Abstract
Patients with coronary artery disease (CAD) are more sedentary compared with the general population, but contemporary cardiac rehabilitation (CR) programmes do not specifically target sedentary behaviour (SB). We developed a 12-week, hybrid (centre-based+home-based) Sedentary behaviour IntervenTion as a personaLisEd Secondary prevention Strategy (SIT LESS). The SIT LESS programme is tailored to the needs of patients with CAD, using evidence-based behavioural change methods and an activity tracker connected to an online dashboard to enable self-monitoring and remote coaching. Following the intervention mapping principles, we first identified determinants of SB from literature to adapt theory-based methods and practical applications to target SB and then evaluated the intervention in advisory board meetings with patients and nurse specialists. This resulted in four core components of SIT LESS: (1) patient education, (2) goal setting, (3) motivational interviewing with coping planning, and (4) (tele)monitoring using a pocket-worn activity tracker connected to a smartphone application and providing vibrotactile feedback after prolonged sedentary bouts. We hypothesise that adding SIT LESS to contemporary CR will reduce SB in patients with CAD to a greater extent compared with usual care. Therefore, 212 patients with CAD will be recruited from two Dutch hospitals and randomised to CR (control) or CR+SIT LESS (intervention). Patients will be assessed prior to, immediately after and 3 months after CR. The primary comparison relates to the pre-CR versus post-CR difference in SB (objectively assessed in min/day) between the control and intervention groups. Secondary outcomes include between-group differences in SB characteristics (eg, number of sedentary bouts); change in SB 3 months after CR; changes in light-intensity and moderate-to-vigorous-intensity physical activity; quality of life; and patients’ competencies for self-management. Outcomes of the SIT LESS randomised clinical trial will provide novel insight into the effectiveness of a structured, hybrid and personalised behaviour change intervention to attenuate SB in patients with CAD participating in CR. Trial registration number NL9263.
Keywords: sedentary behaviour, cardiac rehabilitation, secondary prevention, behaviour change intervention, mobile health, e-health, cardiovascular disease
WHAT IS ALREADY KNOWN ON THIS TOPIC
A sedentary lifestyle is associated with an increased risk of cardiovascular mortality and morbidity.
Patients with cardiovascular disease are more sedentary compared with the general population, while daily time spent sedentary remains high following contemporary cardiac rehabilitation (CR) programmes.
WHAT THIS STUDY ADDS
The Sedentary Behaviour Intervention as a Personalised Secondary Prevention Strategy (SIT LESS) randomised clinical trial evaluates the effects of a 12-week, hybrid (centre-based+home-based), personalised behaviour change intervention on sedentary behaviour (SB) in patients with coronary artery disease.
Insights on the impact of SIT LESS as add-on module to CR on changes in quality of life, functional outcomes and cardiovascular risk factors.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE AND/OR POLICY
Targeting SB may be a novel strategy to improve habitual physical activity of patients with cardiovascular disease beyond supervised exercise training sessions.
Personalised behaviour change interventions, supported by technology-based programmes and supplemented with (digital) coaching, may become the new standard of future CR programmes.
Introduction
Exercise-based cardiac rehabilitation (CR) is strongly recommended for patients with coronary artery disease (CAD) in international guidelines to improve survival and quality of life.1 Contemporary CR programmes adopt a multidisciplinary approach, including exercise training, psychosocial management, smoking cessation, nutrition counselling and management of blood pressure, lipid spectrum and weight, but do not specifically target sedentary behaviour (SB).2
Emerging evidence indicates that SB, defined as any low-intensity behaviour (energy expenditure of ≤1.5 metabolic equivalent of task (MET)) while awake in a seated or reclined posture,3 is high in patients with CAD and remains high after completion of contemporary CR.4–7 High levels of SB are associated with an increased risk of cardiovascular mortality and morbidity.8 Replacement of sedentary time by light-intensity or moderate-to-vigorous-intensity activities has been shown to attenuate the risk for adverse outcomes, subsequently contributing to improved clinical outcomes in patients with CAD.9 10 Furthermore, breaking up SB by taking active breaks could counteract the detrimental effects of prolonged sedentary bouts regardless of total sedentary time.11 Therefore, independent of engagement in exercise, reducing SB may hold great clinical promise in patients with CAD.
