Abstract
Background:
People living with burn injury often face long-term physical and psychological sequelae associated with their injuries. Few studies have examined the impacts of burn injuries on long-term health and function, life satisfaction, and community integration beyond five years post-injury. The purpose of this study was to examine these outcomes up to 20 years after burn injury.
Methods:
Data from the Burn Model System National Longitudinal Database (1993–2020) was analyzed. Patient-reported outcome measures were collected at discharge (pre-injury status recall) and 5, 10, 15, and 20 years after injury. Outcomes examined were the SF-12/VR-12 Physical (PCS) and Mental Component Summaries (MCS), Satisfaction with Life Scale (SWLS), and Community Integration Questionnaire (CIQ). Trajectories were developed using linear mixed models with repeated measures of outcome scores over time, controlling for demographic and clinical variables.
Results:
The study population included 421 adult burn survivors with a mean age of 42.4 years. Lower PCS scores (worse health) were associated with longer length of hospital stay, older age at injury and greater time since injury. Similarly, lower MCS scores were associated with longer length of hospital stay, female sex, and greater time since injury. SWLS scores decrease negatively over time. Lower CIQ scores were associated with burn size and Hispanic/Latino ethnicity.
Conclusions:
Burn survivors’ physical and mental health and satisfaction with life worsened over time up to 20 years after injury. Results strongly suggest that future studies should focus on long term follow-up where clinical interventions may be necessary.
Level of Evidence:
Level 3, Prognostic
Keywords: Burn injuries, chronic conditions, long-term outcomes, patient reported outcomes
Introduction
People living with burn injuries often face long-term physical and psychological sequalae associated with their injury. These limitations may impact their functional status resulting in long-term inpatient care and physical and mental rehabilitation needs.1–6 Number of burn-related operations, hospital-acquired complications and longer hospital admissions negatively impact physical functioning and overall quality of life up to five years post injury.7–9 Further, many people living with burn injury experience physical limitations such as range of motion deficits or amputation as well as pain and impaired sleep that can affect physical and mental health long-term.10 Changes in appearance resulting from scars, contractures and amputations can impact an individual’s satisfaction with their appearance, which is associated with overall worse mental health.4 These sequelae often impact the way burn survivors interact with their family, friends, community.11
Challenges with social reintegration after burn injury may result in survivors feeling less life satisfaction as well as worse quality of life. There are several factors that affect a survivor’s ability to reintegrate into society including changes in appearance due to scarring and decreased functional status.1,3,4 Additionally, return to work is a significant milestone of recovery. Although most burn survivors do eventually return to work, factors such as burn size, contracture, and burn related amputation can delay return to work up to two years and some survivors may not return in the same capacity or the same job as before their injury.12–15
To date, few studies have examined the impact of burn injuries on long-term health, life satisfaction, and participation outcomes beyond five years from injury.9 Prior studies emphasize that people living with burn injury experience changes in quality of life over time and highlight the need for more research examining physical and psychosocial outcomes farther out from initial injury.1,3 Therefore, the purpose of this study was to examine physical and mental health, satisfaction with life, and community integration of burn survivors up to 20 years after injury.
Methods
Burn Model System National Longitudinal Database
This study used data from the Burn Model System (BMS) National Database, funded by the National Institute on Disability, Independent Living, and Rehabilitation Research. The BMS was established in 1993 as a means of exploring the long-term physical and psychosocial outcomes of people living with burn injury. Informed consent is obtained from all participants and each BMS site’s institutional review board oversees data collection. The BMS Database provides detailed sociodemographic, clinical, and long-term patient-reported outcome measures (PROMs). Demographic, clinical and outcome data are collected at hospital discharge and follow-up outcomes are collected at 5, 10, 15 and 20 years after injury.16
Current criteria for inclusion in the BMS Database are those who require autografting surgery for wound closure and meet one of the following criteria:
0–64 years of age with a burn injury ≥20% total body surface area (TBSA) OR
≥65 years of age with a burn injury ≥10% TBSA OR
Any age with a burn injury to their face/neck, hands, or feet OR
Any age with a high-voltage electrical burn injury
BMS Database enrollment criteria have changed over time and these changes are detailed at the BMS National Data and Statistical Center’s website: https://burndata.washington.edu/.
Participants who were burned between 1993 and 2016, age greater than or equal to 18 years at time of injury, and alive at discharge were included in this study. Data was collected between 1993 and 2020; this window allows for capture of 5-year follow-up data for participants injured in 2016. There are additional exclusion criteria based on database follow-up windows and protocols. Some participants did not have follow-up data because they were not due for long-term follow-up data collection. Participants that were not due for their 5-year follow-up were excluded from the study. Participants that were not yet due for their 10,15, or 20-year follow-up were included if they had data for at least one outcome measure at their previous follow-ups (5, 10, or 15 year). Given that long-term follow-up (5, 10, 15 and 20 years after injury) was added to the BMS Database in 2009–2010, existing BMS centers were required to reconsent participants to collect additional long-term data. For participants that consented to long-term follow-up, some of their data collection windows (e.g., 5,10,15 years) had already passed, so data was not collected for those prior time points. Data collection for these participants resumed at their next follow-up window and was included in this study if available. Finally, participants who were lost to follow-up, did not have data in at least one outcome measure, or those who did not consent to long-term follow-up were excluded from this study. The study population is outlined in Figure 1.
Figure 1: Flow Chart of Inclusion and Exclusion Criteria.
