Aneurysmal subarachnoid hemorrhage (aSAH) and the resulting delayed cerebral ischemia (DCI) carry significant morbidity and mortality. Hypercoagulability and microthrombosis are main mediators of DCI.1–3 Since classical laboratory tests do not provide a sensitive assessment of the coagulation status, we sought to examine the coagulation profile of aSAH patients using Thromboelastography (TEG). Published data suggests that TEG indices correlate with aSAH outcomes.1,2 The objective of this prospective study is to determine whether TEG predicts DCI and clinical outcomes after aSAH.
METHODS
The manuscript adheres to the AHA Journals’ implementation of the Transparency and Openness Promotion (TOP) Guidelines and data is available upon reasonable request.
This was a prospective observational study. TEG indices included R, K, MA, G, and alpha angle. These were correlated to DCI and 3-month modified-Rankin Scale(mRS). Samples were collected at predetermined time points: <24 hours(T1), 24–48 hours(T2), 3–5 days(T3), 6–9 days(T4), and ≥10 days(T5). A univariable analysis was conducted to determine variables associated with poor outcomes and DCI. These were validated in a multivariable analysis which included age, Hunt-Hess grade, Fisher scale, and co-morbidities. Receiver operating characteristics (ROC) were performed to determine predictive potential. For expanded methods, see Supplementary Material.
RESULTS
201 patients were enrolled. On univariate analysis, increased Hunt-Hess grade, Fisher scale and age correlated with poor 3-month mRS (3–6). Method of aneurysm treatment (endovascular versus surgical) was neither associated with outcome nor DCI. Of 201 patients, 70 developed DCI. Univariate analysis showed significant association between various TEG parameters and DCI. Findings were lost in multivariate analysis except for R, K and angle at T4 (p=0.03, 0.042 and 0.023 respectively).
Of 144 patients with 3-month follow-up, 63 had poor mRS(3–6). Several indices were significantly associated with poor outcome on univariate analysis. This was lost in multivariate analysis except for higher MA values at T1 and T5 (p=0.019 and 0.043 respectively) and G at T5 (p=0.017).
Using ROC analysis, TEG indices were not predictive of DCI or poor outcomes (Figure 1). 41 patients received antiplatelets (aspirin /Plavix) prior to/during the hospitalization and this did not affect mRS or DCI. Analysis excluding those patients showed that increased MA and G at T5 predicted poor 3-month mRS with an area under the curve (AUC) of 0.75 for each. For detailed results, see Supplementary Material.
Figure 1.
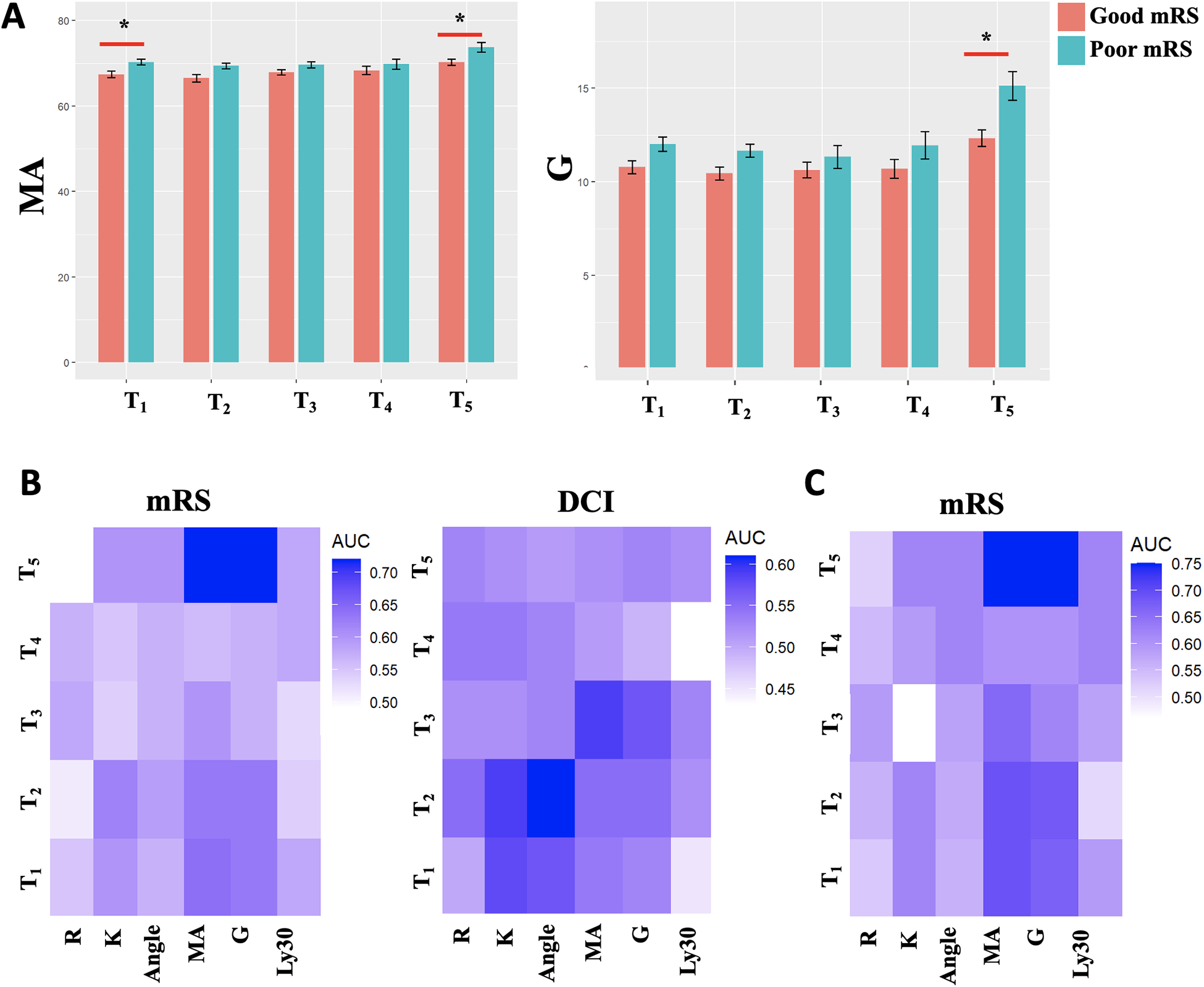