The Sedentary Behaviour Intervention as a Personalised Secondary Prevention Strategy (SIT LESS) study aims to develop and evaluate the effectiveness of a structured, hybrid behaviour change intervention to reduce sedentary time among patients with CAD participating in CR. For this purpose, a pragmatic, multicentre randomised clinical trial (RCT) will be conducted. The primary aim is to investigate the effect of the SIT LESS programme compared with usual care on changes in objectively measured SB, expressed as daily time spent sedentary, following completion of CR. Secondary outcomes include SB characteristics (eg, number and duration of daily sedentary bouts); change in sedentary time at 3 months after CR completion; changes in light-intensity physical activity (LIPA) and moderate to vigorous-intensity physical activity (MVPA); quality of life; and patients’ competencies for self-management, as well as changes in lipid profile and cardiovascular risk score. We hypothesise that SIT LESS results in a greater decrease in time spent sedentary compared with usual care, directly after CR, which may translate to a better quality of life, increased physical activity levels and improved clinical outcomes at follow-up compared with contemporary CR.
Methods
Study design
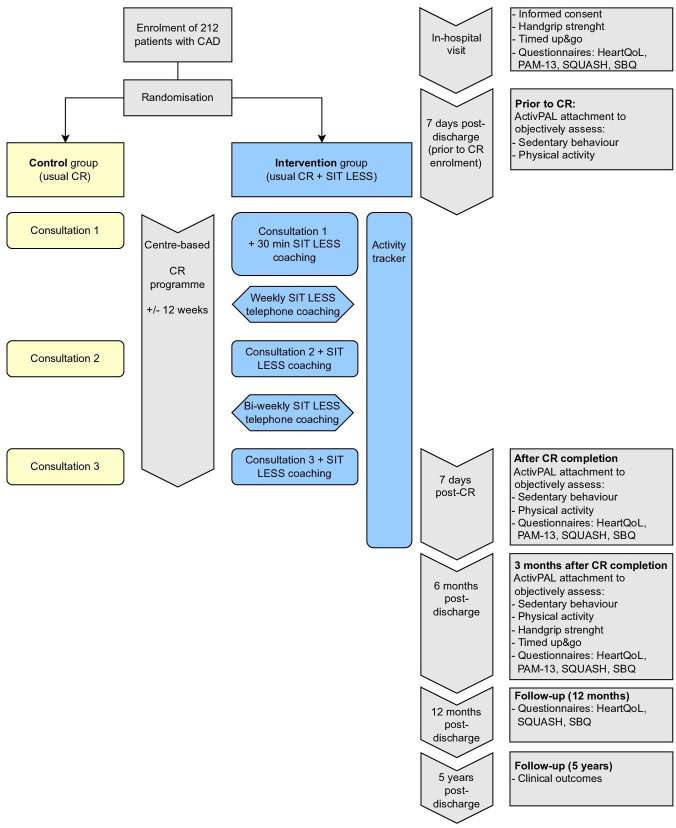
A pragmatic, multicentre RCT will be performed in order to determine the effectiveness of SIT LESS, a 12-week, hybrid and personalised behaviour change intervention in addition to CR, to reduce SB in patients with CAD. Patients will be randomly assigned to either the control (usual care CR) or the intervention group (usual care CR+SIT LESS) (figure 1).
Figure 1.
SIT LESS RCT flowchart. CAD, coronary artery disease; CR, cardiac rehabilitation; HeartQoL, Heart Quality of Life; PAM-13, 13-Item Patient Activation Measure; RCT, randomised clinical trial; SBQ, Sedentary Behaviour Questionnaire; SIT LESS, Sedentary Behaviour Intervention as a Personalised Secondary Prevention Strategy; SQUASH, Short Questionnaire to Assess Health-Enhancing Physical Activity.
