Abstract
Background:
The effects of recent initiatives to better educate unilateral breast cancer (UBC) patients about contralateral prophylactic mastectomy (CPM) have not been fully examined. The purpose of this study was to update and examine recent annual CPM trends by evaluating 2015–2020 data from a large administrative claims database. We also sought to determine if there were any variations in trends among different age groups and reconstructive modalities.
Methods:
Patients diagnosed with UBC between 2015 and 2019 were identified in Optum Clinformatics DataMart. Patients were then categorized by age group, whether they underwent CPM, whether they underwent breast reconstruction (BR), timing of any BR (immediate or delayed), and type of BR (implant-based or autologous).
Results:
Of 55,060 patients who were diagnosed with UBC, 2625 (4.8%) underwent CPM. After a slight decline from 2015 to 2016, the CPM rate among UBC patients increased significantly from 3.4% in 2016 to 6.8% in 2019. Although this upward trend remained consistent across all age groups examined, younger UBC patients represented a significantly higher and faster growing percentage of those undergoing CPM. BR rates among those who underwent CPM also increased between 2015 and 2019, with implant-based and immediate BR becoming more heavily favored over autologous and delayed BR.
Conclusions:
CPM rates continued to rise between 2016 and 2019 and younger women represented a substantially higher and faster growing percentage of UBC patients undergoing CPM than older women. In addition, implant-based and immediate BR are becoming more heavily favored over autologous and delayed BR.
Takeaways
Question: What are recent national trends in contralateral prophylactic mastectomy (CPM) rates among patients with unilateral breast cancer?
Findings: A retrospective analysis of the Optum Clinformatics DataMart, a de-identified administrative health database, revealed a significant increase in CPM rates in recent years, particularly, among younger patients, along with an increase in reconstruction rates.
Meaning: CPM and breast reconstruction rates have risen in recent years, particularly among younger patients. Further research is necessary, however, to understand the age-dependent motivations responsible for these trends, with the goal being to more effectively educate patients with unilateral breast cancer about their treatment options.
INTRODUCTION
Breast cancer is the second most common cause of death from cancer in women in the USA.1 Fortunately, due to advances in breast cancer detection and major treatment advances, breast cancer mortality rates have consistently declined over the last couple decades.2,3 Prior studies and published reports from cancer registries in the USA have also demonstrated a steady decline in contralateral breast cancer incidence rates over the same time period.3,4 Despite advances in detection and treatment, as well as decline in contralateral breast cancer incidence, contralateral prophylactic mastectomy (CPM) rates have increased substantially.5 This trend has alarmed the medical community, as unilateral breast cancer (UBC) patients electing to undergo CPM are at risk for increased postoperative morbidity when compared with unilateral mastectomy or when compared with women undergoing prophylactic bilateral mastectomy (BM) (Shaheen et al., unpublished data).6–8 CPM is also associated with significant financial burden to healthcare costs in the USA.9 Several physician-led initiatives have therefore been undertaken to better educate UBC patients and their providers about CPM.10
The effects of these initiatives over the last few years have not been fully examined. In addition, although the motivations of UBC patients to undergo CPM are wide-ranging,11 understanding the demographics of UBC patients within this trend and the reconstructive factors that may contribute to the decision to undergo CPM may help more effectively tailor efforts to educate UBC patients about their treatment options. The purpose of this study was to update and examine recent annual CPM trends by evaluating 2015–2020 data from a large administrative claims database. We also sought to determine if there were any variations in trends among different age groups and reconstructive modalities. We hypothesized that the rise in CPM is continuing and that an increasing rate of UBC patients who underwent BM are electing to have breast reconstruction (BR).
METHODS
Database
We conducted a retrospective analysis of 2015–2020 data from the Optum Clinformatics DataMart (OptumInsight, Eden Prairie, Minn.) (Optum), a de-identified administrative health database, including claims data from recipients of commercial health insurance and Medicare Advantage. This database does not use sampling weights and is not necessarily nationally representative, but includes data for over 60 million unique individuals, spanning all 50 U.S. states. It therefore represents claims data for a substantial portion of individuals covered by commercial insurance providers in the United States. This database assigns a unique patient identification number, which allows for longitudinal analysis. Our institutional review board considered use of this database to be exempt from institutional review board review.
