Abstract
Background
The mental health effects of healthcare work during the COVID-19 pandemic have been substantial, but it is not known how long they will persist. This study aimed to determine if hospital workers’ burnout and psychological distress increased monotonically over 1 year, during which waves of case numbers and hospitalizations waxed and waned, or followed some other pattern.
Methods
A prospective longitudinal survey was conducted at four time-points over 1 year in a cohort of 538 hospital workers and learners, which included validated measures of burnout (emotional exhaustion scale of Maslach Burnout Inventory) and psychological distress (K6). Repeated measures ANOVA tested changes over time and differences between subjects by occupational role, age and ethnic group. The direction and magnitude of changes over time were investigated by plotting rates of high scores (using cut-offs) at each time-point compared to case rates of COVID-19 in the city in which the study took place.
Results
There were significant effects of occupational role (F = 11.2, p < .001) and age (F = 12.8, p < .001) on emotional exhaustion. The rate of high burnout was highest in nurses, followed by other healthcare professionals, other clinical staff, and lowest in non-clinical staff. Peak rates of high burnout occurred at the second or third measurement point for each occupational group, with lower rates at the fourth measurement point. Similarly to the results for emotional exhaustion, rates of high psychological distress peaked at the spring 2021 measurement point for most occupational groups and were higher in nurses than in other healthcare professionals.
Conclusions
Neither emotional exhaustion nor psychological distress was rising monotonically. Burnout and psychological distress were consistently related to occupational role and were highest in nurses. Although emotional exhaustion improved as the case rate of COVID-19 decreased, rates of high emotional exhaustion in nurses and other healthcare professionals remained higher than was typically measured in hospital-based healthcare workers prior to the pandemic. Ongoing monitoring of healthcare workers’ mental health is warranted. Organizational and individual interventions to support healthcare workers continue to be important.
Keywords: COVID-19, Pandemic, Healthcare workers, Nurses, Burnout, Resilience, Psychological distress
Background
A global pandemic of COVID-19 was declared by the World Health Organization on March 11, 2020 [1]. New cases have occurred in waves lasting months, which vary by geographic region [2]. The mental health effects of working in healthcare during the pandemic are widely appreciated to be substantial, resulting from uncertainty, risk of infection, high volumes of acutely ill patients, and long hours, among other factors. Reports from cross-sectional studies have consistently indicated, for example, high rates of depressive and anxiety symptoms, sleep disturbance and burnout in healthcare workers [3–6].
Professional burnout is a particularly important outcome of occupational stress in healthcare because, in addition to its impact on individual professionals, burnout has adverse consequences for the healthcare system and patients, including absenteeism, higher workforce turnover, reduced productivity, increased medical errors, and reduced quality of care [7–10]. As described by Maslach and colleagues [11], burnout is comprised of three components: emotional exhaustion, depersonalization (becoming indifferent or emotionally distant), and a diminished sense of personal accomplishment. Burnout was recognized prior to the COVID-19 pandemic to be a major occupational risk in health care [12, 13]. Workplace factors that were known to contribute to burnout include high workload, lack of scheduling flexibility, the burden of administrative tasks, and concern about workplace safety [14–20]. In addition to workplace stressors that were present prior to the COVID-19 pandemic, additional potential sources of burnout have emerged, including constraints on care that cause moral distress [21, 22], and redeployment to unfamiliar types of work [23].
While burnout is not considered to be a mental illness, symptoms of common mental disorders have also been measured to determine the impact of the COVID-19 pandemic on healthcare workers’ mental health. A systematic review containing 65 studies that include 97,333 healthcare workers from 21 countries found pooled prevalence’s of 21.7, 22.1, and 21.5% for moderate depression, anxiety, and post-traumatic stress disorder respectively during COVID-19 [24]. Similarly, in a systematic review and meta-analysis including 29 studies and 22,380 hospital staff caring for COVID-19 patients from countries in Europe and Asia, the prevalence of depression, anxiety, and stress was 24.3, 25.8, and 45%, respectively [6].
Regarding which healthcare workers have been at greatest risk of adverse psychological outcomes during the COVID-19 pandemic, a meta-analysis of studies published up to July 2020 indicated rates of distress and burnout were higher in nurses, females and frontline workers than in doctors, males and non-frontline workers [25]. Some studies published since this meta-analysis have also indicated higher rates in nurses than doctors although this finding is not universal [21, 26, 27].
The long-term impact of the COVID-19 pandemic on healthcare workers’ mental health is not known. Some factors suggest that the mental impact of the pandemic will be enduring. In particular, after the 2003 outbreak of severe acute respiratory syndrome (SARS) had resolved, healthcare workers in affected hospitals reported a range of stress effects that continued to be significantly elevated compared to workers in non-affected hospitals for as long as they were followed, which was 18–24 months [28]. Of concern, the COVID-19 pandemic is far more severe, widespread and persistent than the SARS outbreak and has severely affected many aspects of life in the community as well as in the hospital, which suggests its mental impact will be greater, and may resolve more slowly. Furthermore, pre-pandemic rates of burnout in many settings were high, in the range of 20–40% [29–31], indicating that even full resolution of pandemic-related factors would still leave healthcare workers at considerable risk. On the other hand, there is much evidence that in general, the most common long-term response to exposure to highly aversive events is resilience [32].
As evidence emerges, prediction of future negative mental health consequences of the COVID-19 pandemic for healthcare workers will benefit from determining longitudinal trends in burnout and psychological distress among hospital workers. In particular, it would be useful to determine if negative mental health effects are rising monotonically over time, as one would expect to result from accumulating stress effects, or following a different pattern, possibly rising when COVID-19 cases are higher and improving as COVID-19 case rates decrease. Going forward, interventions to support healthcare workers’ well-being could differ in these two scenarios. Longitudinal data published thus far in the COVID-19 pandemic gives little insight into these long-term patterns because it has covered periods early in the pandemic, typically with either two measurement points or over a period of only a few weeks. Studies of longer-term patterns of burnout and psychological distress later in the pandemic have not yet been published.
