Abstract
Stroke family caregiver and dyad literature has expanded over the past few years. The purpose of this review was to build upon two prior systematic reviews to critique, analyze, and synthesize the evidence pertaining to the impact of family caregiver and dyad interventions on stroke survivor and family caregiver outcomes. CINAHL, PsychINFO, PubMed, and reference lists were searched from December 1, 2016 through March 31, 2021. Using PRISMA guidelines, articles were identified that tested outcomes from stroke family caregiver or dyad interventions that targeted the health or well-being of family caregivers. Data from the articles were abstracted into tables for analysis, then compared with recommendations from the two prior systematic reviews. A total of 18 articles met inclusion criteria (10 caregiver interventions; 8 dyad interventions) representing sample sizes ranging from 7 to 349 caregivers or dyads. Most were randomized controlled trials (n=13); 2 were cluster randomized trials; and 3 were single-group quasi-experimental designs. Of the 18 studies, 8 had less than 50 caregivers or dyads, and 5 were small feasibility studies that reported data trends rather than testing for significance. Only 6 studies reported significant survivor outcomes. Eleven studies reported significant caregiver outcomes, the most common being burden. A number of survivor and caregiver outcomes were not significant, or only significant for certain subgroups. The limited number of studies, small sample sizes, and conflicting results, made it difficult to draw firm conclusions regarding the impact of these interventions on outcomes. Based on the available evidence from these 18 studies, recommendations from the two prior reviews were generally supported. Well-designed and well-powered randomized controlled clinical trials are still needed to confirm efficacy of stroke family caregiver and dyad interventions.
Keywords: Stroke, Family Caregiver, Interventions, Clinical Trials, Systematic Review
Introduction
According to the World Health Organization, stroke remains the second leading cause of death worldwide and a major cause of disability.1,2 Of those who survive stroke, almost two-thirds require family caregiver assistance.3–5 Even though caregivers may have diverse situations and needs, they often experience emotional and physical health-related quality of life changes associated with the demands of caregiving.6–9 Because family caregiving serves as the cornerstone of long-term care in the United States, it has increasingly become a significant public health issue affecting the quality of life of millions of individuals.10–13 Approximately 53 million Americans are family caregivers, which is an increase from an estimated 43.5 million in 2015.10,12 A large portion of these caregivers provide as many as 24 hours of care each week.10,12
Despite the expansion of research evidence, caregivers still experience many unmet needs and numerous systematic reviews conclude that there is, at present, a lack of high-quality studies and identification of best practices for family caregiver or dyad interventions.6,7,9,14–17 Variability in the quality of the research methodology, measurement of outcome variables, and strength of family caregiver interventions appears to remain problematic warranting a more systematic examination of this literature.14–17 Several urgent research areas are the need to provide greater and more effective professional support, health information, and community network assistance to family caregivers and the survivors.8–12
The purpose of this systematic review is to build upon prior work6,7 to critique, analyze, and synthesize the evidence pertaining to the impact of family caregiver and dyad interventions on stroke survivor and family caregiver outcomes. Applying the same methodology by Bakas and colleagues,6,7 the rapidly expanding stroke family caregiver literature was reviewed to update the state of the science. Not only does this effort add to the science focusing on family caregiver interventions, but more importantly provides an updated foundation for evidence-based interventions to improve the quality of care for both stroke survivors and their families in various settings. Three questions were addressed in this review and critique of the literature:
Question 1: Do family caregiver and dyad interventions improve survivor outcomes?
Question 2: Do family caregiver and dyad interventions improve caregiver outcomes?
Question 3: What types of stroke family caregiver and dyad interventions have the best evidence?
Methods
The authors declare that all supporting data are available within the article and its online supplementary files. Based upon the methods used in previous systematic reviews of stroke caregiver and dyad interventions by this team,6,7 and the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020 Guidelines,18 we conducted a critical analysis of published studies identified by searching the databases Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsychINFO, and PubMed (includes MEDLINE). Additional articles were located from reference lists of relevant articles. No registers, websites, or organizations were used to identify studies. Searches were based on the keywords stroke, family, caregiver, interventions, experimental studies, and quasi-experimental studies, with date limiters applied (December 2016 through March 2021). Articles were independently assessed by two members of the review team and included if they were: (1) written in English; (2) published from December 2016 through March 2021; (3) used a quasi-experimental or experimental research design; (4) involved a stroke caregiver intervention or a stroke dyad intervention; (5) had an intervention targeting the health or well-being of the caregiver (not just the survivor or the caregiver’s care for the survivor); (6) examined stroke survivor outcomes and/or stroke family caregiver outcomes; and (7) were implemented during any part of the stroke care continuum (acute hospitalization, inpatient rehabilitation, home care, long-term care). Dissertations, books, and conference proceedings were excluded. We tracked the search process using the PRISMA 2020 flow diagram (Figure 1).18
Figure 1.
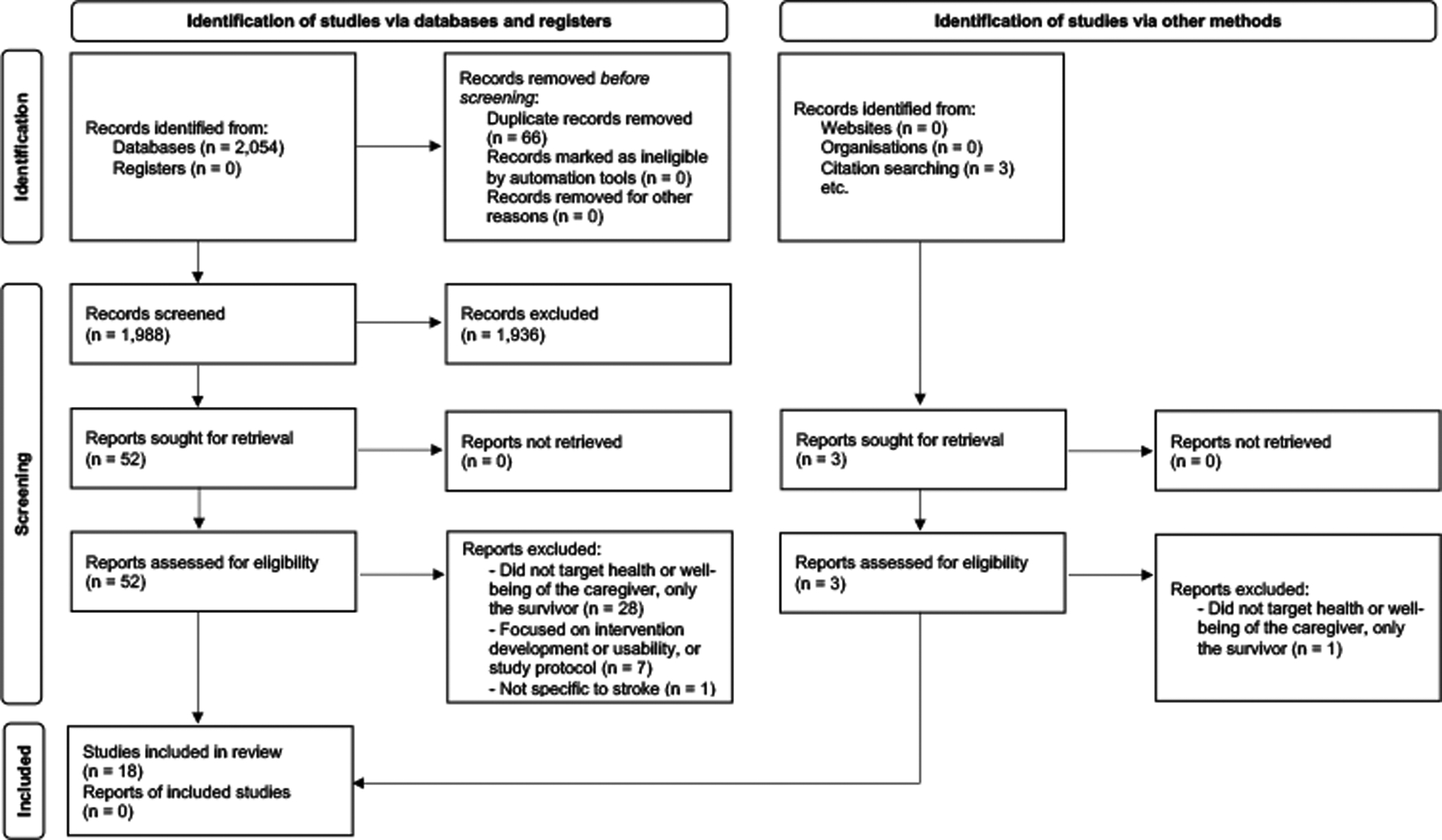
PRISMA 2020 flow diagram.
