Abstract
Objective:
Childhood sleep problems are associated with insufficient parental sleep and adverse maternal mental health symptoms, which may be exacerbated when mothers/toddlers co-sleep (i.e., bed/room sharing). This study examines maternal sleep duration as a mechanism linking perceived toddler sleep problems with maternal mental health and examines whether these associations vary by co-sleeping, in addition to exploring alternative models.
Methods:
Low-income mothers of toddlers (n = 280) (age 12–32 months) recruited from Women, Infants, and Children and pediatric clinics provided demographic information and completed questionnaires on their toddler’s sleep and their own sleep duration and mental health symptoms (depressive symptoms, anxiety, and stress). Indirect and conditional indirect models were conducted to examine the relation between perceived toddler sleep problems and maternal mental health.
Results:
Perceived toddler sleep problems were associated with an average decrease of 51 minutes in maternal sleep when co-sleeping (mean = 6.1 h). Maternal sleep duration mediated the relation between perceived toddler sleep problems and maternal symptoms of depression, anxiety, and stress for co-sleeping mothers. Maternal sleep duration did not mediate relations between maternal mental health symptoms and perceived toddler sleep problems.
Conclusion:
This study provides a conceptual model by which parent and child sleep is related to parental mental health. Practitioners might consider alternatives to co-sleeping when discussing sleep arrangements with parents. Future studies should replicate results longitudinally and examine whether reducing co-sleeping improves maternal sleep duration and reduces perceptions of toddler sleep problems.
Index terms: co-sleeping, maternal sleep duration, perceived toddler sleep problems, maternal mental health, moderated-mediation
Sleep is critical for everyday functioning and can affect physical health, mood, and behavior.1,2 Sleep patterns across the first years of life are frequently changing, with wide individual variability.2 In toddlerhood, most children establish sleep regulation, with night awakenings followed by returning to sleep without parental intervention. However, extended or more frequent night awakenings may occur in some toddlers and may necessitate parental intervention to return to sleep.3 Approximately 20% to 30% of parents report concerns about their infants’ or toddlers’ sleep.4 Such early childhood sleep problems have been repeatedly associated with insufficient parental sleep, parental stress, and maternal depression,1,5–8 especially if the child and parent are co-sleeping.1,6,9–14 Co-sleeping has been studied mainly in parents of infants and less is known about parents of toddlers.
Co-sleeping is defined as a parent and child sleeping on the same surface, and/or sleeping in the same room, but on separate sleeping surfaces.14–17 Views regarding the risks and benefits of co-sleeping in the United States are mixed. During infancy, co-sleeping is associated with an increased risk of Sudden Infant Death Syndrome and is discouraged by health care providers.18 The 2016 American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome recommends that to reduce the risk of sleep-related deaths, infants sleep in the same bedroom as their parents on a separate sleeping surface, such as a crib or bassinet, and never on a soft surface such as a couch or armchair.19 There are not sleeping environment recommendations for toddlers. The risks and benefits of co-sleeping during toddlerhood have not been examined closely.20 Evidence suggests that infant co-sleeping is associated with decreased maternal sleep quality and duration17 as well as poor maternal mental health,9,21 but these relations have not been studied extensively among toddlers.
Co-sleeping is common among minority, low-income families compared with white, high-income families. For example, a 17-year US population–based study found that low-income mothers are 1.7 times more likely to bed share compared with high-income mothers, and black families are 3.5 times more likely to bed share compared with white families.22 Co-sleeping may be an economic necessity for many low-income families. Housing occupies a major part of the budget for low-income families, and many live in crowded conditions, sharing bedrooms and beds.23 Given that both mental health symptoms and co-sleeping are prevalent among low-income populations,20,22,24–26 a detailed understanding of co-sleeping as a risk factor for mental health symptoms could inform efforts to reduce health disparities.27
Maternal perception of toddler sleep problems has separately been associated with shortened maternal sleep and maternal mental health symptoms,1,28,29 but it is not clear how co-sleeping affects these relations, and a comprehensive model has not been examined. Parents who believe that their child has a sleep problem may view co-sleeping as a solution to minimize disruptions from extended and frequent night awakenings.13 Although co-sleeping may provide initial improvement for toddler sleep, repeated extended toddler night awakenings that require maternal intervention could result in chronic shorter maternal sleep duration.13,17 Subsequently, short sleep duration in mothers may be linked with poor maternal mental health symptoms.11
The transactional model emphasizes interactive relations between maternal and toddler sleep, whereby directions may vary.30,31 In the context of co-sleeping, maternal perception of toddler sleep problems may be associated with shortened maternal sleep and subsequently poor maternal mental health outcomes. Alternatively, short maternal sleep duration may affect children’s sleep.30,32 Children’s bedtimes and wake times are often related to maternal bed/wake times, especially in the context of co-sleeping.12,33,34
The purpose of this study is to test an integrated model to examine whether associations between perceived toddler sleep problems and maternal mental health vary by co-sleeping versus independent sleeping. This study addresses gaps in the literature by (1) examining the associated risks of toddler co-sleeping in an age group that has been understudied; (2) examining the relation between sleep and mental health among low-income families (a population at risk for health disparities); and (3) proposing a comprehensive model, currently lacking in the literature.
We tested 2 hypotheses and 1 alternative hypothesis: (1) co-sleeping moderates the relation between perceived toddler sleep problems and maternal sleep duration and (2) maternal sleep duration conditionally mediates the relation between perceived toddler sleep problems and maternal mental health symptoms (i.e., stress, anxiety, and depressive symptoms) based on co-sleeping. Specifically, perceived toddler sleep problems are associated with shortened maternal sleep duration, which in turn is associated with increased maternal stress, anxiety, and depressive symptoms only for mothers who co-sleep. To examine an alternative model in which maternal mental health symptoms are related to perceived toddlers’ sleep problems, we tested whether maternal sleep duration mediates the relation between maternal mental health symptoms and perceived toddler sleep problems.