We report on two mental health measures, namely the emotional exhaustion component of burnout and psychological distress, collected in the same cohort of hospital personnel at four time-points (approximately quarterly) from the fall of 2020 to the summer of 2021. Our primary question is whether indicators of these mental health problems are (i) rising monotonically, or (ii) following some other pattern, such as rising and falling in synchrony with the local epidemiological waves of COVID-19 cases. Our secondary questions are whether this pattern differs between personnel with different occupational roles, what proportion of hospital personnel participating in this survey are reporting levels of emotional exhaustion and psychological distress that are considered high at each time point, and how the depersonalization and personal accomplishment dimensions of burnout change over this period.
Methods
Study design and participants
A survey of the psychological well-being of a cohort of hospital staff, learners (nursing students, medical students, residents), and volunteers during the pandemic was conducted at two sites of Sinai Health (an urban acute care teaching hospital and a rehabilitation hospital, with > 6000 employed staff) in Toronto, Canada at four time-points. The survey methods have been described previously [33]. Briefly, the first survey (T1, “fall 2020”) was conducted from Sept 21-Nov 15, 2020. The first survey was open to all hospital employees, physicians, learners, volunteers, retail employees, and contractors. Potential participants were informed of an online survey link via “all-staff” emails (e.g. communication updates or newsletters) from the hospital or from their chiefs and directors, as well as information posters in high-traffic areas of the hospital. All surveys were completed online using software that is compliant with privacy standards (the Personal Health Information Protection Act, in this jurisdiction) (Alchemer, Louiseville, CO). Of 884 respondents who provided consent in a pre-survey recruitment phase, 538 (61.0%) completed a T1 survey to form the cohort for further follow-up. The denominator for an overall participation rate (i.e. the number of staff who were sufficiently informed to make a decision to participate or not) is not known because the survey was open to all staff and advertised by various means, but individual invitations to participate were not used. The entire salaried workforce who might have participated was approximately 6000. Subsequent surveys of the T1 cohort were conducted in these time periods in 2021: Jan 25-Feb 15 (T2, “winter 2021”), Apr 26-May 16 (T3, “spring 2021”), and Jul 26-Aug 15 (T4, “summer 2021”). All members of the T1 cohort were invited to participate in all subsequent surveys, even if they were on leave or were not working at the hospital at the time of a survey. Each survey included measures of emotional exhaustion and psychological distress, among other measures. Participants were randomized to a shorter (Express) or longer (Enriched) version of the survey. Surveys varied in length over time due to instruments that were included at only some time-points. The total length of the Express survey varied from 45 to 83 items and the total length of the Enriched survey varied from 77 to 137 items. Among those who participated in the first survey, the participation rate at subsequent time points (the numerator calculated as the number of surveys returned that included a valid measure of emotional exhaustion, psychological distress, or both) was: T2 N = 485 (90% of T1 cohort), T3 N = 424 (79%), T4 N = 409 (76%). The numbers of participants who had left the organization at each survey time-point were: T1–9, T2–21, T3–18, T4–24. Given the small amount of attrition, these were not considered further in the analysis. A gift card (about US$15 value) was provided for each completed survey. The study was approved by the Sinai Health Research Ethics Board.
Measures
Burnout was measured with the Maslach Burnout Inventory (MBI-HSS), which measures emotional exhaustion, depersonalization, and diminished personal accomplishment [34]. Various case definitions of burnout based on MBI-HSS scores have been used previously, which differ in the choice of cut-off scores, and various combinations of the three scales [29]. In order to allow comparison to a broad range of prior studies, we used the emotional exhaustion scale as our primary continuous measure of burnout, and defined burnout using a cut-off of ≥27, which is commonly used to identify high emotional exhaustion [29–31]. As secondary measures, to describe trends in other aspects of burnout we measured depersonalization and personal accomplishment in those participants randomly selected for the Enriched survey, using the most common cut-offs of depersonalization ≥10 and personal accomplishment are ≤33 when reporting case numbers [29]. In this cohort Cronbach’s alpha at the four time-points varied from .94 to .95.
Psychological distress is comprised of depressive and anxiety symptoms. Psychological distress was measured with the Kessler K6, which has 6 items scored from 0 to 4, yielding a range of 0–24. The K6 strongly discriminates between community cases and non-cases of psychiatric disorders diagnosed by structured interview and has acceptable sensitivity and specificity [35, 36]. A cut-off of ≥13 indicates likely serious mental illness [37]. In this cohort Cronbach’s alpha at the four time-points varied from .85 to .87.
Analysis
At T1, participants were sorted into four categories of occupational role based on professional qualifications (i.e. classified as “professionals” if their job is regulated by a professional college, or equivalent) and whether they reported close patient contact (if they were within two metres of a patient for more than 15 minutes in the previous month). The four occupational role categories were nurses, other healthcare professionals (as listed in Table 1), other clinical staff (non-professionals who reported close patient contact), and non-clinical roles (non-professionals without close patient contact). Nurses were analyzed separately based on prior evidence that nurses experienced a greater burden of stress than other professionals during an outbreak of extraordinary infectious disease [28], and have during the COVID-19 pandemic [25].
Table 1.
Characteristics of participants
| N (%) | ||
|---|---|---|
| Role typea | Nursing | 134 (24.9) |
| Other clinical professionals | 156 (29.0) | |
| Other clinical personnel | 90 (16.7) | |
| Non-clinical personnel | 158 (29.4) | |
| Gender | Female | 422 (78.6) |
| (Missing 1) | Male | 85 (15.8) |
| Other/Prefer not to say | 30 (5.6) | |
| Highest education | High school | 13 (2.4) |
| College diploma | 79 (14.7) | |
| Undergraduate degree | 176 (32.7) | |
| Professional/Graduate degree | 270 (50.2) | |
| Ethnic group | African/Black | 30 (5.6) |
| (Missing 1) | Asian | 148 (27.6) |
| South Asian | 35 (6.5) | |
| European/White | 278 (51.8) | |
| Hispanic | 15 (2.8) | |
| Other/Mixed/Multiple | 31 (5.8) | |
| Marital status | Single | 211 (39.2) |
| Married/Common-law | 306 (56.9) | |
| Divorced/Separated/Widowed | 21 (3.9) |
aSpecific job types, in descending order of number of participants. Groups with two or fewer members not listed. Some roles appear in both clinical and non-clinical lists as determined by patient contact as described by participant. Other clinical professionals: Physician, resident, dietician, occupational therapist, social worker, physiotherapist, manager of clinical area, speech language pathologist, pharmacist, respiratory therapist, spiritual care practitioner. Other clinical positions: Administrative assistant, medical imaging technologist, assistant to physician/occupational therapist/physiotherapist, retail employee, porter, clinical research staff, volunteer. Non-clinical positions: Research scientist, research staff, laboratory technician, corporate and administrative staff, administrative assistant, volunteer, manager of non-clinical area, building services staff, clerk, laboratory technologist, housekeeper
Participant characteristics were summarized using descriptive statistics. Continuous measures were summarized using means and standard deviations (SD). Categorical measures were summarized using counts and percentages. In order to provide context for changes in case rates of burnout and high psychological distress over time, daily rates of new cases of COVID-19 diagnosed in Toronto and COVID-19-related hospitalizations during the period of this study were downloaded from Public Health Ontario [38].