Two members of the review team screened the initial set of 2054 records, removing 66 duplicates, and excluding 1936 that did not meet inclusion criteria. Three additional records were identified through citation searching. Fifty-five full-text studies (including the 3 from citation searching) were then reviewed by one member of the team, which resulted in 37 additional articles being excluded because they: Did not target the health or well-being of the caregiver (n=29); were focused on intervention development/usability, or were study protocols (n=7), or were not stroke specific (n=1). A second member of the review team confirmed this assessment. Thus, consensus was reached by at least two reviewers before a study was deemed eligible for synthesis. This process was monitored by a third member of the review team. In total, 18 studies19–36 were included and grouped for synthesis according to intervention type (10 stroke caregiver interventions;19–28 8 stroke dyad interventions29–36).
Review templates were populated by two members of the team and confirmed by a third. Data were sought for survivor outcomes including physical functioning, anxiety and depression, health-related quality of life, social functioning, and service use. Caregiver outcomes included preparedness, caregiver burden, stress, strain, anxiety, depressive symptoms, health-related quality of life, social functioning, knowledge, and satisfaction. Relational outcomes, such as dyadic interactions and relationship quality, were included. Data also were sought for participant and intervention characteristics. For each study, information was abstracted about the sample, design, type of intervention (skill-building, psychoeducation, support), delivery mode (face-to-face, telephone, web-based), number of sessions, and significant (p<0.05) survivor and/or caregiver outcomes. Skill-building interventions were defined as, “strategies that focus on processes that facilitate problem solving, goal setting, communicating with health care professionals, stress management, and hands on training in such skills as lifting and mobility techniques, assistance with activities of daily living, and communication tailored to the needs of the stroke patient.”6,7 Psycho-educational interventions were defined as, “provision of information about (a) warning signs for stroke, lifestyle changes, and general resources, (b) managing survivor emotions and behaviors, (c) managing medications and personal care, (d) managing finances and transportation, and (e) managing one’s own emotions and health care needs.”6,7 Support interventions were defined as, “engaging in interactions with peers for support and advice (e.g., support groups, online discussion forums).”6,7
Two reviewers appraised each study’s risk of bias and overall methodological quality according to Consolidated Standards of Reporting Trials (CONSORT) criteria for experimental studies37 or Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) criteria for quasi-experimental studies.38 Each study was further assessed for threats to validity.39 The review team interpreted and narratively synthesized data contained in the review templates in order to answer the review questions. The first two questions asked whether stroke family caregiver and dyad interventions improved stroke survivor and caregiver outcomes. The third question asked about the types of stroke family caregiver and dyad interventions that had the best evidence. Certainty of the findings was assessed by comparing the findings with this review with recommendations made for stroke caregiver and dyad interventions in two prior systematic reviews.6,7 Co-authors provided comments, edits, and additional recommendations based upon observed limitations of the included studies. The process continued until all authors were in agreement about the final synthesis, results, and recommendations.
Results
Critique of the 18 Articles
Designs
Of the total of 18 articles, a majority (n=13) reported using an experimental design where caregivers or dyads were randomized to intervention or attention control/usual care groups.19–21,23,25–29,31,33,34,36 One study used a pragmatic cluster randomized controlled clinical trial design where 36 clusters of service providers were randomized to intervention or control groups within a stroke specialist organization providing long-term in-hospital and home support to stroke survivors and caregivers.24 Another study randomized 12 clusters of service providers to 3 groups: dyads, caregivers only, or a waiting list control group.32 The remaining studies (n=3) used a single-group quasi-experimental design.22,30,35 Several articles (n=5) were small feasibility studies that reported data trends, rather than testing for significance in outcomes.25,29–31,35
Samples
Among the 18 studies, sample sizes ranged from a total of 7 to 349 caregivers or dyads. The study with the largest sample (N=349) involved randomizing 36 clusters to a caregiver intervention (n=175; 18 clusters) or to usual care (n=174; 18 clusters).24 The study with the fewest number of participants was a single-group quasi-experimental study with 7 dyads in a treatment group.30 A large proportion of the studies (n=8) had less than 50 caregivers or dyads enrolled.22,23,25,27,29–31,35 Studies with 50 to 100 participants (n=4) were also common.20,21,32,36 These smaller pilot studies (n=12) provide valuable findings regarding feasibility and data trends for future studies;20–23,25,27,29–32,35,36 however, they must be interpreted with caution. Smaller pilot studies typically lack power for hypothesis testing and result in questionable effect size estimates for larger studies, and are prone to Type I errors if results are significant, or Type II errors if results are not significant.40 Aside from the largest study with 349 caregivers,24 there were 5 studies with over 100 caregivers or dyads;19,26,28,33,34, however, two of the studies reported findings using the same sample.33,34
Interventions
Detailed descriptions of content and procedures for the intervention and control conditions were provided in each of the 18 articles. Only one study reported blinding of participants to the type of intervention they received.19 By knowing which group participants were assigned, the potential for compensatory effects (i.e., participants overcompensating in the control group) or resentful demoralization (i.e., participants receiving less desirable treatment feeling resentful or demoralized, changing their responses to outcome measures) are threats to validity to consider in interpretation of the findings.39 Treatment diffusion (e.g., control group having access to treatment group materials) and treatment fidelity (i.e., design, training, delivery, receipt, enactment) were rarely addressed, unveiling the potential for further threats to validity.39,41 Three of the 18 articles mentioned adherence to the intervention by participants30,35 and use of a treatment fidelity checklist to ensure adherence to protocol by research staff.31
Measurement of Survivor Outcomes
