Abstract
Improving adherence to antiretroviral therapy (ART) is essential for limiting HIV disease progression among young sexual minority men living with HIV. Daily diaries allow for a detailed examination of how fluctuations in psychosocial factors are associated with adherence over time. Across three cities in the United States, this study collected 60 days of quantitative data from 44 young men (between 16–24 years of age) living with HIV who have sex with men. Lagged transition models explored the associations of mood, stress, social support, substance use, and condomless intercourse with daily ART adherence. Baseline levels of illicit substance use and condomless intercourse, and a higher proportion of days with stress or marijuana use, were associated with lower ART adherence. Lapses in adherence predicted non-adherence the following day. Findings suggest prospective data collection may identify different predictors of adherence compared to retrospective recall. Lapse-management strategies are needed to improve adherence following a missed dose.
Keywords: HIV/AIDS, adherence, adolescents, daily diaries, young men who have sex with men
Introduction
Adherence to antiretroviral therapy (ART) is essential for limiting HIV disease progression and preventing onward transmission of the virus 1,2. Young sexual minority men (i.e., gay, bisexual, and other men who have sex with men) contract HIV at disproportionately high rates, and young people living with HIV are the group least likely to be engaged in HIV care and to achieve viral suppression 3. Although ART adherence among adolescents has improved as medication regimens have become less complex, young sexual minority men still face significant barriers to optimal ART adherence 4–8. As such, interventions to improve adherence among young sexual minority men are needed.
Prior research suggests ART adherence is impacted by a number of complex psychosocial factors, including mental health, substance use, social support, and life stressors 5–7,9–11. These and other risk factors are often conceptualized and measured as trait-like variables, which are considered to be static, unchanging features of the person 12,13. Exploring key variables as static trait-like attributes conceals information about the dynamic nature of constructs and may limit our understanding of how risk triggers and protective factors work to influence daily health behaviors 14,15. Alternatively, certain risk factors may be better explored in a situational context and conceptualized as dynamic state-like variables, which fluctuate over time.
The “daily diary,” also known as the Ecological Momentary Assessment (EMA) approach, provides a level of detail on situational risk factors among sexual minority young men living with HIV that goes beyond what can be observed from retrospective, self-report surveys. The daily diary, which is a prospective measurement tool, allows for the identification of state-like (i.e., situation-specific) relationships among mood, stressful events, social support, substance use, medication adherence, and sexual behavior. The daily diary data permits exploration of the temporal ordering of relationships among constructs. For example, the effects of mood on behavior can be examined in such a way that both average levels of mood and day-to-day variations in mood can be linked to behaviors.
In a study among adults living with HIV, Cook and colleagues 16 used a daily diary to examine trait-like (i.e., static) predictors of ART adherence measured at a single time point at baseline and state-like (i.e., fluctuating) predictors of ART adherence measured daily. They found differing trait-like versus state-like predictors of adherence, with perceived control acting as a trait-like predictor and mood and motivation acting as dynamic state-like predictors. Overall, this suggests a daily diary approach can provide more detail on the trait-like and state-like mechanisms driving non-adherence. However, Cook and colleagues 16 focused on adults, and results may not be generalizable to adolescents, who have lower rates of treatment utilization and viral suppression 3.
Over the past decade, there has been a proliferation of promising technology-driven interventions to improve ART adherence 7,17–20. Interventions will become more sustainable and cost-efficient for use in low-resource settings if researchers can identify the ideal timing for intervention delivery 21. There have been mixed findings on whether brief interventions, such as text-message adherence reminders, are more effective when sent on a pre-determined schedule or when triggered by lapses in adherence 20,22–25. Less is known about whether there are other daily variables contributing to adherence lapses that can be used to prompt efficient, personalized technology-delivered interventions.
Using structured electronic daily diaries, the current research aimed to fill a gap in the literature by exploring situational factors related to HIV medication adherence, including mood, stressful events, social support, sexual risk behavior, and substance use, among young men who have sex with men who were living with HIV and prescribed to take ART. A secondary goal was to identify how daily diary data can inform technology-driven adherence interventions.
Methods
Study Design
This study employed a structured daily diary to describe fluctuations in key psychological and behavioral variables impacting daily ART adherence among young men who have sex with men (YMSM) aged 16 to 24 years old living with HIV who had engaged in recent substance use and/or sexual risk behavior. Specifically, the diary examined day-to-day changes in self-reported mood, stressful events, social support, substance use, sexual behavior, and daily adherence to ART. Study methods have been described in prior work examining the feasibility and acceptability of electronic daily diaries 26.
Ethical Considerations
Ethical approval for this study was obtained from institutional review boards at all sites involved in the study. This study was performed in accordance the 1964 Declaration of Helsinki. The authors report no conflicts of interest. All participants provided written informed consent, with a waiver of parental consent for those under 18 due to privacy considerations around HIV status.
Setting
Recruitment took place between April 2013 to November 2013 at three children’s hospitals located in Philadelphia, PA, Detroit, MI, and Aurora, CO that provide comprehensive HIV services for adolescents and young adults.
Participants
All participants were young men who have sex with men (YMSM) receiving services at the clinic site, defined as being between 16–24 years of age, identifying as a cisgender man, and reporting a sexual encounter with another man involving oral or anal sex in the past year. Additional eligibility criteria included reporting condomless intercourse and/or substance use in the past 90 days (defined as having four or more alcoholic drinks in one sitting and/or two or more occasions of drug use), being HIV-infected through sexual behavior, having regular cell phone access and internet access, and meeting requirements for reading comprehension in English at the 5th grade level. The current analysis is limited to participants who indicated that they had been prescribed ART at least once within the 60 diary days. Exclusion criteria included displaying or reporting acute conditions at the informed consent visit that would interfere with the ability to provide true informed consent, including active psychiatric conditions, acute illness, or visible intoxication or self-reported active drug or alcohol use at the time of informed consent.
Procedures
Convenience sampling was used to recruit young men living with HIV at their regularly scheduled clinic visits. Site staff invited interested patients to be screened for eligibility. Those who were eligible and interested in participating were asked to provide written informed consent, with a waiver of parental consent for those under 18. At the baseline visit, all participants completed a self-report assessment including basic demographic and health information and key constructs. The baseline assessment was administered through an audio computer-assisted survey (ACASI) program.
Participants were asked to complete 66 daily dairies, split into 33 days of interactive web response diaries and 33 days of interactive voice response diaries. Web response diaries were available via a secure website accessible on any computer or mobile device with a web browser. Interactive voice response dairies were available via any telephone. An automatic voice read questions aloud and the participant entered a number on their phone keypad to respond. As reported in a prior analysis of the feasibility and acceptability of the diaries, voice diaries took longer to complete (median = 8 minutes 6 seconds) compared to internet diaries (median = 4 minutes 32 seconds)26. Participants were randomly assigned to complete either web response diaries or interactive voice response diaries as their first 33-day modality before switching to the other modality for the final 33 days. Diaries were to be completed every day within a 12-hour window between 6pm to 6am the next morning. Participants received daily reminders at 6pm and 10pm to complete unfinished diaries. For participants who completed the previous diary, questions were asked in regard to “the last 24 hours,” whereas for participants who missed a prior diary, questions were asked in regard to “since your last diary entry.”