Changes over time in emotional exhaustion and psychological distress, as continuous variables, by occupational role were analyzed using repeated measures ANOVA, excluding subjects with missing data at any timepoint. Age was included as a covariate because lower age/less experience have been identified as correlates of higher burnout [39, 40]. Ethnic group (categorized as Asian/South Asian; European/White; Other) was included as a covariate because of discrimination and stigma experienced by Asian people during the pandemic. Gender was not included because it is confounded with occupational role in hospital settings (in particular, in this cohort nurses were 84% female and other non-physician healthcare workers were 87% female). Setting within the hospital (e.g. emergency department, intensive care unit) could not be included in the analysis because (i) many staff members work in multiple settings, and (ii) there were frequent dynamic changes in work settings for many staff members related to having multiple roles or having reassigned duties (e.g. medical nurses re-assigned to intensive care for a period of time and then returning to the medical unit). Within-subjects effects are reported using a Greenhouse-Geisser correction when Mauchly’s test of sphericity indicated a significant deviation from the assumption of sphericity. All analyses were done with IBS SPSS Statistics 28 (Armonk, New York).
Results
The characteristics of personnel in the cohort at T1 are described in Table 1.
Emotional exhaustion
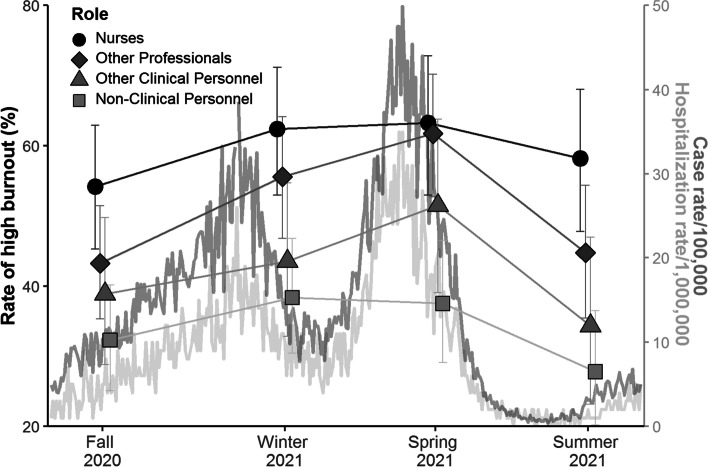
Emotional exhaustion peaked at the winter 2021 or spring 2021 measurement point in each group and was lower by the summer 2021 measurement (Fig. 1). Repeated measures ANOVA of emotional exhaustion for participants for whom there were no missing data over four time-points (82 nurses, 102 other healthcare professionals, 60 other clinical staff, and 118 non-clinical staff) demonstrated significant between-subject effects of occupational role (F = 11.2, p < .001) and age (F = 12.8, p < .001), but not ethnic group (F = 1.3, p = .26). The interaction of occupational role X time was significant (F = 2.0, p = .04), but weak (estimated effect size, eta-squared = .02), indicating a modestly different pattern of change over time in occupational groups. Post hoc testing revealed that the relationship between age and emotional exhaustion was inverse (higher emotional exhaustion with younger age) and grew in strength over time (T1 R = −.06, p = .14, T2 R = −.09, p = .05, T3 R = −.19, p < .001, T4 R = −.21, p < .001). Regarding the direction and magnitude of differences in emotional exhaustion between staff with different occupational roles, the proportion of participants with high emotional exhaustion at each time point, by occupational role, is illustrated in Fig. 1 (with the epidemiological curves of case rates and hospitalization rates in Toronto included for context). The rate of high burnout was highest in nurses, followed by other healthcare professionals, other clinical staff, and lowest in non-clinical staff.
Fig. 1.
Case rates of high burnout by occupational role over 12 months in a Toronto hospital with daily case rates and hospitalization rates of COVID-19 in Toronto during the same period. Note: Figure shows proportion of each occupational group reporting high levels of the emotional exhaustion dimension of burnout, based on a cut-off of ≥ 27
Other burnout dimensions
Mean levels of depersonalization and personal accomplishment at each time point are provided in Table 2, as well as the proportion of participants whose depersonalization scores were high or personal accomplishment scores were low. Participants with high depersonalization scores were rising over time, while the numbers with low personal accomplishment scores were falling. The number of subjects randomly selected to complete these extra measures (the 50% of subjects assigned to the Enriched survey), who completed measures of depersonalization and personal accomplishment at all four time-points included too few participants in one particular occupation category (non-professional staff without patient contact, N = 8) to compare all occupational role groups. However, given the differences found for emotional exhaustion, we compared nurses (N = 41) to other healthcare professionals (N = 55). With respect to depersonalization there were significant differences between these groups, with nurses reporting greater depersonalization (F = 7.4, p = .008), with no significant effect of age. With respect to personal accomplishment there were also significant differences between nurses and other healthcare professionals (F = 9.6, p = .003), with nurses reporting lower personal accomplishment, with no significant effect of age.
Table 2.
