Since its emergence in early 2020 and up until the end of May 2022, the coronavirus SARS-CoV-2 has caused more than 528 million COVID-19 cases globally, with 6.3 million deaths (∼1.2%, case fatality rate, CFR) [1,2]. Today, the risk for concurrent pandemics or the onset of future pandemics is inevitable. In fact, the history of humankind has been shaped by infectious diseases acting as independent forces of societal transformation. Zoonotic viruses represent the greatest threat impacting global health, including not only coronaviruses like the Middle East Respiratory Syndrome (MERS-CoV) [3] but also haemorrhagic fever viruses, hantaviruses, arenaviruses, arboviruses [4], and zoonotic influenza viruses [[5], [6], [7], [8]]. In addition, re-emerging conditions are also a cause of concern, particularly those comprising multiple zoonotic viruses originating from both Africa and Asia.
Amid the COVID-19 pandemic, the increasing reporting of cases of monkeypox virus infection in humans spreading through many countries outside Africa is a major reason for concern [[5], [6], [7], [8], [9], [10], [11], [12]]. Monkeypox virus is a double-stranded DNA virus of the Poxviridae family which also includes the variola virus, the causative agent of smallpox [13,14]. Cessation of vaccination against smallpox in most countries occurred after the World Health Assembly certified the eradication of Smallpox in 1980 [8]. Consequently, it is estimated that more than 70% of the world's population is no longer protected against smallpox which also conferred some indirect degree of protection against other poxviruses including monkeypox [9]. It remains to be seen what the degree of protection is in those individuals who had prior smallpox vaccination over five decades ago [15].
The monkeypox virus has two distinct genetic clades: the Central African clade (Congo Basin) and the West African clade [16]. Monkeypox, has been circulating in Africa for decades. The virus was first discovered in 1958 during synchronous outbreaks on two colonies of research monkeys [17], and the first description of monkeypox in human's dates to 1970 in the Democratic Republic of Congo (DRC). While most circulation of monkeypox occurs in Africa, there has been sporadic descriptions of cases outside Africa over the last two decades.
In 2003, the first outbreak outside of Africa was reported in the United States linked to exposure to pet prairie dogs which were housed together with Gambian pouched rats and dormice imported from Ghana [7]. The West African clade is known to have a more favourable prognosis with a CFR of less than 1% (Table 1 ). On the other hand, the Central Basin clade (Central African clade) is more lethal, with a CFR of up to 10% in unvaccinated children [12,18] (Table 1). Current genomic data from this outbreak has been made publicly available with full genomes accessible now from Belgium (https://bit.ly/3wEgQtE), Portugal (https://bit.ly/3Gd7zgz) and the USA. This multi-country outbreak most likely can be traced to a single origin, given that all sequences are clustering together within the West African clade (https://bit.ly/3Lz174F). These findings suggest very likely the exportation of the virus occurred from Nigeria in 2018 and 2019. Notably, viruses from the recent outbreak diverges a mean of 50 SNPs from those of 2018–2019, this divergence is high considering the estimated substitution rate for Orthopoxviruses (https://bit.ly/3Lz174F). Therefore, intensive genomic surveillance is still needed to rule out the origin and spread of the monkeypox virus causing this recent global outbreak.
Table 1.
Key features of smallpox and monkeypox.
| Orthopoxvirus | |
|---|---|
| Smallpox | Monkeypox |
| More infectious | Less infectious |
| Vaccines used until used up to four decades ago | No specific vaccine is available yet (cross-immunity with Smallpox vaccine) |
| Eradicated in 1980 (last known case in 1977 in Somalia) | Known circulation in Africa since 1958 (1970 first human case in DRC) |
| Similar transmission routes | |
| CFR: Variola minor: 1% Variola major: 30% |
CFR West African clade: 1% Central African clade: 10% |
Transmission of monkeypox to humans occurs mainly through contact with body fluids, skin lesions, or respiratory droplets from infected animals directly or indirectly through contaminated fomites [[14], [16], [17], [18], [19], [20]]. Monkeypox can infect a taxonomically wide range of mammalian species; however, the virus has only been isolated once from a wild animal, a Funisciurus squirrel in the DRC in 1985, and a mangabey monkey found infected in Cote d'Ivoire in 2012 [21]. The extent of viral circulation in animal populations and the range of species that may harbour the virus has not been fully established, although several lines of evidence point to rodents as major potential reservoirs [22]. However, the primary reservoir for human infection remains unknown [23]. Several epidemiological studies from the DRC have implicated squirrels (especially Funisciurus anerythrus) inhabiting agricultural areas as primary candidates to sustain viral transmission among people in nearby settlements [24]. In one environmental survey, Funisciurus spp squirrels had a higher rate of monkeypox seropositivity (24%) than other any animals tested, including Heliosciurus spp squirrels (15%) and primates (8%) [25]. A subsequent seroprevalence study conducted to investigate the DRC outbreak back in February 1997, showed even higher positivity rates amongst these squirrels (39–50% in Funisciurus spp and 50% in Heliosciurus spp squirrels). In addition, 16% of Gambian giant rats tested in this study demonstrated serological evidence of MPV exposure [26].