The outcome measures for the 18 studies addressed a variety of stroke survivor outcomes. For survivor cognitive status, studies used the Mini Mental State Exam,28 the Montreal Cognitive Assessment,28 and the Credibility and Expectancy Questionnaire.29 Physical function and activities of daily living were measured using the Modified Rankin Scale25 and the Barthel Index.25,32 Upper arm function was measured in one study by the Wolf Motor Function Test, Upper Extremity Fugl-Meyer Test, Motor Activity Log, and the Confidence in Arm and Hand Movement Scale.30
Survivor depression and anxiety were measured using a variety of measures including the Hospital Anxiety and Depression Scale,28,29,25 Patient-Reported Outcomes Measurement Information System (PROMIS) Depression Short Form 8b,35 Patient Health Questionnaire (PHQ-9),31 Zung Self-rating Anxiety Scale,28 and Zung Self-Rating Depression Scale.28 Several studies used the Connor Davidson Resilience Scale,35 General Self-Efficacy Scale,29 Cognitive and Affective Mindfulness Scale-Revised,29 Post Traumatic Stress Disorder (PTSD) Checklist Civilian Version for stress symptom severity,29 and Measure of Current Status Part A.29
Two studies used the Stroke Impact Scale,31,35 and one used the Stroke Specific Quality of Life Scale.20 Other studies measured survivor quality of life using the European Quality of Life EuroQol (EQ5D-5L),25 Older People’s Quality of Life Questionnaire,35 and the Satisfaction with Life Scale.32 Several studies addressed the stroke survivor’s social functioning, dyadic interactions, and the quality of relationship with the caregiver and used the Social Relationships Index,35 Active Engagement Communication Scale,31 Protective Buffering Communication Scale,31 McMaster Family Assessment Device General Functioning Subscale,31 Patient Expectations Scale,31 Perceived Criticism Scale,31 Communication in Marriage Questionnaire,33 Intimate Bond Measure,29 Dyadic Adjustment Scale,34 Mutuality Scale,31 and the Relationship Assessment Scale.31
Several studies measured survivor satisfaction with the Client Satisfaction Questionnaire,29 or investigator designed or adapted acceptability measures.31,35 Most studies provided detailed descriptions of psychometric properties of instruments chosen to measure survivor outcomes, but only a few reported internal consistency or other psychometric data using their current sample.29,32
Measurement of Caregiver Outcomes
Caregiver outcomes were measured in all 18 studies. Used in 6 studies, the Zarit Burden Interview was the most common measure.20,21,25–27,36 Other measures for burden, strain, and stress included the Oberst Caregiving Burden Scale,22 Chinese Version of the Caregiver Burden Inventory,32 Caregiving Strain Index,19 Perceived Stress Scale,23 PTSD Checklist Civilian Version for post-traumatic stress symptom severity,29 Family Appraisal of Caring Questionnaire,24 and Measure of Current Status Part A.29
Caregiver preparedness and related concepts were measured using the Caregiving Competency Scale,19 Problem Solving Inventory,19 Cognitive and Affective Mindfulness Scale-Revised,29 Connor Davidson Resilience Scale,35 General Self-Efficacy Scale,29 and the Revised Scale for Caregiving Self-Efficacy.30 Positive aspects of caregiving were measured by the Chinese Version of the Perceived Benefits of Caregiving Scale,20 Chinese Version of Positive Aspects of Caregiver Questionnaire,32 and a Positive Appraisal of the Impact of Caring subscale from the Family Appraisal of Caring Questionnaire.24
Caregiver anxiety and depression were measured in 5 studies using the Hospital Anxiety and Depression Scale.24–26,28,29 Other anxiety and depression measures included the Center for Epidemiological Studies Depression Scale,19,21,30 PROMIS-Depression Short Form 8b,35 Patient Health Questionnaire-9 (PHQ-9),31 Beck Depression Scale,27 Zung Self-rating Anxiety Scale,28 and the Zung Self-Rating Depression Scale.28
Several studies measured caregiver health-related quality of life using the same measures that were used for stroke survivors (i.e., Older People’s Quality of Life Questionnaire,35 the Satisfaction with Life Scale,32 and the EuroQol EQ5D-5L24,25). Other measures for caregiver quality of life included the Medical Outcomes Study Quality of Life Scale Short Form (SF-36; SF-12),19,36 Brief World Health Organization Quality of Life Instrument (WHOQOL-Bref),23 Adult Carer Quality of Life Questionnaire,20 and the Bakas Caregiving Outcomes Scale.22,31 Interestingly, from a health-related quality of life standpoint, one study measured caregiver pain using a Visual Analogue Scale,23 and another measured fatigue using the Piper Fatigue Scale.30
Many of the studies addressed the caregivers’ social functioning, dyadic interactions, and the quality of relationship with the survivor. Measures used were the Social Support Questionnaire,19 Social Relationships Index,35 Active Engagement Communication Scale,31 Protective Buffering Communication Scale,31 McMaster Family Assessment Device General Functioning Subscale,19,31 Patient Expectations Scale,31 Perceived Criticism Scale,31 Communication in Marriage Questionnaire,33 Intimate Bond Measure,29 Dyadic Adjustment Scale,34 Mutuality Scale,31 and the Relationship Assessment Scale.31 One study used the Family Caregiver Conflict Scale.30
A few studies measured caregiver satisfaction with the intervention using the Client Satisfaction Questionnaire29 or acceptability measures designed or adapted by the investigator.31,35 As with measurements for survivor outcomes, instruments chosen to measure caregiver outcomes had good psychometric properties cited from the literature, yet only a few studies reported internal consistency or other psychometric data using their current samples.29,32
Do family caregiver and dyad interventions improve survivor outcomes?
Of the 18 studies reviewed, only 3 caregiver19,20,28 and 3 dyad32–34 intervention studies reported testing for significance in survivor outcomes. One caregiver intervention study reported improvements in survivor cognition, depression, and anxiety.28 Two studies reported improvements in the survivor’s quality of life or life satisfaction.20,32 Another dyad study found improvements in survivor support toward and from the caregiver, engagement from the caregiver, and lower depreciation toward and from the caregiver; however, these findings were only significant for certain subgroups who had fluent and non-fluent aphasia.33 Using the same sample, another study found that the dyad intervention improved overall relationship quality, relationship consensus, relationship satisfaction, and affectional expression.34 One caregiver study reported no significant impact of the intervention on the survivor’s placement into a residential care home.19 Several studies reported survivor outcome data trends, but were not powered to detect significance in survivor outcomes.25,29–31,35 The small number of studies made it difficult to draw any firm conclusions regarding the impact of caregiver and dyad interventions on survivor outcomes.
Do family caregiver and dyad interventions improve caregiver outcomes?
