1. Introduction
Coronavirus disease 2019 (COVID-19) is known to significantly increase the risk of arterial thrombosis (1*). In patients with type I or ST-elevation myocardial infarction (STEMI) who have COVID-19 infection there is data to suggest a poorer in-hospital outcome compared with patients who are COVID negative and suffer from STEMI (with higher thrombus burden, increased incidence of delayed presentation, cardiogenic shock, left ventricular (LV) dysfunction and need for intensive care) [1], [2], [3], [4], [5]. However, there is a paucity of comparative long-term outcome data in this cohort of patients. Here we examine the characteristics and long terms outcomes of a cohort of COVID positive STEMI patients treated with primary percutaneous coronary intervention (PCI) comparing long-term outcomes with a COVID negative group from the first and second waves of the pandemic.
2. Methods
This was a single-centre retrospective observational study of 566 patients with confirmed STEMI admitted to Barts Heart Centre, London, UK between 01/03/2020 and 01/03/2021. The study was designed to assess the incidence of COVID-19 amongst patients admitted with STEMI and to compare their baseline characteristics, angiographic, procedural and clinical outcomes to STEMI patients who were COVID-negative. Individuals included in the analysis were admitted through the emergent activation pathway for primary PCI. Patients were included if they were admitted to Barts Heart Centre via London Ambulance Service either directly from home or via partner district hospitals with cardiac chest pain and STEMI (ST elevation in 2 or more contiguous leads ≥0.2 mV) on their ECG or patients admitted with an out of hospital cardiac arrest (OOHCA) and ECG meeting diagnostic criteria for STEMI on return of spontaneous circulation. Patients with OOHCA that did not achieve ROSC and those with non-STEMI were excluded from the study. All of these patients underwent primary PCI for a culprit coronary occlusion.
All patients with STEMI underwent nasal/throat swab for SARS-CoV-2 using real time-polymerase chain reaction, blood samples and chest imaging using chest X-ray. COVID-19 diagnosis was based on either identification of SARS-CoV-2 on nasal/throat swab or positive serology or symptoms and chest imaging consistent with COVID-19. Demographic, procedural and outcome data were collected as part of a national cardiac audit, all patient-identifiable fields being removed; therefore, formal ethical approval was not required. A panel of three interventional cardiologists, blinded to patient COVID-19 status, retrospectively reviewed cine-angiographic images of all patients and scored pre- and post-PCI TIMI flow in the infarct-related artery, thrombus burden pre- and post-PCI (modified thrombus grade for Grade 5 thrombus post initial balloon inflation) (9*). The primary clinical outcome of all-cause mortality was measured at a median of 350 days (IQR 257-577). All patients were followed up on clinical pathways with electronic capture of data and outcomes.
Descriptive statistical analyses were performed using SPSS Statistics version 25.0 (IBM, New York). A 2-sided p-value <0.05 defined statistical significance. Variables are expressed as counts (percentages), mean ± standard deviation (SD), and median [lower quartile-upper quartile] as appropriate. Chi-squared analysis or Fisher's-exact test was used to compare categorical data between groups. The independent samples Student t-test or ANOVA test was used to compare normally-distributed continuous data between groups and the Mann-Whitney U test was used to compare the distribution of skewed continuous data between groups.
3. Results
Over a 1-year period between 01/03/2020 and 01/03/2021, 101 consecutive patients with COVID-19 presenting with confirmed STEMI and 465 confirmed STEMI patients without COVID 19 infection were included (Table 1 ). Of patients with COVID-19, 12 had established infection undergoing inpatient treatment at time of presentation whereas the remaining 89 were first diagnosed at the time of STEMI presentation.
Table 1.
Baseline patient characteristics. All values are number (%) unless stated otherwise. BMI = Body Mass Index, MI = myocardial infarction, PCI = percutaneous coronary intervention.
