulmonary hypertension: insights from the KARUM hemodynamic database. International Journal of Cardiovascular Imaging 2021;37(9):2637-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wainstein 2017 {published data only}
- Wainstein EJ, Castro HM, Orazi ML, Svetliza GN, Maritano Furcada J, Precerutti JA, et al.Accuracy of ecocardiographic assessment of pulmonary pressure in lung transplant candidates. Journal of Heart and Lung Transplantation 2017;36(4 Suppl 1):S406. [Google Scholar]
References to studies excluded from this review
Aashish 2020 {published data only}
- Aashish A, Giridharan S, Karthikeyan S, Ganesh BA, Prasath PA.Assessment of pulmonary artery pressures by various doppler echocardiographic parameters and its correlation with cardiac catheterization in patients with pulmonary hypertension. Heart Views 2020;21(4):263-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Abaci 1998 {published data only}
- Abaci A, Kabukcu M, Ovünç K, Tokgözoğlu L, Tarrach M, Batur MK, et al.Comparison of the three different formulas for Doppler estimation of pulmonary artery systolic pressure. Angiology 1998;49:463e70. [DOI] [PubMed] [Google Scholar]
Abbas 2003 {published data only}
- Abbas AE, Fortuin FD, Schiller NB, Appleton CP, Moreno CA, Lester SJ.Echocardiographic determination of mean pulmonary artery pressure. American Journal of Cardiology 2003;92(11):1373-6. [DOI] [PubMed] [Google Scholar]
Abreu 1990 {published data only}
- Abreu J, Bernardes L, Soares R, Ramos JM, Quininha J, Salomao S.Non-invasive evaluation of systolic pressure of the pulmonary artery in patients with tricuspid regurgitation, using Doppler echocardiography. Revista Portuguesa de Cardiologia 1990;9(3):199-203. [PubMed] [Google Scholar]
Adrian 2016 {published data only}
- Adrian Lescano A, Lavalle Cobo A, Santa Maria H, Damianich G, Ferro A, Gonzalez N, et al.Accuracy and precision of systolic pulmonary pressure assessed by echocardiography among patients with pulmonary hypertension. European Journal of Heart Failure 2016;18:416. [Google Scholar]
Aduen 2009 {published data only}
- Aduen JF, Castello R, Lozano MM, Hepler GN, Keller CA, Alvarez F, et al.An alternative echocardiographic method to estimate mean pulmonary artery pressure: diagnostic and clinical Implications. Journal of the American Society of Echocardiography 2009;7:814-9. [DOI] [PubMed] [Google Scholar]
Aduen 2011 {published data only}
- Aduen JE, Castello R, Daniels JT, Diaz JA, Safford RE, Heckman MG, et al.Accuracy and precision of three echocardiographic methods for estimating mean pulmonary artery pressure. Chest 2011;2:347-52. [DOI] [PubMed] [Google Scholar]
Agrawal 2019 {published data only}
- Agrawal V, D'Alto M, Naeije R, Romeo E, Xu M, Assad TR, et al.Echocardiographic detection of occult diastolic dysfunction in pulmonary hypertension after fluid challenge. Journal of the American Heart Association 2019;8(17):e012504. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ahmed 2016 {published data only}
- Ahmed I, Hassan Nuri MM, Zakariyya AN, Ahmad SM, Ahmed M.Correlation between doppler echocardiography and right heart catheterization derived pulmonary artery pressures: impact of right atrial pressures. Journal of the College of Physicians and Surgeons 2016;26(4):255-9. [PubMed] [Google Scholar]
Albani 2020 {published data only}
- Albani S, Pinamonti B, Giovinazzo T, De Scordilli M, Fabris E, Stolfo D, et al.Accuracy of right atrial pressure estimation using a multi-parameter approach derived from inferior vena cava semi-automated edge-tracking echocardiography: a pilot study in patients with cardiovascular disorders. International Journal of Cardiovascular Imaging 2020;36(7):1213-25. [DOI] [PubMed] [Google Scholar]
Ali 1987 {published data only}
- Ali AS, Sergakova LM, At'kov OLU.Diagnosis of pulmonary hypertension using Doppler-echocardiography. Terapevticheskii Arkhiv 1987;59(3):138-41. [PubMed] [Google Scholar]
Ali 1988 {published data only}
- Ali SA, Sergakova LM.Quantitative assessment of pulmonary hypertension by doppler echocardiography. Kardiologiya 1988;7:112-5. [PubMed] [Google Scholar]
Alonso 1988 {published data only}
- Alonso F, Garcia Fernandez MA, Moreno M, Martinez Romero P, Rabgo R.Doppler ultrasound imaging of the heart in the assessment of pulmonary hypertension. Ultrasonidos 1988;7(4):149-59. [Google Scholar]
Althammer 1994 {published data only}
- Althammer G, Barnickel H, Siemon G.Doppler echocardiography in pulmonary hypertension. Atemwegs - Und Lungenkrankheiten 1994;20(9):520-4. [Google Scholar]
Antoun 2009 {published data only}
- Antoun P, Breall J, Kwo P, Sadanandan S, Shoemaker T, Singh I, et al.Pre-operative pulmonary hypertension and mortality in patients undergoing liver transplantation. Catheterization and Cardiovascular Interventions 2009;73:S68. [Google Scholar]
Arcasoy 2003 {published data only}
- Arcasoy SM, Christie JD, Ferrari VA, Sutton MS, Zisman DA, Blumenthal NP, et al.Echocardiographic assessment of pulmonary hypertension in patients with advanced lung disease. American Journal of Respiratory and Critical Care Medicine 2003;167(5):735-40. [DOI: 10.1164/rccm.200210-1130OC] [DOI] [PubMed] [Google Scholar]
Arellano 2017 {published data only}
- Arellano Serrano C, Garcia-Izquierdo Jaen E, Monivas Palomero V, Vilches Soria S, Oteo Dominguez JF, Segovia Cubero J, et al.Is the assessment of pulmonary arterial hypertension by echocardiography reliable in patients with severe tricuspid regurgitation? In: 21st Annual Meeting of the European Association of Echocardiography, EUROECHO; 2017 Dec 6-9; Lisbon. 2017:iii272.
Artaud‐Macari 2010 {published data only}
- Artaud-Macari E, Muir JF, Cuvelier A, Molano LC, Viacroze C, Mouton-Schleiffer D, et al.How accurate is trans-thoracic Doppler echocardiography for the hemodynamic assessment of pulmonary hypertension? In: American Thoracic Society International Conference; 2010 May 14-19; New Orleans. 2010.