For each modality, there was a three-day calibration period to ensure participants were able to correctly and consistently use the diary and to alleviate reactive effects. Those who missed one day or more of the first calibration period were discontinued from the study. Therefore, while participants completed 66 days of diaries, only 60 days are included in the final analysis when excluding six calibration period days.
Participants attended in-person check-in visits midway through each modality to obtain gift cards to cover the cost of phone service. Participants were provided with compensation for all study visits and for completing daily diaries.
Measures
Demographics and continuity of HIV care were measured at baseline. Continuity of care was defined as having attended an HIV-related medical appointment in the past three months.
Negative mood was measured at baseline and in the daily diary using an adapted version of the Profile of Mood States-A (POMS-A). Participants were asked to what extent they currently had negative moods, such as being worried, nervous, worn out, exhausted, unhappy, and miserable (standardized alpha at baseline = .91) 27. Response options ranged from 1 = not at all to 5 = extremely. The final variable was the total sum score, with higher scores indicating more negative mood.
On the baseline survey and daily diary, positive mood was evaluated with six items developed by Cohen et al. 28, asking participants to what extent they felt happy, pleased, cheerful, at ease, calm, and relaxed (standardized alpha at baseline = .88). Participants were instructed to answer “how are you feeling right now” with response options ranging from 1 = not at all to 5 = extremely. The final variable was the total sum score, with higher scores indicating more positive mood.
Social support at baseline was measured using the Medical Outcomes Study (MOS) social support survey 29. This 19-item survey measured various dimensions of functional support. Total scores were based on the sum of 19 items, with higher scores indicating greater social support (standardized alpha = .96). For the daily diary, emotional and practical support was measured by asking participants whether they provided or received emotional and/or practical support to or from partners, parents, friends, and other people. For example, participants were asked “whether their parent gave them emotional support since their last call,” with options including “yes,” “no,” and “not applicable.” These items were summarized by a binary indicator for if participants reported reciprocal social support (i.e., gave and received social support) versus if they denied reciprocal social support (i.e., neither gave nor received support, only gave support, or only received support).
Stressors at baseline were measured using a modified version of the Psychiatric Epidemiology Research Interview Life Events Scale (PERI) 30. The modified version contained 18 events with binary response values if the event has happened in the past six months. Scoring was conducted by adding up the number of major life events occurring. On the daily diary, daily stressful events was measured using an adapted version of a checklist of 13 daily events developed by Bolger et al. 31. Response options were dichotomous (yes or no), with items including household duties/chores, problems/fights with family and friends, extra work, financial problems, being sick/injured, insomnia, transportation problems, neighborhood violence/crime, being bullied or teased, and trouble with law enforcement officers or other authorities. The final variable was defined as a binary indicator for having experienced at least one of 13 daily stressors versus none.
At baseline and on the daily diary, participants were asked about recent sexual behaviors, including any anal/vaginal sex, and whether sex acts occurred while wearing a condom. The final variable was dichotomized as “no condomless anal/vaginal intercourse” versus “any condomless anal/vaginal intercourse.”
Substance use was measured in the baseline assessment using the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) 32. Participants responded to items assessing drug and alcohol use over the past three months, including alcohol, tobacco, marijuana, and other illicit drugs (i.e., cocaine, hallucinogens, sedatives, amphetamines, inhalants, and opioids). Responses were dichotomized into 0 = reported no substance use over the past three months or 1 = reported at least one instance of substance use over the past three months. In the daily diary, participants were asked how many alcoholic drinks they had, how many cigarettes they had, and how many times they used marijuana and other illicit drugs (amphetamine, painkillers, sedatives, Ecstasy, and cocaine). These items were then dichotomized into 0 = no daily use or 1 = endorsed daily use.
Daily ART adherence included a four-item self-report HIV medication adherence measure, which asked the following questions: 1) “are you supposed to take HIV medication,” 2) “how many pills were you supposed to take since your last call,” 3) “how many pills did you actually take since your last call,” and 4) “did you take all of your pills on time?” Participants were considered “ART adherent” on a given diary day if they met the following criteria: 1) diary indicates the participant was supposed to take ART, 2) diary indicates the participant took the correct number of pills, and 3) pills were taken on time. There were 112 instances where a participant indicated that they were “not supposed to take ART.” Given how ARTs are prescribed, the most plausible explanation for these instances is that the diary was completed incorrectly (i.e., that the diary entry for this question was not correct and, given the high rate of adherence overall, not inherently suggestive of non-adherence). For this reason, a response of “not prescribed to take ART” on a given day was treated as missing data.
Sample Size
As a result of government sequestration in 2013, unexpected financial constraints caused enrollment to end at 66 participants. The final sample consisted of 44 participants who met eligibility criteria for completing daily diaries and indicated they were supposed to take ART at least once during the 60 non-calibration diary days.
Statistical Analysis
For each time-varying psychosocial predictor of interest (i.e., mood, stress, social support, condomless intercourse, and substance use), we examined the relationship between ART adherence per day and the psychosocial predictor. Due to the small sample size in our dataset, analyses were performed separately for each psychosocial predictor. Regression models included the following: 1) a baseline measure related to the daily dairy psychosocial predictor of interest (e.g., the ASSIST measures for substance use), 2) the value of the psychosocial predictor on the current day, 3) the value of the psychosocial predictor on the prior day, 4) the mean value of the psychosocial predictor over the daily diary period (for binary data, this is the proportion of days with an affirmative response), 5) ART adherence on the prior day, and 6) baseline continuity of care – the baseline variable hypothesized a priori to be most highly associated with ART adherence, which was included in the model to control for baseline adherence. Bonferroni corrections were used to account for multiple comparisons.
Individual lagged transition models were fit using the daily ART adherence outcome and for each psychosocial predictor of interest. Transition models allow one to examine how psychosocial predictors on one day impact adherence on the following day 33. For participant i on current day j, let Yij represent ART adherence status, xij the psychosocial predictor of interest, and zi a vector of baseline covariates. This model can be specified as
Accordingly, β3 is the lagged-day effect for the psychosocial predictor of interest. A participant’s ART adherence status on the preceding day is directly incorporated into the model with α being its corresponding regression coefficient. Lastly, is the participant’s mean psychosocial predictor value over the study period.
Our statistical analysis plan prespecified that analyses would be performed using random effects models in addition to transition models. However, in most cases, the random effects models failed to converge unless overly simplistic assumptions were made regarding the random effects structure; structures that did not reflect the serial nature of our data (e.g., random intercept models). The serial correlation of our time series-like data were well modeled through the use of the lagged transition model. Thus, the results presented in this paper are based on the aforementioned transition models.
