This systematic review and meta-analysis assesses prevalence estimates of preadolescent self-injurious thoughts and behaviors, identifies correlates of these outcomes, and conducts head-to-head comparisons of preadolescent and adolescent self-injurious thoughts and behaviors in terms of associated characteristics.
Key Points
Question
What are the prevalence and correlates of preadolescent suicide and nonsuicidal self-injury?
Findings
In this systematic review and meta-analysis of 58 studies, lifetime prevalence of suicidal ideation, suicide attempts, and nonsuicidal self-injury were 15.1%, 2.6%, and 6.2%, respectively, in community samples, and lifetime prevalence of suicide was 0.79 per 1 million children in the general population. Male sex, child maltreatment, attention-deficit/hyperactivity disorder, and depression were associated with risk, whereas parental support may be protective against suicidal ideation.
Meaning
The prevalence of preadolescent suicidal thoughts and behaviors and nonsuicidal self-injury is concerning and underscores the need for additional research in this area.
Abstract
Importance
Considerably less is known about self-injurious thoughts and behaviors (SITBs) in preadolescence than older age groups, owing partly to the common view that young children are incapable of suicidal thoughts. Yet, preadolescent suicide has increased in recent years and is now the fifth leading cause of death in this age group, leading the National Institute of Mental Health to identify it as a priority for research and intervention.
Objective
To assess prevalence estimates of preadolescent SITBs, identify correlates of these outcomes, and conduct head-to-head comparisons of preadolescent and adolescent SITBs in terms of associated characteristics.
Data Sources
MEDLINE, PsycINFO, and Embase were systematically searched from inception through December 23, 2021, for studies on the prevalence and correlates of preadolescent SITBs. The search was restricted to English language publications and peer-reviewed journals.
Study Selection
Two reviewers independently identified studies providing data on prevalence and correlates of preadolescent SITBs.
Data Extraction and Synthesis
Two reviewers independently extracted data from each study, and the Joanna Briggs Institute Checklist for Prevalence Studies was used to assess study quality. Pooled prevalence and Cohen d were derived from random-effects meta-analyses. Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline was followed.
Main Outcomes and Measures
Prevalence and correlates of suicidal ideation, suicide attempts, suicide deaths, and nonsuicidal self-injury among preadolescents.
Results
Fifty-eight studies with 626 486 590 individuals were included. Lifetime prevalence of suicide in the general population was 0.79 per 1 million children. Prevalence for lifetime suicidal thoughts, suicide attempts, and nonsuicidal self-injury among preadolescents were 15.1%, 2.6%, and 6.2%, respectively, in community samples. These data suggest that approximately 17.0% of preadolescents with suicidal ideation transition to attempting suicide. Across several analyses, male individuals appear more likely to have SITBs in preadolescence than adolescence. Correlate data were modest for SITBs other than suicidal ideation, but among specific disorders, attention-deficit/hyperactivity disorder (suicidal ideation: d = 0.54 [95% CI, 0.34-0.75]) and depression (suicidal ideation: d = 0.90 [95% CI, 0.71-1.09]; suicide attempts: d = 0.47 [95% CI, 0.26-0.68]) emerged as the strongest correlates. Among interpersonal factors, child maltreatment (suicidal ideation: d = 2.62 [95% CI, 1.56-3.67]) and parental support (suicidal ideation: d = −0.34 [95% CI, −0.46 to −0.22]) yielded the largest effect sizes.
Conclusions and Relevance
In this systematic review anda meta-analysis, although preadolescent suicide deaths were rare, other SITB types occur with concerning frequency. Male individuals were at greater risk for SITBs in preadolescence relative to adolescence. Attention-deficit/hyperactivity disorder, child maltreatment, and parental support were especially relevant to suicidal ideation, as well as depression for suicidal thoughts and behaviors, in this age group. Further study, especially of SITBs other than suicidal ideation, is needed.
Introduction
Self-injurious thoughts and behaviors (SITBs) are a long-standing public health issue. Suicide is one of the leading causes of death worldwide.1 Nonsuicidal self-injury (NSSI) has received increasing attention, in part because it is an even stronger predictor of future suicidal behavior than is a history of suicide attempts.2 Identifying characteristics associated with SITBs is imperative for advancing strategies for preventing their occurrence. In contrast to the substantial number of studies focused on adolescents and adults, the amount of research on SITBs in preadolescent children (ie, age <13 years) is modest.3,4 In the case of suicidal thoughts and behaviors, in some measure, this is due to the long-held view that preadolescent children do not possess the cognitive capability to comprehend the nature of death and so are incapable of thoughts or acts of suicide.5,6 Research on NSSI in preadolescent children is rarer still, and this is in part a product of the later emergence of NSSI as a distinct field of inquiry in clinical research. This is important because findings on correlates of SITBs in older age groups may not fully generalize to preadolescents. Indeed, externalizing disorders have been viewed as of greater relevance to this younger age group,7,8 but the strength of the evidence supporting this in the existing literature is unclear. Given that relatively little attention has been devoted to characterizing SITBs in preadolescent children, it is perhaps not surprising that studies on treatments for these clinical outcomes in this age group are all but nonexistent.4
With recent increases in suicide among preadolescent children in the US,3 and with the role that suicidal ideation and NSSI have in this outcome, the need for progress in understanding the scope and nature of SITBs in this demographic is all the more pressing. Indeed, suicide emerged as the tenth leading cause of death among preadolescent children in 2008 and has continued to rise, becoming the fifth leading cause of death in 2019.9 To address this worrying trend, the National Institute of Mental Health convened meetings in 201910 and 202111 to identify priorities and strategies for research on preadolescent suicide.
An important step toward this end is comprehensively to characterize the studies that have been conducted in this area. Although 2 recent overviews of preadolescent suicide exist,3,4 to our knowledge, there has yet to be a systematic review conducted on SITBs. The current review aims to address this need by presenting the first systematic review and quantitative synthesis of the existing research on preadolescent SITBs. It aims to provide (1) prevalence estimates of SITBs among preadolescent children, thereby to characterize the scale of these clinical concerns; (2) an evaluation of potential moderators of lifetime prevalence of these clinical outcomes; (3) an assessment of sociodemographic, clinical, psychological, and other correlates of these outcomes; and (4) direct comparisons of preadolescent and adolescent SITBs in terms of available sociodemographic and other characteristics. Through providing a comprehensive synthesis characterizing the existing research on preadolescent SITBs, our goal is to provide a clear understanding of the current state of evidence on this topic, as well as a foundation to guide future research and ultimately to inform risk identification and intervention strategies.
Methods
Search Strategy and Eligibility Criteria
This project was registered in PROSPERO (CRD42021254670) and followed Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline. A systematic review of the literature was conducted in MEDLINE, PsycINFO, and Embase from inception through December 23, 2021 (search terms used are detailed in the eMethods in the Supplement). The literature search was restricted to English language and peer-reviewed journals. This was supplemented by a search of the references of an earlier review.12
Study inclusion criteria were (1) preadolescent SITBs (suicidal ideation, suicide attempts, suicide deaths, and NSSI) assessed in individuals younger than 13 years (ie, retrospective assessments of preadolescent SITBs in older samples were excluded); (2) SITBs were assessed systematically; (3) SITBs were assessed separately from each other and other constructs; and (4) quantitative data were presented on the prevalence (lifetime or current/past month) of preadolescent SITBs or their correlates. Studies were excluded if they (1) evaluated SITBs as adverse events in clinical trials and (2) assessed stereotypic self-harm in children with developmental disorders.