Depersonalization and personal accomplishment dimensions of attachment at four time-points
| Depersonalization | Personal accomplishment | |||||||
|---|---|---|---|---|---|---|---|---|
| N | mean | SD | High (%) | N | mean | SD | Low (%) | |
| Fall 2020 | 277 | 4.80 | 5.59 | 18.1 | 270 | 34.42 | 10.99 | 37.0 |
| Winter 2021 | 245 | 5.32 | 6.28 | 18.4 | 238 | 34.47 | 10.2 | 36.6 |
| Spring 2021 | 154 | 6.42 | 6.86 | 23.4 | 148 | 37.85 | 7.05 | 20.3 |
| Summer 2021 | 153 | 6.67 | 7.12 | 26.8 | 147 | 37.06 | 8.90 | 29.9 |
Depersonalization scores range from 0 to 30, with higher scores indicating greater burnout. High scores are based on a cut-off of ≥10. Personal accomplishment scores range from 0 to 48 with lower scores indicating greater burnout. Low scores are based on a cut-off of ≤33
Psychological distress
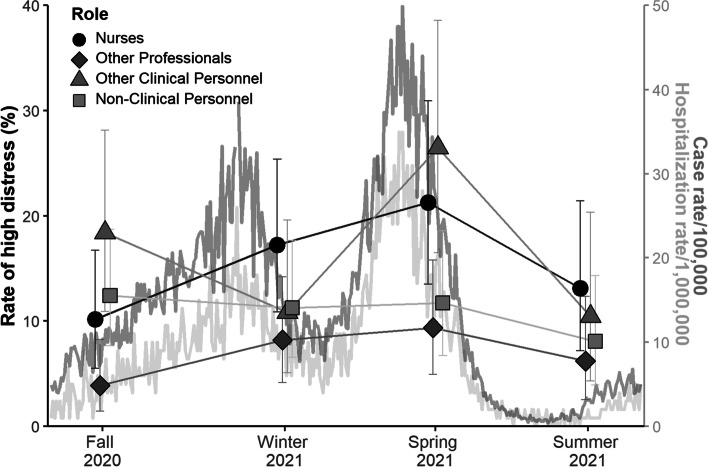
Similarly to the results for emotional exhaustion, psychological distress peaked at the spring 2021 measurement point in most groups (Fig. 2). Repeated measures ANOVA of psychological distress for participants for whom there were no missing data over four time-points (77 nurses, 103 other healthcare professionals, 60 other clinical staff, and 110 non-clinical staff) demonstrated significant between-subject effects of occupational role (F = 3.6, p = .01) and age (F = 33.1, p < .001), but not ethnic group (F = 1.0, p = .33). The interaction of occupation role X time was not significant (F = 0.6, p = .83), indicating a similar pattern of change over time in all groups.
Fig. 2.
Case rates of high psychological distress by occupational role over 12 months in a Toronto hospital with daily case and hospitalization rates of COVID-19 in Toronto during the same period. Note: Figure shows proportion of each occupational group reporting high levels of psychological distress, based on a cut-off of ≥ 13
Post hoc testing revealed that the relationship between age and psychological distress was inverse (higher psychological distress with younger age) and significant at each time point (T1 R = −.24, T2 R = −.29, T3 R = −.24, T4 R = −.29, p < .001 at each time point). The proportion of participants with high psychological distress at each time point, by occupational role, is illustrated in Fig. 2. The severity of psychological distress was highest in nurses.
Discussion
In this longitudinal study of a single cohort of hospital-based health care workers over approximately 1 year during the COVID-19 pandemic, negative mental health indicators measured at 3-month intervals changed significantly over time and varied between workers with different occupational roles. In order to appreciate the relationship of these temporal changes in healthcare worker well-being to dynamic fluctuations in pandemic-related stressors at work and in the community, we have provided local epidemiological curves in Figs. 1 and 2, and a timeline of major events in Fig. 3.
Fig. 3.
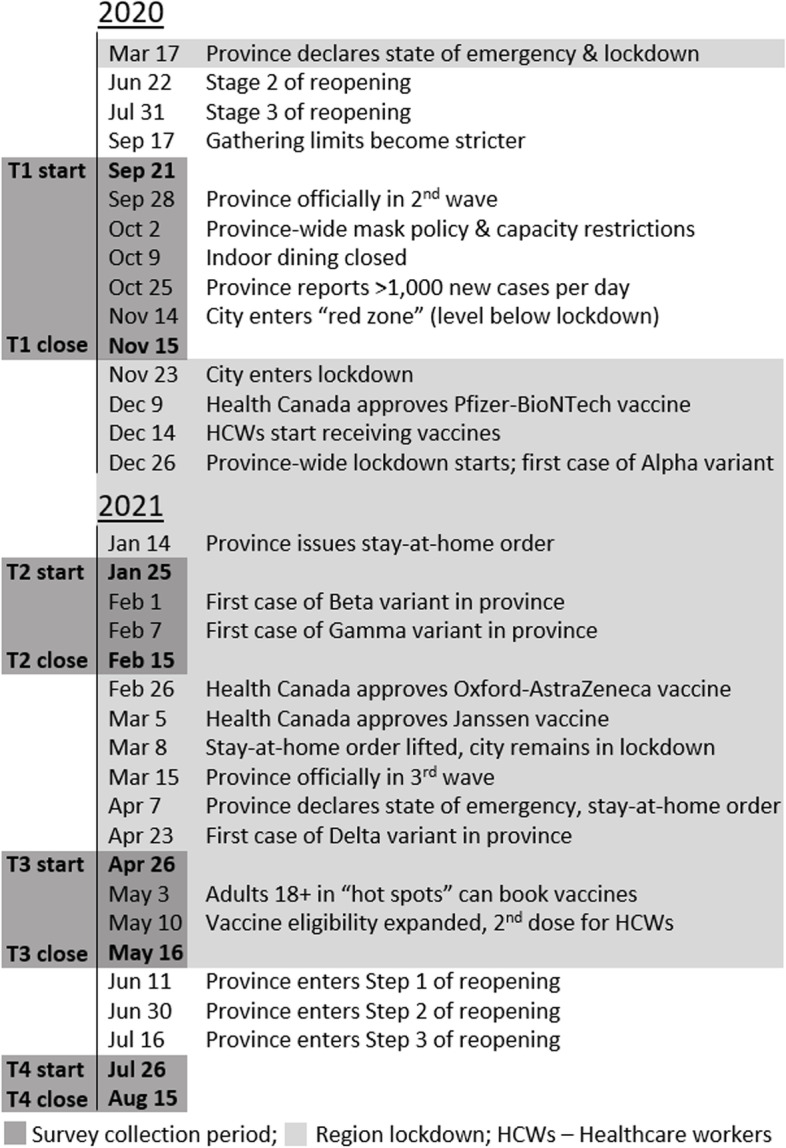
Timeline of major pandemic-related events in Toronto during the study
The severity of emotional exhaustion was greatest in nurses, followed by healthcare professionals of other disciplines, then nonprofessional staff whose work involves close patient contact, with the lowest levels in nonprofessional staff whose work does not involve close patient contact. While workplace factors that contributed to burnout prior to the pandemic, including high workload, lack of scheduling flexibility, and concern about workplace safety [41], have increased during the pandemic for all health professionals, arguably some stressors, such as persistent exposure to high acuity or dying patients, and facilitating patient-families meetings via tablets or other virtual interfaces have been more common for nurses, which could contribute to this difference. In addition, at the hospital at which this study took place, redeployment to critical care units [23], and the experience of working a full shift on a unit under “outbreak status” were more common for nurses than other professions. Pandemic conditions have led to moral distress, which exacerbates burnout [21, 22], but it is not known if this has been disproportionality experienced by particular occupational groups. Although not surprising, rates of high emotional exhaustion in nurses are nonetheless alarming. At the four measurement-points they were 54, 62, 63, and 58% respectively, which is substantially greater than the pre-COVID-19 benchmark of 20–40% found using the same operational case definition [29]. As nurses represent the largest single professional group in hospital care, this degree of mental health burden threatens the function of the healthcare system.