Imputation of missing values for ART adherence and daily diary psychosocial predictors of interest was performed using a fully Bayesian approach that has been shown to provide results comparable to multiple imputation by chained equations 34. Most psychosocial predictors of interest were derived from several diary items on each diary day. Due to the difficulty of imputing the individual items themselves, imputation was done on the derived psychosocial predictors (e.g., the final sum score of individual items). Accordingly, a psychosocial predictor was imputed if at least one of the items used to derive the predictor was missing. Two baseline variables also needed to be imputed for a small number of participants: the ASSIST score for cigarette use and the derived baseline indicator for having condomless intercourse in last three months. Since the number of observations requiring imputation was minimal (one value for ASSIST score and five values for condomless intercourse), values were imputed via single-imputation using the best prediction from a logistic regression model. The analyses for this paper were performed using SAS, version 9.4.
Results
Demographics
Among the 66 participants enrolled in the overall study, seven participants were excluded from analysis due to failing the calibration period or skipping all 60 non-calibration diary entries. Of the 59 participants who began the daily diary, 75% of participants (n = 44) indicated being prescribed ART at least once during the 60-day diary period and were included in the final analysis, resulting in a total of 1,928 initiated diaries. On average, participants completed 73% of diaries during the study period.
The final sample of 44 participants were between the ages of 16–24 (mean (M) = 21.1, standard deviation (SD) = 2.2. The sample was racially diverse with 64% (n = 28) identifying as Black or African American, 23% (n = 10) identifying as White, 9% (n = 4) identifying as American Indian, one identifying as Pacific Islander, and one reporting unknown. In addition, 7% (n = 3) of participants also identified as Hispanic or Latino.
See Figure 1 for a visualization of ART adherence over time. Twenty-two participants indicated taking ART at the baseline visit. The number of days participants indicated they were prescribed to take ART over the course of the diary ranged from 1–59 days (M = 36.1, SD = 16.8). Overall adherence ranged from 0% to 100%, with a mean of 83.1% (SD = 24.8). Eighteen percent (n = 8) of participants had perfect adherence and 38.6% (n = 17) had optimal adherence of 95% or higher on days where the participant indicated they were supposed to take ART.
Figure 1:
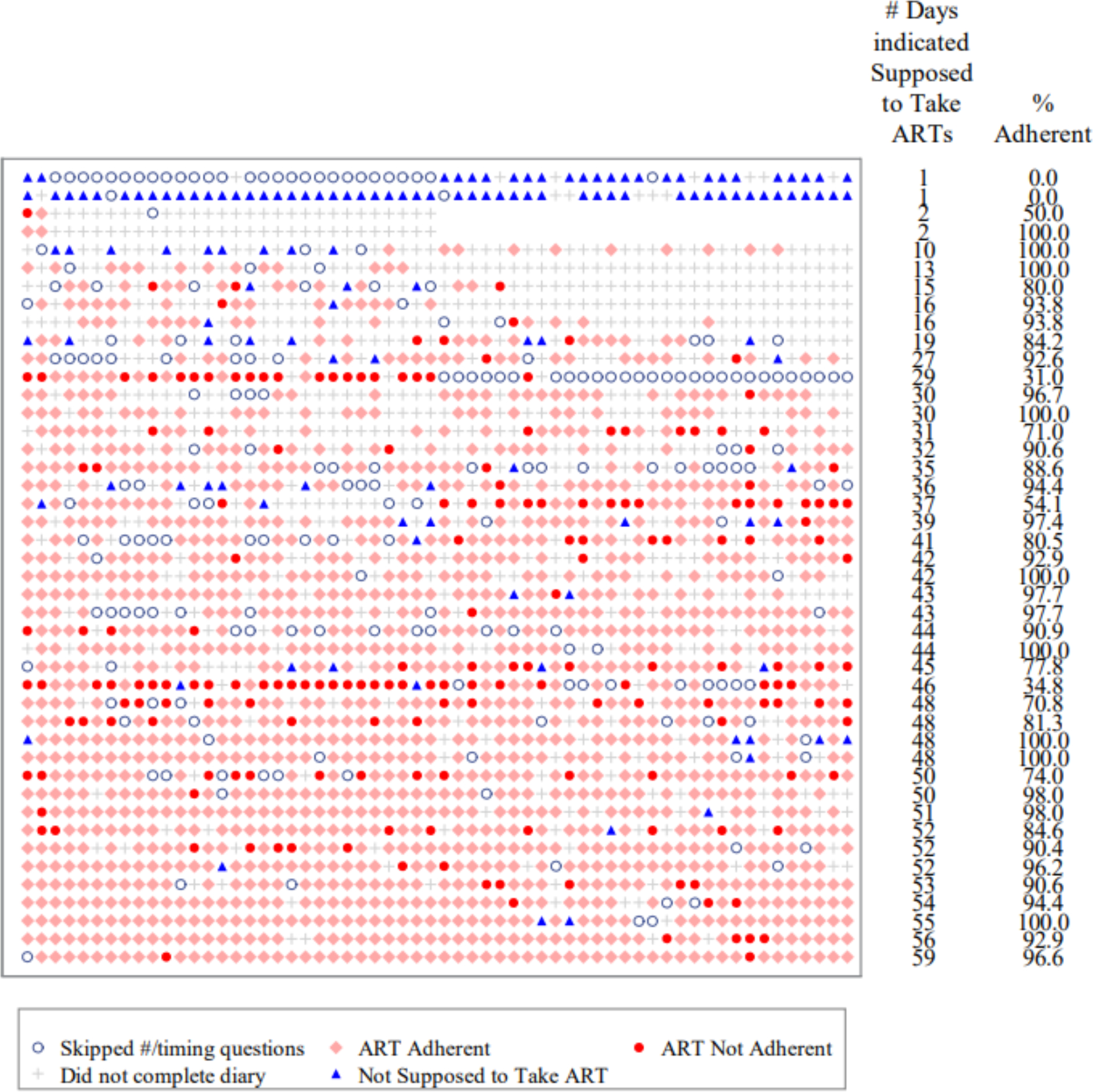
Adherence to ART across 60 daily diary days
Psychosocial Variables and ART Adherence
Descriptive outcomes for each psychosocial variable, including mean scores at baseline and the number and percent of days endorsing behaviors on the daily diary, are listed in Table I. A summary of findings on daily predictors of ART adherence can be found in Table II.
Table I.