Ashrith 2015 {published data only}
- Ashrith G, Fida N, Cordero-Reyes A, Amione-Guerra J, Khan Z, Bhimaraj A, et al.Echocardiographic predictors of combined pre and post capillary pulmonary hypertension (PH) in a population of systolic heart failure with who group II. Journal of the American College of Cardiology 2015;65(10 Suppl 1):A1564. [Google Scholar]
Attaran 2009 {published data only}
- Attaran RR, Ramaraj R, Sorrell VL, Movahed MR.Poor correlation of estimated pulmonary artery systolic pressure between echocardiography and right heart catheterization inpatients awaiting cardiac transplantation: results from the clinical arena. Transplantation Proceedings 2009;41:3827e30. [DOI] [PubMed] [Google Scholar]
Barbier 2020 {published data only}
- Barbier P, Cucco C, Guglielmo M, Simioniuc A, Fabiani I, Pugliese NR, et al.Estimation of increased pulmonary wedge pressure by an algorithm based on noninvasively measured pulmonary diastolic pressure in cardiac patients independent of left ventricular ejection fraction. Echocardiography (Mount Kisco, NY) 2020;37(2):215-22. [DOI] [PubMed] [Google Scholar]
Bech‐Hanssen 2009 {published data only}
- Bech-Hanssen O, Selimovic N, Rundqvist B, Wallentin J.Doppler echocardiography can provide a comprehensive assessment of right ventricular afterload. Journal of the American Society of Echocardiography 2009;22(12):1360-7. [DOI] [PubMed] [Google Scholar]
Bech‐Hanssen 2013 {published data only}
- Bech-Hanssen O, Karason K, Rundqvist B, Bollano E, Lindgren F, Selimovic N.Can pulmonary hypertension and increased pulmonary vascular resistance be ruled in and ruled out by echocardiography? Journal of the American Society of Echocardiography 2013;26(5):469-78. [DOI] [PubMed] [Google Scholar]
Belfort 1994 {published data only}
- Belfort MA, Rokey R, Saade GR, Moise KJ.Rapid echocardiographic assessment of left and right heart hemodynamics in critically ill obstetric patients. American Journal of Obstetrics and Gynecology 1994;4:884-92. [DOI] [PubMed] [Google Scholar]
Bloch 1989 {published data only}
- Bloch A, Mayor C, Guillaume-Gentil M, Vuille C, Suard J.Doppler ultrasound diagnosis of pulmonary hypertension. Revue Medicale de la Suisse Romande 1989;109(11):907-10. [PubMed] [Google Scholar]
Boley 2013 {published data only}
- Boley T, Manning B, Nallamothu N, Markwell S, Henkle J, Vassileva C, et al.Utility of echocardiography and right heart catheterization in pulmonary artery pressure evaluation for lung volume reduction surgery. American Journal of Respiratory and Critical Care Medicine 2013;187:A4328. [Google Scholar]
Bournia 2020 {published data only}
- Bournia VK, Tsangaris I, Rallidis L, Konstantonis D, Frantzeskaki F, Anthi A, et al.Cardiac catheterization versus echocardiography for monitoring pulmonary pressure: a prospective study in patients with connective tissue disease-associated pulmonary arterial hypertension. Diagnostics 2020;10(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Calvin 2011 {published data only}
- Calvin JE, Holoshitz N, Liebson P.Echo estimates of pulmonary artery pressure correlates poorly with right heart catheterization. Journal of the American College of Cardiology 2011;57(14 Suppl 1):E1572. [Google Scholar]
Caravita 2019 {published data only}
- Caravita S, Yerly P, Baratto C, Dewachter C, Rimouche A, Faini A, et al.Validation of noninvasive pulmonary artery pressure/flow relationship: echocardiography vs right heart catheterization. European Heart Journal 2019;40(Suppl 1):ehz745.1066. [Google Scholar]
Castria 2012 {published data only}
- Castria D, Refini RM, Mezzasalma F, Di Sipio P, Bargagli E, Filippi R, et al.Precocious detection of pulmonary hypertension in idiopathic pulmonary fibrosis. European Respiratory Journal 2012;40:P3636. [DOI] [PubMed] [Google Scholar]
Cebrian 2010 {published data only}
- Cebrian J, Balerdi B, Bonastre J, Lopez C.Correlation between systolic pulmonary artery values estimated with Doppler echocardiography and measured with pulmonary artery catheter in patients with suspected pulmonary artery hypertension. Intensive Care Medicine 2010;36:S333. [Google Scholar]
Chan 1987 {published data only}
- Chan KL, Currie PJ, Seward JB, Hagler DJ, Mair DD, Tajik AJ.Comparison of three Doppler ultrasound methods in the prediction of pulmonary artery pressure. Journal of the American College of Cardiology 1987;9:549-54. [DOI] [PubMed] [Google Scholar]
ChiCtr65129 {published data only}
- ChiCtr65129.Analysis of reliability of noninvasive assessment of pulmonary artery pressure by Doppler echocardiography compared to right heart catheterization: a prospective clinical study. www.chictr.org.cn/showproj.aspx?proj=65129 (first received 26 Jan 2021).
Correale 2019 {published data only}
- Correale M, Tricarico L, Padovano G, Ferraretti A, Monaco I, Musci RL, et al.Echocardiographic score for prediction of pulmonary hypertension at catheterization: the Daunia Heart Failure Registry. Journal of Cardiovascular Medicine 2019;20(12):809-15. [DOI] [PubMed] [Google Scholar]
Cottini 2017 {published data only}
- Cottini S, Benden C, Huber LC, Arrigo M.Echocardiography accurately predicts pulmonary hypertension in patients with advanced lung disease. Critical Care 2017;21:115. [DOI: 10.1186/s13054-017-1697-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cotton 2002 {published data only}
- Cotton CL, Ghandi S, Vaitkus PT, Massad VG, Benedetto E, Mrtek RG, et al.Role of echocardiography in detecting portopulmonary hypertension in liver transplant candidates. Liver Transplantation 2002;8(11):1051-4. [DOI] [PubMed] [Google Scholar]
D'Alto 2013 {published data only}
- D'Alto M, Romeo E, Argiento P, D'Andrea A, Vanderpool R, Correra A, et al.Accuracy and precision of echocardiography versus right heart catheterization for the assessment of pulmonary hypertension. International Journal of Cardiology 2013;168(4):4058-62. [DOI] [PubMed] [Google Scholar]
D'Alto 2018 {published data only}
- D'Alto M, Di Marco GM, D'Andrea A, Argiento P, Romeo E, Ferrara F, et al.Invasive and noninvasive evaluation for the diagnosis of pulmonary hypertension how to use and how to combine them. Heart Failure Clinics 2018;14(3):353-60. [DOI] [PubMed] [Google Scholar]
Denton 1997 {published data only}
- Denton CP, Cailes JB, Phillips GD, Wells AU, Black CM, Bois RM.Comparison of Doppler echocardiography and right heart catheterization to assess pulmonary hypertension in systemic sclerosis. British Journal of Rheumatology 1997;36(2):239-43. [DOI] [PubMed] [Google Scholar]
De Scordilli 2019 {published data only}
- De Scordilli M, Pinamonti B, Albani S, Gregorio C, Barbati G, Daneluzzi C, et al.Reliability and challenges in non-invasive hemodynamic assessment with Doppler echocardiography: comparison with the invasive evaluation. European Heart Journal Cardiovascular Imaging 2019;20(Suppl 1):i167. [DOI] [PubMed] [Google Scholar]
Dina 2020 {published data only}
- Dina A, Kennington A, Garrahy P, Chong A, Wahi S.311 Contrast enhancement of the Tricuspid Regurgitant (TR) spectral Doppler signal in pulmonary hypertension (PHTN) - waste of bubbles or truth be told? Heart Lung and Circulation 2020;29:S173. [Google Scholar]
Doutreleau 2016 {published data only}
- Doutreleau S, Canuet M, Enache I, Di Marco P, Lonsdorfer E, Oswald-Mammoser M, et al.Right heart hemodynamics in pulmonary hypertension - an echocardiography and catheterization study. Circulation Journal 2016;80(9):2019-25. [DOI] [PubMed] [Google Scholar]
Etxebeste 1989 {published data only}
- Etxebeste J, Martinez J, Ruiz de Azua E, Urrengoetxea J, Arrillaga M, Ormaetxe J, et al.Diagnosis of pulmonary hypertension by means of continuous, pulsed and color Doppler, and its correlation with hemodynamics. Revista Espanola de Cardiologia 1989;42(2):90-7. [PubMed] [Google Scholar]
Fauvel 2020 {published data only}
- Fauvel C, Raitiere O, Burdeau J, Si Belkacem N, Bauer F.Impact of the new PH guidelines on echocardiographic definition leading to double demand of right heart catheterization. European Heart Journal Cardiovascular Imaging 2020;21(Suppl 1):jez319.951. [Google Scholar]
Fei 2017 {published data only}
- Fei BN, Fan T, Zhao L, Pei XL, Shu XH, Fang XY, et al.Impact of severe tricuspid regurgitation on accuracy of systolic pulmonary arterial pressure measured by Doppler echocardiography: analysis in an unselected patient population. Echocardiography 2017;34(7):1082-8. [DOI] [PubMed] [Google Scholar]
Finkelhor 2014 {published data only}
- Finkelhor RS, Scrocco JD, Madmani M, Rovner A, Pillai D.Discordant doppler right heart catheterization pulmonary artery systolic pressures: importance of pulmonary capillary wedge pressure. Echocardiography 2014;31(3):279-84. [DOI] [PubMed] [Google Scholar]
Fisher 2004 {published data only}
- Fisher MR, Forfia PR, Chamera E, Housten T, Champion HC, Resar J, et al.Accuracy of Doppler echocardiography in the hemodynamic evaluation of pulmonary hypertension. Chest 2004;126(4):883S. [Google Scholar]
Fisher 2007 {published data only}
- Fisher MR, Criner GJ, Fishman AP, Hassoun PM, Minai OA, Scharf SM, et al.Estimating pulmonary artery pressures by echocardiography in patients with emphysema. European Respiratory Journal 2007;30(5):914-21. [DOI: 10.1183/09031936.00033007] [DOI] [PubMed] [Google Scholar]
Fisher 2009 {published data only}