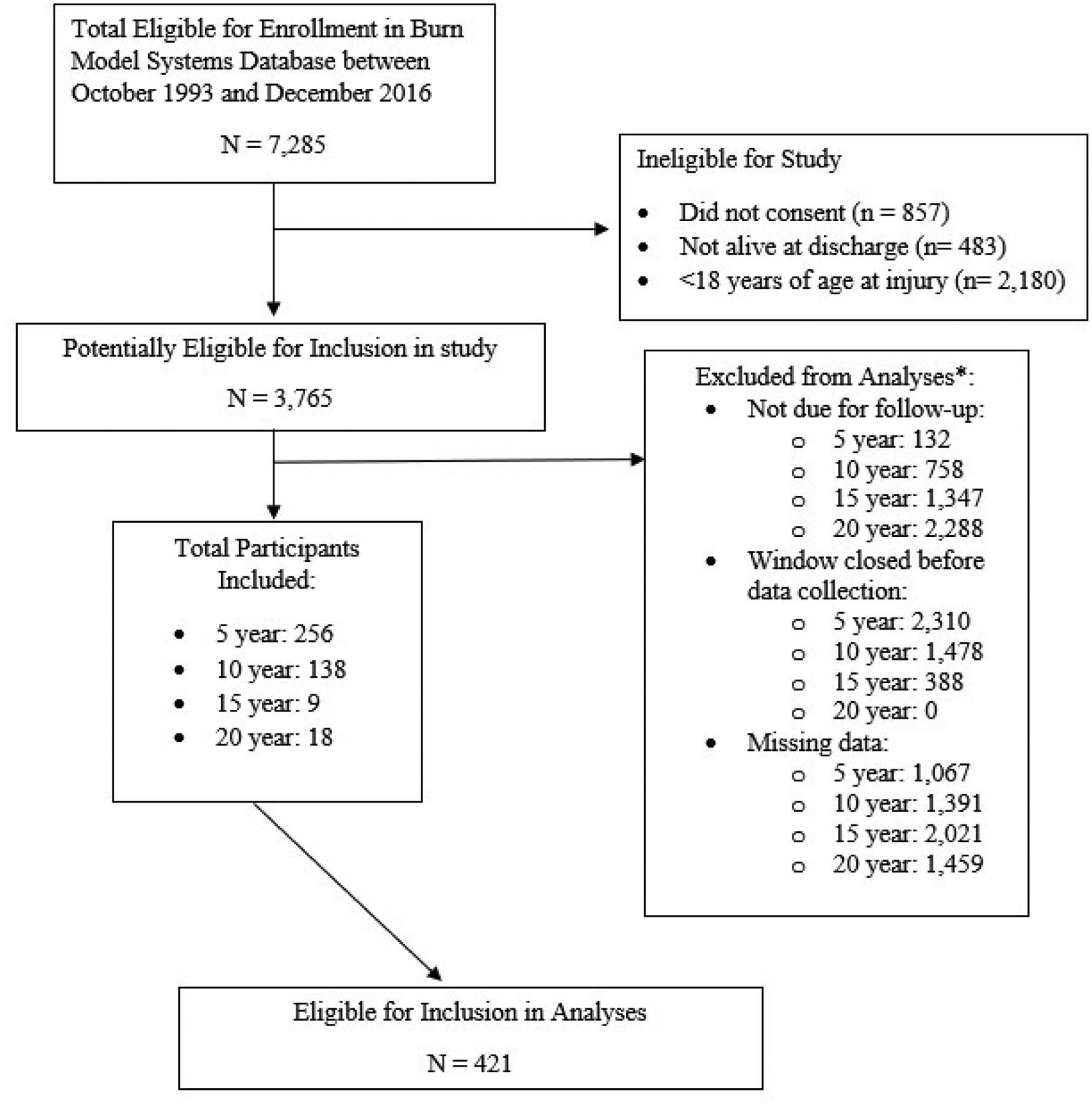
*Includes multiple observations (e.g., participants may have been eligible for 5- and 10-year data collection but not 15 or 20 year data collection). Excluded participants are calculated within each follow-up time point.
Sociodemographic and Clinical Variables
Sociodemographic and clinical information were collected for all participants at hospital discharge. Demographic variables included age, sex (male; female), race (Black or African American; Asian; White; other); ethnicity (Hispanic/Latino; non-Hispanic/Latino); and highest education level (less than bachelor’s degree; bachelor’s degree or higher). Clinical variables included burn etiology (fire/flame; other), burn size (percent TBSA), length of hospital stay, burn to critical area (head/neck, foot, hand, or perineum burn), and amputation due to burn.
Patient Reported Outcome Measures
PROMs were examined at discharge and 5, 10, 15 and 20 years after injury. The discharge survey asks participants to recall their pre-injury physical health, mental health, satisfaction with life, and social integration, which serve as the baseline.
12-Item Short Form Health Survey (SF-12) and Veterans RAND 12-Item Health Survey (VR-12)
The SF-12 and VR-12 measure physical and mental health. The BMS Database collected the SF-36 from 1997 to 2006, SF-12 from 2006 to 2015 and VR-12 since 2015.17,18 The SF-12.v2 was created as a shorter version of the SF-36 which measures physical, psychological, social functioning, and general health perceptions. SF-12 items are contained within the SF-36 and therefore for this study SF-12 scores were examined for the years the SF-36 was collected. The BMS Database currently uses an established and validated crosswalk between SF-12 scores and VR-12 scores.19 In 2015, the BMS replaced the SF-12 with the VR-12. The VR-12 demonstrated an improvement in the precision of the physical and mental summary scores using psychometric approaches for expanding the floor and ceiling of these scales, compared to the SF-12. The SF-12 and VR-12 instruments are composed of two summary scores: Physical Component Summary (PCS) and Mental Component Summary (MCS). PCS and MCS scores are weighted summaries that use factor analytic-based scores with orthogonal rotations indicating that the factors making up the domains are uncorrelated. PCS uses larger weights for physical functioning and role limitations due to physical problems. MCS is based on larger weights for items that assess role limitations due to emotional problems and mental health. PCS and MCS are standardized assessments using a t-score transformation with a mean of 50 and standard deviation of 10, normed to a national US population.18 Higher scores denote better health. Differences of 0.2 of 1 SD or 2 points are considered small, 0.5 of 1 SD or 5 points are moderate and 0.8 of 1 SD or 8 points or greater are large effect sizes.20,21
Satisfaction with Life Scale (SWLS)
The SWLS is a validated 5-item scale that measures life satisfaction and wellbeing based on social relationships, learning, and work or school. Items are scored on a 7-point Likert scale with a maximum score of 35; a score of 20 indicates equal distribution of satisfaction and dissatisfaction, higher scores indicate greater satisfaction with life.22,23 It has established reliability and has been validated in the adult burn injury population.24,25
Community Integration Questionnaire (CIQ)
The CIQ for social integration is a 5-item instrument used to measure an individual’s social integration. Scores range from 0 to 29, higher scores indicate greater social integration. This instrument has been validated in the adult burn injury population.26
Data Analysis
The sociodemographic and clinical characteristics of the sample were described by calculating means and standard deviations of continuous variables, and frequencies and proportions of categorical variables. Means and standard deviation of outcomes were examined at baseline, 5, 10, 15, and 20 years since initial injury. Score trajectories were developed for each outcome using a linear mixed model with repeated measures of scores (PCS, MCS, SWLS, and CIQ) over time, controlling for sociodemographic and clinical variables. The linear mixed model with random effects accounts for variations of baseline outcomes and score trajectories across an individual participant. To assess the representativeness of the included sample, sociodemographic and clinical characteristics for the included and excluded study population were compared. Participants were excluded if they had reached their long-term follow-up timepoint (i.e., 5, 10, 15 or 20 year) but did not provide complete data for outcome measures at those timepoints.
Three different linear mixed models were fit to identify the best trajectory model: (1) a random intercept only model, (2) a model using a random intercept and fixed slope effect, (3) a model with random intercept and slope effects. The optimal model with the lowest Akaike’s Information Criteria and Bayesian Information Criteria values, were selected for each outcome. Sociodemographic and clinical covariates were added to the optimal model. Education was not included in the trajectory model because 30% of participants were missing education information. The race categories were recoded as White vs Other with the Other category including non-White participants and missing. This coding method was applied to all other covariates to include the missing values in the “other” category. The linear mixed models rely on two parameters, intercept and slope, for the fixed effects. These models rely on less data, and therefore fewer missing values, than models with more variables and were used to test the more complex models.