Descriptive Statistics for Psychosocial Variables Reported at Baseline and Across the Daily Diary Period, N=44
| Variable | |
|---|---|
|
| |
| Positive Mood | |
| Baseline, M score (SD) | 12.82 (5.66) |
| Diary, M score (SD) | 10.67 (4.09) |
| Negative Mood | |
| Baseline, M score (SD) | 10.48 (9.03) |
| Diary, M score (SD) | 10.39 (6.53) |
| Social Support | |
| Baseline, M Score (SD) | 47 (19.52) |
| Diary, M days (%) | 12.39 (26) |
| Stressful Events | |
| Baseline, M score (SD) | 3.39 (2.19) |
| Diary, M days (%) | 19.98 (45) |
| Condomless Intercourse | |
| Baseline, n (%) | 26 (60) |
| Diary, M days (%) | 3.80 (8) |
| Alcohol Use | |
| Baseline, n (%) | 42 (95) |
| Diary, M days (%) | 8.86 (20) |
| Marijuana Use | |
| Baseline, n (%) | 32 (73) |
| Diary, M days (%) | 11.64 (26) |
| Other Illicit Drug Use | |
| Baseline, n (%) | 15 (34) |
| Diary, M days (%) | 1.45 (3) |
| Cigarette Use | |
| Baseline, n (%) | 23 (52) |
| Diary, M days (%) | 8.75 (19) |
Note. M = mean. SD = standard deviation. n = number of participants. Mean days endorsed refers to the number of days a variable was endorsed during the 60 daily diary days. Percent days endorsed was calculated based on the number of days the construct was endorsed divided by the number of days the construct was completed and not missing. Number of participants endorsed refers to the number of participants in the final sample that endorsed the construct at baseline.
Table II.
Models for Predictors of Interest on the Daily ART Adherence Outcome
| Predictor of Interest (x) | Model Effect | Estimate | SDa | Z Statistic | Pb | Odds Ratio | 95% CIc | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Positive Mood | Baseline Positive Mood Score | 0.00 | 0.01 | −0.32 | 0.751 | 1.00 | 0.97 | 1.02 |
| Current Day Value – xj | 0.01 | 0.02 | 0.26 | 0.792 | 1.01 | 0.97 | 1.04 | |
| Prior Day Value – xj−1 | 0.01 | 0.02 | 0.55 | 0.585 | 1.01 | 0.97 | 1.05 | |
| Mean Value – d | −0.01 | 0.03 | −0.34 | 0.736 | 0.99 | 0.94 | 1.04 | |
| Baseline Continuity of Care | −1.92 | 0.71 | −2.71 | 0.007 | 0.15 | 0.04 | 0.59 | |
| Lag-day Adherence | 2.17 | 0.19 | 11.71 | 0.000 | 8.79 | 6.11 | 12.64 | |
| Intercept | 2.12 | 0.72 | 2.93 | 0.003 | 8.34 | 2.01 | 34.50 | |
|
| ||||||||
| Social Support | Baseline Social Support | 0.00 | 0.00 | 0.42 | 0.674 | 1.00 | 0.99 | 1.01 |
| Current Day Value - xj | 0.36 | 0.25 | 1.44 | 0.149 | 1.43 | 0.88 | 2.31 | |
| Prior Day Value – xj−1 | −0.33 | 0.24 | −1.34 | 0.181 | 0.72 | 0.45 | 1.16 | |
| Mean Value – d | −0.52 | 0.39 | −1.34 | 0.181 | 0.60 | 0.28 | 1.27 | |
| Baseline Continuity of Care | −1.75 | 0.80 | −2.20 | 0.028 | 0.17 | 0.04 | 0.83 | |
| Lag-day Adherence | 2.23 | 0.18 | 12.22 | 0.000 | 9.28 | 6.49 | 13.27 | |
| Intercept | 2.01 | 0.80 | 2.52 | 0.012 | 7.50 | 1.56 | 35.94 | |
|
| ||||||||
| Stressful Events | Baseline Stressful Events | 0.12 | 0.04 | 3.19 | 0.001 | 1.13 | 1.05 | 1.21 |
| Current Day Value – xj | −0.07 | 0.21 | −0.33 | 0.743 | 0.93 | 0.62 | 1.41 | |
| Prior Day Value – xj−1 | 0.22 | 0.22 | 0.99 | 0.322 | 1.24 | 0.81 | 1.90 | |
| Mean Value – d | −1.39 | 0.38 | −3.65 | 0.000 | 0.25 | 0.12 | 0.53 | |
| Baseline Continuity of Care | −1.73 | 0.70 | −2.48 | 0.013 | 0.18 | 0.05 | 0.70 | |
| Lag-day Adherence | 2.14 | 0.18 | 11.64 | 0.000 | 8.53 | 5.95 | 12.25 | |
| Intercept | 2.19 | 0.73 | 3.00 | 0.003 | 8.96 | 2.14 | 37.52 | |
|
| ||||||||
| Condomless Intercourse | Baseline Condomless Intercourse | −0.48 | 0.17 | −2.83 | 0.005 | 0.62 | 0.45 | 0.86 |
| Current Day Value – xj | 0.20 | 0.32 | 0.63 | 0.532 | 1.22 | 0.65 | 2.29 | |
| Prior Day Value – xj−1 | −0.47 | 0.30 | −1.57 | 0.117 | 0.63 | 0.35 | 1.13 | |
| Mean Value – d | −0.37 | 0.83 | −0.45 | 0.654 | 0.69 | 0.14 | 3.50 | |
| Baseline Continuity of Care | −1.92 | 0.76 | −2.54 | 0.011 | 0.15 | 0.03 | 0.65 | |
| Lag-day Adherence | 2.18 | 0.18 | 11.93 | 0.000 | 8.85 | 6.19 | 12.67 | |
| Intercept | 2.52 | 0.78 | 3.21 | 0.001 | 12.44 | 2.67 | 57.92 | |
|
| ||||||||
| Alcohol Use | Baseline Alcohol Use | 0.68 | 0.28 | 2.47 | 0.013 | 1.97 | 1.15 | 3.38 |
| Current Day Value – xj | 0.07 | 0.22 | 0.33 | 0.739 | 1.08 | 0.70 | 1.67 | |
| Prior Day Value – xj−1 | −0.32 | 0.23 | −1.39 | 0.165 | 0.73 | 0.47 | 1.14 | |
| Mean Value – d | −0.21 | 0.55 | −0.38 | 0.707 | 0.81 | 0.28 | 2.38 | |
| Baseline Continuity of Care | −1.76 | 0.83 | −2.13 | 0.033 | 0.17 | 0.03 | 0.87 | |
| Lag-day Adherence | 2.20 | 0.18 | 12.21 | 0.000 | 9.05 | 6.35 | 12.89 | |
| Intercept | 1.42 | 0.88 | 1.62 | 0.106 | 4.13 | 0.74 | 23.05 | |
|
| ||||||||
| Marijuana Use | Baseline Marijuana Use | 0.85 | 0.16 | 5.39 | 0.000 | 2.34 | 1.72 | 3.18 |
| Current Day Value – xj | 0.36 | 0.33 | 1.10 | 0.273 | 1.43 | 0.75 | 2.71 | |
| Prior Day Value – xj−1 | 0.62 | 0.36 | 1.73 | 0.084 | 1.85 | 0.92 | 3.73 | |
| Mean Value – d | −1.40 | 0.47 | −2.97 | 0.003 | 0.25 | 0.10 | 0.62 | |
| Baseline Continuity of Care | −1.54 | 0.76 | −2.04 | 0.042 | 0.21 | 0.05 | 0.94 | |
| Lag-day Adherence | 2.08 | 0.19 | 10.73 | 0.000 | 8.01 | 5.48 | 11.72 | |
| Intercept | 1.44 | 0.77 | 1.87 | 0.061 | 4.23 | 0.94 | 19.12 | |
|
| ||||||||
| Illicit Drug Use | Baseline Illicit Substance Use | −0.40 | 0.15 | −2.64 | 0.008 | 0.67 | 0.50 | 0.90 |
| Current Day Value – xj | −0.86 | 0.47 | −1.81 | 0.069 | 0.42 | 0.17 | 1.07 | |
| Prior Day Value – xj−1 | 0.51 | 0.54 | 0.95 | 0.343 | 1.66 | 0.58 | 4.75 | |
| Mean Value – d | −0.06 | 1.20 | −0.05 | 0.961 | 0.94 | 0.09 | 9.93 | |
| Baseline Continuity of Care | −1.68 | 0.70 | −2.40 | 0.016 | 0.19 | 0.05 | 0.74 | |
| Lag-day Adherence | 2.20 | 0.18 | 11.94 | 0.000 | 9.04 | 6.30 | 12.97 | |
| Intercept | 2.05 | 0.71 | 2.90 | 0.004 | 7.79 | 1.95 | 31.15 | |
|
| ||||||||