METHODS
Sample
All data were collected at baseline from a larger randomized controlled study aimed at obesity prevention. The larger study was powered on the outcomes of child and parent weight status change. Biological mothers of toddlers (age 12–32 mo) were recruited from 2 sites: a suburban Special Supplemental Nutrition Program for Women, Infants, and Children clinic and an urban pediatric clinic. Both sites served low-income families living in the surrounding communities. University and state institutional review boards approved the study. Maternal eligibility criteria included being aged older than 18 years, not currently pregnant and having no health problems that would interfere with physical activity. Toddler eligibility criteria included born at term with birth weight >2500 g and no known congenital problems or disabilities. All mothers provided written informed consent. Mothers completed self-administered, computer-based questionnaires using voice-generating software and mouse responses. A total of 304 eligible mothers of toddlers were recruited, and 281 mothers completed the full evaluation.
Demographics
Mothers reported their toddler’s age, sex, and race/ethnicity and their own age, marital status, and household income level. Income was used to calculate a poverty ratio based on 2009 thresholds determined by the US Census Bureau.35 Based on income and family size, families were classified as either being above or below the poverty threshold as defined by the 2009 US Census Bureau.
Depressive Symptoms
Depressive symptoms were assessed using the Beck Depression Inventory-II (BDI-II).36 The BDI is a well-validated 21-item self-report scale that assesses mood and associated symptoms of depression over the past 2 weeks. Scores of 0 to 13 indicate minimal depressive symptoms, scores from 14 to 19 indicate mild depression, scores of 20 to 28 indicate moderate depression, and scores above 28 indicate severe depression. The reliability of the measure in this study was high (α = 0.88).
Anxiety Symptoms
Anxiety symptoms were assessed using the 6-item State-Trait Anxiety Inventory (STAI).37 The STAI38 uses a 4-level scale (1 = not at all and 4 = very much) adjusted to yield a similar range of scores to those obtained with the full 20-item version. Validity has been established,37 and internal consistency in the current sample was adequate (α = 0.80).
Perceived Stress
The Perceived Stress Scale (PSS) is a 10-item measure used to assess global, everyday stress experienced in the past week. Responses were rated on a 5-point Likert scale and higher scores indicated greater stress. The PSS possesses adequate psychometric qualities.39,40 Reliability in the current study was adequate (α = 0.63).
Maternal Sleep
The Pittsburgh Sleep Quality Index is a well-validated and widely used sleep measure.41 Mothers were asked to assess their sleep duration (how many hours of actual sleep per night averaged over the past month). Comparable 1-item measures of sleep duration have been used in similar studies,42 in line with recommendations for field trials from the Diagnostic and Statistical Manual of Mental Disorders-5 Sleep-Wake Disorders Workgroup.43
Maternal Perception of Toddler Sleep Problem
A single item from the Brief Infant Sleep Questionnaire (BISQ)44 was used to assess maternal perception of toddlers’ sleep problems. The BISQ has been validated with children from 5 to 30 months with high (>0.82) test-retest reliability.44 Mothers completed this questionnaire based on their child’s sleep over the past week. Mothers reported on whether they thought their toddler experienced “sleep problems” (“not a problem at all,” “a small problem,” or “a very serious problem”). The categories of “a small problem” and “a very serious problem” were collapsed, and responses were dichotomized between “a very serious problem/a small problem” and “not at all a problem.” Maternal perception of toddler sleep problems was used in this study to define toddler sleep problems. Mothers additionally reported on their sleeping arrangement. Answers were dichotomized between mother-toddler bed/room sharing and toddler sleeping in a separate room.
Data Analysis
Data were analyzed using IBM SPSS 22 Statistics Developer Version 22. Bivariate Pearson correlations were conducted to examine relations among the variables of interest (i.e., maternal depressive symptoms, anxiety, and perceived stress) and demographic variables. Categorical variables (marital status, poverty level, sleep arrangement, and toddler sleep problem) were dummy coded (see footnote in Table 2). Point biserial correlations were conducted as necessary. Independent t tests were conducted to examine whether males and females differed on key study variables. Demographic variables that were significantly related to any of the dependent variables were controlled for as covariates in the subsequent mediation models.
Table 2.
Correlations Between Key Study Variables and Key Demographic Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Co-sleepinga | — | ||||||||
| 2. Toddler sleep problemb | 0.116 | — | |||||||
| 3. Maternal depressive symptoms | −0.056 | 0.110 | — | ||||||
| 4. Maternal sleep duration | 0.069 | −0.126* | −0.225** | — | |||||
| 5. Maternal anxiety symptoms | −0.003 | 0.087 | 0.443** | −0.175** | — | ||||
| 6. Parenting stress | 0.101 | 0.096 | 0.540** | −0.218** | 0.413** | — | |||
| 7. At/below poverty linec | 0.268** | −0.025 | 0.068 | 0.057 | −0.035 | 0.068 | |||
| 8. Maternal age | −0.156** | 0.050 | −0.009 | −0.251** | −0.034 | −0.062 | −0.164** | ||
| 9. Marital statusd | −0.301** | 0.021 | −0.039 | −0.069 | −0.016 | −0.085 | −0.401** | 0.312** | |
| Mean (SD) or % | 39.6% | 83.9% | 7.8 (7.5) | 6.73 (1.6) | 10.1 (3.6) | 5.5 (3.2) | 69.3% | 27.11 (6.2) | 73.2% |
Dummy coded in reference to toddler in their separate room from parents (39.6% of toddlers in a separate room).