| Non-COVID |
COVID |
p-Value | |
|---|---|---|---|
| n = 365 | n = 101 | ||
| Age (mean ± SD) | 59.2.7 (11.6) | 60.5 (11.8) | 0.824 |
| Male sex | 297 (81.4%) | 84 (83.2%) | 0.658 |
| Black, Asian, Minority Ethnic | 176 (48.2%) | 51 (50.5%) | 0.289 |
| Median BMI (IQR) | 27.44 (24.8–28.5) | 26.9 (25.1–29.7) | 0.598 |
| Past medical history | |||
| Hypertension | 150 (41.1%) | 67 (66.3%) | 0.028⁎ |
| Hypercholesterolemia | 148 (40.5%) | 58 (57.4%) | 0.049⁎ |
| Diabetes mellitus | 112 (30.7%) | 46 (45.5%) | 0.048⁎ |
| Smoking history | 188 (51.5%) | 60 (59.4%) | 0.095 |
| Previous MI | 37 (10.1%) | 13 (12.9%) | 0.278 |
| Previous PCI | 61 (16.7%) | 20 (19.8)% | 0.116 |
| STEMI presentation: | |||
| ECG presentation | 0.815 | ||
| Anterior/LBBB | 216 (59.2%) | 63 (62.3%) | – |
| Inferior | 106 (29.0%) | 31 (30.7%) | – |
| Lateral | 22 (6.0%) | 4 (4.0%) | – |
| Posterior | 21 (5.8%) | 3 (3.0%) | |
| Cardiac arrest | 18 (4.9%) | 11 (10.9%) | 0.369 |
| Cardiogenic shock | 49 (13.4%) | 15 (14.8%) | 0.458 |
| Intubated | 36 (9.9%) | 12 (11.9%) | 0.312 |
| Procedural details | |||
| Coronary intervention | 358 (98.0%) | 98 (97.0%) | 1.000 |
| Culprit vessel | 0.789 | ||
| LMS | 7 (1.9%) | 2 (2.0%) | – |
| LAD | 218 (59.7%) | 61 (60.4%) | – |
| Cx | 27 (7.4%) | 9 (8.9%) | – |
| RCA | 113 (31.0%) | 29 (28.7%) | – |
| Multi-vessel thrombosis | 26 (7.1%) | 16 (15.8%) | 0.041⁎ |
| Stent thrombosis – no. (%) | 8 (2.2%) | 13 (12.9%) | 0.007⁎⁎ |
| Stent type | 0.567 | ||
| Xience | 271 (75.7%) | 73 (74.5%) | |
| Promus | 70 (19.6%) | 20 (20.4%) | |
| Synergy | 17 (4.7%) | 5 (5.1%) | |
| Heparin dose IQR | 10,450 | 9950 | 0.438 |
| Type of P2Y12 | 0.634 | ||
| Ticagrelor | 252 (69.0%) | 72 (71.3%) | |
| Clopdiogrel | 73 (20.0%) | 20 (19.8%) | |
| Prasugrel | 40 (11.0%) | 9 (8.9%) | |
| Baseline TIMI flow 0–1 | 287 (78.6%) | 85 (84.2%) | 0.887 |
| Baseline thrombus grade (4-5) | 281 (77.0%) | 87 (86.1%) | 0.522 |
| Modified thrombus grade (4-5) | 143 (39.2%) | 70 (69.3%) | 0.008⁎⁎ |
| GP IIb/IIIa inhibitor use | 34 (9.3%) | 60 (59.4%) | <0.0001⁎⁎⁎ |
| Aspiration thrombectomy use | 5 (1.4%) | 18 (17.8%) | 0.0021⁎⁎ |
| Procedural success: | |||
| Post PCI TIMI 3 flow | 344 (96.1%) | 91 (92.9)% | 0.687 |
| Median LV ejection fraction (IQR) | 47 (42–51) | 43.8 (33–46) | 0.017⁎ |
P < 0.05.
P < 0.01.
P < 0.0001.
There were no significant differences in age, sex, ethnic background or body mass index (BMI) between the two groups. COVID positive STEMI patients were more likely to be diabetic, hypertensive, and hyperlipidaemic. ECG presentations, rates of cardiogenic shock and requirement for pre-hospital intubation were similar in both groups.
All patients had occluded coronary arteries and culprits for presentation with the majority of patients undergoing PCI in both groups (98% vs 97%, p = 1.0) (Table 1). A small proportion of patinets in each group were managed medically due to late presentation or high thrombus grade (managed pharmacologically). Median door to balloon times were within 60 min and similar for both groups. As previously published, in this larger cohort higher thrombus burdens were seen in patients with COVID-19 as evidenced by higher modified thrombus grades and use of GPII/IIIa inhibitors [1].