The relationship between each covariate and outcome was tested, and the multivariable models were created that included all covariates. A linear mixed model was applied to describe the outcome change across time. Models used the natural log to transform the years of time since injury (5,10,15, 20 years) to reflect the observed patterns of the mean score change. Time-points were treated as continuous variables with the time since injury variable log-transformed. The plot was generated by converting the log of time into original year units. Statistically significant predictors with p-value less than 0.05 were identified. The model fitted score trajectory was generated with 95% confidence intervals to demonstrate the score change across time and the impact of covariates. Trajectories were depicted graphically using the anti-log for the log of time since injury. In the model, the age at time of injury was categorized based on tertile values. Length of hospital stay was treated as a continuous variable. In the trajectories, the outcome values were calculated based on length of hospital stay at the 25th, 50th, and 75th percentile values. To validate the significant findings 500 bootstrap samples (sample with replacement at subject level) were generated and fitted to the final model for each outcome.
This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines and a complete checklist has been uploaded as Supplemental Digital Content (SDC 1).
Results
Demographic and Clinical Variables
The study population included 421 adults burn survivors who had a mean age of 42.4 years (SD 14.5 years). The majority of the population was male (66%) and White (76%) with an average length of hospital stay of 31 days (SD 32 days) and average burn size of 22% TBSA (18.7% SD). A full description of the demographic and clinical characteristics of the study population is presented in Table 1.
Table 1:
Demographic and Clinical Variables of the Study Population (n= 421)
| Variable | Value |
|---|---|
| Age, mean years (SD) | 42.4 (14.5) |
| Male, N (%) | 277 (65.8) |
| Race, N (%) | |
| White | 321 (76.3) |
| Black | 57 (13.5) |
| Other* | 10 (2.4) |
| Missing | 33 (7.8) |
| Hispanic/Latino, N (%) | 39 (9.3) |
| Missing | 9 (2.1) |
| Highest education level, N (%) | |
| Bachelor’s degree or higher | 61 (14.5) |
| Missing | 124 (29.5) |
| Etiology, N (%) | |
| Fire/flame Injury | 247 (58.7) |
| Missing | 3 (0.7) |
| Burn size, mean % TBSA (SD) | 21.6 (18.7) |
| Burns to Critical Areas, N (%) | |
| Head/Neck Burn | 2301 (54.6) |
| Hand Burn | 3162 (75.1) |
| Foot Burn | 1563(37.1) |
| Perineum Burn | 384 (9.0) |
| Burn-related Amputation, N (%) | 325 (7.6) |
| Length of hospital stay, mean days (SD) | 31.3 (31.7) |
Other race includes: Asian, American Indian/Alaskan, More than one race
# of missing: 1;
# of missing: 2;
#of missing: 2;
# of missing: 18;
# of missing: 32
TBSA = total body surface area
Physical and Mental Component Summary Scores
The mean scores for PROMs at each time point are shown in Table 2. For both PCS and MCS, the majority of the population (85%) had baseline and 5-year data points or baseline and 10-year data points. Mean scores for both the PCS and MCS at all post injury time points were lower than mean scores at baseline. The mean PCS score was 53.2 at baseline and 48.8 at 20 years post-injury, representing a difference of 44% of one SD lower at the most distal time point (i.e., 20-year follow-up). The mean MCS score was 53.5 at baseline and 47.7 at 20 years post-injury, representing a difference of 58% of one SD lower. These differences from baseline to 20 years denote moderate differences that are clinically and socially relevant.27
Table 2:
Patient Reported Outcome Scores Over Time
| Outcome | Pre-Injury* | Year 5 | Year 10 | Year 15 | Year 20 |
|---|---|---|---|---|---|
|
PCS1 mean (SD) |
53.1 (7.9) | 47.0 (10.3) | 48.1 (10.7) | 48.6 (12.5) | 48.7 (10.8) |
|
MCS2 mean (SD) |
53.5 (9.4) | 48.5 (11.9) | 47.5 (13.0) | 50.4 (10.0) | 47.7 (15.2) |
|
SWLS3 mean (SD) |
25.7 (7.7) | 22.7 (8.7) | 22.8 (7.1) | 24.4 (6.9) | 21.7 (10.4) |
|
CIQ4 mean (SD) |
8.4 (2.1) | 8.4 (2.3) | 8.0 (2.5) | 9.1 (2.5) | 8.0 (2.4) |
Physical Component Summary, scores are standardized with a mean of 50, SD of 10;
Mental Component Summary, scores are standardized with a mean of 50, SD of 10;
Satisfaction with Life Scale, score range 0–35;
Community Integration Questionnaire, score range 0–29.
The pre-injury PROM data is collected at discharge.
The discharge survey asks participants to recall their pre-injury physical health, mental health, satisfaction with life, and social integration.
The optimal mixed model for PCS included both the random intercept and slope effects (which yields lowest AIC/BIC values 5855.9/58843 compared with the other two models (5954.6/5968.6 and 5890/5908.8)). The statistically significant predictors for PCS include time since injury (β=−2.57, p< 0.001), age at burn (β=−0.1, p< 0.001), race (β=−2.18, p=0.01), sex (β=1.51, p=0.04), and length of hospital stay (β=−0.07, p< 0.001). Figure 2 displays results for PCS scores over time since injury stratified by age at injury and length of hospital stay. The PCS trajectories demonstrate that longer length of stay, older age at time of burn, and greater time since injury are associated with worse PCS scores. Longer hospital stay was associated with lower scores across the age groups (p<0.001). Trajectories across each age group show decreasing PCS scores over the 20-year period studied. PCS scores at 20 years compared to before the burn injury were as much as 44% of 1 standard deviation lower. This difference is clinically meaningful and considered a small to moderate difference.28
Figure 2: Physical Component Summary (PCS) Trajectories by Time Since Injury, Age at Injury, and Length of Stay.