- Fisher MR, Forfia PR, Chamera E, Housten-Harris T, Champion HC, Girgis RE, et al.Accuracy of Doppler echocardiography in the hemodynamic assessment of pulmonary hypertension. American Journal of Respiratory and Critical Care Medicine 2009;179(7):615-21. [DOI: 10.1164/rccm.200811-1691OC] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fitzgerald 2012 {published data only}
- Fitzgerald M, Fagan K, Herbert DE, Al-Ali M, Mugal M, Haynes J Jr.Misclassification of pulmonary hypertension in adults with sickle hemoglobinopathies using Doppler echocardiography. Southern Medical Journal 2012;105(6):300-5. [DOI] [PubMed] [Google Scholar]
Fontana 2013 {published data only}
- Fontana A, Vincenzi A, Paciocco G, De Vito G, Marinari A, Trocino G, et al.Doppler echocardiography pulmonary artery flow acceleration time: an adjunctive parameter to select candidates with suspected pulmonary hypertension to proceed to right heart catheterization. European Heart Journal 2013;34:48. [Google Scholar]
Gallet 1989 {published data only}
- Gallet B, Saudemont JP, Bourdon D, Bayet G, Babo P, Thenault D, et al.Evaluation of pulmonary arterial hypertension by Doppler echocardiography in chronic respiratory insufficiency. Archives des Maladies du Coeur et des Vaisseaux 1989;82(9):1575-83. [PubMed] [Google Scholar]
Ge 1993 {published data only}
- Ge Z, Zhang Y, Fan D, Kang W, Hatle L, Duran C.Simultaneous measurement of pulmonary artery diastolic pressure by Doppler echocardiography and catheterization in patients with patent ductus arteriosus. American Heart Journal 1993;125(1):263-6. [DOI] [PubMed] [Google Scholar]
Gelape 2011 {published data only}
- Gelape CL, Nunes Mdo C, Braulio R, Nogueira PH, Andrade SA, Machado PA, et al.Pulmonary pressure checked by echocardiography in chagasic patients on the heart transplant waiting list. Revista Brasileira de Cirurgia Cardiovascular 2011;26(1):54-60. [DOI] [PubMed] [Google Scholar]
Glinel 2015 {published data only}
- Glinel B, Bauer F.Pulmonary hypertension and transcatheter aortic valve implantation: prevalence, prognosis impact and evolution. Archives of Cardiovascular Diseases Supplements 2015;7(2):201. [Google Scholar]
Gopal 2014 {published data only}
- Gopal DM, Doldt B, Finch K, Simms RW, Farber HW, Gokce N.Relation of novel echocardiographic measures to invasive hemodynamic assessment in scleroderma-associated pulmonary arterial hypertension. Arthritis Care and Research 2014;66(9):1386-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Granstam 2013 {published data only}
- Granstam SO, Bjorklund E, Wikstrom G, Roos MW.Use of echocardiographic pulmonary acceleration time and estimated vascular resistance for the evaluation of possible pulmonary hypertension. Cardiovascular Ultrasound 2013;11:7. [DOI: 10.1186/1476-7120-11-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guvenc 2020 {published data only}
- Guvenc TS, Poyraz E, Cetin Guvenc R, Can F.Contemporary usefulness of pulmonary venous flow parameters to estimate left ventricular end-diastolic pressure on transthoracic echocardiography. International Journal of Cardiovascular Imaging 2020;36(9):1699-709. [DOI] [PubMed] [Google Scholar]
Habash 2017 {published data only}
- Habash F, Gurram P, Almomani A, Duarte-Rojo A, Hakeem A, Vallurupalli S, et al.Correlation between echocardiographic pulmonary artery pressure estimates and right heart catheterization measurements in patients undergoing liver transplant evaluation: a single center study. Journal of the American College of Cardiology 2017;11(Suppl 1):1888. [Google Scholar]
Habash 2018 {published data only}
- Habash F, Gurram P, Almomani A, Duarte A, Hakeem A, Vallurupalli S, et al.Correlation between echocardiographic pulmonary artery pressure estimates and right heart catheterization measurement in liver transplant candidates. Journal of Cardiovascular Imaging 2018;26(2):75-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hachulla 2004 {published data only}
- Hachulla E, Gressin V, Guillevin L, De Groote P, Cabane J, Carpentier P, et al.Pulmonary arterial hypertension in systemic sclerosis: definition of a screening algorithm for early detection (the ItinerAIR-Sclerodermie Study). Revue de Medecine Interne 2004;25(5):340-7. [DOI] [PubMed] [Google Scholar]
Hachulla 2005 {published data only}
- Hachulla E, Gressin V, Guillevin L, Carpentier P, Diot E, Sibilia J, et al.Early detection of pulmonary arterial hypertension in systemic sclerosis: a French nationwide prospective multicenter study. Arthritis and Rheumatism 2005;52(12):3792-800. [DOI] [PubMed] [Google Scholar]
Held 2014 {published data only}
- Held M, Linke M, Jany B.Echocardiography and right heart catheterization in pulmonal hypertension. Deutsche Medizinische Wochenschrift (1946) 2014;139(30):1511-7. [DOI] [PubMed] [Google Scholar]
Hilde 2012 {published data only}
- Hilde JM, Skjoerten IS, Melsom MNM, Humerfelt SH, Hansteen VH, Hisdal JH, et al.Noninvasive assessment of pulmonary arterial compliance and its impact on right ventricular function in COPD patients. European Heart Journal. Cardiovascular Imaging 2012;13:i118. [Google Scholar]
Hsu 2004 {published data only}
- Hsu VM, Shinnar M, Moreyra A, Shindler D, Wilson A, Wilson JE, et al.Assessment of pulmonary hypertension (PH) in systemic sclerosis (SSc): a comparison of Doppler echocardiography, cardiac MRI and right heart catheterization. Arthritis and Rheumatism 2004;(9):S424. [Google Scholar]
Hua 2009 {published data only}
- Hua R, Sun YW, Wu ZY, Cheng W, Xu Q, Cao H, et al.Role of 2-dimensional Doppler echo-cardiography in screening portopulmonary hypertension in portal hypertension patients. Hepatobiliary & Pancreatic Diseases International 2009;8(2):157-61. [PubMed] [Google Scholar]
Jiang 2017 {published data only}
- Jiang R, Wu C, Pudasaini B, Wang L, Zhao QH, Zhang R, et al.A novel scoring index by Doppler echocardiography for predicting severe pulmonary hypertension due to chronic lung diseases: a cross-sectional diagnostic accuracy study. International Journal of Chronic Obstructive Pulmonary Disease 2017;12:1741-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Julien 2015 {published data only}
- Julien HM, Fields A, Siu H, Scharf M, Mehrotra P.Right ventricular fractional area change predicts invasively-determined hemodynamics in patients with pulmonary arterial hypertension. Journal of the American College of Cardiology 2015;65(10 Suppl 1):A1566. [Google Scholar]
Junsirimongkol 2019 {published data only}
- Junsirimongkol B, Cheewatanakornkul S, Jamulitrat S.Comparison of performances among five prediction formulae using echocardiography in estimation of mean pulmonary arterial pressure. European Heart Journal Cardiovascular Imaging 2019;20(Suppl 1):i363. [Google Scholar]
Khanduja 2012 {published data only}
- Khanduja K, Lakshmanan RV, Roscoe A, Srinivas C, Therapondos G, McCluskey SA.Does the severity of tricuspid regurgitation affect the correlation and agreement between pulmonary systolic artery pressures estimated transthoracic echocardiography and intra-operative right heart catherization? Canadian Journal of Anesthesia 2012;59(Suppl 1):188. [Google Scholar]
Kim 2000 {published data only}
- Kim WR, Krowka MJ, Plevak DJ, Lee J, Rettke SR, Frantz RP, et al.Accuracy of Doppler echocardiography in the assessment of pulmonary hypertension in liver transplant candidates. Liver Transplantation 2000;6(4):453-8. [DOI] [PubMed] [Google Scholar]
Kim 2013 {published data only}
- Kim SM, Faulkner M, Booth D, Campbell C, Hundley J, Charnigo R, et al.Can we rule out significant pulmonary hypertension in liver transplant candidates noninvasively? Journal of the American College of Cardiology 2013;61(10):E1289. [Google Scholar]
Kooranifar 2021 {published data only}
- Kooranifar S, Naghshin R, Sezavar SH, Hajsadeghi S, Talebzadeh SM.Diagnostic value of chest spiral CT scan and Doppler echocardiography compared to right heart catheterization to predict pulmonary arterial hypertension in patients with scleroderma. Acta Bio-Medica 2021;92(1):e2021074. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kovacs 2014 {published data only}
- Kovacs G, Avian A, Foris V, Tscherner M, Kqiku X, Douschan P, et al.Role of simple non-invasive tools to assess pulmonary hypertension. American Journal of Respiratory and Critical Care Medicine 2014;189::A4750. [Google Scholar]
Krowka 1999 {published data only}
- Krowka MJ, Kim WR, Wiesner RH, McGoon MD, Frantz RP.Screening Doppler echocardiography to detect pulmonary hypertension in liver transplant candidates. American Journal of Respiratory and Critical Care Medicine 1999;3:A155. [Google Scholar]
Laaban 1989 {published data only}
- Laaban JP, Diebold B, Lafay M, Rochemaure J, Peronneau P.Detection of pulmonary hypertension by Doppler echocardiography of the inferior vena cava in chronic airflow obstruction. Thorax 1989;44(5):396-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
Laaban 1989a {published data only}
- Laaban JP, Diebold B, Zelinski R, Lafay M, Raffoul H, Rochemaure J.Noninvasive estimation of systolic pulmonary artery pressure using Doppler echocardiography in patients with chronic obstructive pulmonary disease. Chest 1989;96(6):1258-62. [DOI] [PubMed] [Google Scholar]
Lamia 2014 {published data only}
- Lamia B, Molano LC, Viacroze C, Gounane C, Cuvelier A, Muir JF.Relevance of echocardiographic composite index to improve the detection of pulmonary hypertension. In: European Respiratory Society 24th Annual Congress; 2014 Sep 6-10; Munich. 2014.