Each search result was reviewed by 2 or 4 independent coders (R.F.L.W., A.E.S., S.M.C., and C.M.S.) to determine eligibility. When eligibility could not be ruled out based on abstract and title alone, full-text review was conducted. In cases where more information was needed to determine study eligibility or for data extraction, detailed below, every effort was made to obtain further details in other publications describing the measure or study design (eg, other publications with the same data set) or by contacting the study authors, the latter of which resulted in additional prevalence data for 2 studies. Discrepancies in coding eligibility were resolved by the first author (R.T.L.).
Data Extraction
Data on 7 study characteristics were extracted for analysis. These included 3 sample characteristics: (1) mean age of sample, (2) percentage of female participants in the sample, and (3) sample type (community or clinical). Data for 4 study design characteristics were extracted: (1) SITB type assessed (ie, suicide, suicide attempts, suicidal ideation, and NSSI), (2) time frame covered by SITB assessment (lifetime or current/past month), (3) SITB measure type (questionnaire or interview), and (4) the respondent of the assessment (child, parent, or both). Correlate data for adolescent SITBs were extracted whenever possible for head-to-head comparisons between preadolescent and adolescent SITBs.
Study Quality Assessment
Studies reporting lifetime prevalence of SITBs were assessed using the Joanna Briggs Institute Checklist for Prevalence Studies,13 which includes 9 criteria for evaluating study quality. An overall study quality index was derived by summing the number of criteria met, with summed scores above 4 used as the criterion for high study quality.14
Data Analysis
Analyses were conducted using Comprehensive Meta-Analysis version 3.3.070 (Biostat). The standardized mean difference (Cohen d based on the log odds ratio and its SD) was used as the indicator of effect size. Pooled associations were calculated such that values more than 0 reflected positive associations between the correlate of interest and SITBs. In head-to-head comparisons between preadolescent and adolescent SITBs with respect to a correlate of interest, values more than 0 indicated a correlate was more characteristic of preadolescent suicide. For correlates and head-to-head comparisons, analyses were conducted only when the number of unique associations of 3 or more, so as to obtain reliable pooled estimates of effect sizes.15
Random-effects models were generated, accounting for the high expected heterogeneity across studies resulting from differences in samples, measures, and design. Heterogeneity across the studies was evaluated using the I2 statistic,16 which indicates the percentage of the variance in an effect estimate that is a product of heterogeneity across studies rather than sampling error (ie, chance). Substantial heterogeneity across studies is indicated by an I2 value of 75%. High heterogeneity indicates the need for moderator analyses to account for potential sources of heterogeneity. Each moderator was assessed separately, with the effect size at each level of categorical moderators estimated. Study characteristics submitted to moderator analysis are detailed in the eMethods in the Supplement.
Presence of publication bias was assessed with inspection of funnel plots for asymmetry and with Egger regression intercept test,17 which uses a linear regression approach weighing study effect sizes relative to their standard error. Two-sided P values were statistically significant at .05.
Results
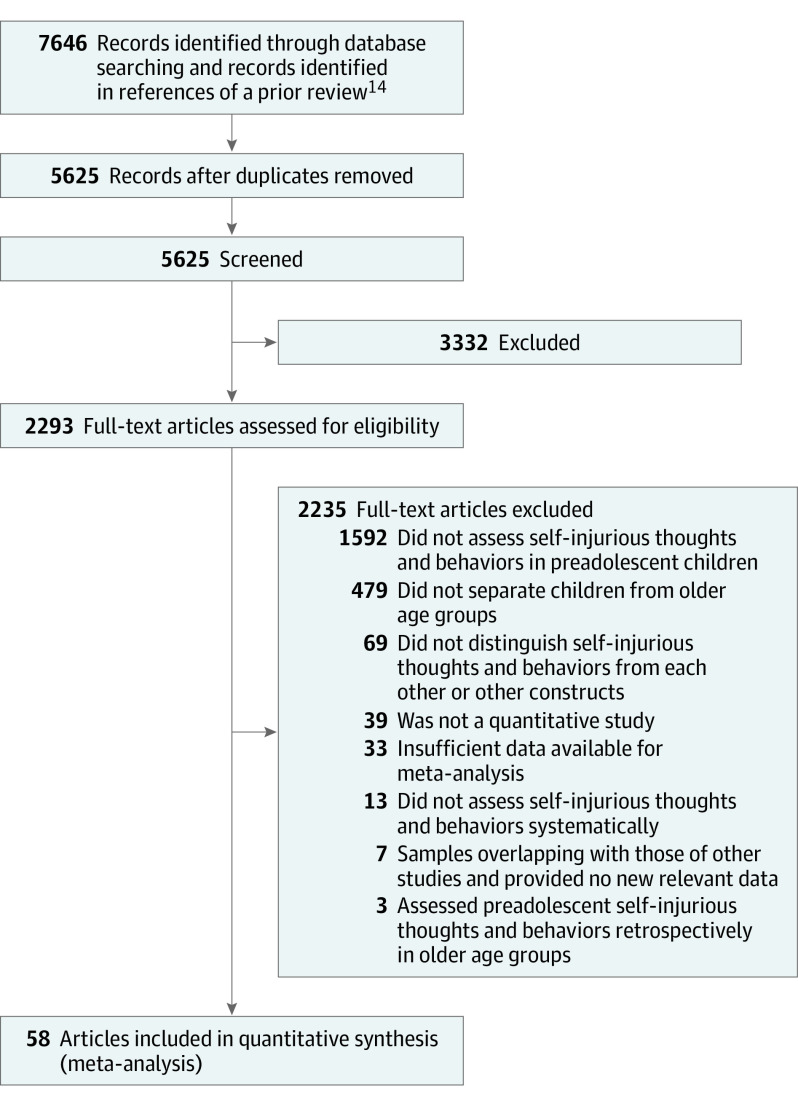
Of 7646 publications our search strategy yielded, 5625 unique records were identified, of which 3332 were excluded based on their titles and abstracts. An additional 2228 were excluded based on a detailed full-text review, leaving a set of 65 publications satisfying the eligibility criteria. In cases where multiple studies used overlapping samples but presented unique data on prevalence and/or correlate for a SITB type, all studies were retained for relevant analyses. In cases where multiple studies assessed the same SITB prevalence or correlate in overlapping samples, determination of which study to include in the meta-analysis was based on largest sample size for relevant analyses. Twenty-one studies featured overlapping samples, and 7 were excluded at this stage, leaving a final set of 58 studies18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75 featuring 52 samples (Figure; eTable 1 in the Supplement).
Figure. PRISMA Flowchart of Literature Search.