A total of 7 caregiver19,20,22,23,26–28 and 4 dyad32–34,36 intervention studies reported significant improvements in caregiver outcomes. Some evidence supports that caregiver and dyad interventions improved caregiver burden at one or more follow-up time points;19,20,22,26,32,36 however, two studies reported non-significant group differences for burden.21,27 Additional improvements in caregiver outcomes included caregiver competence,19 problem solving,19 benefit finding,20 and increased positive aspects;32 although, perceived stress was not significant in one study,23 and carer strain, distress, and positive appraisal were not significant in another.24
Only one study reported significant improvements in caregiver anxiety and depression at 6 and 12 months,26 although anxiety and depression were not significant at 3 months.26 Several studies reported non-significant between group findings regarding depression,24,77 depressive symptoms,19,21 and anxiety.24
Three studies showed significant improvements in quality of life,20 life satisfaction,32 and life changes as a result of providing care;22 conversely, several studies reported non-significant findings regarding several quality of life domains, including perceived physical health.19,23,24,36 Meanwhile, a few studies reported significant improvements in a few quality of life domains such as mental role,36 vitality,36 physical health,23 and pain in the neck, right shoulder, and both knees.23
Some studies reported significant improvements in social support,19 social relations,23 family functioning,19 increased support from the survivor,33 and increased engagement toward and from the survivor;33 however, certain subgroups of caregivers of fluent and non-fluent aphasia survivors had non-significant findings regarding support toward the survivor, engagement toward and from the survivor, and depreciation toward and from the survivor.33 One dyad study found that, although the overall relationship quality and relationship consensus improved between the survivor and the caregiver, there were no significant differences with respect to relationship cohesion, relationship satisfaction, and affectional expression.34
Two caregiver intervention studies reported no significant findings for any of their measured caregiver outcomes.21,24 Another 5 studies reported data trends, but were not powered to detect significance in caregiver outcomes.25,29–31,35 As with the studies that measured survivor outcomes, the small number of studies that tested caregiver outcomes, and conflicting results, made it difficult to draw any firm conclusions regarding the impact of caregiver and dyad interventions on caregiver outcomes.
Generalizability
A majority of the stroke caregiver and dyad intervention studies recruited participants from inpatient acute care settings19,26,28,29–31,33,34 or from the community.20–25,27,32,35,36 Few studies represented longer-term caregivers of stroke survivors providing care for more than one year post stroke,36 or caregivers of younger stroke survivors averaging under 60 years of age.29,33,34,35 While some studies had a mixture of spouse, adult child, and other caregivers,19,20,23,28,30,36 most of the studies had samples that were predominately spousal caregivers making up over 70% of the sample.21,22,24–27,29,31–35 Providing a global perspective, the studies represented 7 countries from around the world including China (n=5),19,20,26,28,32 United States (n=5),21,29–31,35 Poland (n=2),33,34 Turkey (n=2),27,36 United Kingdom (n=2),24,25 Brazil (n=1),23 and Canada (n=1).22 While global representation is important, results should be interpreted with caution as these countries have very different healthcare systems and resources.
What Types of Family Caregiver and Dyad Interventions are the Best?
Target of Interventions
The studies in this review were compared with prior recommendations6,7 and found to be somewhat consistent. Studies testing caregiver interventions rarely tested survivor outcomes,20,28 yet reported improvement in a number of caregiver outcomes.19,20,22,23,26 Dyad interventions appeared to improve more survivor outcomes,32,33,34 yet, unlike prior reviews,6,7 dyad studies in this review improved a number of caregiver outcomes as well.32,33,34,36 Half of the dyad intervention studies (n=4) were too small to test significance of stroke survivor and caregiver outcomes.29–31,35
Types of Interventions
Consistent with prior recommendations,6,7 most studies (n=13) reported interventions that used a combination of skill-building and psychoeducational strategies.19–26,28–32 Although most of these studies were not powered to detect significance,21,25,29–31,35 5 of these studies resulted in positive caregiver and survivor outcomes.19,20,26,28,32 Two studies used skill-building strategies alone; one used relaxation to manage stress with no between group differences in caregiver burden or depression,27 and another used stress management and goal setting that was not powered to detect significance.35 Interestingly, 3 dyad intervention studies used psychoeducational strategies alone, with some improvement in survivor and caregiver outcomes,33,34,36 although two of those studies were from the same sample and had mixed results.33,34 Despite the popularity of stroke support groups and peer support used in practice settings, none of the studies added support groups or peer support (i.e., interactions with peers) as an intervention component. Over half of the studies reported that intervention components or selection of outcomes were theoretically-based (i.e., based on an existing theory, model, or conceptual framework).19–21,25,30–36
Intervention Delivery Design
Prior reviews recommended assessment of caregiver needs, and to tailor or individualize stroke caregiver and dyad interventions.6,7 Less than half of the intervention studies (n=7) mentioned assessment and/or tailoring of the intervention to the needs of stroke family caregivers or dyads.20,21,22,24,29,31,32 Although some were not powered to detect significance,21,29,31 others resulted in improve caregiver and survivor outcomes.20,22,32 Two additional studies implemented assessment and/or tailoring based only on the survivor’s condition or needs.28,36
Mode of Delivery
As in prior reviews,6,7 most interventions were delivered either face to face (n=8),22–26,28,35,36 by telephone (n=5),21,30,32–34 or a combination of face to face and telephone (n=3).19,20,27 Of the studies powered for analysis, most resulted in positive caregiver and survivor outcomes.22,23,26,28,32–34,36 Three of the studies had interventions that were delivered in group sessions.25,33,34 One of these gave caregivers the choice of attending group sessions or receiving one-on-one sessions, yet was not powered to detect significance.25 The other 2 studies were from the same sample using the same group intervention yielding mixed results.33,34 Only 2 studies reported using web-based modes of delivery,29,31 and those were limited to online videoconferencing and were not powered to detect significance. Of these 2 studies, one used a combination of face to face and videoconferencing,29 and the other used a combination of face to face, telephone, and videoconferencing.31 While LeLaurin and colleagues21 reported that their sessions were delivered by telephone, their intervention materials were posted on a website; the small sample size was cited as reason for non-significant results. No other studies reported using a website or electronic means to deliver intervention materials.
Frequency of Sessions
Prior recommendations suggest 5 to 9 sessions for caregiver and dyad interventions, with a wide range of sessions being not as useful.6,7 The frequency of sessions ranged from 1 session23,24,35 to 24 sessions.26 The studies with 1 session had several non-significant findings,23,24 or were not powered to detect significance.35 The study with 24 sessions reported mixed results with respect to improving burden, anxiety, and depression based on different time points.26 Seven of the 18 studies were within the recommended 5 to 9 sessions.19,20,25,29,31,32,36 Of those, 3 were not were powered to detect significance,25,29,31 and 4 resulted in positive caregiver or survivor outcomes.19,20,32,36 None of the studies had a wide range of sessions, although 2 studies offered a varied number of sessions;22,28 one improved survivor outcomes,28 the other caregiver outcomes.22 Overall, the studies reviewed provided further support for the recommendation of 5 to 9 sessions for caregiver and dyad interventions.6,7
Discussion
Best Designed Studies
Among the 10 stroke family caregiver intervention studies cited in this review, one stood out as the best designed study.19 Cheng and colleagues19 conducted a prospective multi-center randomized controlled trial in Hong Kong at one acute care and two rehabilitation facilities. A total of 128 dyads were randomly assigned to either a control group who received usual care or the intervention group who received a 26-week strength oriented psychoeducational program. Dyads received 2 structured face-to-face educational sessions covering stroke and caregiver skills prior to discharge, and 6 problem-solving coping skills training sessions by telephone post discharge. Data collection occurred at baseline, and at 1 and 3 months follow-up. The intervention group had significantly greater improvement in caregiver competence, problem solving abilities, social support, family functioning, and burden. Despite these positive outcome gains in the intervention group, there was no significant positive effect on assisting stroke survivors to remain at home. Study strengths were the Cronbach alpha reliabilities of the seven measurement instruments ranging from .79 to .93 for this sample, and the random assignment of participants to the groups. Possible study weaknesses were the burden of completing six instruments at each data point, and no mention of assessment of intervention fidelity.