Study setting and recruitment
Patients from Bernhoven Hospital (Uden, Netherlands) and Rijnstate Hospital (Arnhem, Netherlands) will be included in the SIT LESS RCT. Patients are eligible for participation if referred to CR because of stable CAD, an acute coronary syndrome and/or after coronary revascularisation. Additional inclusion and exclusion criteria are provided in table 1. Eligible patients will be verbally informed about the SIT LESS RCT procedures by their nurse specialist. When interested in trial participation, they are seen by a member of the research team to obtain written informed consent. We will record the number of participants that reject trial participation and collect the main reason for non-participation. All subjects withdrawn within the first 2 weeks after inclusion will be replaced. The study burden is negligible up to this point, justifying replacing these subjects and to ensure sufficient power to assess our primary outcome. The number of replaced subjects will be recorded and the reason for withdrawal will be carefully documented.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|
|
CABG, coronary artery bypass grafting; NYHA, New York Heart Association; PA, physical activity; SB, sedentary behaviour.
Randomisation, blinding and treatment allocation
After obtaining informed consent, patients are randomly assigned to either the control or the intervention group. Randomisation will be stratified by sex and hospital to ensure balance of the treatment arms. We use a computerised randomisation system (Castor Electronic Data Capture 2021, Ciwit B.V., Amsterdam, Netherlands) with block randomisation in random block sizes (range 4–6) for allocation concealment. The investigators, nurse specialists and patients cannot be blinded for the treatment allocation due to the nature of the intervention.
Usual care
All patients receive usual care and will be seen by their cardiologist and/or general practitioner as clinically appropriate. Usual care consists of a comprehensive CR programme, delivered by healthcare professionals such as specialist trained nurses and physical therapists, with a total duration of ~12 weeks. One to three regular, individual consultations are scheduled with the nurse specialist focussing on lifestyle, medication and psychosocial well-being. Participants are offered an outpatient physical activity programme, consisting of ~12 supervised, 1-hour exercise sessions across 6 weeks. If indicated, a dietary module, psychoeducative prevention module, psychological module and/or additional consultations with the nurse specialist can be added.
Sedentary Behaviour Intervention as a Personalised Secondary Prevention Strategy
Development
Behaviour change interventions based on a theoretical framework, tailored to the target population and consisting of multiple behaviour change strategies, appear most effective to improve physical activity patterns.12 Following these principles, we used an intervention mapping adaptation framework13 to adapt a previously developed, successful and cost-effective self-management intervention for clinical settings14 into SIT LESS and subsequently tailored it to the needs of patients with CAD. First, we identified determinants of physical activity and SB in patients with CAD from literature (online supplemental file 1). Subsequently, we adapted (theory-based) methods and practical applications of the intervention to target SB in patients with CAD. Finally, we evaluated the adapted intervention in two advisory board meetings with three patients with CAD and three nurse specialists. This resulted in a structured SIT LESS manual consisting of four core components: (1) patient education; (2) goal setting; (3) motivational interviewing with coping planning and self-efficacy; and (4) (self-)monitoring, learning, problem solving and maintenance of behaviour change (online supplemental file 2). The SIT LESS manual is used by the nurse specialist during three face-to-face consultations for SIT LESS coaching. Additionally, patients use an activity tracker that provides real-time vibrotactile feedback and enables continuous SB (self-)monitoring. Subsequently, patients are (bi-)weekly contacted by telephone for coaching purposes based on SB monitoring data.
bmjsem-2022-001364supp001.pdf (284.5KB, pdf)
bmjsem-2022-001364supp002.pdf (7.7MB, pdf)
Patient involvement
Three patients with CAD were closely involved in the study development, with one patient representing the Harteraad (Dutch National CAD Patient Advisory Council). The advisory board was consulted once in the preparation phase (study design, outcome measures and recruitment strategy) and twice during development of SIT LESS (full content and design of the SIT LESS manual). After processing feedback of the first meeting, the advisory board critically appraised the SIT LESS manual, ultimately reaching unanimous consensus about the content. Our advisory board will be regularly updated and informed throughout the trial.