Identification of Diagnoses, Patients, and Other Outcomes
Optum was searched for female adult (≥18 years old) patients who were diagnosed with UBC between 2015 and 2019, using Current Procedural Terminology (CPT) and International Classification of Disease (ICD) codes. Patients were excluded if they had bilateral breast cancer, failed to have continuous health plan enrollment for at least 6 months following the UBC diagnosis, or had no encounter within 6 months following the initial UBC diagnosis.
Explanatory variables extracted from the database included age, geographic region of residence, type of insurance plan, race, and Charlson comorbidity index score at the time of the BM procedure. Insurance plans were divided into managed plans (which included point of service plans, preferred provider organizations, health maintenance organizations, and exclusive provider organizations), fee-for-service plans, and other/unspecified plans. The Charlson comorbidity index score, a validated score based on weighted ICD diagnosis codes, was calculated to assess comorbidities.12 Patients were additionally categorized by whether they had BR, timing of the procedure (immediate or delayed), and type (implant-based or autologous). A complete list of all ICD and CPT codes used in this study is set forth in Supplemental Digital Content 1. (See table, Supplemental Digital Content 1, which displays the ICD and CPT Codes. http://links.lww.com/PRSGO/C47.)
Statistical Analysis
Descriptive statistics were calculated to summarize and compare patient characteristics. Chi-square tests were used to determine significant differences in any categorical variables. Two-tailed P-values less than 0.05 were considered statistically significant. All statistical analyses were performed using SAS, version 9.4 (SAS Institute, Cary, N.C.).
RESULTS
Patient Characteristics
A total of 55,060 patients who were diagnosed with UBC were identified, of whom 52,435 (95.2%) had no BM and 2,625 (4.8%) had BM. Patients who had BM were significantly younger, had a greater percentage enrolled in managed care insurance plans, and had fewer comorbidities than patients who did not undergo BM. Almost 75% of women who elected not to undergo BM were 65 years old or older, whereas women who elected to undergo BM were more evenly distributed across age groups. In addition, patients from the South and Midwest and with a managed care insurance plan had a higher percentage of BM than those from the Northeast or West or with a non-managed care insurance plan. There was also an overall disproportionate representation of White patients, those enrolled in managed care insurance plans, and those from the South. Demographics of the patients included in this study are set forth in Table 1.