Among the 8 dyad studies reviewed here, the study by Mei and colleagues32 was exceptionally well-designed and executed. These researchers tested the effects of an 8-week modified reminiscence therapy program for stroke spousal dyads living in Zhengzhou, China. Outcomes were assessed in three groups (therapy group attended by dyads, therapy group attended by caregiving spouses only, control group) with minimal attrition at four time points. Data collectors were blinded to condition. The investigators documented sustained benefits of the program among participants of both therapy groups, compared with controls, for survivor outcomes (increased life satisfaction), as well as caregiver outcomes (increased life satisfaction, increased recognition of the positive aspects of caregiving, decreased burden). Potential weaknesses of the study included its modest sample size (N=75 dyads), randomization at the provider level rather than at the participant level, and lack of generalizability to other dyads types including adult child-parent dyads.
The two previous systematic reviews on stroke caregiver and dyad interventions6,7 cited 4 best designed studies based on adequate sample size and rigorous randomized controlled clinical trial designs.42–45 One of these studies42 used an attention control group who received the same number of sessions as the intervention group, reported detailed procedures for monitoring and maintaining treatment fidelity,41,42 and used more than one type of skill-building as part of the intervention.42 A newer version of this intervention is underway adding telehealth technology preferences for caregivers to access the intervention,46 and an additional skill-building tip sheet on goal setting to improve caregiver health.47 Of the 4 well-designed studies previously reviewed,6,7 only 2 reported stroke survivor outcomes,43,44 one of which was a dyad intervention study.44
As reported in the two prior systematic reviews,6,7 as well as the current review, there were many feasibility studies with small sample sizes that need to be tested in larger, well-powered randomized controlled clinical trials. Unfortunately, the smaller feasibility studies from the prior reviews6,7 were not found as larger randomized controlled clinical trials in the current review. Although there are several possible reasons for this lack of progression, such as an increasingly competitive funding climate for larger trials, much can be learned from smaller feasibility pilot studies. Researchers are encouraged to build upon and refine their preliminary work in pursuing larger, more rigorous randomized controlled clinical trials in the future.
Comparison of Findings with Recommendations
Recommendations from the two prior systematic reviews of stroke family caregiver and dyad interventions6,7 were supported, with insufficient evidence from this review to suggest changes. Few caregiver interventions measured survivor outcomes, yet resulted in improvement in a number of caregiver outcomes. Dyad interventions were associated with improvement in survivor outcomes, with some studies reporting improvement in caregiver outcomes. This is an improvement over prior reviews,6,7 showing that some dyad interventions are resulting in better outcomes for caregivers.32,33,34,36 Consistent with recommendations,6,7 most of the interventions combined skill-building strategies (e.g., problem solving, stress management, goal setting) with psychoeducation, and resulted in better caregiver and survivor outcomes.19,20,26,28,32 The studies that used assessment and tailoring of interventions were more successful.20,22,32 The recommendation of 5 to 9 sessions6,7 was supported as well; all studies powered to detect improvement that fell within this range showed significant improvement.19,20,32,36
As in prior reviews,6,7 most studies were delivered in person, by telephone, or a combination of the two. These studies resulted in better survivor and caregiver outcomes.22,23,26,28,32–34,36 Only a few studies used online videoconferencing,29,31 or provided intervention materials on a website.21 Unfortunately, the sample sizes in these studies were too small to detect significant outcomes.21,29,31 The recommendation to consider interventions delivered by the Web for those with computer access6,7 was consistent with findings from the literature.46,48–51 According to a systematic review of technology-based dyadic interventions targeting chronically ill adults (e.g., heart failure, diabetes, cancer, and depression) and their family caregivers,51 educational, behavioral, and support interventions have been successfully delivered using a variety of technologies (e.g., text messaging, email, discussion board, videoconference, website, video, and interactive voice response calls). However, challenges were reported, such as connectivity issues and impersonality of the computer when accessing web-based interventions.51 Social networking may be a viable option for future stroke caregiver and dyad interventions, although stroke caregivers have reported mixed feelings about the use of Facebook.46 Some caregivers said they would use this social network to “look up things” or to “get little ideas,” and others stated that Facebook has “so many fake things,” or that they do not use social media.46 Several sources have advocated for the need to deliver interventions based on caregiver preferences for the use of technology,46,48–50 especially during the COVID-19 pandemic when in person resources are scarce.52–55 While several studies have revealed that family caregivers are receptive to new technologies,46,48–51 not all caregivers possess the skills, electronic devices, or Wifi connections needed to use new technologies, such as websites, apps, eBooks, videoconferencing, or social networking.46,51 Designing multiple modes of delivery for interventions will allow stroke caregivers to choose types of technologies based on their own preferences that best meet their needs.46,48–50 During the COVID-19 pandemic, the use of technology became more urgent when institutions limited family caregiver access to patients during acute and rehabilitation inpatient stays.52–54 One study reported that stroke family caregiver training during COVID-19 was limited to the day of inpatient rehabilitation discharge.54 Another study highlighted the impact of the COVID-19 pandemic on stroke family caregivers struggling to provide care in the community.55 Remote caregiver education is needed given the impact that the COVID-19 pandemic has had on stroke systems of care and the training of stroke family caregivers.52,54,55
Limitations
A major limitation for most of the 18 studies reviewed pertained to sample size, as well as generalizability. Adult child and other types of non-spousal caregivers were poorly represented, as were caregivers who had been providing care for younger stroke survivors, or long-term caregivers providing care for more than a year. While the studies were conducted in a variety of countries, different healthcare systems and resources raise caution in interpretation of the findings. Furthermore, the promotion of health equity, which includes targeting interventions to underserved communities and working to ensure equal access regardless of ethnicity, race, or socioeconomic status, was not addressed in the studies reviewed; yet is urgently needed to ensure better care for all stroke survivors and their family caregivers. Access to care and tailoring to marginalized communities are critical in designing, testing, and implementing stroke caregiver and dyad interventions. Treatment fidelity and the potential for treatment diffusion were rarely addressed, as were internal consistency reliability of measures for the samples in which they were used. Despite most studies using a randomized controlled clinical trial design, a few randomized clusters based on healthcare organizations or providers,24,32 or used less rigorous single-group quasi-experimental designs.22,30,35 While over half of the studies were theoretically-based in some way,19–21,25,30–36 only a few cited the use of theoretical mechanisms around family systems or dyadic principles.31,34,35 These types of theoretical mechanisms could enhance future stroke caregiver and dyad intervention development.51
This review was limited in that only stroke caregiver and dyad interventions that targeted the health and well-being of family caregivers met inclusion criteria. There may have been studies that benefitted caregivers that were targeted solely on the survivor’s care needs. While this review was narrowly focused on interventions that specifically targeted family caregivers, it provided an important update to two other prior systematic reviews6,7 that used the same rigorous methods for article selection, critique, analysis, and synthesis of the evidence pertaining to the impact of family caregiver and dyad interventions.