Prevalence of Preadolescent SITBs
Weighted SITB prevalence (Table 1) was calculated for each sample type (community and clinical) stratified by time frame (lifetime or current/past month). Pooled prevalence was calculated when at least 2 unique associations were available for a given SITB type. For suicide, the pooled community prevalence was based entirely on epidemiological samples and therefore presented as number of deaths per 1 million children. Apart from the 0.79 suicides per 1 million children in epidemiological samples, lifetime prevalence of preadolescent SITBs ranged from 2.56% for suicide attempts to 15.08% for suicidal ideation in community samples and from 0.46% for suicides to 43.18% for suicidal ideation in clinical samples. Current prevalence ranged from 11.65% for suicide attempts to 38.19% for suicidal ideation in clinical samples and was available only for available for suicidal ideation (12.08%) in community samples.
Table 1. Prevalence Rates of Self-injurious Thoughts and Behaviors by Sample Type and Time Frame.
| Self-injury type | Sample | Lifetime | Current/past month | ||||
|---|---|---|---|---|---|---|---|
| k a | No. of individuals | % (95% CI) | k a | No. of individuals | % (95% CI) | ||
| Suicide death | Community | 11 | 626 350 284 | 0.79 (0.40-1.59)b | NA | NA | NA |
| Clinical | 4 | 10 401 | 0.46 (0.11-1.96) | NA | NA | NA | |
| Suicide attempt | Community | 4 | 100 893 | 2.56 (1.86-3.53) | NA | NA | NA |
| Clinical | 14 | 897 | 17.76 (10.19-29.13) | 4 | 459 | 11.65 (4.03-29.27) | |
| Suicidal ideation | Community | 5 | 101 337 | 15.08 (14.41-15.78) | 12 | 20 887 | 12.08 (7.92-17.99) |
| Clinical | 7 | 482 | 43.18 (21.87-67.35) | 4 | 575 | 38.19 (13.81-70.44) | |
| Nonsuicidal self-injury | Community | 3 | 13 214 | 6.25 (3.82-10.06) | NA | NA | NA |
| Clinical | 2 | 43 | 37.38 (24.26-52.66) | 2 | 177 | 21.50 (8.40-44.99) | |
Abbreviation: NA, not applicable.
k Indicates the number of unique associations; effect size estimates in which k = 2 should be interpreted with caution.
The community prevalence estimate for suicide deaths is based entirely on epidemiological samples and presented as number of deaths per 1 million children.
Although study quality index scores were generally high (mean [SD], 6.45 [1.96]), 3 studies with 10 unique associations scored below 5. Sensitivity analyses were conducted excluding these studies,14 except for lifetime prevalence of NSSI in community samples, as only 1 relevant study remained. These analyses are presented in eTable 2 in the Supplement.
Heterogeneity was high across lifetime prevalence analyses (suicide: I2 = 95.88 [clinical sample] and 98.58 [community sample]; P < .001; suicide attempts: I2 = 87.27 [clinical sample] and 97.92 [community sample]; P < .001; suicidal ideation: I2 = 79.53 [community sample] and 91.66 [clinical sample]; P < .001), indicating that moderator analyses were warranted. Moderator analyses were not conducted for NSSI, given its few unique associations. Age, percentage of female participants in each sample, measure type, and respondent were evaluated as candidate moderators for suicide attempts and suicidal ideation. Only percentage of female participants was assessed as a moderator for suicide prevalence, as none of the relevant studies reported mean age, and data were derived from death records, making respondent and measure type not applicable.
In moderator analyses (eTable 3 in the Supplement), percentage of female participants was negatively associated with prevalence of suicide attempts and suicidal ideation. Although it did not moderate suicide prevalence overall, when weighted prevalence estimates were stratified by sample type, it was negatively associated with suicide prevalence in epidemiological/community samples (b = −0.02; SE < .01; P < .001). Measure type also emerged as a moderator of prevalence for suicide attempts and suicidal ideation, with higher pooled prevalence observed with interview-based measures. However, these findings are likely artifacts of all relevant studies with self-report measures having community samples, in contrast to 14 of 16 studies of suicide attempts and 7 of 10 studies of suicidal ideation with interview-based measures featuring clinical samples. Suicide attempts and suicidal ideation prevalence were not moderated by age, as may be expected with restricted range in the samples, and respondent.
Publication bias was assessed for lifetime prevalence of each SITB type, except for NSSI, given its few unique associations. Some evidence of publication bias emerged in Egger test for suicide deaths and attempts and in funnel plots for suicide deaths and suicidal ideation (eFigure in the Supplement).
Correlates of Preadolescent SITBs
For correlates of suicide attempts (Table 2), neither sociodemographic characteristics nor family history of suicidal thoughts and behaviors were significant. However, clinical correlates were consistently associated with this outcome. Pooled effect sizes ranged from small for anxiety to medium for depression, and small-to-medium effect sizes were observed for psychopathology overall.
Table 2. Correlates of Suicide Attempts.
| Correlate | k a | No. of individuals | d (95% CI) | P value |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Sex (female) | 9 | 14 738 | −0.05 (−0.28 to 0.19) | .69 |
| Race (minority group)b | 3 | 13 775 | −0.02 (−0.29 to 0.26) | .90 |
| Race (Black, with White as reference) | 4 | 9069 | −0.07 (−0.55 to 0.41) | .77 |
| Ethnicity (Hispanic, with non-Hispanic White as reference) | 3 | 9961 | −0.19 (−0.67 to 0.28) | .42 |
| Family characteristics | ||||
| Family history of suicidal thoughts and behaviors | 3 | 1558 | 0.15 (−0.04 to 0.34) | .13 |
| Clinical correlates | ||||
| Overall psychopathology | 6 | 1904 | 0.42 (0.20 to 0.65) | <.001 |
| Internalizing psychopathology | 6 | 1895 | 0.33 (0.19 to 0.48) | <.001 |
| Anxiety | 4 | 1648 | 0.17 (0.00 to 0.34)c | .04 |
| Depression | 6 | 1895 | 0.47 (0.26 to 0.68) | <.001 |
k Indicates the number of unique associations.
Any racial group besides White.
The lower end of the confidence interval was rounded down but exceeded 0.00.
Table 3 presents analyses for correlates of suicidal ideation. For sociodemographic characteristics, only race was significant, with a small negative association indicating that children from racial minority groups were less likely to have suicidal thoughts. Among family characteristics, only ones involving family dysfunction and psychopathology were significant correlates, except for parental depression. Effect sizes ranged from small for overall psychopathology to small-to-medium effect sizes for parental history of suicidal thoughts and behaviors.