| Cigarette Use | Baseline Cigarette Use | 0.09 | 0.17 | 0.51 | 0.609 | 1.09 | 0.78 | 1.51 |
| Current Day Value – xj | 0.48 | 0.37 | 1.29 | 0.197 | 1.61 | 0.78 | 3.35 | |
| Prior Day Value – xj−1 | −0.55 | 0.36 | −1.52 | 0.129 | 0.58 | 0.28 | 1.17 | |
| Mean Value – d | 0.88 | 0.53 | 1.66 | 0.097 | 2.41 | 0.85 | 6.82 | |
| Baseline Continuity of Care | −1.74 | 0.67 | −2.58 | 0.009 | 0.18 | 0.05 | 0.66 | |
| Lag-day Adherence | 2.12 | 0.18 | 11.88 | 0.000 | 8.30 | 5.85 | 11.76 | |
| Intercept | 1.81 | 0.69 | 2.64 | 0.008 | 6.11 | 1.59 | 23.48 | |
Note.
SD = standard deviation
P = probability value
CI = 95% confidence interval
For a binary predictor, the mean value is equal to the proportion of days where the predictor was equal to 1
Mood and Social Support
No relationship was identified between ART adherence and positive mood. Due to limited variability in diary responses to negative mood items, we were unable to estimate a transition model using that psychosocial predictor. In other words, for the negative mood construct, most diary responses were identical for participants over the entire study period. No associations were found between social support and ART adherence
Stressful Events
On the baseline measure of the number of stressful events occurring over the past six months, the estimated adjusted odds of being adherent to ART increased by 13% for each additional stressful event reported, with a corresponding 95% confidence interval (CI) of 5% - 21% (i.e., Odds Ratio (OR) = 1.13 with 95% CI [1.05, 1.21]). The reverse relationship was found when examining the proportion of days with stressful events occurring over the 60-day course of the diary; the proportion of days experiencing a stressful event on the diary was negatively associated with adherence, with an increase of one in the average number of days where a stressful event occurred being associated with a 75% decrease (95% CI [47%, 88%]) in the odds of being adherent (i.e., OR = 0.25 with 95% CI [0.12, 0.53]).
Condomless Intercourse
The odds of being adherent to ART were estimated to be 38% lower (95% CI [14% - 55%]) among participants who reported condomless intercourse at baseline compared to participants who denied condomless intercourse at baseline (i.e., OR = 0.62 with 95% CI [0.45, 0.86]). Condomless intercourse throughout the daily diary was not associated with ART adherence.
Substance Use
For alcohol use, the odds of being adherent to ART were estimated to be 97% higher (95% CI [15%, 238%) for participants who endorsed alcohol use over the past three months at baseline compared to participants who did not (i.e., OR = 1.97 with 95% CI [1.15, 3.38]. On the daily diary, participants who indicated alcohol use on a given day had a lower level of adherence, but the difference was not substantial with an odds ratio of 1.08 (95% CI: 0.70 – 1.67).
When examining marijuana use at baseline, the odds of being adherent to ART were estimated to be 2.34 times higher among participants who endorsed marijuana use over the past three months compared to participants who did not (95% CI [1.72 – 3.18]). A reverse relationship was found between the proportion of days using marijuana over the course of the diary, with a one-unit increase in the proportion of marijuana use across the diary associated with a 75% decrease (95% CI [38% - 90%]) in the odds of daily adherence (i.e., OR = 0.25, 95% CI [0.10, 0.62]).
Individuals who reported illicit substance use over the past three months were associated with a 33% decrease (95% CI [10%, 50%]) in the odds of being adherent to ART compared to participants who did not report illicit substance use (i.e., OR = 0.67, 95% CI [0.10, 0.50]. On the daily diary, illicit substance use was not associated with adherence. Cigarette use was also not associated with adherence.
Previous Day Adherence
In all models, ART adherence on the previous day was associated with ART adherence on the following day. While controlling for all psychosocial covariates in separate models, adherence on the previous day was associated with between 8.01 to 9.28 times the odds of being adherent on the following day.
Discussion
In summary, in the present daily diary study, lower ART adherence on a given day among YMSM living with HIV was associated with the following baseline variables: (1) a lower number of stressful events over the prior six months; (3) any unprotected intercourse over the past three months (compared to none); (4) no alcohol use over the past three months (compared to any use); (5) any illicit substance use over the past three months (compared to none); and (6) no marijuana use over the past three months (compared to any use). However, lower ART adherence was associated with a greater proportion of days using marijuana and a higher proportion of stressful events across the daily diary period. Non-adherence on a prior day was strongly associated subsequent non-adherence, even after controlling for psychosocial variables.
The present study suggests that retrospectively measuring trait-like variables compared to prospectively measuring state-like variables can lead to different, and potentially contradictory, findings about predictors of daily ART adherence. Similar findings were found by Cook and colleagues 16, who measured trait factors at baseline and state factors prospectively in daily diaries and reported differing trait versus state predictors of ART adherence. Although some of these findings appear counter-intuitive (for example, endorsing marijuana use and alcohol use over the past three months at baseline was associated with better adherence), there could be a number of explanations for these findings.