The clinical manifestations of monkeypox resembles that of smallpox [16] including non-specific clinical features such as fever, chills, myalgia, headache, lethargy, and lymphadenopathy followed by a vesiculo-pustular rash, with an incubation period ranging from 5 to 21 days [[26], [27], [28], [29]]. Even though the incubation period for this current outbreak has not been established, its often long period of incubation suggests that initial exposure events may have occurred in early April 2022. The differential diagnosis of monkeypox includes a variety of infections such as Rickettsialpox caused by Rickettsia akari, smallpox, measles, chickenpox, and syphilis, and others, depending also on the local epidemiology (e.g. Peruvian warts in some Latin American countries, or Buruli ulcer in Africa) [[29], [30], [31], [32]]. A definitive diagnosis of monkeypox can only be established by laboratory testing. Therefore, the World Health Organization (WHO) recommends that the optimal specimens for diagnosis include direct sampling from lesions: smears of exudate from vesicular lesions or scabs stored in a dry, sterile, non-viral transport medium and cold test tube [16].
Endemic cases of monkeypox are common in Nigeria. According to the latest report from the Nigerian Centre for Disease Control (NCDC), the country recorded 558 cases of monkeypox and eight deaths between 2017 and 2022 [31]. The recent geographic spread of the ongoing monkeypox outbreak has expanded beyond the forests of central Africa, where patients were initially found, to other parts of the world [28]. The impact of monkeypox has been highlighted by the recent registration of 56 cases in the United Kingdom, 41 in Spain and 37 confirmed cases in Portugal, among other countries [29]. The alert of this zoonotic virus has caught by surprise even the European Centre for Disease Prevention and Control (ECDC), which until the weekend did not count monkeypox as one of the potential threats within the European Union, but only observed the evolution of the alert in the British Isles.
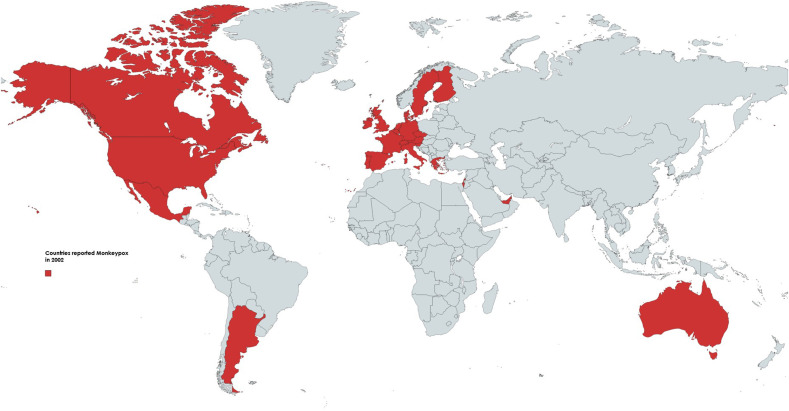
As of May 29, 2022, multiple countries in Europe, in addition to United Kingdom, Spain and Portugal, have reported monkeypox (Fig. 1 ). In North America, Canada and United States of America, have confirmed cases. Beyond Europe, Israel and Australia have also notified suspected and confirmed cases, with confirmed cases in Mexico and Argentina, and suspected cases in Ecuador and Bolivia (Fig. 1), for a total of 506 cases, 421 of them confirmed (83%). As expected, Latin America has been also affected with cases [[33], [34]].
Fig. 1.
Geographical distribution of confirmed and suspected cases of monkeypox in non-endemic countries in 2022, up to May 29.