Dummy coded in reference to [sleep is] “not a problem” (83.9% did not have a sleep problem).
Dummy coded in reference to living at or below the poverty line (69.3% of families were at or below the poverty line).
Coded in reference to not married (73.2% mothers not married).
p < 0.05,
p < 0.01. SD, standard deviation.
To test for conditional indirect effects, 3 separate moderated mediation analyses were conducted, each predicting 1 of the mental health variables (e.g., maternal depressive symptoms, anxiety, and perceived stress). Moderated mediation analyses were conducted using the SPSS macro PROCESS45 (Model 7). PROCESS is an ordinary least squares regression-based path analytic tool for SPSS used for observed variable mediation, moderation, and moderated mediation (also known as conditional process modeling).
Last, to examine the possibility of alternative models, bootstrapped mediation models were conducted using PROCESS to examine the indirect effect of maternal sleep duration on the association between maternal mental health symptoms and perceived toddler sleep problems. Three separate mediation models were conducted, with perceived toddler sleep problems as the dependent variable and mental health variables as the independent variables (e.g., maternal depressive symptoms, anxiety, and perceived stress).
All mediation models were conducted using bootstrapping. Bootstrapping is a statistical method that involves drawing repeated samples from the data with replacement to gain multiple estimates of the indirect effect.45 Using this method, we generated 5000 bootstrapped samples. Advantages to using this statistical approach to test mediation over Baron and Kenny’s approach46 are that it does not assume normality for the indirect effects, multiple mediators and moderators can be tested simultaneously, and Type II errors are reduced because fewer inferential tests are required.45 Bootstrapping bases significant results on finding that the 95% confidence interval does not contain 0.
RESULTS
Description
The final sample included 280 mothers, 67.9% identified as African American, 26.8% as white, and 5.3% as “other.” Toddlers were a mean age of 20.2 months (SD = 5.6), and 54% were male. Mothers slept an average of 6.73 hours per night (SD = 1.6) (Table 1). Mothers of toddlers with perceived sleep problems slept significantly less (M = 6.27, SD = 1.60) compared with mothers of toddlers without sleep problems (M = 6.82, SD = 1.68; t(278) = 2.12, p < 0.05).
Table 1.
Sample Demographics, n = 280
| Mean/% | SD | Range | |
|---|---|---|---|
| Toddler age, mo | 20.2 | 5.6 | 12–32 |
| Toddler sex (male) | 53.9% | ||
| Mother age, yr | 27.1 | 6.2 | 18–46 |
| Living at or below poverty line | 69.3% | ||
| Race/ethnicity | |||
| African American | 67.9% | ||
| White | 26.8% | ||
| Other | 5.3% | ||
| Marital status | |||
| Married | 26.8% | ||
| Not married | 73.2% | ||
| Co-sleeping | 60.4% | ||
| Maternal anxiety symptomsa | 10.1 | 3.6 | 6–21 |
| Maternal depressive symptomsb | 7.8 | 7.5 | 0–59 |
| Parenting stressc,d | 5.5 | 3.1 | 0–16 |
| Maternal sleep, hr | 6.73 | 1.6 | 2–12 |
| Perceived toddler sleep problem | 16% |
State-Trait Anxiety Inventory.
Beck Depression Inventory.
The Perceived Stress Scale.
n = 279. SD, standard deviation.
Preliminary Analyses
No toddler sex differences were found on any study variables of interest (p > 0.05). Correlational analyses between demographic variables (maternal age, marital status, and poverty level) are presented in Table 2. Poverty, maternal age, and marital status were significantly related to at least 1 mental health variable and were controlled for in subsequent models.
Conditional Indirect Effects
The interaction between perceived toddler sleep problems and co-sleeping was significantly related to maternal sleep duration (Fig. 1). Consistent with the first hypothesis, perceived toddler sleep problems were significantly related to short maternal sleep only among co-sleeping mothers (B = −0.85, standard error [SE] = 0.30, p < 0.01), with no relation between perceived toddler sleep problems and maternal sleep duration for non–co-sleeping mothers (B = 0.28, SE = 0.48, p = 0.56) (Fig. 2). The model accounted for nearly 10% of the variation in maternal sleep duration (R2 = 0.10).
Figure 1.