First, differences in findings for state-like versus trait-like variables may be due to measurement. Participants may be less accurate recalling variables retrospectively at baseline compared to prospective daily measurement. Retrospective versus daily surveys may prompt the use of different cognitive recall strategies, with retrospective surveys more strongly influenced by generalized beliefs about oneself and the world15,35. It is also possible that participants miscalculated whether stressful events and/or substance use occurred in the specific time frame requested in the instructions for the retrospective survey, whereas the daily surveys would presumably reduce this source of error. The possibility that daily diaries provide more accurate data on psychosocial constructs and health behaviors among YMSM should be considered and investigated in future research.
Furthermore, for stressful events, our measure at baseline captured the number of different types of stressful events over the past six months, but not the frequency of stressful events, which was captured in the diary. Prior research shows long-term chronic stress is more detrimental to health than short-term acute stress 36,37. However, to understand the impact of chronic stress on health, it may be essential to measure the type, frequency, and duration of prior stressful events at baseline rather than just their presence or absence. Findings regarding stress and mood also differed from Cook and colleagues’16 daily diary study of adherence in adults. Cook et al.,16 found a strong relationship between mood and adherence and a weaker relationship between stress and adherence among adults, whereas we failed to find a relationship between mood and adherence and found a stronger relationship between stress and adherence among adolescents/young adults. This raises the potential that there are different predictors of adherence between adolescents/young adults and older adults, particularly when it comes to stress and mood. However, discrepancies may also be due to the use of divergent measures across studies, and additional research is needed to explore reasons for differences between adolescents and adults.
Findings regarding substance use were particularly complex, which is in line with previous research showing that the impact of chronic substance use versus occasional substance use is different for each drug class and depends on type of outcome. For example, research on cannabis shows occasional marijuana users show greater impairment after marijuana consumption compared to chronic marijuana users, whereas self-reported memory and motivation are lower among chronic cannabis users compared to occasional cannabis users 38,39. In our model, endorsing any marijuana use and alcohol use at baseline (i.e., at least once over the past three months) was associated with better adherence, whereas frequency of use across the diary was associated with worse adherence, although this was only statistically significant for marijuana use. There may be important confounding variables or mechanisms, such as increased relaxation and social engagement, that would explain why individuals with low or moderate amounts of substance use would have increased adherence compared to those with no use or high use 40. Understanding the nuanced impact of marijuana use on health is particularly relevant as medical and recreational cannabis becomes more widely available. During the study period, recreational use was only legal in Colorado; since then, medical use has been legalized in Pennsylvania and recreational use has been legalized in Michigan. Research is needed to examine how changes in legality might impact findings, although for the current research, cannabis use would have remained illegal for most participants, including all participants under 21-years-old and those outside of Colorado. Overall, these findings highlight the dynamic and complex interactions between psychosocial risk factors and health behaviors such as ART adherence and emphasize the need to consider not only the presence or absence of factors, but also their duration and chronicity over time.
The only variable that was associated with the following day’s non-adherence across all models was non-adherence on the previous day, with a single day of non-adherence more likely to be followed by a continued lapse. This may be due to unmeasured factors causing extended adherence lapses, such as a multiple-day disruption in routine 41. Alternatively, it is possible that missing one dose triggers the following day’s non-adherence, which is supported by research across topics in health behavior showing the lapses pose a risk for behavior change 42. Further research is needed to explore the mechanisms leading to multiple-day lapses in adherence.
Limitations
Overall, our study is limited due to small sample size and missing data. In particular, there is a risk that missing data is non-random, with participants skipping the diary on days where they were not adherent. A prior mixed-methods analysis of the feasibility and acceptability of completing diaries in this sample suggests that reasons for missed diaries were varied, with no participants reporting that missing diaries was related to ART adherence specifically 26. Furthermore, diary compliance was unrelated to key baseline variables and may be more closely related to daily diary modality, with voice diaries completed less frequently than web diaries 26.
The small sample size of the study led us to evaluate the potential impact of each of the predictors of interest using a separate model and control for multiple comparisons using standard methods. This was done, as opposed to attempting to fit one or more multivariate models that incorporated several predictors simultaneously, primarily due to general instability of regression models when even a moderate number of predictors are included in small sample settings and because our focus was not building a predictive model for longitudinal ART adherence. Moreover, the use of transition models to account for series correlation in the data over perhaps more common methods such as random effects models was, in part, a result of inability to model serial correlation adequately using random effects and obtain stable estimates of the model (e.g., in many cases, random effects models could not be estimated). The transition model provides a much more parsimonious mechanism for modeling serial correlation in the data and provides a very interpretable effect of prior day adherence on adherence.
In addition, the direction of the estimated effect for continuity of care in each of the adherence analyses is counterintuitive. These results must be viewed with skepticism due to the limited number of participants (two out of 44) who reported having no HIV-related medical appointment in the past three months. The statistical significance of these results is driven by the very high adherence reported by those two participants (>97%) relative to the group of 42 participants who met the continuity of care criteria and who, on average, had high but notably lower reported adherence. The associated p-values are likely anti-conservative as a result of the very small sample size in the group reporting a lack of continuity of care.
Generalizability
Our study included a racially and ethnically diverse sample of YMSM living with HIV who were attending services at youth-focused HIV clinics across three major US cities. Although the requirement to complete the calibration days may lead to a sample that has more stable life circumstances, compensation for cell phone service was provided throughout the study to increase the likelihood that participants from varied socioeconomic backgrounds would have equal opportunity to complete the dairies. The current sample may be limited in that all youth were engaged in HIV services at baseline, although not all participants were prescribed ART at the baseline visit. In addition, ART adherence was varied, indicating that being engaged at the clinic did not lead to universally high adherence. The use of convenience sampling may have led to sampling bias; however, the goal of enrolling participants who were attending regular clinic visits mirrors realistic procedures in HIV clinics, as clinic-based interventions can only be offered to individuals seeking care. Overall, the regional and racial/ethnic diversity of our sample suggests results may be generalizable to similar young men who have sex with men seeking HIV services in urban locations in the US.
Implications
An aim of this study was to identify triggers to adherence lapses that may inform efficient strategies for technology-driven adherence interventions for young sexual minority men living with HIV. There are a number of adherence interventions that take a holistic approach to simultaneously improve mental health, risk behaviors, and ART adherence, such as cognitive behavioral therapy 7,43. One strategy is to prioritize interventions for youth who report any risk factors at a screening visit, such as targeted interventions for youth who indicate having condomless intercourse or illicit substance use. A second strategy is to prioritize interventions for youth who show chronically high levels of daily risk factors. For example, individuals who indicate a high daily frequency of marijuana use and stressful events may require additional interventions to improve adherence.