Twenty out of 101 COVID positive patients died in-hospital (19.8%), 10 of these were in the 12 patients with established COVID-19 (83.3%) at presentation time, with 11.2% in patients with new diagnoses (Fig. 1a). There was a significantly higher in-hospital mortality observed in COVID positive patients (19.8%) compared with COVID negative patients (4.3%, P < 0.0001).
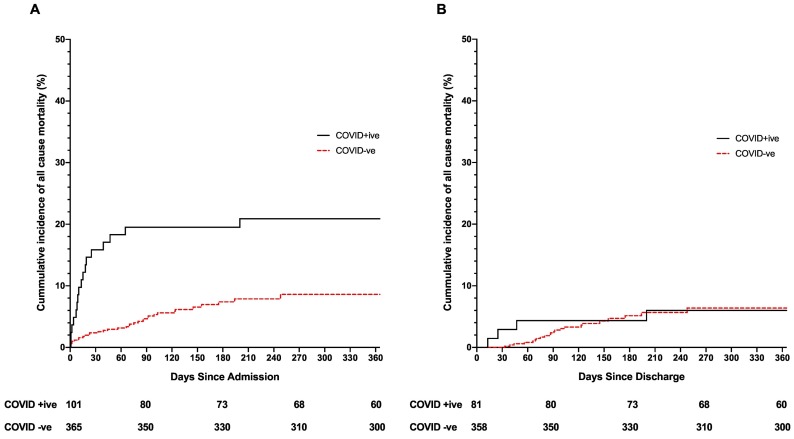
Fig. 1.
K-M Curves detailing mortality post primary PCI for STEMI. Panel A shows all events following admission to hospital for primary PCI for STEMI. Panel B shows events in patients that survived to discharge (so events post discharge only).
Of the 81 COVID positive patients that survived to discharge, a further 5 (6.1%) died during follow-up (Median 360 days IQR 260-680). Kaplan-Meier analysis demonstrates comparable cumulative incidence of all-cause mortality between COVID positive (6.1%) (who survived to discharge) and COVID negative groups (5.9%, P = 0.768) post discharge over the follow-up period (Fig. 1b).
Of the 81 COVID positive patients that were discharged, 56.8% (46/81) were discharged on aspirin and a potent P2Y12 inhibitor (ticagrelor or prasugrel), 24.6% (20/81) were discharged on triple therapy (aspirin, P2Y12 and DOAC) and 18.5% (15/81) were discharged on aspirin and clopidogrel alone. 4/5 deaths in the COVID positive group occurred in patients on aspirin and clopidogrel therapy of which 2 were confirmed and 2 were possible stent thromboses.
4. Discussion
We report for the first-time long-term outcomes in a large single centre COVID positive STEMI cohort. ACS and STEMI occurring in patients with COVID-19 have been shown to be associated with poor outcomes in several series [1], [2], [3], [4], [5] but little data has been shown post discharge. In this study we demonstrate favourable long term mortality rates (5%) in COVID positive STEMI patients who survive to discharge comparable to a COVID negative STEMI cohort.
In-hospital mortality in COVID positive STEMI patients treated with PCI has previously been reported between 18% and 32% [1], [2], [3], [4], [5]. Our own study reported an 18% in-hospital mortality1, with a 23% in-hospital mortality rate reported in the Spanish COVID positive STEMI cohort2. In the international COVID-ACS registry that enrolled 144 COVID positive STEMI patients, mortality was found to be 22.9% related to increased incidence of cardiogenic shock and late presentation in this cohort3. The North American COVID-19 STEMI registry enrolled 594 STEMI patients at 64 sites: 171 of whom were confirmed COVID-19 positive. Similarly, the in-hospital mortality was found to be 33% in the COVID-STEMI cohort with higher rates of cardiogenic shock, with longer hospital stays [4]. Together the findings of these registries highlight the poor outcomes associated with the presence of COVID-19 infection in patients with ACS, whether related to respiratory complications, greater thrombotic complications or thrombus burden. In this study we show that long term outcomes in COVID positive STEMI patients surviving to discharge are similar to COVID negative STEMI patients. The adverse events in this high-risk cohort appear to occur during the in-hospital stay associated with reduced ejection fraction and increased thrombus burden with no signal towards increased events post-discharge out to 18 months.