(A)MA values across time in relation to 3-month modified Rankin Scale(mRS). Asterix indicates significant difference on multivariate analysis. (B)Heatmap showing the area under the curve(AUC) for TEG indices across time to predict 3-month mRS(left) or delayed cerebral ischemia(right). (C)Heatmap for patients not on antiplatelets therapy
DISCUSSION
Evidence for hypercoagulability and microthrombosis after aSAH continues to accumulate. There is increased interest for evaluating platelet function and the coagulation cascade in association with outcomes and DCI. Prior studies have revealed associations between TEG indices and outcomes1,2 and proposed TEG as a predictive biomarker.3 These results were a promising development since TEG is a rapidly available test and widely used in ICU management. Our study reports the largest prospective cohort of aSAH undergoing serial TEG measurements in relation to mRS and DCI, and we hoped to confirm prior findings.
In our analysis, higher MA (hypercoagulable state) was associated with worse 3-month mRS. However, no parameter had a reliable predictive value for outcomes or DCI. Our data does not support the generalized use of TEG as a predictive biomarker in aSAH but suggests an association between poor outcomes and hypercoagulability. In the subset of patients that had not received antiplatelets, MA and G-values at T5 were predictive of poor outcomes at 3 months with acceptable accuracy. This finding is of unclear significance and necessitates further studies.
Supplementary Material
Funding:
Dr. Blackburn is supported by K23NS106054, R44NS110247
Dr. Li by UL1TR003167
Dr. McBride by 1R01NS115887
Dr. Pandit by 1R01NS121339
Disclosures:
Dr James Grotta serves as a consultant for Frazer ltd and Haemonetics Corporation. He received a TEG machine from Haemonetics to conduct reseatch. He received grant support from Chiesi USA, Inc, CSL Behring and Genetech.
Non-standard Abbreviations and Acronyms:
- DCI
Delayed cerebral ischemia
Footnotes
Supplemental Material:
References
- 1.Frontera JA, Aledort L, Gordon E, Egorova N, Moyle H, Patel A, Bederson JB, Sehba F. Early platelet activation, inflammation and acute brain injury after a subarachnoid hemorrhage:a pilot study. J Thromb Haemost. 2012;10:711–713.doi: 10.1111/j.1538-7836.2012.04651.x [DOI] [PubMed] [Google Scholar]
- 2.Frontera JA, Provencio JJ, Sehba FA, McIntyre TM, Nowacki AS, Gordon E, Weimer JM, Aledort L. The Role of Platelet Activation and Inflammation in Early Brain Injury Following Subarachnoid Hemorrhage. Neurocrit Care. 2017;26:48–57.doi: 10.1007/s12028-016-0292-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramchand P, Nyirjesy S, Frangos S, Doerfler S, Nawalinski K, Quattrone F, Ju C, Patel H, Driscoll N, Maloney-Wilensky E, et al. Thromboelastography Parameter Predicts Outcome After Subarachnoid Hemorrhage:An Exploratory Analysis. World Neurosurg. 2016.doi: 10.1016/j.wneu.2016.04.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