The classic mode of transmission of this infection relies on exposure to live or dead animals through hunting or handling bush meat. The animal reservoir of the monkeypox virus is unknown; however, there is evidence that places native African rodents as a potential source, which may explain the spread of the disease outside this continent. Since the first reported case in Zaire in 1970, 95% of the informed cases to date are from the DRC. Since the 2000s, there has been an increased number of monkeypox cases throughout the New World and outbreaks associated with contact with African rodents sold as pets. One of the factors related to the gradual increase in cases is the cessation of routine vaccination against Smallpox, which was mandatory until 1972 and ceased after its eradication in 1980 [32]. An interesting aspect about the current outbreak relates to the fact that disease clusters are known to include high risk groups like men who have sex with men (MSM). This is important from a disease dynamics standpoint for several reasons: 1. it could explain why despite the relatively inefficient transmission of monkeypox, so many cases are being reported in such a broad geographical extension. 2. Provides evidence on close contact as the potential source of transmission and 3. Argue in favour of a possible sexual link for all these seemingly unconnected outbreaks throughout MSM communities. Naturally, its differential diagnosis would be challenging, including other exanthematic febrile diseases, including Smallpox, Measles, Chickenpox, and Syphilis, depending on the local epidemiology (e.g. Peruvian warts in some Latin American countries, or Buruli ulcer in Africa) [35].
Predicting the ongoing spread of monkeypox to other geographic settings is challenging. Monkeypox is a significant health concern for people living in endemic regions across Africa where virus circulation is confirmed. However, it is also a global health security issue, and appropriate and effective interventions such as active surveillance and contact tracing are urgently needed to prevent delayed identification of cases and implementation of public health measures [[16], [17], [18]]. All efforts should be now focused towards containment of cases in order to prevent the virus entering other human networks (healthcare personal) which is still facing the challenges imposed by the current SARS-CoV-2 pandemic. As for monkeypox, vigilance most be doubled for other viruses circulating in wild animal populations, which can sporadically spillover to human populations, as it most likely occurred with SARS-CoV-2 [36]. Prevention and control of these emerging zoonoses depend upon a reduction of exposure to and conservation of both wildlife in their natural habitats.
The general recommendation for preventing monkeypox virus transmission includes the use of the smallpox vaccine [37]. This vaccine which confers apparently 85% of cross-protection against monkeypox remains to face the challenge of these ongoing outbreaks. Although there are no specific treatments for monkeypox, the Centers for Disease Control (CDC) recommends smallpox vaccine as post-exposure prophylaxis for high-risk contacts within 4 days and up to 14 days of contact, but if given between 4 and 14 days after date of exposure, vaccination may reduce the symptoms of disease, but not prevent the disease [38]. In addition to smallpox vaccine, immune globulin is available and can be used as prophylaxis for severely immunocompromised patients, although the benefit still remains unclear [39]. Antiviral drugs approved to treat smallpox including tecovirimat and brincidofovir, can be potentially deployed for its use on treating monkeypox [40].
Currently, residents and travellers from endemic areas and where monkeypox cases are currently being reported should maintain contact precautions and health personnel who care, especially for men who have sex with men which may indicate a potential risk of sexual transmission [41]. However, there may be other factors related to the predilection of cases among this specific at-risk population that require further epidemiologic assessments. Indeed, given the significant knowledge gap on monkeypox [42], there is a clear need to increase the previous low level of global scientific research that has been done on this reemerging zoonosis, as recently demonstrated [43].
The SARS, Influenza, MERS, and SARS-CoV-2/COVID-19 pandemics of the 21st century demonstrate that there is a perennial risk of pandemics. While we cannot predict their occurrence, there is an urgent need to decrease vulnerability to become infected with any of these pathogens. Responding to the current outbreak of monkeypox involving many countries requires global collaboration and the institution of best practices learned during the current SARS-CoV-2 pandemic.
Acknowledgments
To Juan E Ludert (Department of Infectomics and Molecular Pathogenesis, Center for Research and Advanced Studies (CINVESTAV-IPN), Mexico City, 07360, Mexico), Tomas Orduna (Hospital de Infecciosas F. Muñíz, Buenos Aires, Argentina), and Mario Massana Wilson (Argentina), for their critical comments to the manuscript during proofs correction.