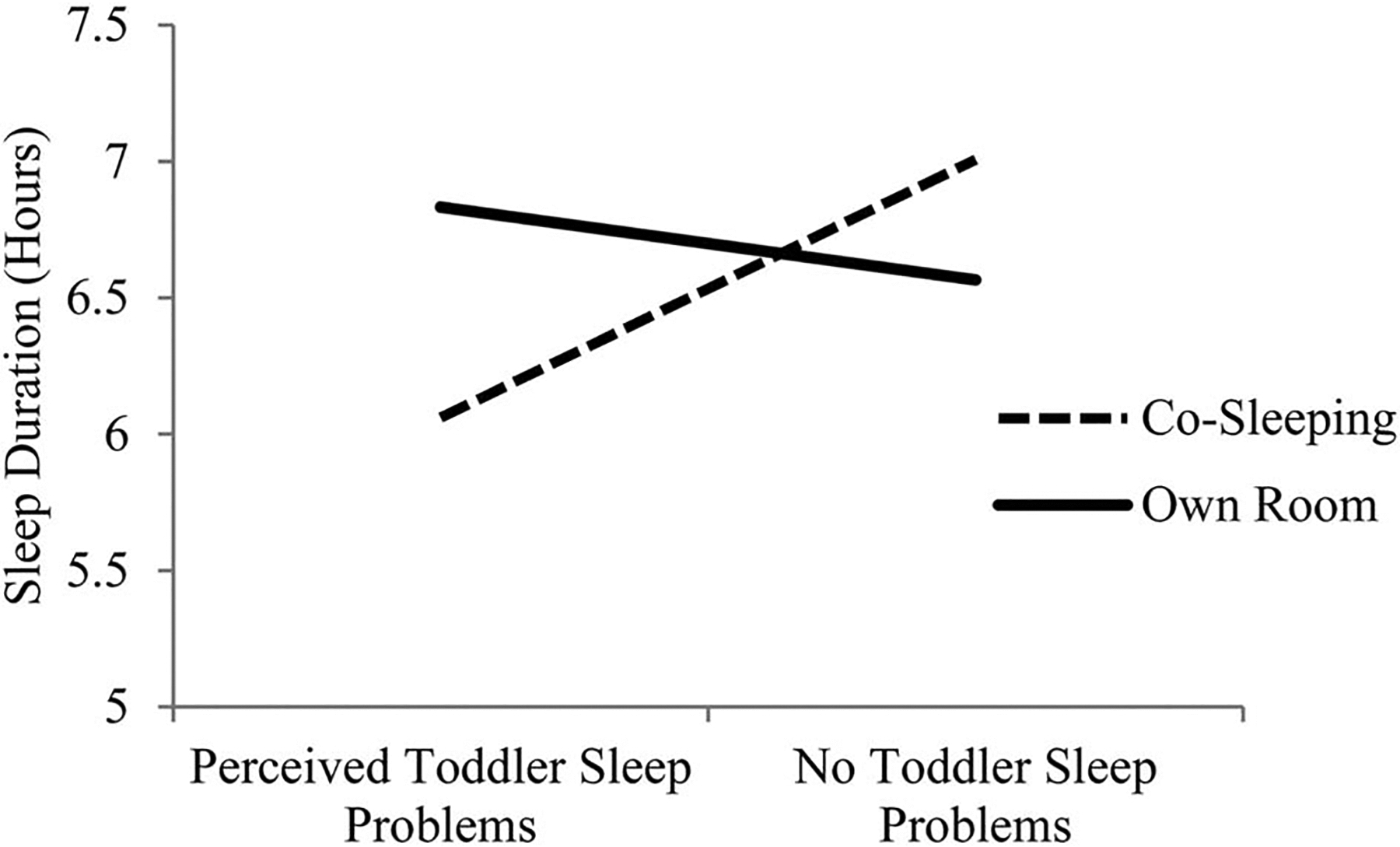
Co-sleeping moderates the relation between perceived toddler sleep problems and maternal sleep duration.
Figure 2.
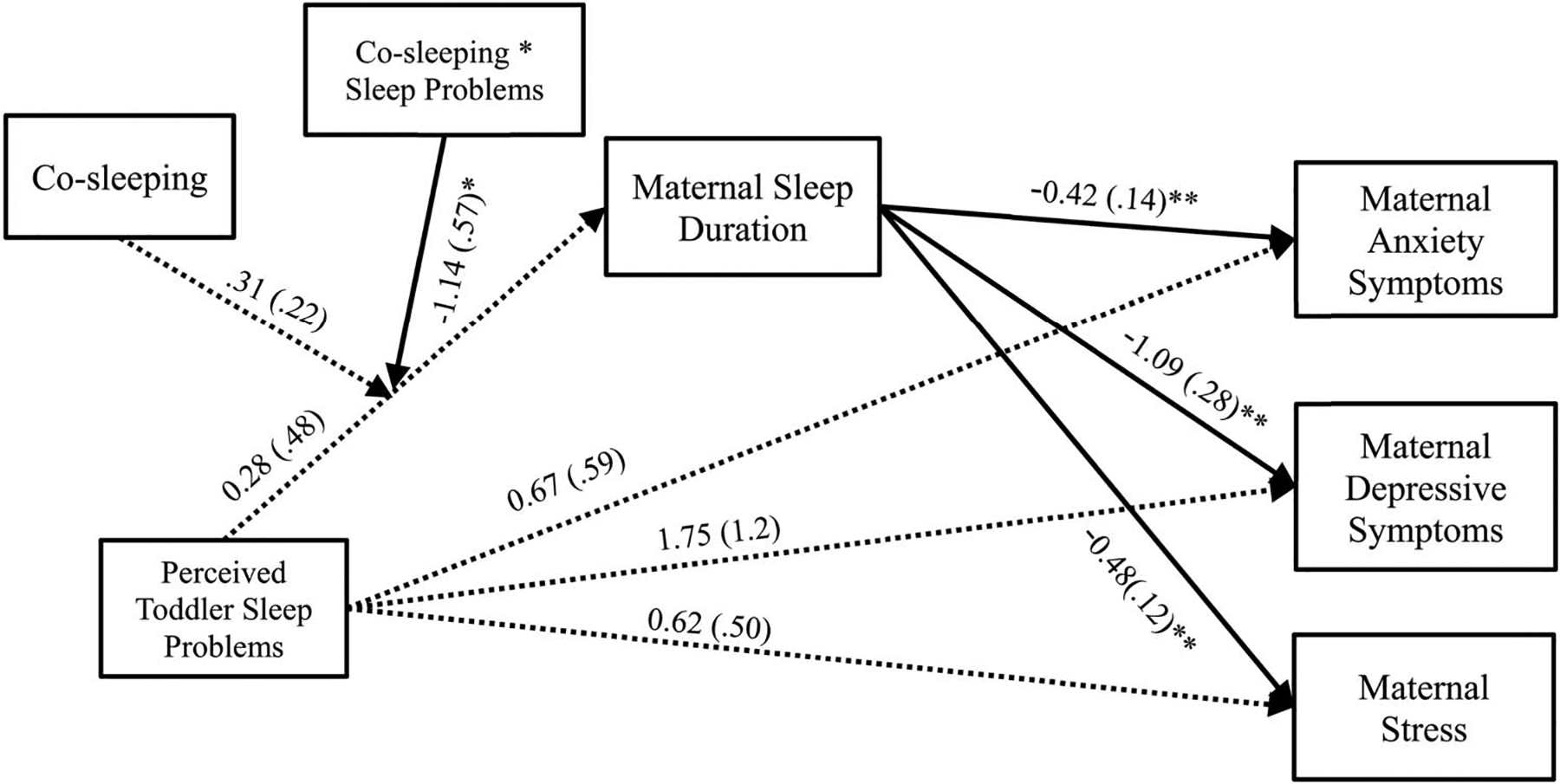
Conditional indirect effects of maternal sleep duration on the relationship between perceived toddler sleep problems and maternal mental health. Unstandardized B weights and SEs are presented along each path. *p = 0.05; **p < 0.01. Nonsignificant paths noted by the dotted line.