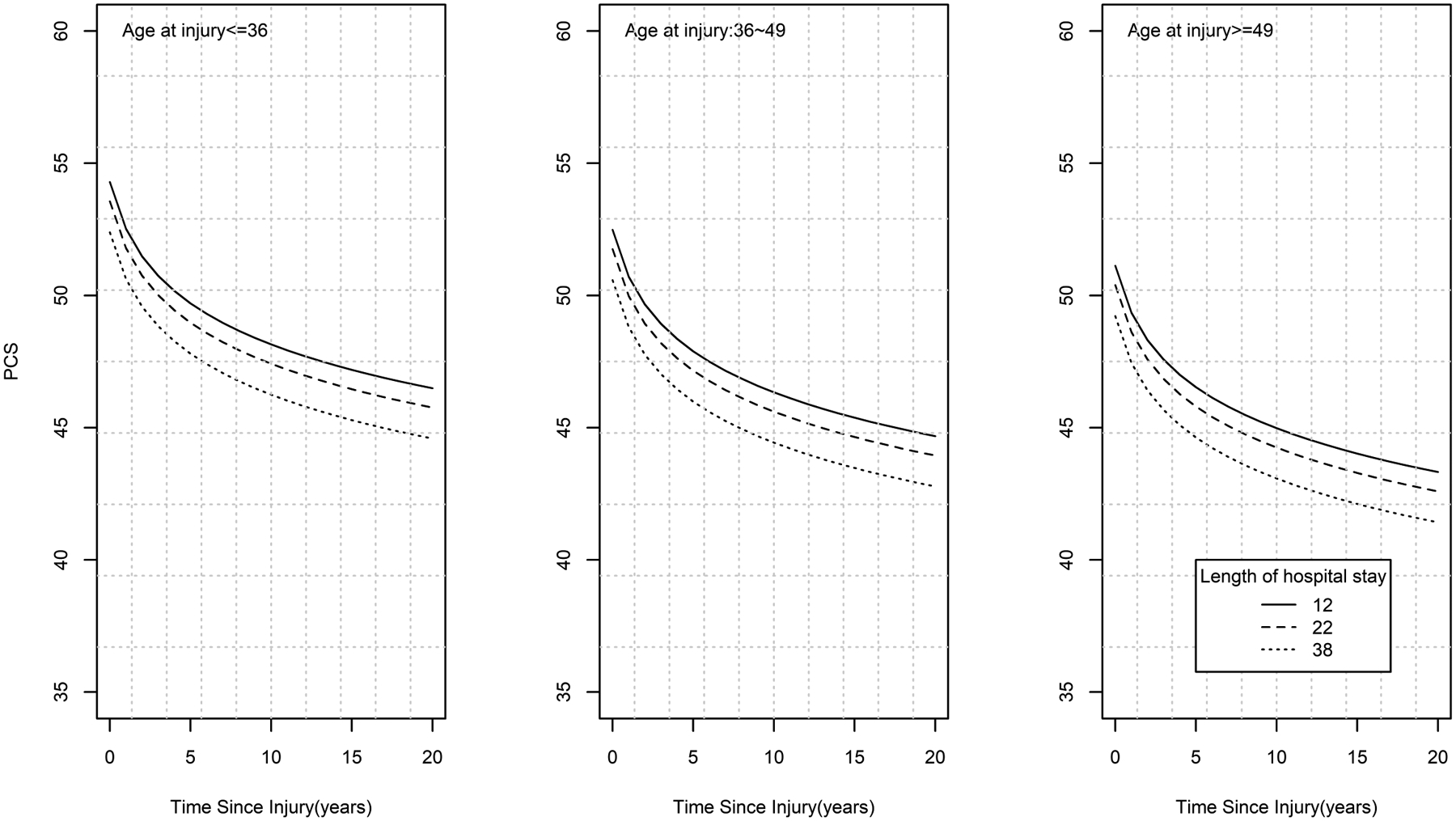
demonstrates that longer length of stay, older age at time of burn, and greater time since burn are associated with worse PCS scores. Longer hospital stays are associated with lower PCS scores across the three age groups. Trajectories across each age group show decreasing PCS scores over the duration of time since injury. Those with the longest hospital stays demonstrate greater worsening in PCS scores over the long term with a steeper change in the slopes initially. Age was categorized into 3 groups based on tertiles (<=36, 36~49 and >=49). Length of hospital stay was categorized into quartiles and the 25th (12 days), 50th (22 days) and 75th (38 days) percentile values are represented in the figure.
The optimal mixed model for MCS is the random intercept and fixed slope effect model (yields lower AIC/BIC values 6133.4/6152.1 compared with random intercept model (6185.1/6199.2), random intercept and random slope model did not converge). The statistically significant predictors for MCS include time since burn (β=−2.46, p< 0.001), length of hospital stay (β=−0.04, p= 0.03), and sex (β=−3.5, p= 0.0002). Figure 3 shows the MCS trajectories, which are presented over time since injury stratified by sex and length of hospital stay. Trajectories demonstrate that female sex, longer length of stay, and greater time since injury are associated with worse MCS scores. Males showed higher scores at baseline, however both sexes demonstrate diminishing scores over time, up to 20 years after injury (p= 0.0002).
Figure 3: Mental Component Summary (MCS) Trajectories by Time Since Injury, Sex and Length of Stay.
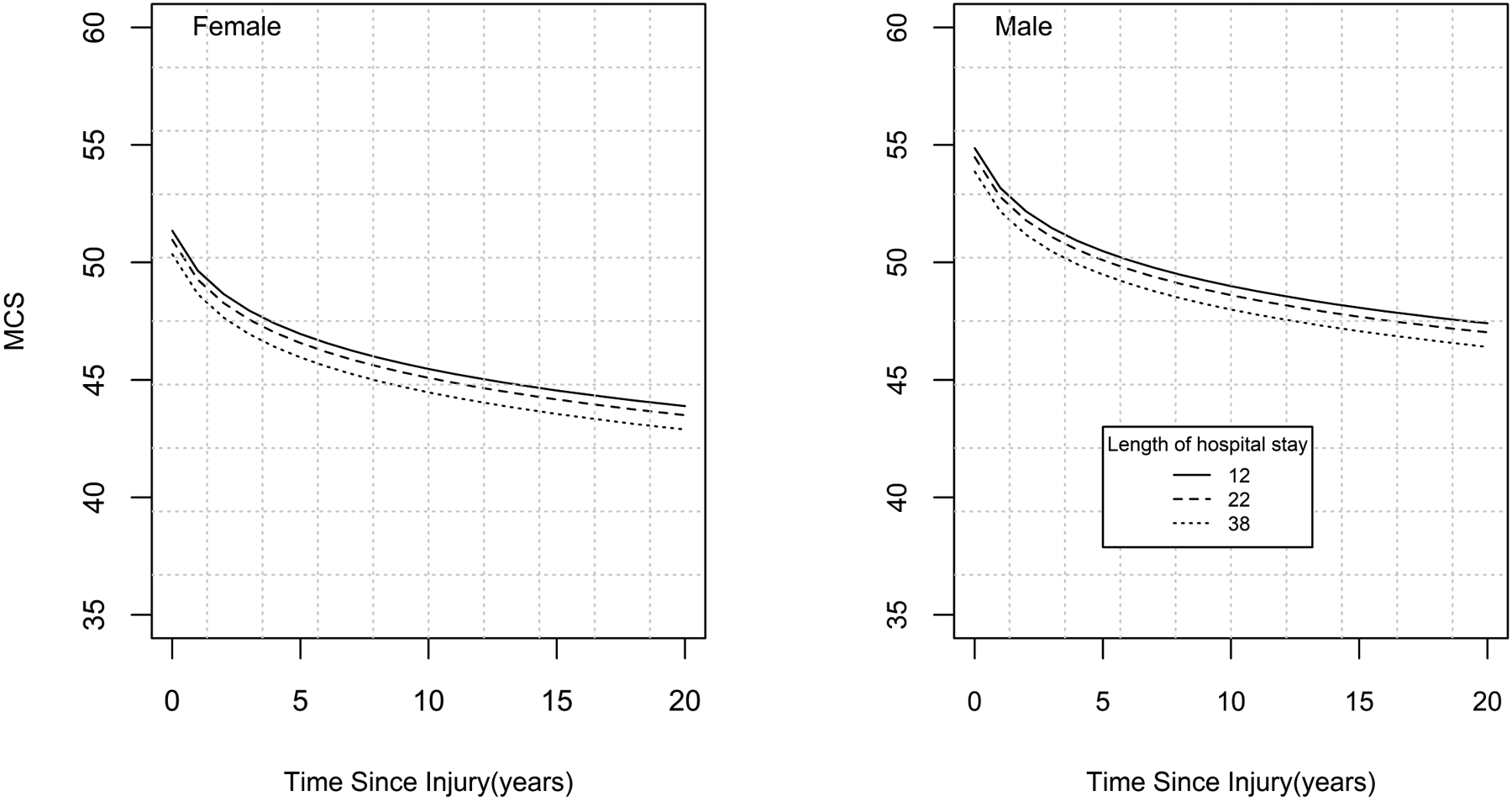
demonstrates that longer length of stay, female sex, and greater time since injury are associated with worse MCS scores. Males have higher scores at baseline than females, however both sexes demonstrate diminishing scores over time that extend to 20 years after injury. Length of hospital stay was categorized into quartiles and the 25th (12 days), 50th (22 days) and 75th (38 days) percentile values are represented in the figure.