References
- 1.Rodriguez-Morales AJ, Cardona-Ospina JA, Gutierrez-Ocampo E, Villamizar-Pena R, Holguin-Rivera Y, Escalera-Antezana JP, Alvarado-Arnez LE, Bonilla-Aldana DK, Franco-Paredes C, Henao-Martinez AF, Paniz-Mondolfi A, Lagos-Grisales GJ, Ramirez-Vallejo E, Suarez JA, Zambrano LI, Villamil-Gomez WE, Balbin-Ramon GJ, Rabaan AA, Harapan H, Dhama K, Nishiura H, Kataoka H, Ahmad T, Sah R; Latin American Network of Coronavirus Disease 2019-COVID-19 Research (LANCOVID-19). Electronic address: https://www.lancovid.org. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 2020 Mar-Apr;34:101623. doi: 10.1016/j.tmaid.2020.101623. Epub 2020 Mar 13. PMID: 32179124; PMCID: PMC7102608. [DOI] [PMC free article] [PubMed]
- 2.Dhama K., Khan S., Tiwari R., Sircar S., Bhat S., Malik Y.S., Singh K.P., Chaicumpa W., Bonilla-Aldana D.K., Rodriguez-Morales A.J. Coronavirus disease 2019-COVID-19. Clin Microbiol Rev. 2020 Jun 24;33(4) doi: 10.1128/CMR.00028-20. 20. PMID: 32580969; PMCID: PMC7405836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rabaan A.A., Al-Ahmed S.H., Sah R., Alqumber M.A., Haque S., Patel S.K., Pathak M., Tiwari R., Yatoo M.I., Haq A.U., Bilal M., Dhama K., Rodriguez-Morales A.J. MERS-CoV: epidemiology, molecular dynamics, therapeutics, and future challenges. Ann Clin Microbiol Antimicrob. 2021 January 18;20(1):8. doi: 10.1186/s12941-020-00414-7. PMID: 33461573; PMCID: PMC7812981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reed K.D. 2018. p. 95729. (Viral zoonoses. Reference module in biomedical sciences). B978-0-12-801238-3. 5. [DOI] [Google Scholar]
- 5.Bonilla-Aldana D.K., Aguirre-Florez M., Villamizar-Peña R., Gutiérrez-Ocampo E., Henao-Martínez J.F., Cvetkovic-Vega A., Dhama K., Rabaan A., Sah R., Rodriguez-Morales A.J., Schlagenhauf P., Paniz-Mondolfi A. After SARS-CoV-2, will H5N6 and other influenza viruses follow the pandemic path? Infez Med. 2020 Dec 1;28(4):475–485. PMID: 33257621. [PubMed] [Google Scholar]
- 6.Rodriguez-Morales A.J., Bonilla-Aldana D.K., Paniz-Mondolfi A.E. Concerns about influenza H5N8 outbreaks in humans and birds: Facing the next airborne pandemic? Travel Med Infect Dis. 2021;41 doi: 10.1016/j.tmaid.2021.102054. PMID: 33823287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Monkeypox W.H.O. https://www.who.int/news-room/fact-sheets/detail/monkeypox
- 8.WHO WHO commemorates the 40th anniversary of smallpox eradication. https://www.who.int/es/news/item/13-12-2019-who-commemorates-the-40th-anniversary-of-smallpox-eradication
- 9.Simpson K., Heymann D., Brown C.S., Edmunds W.J., Elsgaard J., Fine P., et al. Human Monkeypox – after 40 years, an unintended consequence of smallpox eradication. Vaccine. 2020;38:5077–5081. doi: 10.1016/J.VACCINE.2020.04.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yinka-Ogunleye A., Aruna O., Dalhat M., Ogoina D., McCollum A., Disu Y., et al. Outbreak of human Monkeypox in Nigeria in 2017–18: a clinical and epidemiological report. Lancet Infect Dis. 2019;19:872–879. doi: 10.1016/S1473-3099(19)30294-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berthet N., Descorps-Declère S., Besombes C., Curaudeau M., Nkili Meyong A.A., Selekon B., et al. Genomic history of human monkey pox infections in the Central African Republic between 2001 and 2018. Sci Rep. 2021:11. doi: 10.1038/S41598-021-92315-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moore M., Zahra F. Monkeypox. StatPearls. 2022 https://www.ncbi.nlm.nih.gov/books/NBK574519/ [Google Scholar]