Lange 2013 {published data only}
- Lange TJ, Baumgartner S, Arzt M, Pfeifer M.Qualitative echocardiography parameters for prediction of pulmonary hypertension. International Journal of Clinical Practice 2013;67(Suppl 179):5-12. [DOI] [PubMed] [Google Scholar]
Lanzarini 2005 {published data only}
- Lanzarini L, Fontana A, Campana C, Klersy C.Two simple echo-Doppler measurements can accurately identify pulmonary hypertension in the large majority of patients with chronic heart failure. Journal of Heart and Lung Transplantation 2005;24(6):745-54. [DOI] [PubMed] [Google Scholar]
Li 1988 {published data only}
- Li LG.Pulmonary hypertension measured by Doppler echocardiography. Chung-hua Hsin Hsueh Kuan Ping Tsa Chih [Chinese Journal of Cardiology] 1988;16(1):39-40. [PubMed] [Google Scholar]
Lindgren 2009 {published data only}
- Lindgren F, Rundqvist B, Petersson S, Selimovic N, Bech-Hanssen O.Pressure increase after peak velocity in the pulmonary artery: a novel echocardiography method to identify patients with increased pulmonary vascular resistance. European Heart Journal 2009;30:897. [Google Scholar]
Lindqvist 2011 {published data only}
- Lindqvist P, Soderberg S, Gonzalez M, Tossavainen E, Henein MY.Doppler echocardiography based estimation of pulmonary vascular resistance in patients with pulmonary hypertension: a simultaneous echocardiographic and cardiac catheterization study. European Heart Journal. Cardiovascular Imaging 2011;12:ii51. [DOI] [PubMed] [Google Scholar]
Lindqvist 2012 {published data only}
- Lindqvist P, Henein M, Soderberg S, Tossavainen E, Gonzalez M, Henein MY.Echo-based estimation of pulmonary vascular resistance and pulmonary capillary wedge pressure correlate closely with catheter-based measurements. European Heart Journal. Cardiovascular Imaging 2012;13:i167-8. [Google Scholar]
Lindqvist 2013 {published data only}
- Lindqvist P, Tossavainen E, Gonzalez M, Henein M, Soderberg S.Echo-based estimation of pulmonary vascular resistance and pulmonary capillary wedge pressure correlate closely with catheter-based measurements. Scandinavian Cardiovascular Journal 2013;47:1-2. [Google Scholar]
Maeder 2010 {published data only}
- Maeder MT, Htun NM, Karapanagiotidis S, Dewar L, Kaye DM.Accuracy of non-invasive right heart catheterisation to predict haemodynamics in subjects with normal left ventricular ejection fraction. European Heart Journal 2010;31:725. [Google Scholar]
Maeder 2011 {published data only}
- Maeder MT, Karapanagiotidis S, Dewar EM, Gamboni SE, Htun N, Kaye DM.Accuracy of Doppler echocardiography to estimate key hemodynamic variables in subjects with normal left ventricular ejection fraction. Journal of Cardiac Failure 2011;17(5):405-12. [DOI] [PubMed] [Google Scholar]
Marangoni 1988 {published data only}
- Marangoni S, Quadri A, Dotti A, Scalvini S, Volterrani M, Schena M, et al.Noninvasive assessment of pulmonary hypertension: a simultaneous echo-Doppler hemodynamic study. Cardiology 1988;75(6):401-8. [DOI] [PubMed] [Google Scholar]
Matos 1988 {published data only}
- Matos P, Pereira A, De Oliveira LM, Ramos JS, Quininha J, Ferreira T, et al.Pulsed 2D Doppler echocardiography in pulmonary arterial hypertension. Revista Portuguesa de Cardiologia 1988;7(5):479-84. [PubMed] [Google Scholar]
McClanahan 2011 {published data only}
- McClanahan A, Guglin M.Right ventricular dysfunction compromises accuracy of echocardiographic diagnosis of pulmonary hypertension in heart failure. Journal of Cardiac Failure 2011;17(12):1023-7. [DOI] [PubMed] [Google Scholar]
Mercado 2019 {published data only}
- Mercado P, Maizel J, Beyls C, Kontar L, Orde S, Huang S, et al.Reassessment of the accuracy of cardiac Doppler pulmonary artery pressure measurements in ventilated ICU patients: a simultaneous doppler-catheterization study. Critical Care Medicine 2019;47(1):41-8. [DOI] [PubMed] [Google Scholar]
Metz 1987 {published data only}
- Metz D, Laudinat JM, Beruben E, Marchal E, Blaise C, Deschildre A, et al.Evaluation of pulmonary systolic arterial pressures by continuous Doppler in tricuspid regurgitation in adults. Apropos of 43 cases. Archives des Maladies du Coeur et des Vaisseaux 1987;80(11):1605-9. [PubMed] [Google Scholar]
Metz 1991 {published data only}
- Metz D, Chapoutot L, Ouzan J, Chabert JP, Pollet E, Elaerts J, et al.Doppler echocardiographic assessment of the severity of acute pulmonary embolism. A correlative angiographic study in forty-eight adult patients. American Journal of Noninvasive Cardiology 1991;5(4):223-8. [Google Scholar]
Minai 2010 {published data only}
- Minai OA, Criner GJ, Scharf SM, Fessler H, Meli Y, Nutter B, et al.Pulmonary hemodynamics in moderate to severe emphysema: characteristics and predictors. In: American Thoracic Society International Conference; 2010 May 14-19; New Orleans. 2010:181.