Next, we examined the conditional indirect effects of perceived toddler sleep problems on maternal mental health symptoms through maternal sleep duration was based on co-sleeping arrangement. Specific path estimates are presented in Figure 2. Maternal sleep duration significantly mediated relations between perceived toddler sleep problems and maternal depressive symptoms, anxiety symptoms, and stress. Specifically, perceived toddler sleep problems were related to short maternal sleep duration, which was in turn related to increased depressive symptoms, anxiety symptoms, and stress. These associations were moderated by co-sleeping, such that short maternal sleep mediated the relationship between perceived toddler sleep problems and mental health symptoms only among co-sleeping mothers (Table 3). The final models accounted for 7% of the variation in depressive symptoms (R2 = 0.07), 4% of the variation in anxiety symptoms (R2 = 0.04), and 7% of the variation in stress (R2 = 0.07).
Table 3.
Conditional Indirect Effects of Perceived Toddler Sleep Problems on Maternal Mental Health Based on Sleep Arrangement
| Dependent Variable | Toddler Separate Room | Toddler Parents’ Room | Index of Moderated Mediation | |||
|---|---|---|---|---|---|---|
| Estimate | Bootstrapped CI | Estimate | Bootstrapped CI | Index | Bootstrapped CI | |
| Depression | −0.3060 | −1.264 to 0.5363 | 0.9228a | 0.1963–1.9836 | 1.2347a | 0.1086–2.8259 |
| Anxiety | −0.1175 | −0.5448 to 0.1794 | 0.3568a | 0.0759–0.8350 | 0.4744a | 0.0657–1.1858 |
| Stress | −0.1502 | −0.6243 to 0.1767 | 0.4046a | 0.0874–0.8991 | 0.5548a | 0.0775–1.2854 |
Significance is based on the bootstrapped confidence interval (CI) not containing contain 0.
The index of moderated mediation showed that the indirect effects differed significantly for parents who reported co-sleeping (Table 3), supporting the second hypothesis of moderated mediation (conditional indirect effects).45
Alternative Models
To investigate the possibility of alternative models, we estimated 3 indirect effects models, each with perceived toddler sleep problems as the dependent variable. The indirect effects from maternal depressive symptoms (estimate = 0.0089, 95% confidence interval [CI]: −0.0029 to 0.0260), anxiety (estimate = 0.0158, 95% CI: −0.0022 to 0.0449), or stress (estimate = 0.0211, 95% CI: −0.0091 to 0.0606) through maternal sleep duration were not significantly different from 0.
DISCUSSION
This study found that maternal perception of toddler sleep problems is related to maternal mental health symptoms, mediated through maternal sleep duration. This relation holds only when co-sleeping, which appears to strengthen the negative association between perceived toddler sleep problems and maternal sleep duration. In the absence of maternal perceptions of toddler sleep problems, there were no significant differences in maternal sleep duration based on sleeping arrangement. Extrapolating from the results, believing that a toddler has a sleep problem is associated with an average of 51 minutes less sleep when mothers reported co-sleeping. Specifically, co-sleeping mothers of toddlers with perceived sleep problems slept an average of about 6 hours per night, which is less than the National Sleep Foundation recommended 7 to 9 hours of sleep per night.47 A decrease of nearly an hour of sleep for mothers is likely meaningful given that even limited sleep restriction has been associated with decreased functioning in adults, and studies that have restricted sleep to 6 hours have found significant impairments across cognitive and mood domains.48 However, regardless of sleeping arrangements or perceptions of toddler sleep problems, mothers in this study reported sleeping an average of less than 7 hours per night, which may warrant attention in correspondence with other clinical conditions.
Findings linking maternal mental health with child sleep problems are consistent with previous literature across all developmental ages.5–7,9,10,29 This study extends previous findings by demonstrating this association among low-income toddlers and identifying a potential mechanism. This association is concerning given that maternal mental health can affect parenting and ultimately the health and well-being of children.29 For example, maternal depressive symptoms have been associated with child health problems,11,32 low cognitive performance,49 behavior problems, and psychopathology.50 Toddlers in low-income families are especially vulnerable to negative outcomes associated with their mother’s psychological well-being and functioning, compared with high-income families.1
The finding that perceived toddler sleep problems were associated with an average loss of 51 minutes of maternal sleep28 contingent on co-sleeping is also consistent with previous literature.9,11 It is intuitive that mothers who co-sleep may be more likely to notice their toddler’s awakenings and feel as if they need to intervene to help them return to sleep. When mothers are in close proximity to their toddler, even the smallest movements may disrupt maternal sleep.15 The current study suggests that a mother’s sleep is likely to be disturbed if she perceives her toddler to have a sleep problem and if she is sharing a room or bed with her toddler.