The rates of burnout in this study can be compared to those reported elsewhere, although most reports currently available relate to studies completed before 2021. In August – October 2020 a survey of Australian nurses using an abbreviated version of the MBI found high emotional exhaustion scores in 44% [42]. A US study conducted over the same time span using a single item burnout measure found high burnout in 66% of nurses [43]. A study of nurses in Uganda in May–June 2021 using the ProQOL instrument found high burnout in 40% [44]. The use of different measurement instruments precludes direct comparison, but these studies confirm multiple reports of high rates of burnout in nurses. A survey of internists at two hospitals in Vancouver, Canada from August–October 2020, found high emotional exhaustion in 63% using the same operational definition used in this study [45], which is consistent with our results. Burnout has not often been measured previously in hospital employees with roles other than regulated professionals, and so there is little historical context from which to interpret the degree of burnout found in that group.
The temporal pattern of change in emotional exhaustion differed very little between occupational groups. Inspection of Fig. 1 indicates that in three of the four groups this pattern consisted of a monotonic increase from fall 2020 to spring 2021, with a decrease from spring to summer 2021. The fourth group, nonprofessional staff with no close patient contact, appeared to differ only by beginning the descending trend sooner, peaking in winter 2021. Since the decrease in rates of high emotional exhaustion in summer 2021 corresponds to a period of low levels of new COVID-19 cases in the community, and corresponding low rates of COVID-19 related hospitalization, the trend may indicate that emotional exhaustion in hospital-based healthcare workers is able to recover somewhat as COVID-19 stresses subside. It is noteworthy that COVID-19 vaccination rates in the general public and in healthcare workers increased markedly in Ontario between the spring and summer 2021 surveys, which may have also contributed to reduced burnout. Importantly, the improvement in high emotional exhaustion during the summer of 2021 was an improvement to levels that remain much higher than the pre-COVID-19 benchmark.
Rates of high depersonalization and low personal accomplishment observed in this study are also concerning. Rates of depersonalization increased steadily over this time, which may indicate that depersonalization is a cumulative effect of pandemic related stress that is less responsive to decreasing case rates than emotional exhaustion. Alternatively, depersonalization could be viewed as a coping strategy (i.e. sacrificing empathic patient care in the service of maintaining personal function). Further observation to determine the down-stream consequences of these changes would help distinguish whether increasing depersonalization provides any adaptive benefit. Our participants’ sense of personal accomplishment may have been quicker to recover. Alternatively, the improvement in mean levels of personal accomplishment from winter 2021 to spring 2021 may have been the result of participants with low personal accomplishment scores in the winter 2021 dropping out. Post hoc testing reveals that at the winter 2021 measurement, the mean personal accomplishment scores of those who completed surveys in spring 2021 was 6.0 ± 7.0, whereas the mean score in those who did not complete surveys in spring 2021 was 4.3 ± 4.9 (p = .03). Of note, dropping out from the survey cohort could be related to factors which also contribute to staff choosing to leave their jobs. The risk that pandemic-related burnout will contribute to workforce shortages is an important issue [41] and the role of personal accomplishment merits further investigation as a potential mediator.
Previous longitudinal studies of burnout during the pandemic have used different measures (including single-item measures) which reduces the utility of comparing scores, but with respect to longitudinal trends studies have reported an increase from pre-pandemic to early-pandemic levels in intensive care settings [21] and an increase from April/May 2020 to July/August 2020 in oncology professionals [46]. Two studies have reported multiple serial measurements of burnout over a period of approximately 1 month. Four measurements of burnout at weekly intervals in April 2020, revealed stable levels of burnout in emergency medicine providers [47]. In contrast, burnout measured in physicians at five time-points over 25–31 days (following joining the COVID-19 treatment team) in Italy revealed variation over time [48]. The results of the current study, which indicate variability over time, rather than monotonic changes in emotional exhaustion and personal accomplishment provide new insight into the temporal pattern of burnout when it is measured over more than two time-points and for longer than a few weeks.
Psychological distress also changed over time in these hospital-based workers. As with emotional exhaustion, psychological distress was higher in nurses than in other healthcare professionals at each time point. Rates of psychological distress above the cut-off used in this study are clinically meaningful, because they indicate likely serious mental illness [37]. Thus, it is concerning that the case rate of high psychological distress was 10.2, 17.2, 21.3, and 13.1% in nurses at the four measurement points. Although temporal patterns of psychological distress appeared more variable than the patterns of burnout, inspection of Fig. 2 indicates that psychological distress was not monotonically rising in any occupational group.