Table 3. Correlates of Suicidal Ideation.
| Correlate | k a | No. of individuals | d (95% CI) | P value |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Sex (female) | 16 | 107 881 | −0.03 (−0.10 to 0.05) | .50 |
| Race (minority group)b | 5 | 16 638 | −0.22 (−0.38 to −0.06) | <.01 |
| Race (Black, with White as reference) | 4 | 11 076 | −0.31 (−0.61 to 0.00)c | .05 |
| Family characteristics | ||||
| Parental marital status (married) | 5 | 22 672 | 0.05 (−0.17 to 0.26) | .65 |
| Parental education | 6 | 14 666 | <0.01 (−0.09 to 0.09) | .99 |
| Family income | 8 | 94 230 | −0.07 (−0.18 to 0.04) | .21 |
| Family conflict and dysfunction | 5 | 2805 | 0.36 (0.11 to 0.60) | <.01 |
| Family psychopathology | 8 | 12 322 | 0.18 (0.09 to 0.26) | <.001 |
| Parental depression | 4 | 5001 | 0.37 (−0.11 to 0.85) | .13 |
| Parental history of suicidal thoughts and behaviors | 4 | 1208 | 0.45 (0.05 to 0.86) | .03 |
| Clinical correlates | ||||
| Overall psychopathology | 19 | 25 219 | 0.62 (0.47 to 0.77) | <.001 |
| Internalizing psychopathology | 16 | 19 235 | 0.71 (0.47 to 0.94) | <.001 |
| Anxiety | 6 | 13 062 | 0.13 (−0.19 to 0.46) | .42 |
| Depression | 13 | 15 185 | 0.90 (0.71 to 1.09) | <.001 |
| PTSD | 3 | 12 879 | 0.32 (−0.14 to 0.78) | .18 |
| Externalizing psychopathology | 8 | 23 619 | 0.32 (0.08 to 0.56) | <.01 |
| ADHD | 6 | 22 445 | 0.54 (0.34 to 0.75) | <.001 |
| Conduct disorder/oppositional defiant disorder | 4 | 18 936 | 0.02 (−0.42 to 0.47) | .91 |
| Psychosis | 3 | 11 847 | 0.39 (0.16 to 0.63) | <.01 |
| Psychological correlates | ||||
| Aggression | 7 | 4967 | 0.65 (0.04 to 1.27) | .04 |
| Cognitive functioning | 4 | 1903 | 0.11 (−0.19 to 0.42) | .46 |
| Negative affect | 3 | 863 | 0.80 (0.12 to 1.47) | .02 |
| Self-esteem | 4 | 916 | −0.53 (−0.84 to −0.22) | <.001 |
| Interpersonal correlates | ||||
| Overall social support | 8 | 85 128 | −0.25 (−0.36 to −0.15) | <.001 |
| Parental support | 5 | 84 934 | −0.34 (−0.46 to −0.22)d | <.001 |
| Peer support | 5 | 84 469 | −0.13 (−0.22 to −0.04)d | <.01 |
| Experienced bullying | 4 | 86 166 | 0.29 (0.26 to 0.33) | <.001 |
| Child maltreatment | 5 | 86 957 | 2.62 (1.56 to 3.67) | <.001 |
| Child physical abuse | 4 | 84 078 | 0.66 (0.46 to 0.86) | <.001 |
| Child sexual abuse | 4 | 84 077 | 0.55 (0.30 to 0.80) | <.001 |
| Other correlates | ||||
| Academic stress | 4 | 2861 | 0.24 (0.11 to 0.37) | <.001 |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; PTSD, posttraumatic stress disorder.
k Indicates the number of unique associations.
Any racial group besides White.
The upper end of the confidence interval was rounded down but exceeded 0.00.
When unrounded, the upper end of the confidence interval for parental support does not overlap with the lower end of the confidence interval for peer support.
All clinical correlates of suicidal ideation were significant, save anxiety, posttraumatic stress disorder, and conduct disorder/oppositional defiant disorder. The largest effect sizes were observed for depression (large effect size), overall psychopathology and internalizing psychopathology (medium-to-large effect size), and attention-deficit/hyperactivity disorder (ADHD) (medium). Psychosis had a small-to-medium effect size.
All psychological correlates for suicidal ideation, except general cognitive functioning, had significant medium-to-large effect sizes. These associations were positive for aggression and negative affect and negative for self-esteem. Significant effect sizes were observed for all interpersonal correlates and academic stress, with negative small to small-to-medium effect sizes for social support and medium to large for child maltreatment.
For suicide and NSSI, meta-analysis of correlates was limited to female sex, which was negatively associated with both outcomes (suicide: d = −0.77 [95% CI, −1.03 to −0.52]; P < .001; NSSI: d = −0.17 [95% CI, −0.30 to −0.04]; P = .008).
Head-to-Head Comparisons of Preadolescent and Adolescent Suicide
Head-to-head comparisons between preadolescent and adolescent SITBs were only possible for suicide deaths, as a sufficient number of unique associations for this outcome was available for meta-analysis. Female sex and depression were more characteristic of adolescent than preadolescent suicide (Table 4). No group differences were observed for overall psychopathology, psychiatric treatment history, or academic stress.
Table 4. Head-to-Head Comparisons of Preadolescent and Adolescent Suicide Deathsa.
| Characteristic | k b | No. of individuals | d (95% CI) | P value |
|---|---|---|---|---|
| Sex (female) | 4 | 3173 | −0.52 (−0.69 to −0.36) | <.001 |
| Overall psychopathology | 3 | 891 | −0.06 (−0.32 to 0.21) | .69 |
| Depression | 3 | 904 | −0.41 (−0.71 to −0.10) | .01 |
| History of psychiatric treatment | 3 | 809 | −0.16 (−0.48 to 0.15) | .31 |
| Academic stress | 3 | 904 | −0.30 (−0.78 to 0.18) | .22 |
Adolescent suicide served as the reference group in these comparisons; positive d values indicate a variable is more characteristic of preadolescent suicide, whereas negative d values indicate a variable is more characteristic of adolescent suicide.
k Indicates the number of unique associations.