This study fills a gap in the literature by providing evidence for a conceptual model by which parent and child sleep are related to parental mental health among low-income families. Sleep is essential for cognitive and emotional daytime functioning, in addition to broader family functioning.29 Co-sleeping may be a vulnerability factor for mothers in that it is related to increased mental health symptoms in the presence of adversity (i.e., perceived toddler sleep problems). However, co-sleeping is potentially a modifiable behavior and thus a possible point of intervention. Future research should aim to examine whether avoiding co-sleeping when toddlers have perceived sleep problems improves maternal sleep and subsequently mental health. In addition, future research should examine whether other behavioral sleep interventions may be effective in improving maternal sleep if co-sleeping continues to occur. For example, such interventions may include developing a short, pleasurable bedtime routine to assist toddlers with sleep initiation and sleep reinitiation in response to normal nighttime awakenings. Additional behavioral principles such as stimulus control, shaping, and planned ignoring may be used in treatment with families to address sleep-onset associations and night awakenings.51
Results of this study should be interpreted in the context of its limitations. Perceived toddler sleep problems were assessed using a 1-item measure of the mother’s perception of sleep problems, not by an objective measure or a clinical diagnosis.13,52 Similar single-item self-report measures have been used in previous studies to identify sleep problems in infants and toddlers and are associated with frequent night awakenings.4,33,53–57 Perceptions of sleep disruptions have been shown to be stronger predictors of mood disturbances among mothers of young children compared with objective sleep quality or quantity.58 In addition, poor maternal sleep quality has been associated with increased reporting of child sleep problems.59 Future research should examine both objective and subjective sleep quality in mothers and toddlers and further explore how maternal sleep quality relates to the reporting of toddler sleep problems.29,59
The limitations of analyses of mediation, moderation, and their integration are linked inextricably to the research design underlying these analytical techniques.60 The cross-sectional nature of the data may inflate estimations of mediation and precludes conclusions of directionality.1,61 Alternative model paths may exist. For example, maternal psychological factors have been linked to decreased maternal sleep, which in turn might increase the likelihood of perceiving that a toddler has sleep difficulties. However, this study did not find evidence for this model. Therefore, reversing the independent and dependent variables cannot fully explain the observed indirect effects, and our study provides tentative evidence for the suggested conceptual model. Future work should seek to replicate these results using longitudinal data and more complex path analytic models (such as those examining co-sleeping and subsequent toddler sleep) to fully explore potential directional and bidirectional relations among these constructs.42
In addition, this study did not assess if co-sleeping was continuous throughout the night. Toddlers may be put to bed in a separate room but move to the parent’s bed/room during the night.16 Future studies should examine the effects of consistency and/or duration of co-sleeping among toddlers with sleep problems.26
There are several important clinical implications for these findings. Pediatricians are particularly poised to identify problems related to sleep in young children or normalize parental perceptions of sleep problems. Although the American Academy of Pediatrics recommends annual sleep screening, only a fraction of children seen for well-care visits are appropriately screened for sleep problems.62,63 Given that many sleep problems are behavioral in nature, and that behavior interventions have shown to be effective,64 this is an area of unmet treatment opportunity. Interventions to address child sleep problems may result not only in improved sleep for toddlers but also improved sleep and well-being for mothers.29 For example, in a study conducted among mothers of infants with sleep problems, postbehavioral intervention, the mothers experienced decreased depressive symptoms.65 Providers may consider maternal sleep and mental health as they relate to toddler sleep and sleep problems.59 Maternal mental health and well-being affect parenting,29 and maternal sleep duration may be a mechanism by which to intervene. Although co-sleeping may be an economic necessity for low-income families, providers should be aware of the potential negative impacts and advise accordingly when discussing the decision to co-sleep.
Acknowledgments
Supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), R01HD056099 [to M.M. Black].
Footnotes
Disclosure: The authors declare no conflict of interest.
Clinical Trials Registration: NCT02615158.
REFERENCES
- 1.Bernier A, Bélanger MÈ, Bordeleau S, et al. Mothers, fathers, and toddlers: parental psychosocial functioning as a context for young children’s sleep. Dev Psychol. 2013;49:1375–1384. [DOI] [PubMed] [Google Scholar]
- 2.Mindell JA, Leichman ES, Composto J, et al. Development of infant and toddler sleep patterns: real-world data from a mobile application. J Sleep Res. 2016;25:508–516. [DOI] [PubMed] [Google Scholar]
- 3.Hayes MJ, McCoy SK, Fukumizu M, et al. Temperament and sleep–wake behaviour from infancy to toddlerhood. Infant Child Dev. 2011;20:495–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mindell JA, Telofski LS, Wiegand B, et al. A nightly bedtime routine: impact on sleep in young children and maternal mood. Sleep. 2009; 32:599–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Germo GR, Chang ES, Keller MA, et al. Child sleep arrangements and family life: perspectives from mothers and fathers. Infant Child Dev. 2007;16:433–456. [Google Scholar]