Satisfaction with Life and Community Integration Scores
For both SWLS and CIQ, the majority of the cohort (79%) had baseline data points and 5-year data points. Mean scores for SWLS at all post-injury time points were lower than mean scores at baseline (pre-injury recall). The mean SWLS score was 25.7 at baseline and 21.7 at 20 years post injury. The statistically significant associations with SWLS, based on the random intercept and fixed slope effect model (which yields lowest AIC/BIC values 2288.2/2303.3 compared with the other two models (2298.7/2310.1 and 2290/2312.7)), included time since burn (β=−1.2, p=0.002) and length of hospital stay (β= −0.06, p=0.0003). Stratified analysis by length of hospital stay indicated lower trajectory scores over time and worse scores with longer hospital stays, as presented in Figure 4. Mean scores for CIQ were relatively stable over time. The optimal model for CIQ was the model with a random intercept without the fixed slope effect (yields lower AIC/BIC values 1438.1/1449.4 compared with random intercept, fixed slope model (1442.5/1457), random intercept and random slope model did not converge). The statistically significant associations with CIQ included burn size (β=−0.02, p=0.03), and Hispanic/Latino ethnicity (β= −1.29, p=0.006). Larger burn size and Hispanic/Latino ethnicity are associated with worse CIQ scores.
Figure 4: Satisfaction with Life Scale Trajectory by Time Since Injury and Length of Stay.
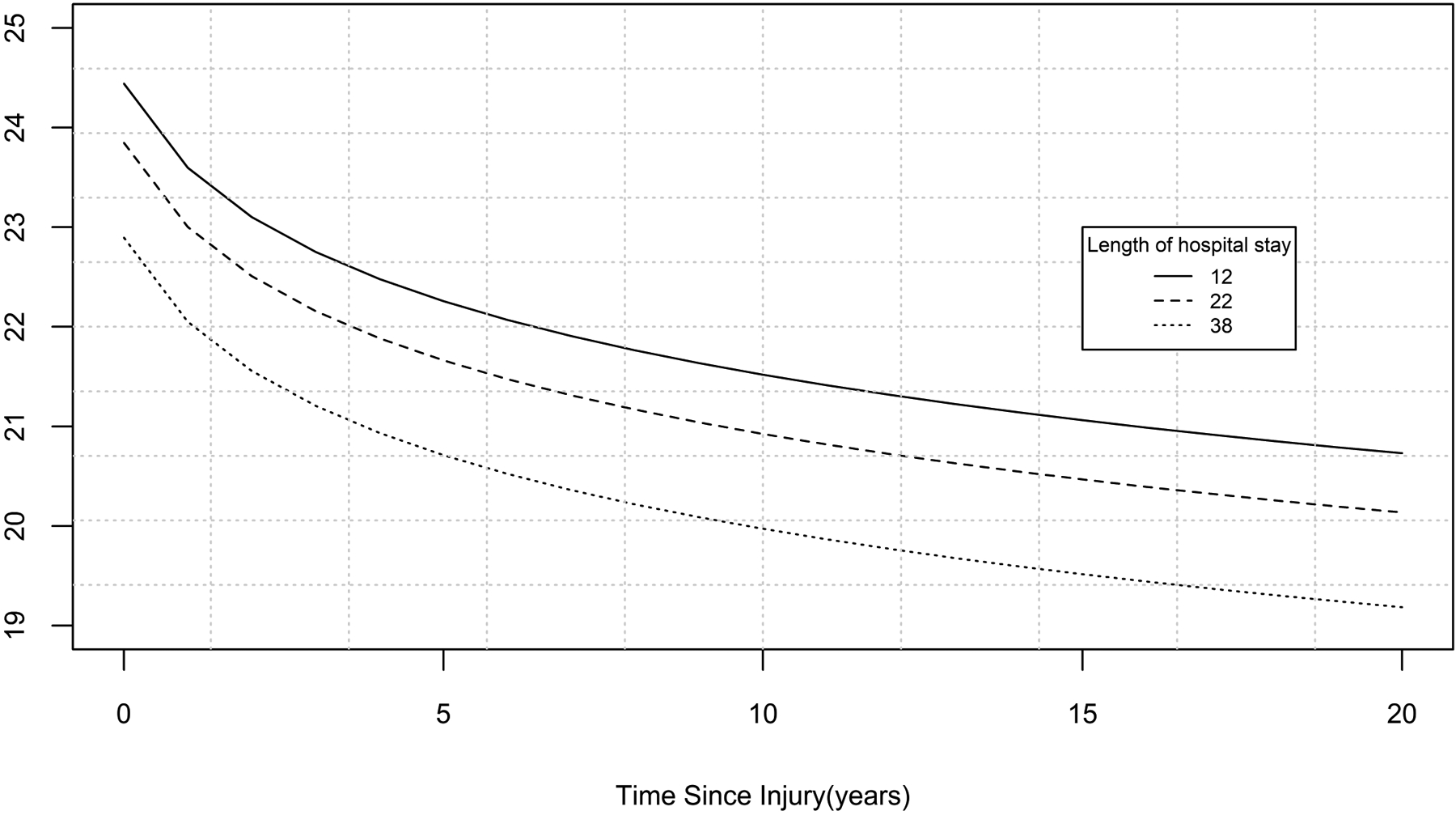
demonstrates that satisfaction with life trajectories decrease over time since injury and these decreases persist over the 20-year period from time of injury. Stratified analysis by length of hospital stay indicated lower trajectory scores over time with greater duration of hospital stays. Length of hospital stay was categorized into quartiles and the 25th (12 days), 50th (22 days) and 75th (38 days) percentile values are represented in the figure.