SIT LESS manual
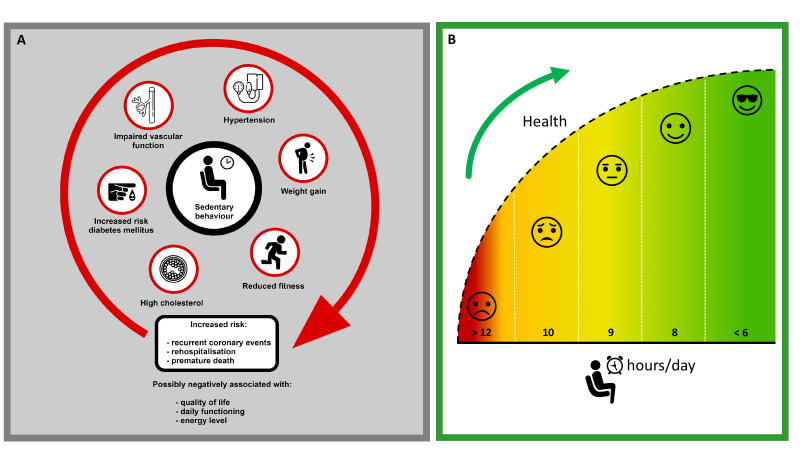
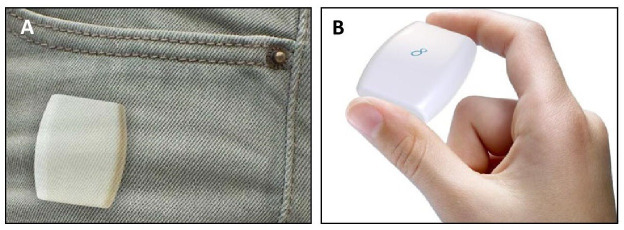
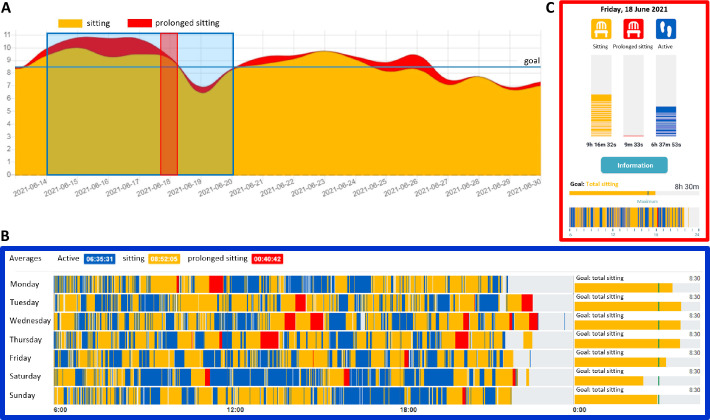
Tailoring the information to the needs and abilities of the patient is essential throughout the SIT LESS manual (online supplemental file 2). Therefore, steps 1 and 2 are focused on patient education to enhance the patient’s knowledge regarding the risks of SB and benefits of reducing SB, using visual materials (figure 2). In step 3, motivation to reduce SB is discussed, focussing on underlying personal reasons and addressing possible concerns. In step 4, the goal of maximal daily SB is set and patients select an expected scenario regarding their SB. Based on the selected scenario, patients are challenged to explain personal reasons for sitting less and to identify potential barriers. Motivational interviewing is an important part of patient counselling and adopts language designed to strengthen personal motivation and commitment to a specific goal.13 To improve chances to achieve the planned outcomes, a specific plan (if–then planning) is defined and challenging situations and possible solutions are discussed (step 5). In step 6, the patient’s confidence achieving the goal is determined and reasons for change are reinforced, while potential residual barriers are evaluated and discussed. In step 7, the pocket-worn activity tracker is introduced (Activ8 sit tracker; 2M Engineering, Valkenswaard, Netherlands; figure 3). This is a commercially available, small (30×32×10 mm), lightweight (20 g) and validated device to monitor SB.15 Self-monitoring is a valuable behaviour change method,13 16 prompting patients to record their SB. The activity tracker can be connected to a secured, personalised, patient-centred smartphone application (RISE; Appbakkers B.V., Zwolle, Netherlands) that enables patients and nurse specialists to (1) register and adjust personal goals and (2) upload and review daily SB (figure 4). The activity tracker allows for recognising prolonged bouts of uninterrupted sitting (ie, ≥30 min). By default, the activity tracker provides direct vibrotactile feedback after each prolonged sedentary bout. Patients can (temporarily) switch off the vibrotactile feedback using the smartphone application. Using the activity tracker with vibrotactile feedback enables 24/7 monitoring of SB. Based on monitored SB, patients are regularly contacted by telephone for supportive coaching and to evaluate predefined SB targets using motivational interviewing techniques. To ensure similar mode of operation, a standard operating procedure was used for the telephone coaching (online supplemental file 3). In step 8, patients evaluate their SB during a follow-up face-to-face meeting with the nurse specialist. Obstacles are discussed and possible causes are identified. Subsequently, a new concrete plan for the upcoming period is formulated. All steps of the SIT LESS manual are summarised in table 2. The participating nurse specialists are registered with the Dutch Association for Cardiovascular Nurses and are trained in the basics of motivational interviewing as part of their education. Prior to delivering SIT LESS to the intervention group, all nurse specialists received a comprehensive and accredited additional training course in delivering the intervention consultations and applying motivational interviewing, under the guidance of a behavioural psychologist. The training course consisted of a self-study document (±3 hours of preparation), followed by an on-site group training (±8 hours) where theory was explained and subsequently practised through active role-play.