Summary and Conclusions
Recommendations from two prior reviews6,7 were generally supported based on a rigorous review of 18 stroke caregiver and dyad intervention studies. There was no compelling evidence to modify these recommendations.6,7 When designing and implementing stroke caregiver and dyad interventions, researchers and clinicians are urged to consider these recommendations (Bakas et al., 2014 p. 2843; Bakas et al., 2017 p. 1 Supplemental Material):6,7
“Stroke caregiver interventions are probably recommended over dyad interventions for caregiver outcomes; vice versa for survivor outcomes.” However, a few dyad intervention studies in this review have shown improvement in caregiver outcomes.32,33,34,36
“Interventions that combine skill building (e.g., problem solving, stress management, goal setting) with psychoeducational strategies should be chosen; interventions that involve only psycho-education are not recommended; interventions that consist of support only or a combination of psycho-education and support do not have sufficiently strong evidence.” Studies that combined skilled building with psychoeducation in this review provided the most positive caregiver and survivor outcomes.19,20,26,28,32
“Interventions that are tailored or individualized on the basis of the needs of stroke caregivers should be chosen; post-discharge assessments with tailored interventions based on changing needs should be performed; individual approaches are probably recommended over group interventions.” There was evidence in this review that tailoring based on caregiver needs improved caregiver and survivor outcomes.20,22,32
“Interventions that are delivered face to face and/or by telephone are recommended; Interventions delivered completely by telephone can be useful; interventions by the Web might be considered for those with computer access.” Studies in this review that had interventions delivered face to face and/or by telephone resulted in positive caregiver and survivor outcomes.22,23,26,28,32–34,36
“Interventions consisting of 5 to 9 sessions are recommended; those with a wide range of sessions are not as useful.” Most studies in this review were within the recommended 5 to 9 sessions; four provided evidence of improving survivor or caregiver outcomes.19,20,32,36
Only 6 of the 18 stroke caregiver and dyad intervention studies reported significant survivor outcomes. Only 11 of the 18 stroke caregiver and dyad intervention studies reported significant caregiver outcomes, the most common being burden. A number of survivor and caregiver outcomes were not significant, or only significant for certain subgroups. The limited number of studies, small sample sizes, and conflicting results, made it difficult to draw firm conclusions regarding the impact of these interventions on outcomes. Well-designed and well-powered randomized controlled clinical trials are still needed to confirm efficacy of stroke family caregiver and dyad interventions. Researchers are encouraged to build upon their preliminary feasibility work to generate larger, more rigorous trials.
Supplementary Material
Acknowledgements
We would like to acknowledge the assistance of Angelica Sanchez, a graduate student at Northern Arizona University in Flagstaff, AZ. Ms. Sanchez assisted with the search and location of full-text articles for the review. No other persons have made substantial contributions to this manuscript.
Sources of Funding
Dr. Bakas’ time in preparing this manuscript was supported by the National Institute of Nursing Research of the National Institutes of Health (R21NR016992). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflicts of Interest and Disclosures
Dr. Bakas has received prior stroke family caregiver research funding from the National Institutes of Health, National Institute of Nursing Research, R21NR016992, R01NR010388, K01NR008712. Dr. McCarthy has received prior stroke dyad research funding from the American Heart Association, 17MCPRP33670674. The other author reports no conflicts.
Non-standard Abbreviations and Acronyms:
- CINAHL
Cumulative Index to Nursing and Allied Health Literature
- CONSORT
Consolidated Standards of Reporting Trials
- EQ5D-5L
European Quality of Life EuroQol
- PRISMA
Preferred Reporting Items for Systematic reviews and Meta-Analyses
- PHQ-9
Patient Health Questionnaire
- PROMIS
Patient-Reported Outcomes Measurement Information System
- PTSD
Post Traumatic Stress Disorder
- SF-36; SF-12
Medical Outcomes Study Quality of Life Scale Short Form
- TREND
Transparent Reporting of Evaluations with Nonrandomized Designs
- WHOQOL-Bref
Brief World Health Organization Quality of Life Instrument
Footnotes
Registration and Protocol
The review was not registered, and a protocol was not prepared.
Supplemental Materials
Supplemental Tables S1–S3 provide the search strategy text, and summarize information from the 10 caregiver and 8 dyad intervention articles. These are provided as an online supplement for the journal Stroke. Please see https://www.ahajournals.org/journal/str.
(STROKE/2020/034090R5)
References
- 1.World Health Organization: The Top 10 Causes of Death. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed March 29, 2021.
- 2.Katan M, Luft A. Global Burden of Stroke. Seminars in Neurology. 2018;38:208–211. 10.1055/s-0038-1649503. [DOI] [PubMed] [Google Scholar]
- 3.Battersby M, Hoffmann S, Cadilhac D, Osborne R, Lalor E, Lindley R. ‘Getting Your Life Back on Track After Stroke’: A Phase II Multi‐Centered, Single-Blind, Randomized, Controlled Trial of the Stroke Self‐Management Program vs. The Stanford Chronic Condition Self‐Management Program or Standard Care in Stroke Survivors. International Journal of Stroke. 2009;4:137–144. 10.1111/j.1747-4949.2009.00261.x. [DOI] [PubMed] [Google Scholar]
- 4.Skolarus Lesli E., Freedman Vicki A., Feng Chunyang, Wing Jeffrey J., Burke James F.. Care Received by Elderly US Stroke Survivors May Be Underestimated. Stroke. 2016;47:2090–2095. 10.1161/STROKEAHA.116.012704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oliva-Moreno J, Aranda-Reneo I, Vilaplana-Prieto C, González-Domínguez A, Hidalgo-Vega A. Economic Valuation of Informal Care in Cerebrovascular Accident Survivors in Spain. BMC Health Serv Res. 2013;13:508. 10.1186/1472-6963-13-508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bakas T, Clark PC, Kelly-Hayes M, King RB, Lutz BJ, Miller E. on Behalf of the American Heart Association Council on Cardiovascular and Stroke Nursing and the Stroke Council. Evidence for Stroke Family Caregiver and Dyad Interventions: A Statement for Healthcare Professionals from the American Heart Association. Stroke. 2014;45:2836–2852. 10.1161/STR.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 7.Bakas T, McCarthy M, Miller E. An Update on the State of the Evidence for Stroke Family Caregiver and Dyad Interventions. Stroke. 2017;48; e122–e125. 10.1161/STROKEAHA.117.016052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farahani MA, Bahloli S, JamshidiOrak R, Ghaffari J. Investigating the Needs of Family Caregivers of Older Stroke Patients: A Longitudinal Study in Iran.” BMC Geriatrics. 2020;20:313. 10.1186/s12877-020-01670-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Young HM, Bell JF, Whitney RL, Ridberg RA, Reed SC, Vitaliano PP. Social Determinants of Health: Underreported Heterogeneity in Systematic Reviews of Caregiver Interventions. Gerontologist. 2020;60(Suppl 1):S14–S28. 10.1093/geront/gnz148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.AARP and NAC. Caregiving in the U.S May 2020. https://www.aarp.org/content/dam/aarp/ppi/2020/05/full-report-caregiving-in-the-united-states.doi.10.26419-2Fppi.00103.001.pdf. Accessed March 29, 2021.