Table 1.
Baseline Characteristics of UBC Patients
| Characteristic | Total (n = 55,060) | Bilateral Mastectomy | P (UBC Patients with versus without BM) | |
|---|---|---|---|---|
| Yes (n = 2625) | No (n = 52,435) | |||
| Age, y | ||||
| 18–34 | 177 (0.3%) | 52 (2.0%) | 125 (0.2%) | <0.0001 |
| 35–44 | 1588 (2.9%) | 344 (13.1%) | 1244 (2.4%) | <0.0001 |
| 45–54 | 5345 (9.7%) | 747 (28.5%) | 4598 (8.8%) | <0.0001 |
| 55–64 | 8122 (14.8%) | 643 (24.5%) | 7479 (14.3%) | <0.0001 |
| ≥65 | 39,828 (72.3%) | 839 (32.0%) | 38,989 (74.4%) | <0.0001 |
| Geographic region | ||||
| Northeast | 6963 (12.6%) | 243 (9.3%) | 6720 (12.8%) | <0.0001 |
| South | 20,759 (37.7%) | 1072 (40.8%) | 19,687 (37.5%) | 00.0007 |
| Midwest | 11,837 (21.5%) | 867 (33.0%) | 10,970 (20.9%) | <0.0001 |
| West | 15,336 (27.9%) | 441 (16.8%) | 14,895 (28.4%) | <0.0001 |
| Unspecified | 165 (0.3%) | 2 (0.1%) | 163 (0.3%) | <0.0001 |
| Type of insurance plan | ||||
| Managed care | 37,069 (67.3%) | 2100 (80.0%) | 34,969 (66.7%) | <0.0001 |
| Fee-for-service | 903 (1.6%) | 22 (0.8%) | 881 (1.7%) | 00.0009 |
| Other/unspecified | 17,088 (31.0%) | 503 (19.2%) | 16,585 (31.6%) | <0.0001 |
| Race | ||||
| White | 38,597 (70.1%) | 2,075 (79.0%) | 36,522 (69.7%) | <0.0001 |
| Black | 5128 (9.3%) | 215 (8.2%) | 4913 (9.4%) | 00.0424 |
| Hispanic | 4897 (8.9%) | 155 (5.9%) | 4742 (9.0%) | <0.0001 |
| Asian | 1660 (3.0%) | 62 (2.4%) | 1598 (3.0%) | 00.0455 |
| Other/unspecified | 4778 (8.7%) | 118 (4.5%) | 4660 (8.9%) | <0.0001 |
| Charlson comorbidity index score | ||||
| 0–1 | 4474 (8.1%) | 347 (13.2%) | 4127 (7.5%) | <0.0001 |
| 2–3 | 33,772 (61.3%) | 1858 (70.8%) | 31,914 (58.0%) | <0.0001 |
| ≥4 | 16,814 (30.5%) | 420 (16.0%) | 16,394 (29.8%) | <0.0001 |
Annual Trends
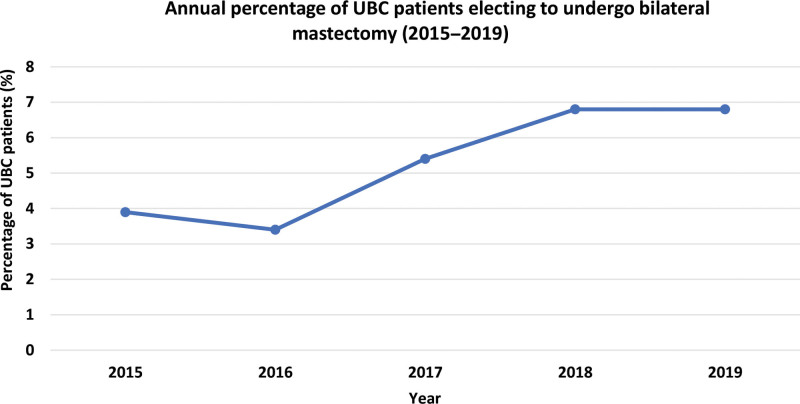
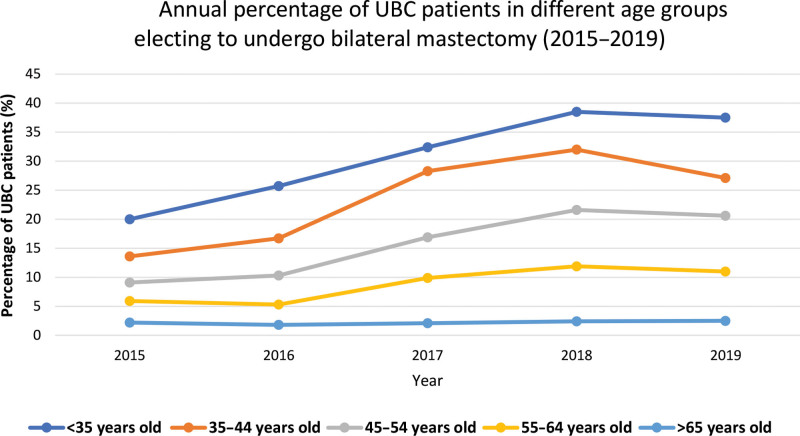
After a slight decline from 2015 to 2016, the rate of BM among patients who had UBC increased significantly from 3.4% in 2016 to 6.8% in 2019 (Fig. 1). This trend of an increasing percentage of UBC patients undergoing BM during the study period remained consistent across all age groups examined (Fig. 2). However, the percentage of UBC patients who elected to undergo BM varied significantly between age groups, with younger UBC patients consistently having higher rates of BM than older UBC patients (Fig. 2). In addition, the percentage of younger UBC patients who underwent BM generally increased at a higher rate than older UBC patients. For example, the percentage of UBC patients younger than 35 years old who underwent BM increased from 20% in 2015 to 37.5% in 2019, whereas the percentage of UBC patients older than 65 years old who underwent BM increased from 2.2% in 2015 to 2.5% in 2019 (Fig. 2).