- 13.Petersen E., Kantele A., Koopmans M., Asogun D., Yinka-Ogunleye A., Ihekweazu C., et al. Human monkeypox: epidemiologic and clinical characteristics, diagnosis, and prevention. Infect Dis Clin. 2019;33:1027–1043. doi: 10.1016/J.IDC.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alakunle E., Moens U., Nchinda G., Okeke M.I. Monkeypox virus in Nigeria: infection biology, epidemiology, and evolution. Viruses. 2020;12 doi: 10.3390/V12111257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rezza G. Emergence of human monkeypox in West Africa. Lancet Infect Dis. 2019;19:797–799. doi: 10.1016/S1473-3099(19)30281-6. [DOI] [PubMed] [Google Scholar]
- 16.WHO . 2022. Multi-country monkeypox outbreak in non-endemic countries. [Google Scholar]
- 17.Arita I., Gispen R., Kalter S.S., Wah L.T., Marennikova S.S., Netter R., Tagaya I. Outbreaks of monkeypox and serological surveys in nonhuman primates. Bull World Health Organ. 1972;46(5):625–631. PMID: 4340222; PMCID: PMC2480785. [PMC free article] [PubMed] [Google Scholar]
- 18.Sklenovská N., van Ranst M. Emergence of monkeypox as the most important orthopoxvirus infection in humans. Front Public Health. 2018;6 doi: 10.3389/FPUBH.2018.00241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peter O.J., Kumar S., Kumari N., Oguntolu F.A., Oshinubi K., Musa R. Transmission dynamics of Monkeypox virus: a mathematical modelling approach. Modeling Earth Systems and Environment. 2021;1:1. doi: 10.1007/S40808-021-01313-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heymann D.L., Simpson K. The evolving epidemiology of human monkeypox: questions still to Be answered. J Infect Dis. 2021;223:1839–1841. doi: 10.1093/INFDIS/JIAB135. [DOI] [PubMed] [Google Scholar]
- 21.Radonić A., Metzger S., Dabrowski P.W., Couacy-Hymann E., Schuenadel L., Kurth A., Mätz-Rensing K., Boesch C., Leendertz F.H., Nitsche A. Fatal monkeypox in wild-living sooty mangabey, Côte d'Ivoire, 2012. Emerg Infect Dis. 2014 Jun;20(6):1009–1011. doi: 10.3201/eid2006.13-1329. PMID: 24857667; PMCID: PMC4036778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reynolds M.G., Carroll D.S., Karem K.L. Factors affecting the likelihood of Monkeypox's emergence and spread in the post-smallpox era. Curr Opin Virol. 2012 Jun;2(3):335–343. doi: 10.1016/j.coviro.2012.02.004. Epub 2012 March 6. PMID: 22709519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.WHO The current status of human Monkeypox: memorandum from a WHO meeting. Bull World Health Organ. 1984;62(5):703–713. PMID: 6096036; PMCID: PMC2536211. [PMC free article] [PubMed] [Google Scholar]
- 24.Khodakevich L., Jezek Z., Kinzanzka K. Isolation of monkeypox virus from wild squirrel infected in nature. Lancet. 1986;1:98–99. doi: 10.1016/S0140-6736(86)90748-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khodakevich L., Jezek Z., Messinger D. Monkeypox virus: ecology and public health significance. Bull World Health Organ. 1988;66(6):747–752. PMID: 2853010; PMCID: PMC2491157. [PMC free article] [PubMed] [Google Scholar]
- 26.Hutin Y.J., Williams R.J., Malfait P., Pebody R., Loparev V.N., Ropp S.L., Rodriguez M., Knight J.C., Tshioko F.K., Khan A.S., Szczeniowski M.V., Esposito J.J. Outbreak of human monkeypox, democratic Republic of Congo, 1996 to 1997. Emerg Infect Dis. 2001 May-Jun;7(3):434–438. doi: 10.3201/eid0703.010311. PMID: 11384521; PMCID: PMC2631782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bunge E.M., Hoet B., Chen L., Lienert F., Weidenthaler H., Baer L.R., et al. The changing epidemiology of human monkeypox-A potential threat? A systematic review. PLoS Neglected Trop Dis. 2022:16. doi: 10.1371/JOURNAL.PNTD.0010141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ihekweazu C., Yinka-Ogunleye A., Lule S., Ibrahim A. Importance of epidemiological research of Monkeypox: is incidence increasing? 2020. 18:389-392. [DOI] [PMC free article] [PubMed]
- 29.Grant R., Nguyen L.B.L., Breban R. Modelling human-to-human transmission of Monkeypox. Bull World Health Organ. 2020;98:638. doi: 10.2471/BLT.19.242347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Viruela del mono en España | Ascienden a 23 los casos de viruela no humana confirmados en España | Salud. https://www.elmundo.es/ciencia-y-salud/salud/2022/05/20/628721ab5b2dae00216b3286-directo.html (accessed May 19, 2022)