- 11.Centers for Disease Control. Caregiving for the Family and Friends – A Public Health Issue. 2018. https://www.cdc.gov/aging/agingdata/docs/caregiver-brief-508.pdf. Accessed April 28, 2021.
- 12.National Alliance for Caregiving. 2020. https://www.caregiving.org/. Accessed April 29, 2021.
- 13.Schulz R, Beach SR, Czaja SJ, Martire LM, Monin JK. Family Caregiving for Older Adults. Annual Review of Psychology. 2020;71:635–659. 10.1146/annurev-psych-010419-050754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Denham AM, Wynne O, Baker AL, Spratt NJ, Bonevski B. The Unmet Needs of Carers of Stroke Survivors: An Evaluation of Google Search Results. Health Informatics Journal. 2020;26:934–944. 10.1177/1460458219852530. [DOI] [PubMed] [Google Scholar]
- 15.Drummond M, Johnston B, Quinn TJ. Measuring the Success of Interventions for Caregivers: A Focused Systematic Review. Current Opinion in Supportive and Palliative Care. 2019;13:351–159. 10.1097/SPC.0000000000000461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thomas S, Dalton J, Harden M, Eastwood A, Parker G. Updated Meta-Review of Evidence on Support for Carers. NIHR Journals Library. 2017. 10.3310/hsdr05120. [DOI] [PubMed] [Google Scholar]
- 17.Pucciarelli G, Lommi M, Magwood GS, Simeone S, Colaceci S, Vellone E, Alvaro R. Effectiveness of Dyadic Interventions to Improve Stroke Patient-Caregiver Dyads’ Outcomes After Discharge: A Systematic Review and Meta-Analysis Study. Eur J Cardiovas Nurs. 2021;20:14–33. 10.1177/1474515120926069. [DOI] [PubMed] [Google Scholar]
- 18.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ. 2021;372:n71. 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheng HY, Chair SY, Chau JPC. Effectiveness of a Strength-Oriented Psychoeducation on Caregiving Competence, Problem-Solving Abilities, Psychosocial Outcomes and Physical Health Among Family Caregiver of Stroke Survivors: A Randomised Controlled Trial. International Journal of Nursing Studies. 2018;87:84–93. 10.1016/j.ijnurstu.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 20.Fu B, Mei Y, Lin B, Guo Y, Zhang Z, Qi B, Wang Y. Effects of a Benefit-Finding Intervention in Stroke Caregivers in Communities. Clinical Gerontologist. 2020. 10.1080/07317115.2020.1765062. Accessed April 27, 2021. [DOI] [PubMed] [Google Scholar]
- 21.LeLaurin JH, Freytes IM, Findley KE, Schmitzberger MK, Eliazar-Macke ND, Orozco T, Uphold CR. Feasibility and Acceptability of a Telephone and Web-Based Stroke Caregiver Intervention: A Pilot Randomized Controlled Trial of the RESCUE Intervention. Clinical Rehabilitation. 2021;35:253–265. 10.1177/0269215520957004. [DOI] [PubMed] [Google Scholar]
- 22.Mores G, Whiteman RM, Ploeg J, Knobl P, Cahn M, Klaponski L, Lindley A, Fisher K. An Evaluation of the Family Informal Caregiver Stroke Self-Management Program. Canadian Journal of Neurological Sciences Inc. 2018;45:660–668. 10.1017/cjn.2018.335. [DOI] [PubMed] [Google Scholar]
- 23.Moreira KLdeA, Abalos-Medina GM, Villaverde-Gutierrez C, de Lucena MG, de Oliveira ABC, Perez-Marmol JM. Effectiveness of Two Home Ergonomic Programs in Reducing Pain and Enhancing Quality of Life in Informal Caregivers of Post-Stroke Patients: A Pilot Randomized Controlled Clinical Trial. Disability and Health Journal. 2018;11:471–477. 10.1016/j.dhjo.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 24.Patchwood E, Woodward-Nutt K, Rhodes SA, Batistatou E, Camacho E, Knowles S, Darley S, Grande G, Ewing G, Bowen A. Organising Support for Carers of Stroke Survivors (OSCARSS): A Cluster Randomized Controlled Trial with Economic Evaluation. BMJ Open. 2021;11:e038777. 10.1136/bmjopen-2020-038777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walker MF, Birchall S, Cobley C, Condon L, Fisher R, Fletcher-Smith J, Golding-Day MR, Greensmith C, Kontou E, Matias O et al. Biopsychosocial Intervention for Stroke Carers (BISC): Results of a Feasibility Randomized Controlled Trial and Nested Qualitative Interview Study. Clinical Rehabilitation. 2020;34:1268–1281. 10.1177/0269215520937039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang J, Liu J, Li L, Man J, Yue S, Liu Z. Effect of Education and Muscle Relaxation Program on Anxiety, Depression, and Care Burden in Caregivers of Acute Stroke Survivors: A Randomized, Controlled Study. Medicine. 2021;100:r(e24154). 10.1097/MD.0000000000024154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yilmaz CK, Asiret GD, Cetinkaya F, Oludag G, Kapucu S. Effect of Progressive Muscle Relaxation on the Caregiver Burden and Level of Depression Among Caregivers of Older Patients with a Stroke: A Randomized Controlled Trial. Japan Journal of Nursing Science. 2019;16:202–211. 10.1111/jjns.12234. [DOI] [PubMed] [Google Scholar]
- 28.Zhang L, Zhang T, Sun Y. A Newly Designed Intensive Caregiver Education Program Reduces Cognitive Impairment, Anxiety, and Depression in Patients with Acute Ischemic Stroke. Brazilian Journal of Medical and Biological Research. 2019;52:e8533. 10.1590/1414-431X20198533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bannon S, Lester EG, Gates MV, McCurley J, Lin A, Rosand J, Vranceanu A. Recovering Together: Building Resiliency in Dyads of Stroke Patients and Their Caregivers At Risk for Chronic Emotional Distress; A Feasibility Study. Pilot and Feasibility Studies. 2020;6:75. 10.1186/s40814-020-00615-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Blanton S, Scheibe DC, Rutledge AH, Regan B, O-Sullivan CS, Clark PC. Family-Centered Care During Constraint-Induced Therapy After Chronic Stroke: A Feasibility Study. Rehabilitation Nursing. 2019;44:349–357. 10.1097/rnj.0000000000000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCarthy MJ, Sanchez A, Garcia YE, Lyons KS, Bakas T. Feasibility of the Hand in Hand Relationship Intervention for Stroke Survivor-Caregiver Dyads: A Randomized Trial. Research on Social Work Practice. 2020. 10.1177/1049731520961172. [DOI] [Google Scholar]
- 32.Mei Y, Lin B, Li Y, Ding C, Zhang Z. Effects of Modified 8-Week Reminiscence Therapy on the Older Spouse Caregivers of Stroke Survivors in Chinese Communities: A Randomized Controlled Trial. International Journal of Geriatric Psychiatry. 2018;33:633–641. 10.1002/gps.4833. [DOI] [PubMed] [Google Scholar]