While samples with different durations in the study were observed, results indicated there are no systematic biases in demographic characteristics for the portion of the study population with baseline and 5-year data compared to the sample with baseline and 10-year data for PCS and MCS. Similarly, no systematic biases were found in demographic characteristics for subjects with only baseline data and those with baseline and 5-year follow-up data for SWLS and CIQ. Overall, results suggested that the degree of missingness was mostly random and did not impact the outcomes shown.
Bootstrapping confidence intervals were generated for all four outcome models. The confidence intervals matched with the significant coefficients in the final models reflecting the robustness of the coefficients.
Sensitivity Analysis
Comparison of the included and excluded study sample found that most sociodemographic and clinical variables were similar between groups with a few exceptions. The excluded sample had fewer females (24.5% vs. 34.2%, p<0.0001) and more Black/African American participants (17.7 vs 14.7, p = 0.0015) than the included sample. The excluded sample exhibited a shorter length of stay (26.5 days vs. 31.3 days, p = 0.004, smaller burn size (18.7 vs. 21.6, p= 0.0004), as well as fewer hand (66.9% vs. 75.4%, p=0.0004) and foot burns (26.9% vs. 37.2%, p<0.0001).
Discussion
This study is one of the first to analyze outcomes of burn survivors up to 20 years after injury. Results suggest that burn survivors’ physical and mental health as well as satisfaction with life decline significantly over time. Further, females were found to have worse mental health outcomes compared to males. Longer hospital stays were negatively associated with long-term physical health, mental health, and satisfaction with life.
Importantly, burn survivors’ PCS and MCS scores never recover to their pre-injury levels at any follow-up time point. PCS scores for the study sample were between 20% to 30% of a standard deviation lower than the U.S. norm overall. PCS scores in the general U.S. population have been found to be lower than 50 for select age groups between 18 and 75+ years old.18 In addition, after 55 years of age there is a gradual decline in general population PCS scores, with a slightly steeper decline after 65 years.18,29 The decline in physical function of burn survivors over time is visualized in the trajectory curve where the scores demonstrate the steepest decline in the first five years after injury, and continue to steadily decline after 5 years (Table 2; Figure 2). Female burn survivors reported worse mental health than male survivors, which is a pattern also seen in the general population.30 Both male and female burn survivors scored lower on the MCS than the general population.
Similarly, SWLS of people living with burn injury never recover to their pre-injury levels at any time point and were found to decline over time. There are few studies that examine satisfaction with life within the general U.S. population. Prior work examined SWLS in North American and European populations and found that most groups reported SWLS scores between 23 and 28 (“slightly satisfied” to “satisfied” with life).25,32 The study sample exhibited mean scores (21–24) across all time points at the lower end of the scores reported in the general population.
Worse CIQ scores were correlated with larger burn size and Hispanic/Latino ethnicity. The influence of burn size on quality of life has been explored with varying conclusions.8,33,34 A recent report found that burn survivors with larger burns scored worse in employment and social activities, but better in family and friends as well as sexual relationships than those with smaller burns.34 The current study’s findings related to burn size could be due to survivors limited physical functioning compared to their community.35 The impact on community integration could also be due to changes in survivors’ appearance. People living with head and neck burns report higher levels of dissatisfaction with appearance.4 Limited conclusions can be drawn about the relationship between ethnicity and CIQ scores without data on related socio-economic variables such as employment and education. Prior work studied CIQ scores up to 2 years post-injury and found that Black and Hispanic/Latino participants had lower CIQ scores over time than White participants.36 Continuing to explore associations and interactions between burn size, socioeconomic variables, and community integration is necessary to determine how to best support people living with burn injury.
These findings strongly support that burn injury is a chronic condition by demonstrating the persistent physical and mental deficits of burn survivors compared to the general population.37,38 The underlying chronic nature of burn injuries is defined by both long-term symptoms (e.g. pruritus, paresthesia, and trouble with temperature regulation) and clinical sequelae (e.g. contractures, scarring, balance disorders, swelling of extremities, and cognitive issues).37,39–41 Formally recognizing burns as a chronic condition underscores the importance of educating providers, survivors and their families about the chronic sequelae, and developing long-term care models tailored to the needs of survivors.37,42–44 Other traumatic injury fields, such as the traumatic brain injury community, have advocated for this framework.43 Additionally, the results of the current study highlight the importance of continued research investigating physical and mental health outcomes beyond a few years after burn injury.9
Although the findings of this study highlight a decline in patient-reported health and life satisfaction after injury, these results should be understood in the context of other literature and do not necessarily portend a negative outlook for the entire community. Recent research demonstrates that burn survivors have diverse experiences with their injury and exhibit many different recovery trajectories1,45 A study examining satisfaction with life identified two classes of life satisfaction trajectories for burn survivors (‘unchanged’ and ‘dissatisfied’).24 Within these subgroups there were varying levels of life satisfaction after injury that were dependent on variables such as age, sex, pre-injury employment, and pre-injury mental health status.24 Further exploring subgroups within the burn survivor community is necessary for a more nuanced understanding of long-term recovery. It is also necessary to highlight the lack of permanence of these long-term obstacles for burn survivors; for example, this study does not explore the efficacy of mental health strategies like peer support, psychological therapy, or psychiatric medication to mediate mental health issues and allow survivors to live well.46,47 This study provides some evidence of the need for long term follow-up and interventions for the burn survivor population.
This study has a few limitations to note. First, over study period, not every participant completed all follow-up repeated measures. The mixed methods models controlled for correlated error and random effects dealing with in part missing values and regression towards the mean effects. The basic trajectory model relied on two parameters for fixed effects which is less data demanding than more complex models; this balanced the missing data in the model to describe the changes in outcomes. There were fewer data points followed over the longer term, limiting the statistical power to detect significant derivations of the trajectories with larger prediction errors for the outcomes at more distal time points. A final limitation is that the baseline assessment is collected at hospital discharge and is the subject’s perception of their health prior to their burn injury. There is potential “response shift” bias related to the frame of reference used by the respondent that may have shifted over time.48–50 Response shift may occur due to a burn survivor’s physical functionality changing or a shift in their mental health, altering their perceived overall health status before the burn.49
In conclusion, burn survivors’ physical health, mental health and satisfaction with life worsened over time, through the 20 years examined. Physical and mental health of survivors was associated with sex, time since injury, length of hospitalization, and age at injury. Satisfaction with life was affected by length of stay and time since injury, and community integration was influenced by burn size and ethnicity. The findings suggest burn injury can be a chronic, dynamic health condition with complex and persistent health and psychosocial consequences rather than a static state. Findings begin to evidence the need for the development of interventions and application of chronic disease management to improve long-term burn outcomes.
Supplementary Material
Conflicts of Interest and Source of Funding:
No conflicts of interest.