- 31.Nigeria Centre for Disease Control https://ncdc.gov.ng/diseases/sitreps/?cat=8&name=An%20Update%20of%20Monkeypox%20Outbreak%20in%20Nigeria (accessed May 19, 2022)
- 32.Nalca A., Rimoin A.W., Bavari S., Whitehouse C.A. Reemergence of Monkeypox: prevalence, diagnostics, and countermeasures. Clin Infect Dis. 2005 December 15;41(12):1765–1771. doi: 10.1086/498155.Epub.2005.November.11. PMID: 16288402. [DOI] [PubMed] [Google Scholar]
- 33.Bonilla-Aldana DK, Thormann M, Lopardo G, Rodriguez-Morales AJ. Monkeypox virus – Would it arrive in Latin America? Rev Panam Enf Inf. 2022;5(1):e1. [Google Scholar]
- 34.Cimerman S, Chebabo A, Arns da Cunha C, Barbosa AN, Rodríguez-Morales AJ. Human Monkeypox Preparedness in Latin America – Are we ready for the next viral zoonotic disease outbreak after COVID-19? Braz J Infect Dis. 2022 doi: 10.1016/j.bjid.2022.102372. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kamimura-Nishimura K., Rudikoff D., Purswani M., Hagmann S. Dermatological conditions in international pediatric travelers: epidemiology, prevention and management. Trav Med Infect Dis. 2013 Nov-Dec;11(6):350–356. doi: 10.1016/j.tmaid.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 36.Bonilla-Aldana D.K., Jimenez-Diaz S.D., Arango-Duque J.S., Aguirre-Florez M., Balbin-Ramon G.J., Paniz-Mondolfi A., Suárez J.A., Pachar M.R., Perez-Garcia L.A., Delgado-Noguera L.A., Sierra M.A., Muñoz-Lara F., Zambrano L.I., Rodriguez-Morales A.J. Bats in ecosystems and their Wide spectrum of viral infectious potential threats: SARS-CoV-2 and other emerging viruses. Int J Infect Dis. 2021 Jan;102:87–96. doi: 10.1016/j.ijid.2020.08.050. Epub 2020 Aug 20. PMID: 32829048; PMCID: PMC7440229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Di Giulio D.B., Eckburg P.B. Human monkeypox: an emerging zoonosis. Lancet Infect Dis. 2004 Jan;4(1):15–25. doi: 10.1016/s1473-3099(03)00856-9. Erratum in: Lancet Infect Dis. 2004 Apr;4(4):251. PMID: 14720564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.CDC Monkeypox and smallpox vaccine guidance. https://www.cdc.gov/poxvirus/monkeypox/clinicians/smallpox-vaccine.html. Access
- 39.Brown K., Leggat P.A. Human monkeypox: current state of knowledge and implications for the future. Trav Med Infect Dis. 2016 Dec 20;1(1):8. doi: 10.3390/tropicalmed1010008. PMID: 30270859; PMCID: PMC6082047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hutson C.L., Kondas A.V., Mauldin M.R., Doty J.B., Grossi I.M., Morgan C.N., Ostergaard S.D., Hughes C.M., Nakazawa Y., Kling C., Martin B.E., Ellison J.A., Carroll D.S., Gallardo-Romero N.F., Olson V.A. Pharmacokinetics and efficacy of a potential smallpox therapeutic, brincidofovir, in a lethal monkeypox virus animal model. mSphere. 2021 Feb 3;6(1) doi: 10.1128/mSphere.00927-20. 20. Erratum in: mSphere. 2021 Feb 17;6(1): PMID: 33536322; PMCID: PMC7860987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Monkeypox C.D.C. Case definition. https://www.cdc.gov/poxvirus/monkeypox/clinicians/case-definition.html. Access
- 42.Al-Tawfiq JA, Barry M, Memish ZA. International Outbreaks of Monkeypox Virus Infection with no Established travel: A public health concern with significant knowledge gap. Travel Med Infect Dis. 2022 doi: 10.1016/j.tmaid.2022.102364. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rodríguez-Morales AJ, Ortiz-Martínez Y, Bonilla-Aldana DK. What has been researched about Monkeypox? A bibliometric analysis of an old zoonotic virus causing global concern. New Microbes New Infect. 2022 doi: 10.1016/j.nmni.2022.100993. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]