Figure 2.
Example of visual material from the Sedentary Behaviour Intervention as a Personalised Secondary Prevention Strategy intervention manual to enhance patients’ knowledge regarding the risks of too much time spent sedentary (A) and the benefits of reducing it (B).
Figure 3.
Activity tracker. The Activ8 sit tracker can be easily worn in the trouser pocket (A) and is a small, lightweight activity tracker (B).
Figure 4.
Impression of the sedentary behaviour data in the online dashboard and smartphone application collected by the Activ8 sit tracker. (A) Part of the monthly overview in the online dashboard with the date on the x-axis and the sedentary hours/day on the y-axis. Maximum total sedentary goal was set at 8 hours/day, as shown by the blue horizontal line. A decreasing trend can be observed in the total sedentary time, as well as the amount of prolonged sedentary time. (B) Weekly overview in the online dashboard representing the time frame depicted by the blue box (A). Data regarding time spent being physically active, sitting and prolonged sitting throughout the day are visible on the left, with the total amount of sitting (sitting+prolonged sitting) on the right. (C) Screenshot of the day view on the smartphone application; the selected day corresponds to the red box (A).
Table 2.
Summary of the core components of the SIT LESS manual
| Step | Core component | Aim | Content* |
| 1 A Risk factors |
Patient education | To introduce prolonged sitting as a risk factor for CVD progression | Online supplemental figure S2-1A with CVD risk factors, verbal introduction of SB as one of the CVD risk factors and correcting possible misconceptions |
| 1 B CR |
Patient education | To inform about facilitating role of CR in targeting CVD risk factors | Verbal explanation of CR and specifically targeting SB in an individually tailored CR programme |
| 2 A SB |
Patient education | To explain SB with examples of several SB settings |
Online supplemental figure S2-2A1, an easy-to-understand figure with examples of sedentary everyday life situations Online supplemental figure S2-2A2, an example of two daily schedules to illustrate that most part of the day is spent sitting (without noticing) |
| 2 B Detrimental health consequences of SB |
Patient education | To increase knowledge about the detrimental health effects of SB | Online supplemental figure S2-2B, an insightful figure to clarify the ways in which SB could lead to adverse health effects |
| 2 C Sitting less and regularly standing up improves health |
Patient education | To discuss (health) benefits of sitting less and interrupting prolonged sitting bouts | Online supplemental figure S2-2C, easy-to-remember graphs explaining how reduced sitting and regular sitting interruption can improve health status using colours and emoticons |
| 2 D More PA improves health |
Patient education | To explain (health) benefits of increasing regular PA | Online supplemental figure S2-2D, easy-to-remember graph to explain health benefits of increasing daily PA volumes using colours and emoticons |
| 3 A Reasons to sit less |
Motivation and goal setting | To identify personal reasons for sitting less and enforce identified benefits/introduce new benefits | Drop-down list with common reasons to reduce SB to explore whether these are applicable to the patient |
| 3 B Concerns regarding sitting less |
Motivation and goal setting | To identify personal concerns for sitting less and (if inaccurate) correct identified concerns/discuss solutions | Drop-down list with common concerns regarding reducing SB to explore whether these are applicable to the patient |
| 4 A Scenario selection and goal setting |
Motivation and goal setting | To set the goal of daily sedentary time and provoke language of change using scenario selection | Online supplemental figure S2-4A, four examples of activity tracker-based SB reports ranging from excellent to poor regarding goal achievement; patient sets a sitting goal, selects a (desired) scenario and elaborates why |