Discussion
This systematic review and meta-analysis provides, to our knowledge, the first pooled prevalence estimates of SITBs in preadolescent children, a necessary preliminary step for accurately evaluating the scale of these clinical concerns. The available evidence yielded concerning prevalence estimates for preadolescent SITBs, particularly in clinical samples. Even in community samples, pooled prevalence estimates for lifetime suicidal ideation, suicide attempts, and NSSI were 15.1%, 2.6%, and 6.2%, respectively. Although lower than for adolescents with lifetime prevalence of 19.8% to 24.0% for suicidal ideation and 3.1% to 8.8% for suicide attempts76 and adolescent NSSI prevalence of 17.2% to 18.0%,77,78 the current findings indicate that preadolescent SITBs, particularly suicidal ideation and NSSI, are not uncommon. Additionally, the current data suggest that approximately 17.0% of preadolescent children with suicidal ideation transition to attempting suicide, whereas between 15.7% and 36.7% of suicidal adolescents act on their suicidal thoughts. Although suicide deaths among preadolescents are rare, at approximately 1 of 1 million children, compared with 3.8 of 100 000 adolescents in a recent meta-analytic review,79 preadolescent suicide is a growing public health concern, given recent evidence that they have been increasing in the US3,9 and the outsized and long-term impact that they have on families80 (eg, increased parental mortality81) and communities.3 Collectively, the current findings also challenge the long-standing view that preadolescent children do not possess the cognitive capacity to experience suicidal thoughts and to engage in suicidal behavior.5,6
Only sex emerged as a moderator of prevalence of suicidal ideation and suicide attempts, such that samples with more male individuals had higher lifetime prevalence. When assessed directly in relation with SITBs, male individuals were more likely to die by suicide and to engage in NSSI, but sex was uncorrelated with suicidal ideation and suicide attempts. Although the precise nature of how sex is associated with preadolescent SITBs remains to be clarified, these findings are consistent in indicating that the higher prevalence of suicidal ideation and suicide attempts among female individuals in adolescence76,82 do not generalize to preadolescence. Even in the case of suicide, head-to-head comparisons between preadolescent and adolescent suicide decedents suggest that the higher risk of suicide among male individuals in adolescence76,82 may be more pronounced in preadolescence. Given the size of this association, it cannot be accounted for by the male-biased sex ratio at birth and its decline over the life course.83
For correlates of SITBs, additional developmental differences may be found in the social support factors, with nonoverlapping confidence intervals indicating that parental support was significantly more associated with suicidal ideation than is peer support, a finding consistent with the tendency for parental relationships to have greater weight prior to adolescence.84,85 On the other end of the spectrum, the large association for child maltreatment and suicidal ideation is notable, especially within the context of findings that it may be more associated with suicide attempts in childhood than adolescence.8 Additionally, among specific disorders, ADHD was the second strongest clinical correlate of suicidal ideation, which is congruent with the view that this disorder is more characteristic of suicide outcomes in preadolescence than adolescence.7
However, other associations appear to generalize across development; depression had the largest association among specific disorders in relation to suicidal ideation and moreover was more strongly correlated with this outcome than with suicide attempts, as indicated by nonoverlapping confidence intervals. These findings fit well with the adult literature, in which depression is more strongly implicated in risk for suicidal ideation than suicide attempts.86
Furthermore, based on the aforementioned findings, support for the commonly held view that externalizing psychopathology is more central to suicidal thoughts and behaviors outcomes in preadolescence, whereas depression is in adolescence,7,8 should be regarded as modest and its evaluation incomplete. Although ADHD had the second largest association among specific disorders in relation to suicidal ideation, all other externalizing disorders had negligible associations. Additionally, only 1 study examined these disorders with suicide attempts,73 making meta-analytic evaluation impossible. Given that depression had a large association, the largest among individual disorders, in relation to suicidal ideation and a medium association in relation to suicide attempts, depression should not be discounted in preference to externalizing disorders in evaluating preadolescent suicidal thoughts and behaviors. Moreover, head-to-head comparisons indicating greater prevalence of depression in adolescent than preadolescent suicide cannot be taken to mean risk for suicide death associated with this disorder is stronger in adolescence, without direct comparisons of the associations for depression and suicide between these age groups; greater depression prevalence in suicidal adolescents may reflect greater prevalence at this age more generally.87 When considered with recent findings of genetic associations for ADHD and depression with preadolescent suicidal ideation and attempts,88 the available evidence suggests that both disorders may be important for determining risk for these outcomes.
Limitations
Although no racial or ethnic differences were found, except for racial minority status with suicidal ideation, these findings likely reflect historical patterns; the current meta-analysis cannot speak to recent temporal trends, an important one being the identification of higher, and increasing, suicide rates among Black children in the US.21,89 Temporal definition in another sense, whether identified correlates precede SITBs, was evaluated in 1 study25 and thus requires further investigation. Although head-to-head comparisons of preadolescent and adolescent suicide were sometimes possible and provide value in characterizing suicidal youth at each age, complementary analyses comparing the effect size for a given correlate of SITBs at each age, as mentioned above, is necessary to understand the correlate’s relative importance to SITBs in preadolescence vs adolescence. There was also a general paucity of NSSI prevalence studies, limiting analyses of prevalence and precluding head-to-head comparisons of preadolescent and adolescent NSSI. Additionally, except in the case of biological sex, there was a notable absence of data on correlates of suicide attempts and NSSI, an important gap to be addressed in future research. Finally, almost all studies presented data from Asian countries, North America, and Europe. Future studies including samples from other parts of the world (eg, Africa and Australia) are needed to characterize the scope and nature of preadolescent SITBs across the world.
Conclusions