The levels and patterns of emotional exhaustion and psychological distress measured in this hospital-based cohort raise concern for both the well-being of hospital-based healthcare workers and for the resilience of the healthcare system. Broad surveys of healthcare professionals in the same region during the COVID-19 pandemic indicate not only high rates of stress and burnout, but also that 43% of nurses surveyed were considering leaving healthcare work, and that this consideration was linked to feelings of high stress [49, 50]. While in other contexts the intention to leave one’s profession does not necessarily translate into action, multiple media reports of emergency department closures, cancelled surgeries due to understaffing, and a “signing bonus” for new emergency department nursing hires, indicate that pandemic-related workforce shortages are emerging [51–55]. This may be due to a vicious cycle of workplace conditions in which understaffing and increased workload are both a cause and consequence of high levels of emotional exhaustion, depersonalization, and psychological distress, as workers choose other alternatives [41].
Recognition of the mental health costs of healthcare work during the pandemic, and the related threat to the healthcare workforce, have led to recommendations for interventions to support healthcare workers that can be implemented at the level of healthcare systems and organizations, supplemented by individual [41]. Recommended interventions have included limiting shift lengths, maximizing scheduling flexibility, ensuring adequate training for unfamiliar tasks, providing support for moral distress, and promoting effective authentic leadership [41].
Our study’s finding that lower age and, by implication, less experience in healthcare, is associated with greater emotional exhaustion and psychological distress is consistent with numerous previous studies [27, 39, 56, 57]. It is also relevant that younger adults may be more likely to have children at home, which is known to have added stress during the pandemic [33]. Special efforts to support trainees and new graduates may include transition to practice programs that include formal teaching and mentorship over several months [58]. This consideration is especially relevant because widespread healthcare workforce shortages may lead to increases in training positions for healthcare professionals in order to increase the size of the pool of workers, leading to a younger healthcare workforce and a relative loss of senior mentors.
Our finding that rates of both burnout and psychological distress rise and fall in a pattern that is possibly attributable to changes in community-level and organization-level stressors is a pattern that suggests healthcare workers are resilient in spite of substantial adversity. Further research is required to identify factors that may promote faster and more complete recovery.
The strengths of this study include its prospective measurement of psychological distress and burnout with validated instruments over a one-year period in a single cohort of healthcare workers and its relatively high retention rate considering the extraordinary circumstances of hospital work during this time. It is also a strength that the survey extended to all workers and learners in the hospital, not just those in regulated professions. Although we consider retaining 76% of participants over four survey waves in 1 year to be a strength, the loss of 24% of the cohort nonetheless introduces the possibility that non-participation results in biases. Several aspects of the study may limit generalizability including that it did not using a sampling strategy that would ensure a representative sample, evidence that psychological indices (i.e. burnout) differ in participants who completed all four surveys and those who did not, its setting in an urban teaching hospital, and high rates of vaccination among healthcare workers after the second survey. Despite enrolling participants based on their willingness to participate, the distribution of occupations and demographic measures suggest that most occupational groups are represented among the survey’s participants. A further limitation is that classifying heterogeneous occupational roles into four occupational groups does not attend to differences in the impact of the pandemic between roles that are sorted together.
Conclusions
In this cohort, neither emotional exhaustion nor psychological distress was rising monotonically, which provides hope that the negative mental health consequences of working in healthcare during the COVID-19 pandemic may improve as occupational stressors diminish. The depersonalization dimension of burnout, however, was found to rise consistently from one time point to the next. Burnout and psychological distress were consistently related to occupational role and were highest in nurses. Although emotional exhaustion improved as the case rate of COVID-19 decreased, rates of high emotional exhaustion remained much higher than was typically measured in hospital-based healthcare workers prior to the pandemic.
These results indicate that ongoing monitoring of healthcare workers’ mental health is warranted to determine the rate of recovery of burnout and distress as the COVID-19 pandemic recedes. Attention to organizational and individual interventions to support healthcare workers to maintain the resilience of the health care system continues to be important.
Acknowledgements
Not applicable.
Abbreviations
- ANOVA
Analysis of variance
- COVID-19
Coronavirus disease
Authors’ contributions
RGM, JJH, LPJ, LG, JJ, AK, CAL, LAW designed the study. RGM and NDH analyzed the data. All authors contributed to the interpretation of the data, provided critical feedback, and read and approved the final manuscript.