| 5 A Possibilities, difficult situations and solutions to sit less |
Planning and self-efficacy | To determine possibilities to sit less in everyday life situations, discuss obstacles and define effective solutions | Drop-down list with common obstacles and corresponding solutions to explore whether these are applicable to the patient |
| 5 B A plan to sit less |
Planning and self-efficacy | To define a clear action and coping plan to reduce SB and regularly break up sitting | Templates for action and coping plans (if–then) to effectively reduce SB |
| 6 A Confidence in the ability to accomplish the goal |
Planning and self-efficacy | To determine the confidence in reducing SB (reaching the defined goal) | Ruler (1–10 scale) to score confidence in reaching the reduced sitting goal; if confidence is low, residual barriers are explored and/or the goal is set less ambitious |
| 7 A Introduction of the activity tracker |
Monitoring, learning, problem solving and maintenance of behaviour change | To give an introduction of the activity tracker with smartphone application for monitoring SB and coaching in the home environment | Live demonstration of the functionalities of the activity tracker and smartphone application and introduce telephone consultations for coaching purposes to continue the behaviour change intervention in the home environment |
| 8 A Evaluation of SB report |
Monitoring, learning, problem solving and maintenance of behaviour change | To evaluate the SB over the past period, identify days when sitting goals were not achieved and explore the patient’s thoughts | Patient’s own SB report using the online dashboard; reinforce good periods and highlight discrepancies between the desired and actual SB with regard to the goal that is set |
| 8 B Learning, problem solving and maintenance of behaviour change |
Monitoring, learning, problem solving and maintenance of behaviour change | To identify patterns of success or failure reducing SB over the past period and to evaluate obstacles and solutions and define a clear action plan for the upcoming period; the patient continues monitoring at home using the activity tracker with smartphone application and coaching by telephone consultations | Templates to discuss experienced obstacles and effective solutions to reduce SB; use the online dashboard to set the goal for the upcoming period, identify potential barriers and ways to overcome these, resulting in a concrete plan (what to do when) |
*For the SIT LESS intervention manual including online supplemental figures S2-1A–S2-4A (see online supplemental file 2, SIT LESS intervention manual).
CR, cardiac rehabilitation; CVD, cardiovascular disease; PA, physical activity; SB, sedentary behaviour; SIT LESS, Sedentary Behaviour Intervention as a Personalised Secondary Prevention Strategy.
bmjsem-2022-001364supp003.pdf (651.5KB, pdf)
SIT LESS timeline
SIT LESS is a 12-week, in-person and nurse-delivered, hybrid (centre-based+home-based) behaviour change intervention that is offered alongside regular CR (usual care) (figure 1). SIT LESS consists of three face-to-face consultations, (bi)weekly telephone coaching and continuous monitoring of SB in the home environment using a pocket-worn activity tracker that provides real-time vibrotactile feedback and ability to monitor SB throughout the intervention.
Consultation 1: SIT LESS coaching
This consultation starts with patient education regarding the risks of SB and benefits of reducing SB (steps 1 and 2). Subsequently, motivation and goal-setting are discussed (steps 3 and 4) and a clear, individualised action plan to reduce and regularly interrupt SB is defined (steps 5 and 6). Then patients are provided with the activity tracker, including real-time, vibrotactile feedback throughout the intervention period (±12 weeks), after they received an extensive introduction on the tracker and smartphone application (step 7). This first SIT LESS consultation takes place at the start of CR and takes ±30 min.