In this systematic review and meta-analysis, SITBs, particularly suicidal ideation, suicide attempts, and NSSI, occurred at concerning rates in preadolescent children. Most studies have focused on suicidal ideation and limited research exists for suicide attempts, suicide, and NSSI. Male individuals appeared to be at greater risk for SITBs in preadolescence than older age groups. Parental support was a particularly key protective factor during childhood, whereas child maltreatment was an important correlate of risk for suicidal ideation. Preliminary evidence suggested that ADHD is especially important for ascertaining risk in the case of suicidal thoughts, and depression in the case of suicidal thoughts and behaviors, in preadolescence.
eMethods.
eTable 1. Study characteristics
eTable 2. Sensitivity analyses of prevalence rates of self-injurious thoughts and behaviors
eTable 3. Univariate moderator analyses for Lifetime self-injurious thoughts and behaviors
eFigure. Funnel plots for effect sizes in the meta-analyses
References
- 1.World Health Organization . Preventing Suicide: A Global Imperative. World Health Organization; 2014. [Google Scholar]
- 2.Ribeiro JD, Franklin JC, Fox KR, et al. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychol Med. 2016;46(2):225-236. doi: 10.1017/S0033291715001804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ayer L, Colpe L, Pearson J, Rooney M, Murphy E. Advancing research in child suicide: a call to action. J Am Acad Child Adolesc Psychiatry. 2020;59(9):1028-1035. doi: 10.1016/j.jaac.2020.02.010 [DOI] [PubMed] [Google Scholar]
- 4.Ridge Anderson A, Keyes GM, Jobes DA. Understanding and treating suicidal risk in young children. Pract Innov (Wash D C). 2016;1:3-19. doi: 10.1037/pri0000018 [DOI] [Google Scholar]
- 5.Bolger N, Downey G, Walker E, Steininger P. The onset of suicidal ideation in childhood and adolescence. J Youth Adolesc. 1989;18(2):175-190. doi: 10.1007/BF02138799 [DOI] [PubMed] [Google Scholar]
- 6.Cuddy-Casey M, Orvaschel H. Children’s understanding of death in relation to child suicidality and homicidality. Clin Psychol Rev. 1997;17(1):33-45. doi: 10.1016/S0272-7358(96)00044-X [DOI] [PubMed] [Google Scholar]
- 7.Ben-Yehuda A, Aviram S, Govezensky J, Nitzan U, Levkovitz Y, Bloch Y. Suicidal behavior in minors: diagnostic differences between children and adolescents. J Dev Behav Pediatr. 2012;33(7):542-547. doi: 10.1097/01.DBP.0000415830.85996.e6 [DOI] [PubMed] [Google Scholar]
- 8.Peyre H, Hoertel N, Stordeur C, et al. Contributing factors and mental health outcomes of first suicide attempt during childhood and adolescence: results from a nationally representative study. J Clin Psychiatry. 2017;78(6):e622-e630. doi: 10.4088/JCP.16m10876 [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention . Injury prevention & control: leading causes of death and injury. Accessed April 20, 2022. https://www.cdc.gov/injury/wisqars/LeadingCauses.html
- 10.National Institute of Mental Health . Identifying research priorities in child suicide risk. Accessed April 20, 2022. https://www.nimh.nih.gov/news/events/announcements/identifying-research-priorities-in-child-suicide-risk
- 11.National Institute of Mental Health . Understanding suicide risk among children and pre-teens: a synthesis workshop. Accessed April 20, 2022. https://www.nimh.nih.gov/news/events/2021/understanding-suicide-risk-among-children-and-pre-teens-a-synthesis-workshop
- 12.Pfeffer CR. Studies of suicidal preadolescent and adolescent inpatients: a critique of research methods. Suicide Life Threat Behav. 1989;19(1):58-77. doi: 10.1111/j.1943-278X.1989.tb00366.x [DOI] [PubMed] [Google Scholar]
- 13.The Joanna Briggs Institute . Checklist for prevalence studies. Published 2017. Accessed April 20, 2022. http://joannabriggs.org/research/critical-appraisal-tools.html
- 14.Cénat JM, Blais-Rochette C, Morse C, et al. Prevalence and risk factors associated with attention-deficit/hyperactivity disorder among US Black individuals: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78(1):21-28. doi: 10.1001/jamapsychiatry.2020.2788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Favril L, Yu R, Hawton K, Fazel S. Risk factors for self-harm in prison: a systematic review and meta-analysis. Lancet Psychiatry. 2020;7(8):682-691. doi: 10.1016/S2215-0366(20)30190-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557-560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629-634. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baetens I, Claes L, Martin G, et al. Is nonsuicidal self-injury associated with parenting and family factors? J Early Adolesc. 2014;34:387-405. doi: 10.1177/0272431613494006 [DOI] [Google Scholar]
- 19.Bauer BW, Gustafsson HC, Nigg J, Karalunas SL. Working memory mediates increased negative affect and suicidal ideation in childhood attention-deficit/hyperactivity disorder. J Psychopathol Behav Assess. 2018;40(2):180-193. doi: 10.1007/s10862-017-9635-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borchardt CM, Meller WH. Symptoms of affective disorder in pre-adolescent vs. adolescent inpatients. J Adolesc. 1996;19(2):155-161. doi: 10.1006/jado.1996.0015 [DOI] [PubMed] [Google Scholar]
- 21.Bridge JA, Asti L, Horowitz LM, et al. Suicide trends among elementary school-aged children in the United States from 1993 to 2012. JAMA Pediatr. 2015;169(7):673-677. doi: 10.1001/jamapediatrics.2015.0465 [DOI] [PubMed] [Google Scholar]
- 22.Cairns RB, Peterson G, Neckerman HJ. Suicidal behavior in aggressive adolescents. J Clin Child Psychol. 1988;17:298-309. doi: 10.1207/s15374424jccp1704_1 [DOI] [Google Scholar]
- 23.Carlson GA, Asarnow JR, Orbach I. Developmental aspects of suicidal behavior in children. I. J Am Acad Child Adolesc Psychiatry. 1987;26(2):186-192. doi: 10.1097/00004583-198703000-00011 [DOI] [PubMed] [Google Scholar]
- 24.Causey DL, Robertson JM, Elam SM. Characteristics of toddlers and preschoolers exhibiting severe psychiatric disturbance. Child Psychiatry Hum Dev. 1998;29(1):33-48. doi: 10.1023/A:1022631113688 [DOI] [PubMed] [Google Scholar]
- 25.Chen J, Huebner ES, Tian L. Longitudinal associations among academic achievement and depressive symptoms and suicidal ideation in elementary schoolchildren: disentangling between- and within-person associations. Eur Child Adolesc Psychiatry. Published online April 22, 2021. doi: 10.1007/s00787-021-01781-y [DOI] [PubMed] [Google Scholar]
- 26.Chiang YC, Lee TSH, Yen LL, et al. Influence of stressors and possible pathways of onset of seventh graders’ suicidal ideation in urban and rural areas in Taiwan. BMC Public Health. 2013;13:1233. doi: 10.1186/1471-2458-13-1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cowell JM, Gross D, McNaughton D, Ailey S, Fogg L. Depression and suicidal ideation among Mexican American school-aged children. Res Theory Nurs Pract. 2005;19(1):77-94. doi: 10.1891/rtnp.19.1.77.66337 [DOI] [PubMed] [Google Scholar]
- 28.DeVille DC, Whalen D, Breslin FJ, et al. Prevalence and family-related factors associated with suicidal ideation, suicide attempts, and self-injury in children aged 9 to 10 years. JAMA Netw Open. 2020;3(2):e1920956. doi: 10.1001/jamanetworkopen.2019.20956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greening L, Stoppelbein L, Luebbe A, Fite PJ. Aggression and the risk for suicidal behaviors among children. Suicide Life Threat Behav. 2010;40(4):337-345. doi: 10.1521/suli.2010.40.4.337 [DOI] [PubMed] [Google Scholar]