Fig. 1.
Annual percentage of UBC patients electing to undergo bilateral mastectomy.
Fig. 2.
Annual percentage of UBC patients in different age groups electing to undergo bilateral mastectomy.
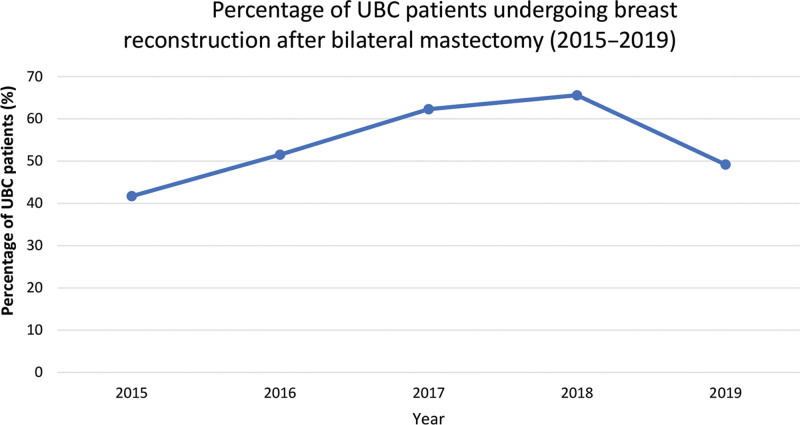
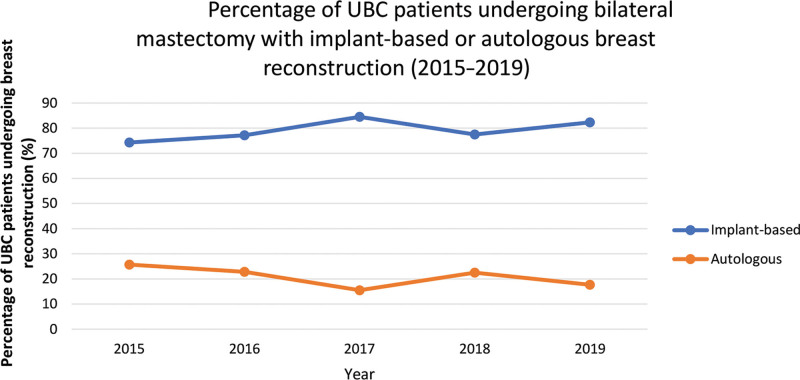
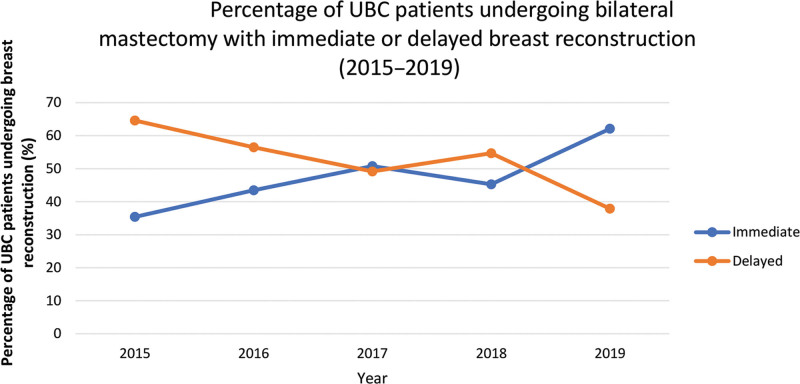
BR rates among UBC patients who elected to undergo BM increased steadily from 41.7% in 2015 to 65.6% in 2018, but declined to 49.3% in 2019 (Fig. 3). Among UBC patients who elected to undergo BM with BR, the rate of implant-based (versus autologous) BR increased from 74.3% in 2015 to 82.3% in 2019 (Fig. 4). The percentage of these patients who elected to undergo immediate (versus delayed) BR also significantly increased from 35.4% in 2015 to 62.1% in 2019 (Fig. 5).