Consultation 2: SIT LESS coaching
The face-to-face interim evaluation (consultation 2) takes place at ±6 weeks after consultation 1. This consultation is focused on (self-)monitoring, learning, problem solving and maintenance of behaviour change. Data collected by the activity tracker are summarised in an SB report from the online dashboard, which is evaluated together with the patient. Patterns of success or failure in achieving SB goals are identified (step 8). Subsequently, an updated, personal action plan is defined, and additional/novel barriers and ways to overcome these are considered. If indicated, previous steps of the SIT LESS manual can be discussed, reviewed and adjusted. This consultation will take ±30 min.
Consultation 3: SIT LESS coaching
The last face-to-face evaluation (consultation 3) takes place at ±12 weeks after consultation 1. During this closing visit, the course of SB throughout the intervention period is re-evaluated and, again, patterns of success or failure in achieving SB goals are identified (step 8). The SB goal with action plan is updated in the personalised online dashboard. Special focus during this consultation is on maintenance of behaviour change, also after the intervention period. If indicated, previous steps of the SIT LESS manual can be repeated (steps 1–6). This consultation will take ±30 min.
Telephone coaching
Patients will be contacted by telephone for supportive coaching based on their SB reports collected through the activity tracker throughout the intervention period. During weeks 1–6, telephone coaching takes place on a weekly basis, followed by biweekly telephone coaching during weeks 7–12. Any problems using the activity tracker that the patient may have encountered will be resolved. The SB goals are evaluated by motivational interviewing techniques to stimulate patients to (further) reduce SB (online supplemental file 3). Telephone coaching will take ±10 min per consultation.
Outcome measures
The primary outcome of the SIT LESS RCT is the change in objectively measured SB, expressed in daily time spent sedentary, following CR completion. Secondary outcomes include SB characteristics (eg, number and duration of daily sedentary bouts and proportion of participants with a 30 or 60 min/day decrease in sedentary time after CR); change in time spent sedentary at 3 months after CR completion; changes in LIPA and MVPA (assessed prior to CR, after CR completion and 3 months after CR completion); and changes in quality of life, patients’ competencies for self-management, as well as changes in lipid profile and cardiovascular risk score. Other outcome measures include Timed Up and Go; handgrip strength; process-evaluation data (eg, number of visits attended, delivered CR modules, number of physiotherapy sessions and valid wear days of the activity tracker); and incidence of clinical endpoints (ie, all-cause mortality, cardiovascular mortality, and rehospitalisation and recurrence of acute coronary events) during 5 years of follow-up (figure 1). The data catalogue can be found in online supplemental file 4.
bmjsem-2022-001364supp004.pdf (150.8KB, pdf)
Measurements
SB and physical activity
SB and physical activity will be objectively assessed using a validated accelerometer (ActivPAL3 micro; PAL Technologies, Glasgow, UK).17 The ActivPAL is a small device (25×45×5 mm) attached to the patient’s thigh using hypoallergenic tape. The ActivPAL is sealed with a nitrile sleeve and transparent tape for waterproof protection to allow for continuous monitoring. Patients are instructed to wear the ActivPAL 24 hours/day for 8 consecutive days and are instructed to fill in a sleep diary. After this measurement, the ActivPAL will be send back to our research institute by mail. The ActivPAL combines a triaxial accelerometer with an inclinometer which accurately distinguishes between sitting, standing and walking.17 Raw data are analysed by a modified version of the script of Winkler et al.18 In the analysis of SB and physical activity, we will remove the first 24 hours of the measurement to counteract a possible Hawthorne effect. Total sedentary time is expressed in hours per day and accumulation of sedentary time will be examined by calculating the number of prolonged (≥30 min) and short (<30 min) sedentary bouts. Activities are categorised as LIPA (MET score <3) or MVPA (ME score ≥3) and expressed in hours per day.