Miyamoto 1993 {published data only}
- Miyamoto K, Aida A, Kawakami Y.Diagnosis of cor pulmonale by echocardiography. Nippon Naika Gakkai Zasshi (Journal of Japanese Society of Internal Medicine) 1993;82(6):818-23. [PubMed] [Google Scholar]
Mo 2015b {published data only}
- Mo VY, Fisher JM, Balekian AA.Pulmonary artery acceleration time and right ventricular ejection time for the echocardiographic screening of elevated pulmonary vascular resistance in patients with right ventricular systolic failure. American Journal of Respiratory and Critical Care Medicine 2015;191:A4856. [Google Scholar]
Modrykamien 2010 {published data only}
- Modrykamien AM, Gudavalli R, McCarthy K, Parambil J.Echocardiography, 6-minute walk distance, and distance-saturation product as predictors of pulmonary arterial hypertension in idiopathic pulmonary fibrosis. Respiratory Care 2010;55(5):584-8. [PubMed] [Google Scholar]
Mogollon 2008 {published data only}
- Mogollón Jiménez MV, Escoresca Ortega AM, Cabeza Letrán ML, Hinojosa Pérez R, Lage Gallé E, Sobrino Márquez JM.Correlation of echocardiographic and haemodynamic parameters in pulmonary hypertension assessment prior to heart transplantation. Transplant Proceedings 2008;40:3023e4. [DOI] [PubMed] [Google Scholar]
Mukerjee 2004 {published data only}
- Mukerjee D, St George D, Knight C, Davar J, Wells AU, Du Bois RM.Echocardiography and pulmonary function as screening tests for pulmonary arterial hypertension in systemic sclerosis. Rheumatology 2004;43:461e6. [DOI] [PubMed] [Google Scholar]
Naeije 1995 {published data only}
- Naeije R, Torbicki A.More on the noninvasive diagnosis of pulmonary hypertension: Doppler echocardiography revisited. European Respiratory Journal 1995;8(9):1445-9. [PubMed] [Google Scholar]
Nathan 2008 {published data only}
- Nathan SD, Shlobin OA, Barnett SD, Saggar R, Belperio JA, Ross DJ, et al.Right ventricular systolic pressure by echocardiography as a predictor of pulmonary hypertension in idiopathic pulmonary fibrosis. Respiratory Medicine 2008;102:1305–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Niederle 1988 {published data only}
- Niederle P, Starek A, Jezek V, Hes I.Doppler echocardiography in the diagnosis of pulmonary hypertension. Vnitrni Lekarstvi 1988;34(10):950-6. [PubMed] [Google Scholar]
Niederle 1990 {published data only}
- Niederle P, Jezek V, Jezkova J.Estimation of systolic pressure in the right ventricle (pulmonary artery) using Doppler and its importance in the detection of pulmonary hypertension. Casopis Lekaru Ceskych 1990;129(49):1553-6. [PubMed] [Google Scholar]
Nishimaki 1991 {published data only}
- Nishimaki T, Aotsuka S, Kunieda T, Yokohari R.Preliminary criteria for the diagnosis of pulmonary hypertension in mixed connective tissue disease. Ryumachi [Rheumatism] 1991;31(2):159-66. [PubMed] [Google Scholar]
Nogami 2009 {published data only}
- Nogami M, Ohno Y, Koyama H, Kono A, Takenaka D, Kataoka T, et al.Utility of phase contrast MR imaging for assessment of pulmonary flow and pressure estimation in patients with pulmonary hypertension: comparison with right heart catheterization and echocardiography. Journal of Magnetic Resonance Imaging 2009;30(5):973e80. [DOI] [PubMed] [Google Scholar]
O'Leary 2018 {published data only}
- O'Leary JM, Assad TR, Xu M, Farber-Eger E, Wells QS, Hemnes AR, et al.Lack of a tricuspid regurgitation doppler signal and pulmonary hypertension by invasive measurement. Journal of the American Heart Association 2018;7(13):e009362. [DOI: 10.1161/JAHA.118.009362] [DOI] [PMC free article] [PubMed] [Google Scholar]
Okubo 1988 {published data only}
- Okubo S, Nakayama R.Modern Doppler echocardiography as a diagnostic aid for cor pulmonale. Rinsho Byori (Japanese Journal of Clinical Pathology) 1988;36(5):573-7. [PubMed] [Google Scholar]
Okubo 1989 {published data only}
- Okubo S, Miyatake K, Nagata S, Nakanishi N, Yoshioka T, Kunieda T.Role of echocardiography in acute pulmonary embolism. Japanese Heart Journal 1989;30(5):655-64. [DOI] [PubMed] [Google Scholar]
Oudiz 2003 {published data only}
- Oudiz RJ, Ginzton L.Pulmonary artery systolic pressure estimated by echocardiogram vs catheterization in patients awaiting lung transplantation. Journal of Heart and Lung Transplantation 2003;22(7):832-3; author reply 833. [DOI] [PubMed] [Google Scholar]
Pande 2014 {published data only}
- Pande A, Sarkar A, Ahmed I, Naveen Chandra G, Patil SK, Kundu CK, et al.Non-invasive estimation of pulmonary vascular resistance in patients of pulmonary hypertension in congenital heart disease with unobstructed pulmonary flow. Annals of Pediatric Cardiology 2014;7(2):92-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Parsaee 2016 {published data only}
- Parsaee M, Ghaderi F, Alizadehasl A, Bakhshandeh H.Time from the beginning of the right ventricle isovolumetric contraction to the peak of the S wave: a new TDI indicator for the non-invasive estimation of pulmonary hypertension. Research in Cardiovascular Medicine 2016;5(3):e26494. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pasierski 1993 {published data only}
- Pasierski TJ, Starling RC, Binkley PF, Pearson AC.Echocardiographic evaluation of pulmonary artery distensibility. Chest 1993;103(4):1080-3. [DOI] [PubMed] [Google Scholar]
Penning 2001 {published data only}
- Penning S, Robinson KD, Major CA, Garite TJ.A comparison of echocardiography and pulmonary artery catheterization for evaluation of pulmonary artery pressures in pregnant patients with suspected pulmonary hypertension. American Journal of Obstetrics and Gynecology 2001;184:1568e70. [DOI] [PubMed] [Google Scholar]
Phetcharat 2019 {published data only}
- Phetcharat S, Kavouras C, Ilagan L, Roxy S, Wort J, Gatzoulis M, et al.Echocardiographic assessment of pulmonary pressures: the value of pulmonary regurgitation and pulmonary acceleration time. European Heart Journal Cardiovascular Imaging 2019;20(Suppl 1):i35. [Google Scholar]
Philip 2013 {published data only}
- Philip RT, Balekian A.Utility of trans-thoracic Doppler echocardiography in avoiding invasive right heart catheterization in end-stage liver disease patients undergoing evaluation for liver transplantation. American Journal of Respiratory and Critical Care Medicine 2013;187:A2542. [Google Scholar]
Polak‐Slaboszewska 1989 {published data only}
- Polak-Slaboszewska D, Bolinska H, Moczak R, Kowalewski J, Radominski S, Kaczmarek A.Usefulness of Doppler echocardiography for evaluation of pulmonary hypertension based on the analysis of blood flow through the pulmonary artery. Kardiologia Polska 1989;32(5):248-54. [PubMed] [Google Scholar]
Prasanna 2009 {published data only}
- Prasanna V, Opotowsky A, Ojeda J, Arkles J, Palevsky H, Taichman D, et al.Echo-Doppler scoring system provides simple noninvasive assessment of the pathophysiology of pulmonary hypertension in a mixed pulmonary hypertension cohort. Chest 2009;136(4):32S. [Google Scholar]
Raevens 2013 {published data only}
- Raevens S, Colle I, Geerts A, Reyntjens K, Troisi R, Berrevoet F, et al.Detection of portopulmonary hypertension in liver transplant candidates with echocardiography. In: 32nd Annual Scientific Meeting of the Belgian Society of Cardiology; 2013 Jan 31-1 Feb; Brussels. 2013:118.