Fig. 3.
Percentage of UBC patients undergoing breast reconstruction after bilateral mastectomy.
Fig. 4.
Percentage of UBC patients undergoing bilateral mastectomy with implant-based or autologous breast reconstruction.
Fig. 5.
Percentage of UBC patients undergoing bilateral mastectomy with immediate or delayed breast reconstruction.
In our trends analysis, we observed either a plateau or declining trend in BM and BR rates in the transition from 2018 to 2019. For example, in our review of BM rates among UBC patients, BM rates overall and in almost every age group plateaued or declined between 2018 and 2019. Similarly, there was a decline in the rate of BR among UBC patients who underwent BM from 65.6% in 2018 to 49.2% in 2019. We suspect this aberration in 2019 was likely the result of data limitation rather than actual reflection of nationwide trends. At the time of this study, Optum data after June 30, 2020 were not available and patients who were diagnosed with UBC in 2019 but elected to undergo BM or BR after June 30, 2020 would not be captured in the BR trend analysis. We suspect 2019 would reflect higher BM and BR rates (in line with the trend of the past few years) once more current data become available.
DISCUSSION
The primary objective of this study was to update and examine annual CPM trends by evaluating national data between 2015 and 2020. To our knowledge, this study is the most current assessment of CPM trends in the United States. In our analysis of 55,060 UBC patients nationwide, we found an increasing rate of UBC patients electing to undergo BM. This trend strongly correlated with age, with younger women representing a substantially faster growing percentage of UBC patients undergoing BM than older women. UBC patients electing to undergo BM were also well distributed across different age groups, but almost 75% of UBC patients who elected not to undergo BM were 65 years old or older. There was also an increasing rate of UBC patients who elected to undergo BR after BM between 2015 and 2019, with implant-based and immediate BR becoming more heavily favored over autologous and delayed BR. During the course of the study period, we in fact found immediate BR overtake delayed BR as the most common form of BR among UBC patients.
The steady rise in BM rates among UBC patients found in the present study aligns with the results of prior studies.13,14 Given the lack of a clear survival benefit over unilateral mastectomy,5,15 this strong rise in CPM rates has prompted efforts to better educate breast cancer patients.16,17 Reflecting the impact that position statements of the Society of Surgical Oncology and other initiatives ostensibly had on better educating breast cancer patients about their treatment options, one recent study found a modest decline in CPM rates between 2013 to 2016 among early stage breast cancer patients.10,18 Although our study similarly reflected a slight decline in CPM rates between 2015 and 2016, it demonstrates a return to climbing CPM rates in subsequent years overall and across all age groups. By elucidating which age cohorts are most affected by rising CPM rates, this study will hopefully help focus initiatives intended to educate UBC patients.
There are a wide number of factors that may contribute to rising BM among UBC patients. Despite a recent study demonstrating that UBC patients undergoing CPM face greater odds of overall complications than those undergoing BM prophylactically (Shaheen et al, unpublished data), UBC patients seem to be influenced toward BM due to the Jolie effect and other media exposure to prophylactic treatment options.16,19 Another principal reason for UBC patients to undergo CPM is the peace of mind from not having to continue ongoing surveillance of the contralateral breast.20,21 While overestimation of the risk of developing contralateral breast cancer in newly diagnosed UBC patients may factor into the rise in BMs,22 the presence of occult neoplastic tissue in the contralateral breast in up to 7% of patients lends support to these fears.7 Prior studies have also found that, among women who elect to undergo CPM with BR, breast symmetry is another significant factor in deciding to undergo CPM.22,23 These driving factors should be taken into consideration in educating UBC patients about their treatment options.