- 30.Haavisto A, Sourander A, Ellilä H, Välimäki M, Santalahti P, Helenius H. Suicidal ideation and suicide attempts among child and adolescent psychiatric inpatients in Finland. J Affect Disord. 2003;76(1-3):211-221. doi: 10.1016/S0165-0327(02)00093-9 [DOI] [PubMed] [Google Scholar]
- 31.Hunsche MC, Saqui S, Mirenda P, et al. Parent-reported rates and clinical correlates of suicidality in children with autism spectrum disorder: a longitudinal study. J Autism Dev Disord. 2020;50(10):3496-3509. doi: 10.1007/s10803-020-04373-y [DOI] [PubMed] [Google Scholar]
- 32.Husky MM, Bitfoi A, Carta MG, et al. Bullying involvement and suicidal ideation in elementary school children across Europe. J Affect Disord. 2022;299:281-286. doi: 10.1016/j.jad.2021.12.023 [DOI] [PubMed] [Google Scholar]
- 33.James KM, Kudinova AY, Woody ML, Feurer C, Foster CE, Gibb BE. Children’s history of suicidal ideation and synchrony of facial displays of affect during mother-child interactions. J Child Psychol Psychiatry. 2021;62(1):40-47. doi: 10.1111/jcpp.13231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim JW, Lee K, Lee YS, et al. Factors associated with group bullying and psychopathology in elementary school students using child-welfare facilities. Neuropsychiatr Dis Treat. 2015;11:991-998. doi: 10.2147/NDT.S76105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kovess-Masfety V, Pilowsky DJ, Goelitz D, et al. Suicidal ideation and mental health disorders in young school children across Europe. J Affect Disord. 2015;177:28-35. doi: 10.1016/j.jad.2015.02.008 [DOI] [PubMed] [Google Scholar]
- 36.Larzelere RE, Andersen JJ, Ringle JL, Jorgensen DD. The child suicide risk assessment: a screening measure of suicide risk in pre-adolescents. Death Stud. 2004;28(9):809-827. doi: 10.1080/07481180490490861 [DOI] [PubMed] [Google Scholar]
- 37.Lawrence HR, Burke TA, Sheehan AE, et al. Prevalence and correlates of suicidal ideation and suicide attempts in preadolescent children: a US population-based study. Transl Psychiatry. 2021;11(1):489. doi: 10.1038/s41398-021-01593-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee D, Jung S, Park S, et al. Youth suicide in Korea across the educational stages. Crisis. 2020;41(3):187-195. doi: 10.1027/0227-5910/a000624 [DOI] [PubMed] [Google Scholar]
- 39.Lewis DO, Shanok SS, Grant M, Ritvo E. Homicidally aggressive young children: neuropsychiatric and experiential correlates. Am J Psychiatry. 1983;140(2):148-153. doi: 10.1176/ajp.140.2.148 [DOI] [PubMed] [Google Scholar]
- 40.Lin FG, Lin JD, Hsieh YH, Chang CY. Quarrelsome family environment as an enhanced factor on child suicidal ideation. Res Dev Disabil. 2014;35(12):3245-3253. doi: 10.1016/j.ridd.2014.08.007 [DOI] [PubMed] [Google Scholar]
- 41.Livingston R, Bracha HS. Psychotic symptoms and suicidal behavior in hospitalized children. Am J Psychiatry. 1992;149(11):1585-1586. doi: 10.1176/ajp.149.11.1585 [DOI] [PubMed] [Google Scholar]
- 42.Lo HHM, Kwok SYCL, Yeung JWK, Low AYT, Tam CHL. The moderating effects of gratitude on the association between perceived parenting styles and suicidal ideation. J Child Fam Stud. 2017;26:1671-1680. doi: 10.1007/s10826-017-0683-y [DOI] [Google Scholar]
- 43.Luby JL, Whalen D, Tillman R, Barch DM. Clinical and psychosocial characteristics of young children with suicidal ideation, behaviors, and nonsuicidal self-injurious behaviors. J Am Acad Child Adolesc Psychiatry. 2019;58(1):117-127. doi: 10.1016/j.jaac.2018.06.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marraccini ME, Drapeau CW, Stein R, et al. Characterizing children hospitalized for suicide-related thoughts and behaviors. Child Adolesc Ment Health. 2021;26(4):331-338. doi: 10.1111/camh.12454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Martin SE, Liu RT, Mernick LR, et al. Suicidal thoughts and behaviors in psychiatrically referred young children. Psychiatry Res. 2016;246:308-313. doi: 10.1016/j.psychres.2016.09.038 [DOI] [PubMed] [Google Scholar]
- 46.Milling L, Campbell NB, Bush E, Laughlin A. Affective and behavioral correlates of suicidality among hospitalized preadolescent children. J Clin Child Psychol. 1996;25:454-462. doi: 10.1207/s15374424jccp2504_10 [DOI] [Google Scholar]
- 47.Min HJ, Jon DI, Jung MH, et al. Depression, aggression, and suicidal ideation in first graders: a school-based cross-sectional study. Compr Psychiatry. 2012;53(8):1145-1152. doi: 10.1016/j.comppsych.2012.05.004 [DOI] [PubMed] [Google Scholar]
- 48.Mishra N, Shrestha D, Poudyal RB, Mishra P. Retrospective study of suicide among children and young adults. J Nepal Paediatr Soc. 2013;33:110-116. doi: 10.3126/jnps.v33i2.7512 [DOI] [Google Scholar]
- 49.Myers KM, Burke P, McCauley E. Suicidal behavior by hospitalized preadolescent children on a psychiatric unit. J Am Acad Child Psychiatry. 1985;24(4):474-480. doi: 10.1016/S0002-7138(09)60567-7 [DOI] [PubMed] [Google Scholar]
- 50.O’Leary CC, Frank DA, Grant-Knight W, et al. Suicidal ideation among urban nine and ten year olds. J Dev Behav Pediatr. 2006;27(1):33-39. doi: 10.1097/00004703-200602000-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ong MS, Lakoma M, Gees Bhosrekar S, et al. Risk factors for suicide attempt in children, adolescents, and young adults hospitalized for mental health disorders. Child Adolesc Ment Health. 2021;26(2):134-142. doi: 10.1111/camh.12400 [DOI] [PubMed] [Google Scholar]
- 52.Paul E, Ortin A. Correlates of suicidal ideation and self-harm in early childhood in a cohort at risk for child abuse and neglect. Arch Suicide Res. 2019;23(1):134-150. doi: 10.1080/13811118.2017.1413468 [DOI] [PubMed] [Google Scholar]
- 53.Paul E, Ortin A. Psychopathological mechanisms of early neglect and abuse on suicidal ideation and self-harm in middle childhood. Eur Child Adolesc Psychiatry. 2019;28(10):1311-1319. doi: 10.1007/s00787-019-01287-8 [DOI] [PubMed] [Google Scholar]
- 54.Perepletchikova F, Nathanson D, Axelrod SR, et al. Randomized clinical trial of dialectical behavior therapy for preadolescent children with disruptive mood dysregulation disorder: feasibility and outcomes. J Am Acad Child Adolesc Psychiatry. 2017;56(10):832-840. doi: 10.1016/j.jaac.2017.07.789 [DOI] [PubMed] [Google Scholar]
- 55.Pfeffer CR, Plutchik R, Mizruchi MS, Lipkins R. Suicidal behavior in child psychiatric inpatients and outpatients and in nonpatients. Am J Psychiatry. 1986;143(6):733-738. doi: 10.1176/ajp.143.6.733 [DOI] [PubMed] [Google Scholar]
- 56.Pfeffer CR, Solomon G, Plutchik R, Mizruchi MS, Weiner A. Suicidal behavior in latency-age psychiatric inpatients: a replication and cross validation. J Am Acad Child Psychiatry. 1982;21(6):564-569. doi: 10.1097/00004583-198211000-00008 [DOI] [PubMed] [Google Scholar]
- 57.Puig-Antich J, Goetz D, Davies M, et al. A controlled family history study of prepubertal major depressive disorder. Arch Gen Psychiatry. 1989;46(5):406-418. doi: 10.1001/archpsyc.1989.01810050020005 [DOI] [PubMed] [Google Scholar]
- 58.Read K, Schwartz J, Martinez J, Bennett Smith S, Monroe K. Characterization of young children presenting to the emergency department for mental health complaints. South Med J. 2020;113(3):116-118. doi: 10.14423/SMJ.0000000000001076 [DOI] [PubMed] [Google Scholar]
- 59.Rosenthal PA, Rosenthal S. Suicidal behavior by preschool children. Am J Psychiatry. 1984;141(4):520-525. doi: 10.1176/ajp.141.4.520 [DOI] [PubMed] [Google Scholar]