Funding
This work was funded by a CIHR Canadian 2019 Novel Coronavirus (COVID-19) Rapid Research Grant (FRN 170642).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
All participants provided consent to participate and the study was approved by the Sinai Health Research Ethics Board.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . Novel Coronavirus 2019 Interactive Timeline. Vol. 2019. 2021. [Google Scholar]
- 2.Worldometers . Worldometers Coronavirus. Vol. 2021. 2021. [Google Scholar]
- 3.Shaukat N, Ali DM, Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emerg Med. 2020;13(1):40. doi: 10.1186/s12245-020-00299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lasalvia A, Amaddeo F, Porru S, Carta A, Tardivo S, Bovo C, et al. Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: a cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open. 2021;11(1):e045127. doi: 10.1136/bmjopen-2020-045127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salari N, Khazaie H, Hosseinian-Far A, Ghasemi H, Mohammadi M, Shohaimi S, et al. The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: a systematic review and meta-analysis. Global Health. 2020;16(1):92. doi: 10.1186/s12992-020-00620-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dall’Ora C, Griffiths P, Ball J, Simon M, Aiken LH. Association of 12 h shifts and nurses’ job satisfaction, burnout and intention to leave: findings from a cross-sectional study of 12 European countries. BMJ Open. 2015;5(9):e008331. doi: 10.1136/bmjopen-2015-008331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall LH, Johnson J, Watt I, Tsipa A, O’Connor DB. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. PLoS One. 2016;11(7):e0159015. doi: 10.1371/journal.pone.0159015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dewa CS, Loong D, Bonato S, Thanh NX, Jacobs P. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res. 2014;14:325. doi: 10.1186/1472-6963-14-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grossman Z, Chodick G, Kushnir T, Cohen HA, Chapnick G, Ashkenazi S. Burnout and intentions to quit the practice among community pediatricians: associations with specific professional activities. Isr J Health Policy Res. 2019;8(1):2. doi: 10.1186/s13584-018-0268-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 12.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 13.Jun J, Ojemeni MM, Kalamani R, Tong J, Crecelius ML. Relationship between nurse burnout, patient and organizational outcomes: Systematic review. Int J Nurs Stud. 2021;119:103933. doi: 10.1016/j.ijnurstu.2021.103933. [DOI] [PubMed] [Google Scholar]
- 14.Azam K, Khan A, Alam MT, Toqeer M. Introduction causes and adverse impact of physician burnout: a systematic review. J Coll Physicians Surg Pak. 2017;27(8):495–501. [PubMed] [Google Scholar]
- 15.MacPhee M, Dahinten VS, Havaei F. The Impact of Heavy Perceived Nurse Workloads on Patient and Nurse Outcomes. Adm Sci. 2017;7(1):7. doi: 10.3390/admsci7010007. [DOI] [Google Scholar]
- 16.Phillips C. Relationships between workload perception, burnout, and intent to leave among medical-surgical nurses. Int J Evid Based Healthc. 2020;18(2):265–273. doi: 10.1097/XEB.0000000000000220. [DOI] [PubMed] [Google Scholar]
- 17.Melnick ER, Dyrbye LN, Sinsky CA, Trockel M, West CP, Nedelec L, et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among US Physicians. Mayo Clin Proc. 2020;95(3):476–487. doi: 10.1016/j.mayocp.2019.09.024. [DOI] [PubMed] [Google Scholar]
- 18.Liu W, Zhao S, Shi L, Zhang Z, Liu X, Li L, et al. Workplace violence, job satisfaction, burnout, perceived organisational support and their effects on turnover intention among Chinese nurses in tertiary hospitals: a cross-sectional study. BMJ Open. 2018;8(6):e019525. doi: 10.1136/bmjopen-2017-019525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Havaei F, Astivia OLO, MacPhee M. The impact of workplace violence on medical-surgical nurses’ health outcome: A moderated mediation model of work environment conditions and burnout using secondary data. Int J Nurs Stud. 2020;109:103666. doi: 10.1016/j.ijnurstu.2020.103666. [DOI] [PubMed] [Google Scholar]
- 20.Yoon HS, Sok SR. Experiences of violence, burnout and job satisfaction in Korean nurses in the emergency medical centre setting. Int J Nurs Pract. 2016;22(6):596–604. doi: 10.1111/ijn.12479. [DOI] [PubMed] [Google Scholar]
- 21.Kok N, van Gurp J, Teerenstra S, van der Hoeven H, Fuchs M, Hoedemaekers C, et al. Coronavirus Disease 2019 Immediately Increases Burnout Symptoms in ICU Professionals: A Longitudinal Cohort Study. Crit Care Med. 2021;49(3):419–427. doi: 10.1097/CCM.0000000000004865. [DOI] [PubMed] [Google Scholar]
- 22.Sriharan A, West K, Almost J, Hamza A. COVID-19-Related Occupational Burnout and Moral Distress among Nurses: A Rapid Scoping Review. Nurs Leadersh (Toronto, Ont) 2021;34(1):7–19. doi: 10.12927/cjnl.2021.26459. [DOI] [PubMed] [Google Scholar]
- 23.Morgantini LA, Naha U, Wang H, Francavilla S, Acar Ö, Flores JM, et al. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PLOS ONE. 2020;15(9):e0238217. doi: 10.1371/journal.pone.0238217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li Y, Scherer N, Felix L, Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLOS ONE. 2021;16(3):e0246454. doi: 10.1371/journal.pone.0246454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Batra K, Singh TP, Sharma M, Batra R, Schvaneveldt N. Investigating the Psychological Impact of COVID-19 among Healthcare Workers: A Meta-Analysis. Int J Environ Res Public Health. 2020;17(23):1–33. doi: 10.3390/ijerph17239096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lou NM, Montreuil T, Feldman LS, Fried GM, Lavoie-Tremblay M, Bhanji F, et al. Nurses’ and Physicians’ Distress, Burnout, and Coping Strategies During COVID-19: Stress and Impact on Perceived Performance and Intentions to Quit. J Contin Educ Health Prof. 2022;42(1):e44–e52. doi: 10.1097/CEH.0000000000000365. [DOI] [PubMed] [Google Scholar]
- 27.Jalili M, Niroomand M, Hadavand F, Zeinali K, Fotouhi A. Burnout among healthcare professionals during COVID-19 pandemic: a cross-sectional study. Int Arch Occup Environ Health. 2021;94(6):1345–1352. doi: 10.1007/s00420-021-01695-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA. 2018;320(11):1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Canadas-De la Fuente GA, Gomez-Urquiza JL, Ortega-Campos EM, Canadas GR, Albendin-Garcia L, de la Fuente-Solana EI. Prevalence of burnout syndrome in oncology nursing: A meta-analytic study. Psychooncology. 2018;27(5):1426–1433. doi: 10.1002/pon.4632. [DOI] [PubMed] [Google Scholar]