Furthermore, there is a need for additional research to explore mechanisms through which engaging in marijuana and alcohol use at baseline was associated with improved adherence. For example, if moderate marijuana use is a proxy for social engagement, then interventions to improve social engagement may be necessary; alternatively, if moderate marijuana use decreases stress, then stress-management interventions may be more appropriate.
Lastly, although research has been inconsistent as to whether there is a benefit to lapse-triggered reminders to improve ART adherence, research in the field of health behavior change more broadly suggests there are benefits to interventions that give participants tools to manage lapses without becoming discouraged 42. For example, Agapie and colleagues 42 developed a technology-driven lapse management intervention to reduce time spent on social media websites. In this study, all participants were awarded digital “gold stars” on days when they reached their goal for reduced minutes spent on social media. Half of the participants were also given a limited number of “cheat minutes” that they could use to obtain gold stars on days where they did not achieve their goal. Participants given “cheat minutes” had lower social media use overall compared to participants who were not given cheat minutes. Although additional research is needed to explore mechanisms driving behavior change in lapse management interventions, it is possible that lapse management strategies may improve positive attitudes and self-efficacy around adherence and decrease the likelihood that a single lapse will turn into a lengthier period of non-adherence. Combining daily reminders with lapse-management tools may therefore be one way to improve ART adherence to optimal levels.
Conclusions
Overall, the current study suggests that consistently high levels of stress and marijuana use, as well as reporting any condomless intercourse and illicit substance use over the past three months, were predictive of daily ART non-adherence among young sexual minority men living with HIV. Furthermore, a single lapse in adherence was associated with non-adherence on the following day. Together, this suggests it may be beneficial to deliver more resource-intensive adherence interventions to YMSM who report chronic or severe stress, substance use, and sexual risk behavior, whereas daily interventions might choose to capitalize on lapse-management strategies to prevent future lapses from occurring. Future research is needed to determine the efficacy of these approaches among young sexual minority men with HIV, as well as the importance of daily diaries as a tool for understanding treatment efficacy and situational mechanisms leading to improved adherence.
Acknowledgements
We acknowledge NICHD DASH for providing the data that was used for this research. We thank the Adolescent Medicine Trials Network for HIV/AIDS Interventions, ATN 112 protocol team HIV clinic sites, and all of the clinic staff involved in this study, including Dr. Craig Wilson, ATN Principal Investigator; Dr. Patrick A. Wilson, ATN 112 Protocol Chair; The Adolescent Medicine Trials Network for HIV /AIDS Interventions (ATN), with NIH support through NICHD (Kapogiannis, B and Lee, S), with supplemental funding from NIDA (Davenny, K) and NIMH (Allison, S): U01 HD 40533 and U01 HD 40474. We extend our sincerest gratitude to each participant for their effort and willingness to take part in this research.
Funding
This work was supported by the Adolescent Medicine Trials Network for HIV/AIDS Interventions (ATN) from the National Institutes of Health (U24HD089880) through the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), National Institute on Minority Health and Health Disparities (NIMHD), National Institute of Mental Health (NIMH), and National Institute on Drug Abuse (NIDA). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Reference List
- 1.Ford N, Darder M, Spelman T, Maclean E, Mills E, Boulle A. Early adherence to antiretroviral medication as a predictor of long-term HIV virological suppression: Five-year follow up of an observational cohort. Ndhlovu LC, ed. PLoS ONE. 2010;5(5):e10460. doi: 10.1371/journal.pone.0010460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21. doi: 10.7326/0003-4819-133-1-200007040-00004 [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. HIV and Youth. Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention; 2020. https://www.cdc.gov/hiv/pdf/group/age/youth/cdc-hiv-youth.pdf [Google Scholar]
- 4.Beer L, Mattson CL, Bradley H, Shouse RL. Trends in ART prescription and viral suppression among HIV-positive young adults in care in the United States, 2009–2013. JAIDS J Acquir Immune Defic Syndr. 2017;76(1):e1–e6. doi: 10.1097/QAI.0000000000001427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hosek SG, Harper GW, Domanico R. Predictors of medication adherence among HIV-infected youth. Psychol Health Med. 2005;10(2):166–179. doi: 10.1080/1354350042000326584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murphy DA, Belzer M, Durako SJ, Sarr M, Wilson CM, Muenz LR. Longitudinal antiretroviral adherence among adolescents infected with Human Immunodeficiency Virus. Arch Pediatr Adolesc Med. 2005;159(8):764. doi: 10.1001/archpedi.159.8.764 [DOI] [PubMed] [Google Scholar]
- 7.Reisner SL, Mimiaga MJ, Skeer M, Perkovich B, Johnson CV, Safren SA. A review of HIV antiretroviral adherence and intervention studies among HIV-infected youth. Top HIV Med Publ Int AIDS Soc USA. 2009;17(1):14–25. [PMC free article] [PubMed] [Google Scholar]
- 8.Williams PL, Storm D, Montepiedra G, et al. Predictors of adherence to antiretroviral medications in children and adolescents with HIV infection. Pediatrics. 2006;118(6):e1745–e1757. doi: 10.1542/peds.2006-0493 [DOI] [PubMed] [Google Scholar]
- 9.Halkitis PN, Kutnick AH, Slater S. The social realities of adherence to protease inhibitor regimens: Substance use, health care and psychological states. J Health Psychol. 2005;10(4):545–558. doi: 10.1177/1359105305053422 [DOI] [PubMed] [Google Scholar]
- 10.Harkness A, Bainter SA, O’Cleirigh C, Mendez NA, Mayer KH, Safren SA. Longitudinal effects of syndemics on ART non-adherence among sexual minority men. AIDS Behav. 2018;22(8):2564–2574. doi: 10.1007/s10461-018-2180-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.White JM, Gordon JR, Mimiaga MJ . The role of substance use and mental health problems in medication adherence among HIV-infected MSM. LGBT Health. 2014;1(4):319–322. doi: 10.1089/lgbt.2014.0020 [DOI] [PubMed] [Google Scholar]
- 12.Bajos N Social factors and the process of risk construction in HIV sexual transmission. AIDS Care. 1997;9(2):222–237. [DOI] [PubMed] [Google Scholar]
- 13.Schroder KEE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Ann Behav Med. 2003;26(2):104–123. doi: 10.1207/S15324796ABM2602_03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bylsma LM, Rottenberg J. Uncovering the dynamics of emotion regulation and dysfunction in daily life with ecological momentary assessment. In: Nyklicek I, Vingerhoets A, Zeelenberg M, eds. Emotion Regulation and Well-Being. Springer; 2011:225–244. [Google Scholar]