- 60.Rosenthal PA, Rosenthal S, Doherty MB, Santora D. Suicidal thoughts and behaviors in depressed hospitalized preschoolers. Am J Psychother. 1986;40(2):201-212. doi: 10.1176/appi.psychotherapy.1986.40.2.201 [DOI] [PubMed] [Google Scholar]
- 61.Ryan ND, Puig-Antich J, Ambrosini P, et al. The clinical picture of major depression in children and adolescents. Arch Gen Psychiatry. 1987;44(10):854-861. doi: 10.1001/archpsyc.1987.01800220016003 [DOI] [PubMed] [Google Scholar]
- 62.Sheftall AH, Asti L, Horowitz LM, et al. Suicide in elementary school-aged children and early adolescents. Pediatrics. 2016;138(4):e20160436. doi: 10.1542/peds.2016-0436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sheftall AH, Bergdoll EE, James M, et al. Emotion regulation in elementary school-aged children with a maternal history of suicidal behavior: a pilot study. Child Psychiatry Hum Dev. 2020;51(5):792-800. doi: 10.1007/s10578-020-01010-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sheftall AH, Vakil F, Armstrong SE, et al. Clinical risk factors, emotional reactivity/regulation and suicidal ideation in elementary school-aged children. J Psychiatr Res. 2021;138:360-365. doi: 10.1016/j.jpsychires.2021.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shinsugi C, Stickley A, Konishi S, Ng CFS, Watanabe C. Seasonality of child and adolescent injury mortality in Japan, 2000-2010. Environ Health Prev Med. 2015;20(1):36-43. doi: 10.1007/s12199-014-0421-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sourander A, Aromaa M, Pihlakoski L, et al. Early predictors of deliberate self-harm among adolescents. A prospective follow-up study from age 3 to age 15. J Affect Disord. 2006;93(1-3):87-96. doi: 10.1016/j.jad.2006.02.015 [DOI] [PubMed] [Google Scholar]
- 67.Studart-Bottó P, Martins-Junior DF, Sarmento S, Argolo L, Galvão-de-Almeida A, Miranda-Scippa Â. Self-injurious behavior and related mortality in children under 10 years of age: a retrospective health record study in Brazil. Braz J Psychiatry. 2020;42(1):40-45. doi: 10.1590/1516-4446-2018-0355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Taussig HN, Harpin SB, Maguire SA. Suicidality among preadolescent maltreated children in foster care. Child Maltreat. 2014;19(1):17-26. doi: 10.1177/1077559514525503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Thompson R, Briggs E, English DJ, et al. Suicidal ideation among 8-year-olds who are maltreated and at risk: findings from the LONGSCAN studies. Child Maltreat. 2005;10(1):26-36. doi: 10.1177/1077559504271271 [DOI] [PubMed] [Google Scholar]
- 70.Väli M, Lang K, Soonets R, Talumäe M, Grjibovski AM. Childhood deaths from external causes in Estonia, 2001-2005. BMC Public Health. 2007;7:158. doi: 10.1186/1471-2458-7-158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Viñas F, Canals J, Gras ME, Ros C, Domènech-Llaberia E. Psychological and family factors associated with suicidal ideation in pre-adolescents. Span J Psychol. 2002;5(1):20-28. doi: 10.1017/S1138741600005795 [DOI] [PubMed] [Google Scholar]
- 72.Walsh RFL, Sheehan AE, Liu RT. Suicidal thoughts and behaviors in preadolescents: findings and replication in two population-based samples. Depress Anxiety. 2021;38(1):48-56. doi: 10.1002/da.23087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Weiner AS, Pfeffer CR. Suicidal status, depression, and intellectual functioning in preadolescent psychiatric inpatients. Compr Psychiatry. 1986;27(4):372-380. doi: 10.1016/0010-440X(86)90013-1 [DOI] [PubMed] [Google Scholar]
- 74.Williams K, Levine AR, Ledgerwood DM, Amirsadri A, Lundahl LH. Characteristics and triage of children presenting in mental health crisis to emergency departments at Detroit regional hospitals. Pediatr Emerg Care. 2018;34(5):317-321. doi: 10.1097/PEC.0000000000001057 [DOI] [PubMed] [Google Scholar]
- 75.Zhu X, Tian L, Huebner ES. Trajectories of suicidal ideation from middle childhood to early adolescence: risk and protective factors. J Youth Adolesc. 2019;48(9):1818-1834. doi: 10.1007/s10964-019-01087-y [DOI] [PubMed] [Google Scholar]
- 76.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133-154. doi: 10.1093/epirev/mxn002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threat Behav. 2014;44(3):273-303. doi: 10.1111/sltb.12070 [DOI] [PubMed] [Google Scholar]
- 78.Muehlenkamp JJ, Claes L, Havertape L, Plener PL. International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child Adolesc Psychiatry Ment Health. 2012;6:10. doi: 10.1186/1753-2000-6-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Glenn CR, Kleiman EM, Kellerman J, et al. Annual research review: a meta-analytic review of worldwide suicide rates in adolescents. J Child Psychol Psychiatry. 2020;61(3):294-308. doi: 10.1111/jcpp.13106 [DOI] [PubMed] [Google Scholar]
- 80.Westefeld JS, Bell A, Bermingham C, et al. Suicide among preadolescents: a call to action. J Loss Trauma. 2010;15:381-407. doi: 10.1080/15325024.2010.507655 [DOI] [Google Scholar]
- 81.Li J, Precht DH, Mortensen PB, Olsen J. Mortality in parents after death of a child in Denmark: a nationwide follow-up study. Lancet. 2003;361(9355):363-367. doi: 10.1016/S0140-6736(03)12387-2 [DOI] [PubMed] [Google Scholar]
- 82.Cha CB, Franz PJ, M Guzmán E, Glenn CR, Kleiman EM, Nock MK. Annual research review: suicide among youth: epidemiology, (potential) etiology, and treatment. J Child Psychol Psychiatry. 2018;59(4):460-482. doi: 10.1111/jcpp.12831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ritchie H, Roser M. Gender ratio. Our World In Data. Published June 2019. Accessed April 20, 2022. https://ourworldindata.org/gender-ratio
- 84.Hostinar CE, Johnson AE, Gunnar MR. Parent support is less effective in buffering cortisol stress reactivity for adolescents compared to children. Dev Sci. 2015;18(2):281-297. doi: 10.1111/desc.12195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Steinberg L, Silverberg SB. The vicissitudes of autonomy in early adolescence. Child Dev. 1986;57(4):841-851. doi: 10.2307/1130361 [DOI] [PubMed] [Google Scholar]
- 86.May AM, Klonsky ED. What distinguishes suicide attempters from suicide ideators? a meta-analysis of potential factors. Clin Psychol Sci Pract. 2016;23:5-20. [Google Scholar]
- 87.Kessler RC, Berglund P, Demler O, et al. ; National Comorbidity Survey Replication . The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289(23):3095-3105. doi: 10.1001/jama.289.23.3095 [DOI] [PubMed] [Google Scholar]
- 88.Lee PH, Doyle AE, Li X, et al. Genetic association of attention-deficit/hyperactivity disorder and major depression with suicidal ideation and attempts in children: the Adolescent Brain Cognitive Development Study. Biol Psychiatry. 2021;S0006-3223(21)01864-3. doi: 10.1016/j.biopsych.2021.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bridge JA, Horowitz LM, Fontanella CA, et al. Age-related racial disparity in suicide rates among US youths from 2001 through 2015. JAMA Pediatr. 2018;172(7):697-699. doi: 10.1001/jamapediatrics.2018.0399 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eTable 1. Study characteristics
eTable 2. Sensitivity analyses of prevalence rates of self-injurious thoughts and behaviors
eTable 3. Univariate moderator analyses for Lifetime self-injurious thoughts and behaviors
eFigure. Funnel plots for effect sizes in the meta-analyses