Raevens 2013a {published data only}
- Raevens S, Colle I, Reyntjens K, Geerts A, Berrevoet F, Rogiers X, et al.Echocardiography for the detection of portopulmonary hypertension in liver transplant candidates: an analysis of cutoff values. Liver Transplantation 2013;19(6):602-10. [DOI] [PubMed] [Google Scholar]
Rajagopalan 2009 {published data only}
- Rajagopalan N, Simon MA, Suffoletto MS, Shah H, Edelman K, Mathier MA, et al.Noninvasive estimation of pulmonary vascular resistance in pulmonary hypertension. Echocardiography 2009;26(5):489-94. [DOI] [PubMed] [Google Scholar]
Rallidis 2020 {published data only}
- Rallidis L, Papangelopoulou K, Anthi A, Makavos G, Konstantonis D, Tsangaris I, et al.Is there any role of exercise Doppler echocardiography to unmask pulmonary hypertension (PH) in patients with systemic sclerosis and baseline echocardiographic measurements for PH in the gray zone? European Heart Journal Cardiovascular Imaging 2020;21(Suppl 1):jez319.1146. [Google Scholar]
Rallidis 2021 {published data only}
- Rallidis LS, Papangelopoulou K, Anthi A, Tsangaris I, Varounis C, Makavos G, et al.The role of exercise Doppler echocardiography to unmask pulmonary arterial hypertension in selected patients with systemic sclerosis and equivocal baseline echocardiographic values for pulmonary hypertension. Diagnostics 2021;11(7):1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Refini 2021 {published data only}
- Refini RM, Bettini G, Kacerja E, Cameli P, D'Alessandro M, Bergantini L, et al.The role of the combination of echo-HRCT score as a tool to evaluate the presence of pulmonary hypertension in idiopathic pulmonary fibrosis. Internal and Emergency Medicine 2021;16(4):941-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rich 2010 {published data only}
- Rich J, Shah S, Swamy R, Kamp A, Rich S.Doppler echocardiographic estimates of pulmonary artery systolic pressure in patients with pulmonary hypertension are inaccurate. In: American Thoracic Society International Conference; 2010 May 14-19; New Orleans. 2010:181.
Rich 2011 {published data only}
- Rich JD, Shah SJ, Swamy RS, Kamp A, Rich S.Inaccuracy of Doppler echocardiographic estimates of pulmonary artery pressures in patients with pulmonary hypertension: implications for clinical practice. CHEST 2011;139(5):988-93. [DOI: 10.1378/chest.10-1269] [DOI] [PubMed] [Google Scholar]
Roodpeyma 2015 {published data only}
- Roodpeyma S, Mojtahedzadeh S, Rafieyian S, Behbahani SR.Accuracy of electrocardiography and echocardiography in the assessment of pulmonary arterial hypertension in patients with congenital heart disease. Iranian Heart Journal 2015;15(4):20-5. [Google Scholar]
Saner 2006 {published data only}
- Saner FH, Nadalin S, Pavlakovic G, Gu Y, Olde Damink SW, Gensicke J, et al.Portopulmonary hypertension in the early phase following liver transplantation. Transplantation 2006;82(7):887-91. [DOI] [PubMed] [Google Scholar]
Schewel 2020 {published data only}
- Schewel J, Schluter M, Schmidt T, Kuck KH, Frerker C, Schewel D.Correlation between Doppler echocardiography and right heart catheterization assessment of systolic pulmonary artery pressure in patients with severe aortic stenosis. Echocardiography 2020;37(3):380-7. [DOI] [PubMed] [Google Scholar]
Schiopu 2010 {published data only}
- Schiopu E, Impens AJ, Rubenfire M, Mahmood F, Phillips K.Comparison of estimated pulmonary artery systolic pressure by echocardiography (PASPECHO) and right heart catheterization (PASPRHC) in patients with systemic sclerosis (scleroderma, SSc). Arthritis and Rheumatism 2010;62:567. [Google Scholar]
Seidova 2020 {published data only}
- Seidova N, Manouras A, Lund LH, Venkateshvaran A.Comparison between echocardiographic right ventricular-pulmonary arterial coupling and right ventricular longitudinal strain to identify pulmonary hypertension in heart failure. European Heart Journal Cardiovascular Imaging 2020;21(Suppl 1):i988. [Google Scholar]
Selby 2012 {published data only}
- Selby VN, Scherzer R, Barnett CF, MacGregor JS, Morelli J, Donovan C, et al.Doppler echocardiography does not accurately estimate pulmonary artery systolic pressure in HIV-infected patients. AIDS 2012;26(15):1967-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shen 1989 {published data only}
- Shen XD, Jiang L, He J.A quantitative study of pulmonary artery systolic pressure in patients with tricuspid regurgitation using continuous wave Doppler. Chung-hua Hsin Hsueh Kuan Ping Tsa Chih [Chinese Journal of Cardiology] 1989;17(6):347-9, 382. [PubMed] [Google Scholar]
Shim 2018 {published data only}
- Shim CY.Issues on estimated pulmonary artery pressure in liver transplant candidates. Journal of Cardiovascular Imaging 2018;26(2):61-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Skjaerpe 1986 {published data only}
- Skjaerpe T, Hatle L.Noninvasive estimation of systolic pressure in the right ventricle in patients with tricuspid regurgitation. European Heart Journal 1986;7:704-10. [DOI] [PubMed] [Google Scholar]
Slegg 2021 {published data only}
- Slegg O, Willis J, Gibson C, Kendler-Rhodes A, Wilkinson F, Rossdale J, et al.Audit of echocardiographic probability of pulmonary hypertension in a real world population referred to a specialist centre. Heart (British Cardiac Society) 2021;107:A62-4. [Google Scholar]
Sohrabi 2016 {published data only}
- Sohrabi B, Kazemi B, Mehryar A, Teimouri-Dereshki A, Toufan M, Aslanabadi N.Correlation between pulmonary artery pressure measured by echocardiography and right heart catheterization in patients with rheumatic mitral valve stenosis (a prospective study). Echocardiography 2016;33(1):7-13. [DOI] [PubMed] [Google Scholar]
Solik 2013 {published data only}
- Solik P, Lesny P, Luknar M, Varga I, Wimmerova S, Goncalvesova E.Pulmonary artery systolic pressure - direct measurement versus echocardiographic estimation in patients with pulmonary arterial hypertension and pulmonary venous hypertension. Cardiology Letters 2013;22(6):459-65. [Google Scholar]
Sonaglioni 2021 {published data only}
- Sonaglioni A, Cassandro R, Luisi F, Ferrante D, Nicolosi GL, Lombardo M, et al.Correlation between Doppler echocardiography and right heart catheterisation-derived systolic and mean pulmonary artery pressures: determinants of discrepancies between the two methods. Heart, Lung & Circulation 2021;30(5):656-64. [DOI] [PubMed] [Google Scholar]
Torbicki 1987 {published data only}
- Torbicki A, Pasierski T, Miskiewicz Z.Noninvasive evaluation of blood pressure in the pulmonary artery using a Doppler method. Kardiologia Polska 1987;30(12):783-90. [PubMed] [Google Scholar]
Torbicki 1989 {published data only}
- Torbicki A, Skwarski K, Hawrylkiewicz I, Pasierski T, Miskiewicz Z, Zielinski J.Attempts at measuring pulmonary arterial pressure by means of Doppler echocardiography in patients with chronic lung disease. European Respiratory Journal 1989;2(9):856-60. [PubMed] [Google Scholar]
Torregrosa 2001 {published data only}