Current trends in postmastectomy reconstructive decisions identified in this study reflect a continuation of trends reported in prior studies that have shown a steady rise in BR, immediate (versus delayed) reconstruction, and implant-based (versus autologous) reconstruction.24,25 The rise in BR has been attributable to a number of factors, including the federal enactment of the Women’s Health & Cancer Rights Act in 1998, which required insurance coverage of BR after mastectomy,25 passage of state legislation mandating mastectomy patients to be informed of BR options,26 and greater general awareness of BR options through advocacy groups and social media.27 The overall increase in BR may also be the direct result of rapidly rising BM rates among UBC patients. The driving factors behind the increased rate of immediate (versus delayed) reconstruction is also likely multifactorial. Certain studies have linked the rise in immediate BR to the aforementioned federal and state legislations.28 Others have noted improved quality of life and satisfaction with appearance as important motivations for patients electing to undergo immediate (versus delayed) BR.29 With respect to the increase in implant-based (versus autologous) BR, historical changes in financial incentives for surgeons, which included increased private insurance payments for implant-based BR but unchanged payments for autologous BR, likely had a significant impact.24,30 In addition, prior disadvantages of subpectoral implant-based BR, which frequently resulted in acute pain and animation deformity, have been overcome with the use of a prepectoral approach.31 The relatively recent resurgence of the prepectoral approach, which was made possible through the advent of acellular dermal matrices (ADM), advances in tissue expander technology, and the use of adjunctive fat grafting, has resulted in decreased pain, better muscle function, and prevention of animation deformity.32 This change in surgical technique may have also contributed to implant-based BR becoming a more attractive option for some patients than autologous BR. Improved implant technology, shorter operative time, less demanding technical skill of the surgeons, and quicker recovery time are likely other important contributors to rising implant-based BR rates. The continuation of these trends toward increasing BR, immediate (versus delayed) reconstruction, and implant-based (versus autologous) reconstruction emphasizes the need to better understand the increased risks, if any, presented by CPM.
This study has several strengths, including being the most current study evaluating trends in BM rates among UBC patients nationwide and providing data for over 55,000 UBC patients after analyzing large-scale data with over 60 million unique individuals in all 50 U.S. states. There were also several limitations to our study. This study relied on the accuracy of billing codes included in the Optum database to identify cohorts, comorbidities, and procedures, and misclassification is possible. However, systemic misclassification on a nationwide basis is unlikely and this alone should not undermine the validity of the results of this study. Our sample also had a disproportionate representation of White patients, those from the South and Midwest in the United States, and those in managed health care insurance plans. Our sample additionally had a disproportionate representation of patients older than 55 years old. Incidence of breast cancer appears to be several-fold higher in this age cohort (versus younger age cohorts) and our sample may therefore simply reflect recent demographics of breast cancer.33 Nevertheless, racial, age, and regional differences in outcomes, as well as health disparities in underinsured populations, may affect generalizability of the results of this study. In addition, the rate of BM among UBC patients in our study was relatively low compared with prior studies. We attribute this to two main factors. First, the population samples are different and, as described above, our sample had a disproportionate representation of White patients residing in certain geographic locations in the United States. Second, prior studies have used alternative inclusion or exclusion criteria for UBC patients, such as exclusion of patients who did not meet certain histological and staging requirements,5 inclusion of patients exclusively in the State of New York,34 or exclusion of patients whose tumor size did not meet certain metrics or who were diagnosed through an excisional biopsy.18
CONCLUSIONS
The continued rise in CPM rates in recent years demonstrates the persistence of this trend and highlights the need to effectively tailor efforts to educate UBC patients about their treatment options. After analyzing over 55,000 patients nationwide, this study demonstrated that the trend strongly correlates with age, with younger women representing a substantially faster growing percentage of UBC patients electing to undergo CPM. In addition, this study has shown that implant-based and immediate BR are becoming more heavily favored over autologous and delayed BR. Further research is necessary to understand how motivations for electing CPM among UBC patients differs among age groups and whether patient education should include more information about certain reconstructive modalities. UBC patients may otherwise be undergoing potentially unnecessary surgery that carries increased risk of postoperative complications and substantially higher financial burden. The results of this study update our understanding of nationwide temporal CPM trends and provide important data points for future research and understanding of how to more effectively educate UBC patients about their treatment options.