While there is no data for increased stent thrombosis in long term follow-up in COVID positive STEMI there is however increased stent thrombosis observed in acute STEMI patients presenting with con-current COVID-19 infection. This study, describes a higher thrombus burden, multivessel thrombus and in-stent thrombosis amongst COVID-19 STEMI patients, a finding that is replicated in other series and case reports [1], [2], [6], [7], [8], [9]. The mechanism of acute stent thrombosis is still uncertain, and although we speculate regarding longer term thrombosis signals this does not appear to be the case based on comparable outcomes between the groups.
Limitations: This is a retrospective observational study in a single centre and therefore has all the limitations of this type of analysis including bias and the potential for confounding. Furthermore, as has been universally accepted, the sensitivity of diagnostic testing for SARS-CoV-2 is modest at approximately 60–70% with nasal/pharyngeal swab 5. In addition, another limitation to this study is that there was a large heterogeneity in the discharge medications, which could have an impact on the outcome.
Further study and longer follow up is needed to fully understand the long-term effects of COVID-19 infection in this cohort. Furthermore, the study population was unvaccinated, it would be interesting to compare to a population going forward of the population in the third wave of COVID-19 who in the UK would have high rates of vaccination.
5. Conclusion
In this study we demonstrate favourable long term mortality rates (5% at 12 months) in COVID positive STEMI patients who survive to discharge, comparable to a COVID negative STEMI cohort. This suggests no long-term adverse effect of COVID-19 in this patient cohort although further study and longer follow up is needed.
Funding
No funding was used for this study.
Data availability statement
The data underlying this article will be shared on reasonable request to the corresponding author.
Declaration of competing interest
All authors: No conflicts of interest, nothing to disclose.
References
- 1.Choudry F.A., Hamshere S.M., Rathod K.S., Akhtar M.M., Archbold R.A., Guttmann O.P., et al. High thrombus burden in patients with COVID- 19 presenting with ST-elevation myocardial infarction. J Am Coll Cardiol. 2020;76:1168–1176. doi: 10.1016/j.jacc.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodriguez-Lior O., Alvarez ABC., Pérez de Prado A., Rossello X., Ojeda S., Serrador A., et al. In-hospital outcomes of COVID-19 ST-elevation myocardial infarction patients. EuroIntervention. 2021;16:1426–1433. doi: 10.4244/EIJ-D-20-00935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kite T.A., Ludman P.F., Gale C.P., Wu J., Caixeta A., Mansourati J. International prospective registry of acute coronary syndromes in patients with COVID-19. J Am Coll Cardiol. 2021 May doi: 10.1016/j.jacc.2021.03.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garcia S., Dehghani P., Grines C., Davidson L., Nayak K.R., Saw J. Initial findings from the North American COVID-19 Myocardial Infarction Registry. J Am Coll Cardiol. 2021 Apr;77:1994–2003. doi: 10.1016/j.jacc.2021.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Medranda G.A., Brahmbhatt K., Alawneh B., Marzo K.P., Schwartz R.K., Green S.J. Initial single-center ST-segment elevation myocardial infarction experience in New York before and during the COVID-19 pandemic. Cardiovasc Revasc Med. 2022 Jan;34:80–85. doi: 10.1016/j.carrev.2021.01.026. Epub 2021 Jan 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamadeh A., Aldujeli A., Briedis K., Tecson K.M., Sanz-Sánchez J., Al dujeili M., et al. Characteristics and outcomes in patients presenting with COVID-19 and ST-segment elevation myocardial infarction. Am J Cardiol. 2020;131:1–6. doi: 10.1016/j.amjcard.2020.06.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prieto-Lobato A., Ramos-Martínez R., Vallejo-Calcerrada N., Corbí-Pascual M., Córdoba-Soriano J.G. A case series of stent thrombosis during the COVID-19 pandemic. JACC Case Rep. 2020;2:1291–1296. doi: 10.1016/j.jaccas.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lacour T., Semaan C., Genet T., Ivanes F. Insights for increased risk of failed fibrinolytic therapy and stent thrombosis associated with COVID-19 in ST-segment elevation myocardial infarction patients. Catheter Cardiovasc Interv. 2021;97:E241–E243. doi: 10.1002/ccd.28948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hinterseer M., Zens M., Wimmer R.J., Delladio S., Lederle S., Kupatt C., et al. Acute myocardial infarction due to coronary stent thrombosis in a symptomatic COVID-19 patient. Clin Res Cardiol. 2021;110:302–306. doi: 10.1007/s00392-020-01663-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.