- 15.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4(1):1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415 [DOI] [PubMed] [Google Scholar]
- 16.Cook PF, Schmiege SJ, Starr W, Carrington JM, Bradley-Springer L. Prospective state and trait predictors of daily medication adherence behavior in HIV. Nurs Res. 2017;66(4):275–285. doi: 10.1097/NNR.0000000000000216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Amico KR. Evidence for technology interventions to promote ART adherence in adult populations: A review of the literature 2012–2015. Curr HIV/AIDS Rep. 2015;12(4):441–450. doi: 10.1007/s11904-015-0286-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dowshen N, Kuhns LM, Johnson A, Holoyda BJ, Garofalo R. Improving adherence to antiretroviral therapy for youth living with HIV/AIDS: A pilot study using personalized, interactive, daily text message reminders. J Med Internet Res. 2012;14(2):e51. doi: 10.2196/jmir.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mbuagbaw L, Sivaramalingam B, Navarro T, et al. Interventions for enhancing adherence to antiretroviral therapy (ART): A systematic review of high quality studies. AIDS Patient Care STDs. 2015;29(5):248–266. doi: 10.1089/apc.2014.0308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thakkar J, Kurup R, Laba T-L, et al. Mobile telephone text messaging for medication adherence in chronic disease: A meta-analysis. JAMA Intern Med. 2016;176(3):340. doi: 10.1001/jamainternmed.2015.7667 [DOI] [PubMed] [Google Scholar]
- 21.Haberer JE, Sabin L, Amico KR, et al. Improving antiretroviral therapy adherence in resource-limited settings at scale: a discussion of interventions and recommendations. J Int AIDS Soc. 2017;20(1):21371. doi: 10.7448/IAS.20.1.21371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): A meta-analysis of randomized controlled trials. Winston A, ed. PLoS ONE. 2014;9(2):e88166. doi: 10.1371/journal.pone.0088166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haberer JE, Musiimenta A, Atukunda EC, et al. Short message service (SMS) reminders and real-time adherence monitoring improve antiretroviral therapy adherence in rural Uganda. AIDS. 2016;30(8):1295–1299. doi: 10.1097/QAD.0000000000001021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Orrell C, Cohen K, Mauff K, Bangsberg DR, Maartens G, Wood R. A randomized controlled trial of real-time electronic adherence monitoring with text message dosing reminders in people starting first-line antiretroviral therapy. JAIDS J Acquir Immune Defic Syndr. 2015;70(5):495–502. doi: 10.1097/QAI.0000000000000770 [DOI] [PubMed] [Google Scholar]
- 25.Sabin LL, Bachman DeSilva M, Gill CJ, et al. Improving adherence to antiretroviral therapy with triggered real-time text message reminders: The China adherence through technology study. JAIDS J Acquir Immune Defic Syndr. 2015;69(5):551–559. doi: 10.1097/QAI.0000000000000651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cherenack EM, Wilson PA, Kreuzman AM, Price GN, The Adolescent Medicine Trials Network for HIV/AIDS Interventions. The feasibility and acceptability of using technology-based daily diaries with HIV-infected young men who have sex with men: A comparison of internet and voice modalities. AIDS Behav. 2016;20(8):1744–1753. doi: 10.1007/s10461-016-1302-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Terry PC, Lane AM, Lane HJ, Keohane L. Development and validation of a mood measure for adolescents. J Sports Sci. 1999;17(11):861–872. doi: 10.1080/026404199365425 [DOI] [PubMed] [Google Scholar]
- 28.Cohen S, Doyle WJ, Turner RB, Alper CM, Skoner DP. Emotional style and susceptibility to the common cold. Psychosom Med. 2003;65(4):652–657. doi: 10.1097/01.PSY.0000077508.57784.DA [DOI] [PubMed] [Google Scholar]
- 29.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. [DOI] [PubMed] [Google Scholar]
- 30.Dohrenwend BS, Krasnoff L, Askenasy AR, Dohrenwend BP. The Psychiatric Epidemiology Research Interview Life Events Scale (PERI). In: Handbook of Stress: Theoretical and Clinical Aspects. Free Press New York; 1982:332–363. [Google Scholar]
- 31.Bolger N, Davis A, Rafaeli E. Effects of daily stress on negative mood. Annu Rev Psychol. 1989;57(5):808–818. [DOI] [PubMed] [Google Scholar]
- 32.WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability and feasibility. Addiction. 2002;97(9):1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x [DOI] [PubMed] [Google Scholar]
- 33.Fitzmaurice G, Laird NM, Ware JH. Applied Longitudinal Analysis. 2nd ed. John Wiley & Sons, Inc.; 2011. [Google Scholar]
- 34.Ibrahim JG, Chen M-H, Lipsitz SR, Herring AH. Missing-data methods for Generalized Linear Models: A comparative review. J Am Stat Assoc. 2005;100(469):332–346. doi: 10.1198/016214504000001844 [DOI] [Google Scholar]
- 35.Cook PF, Schmiege SJ, Reeder B, Horton-Deutsch S, Lowe NK, Meek P. Temporal immediacy: A two-system theory of mind for understanding and changing health behaviors. Nurs Res. 2018;67(2):108–121. doi: 10.1097/NNR.0000000000000265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cohen S, Janicki-Deverts D, Doyle WJ, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci. 2012;109(16):5995–5999. doi: 10.1073/pnas.1118355109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dhabhar FS. Acute stress enhances while chronic stress suppresses skin immunity: The role of stress hormones and leukocyte trafficking. Ann N Y Acad Sci. 2006;917(1):876–893. doi: 10.1111/j.1749-6632.2000.tb05454.x [DOI] [PubMed] [Google Scholar]
- 38.Hartley S, Simon N, Larabi A, et al. Effect of smoked cannabis on vigilance and accident risk using simulated driving in occasional and chronic users and the pharmacokinetic–pharmacodynamic relationship. Clin Chem. 2019;65(5):684–693. doi: 10.1373/clinchem.2018.299727 [DOI] [PubMed] [Google Scholar]
- 39.Kouri E, Pope GH, Yurgelun-Todd D, Grub S. Attributes of heavy vs. occasional marijuana smokers in a college population. Biol Psychiatry. 1995;38:475–481. [DOI] [PubMed] [Google Scholar]
- 40.Hammersley R, Leon V. Patterns of cannabis use and positive and negative experiences of use amongst university students. Addict Res Theory. 2006;14(2):189–205. doi: 10.1080/16066350500453309 [DOI] [Google Scholar]
- 41.Blackstone K, Woods SP, Weber E, Grant I, Moore DJ, the HNRP Group. Memory-based strategies for antiretroviral medication management: An evaluation of clinical predictors, adherence behavior awareness, and effectiveness. AIDS Behav. 2013;17(1):74–85. doi: 10.1007/s10461-012-0308-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Agapie E, Avrahami D, Marlow J. Staying the course: System-driven lapse management for supporting behavior change. In: Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems. ACM; 2016:1072–1083. doi: 10.1145/2858036.2858142 [DOI] [Google Scholar]
- 43.Safren SA, O’Cleirigh C, Tan JY, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychol. 2009;28(1):1–10. doi: 10.1037/a0012715 [DOI] [PMC free article] [PubMed] [Google Scholar]