- 33.Orlowska E, Rasmus A, Goral-Polrola J, Morga R, Pachalska M. The Long-Time Effects of Group Therapy Intervention on Marriage Communication Between Fluent and Non-Fluent Aphasic Patients and their Spouses: Who Benefits the Most? ACTA Neuropsychologica. 2018;16:229–241. [Google Scholar]
- 34.Rasmus A, Orlowska E. Marriage and PostStroke Aphasia: The Long-Time Effects of Group Therapy of Fluent and Non-Fluent Aphasic Patients and Their Spouses. Frontiers in Psychology. 2020. 10.3389/fpsyg.2020.01574.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Terrill AL, Reblin M, MacKenzie JJ, Cardell B, Einerson J, Berg C, Majersik JJ, Richards L. Development of a Novel Positive Psychology-Based Intervention for Couples Post-Stroke. Rehabilitation Psychology. 2018;63:43–54. 10.1037/rep0000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ugur HG, Erci B. The Effect of Home Care for Stroke Patients and Education of Caregivers on the Caregiver Burden and Quality of Life. Acta Clin Croat. 2019;58:321–332. 10.20471/acc.2019.58.02.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schulz KF, Altman DG, Moher D for the CONSORT Group. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomized Trials. BMJ. 2010;340:698–702. 10.1136/bmj.c332. [DOI] [Google Scholar]
- 38.Des Jarlais DC, Lyles C, Crepaz N, and the TREND Group. Improving the Reporting Quality of Nonrandomized Evaluations of Behavioral and Public Health Interventions: The TREND Statement. American Journal of Public Health. 2004;94:361–366. 10.2105/ajph.94.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston: Houghton Mifflin Company; 2002. [Google Scholar]
- 40.Leon AC, Davis LL, Kraemer HC. The Role and Interpretation of Pilot Studies in Clinical Research. J Psychiatr Res. 2011;45:626–629. 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McLennon SM, Hancock RD, Redelman K, Scarton LL, Riley E, Sweeney B, Habermann B, Jessup NM, Bakas T. Comparing Treatment Fidelity Between Study Arms of a Randomized Controlled Clinical Trial for Stroke Family Caregivers. Clinical Rehabilitation. 2016;30:495–507. 10.1177/0269215515585134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bakas T, Austin JK, Habermann B, Jessup NM, McLennon SM, Mitchell PH, Morrison G, Yang Z, Stump TE, Weaver MT. Telephone Assessment and Skill-Building Kit for Stroke Caregivers: A Randomized Controlled Clinical Trial. Stroke. 2015;46:3478–3487. 10.1161/STROKEAHA.115.011099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kalra L, Evans A, Perez I, Melbourn A, Patel A, Knapp M, Donaldson N. Training Carers of Stroke Patients: Randomised Controlled Trial. BMJ. 2004;328:1099. 10.1136/bmj.328.7448.1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ostwald SK, Godwin KM, Cron SG, Kelley CP, Hersch G, Davis S. Home-Based Psychoeducational and Mailed Information Programs for Stroke-Caregiving Dyads Post-Discharge: A Randomized Trial. Disabil Rehabil. 2014;36:55–62. 10.3109/09638288.2013.777806. [DOI] [PubMed] [Google Scholar]
- 45.Pfeiffer K, Beische D, Hautzinger M, Berry JW, Wengert J, Hoffrichter R, Becker C, van Schack R, Ellitott TR. Telephone-Based Problem-Solving Intervention for Family Caregivers of Stroke Survivors: A Randomized Controlled Trial. J Consult Clin Psychol. 2014;82:628–643. 10.1037/a0036987. [DOI] [PubMed] [Google Scholar]
- 46.Bakas T, McCarthy MJ, Israel J, Brehm BJ, Dunning K, Rota M, Turner M, Miller EL. Adapting the Telephone Assessment and Skill-Building Kit to the Telehealth Technology Preferences of Stroke Family Caregivers. Research in Nursing and Health (RINAH). 2021;44:81–91. 10.1002/nur.22075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bakas T, Jones H, Israel J, Kum C, Miller EL. Designing and Evaluating a Goal Setting Tip Sheet for Stroke Family Caregiver Health. Rehabilitation Nursing. 2021;46:279–288. 10.1097/RNJ.0000000000000306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.National Alliance for Caregiving. E‐connected family caregiver: Bringing caregiving into the 21st century. 2011. https://www.caregiving.org/wp-content/uploads/2020/05/FINAL_eConnected_Family_Caregiver_Study_Jan-2011.pdf. Accessed April 28, 2021.
- 49.Aldehaim AY, Alotaibi FF, Uphold CR, Dang S. The Impact of Technology‐Based Interventions on Informal Caregivers of Stroke Survivors: A Systematic Review. Telemedicine and e‐Health. 2016;22:223–231. 10.1089/tmj.2015.0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chi N, Demiris D. A Systematic Review of Telehealth Tools and Interventions to Support Family Caregivers. Journal of Telemedicine and Telecare. 2015;21:37–44. 10.1177/1357633X14562734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Irani E, Niyomyart A, Hickman RL. Systematic Review of Technology-Based Interventions Targeting Chronically Ill Adults and Their Caregivers. Western Journal of Nursing Research. 2020;42:974–992. 10.1177/0193945919897011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bakas T, Commiskey P. Stroke Family Caregiving and the COVID-19 Pandemic: Impact and Future Directions. Stroke. 2021;52:1415–1417. 10.1161/STROKEAHA.120.033525. [DOI] [PubMed] [Google Scholar]
- 53.Leira EC, Russman AN, Biller J, Brown DL, Bushnell CD, Caso V, Chamorro A, Creutzfeldt CJ, Cruz-Flores S, Elkind MSV, et al. Preserving Stroke Care During the COVID-19 Pandemic: Potential Issues and Solutions. Neurology. 2020;95:124–133. 10.1212/WNL.0000000000009713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sutter-Leve R, Passint E, Ness D, Rindflesch A. The Caregiver Experience After Stroke in a COVID-19 Environment: A Qualitative Study in Inpatient Rehabilitation. J Neuro Phys Ther. 2021;45:14–20. 10.1097/NPT.0000000000000336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee JJ, Tsang WN, Yang S, Kwok JYY, Lou V, Lau KK. Qualitative Study of Chinese Stroke Caregivers’ Caregiving Experience During COVID-19 Pandemic. Stroke. 2020;52:1047–1414. 10.1161/STROKEAHA.120.032250. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