ACKNOWLEDGMENTS
M.S.S. was supported by a MedScholars research award from Stanford University School of Medicine for this project. Data for this project were accessed using the Stanford Center for Population Health Sciences Data Core. The PHS Data Core is supported by a National Institutes of Health National Center for Advancing Translational Science Clinical and Translational Science Award (UL1 TR001085) and from Internal Stanford funding. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Supplementary Material
Footnotes
Published online 25 May 2022.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Trayes KP, Cokenakes SEH. Breast cancer treatment. Am Fam Physician. 2021;104:171–178. [PubMed] [Google Scholar]
- 2.DeSantis CE, Ma J, Gaudet MM, et al. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69:438–451. [DOI] [PubMed] [Google Scholar]
- 3.Nichols HB, Berrington de González A, Lacey JV, Jr, et al. Declining incidence of contralateral breast cancer in the United States from 1975 to 2006. J Clin Oncol. 2011;29:1564–1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bernstein JL, Lapinski RH, Thakore SS, et al. The descriptive epidemiology of second primary breast cancer. Epidemiology. 2003;14:552–558. [DOI] [PubMed] [Google Scholar]
- 5.Wong SM, Freedman RA, Sagara Y, et al. Growing use of contralateral prophylactic mastectomy despite no improvement in long-term survival for invasive breast cancer. Ann Surg. 2017;265:581–589. [DOI] [PubMed] [Google Scholar]
- 6.Eck DL, Perdikis G, Rawal B, et al. Incremental risk associated with contralateral prophylactic mastectomy and the effect on adjuvant therapy. Ann Surg Oncol. 2014;21:3297–3303. [DOI] [PubMed] [Google Scholar]
- 7.Alba B, Schultz BD, Cohen D, et al. Risk-to-benefit relationship of contralateral prophylactic mastectomy: the argument for bilateral mastectomies with immediate reconstruction. Plast Reconstr Surg. 2019;144:1–9. [DOI] [PubMed] [Google Scholar]
- 8.Chadab TM, Bernstein JL, Lifrieri A, et al. Is it worth the risk? Contralateral prophylactic mastectomy with immediate bilateral breast reconstruction. Ann Plast Surg. 2021;87(1s suppl 1):S2–S6. [DOI] [PubMed] [Google Scholar]
- 9.Billig JI, Duncan A, Zhong L, et al. The cost of contralateral prophylactic mastectomy in women with unilateral breast cancer. Plast Reconstr Surg. 2018;141:1094–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hunt KK, Euhus DM, Boughey JC, et al. Society of surgical oncology breast disease working group statement on prophylactic (risk-reducing) mastectomy. Ann Surg Oncol. 2017;24:375–397. [DOI] [PubMed] [Google Scholar]
- 11.Buchanan PJ, Abdulghani M, Waljee JF, et al. An analysis of the decisions made for contralateral prophylactic mastectomy and breast reconstruction. Plast Reconstr Surg. 2016;138:29–40. [DOI] [PubMed] [Google Scholar]
- 12.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 13.Wang T, Baskin AS, Dossett LA. Deimplementation of the choosing wisely recommendations for low-value breast cancer surgery: a systematic review. JAMA Surg. 2020;155:759–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kummerow KL, Du L, Penson DF, et al. Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg. 2015;150:9–16. [DOI] [PubMed] [Google Scholar]
- 15.Tuttle TM, Habermann EB, Grund EH, et al. Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. J Clin Oncol. 2007;25:5203–5209. [DOI] [PubMed] [Google Scholar]
- 16.Boughey JC, Attai DJ, Chen SL, et al. Contralateral prophylactic mastectomy (CPM) consensus statement from the American society of breast surgeons: data on CPM outcomes and risks. Ann Surg Oncol. 2016;23:3100–3105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Choosing Wisely. Double mastectomies. Available at https://www.choosingwisely.org/clinician-lists/breast-surgeons-mastectomies-for-single-breast-cancer-patients/. Published June 27, 2016. Accessed August 16, 2021.