This work was supported by the National Institute on Disability, Independent Living, and Rehabilitation Research (grant #90DPBU0001). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this manuscript do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
This work was also partially supported by the Fraser Fund at Massachusetts General Hospital.
Footnotes
Presented at the 2021 American Burn Association annual meeting in the top six abstract plenary.
References
- 1.McAleavey AA, Wyka K, Peskin M, Difede JA. Physical, functional, and psychosocial recovery from burn injury are related and their relationship changes over time: A Burn Model System study. Burns [Internet]. 2018;44(4):793–9. [DOI] [PubMed] [Google Scholar]
- 2.Falder S, Browne A, Edgar D, Staples E, Fong J, Rea S, Wood F. Core outcomes for adult burn survivors: A clinical overview. Burns. 2009;35(5):618–41. [DOI] [PubMed] [Google Scholar]
- 3.Goverman J, Mathews K, Nadler D, Henderson E, McMullen K, Herndon D, Meyer W, Fauerbach JA, Wiechman S, Carrougher G, et al. Satisfaction with life after burn: A Burn Model System National Database Study. Burns [Internet]. 2016;42(5):1067–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sinha I, Nabi M, Simko LC, Wolfe AW, Wiechman S, Giatsidis G, Bharadia D, McMullen K, Gibran NS, Kowalske K, et al. Head and neck burns are associated with long-term patient-reported dissatisfaction with appearance: A Burn Model System National Database study. Burns [Internet]. 2019;45(2):293–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carrougher GJ, Martinez EM, McMullen KS, Fauerbach JA, Holavanahalli RK, Herndon DN, Wiechman SA, Engrav LH, Gibran NS. Pruritus in adult burn survivors: Postburn prevalence and risk factors associated with increased intensity. J Burn Care Res. 2013;34(1):94–101. [DOI] [PubMed] [Google Scholar]
- 6.Schneider JC, Nadler DL, Herndon DN, Kowalske K, Matthews K, Wiechman SA, Carrougher GJ, Gibran NS, Meyer WJ, Sheridan RL, et al. Pruritus in pediatric burn survivors: Defining the clinical course. J Burn Care Res. 2015;36(1):151–8. [DOI] [PubMed] [Google Scholar]
- 7.Deeter L, Seaton M, Carrougher GJ, McMullen K, Mandell SP, Amtmann D, Gibran NS. Hospital-acquired complications alter quality of life in adult burn survivors: Report from a burn model system. Burns [Internet]. 2019;45(1):42–7. [DOI] [PubMed] [Google Scholar]
- 8.Kishawi D, Wozniak AW, Mosier MJ. TBSA and length of stay impact quality of life following burn injury. Burns [Internet]. 2020;46(3):616–20. [DOI] [PubMed] [Google Scholar]
- 9.Cimino SR, Rios JN, Godleski M, Hitzig SL. A scoping review on the long-term outcomes in persons with adult-acquired burn injuries. J Burn Care Res. 2020;41(3):472–502. [DOI] [PubMed] [Google Scholar]
- 10.Wiechman SA, McMullen K, Carrougher GJ, Fauerbach JA, Ryan CM, Herndon DN, Holavanahalli R, Gibran NS, Roaten K. Reasons for Distress Among Burn Survivors at 6, 12, and 24 Months Postdischarge: A Burn Injury Model System Investigation. Arch Phys Med Rehabil [Internet]. 2018;99(7):1311–7. [DOI] [PubMed] [Google Scholar]
- 11.Marino M, Soley-Bori M, Jette AM, Slavin MD, Ryan CM, Schneider JC, Acton A, Amaya F, Rossi M, Soria-Saucedo R, et al. Measuring the Social Impact of Burns on Survivors. J Burn Care Res. 2017;38(1):e377–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carrougher GJ, McMullen K, Mandell SP, Amtmann D, Kowalske KJ, Schneider JC, Herndon DN, Gibran NS. Impact of burn-related amputations on return to work: Findings from the burn injury model system national database. J Burn Care Res. 2019;40(1):21–8. [DOI] [PubMed] [Google Scholar]
- 13.Pham TN, Goldstein R, Carrougher GJ, Gibran NS, Goverman J, Esselman PC, Kazis LE, Ryan CM, Schneider JC. The impact of discharge contracture on return to work after burn injury: A Burn Model System investigation. Burns [Internet]. 2020;46(3):539–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van Baar ME, Essink-Bot ML, Oen IMMH, Dokter J, Boxma H, Van Beeck EF. Functional outcome after burns: A review. Burns. 2006;32(1):1–9. [DOI] [PubMed] [Google Scholar]
- 15.Bajorek AJ, Slocum C, Goldstein R, Mix J, Niewczyk P, Ryan CM, Hendricks CT, Zafonte R, Schneider JC. Impact of Cognition on Burn Inpatient Rehabilitation Outcomes. PM R [Internet]. 2017;9(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goverman J, Mathews K, Holavanahalli RK, Vardanian A, Herndon DN, Meyer WJ, Kowalske K, Fauerbach J, Gibran NS, Carrougher GJ, et al. The National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System: Twenty Years of Contributions to Clinical Service and Research. J Burn Care Res. 2017;38(1):e240–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ware JE, Keller SD, Kosinski M. SF-12: How to Score the Sf-12 Physical and Mental Health Summary Scales: A User’s Manual. Second. Boston, MA: Health Institute, New England Medical Center; 1995. [Google Scholar]
- 18.Selim AJ, Rogers W, Fleishman JA, Qian SX, Fincke BG, Rothendler JA, Kazis LE. Updated U.S. population standard for the Veterans RAND 12-item Health Survey (VR-12). Qual Life Res. 2009;18(1):43–52. [DOI] [PubMed] [Google Scholar]
- 19.Selim A, Rogers W, Qian S, Rothendler JA, Kent EE, Kazis LE. A new algorithm to build bridges between two patient-reported health outcome instruments: the MOS SF-36® and the VR-12 Health Survey. Qual Life Res. 2018;27(8):2195–206. [DOI] [PubMed] [Google Scholar]
- 20.Sullivan GM, Feinn R. Using Effect Size—or Why the P Value Is Not Enough. J Grad Med Educ. 2012;4(3):279–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lewis E Kazis S, Jennifer j. Anderson P, Robert F. Meenan MDM. Effect Sizes for Interpreting Changes in Health Status. J Med Care. 1989;27(3):178–89. [DOI] [PubMed] [Google Scholar]
- 22.Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction with Life Scale. J Pers Assess. 1985;49(1):71–5. [DOI] [PubMed] [Google Scholar]
- 23.Diener E Assessing Well-Being: The Collected Works of Ed Diener. Diener E, editor. Springer Science and Business Media; 2009. [Google Scholar]
- 24.Amtmann D, Bocell FD, McMullen K, Bamer AM, Johnson KL, Wiechman SA, Schneider JC. Satisfaction With Life Over Time in People With Burn Injury: A National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System Study. Arch Phys Med Rehabil [Internet]. 2020;101(1):S63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pavot W, Diener E, Colvin CR, Sandvik E. Further validation of the satisfaction with life scale.pdf. Vol. 57, Journal of Personality Assessment. 1991. p. 149–61. [DOI] [PubMed] [Google Scholar]
- 26.Gerrard P, Kazis LE, Ryan CM, Shie VL, Holavanahalli R, Lee A, Jette A, Fauerbach JA, Esselman P, Herndon D, et al. Validation of the Community Integration Questionnaire in the adult burn injury population. Qual Life Res. 2015;24(11):2651–5. [DOI] [PubMed] [Google Scholar]
- 27.Boston University School of Public Health. MCS and PCS Score Interpretation [Internet].