- Torregrosa M, Genesca J, Gonzalez A, Evangelista A, Mora A, Margarit C, et al.Role of Doppler echocardiography in the assessment of portopulmonary hypertension in liver transplantation candidates. Transplantation 2001;71(4):572-4. [DOI] [PubMed] [Google Scholar]
Tramarin 1991 {published data only}
- Tramarin R, Torbicki A, Marchandise B, Laaban JP, Morpurgo M.Doppler echocardiographic evaluation of pulmonary artery pressure in chronic obstructive pulmonary disease. A European multicentre study. European Heart Journal 1991;12:103–11. [DOI] [PubMed] [Google Scholar]
Wahi 2015 {published data only}
- Wahi S, Chong A.Direct comparison of non-invasive estimation of mean pulmonary artery pressure with right heart catheter measurements - which echocardiographic technique is best? European Heart Journal Cardiovascular Imaging 2015;16:ii154. [Google Scholar]
Wang 2016 {published data only}
- Wang B, Zhou HX, Yang J, Liang BM, Feng YL.Accuracy of doppler echocardiography in the assessment of pulmonary arterial hypertension in patients with congenital heart disease. Chest 2016;149(4 Suppl 1):509A. [PubMed] [Google Scholar]
Wilansky 1998 {published data only}
- Wilansky S.Two-dimensional and Doppler echocardiography for the assessment of congestive heart failure. Texas Heart Institute Journal 1998;25(4):260-4. [PMC free article] [PubMed] [Google Scholar]
Wurtemberger 1992 {published data only}
- Wurtemberger G, Tiede N, Wencker M, Mathys H.Pulmonary hypertension in patients with chronic lung disease. Validity of Doppler echocardiography. Atemwegs - und Lungenkrankheiten 1992;18(11):489-95. [Google Scholar]
Wylie 2007 {published data only}
- Wylie BJ, Epps KC, Gaddipati S, Waksmonski CA.Correlation of transthoracic echocardiography and right heart catheterization in pregnancy. Journal of Perinatal Medicine 2007;35(6):497-502. [DOI] [PubMed] [Google Scholar]
Yagi 1988 {published data only}
- Yagi H, Yamada H, Ookubo S, Koyama S, Kawashima A, Fukushima M, et al.Noninvasive prediction of pulmonary-hypertension induced by hypoxic breathing in subjects susceptible to high-altitude pulmonary-edema by Doppler echocardiography and the role of prostanoids. Japanese Circulation Journal 1988;9:1023. [Google Scholar]
Yamamoto 2013 {published data only}
- Yamamoto S, Matsumoto Y, Nochioka K, Miura M, Tatebe S, Sugimura K, et al.Potential involvement of functional tricuspid regurgitation in the diagnostic error to assess pulmonary arterial pressure by Doppler echocardiography. Life Sciences 2013;93(25-6):e44. [Google Scholar]
Yamamoto 2013a {published data only}
- Yamamoto S, Matsumoto Y, Nochioka K, Miura M, Tatebe S, Sugimura K, et al.Potential involvement of functional tricuspid regurgitation in the diagnostic error to assess pulmonary arterial pressure by Doppler echocardiography. European Heart Journal 2013;34:37. [Google Scholar]
Yock 1984 {published data only}
- Yock P, Popp R.Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation 1984;70:657–62. [DOI] [PubMed] [Google Scholar]
Zenker 1987 {published data only}
- Zenker G, Metzler H, Stenzl W, Rehak F, Gombotz H, Forche G, et al.Quantifying pulmonary artery hypertension by Doppler echocardiography measurement of tricuspid valve insufficiency. Wiener Medizinische Wochenschrift 1987;103:42-3. [PubMed] [Google Scholar]
Zhuravlev 2004 {published data only}
- Zhuravlev VF, Zhuravleva NV.A new technique for evaluation of the functional state of the cardiovascular system. Biomedical Engineering 2004;38(4):187-92. [Google Scholar]
Zompatori 1993 {published data only}
- Zompatori M, Rimondi MR, Canini R, Battaglia M.Chronic cor pulmonale in obstructive lung disease. Diagnostic evaluation with Doppler echography and other non-invasive imaging techniques. Radiologia Medica 1993;85(3):247-53. [PubMed] [Google Scholar]
Additional references
Andersen 2012
- Andersen KH, Iversen M, Kjaergaard J, Mortensen J, Nielsen-Kudsk JE, Bendstrup E, et al.Prevalence, predictors, and survival in pulmonary hypertension related to end-stage chronic obstructive pulmonary disease. Journal of Heart Lung Transplantation 2012;31(4):373-80. [DOI] [PubMed] [Google Scholar]
Avouac 2010
- Avouac J, Airo P, Meune C, Beretta L, Dieude P, Caramaschi P, et al.Prevalence of pulmonary hypertension in systemic sclerosis in European Caucasians and meta-analysis of 5 studies. Journal of Rheumatology 2010;37(11):2290-8. [DOI] [PubMed] [Google Scholar]
Benza 2010
- Benza RL, Miller DP, Gomberg-Maitland M, Frantz RP, Foreman AJ, Coffey CS, et al.Predicting survival in pulmonary arterial hypertension: insights from the registry to evaluate early and long-term pulmonary arterial hypertension disease management (REVEAL). Circulation 2010;122(2):164-72. [DOI] [PubMed] [Google Scholar]
Berger 1985
- Berger M, Haimowitz A, Van A, Berdoff RL, Goldberg E.Quantitative assessment of pulmonary hypertension in patients with tricuspid regurgitation using continuous wave Doppler ultrasound. Journal of the American College of Cardiology 1985;6(2):359-65. [DOI: 10.1016/S0735-1097(85)80172-8] [DOI] [PubMed] [Google Scholar]
Best 2018
- Best LM, Takwoingi Y, Siddique S, Selladurai A, Gandhi A, Low B, et al.Non-invasive diagnostic tests for Helicobacter pylori infection. Cochrane Database of Systematic Reviews 2018, Issue 3. Art. No: CD012080. [DOI: 10.1002/14651858.CD012080.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beynon 2013
- Beynon R, Leeflang MM, McDonald S, Eisinga A, Mitchell RL, Whiting P, et al.Search strategies to identify diagnostic accuracy studies in MEDLINE and EMBASE. Cochrane Database of Systematic Reviews 2013, Issue 9. Art. No: MR000022. [DOI: 10.1002/14651858.MR000022.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 2011
- Brown LM, Chen H, Halpern S, Taichman D, McGoon MD, Farber HW, et al.Delay in recognition of pulmonary arterial hypertension: factors identified from the REVEAL Registry. Chest 2011;140(1):19-26. [DOI: 10.1378/chest.10-1166] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bursi 2012
- Bursi F, McNallan SM, Redfield MM, Nkomo VT, Lam CS, Weston SA, et al.Pulmonary pressures and death in heart failure: a community study. Journal of the American College of Cardiology 2012;59(3):222-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Connors 1996
- Connors AF, Speroff T, Dawson NV, Thomas C, Harrell FE, Wagner D, et al, SUPPORT Investigators.The effectiveness of right heart catheterization in the initial care of critically ill patients. JAMA 1996;276(11):889-97. [DOI: 10.1001/jama.1996.03540110043030] [DOI] [PubMed] [Google Scholar]
De Vet 2008
- De Vet HCW, Eisinga A, Riphagen II, Aertgeerts B, Pewsner D, editor(s).Chapter 7: Searching for studies. In: Deeks JJ, Bossuyt PM, Gatsonis C, editor(s). Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 1.0.0. The Cochrane Collaboration, 2013. Available from methods.cochrane.org/sdt/handbook-dta-reviews.
Deeks 2013
- Deeks JJ, Bossuyt PM, Gatsonis C (editors).Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 1.0.0. The Cochrane Collaboration, 2013. Available from srdta.cochrane.org.