- 31.Gomez-Urquiza JL, de la Fuente-Solana EI, Albendin-Garcia L, Vargas-Pecino C, Ortega-Campos EM, Canadas-De la Fuente GA. Prevalence of Burnout Syndrome in Emergency Nurses: A Meta-Analysis. Crit Care Nurse. 2017;37(5):e1–e9. doi: 10.4037/ccn2017508. [DOI] [PubMed] [Google Scholar]
- 32.Chen S, Bonanno GA. Psychological adjustment during the global outbreak of COVID-19: A resilience perspective. Psychol Trauma. 2020;12(S1):S51–S54. doi: 10.1037/tra0000685. [DOI] [PubMed] [Google Scholar]
- 33.Maunder RG, Heeney ND, Kiss A, Hunter JJ, Jeffs LP, Ginty L, et al. Psychological impact of the COVID-19 pandemic on hospital workers over time: Relationship to occupational role, living with children and elders, and modifiable factors. Gen Hosp Psychiatry. 2021;71:88–94. doi: 10.1016/j.genhosppsych.2021.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maslach C, Jackson S, Leiter M. Maslach Burnout Inventory Manual. Consulting Psychologists Press; 1996. [Google Scholar]
- 35.Staples LG, Dear BF, Gandy M, Fogliati V, Fogliati R, Karin E, et al. Psychometric properties and clinical utility of brief measures of depression, anxiety, and general distress: The PHQ-2, GAD-2, and K-6. Gen Hosp Psychiatry. 2019;56:13–18. doi: 10.1016/j.genhosppsych.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 36.Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 37.Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, et al. Screening for Serious Mental Illness in the General Population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 38.Public Health Ontario . Ontario COVID-19 Data Tool | Public Health Ontario. 2022. [Google Scholar]
- 39.Pulcrano M, SRT E, Sosin M. Quality of Life and Burnout Rates Across Surgical Specialties: A Systematic Review. JAMA Surg. 2016;151(10):970–978. doi: 10.1001/jamasurg.2016.1647. [DOI] [PubMed] [Google Scholar]
- 40.Garrosa E, Moreno-Jiménez B, Liang Y, González JL. The relationship between socio-demographic variables, job stressors, burnout, and hardy personality in nurses: An exploratory study. Int J Nurs Stud. 2008;45(3):418–427. doi: 10.1016/j.ijnurstu.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 41.Maunder RG, Heeney ND, Strudwick G, Shin HD, O’Neill B, Young N, et al. Burnout in Hospital-Based Healthcare Workers during COVID-19. 2021. [Google Scholar]
- 42.Smallwood N, Karimi L, Bismark M, Putland M, Johnson D, Dharmage S, et al. High levels of psychosocial distress among Australian frontline healthcare workers during the COVID-19 pandemic: a cross-sectional survey. Gen Psychiatr. 2021;34(5):e100577. doi: 10.1136/gpsych-2021-100577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Melnyk B, Hsieh A, Tan A, Teall A, Weberg D, Jun J, et al. Associations Among Nurses’ Mental/Physical Health, Lifestyle Behaviors, Shift Length, and Workplace Wellness Support During COVID-19: Important Implications for Health Care Systems. Nurs Adm Q. 2021;Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 44.Kabunga A, Okalo P. Prevalence and predictors of burnout among nurses during COVID-19: a cross-sectional study in hospitals in central Uganda. BMJ Open. 2021;11:54284. doi: 10.1136/bmjopen-2021-054284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Khan N, Palepu A, Dodek P, Salmon A, Leitch H, Ruzycki S, et al. Cross-sectional survey on physician burnout during the COVID-19 pandemic in Vancouver, Canada: the role of gender, ethnicity and sexual orientation. BMJ Open. 2021;11(5):e050380. doi: 10.1136/bmjopen-2021-050380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lim KHJ, Murali K, Kamposioras K, Punie K, Oing C, O’Connor M, et al. The concerns of oncology professionals during the COVID-19 pandemic: results from the ESMO Resilience Task Force survey II. ESMO Open. 2021;6(4):100199. doi: 10.1016/j.esmoop.2021.100199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kelker H, Yoder K, Musey P, Jr, Harris M, Johnson O, Sarmiento E, et al. Prospective study of emergency medicine provider wellness across ten academic and community hospitals during the initial surge of the COVID-19 pandemic. BMC Emerg Med. 2021;21(1):36. doi: 10.1186/s12873-021-00425-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dionisi T, Sestito L, Tarli C, Antonelli M, Tosoni A, D’Addio S, et al. Risk of burnout and stress in physicians working in a COVID team: A longitudinal survey. Int J Clin Pract. 2021;75(11):e14755. doi: 10.1111/ijcp.14755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ontario Medical Association . Healing the Healers: System-Level Solutions to Physician Burnout Recommendations of the Ontario Medical Association Burnout Task Force. 2021. [Google Scholar]
- 50.Registered Nurses Association of Ontario . Work and Wellbeing Survey Results. 2021. [Google Scholar]
- 51.Staff shortages at 2 N.B. hospitals lead to closures of labour and obstetrics units | CBC News. [cited 2021 Oct 31]. Available from: https://www.cbc.ca/news/canada/new-brunswick/hospital-labour-obstetrics-new-brunswick-1.6146501
- 52.Signing bonuses are a sign of the times as desperate hospitals seek nurses | Ottawa Citizen. [cited 2021 Oct 31]. Available from: https://ottawacitizen.com/news/local-news/signing-bonuses-are-a-sign-of-the-times-as-desperate-hospitals-seek-nurses
- 53.Another Quebec ER had to shut down because of a lack of nurses, who are exhausted | CBC News. [cited 2021 Oct 31]. Available from: https://www.cbc.ca/news/canada/montreal/suroit-hospital-er-closes-overnight-1.6178786
- 54.Elective surgeries cancelled in Calgary, Fort Macleod emergency room closed as COVID-19 surge continues | CTV News. [cited 2021 Oct 31]. Available from: https://calgary.ctvnews.ca/elective-surgeries-cancelled-in-calgary-fort-macleod-emergency-room-closed-as-covid-19-surge-continues-1.5578056
- 55.Nova Scotia Health to close some surgery beds, redeploy nurses to areas with critical needs | CBC News. [cited 2021 Oct 31]. Available from: https://www.cbc.ca/news/canada/nova-scotia/health-care-nurses-emergency-department-staffing-1.6151994
- 56.Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. J Adv Nurs. 2021;77(8):3286–3302. doi: 10.1111/jan.14839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Abdelhafiz AS, Ali A, Ziady HH, Maaly AM, Alorabi M, Sultan EA. Prevalence, Associated Factors, and Consequences of Burnout Among Egyptian Physicians During COVID-19 Pandemic. Front Public Health. 2020;0:864. doi: 10.3389/fpubh.2020.590190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Brook J, Aitken L, Webb R, MacLaren J, Salmon D. Characteristics of successful interventions to reduce turnover and increase retention of early career nurses: A systematic review. Int J Nurs Stud. 2019;91:47–59. doi: 10.1016/j.ijnurstu.2018.11.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.