- 6.Giallo R, Rose N, Vittorino R. Fatigue, wellbeing and parenting in mothers of infants and toddlers with sleep problems. J Reprod Infant Psychol. 2011;29:236–249. [Google Scholar]
- 7.Petzoldt J, Wittchen HU, Einsle F, et al. Maternal anxiety versus depressive disorders: specific relations to infants’ crying, feeding and sleeping problems. Child Care Health Dev. 2016;42:231–245. [DOI] [PubMed] [Google Scholar]
- 8.Sadeh A, Mindell JA, Owens J. Why care about sleep of infants and their parents? Sleep Med Rev. 2011;15:335–337. [DOI] [PubMed] [Google Scholar]
- 9.Bayer JK, Hiscock H, Hampton A, et al. Sleep problems in young infants and maternal mental and physical health. J Pediatr Child Health. 2007;43:66–73. [DOI] [PubMed] [Google Scholar]
- 10.Cortesi F, Giannotti F, Sebastiani T, et al. Cosleeping versus solitary sleeping in children with bedtime problems: child emotional problems and parental distress. Behav Sleep Med. 2008;6:89–105. [DOI] [PubMed] [Google Scholar]
- 11.Countermine MS, Teti DM. Sleep arrangements and maternal adaptation in infancy. Infant Ment Health J. 2010;31:647–663. [DOI] [PubMed] [Google Scholar]
- 12.Mindell JA, Sadeh A, Kohyama J, et al. Parental behaviors and sleep outcomes in infants and toddlers: a cross-cultural comparison. Sleep Med. 2010;11:393–399. [DOI] [PubMed] [Google Scholar]
- 13.Ramos KD, Youngclarke D, Anderson JE. Parental perceptions of sleep problems among co-sleeping and solitary sleeping children. Infant Child Dev. 2007;16:417–431. [Google Scholar]
- 14.Teti DM, Shimizu M, Crosby B, et al. Sleep arrangements, parent–infant sleep during the first year, and family functioning. Dev Psychol. 2016;52:1169–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldberg WA, Keller MA. Co-sleeping during infancy and early childhood: key findings and future directions. Infant Child Dev. 2007;16:457–469. [Google Scholar]
- 16.Li S, Jin X, Yan C, et al. Bed-and room-sharing in Chinese school-aged children: prevalence and association with sleep behaviors. Sleep Med. 2009;9:555–563. [DOI] [PubMed] [Google Scholar]
- 17.Volkovich E, Ben-Zion H, Karny D, et al. Sleep patterns of co-sleeping and solitary sleeping infants and mothers: a longitudinal study. Sleep Med. 2015;16:1305–1312. [DOI] [PubMed] [Google Scholar]
- 18.American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome. The changing concept of sudden infant death syndrome: diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk. Pediatrics. 2005;116:1245–1255. [DOI] [PubMed] [Google Scholar]
- 19.American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome. SIDS and other sleep-related infant deaths: updated 2016 recommendations for a safe infant sleeping environment. Pediatrics. 2016;138:e20162938. [DOI] [PubMed] [Google Scholar]
- 20.Barajas RG, Martin A, Brooks-Gunn J, et al. Mother-child bed-sharing in toddlerhood and cognitive and behavioral outcomes. Pediatrics. 2011;128:e339–e347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Teti DM, Crosby B, McDaniel BT, et al. Marital and emotional adjustment in mothers and infant sleep arrangements during the first six months. Monogr Soc Res Child Dev. 2015;80:160–176. [DOI] [PubMed] [Google Scholar]
- 22.Colson ER, Willinger M, Rybin D, et al. Trends and factors associated with infant bed sharing, 1993–2010: the national infant sleep position study. JAMA Pediatr. 2013;167:1032–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mykyta L, Macartney S. The Effects of Recession on Household Composition: “Doubling up” and Economic Well-being (SEHSD Working Paper No. 2011–4). Washington, DC: U.S. Census Bureau; 2010. [Google Scholar]
- 24.Glenn LL, Quillin SI. Opposing effects of maternal and paternal socioeconomic status on neonatal feeding method, place of sleep, and maternal sleep time. J Perinat Neonatal Nurs. 2007;21:165–172. [DOI] [PubMed] [Google Scholar]
- 25.Milan S, Snow S, Belay S. The context of preschool children’s sleep: racial/ethnic differences in sleep locations, routines, and concerns. J Fam Psychol. 2007;21:20. [DOI] [PubMed] [Google Scholar]
- 26.Ward TCS, Robb SW, Kanu FA. Prevalence and characteristics of bed-sharing among black and white infants in Georgia. Matern Child Health J. 2016;20:347–362. [DOI] [PubMed] [Google Scholar]
- 27.Jackson CL, Redline S, Emmons KM. Sleep as a potential fundamental contributor to disparities in cardiovascular health. Annu Rev Public Health. 2015;36:417–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boergers J, Hart C, Owens JA, et al. Child sleep disorders: associations with parental sleep duration and daytime sleepiness. J Fam Psychol. 2007;21:88. [DOI] [PubMed] [Google Scholar]
- 29.Meltzer LJ, Mindell JA. Relationship between child sleep disturbances and maternal sleep, mood, and parenting stress: a pilot study. J Fam Psychol. 2007;21:67. [DOI] [PubMed] [Google Scholar]
- 30.Caldwell BA, Redeker NS. Maternal stress and psychological status and sleep in minority preschool children. Public Health Nurs. 2015;32:101–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep Med Rev. 2010;14:89–96. [DOI] [PubMed] [Google Scholar]
- 32.Gress-Smith JL, Luecken LJ, Lemery-Chalfant K, et al. Postpartum depression prevalence and impact on infant health, weight, and sleep in low-income and ethnic minority women and infants. Matern Child Health. 2012;16:887–893. [DOI] [PubMed] [Google Scholar]
- 33.Mindell JA, Sadeh A, Wiegand B, et al. Cross-cultural differences in infant and toddler sleep. Sleep Med. 2010;11:274–280. [DOI] [PubMed] [Google Scholar]
- 34.Simard V, Nielsen TA, Tremblay RE, et al. Longitudinal study of preschool sleep disturbance: the predictive role of maladaptive parental behaviors, early sleep problems, and child/mother psychological factors. Arch Pediatr Adolesc Med. 2008;162:360–367. [DOI] [PubMed] [Google Scholar]
- 35.US Census Bureau. Poverty Thresholds. 2009. Available at https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html. Accessed August 25, 2017.