Delcroix 2010
- Delcroix M, Naeije R.Optimising the management of pulmonary arterial hypertension patients: emergency treatments. European Respiratory Review 2010;19(117):204-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dzudie 2014
- Dzudie A, Kengne AP, Thienemann F, Sliwa K.Predictors of hospitalisations for heart failure and mortality in patients with pulmonary hypertension associated with left heart disease: a systematic review. BMJ Open 2014;4(7):e004843. [DOI] [PMC free article] [PubMed] [Google Scholar]
Freed 2016
- Freed BH, Collins JD, Francois CJ, Barker AJ, Cuttica MJ, Chesler NC, et al.MR and CT imaging for the evaluation of pulmonary hypertension. Journal of the American College of Cardiology: Cardiovascular Imaging 2016;9(6):715-32. [DOI: 10.1016/j.jcmg.2015.12.015] [DOI] [PMC free article] [PubMed] [Google Scholar]
Galie 2013
- Galiè N, Corris PA, Frost A, Girgis RE, Granton J, Jing ZC, et al.Updated treatment algorithm of pulmonary arterial hypertension. Journal of the American College of Cardiology 2013;62(25 Suppl):D60-72. [DOI: 10.1016/j.jacc.2013.10.031] [DOI] [PubMed] [Google Scholar]
Galie 2016
- Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, et al.2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS). European Heart Journal 2016;37(1):67-119. [DOI: 10.1093/eurheartj/ehv317] [DOI] [PubMed] [Google Scholar]
Heazell 2019
- Heazell AEP, Hayes DJL, Whitworth M, Takwoingi Y, Bayliss SE, Davenport C.Biochemical tests of placental function versus ultrasound assessment of fetal size for stillbirth and small-for-gestational-age infants. Cochrane Database of Systematic Reviews 2019, Issue 5. Art. No: CD012245. [DOI: 10.1002/14651858.CD012245.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoeper 2013
- Hoeper MM, Bogaard HJ, Condliffe R, Frantz R, Khanna D, Kurzyna M, et al.Definitions and diagnosis of pulmonary hypertension. Journal of the American College of Cardiology 2013;62(25 Suppl):D42-50. [DOI: 10.1016/j.jacc.2013.10.032] [DOI] [PubMed] [Google Scholar]
Humbert 2006
- Humbert M, Sitbon O, Chaouat A, Bertocchi M, Habib G, Gressin V, et al.Pulmonary arterial hypertension in France: results from a national registry. American Journal of Respiratory Care Medicine 2006;173(9):1023. [DOI] [PubMed] [Google Scholar]
Janda 2011
- Janda S, Shahidi N, Gin K, Swiston J.Diagnostic accuracy of echocardiography for pulmonary hypertension: a systematic review and meta-analysis. Heart 2011;97:612-22. [DOI] [PubMed] [Google Scholar]
Kaplan 2010
- Kaplan A, Mc Lean A, Vieillard-Baron A.Hemodynamic Monitoring Using Echocardiography in the Critically Ill. Berlin, Heidelberg: Springer, 2010. [DOI: 10.1007/978-3-540-87956-5_13] [DOI] [Google Scholar]
Lang 2015
- Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al.Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Journal of the American Society of Echocardiography 2015;28(1):1-39.e14. [DOI] [PubMed] [Google Scholar]
Lewis 2016
- Lewis R, William H.Clinical features and diagnosis of pulmonary hypertension in adults. www.uptodate.com/contents/clinical-features-and-diagnosis-of-pulmonary-hypertension-in-adults (accessed 6 December 2016).
Ling 2012
- Ling Y, Johnson MK, Kiely DG, Condliffe R, Elliot CA, Gibbs JS.Changing demographics, epidemiology, and survival of incident pulmonary arterial hypertension. American Journal of Respiratory and Critical Care Medicine 2012;186(8):790-6. [DOI] [PubMed] [Google Scholar]
Macaskill 2021
- Macaskill P, Takwoingi Y, Deeks JJ, Gatsonis C.Chapter 10: Understanding meta-analysis draft version (17 June 2021). In: Deeks JJ, Bossuyt PM, Leeflang MM, Takwoingi Y, editor(s). Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 2. Cochrane, 2021. Available from srdta.cochrane.org.
Marcus 2008
- Marcus JT, Gan CT, Zwanenburg JJ, Boonstra A, Allaart CP, Gotte MJW.Interventricular mechanical asynchrony in pulmonary arterial hypertension: left-to-right delay in peak shortening is related to right ventricular overload and left ventricular underfilling. Journal of the American College of Cardiology 2008;51:750-7. [DOI] [PubMed] [Google Scholar]
McLaughlin 2009
- McLaughlin VV, Archer SL, Badesch DB, Barst RJ, Farber HW, Lindner JR, Mathier MA, McGoon MD, Park MH, Rosenson RS, Rubin LJ, Tapson VF, Varga J.ACCF/AHA 2009 expert consensus document on pulmonary hypertension: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association. Journal of the American College of Cardiology 2009;53(17):1573-619. [DOI] [PubMed] [Google Scholar]
Meredith 2014
- Meredith EP, Lakshmi S, Li W, Ivan MR, John HN, Anna RH.Causes of pulmonary hypertension in the elderly. CHEST 2014;146(1):159-66. [DOI: 10.1378/chest.13-1900] [DOI] [PMC free article] [PubMed] [Google Scholar]
Molano 2019
- Molano Franco D, Arevalo-Rodriguez I, Roque I Figuls M, Montero Oleas NG, Nuvials X, Zamora J.Plasma interleukin-6 concentration for the diagnosis of sepsis in critically ill adults. Cochrane Database of Systematic Reviews 2019, Issue 4. Art. No: CD011811. [DOI: 10.1002/14651858.CD011811.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moreira 2015
- Moreira EM, Gall H, Leening MJ, Lahousse L, Loth DW, Krijthe BP, et al.Prevalence of pulmonary hypertension in the general population: the Rotterdam study. PLOS One 2015;10(6):e0130072. [DOI] [PMC free article] [PubMed] [Google Scholar]
Paulus 2007
- Paulus WJ, Tschope C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE, et al.How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the heart failure and echocardiography. European Heart Journal 2007;28:2539-50. [DOI] [PubMed] [Google Scholar]
Peacock 2007
- Peacock AJ, Murphy NF, McMurray JJV, Caballero L, Stewart S.An epidemiological study of pulmonary arterial hypertension. European Respiratory Journal 2007;30:104-9. [DOI] [PubMed] [Google Scholar]
Reitsma 2005
- Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH.Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. Journal of Clinical Epidemiology 2005;58(10):982-90. [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Review Manager.Version 5.3. Copenhagen: Nordic Cochrane Center, The Cochrane Collaboration, 2014.
Rubin 2016
- Rubin LJ, Hopkins W.Clinical features and diagnosis of pulmonary hypertension in adults. www.uptodate.com/contents/clinical-features-and-diagnosis-of-pulmonary-hypertension-in-adults (accessed 24 Jan 2017).
Rudski 2010
- Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al.Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. Journal of the American Society of Echocardiography 2010;23(7):685-713. [DOI: 10.1016/j.echo.2010.05.010] [DOI] [PubMed] [Google Scholar]
Rutjes 2005
- Rutjes AWS, Reitsma JB, Vandenbrouke JP, Glas AS, Bossuyt PMM.Case-control and two-gate designs in diagnostic accuracy studies. Clinical Chemistry 2005;51(8):1335-41. [DOI: 10.1373/clinchem.2005.048595] [DOI] [PubMed] [Google Scholar]
Rutter 2001
- Rutter CM, Gatsonis CA.A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Statistics in Medicine 2001;20(19):2865-84. [DOI] [PubMed] [Google Scholar]
Schermuly 2011
- Schermuly RT, Janssen W, Weissmann N, Stasch JP, Grimminger F, Ghofrani HA.Riociguat for the treatment of pulmonary hypertension. Expert Opinion on Investigational Drugs 2011;20(4):567-76. [DOI] [PubMed] [Google Scholar]
Simonneau 2013
- Simonneau G, Gatzoulis MA, Adatia I, Celermajer D, Denton C, Ghofrani A, et al.Updated clinical classification of pulmonary hypertension. Journal of the American College of Cardiology 2013;62(25 Suppl):D34-41. [DOI: 10.1016/j.jacc.2013.10.029] [DOI] [PubMed] [Google Scholar]
Stata 2013 [Computer program]
- Stata.Version 13.0. College Station (TX): Stata Corporation, 2013.
Taleb 2013
- Taleb M, Khuder S, Tinkel J, Khouri SJ.The diagnostic accuracy of Doppler echocardiography in assessment of pulmonary artery systolic pressure: a meta-analysis. Echocardiography 2013;30(3):258-65. [DOI] [PubMed] [Google Scholar]
Testani 2010
- Testani JM, St John Sutton MG, Wiegers SE, Khera AV, Shannon RP, Kirkpatrick JN.Accuracy of noninvasively determined pulmonary artery systolic pressure. American Journal of Cardiology 2010;105(8):1192-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Torbicki 2007
- Torbicki A.Cardiac magnetic resonance in pulmonary arterial hypertension: a step in the right direction. European Heart Journal 2007;28:1187-9. [DOI] [PubMed] [Google Scholar]
Whiting 2011
- Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al.QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine 2011;155(8):529-36. [PMID: ] [DOI] [PubMed] [Google Scholar]
Zhang 2010
- Zhang RF, Zhou L, Ma GF, Shao FC, Wu XH, Ying KJ.Diagnostic value of transthoracic Doppler echocardiography in pulmonary hypertension: a meta-analysis. American Journal of Hypertension 2010;23:1261-4. [DOI: 10.1038/ajh.2010.188] [DOI] [PubMed] [Google Scholar]