- 18.Baskin AS, Wang T, Bredbeck BC, et al. Trends in contralateral prophylactic mastectomy utilization for small unilateral breast cancer. J Surg Res. 2021;262:71–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Basu NN, Hodson J, Chatterjee S, et al. The Angelina Jolie effect: contralateral risk-reducing mastectomy trends in patients at increased risk of breast cancer. Sci Rep. 2021;11:2847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang J, Chagpar A. Factors associated with decision to undergo contralateral prophylactic mastectomy versus unilateral mastectomy. Am J Surg. 2019;218:170–174. [DOI] [PubMed] [Google Scholar]
- 21.Katz SJ, Morrow M. Contralateral prophylactic mastectomy for breast cancer: addressing peace of mind. JAMA. 2013;310:793–794. [DOI] [PubMed] [Google Scholar]
- 22.Farhangkhoee H, Matros E, Disa J. Trends and concepts in post-mastectomy breast reconstruction. J Surg Oncol. 2016;113:891–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agarwal S, Kidwell KM, Kraft CT, et al. Defining the relationship between patient decisions to undergo breast reconstruction and contralateral prophylactic mastectomy. Plast Reconstr Surg. 2015;135:661–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hernandez-Boussard T, Zeidler K, Barzin A, et al. Breast reconstruction national trends and healthcare implications. Breast J. 2013;19:463–469. [DOI] [PubMed] [Google Scholar]
- 25.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23. [DOI] [PubMed] [Google Scholar]
- 26.Garfein ES. The privilege of advocacy: legislating awareness of breast reconstruction. Plast Reconstr Surg. 2011;128:803–804. [DOI] [PubMed] [Google Scholar]
- 27.Panchal H, Matros E. Current trends in postmastectomy breast reconstruction. Plast Reconstr Surg. 2017;140:7S–13S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang RL, Newman AS, Lin IC, et al. Trends in immediate breast reconstruction across insurance groups after enactment of breast cancer legislation. Cancer. 2013;119:2462–2468. [DOI] [PubMed] [Google Scholar]
- 29.Eltahir Y, Werners LLCH, Dreise MM, et al. Quality-of-life outcomes between mastectomy alone and breast reconstruction: comparison of patient-reported BREAST-Q and other health-related quality-of-life measures. Plast Reconstr Surg. 2013;132:201e–209e. [DOI] [PubMed] [Google Scholar]
- 30.Alderman AK, Storey AF, Nair NS, et al. Financial impact of breast reconstruction on an academic surgical practice. Plast Reconstr Surg. 2009;123:1408–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jafferbhoy S, Chandarana M, Houlihan M, et al. Early multicentre experience of pre-pectoral implant based immediate breast reconstruction using Braxon. Gland Surg. 2017;6:682–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marks JM, Farmer RL, Afifi AM. Current trends in prepectoral breast reconstruction: a survey of American society of plastic surgeons members. Plast Reconstr Surg Glob Open. 2020;8:e3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.SEER*Explorer: An interactive website for SEER cancer statistics. Surveillance Research Program, National Cancer Institute. Available at https://seer.cancer.gov/explorer/index.html. Accessed March 8, 2022.
- 34.Schroeder MC, Tien YY, Erdahl LM, et al. The relationship between contralateral prophylactic mastectomy and breast reconstruction, complications, breast-related procedures, and costs: a population-based study of health insurance data. Surgery. 2020;168:859–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.