- 28.Selim AJ, Qian SX, Rogers W, Arya D, Simmons K, Shapiro GD, Sonis LA, Kazis LE. Health Status in Adults with Chronic Conditions: Intervention Strategies for Improving Patient-Reported Outcomes. J Ambul Care Manage. 2019;42(1):2–20. [DOI] [PubMed] [Google Scholar]
- 29.Kazis LE, Lee A, Spiro A, Rogers W, Ren XS, Miller DR, Selim A, Hamed A, Haffer SC. Measurement comparisons of the Medical Outcomes Study and Veterans SF-36® Health Survey. Health Care Financ Rev. 2004;25(4):43–58. [PMC free article] [PubMed] [Google Scholar]
- 30.Ware JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Med Care. 1996;34(3):220–33. [DOI] [PubMed] [Google Scholar]
- 31.Kazis LE, Lee AF, Rose M, Liang MH, Li NC, Ren XS, Sheridan R, Gilroy-Lewis J, Stoddard F, Hinson M, et al. Recovery curves for pediatric burn survivors advances in patient-oriented outcomes. JAMA Pediatr. 2016;170(6):534–42. [DOI] [PubMed] [Google Scholar]
- 32.Morrison M, Tay L, Diener E. Subjective Well-Being and National Satisfaction: Findings From a Worldwide Survey. J Psychol Sci. 2011;22(2):166–71. [DOI] [PubMed] [Google Scholar]
- 33.Ryan CM, Lee A, Kazis LE, Schneider JC, Shapiro GD, Sheridan RL, Meyer WJ, Palmieri T, Pidcock FS, Reilly D, et al. Recovery trajectories after burn injury in young adults: Does burn size matter? J Burn Care Res. 2015;36(1):118–29. [DOI] [PubMed] [Google Scholar]
- 34.Ryan CM, Shapiro GD, Rencken CA, Griggs C, Jeng JC, Hickerson WL, Marino M, Goverman J, Kazis LE, Schneider JC. The Impact of Burn Size on Community Participation. Ann Surg. 2020;Publish Ah(May 2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stoddard FJ, Ryan CM, Schneider JC. Physical and psychiatric recovery from burns. Psychiatr Clin North Am [Internet]. 2015;38(1):105–20. [DOI] [PubMed] [Google Scholar]
- 36.Pierce BS, Perrin PB, Perrin PB, Pugh M, Cariello AN, Henry RS, Sutter ME, Wiechman SA, Schneider JC. Racial/Ethnic Disparities in Longitudinal Trajectories of Community Integration after Burn Injury. Am J Phys Med Rehabil. 2020;99(7):602–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kelter BM, Holavanahalli R, Suman OE, Ryan CM, Schneider JC. Recognizing the long-term sequelae of burns as a chronic medical condition. Burns. 2020;46(2):493–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barrett LW, Fear VS, Waithman JC, Wood FM, Fear MW. Understanding acute burn injury as a chronic disease. Burn Trauma. 2019;7:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xiao Y, Sun Y, Zhu B, Wang K, Liang P, Liu W, Fu J, Zheng S, Xiao S, Xia Z. Risk factors for hypertrophic burn scar pain, pruritus, and paresthesia development. Wound Repair Regen. 2018;26(2):172–81. [DOI] [PubMed] [Google Scholar]
- 40.Oh J, Madison C, Flott G, Brownson EG, Sibbett S, Seek C, Carrougher GJ, Ryan CM, Kowalske K, Gibran NS, et al. Temperature Sensitivity After Burn Injury: A Burn Model System National Database Hot Topic. J Burn Care Res. 2021; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nedelec B, Carrougher GJ. Pain and pruritus postburn injury. J Burn Care Res. 2017;38(3):142–5. [DOI] [PubMed] [Google Scholar]
- 42.Rees S, Williams A. Promoting and supporting self-management for adults living in the community with physical chronic illness: A systematic review of the effectiveness and meaningfulness of the patient-practitioner encounter. JBI Libr Syst Rev [Internet]. 2009;7(13):492–582. [DOI] [PubMed] [Google Scholar]
- 43.Corrigan JD, Hammond FM. Traumatic brain injury as a chronic health condition. Arch Phys Med Rehabil [Internet]. 2013;94(6):1199–201. [DOI] [PubMed] [Google Scholar]
- 44.Ryan CM, Lee AF, Kazis LE, Shapiro GD, Schneider JC, Goverman J, Fagan SP, Wang C, Kim J, Sheridan RL, et al. Is real-time feedback of burn-specific patient-reported outcome measures in clinical settings practical and useful? a pilot study implementing the young adult burn outcome questionnaire. J Burn Care Res. 2016;37(1):64–74. [DOI] [PubMed] [Google Scholar]
- 45.Wiechman S, Hoyt MA, Patterson DR. Using a Biopsychosocial Model to Understand Long-Term Outcomes in Persons With Burn Injuries. Arch Phys Med Rehabil [Internet]. 2020;101(1):S55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Al-Ghabeesh SH. How does coping strategies, social support, and mindfulness improve the psychological well-being of Jordanian burn survivors? A descriptive correlational study. Burns [Internet]. 2021;1–7. [DOI] [PubMed] [Google Scholar]
- 47.Grieve B, Shapiro GD, Wibbenmeyer L, Acton A, Lee A, Marino M, Jette A, Schneider JC, Kazis LE, Ryan CM, et al. Long-Term Social Reintegration Outcomes for Burn Survivors With and Without Peer Support Attendance: A Life Impact Burn Recovery Evaluation (LIBRE) Study. Arch Phys Med Rehabil. 2020;101(1):S92–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schwartz CE, Andresen EM, Nosek MA, Krahn GL. Response Shift Theory: Important Implications for Measuring Quality of Life in People With Disability. Arch Phys Med Rehabil. 2007;88(4):529–36. [DOI] [PubMed] [Google Scholar]
- 49.Spronk I, Geraerds AJLM, Bonsel GJ, de Jongh MAC, Polinder S, Haagsma JA. Correspondence of directly reported and recalled health-related quality of life in a large heterogeneous sample of trauma patients. Qual Life Res. 2019;28(11):3005–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haagsma JA, Spronk I, De Jongh MAC, Bonsel GJ, Polinder S. Conventional and retrospective change in health-related quality of life of trauma patients: An explorative observational follow-up study. Health Qual Life Outcomes. 2020;18(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