- 36.Beck AT, Steer RA, Carbin MG. Psychometric properties of the beck depression inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 37.Marteau TM, Bekker H. The development of a six-item short-form of the state scale of the spielberger state—trait anxiety inventory (STAI). Br J Clin Psychol. 1992;31:301–306. [DOI] [PubMed] [Google Scholar]
- 38.Spielberger CD, Gorsuch RL, Lushene RE, et al. Manual for the State-trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 39.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Social Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 40.Lee SY, Hsu HC. Stress and health-related well-being among mothers with a low birth weight infant: the role of sleep. Soc Sci Med. 2012;74:958–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buysse DJ, Reynolds CF, Monk TH, et al. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. [DOI] [PubMed] [Google Scholar]
- 42.Saxbe DE, Schetter CD, Guardino CM, et al. Sleep quality predicts persistence of parental postpartum depressive symptoms and transmission of depressive symptoms from mothers to fathers. Ann Behav Med. 2016;50:862–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Reynolds CF III, Redline S. The DSM-V sleep-wake disorders nosology: an update and an invitation to the sleep community. Sleep. 2010;33:10–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sadeh A A brief screening questionnaire for infant sleep problems: validation and findings for an internet sample. Pediatrics. 2004; 113:e570–e577. [DOI] [PubMed] [Google Scholar]
- 45.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Press; 2013. [Google Scholar]
- 46.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Personal Social Psychol. 1986;51:1173–1182. [DOI] [PubMed] [Google Scholar]
- 47.Hirshkowitz M, Whiton K, Albert SM, et al. National sleep foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1:40–43. [DOI] [PubMed] [Google Scholar]
- 48.Short MA, Banks S. The functional impact of sleep deprivation, sleep restriction, and sleep fragmentation. In: Bianchi M, ed. Sleep Deprivation and Disease. New York, NY: Springer; 2014:13–26. [Google Scholar]
- 49.Smith-Nielsen J, Tharner A, Krogh MT, et al. Effects of maternal postpartum depression in a well-resourced sample: early concurrent and long-term effects on infant cognitive, language, and motor development. Scand J Psychol. 2016;57:571–583. [DOI] [PubMed] [Google Scholar]
- 50.Prenoveau JM, Craske MG, West V, et al. Maternal postnatal depression and anxiety and their association with child emotional negativity and behavior problems at two years. Dev Psychol. 2017; 53:50–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Meltzer LJ, Crabtree VM. Pediatric Sleep Problems: A Clinician’s Guide to Behavioral Interventions. Washington, DC: American Psychological Association; 2015. [Google Scholar]
- 52.Loutzenhiser L, Ahlquist A, Hoffman J. Infant and maternal factors associated with maternal perceptions of infant sleep problems. J Reprod Infant Psychol. 2011;29:460–471. [Google Scholar]
- 53.Mindell JA, Du Mond CE, Sadeh A, et al. Efficacy of an internet-based intervention for infant and toddler sleep disturbances. Sleep. 2011;34:451–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sadeh A, Mindell J, Rivera L. “My child has a sleep problem”: a cross-cultural comparison of parental definitions. Sleep Med. 2010;12:478–482. [DOI] [PubMed] [Google Scholar]
- 55.Sadeh A, Mindell JA, Luedtke K, et al. Sleep and sleep ecology in the first 3 years: a web-based study. J Sleep Res. 2009;18:60–73. [DOI] [PubMed] [Google Scholar]
- 56.Twomey JE. A consideration of maternal developmental needs in the treatment of infant sleep problems. Clin Social Work J. 2016; 44:309–318. [Google Scholar]
- 57.Zambrano DN, Mindell JA, Reyes NR, et al. “It’s not all about my baby’s sleep”: a qualitative study of factors influencing low-income African American mothers’ sleep quality. Behav Sleep Med. 2016;14:489–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bei B, Milgrom J, Ericksen J, et al. Subjective perception of sleep, but not its objective quality, is associated with immediate postpartum mood disturbances in healthy women. Sleep. 2010;33: 531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rönnlund H, Elovainio M, Virtanen I, et al. Poor parental sleep and the reported sleep quality of their children. Pediatrics. 2016;137: e20153425. [DOI] [PubMed] [Google Scholar]
- 60.Karazsia BT, Berlin KS, Armstrong B, et al. Integrating mediation and moderation to advance theory development and testing. J Pediatr Psychol. 2014;39:163–173. [DOI] [PubMed] [Google Scholar]
- 61.Maxwell SE, Cole DA. Bias in cross-sectional analyses of longitudinal mediation. Psychol Methods. 2007;12:23–44. [DOI] [PubMed] [Google Scholar]
- 62.Ersu R, Boran P, Akın Y, et al. Effectiveness of a sleep education program for pediatricians. Pediatr Int. 2016;59:280–285. [DOI] [PubMed] [Google Scholar]
- 63.Meltzer LJ, Plaufcan MR, Thomas JH, et al. Sleep problems and sleep disorders in pediatric primary care: treatment recommendations, persistence, and health care utilization. J Clin Sleep Med. 2014;10:421–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mindell JA, Kuhn B, Lewin DS, et al. Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep. 2006;29:1263–1276. [PubMed] [Google Scholar]
- 65.Hall WA, Moynihan M, Bhagat R, et al. Relationships between parental sleep quality, fatigue, cognitions about infant sleep, and parental depression pre and post-intervention for infant behavioral sleep problems. BMC Pregnancy Childbirth. 2017;17:104. [DOI] [PMC free article] [PubMed] [Google Scholar]