Questionnaires
Quality of life
The health-related quality of life will be assessed using the HeartQoL questionnaire, which is designed and validated specifically for patients with CAD.19 It consists of 14-items (10-item physical and 4-item emotional) resulting in subscales ranging from 0 (poor) to 3 (better) and a global score.19
Patients’ competencies for self-management
Patients’ competencies for self-management of their health will be assessed using the 13-Item Patient Activation Measure. This 13-item questionnaire is validated in the Dutch language and results in a theoretical score ranging from 0 (poor) to 100 (better).20
Self-reported SB and physical activity
To understand different SB and physical activity settings, we added the Sedentary Behaviour Questionnaire (SBQ)21 and Short Questionnaire to Assess Health-Enhancing Physical Activity (SQUASH).22 The SBQ determines time spent sedentary in nine distinct everyday life situations. The SQUASH determines time spent performing physical activity in four different settings: work, transportation, household and leisure time.
Blood samples
A venous blood sample, obtained by venepuncture, is collected to assess low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, total cholesterol, triglycerides, haemoglobin, leucocytes, and thrombocytes at baseline and after CR.
Cardiovascular risk score
The SMART risk score, containing 14 clinical predictors, estimates the 10-year risk of recurrent cardiovascular events23 and is calculated prior to CR and after CR completion. The clinical predictors are derived from the electronic patient file.
Functional tests
Timed Up and Go test
Timed Up and Go will be assessed by observing the time while a patient rises from an arm chair, walks 3 m, turns, walks back and sits down again. The test is contraindicated when the patient is (temporarily) bed or chair bound.
Handgrip strength test
Handgrip strength will be assessed with a hydraulic, analogue hand size adjusted dynamometer (Jamar, Jackson, Michigan, USA). The patient is seated in a chair without armrest with the elbow flexed in a 90° angle position. Both hands will perform three measurements with ±30 s rest between measurements. The maximum strength effort in kilogram will be used for analysis. Contraindications for performing the test are a coronary artery bypass grafting within the past 2 weeks or a coronary angiography within the past 48 hours.
Patient characteristics and clinical outcomes
Patient characteristics (eg, age, sex, medical history and index diagnosis) and process evaluation data (eg, delivered CR modules and number of attended physiotherapy sessions) will be derived from the electronic patient file. Additionally, we will assess socioeconomic status and ethnicity and verify whether patients are generally using a smartwatch and/or any activity tracker to count their daily steps. Incidence of clinical outcomes such as all-cause mortality, cardiovascular mortality, rehospitalisation and recurrence of acute coronary events will be evaluated by checking the electronic patient files and/or by consulting the Dutch Population Register during 5 years of follow-up.
Adherence of activity tracker
For patients in the intervention group, we will calculate the number of valid wear days of the activity tracker (≥10 hours/day) to assess adherence, and we will evaluate the course of SB throughout the intervention period (ie, weekly average of sedentary time (hours/day) and the number of (prolonged) sitting bouts). This assessment is additional to the objective SB and PA measurements prior to, immediately after and 3 months after CR. This way, we determine changes in SB throughout the intervention period. We will also monitor the number of SIT LESS telephone coaching sessions and attended face-to-face consultations.
Data management and accessibility
All data will be stored in the Digital Research Environment (DRE, mydre.org), an online, cloud-based, globally available research platform. The DRE facilitates users to collaborate on research projects within the boundaries of data management regulations (General Data Protection Regulation and Good Clinical Practice compliant) in a flexible and safe way regarding security, Information and Communication Technology (ICT) infrastructure and audit trail. Standard software packages are available for data handling and statistical analysis (eg, SPSS and R Studio). In line with the Open Science initiative and FAIR principles, SIT LESS data will be available for reuse on reasonable request via the corresponding author.
Sample size
Sample size was calculated using Russ-Lenth software (JavaApplets for Power and Sample Size, 2016, Iowa, USA). A power calculation was performed based on detecting a difference in the CR-related change in objectively measured SB between the intervention and control group. The sample size (N) was calculated with a power of 80% (1−β=0.80) and a level of significance of 5% (α=0.05, two-tailed). Previous studies reported that replacement of 0.5-hour/day sitting by LIPA is associated with a 17% risk reduction of all-cause mortality,24 which is feasible and clinically relevant for patients with CAD. Using an SD of 70.7 min/day25 and an expected reduction of 0.5-hour/day sitting, a sample size of 90 patients per arm is needed. Taking a dropout of 15% into consideration, we will include 212 patients in our study.
Statistical analysis
Statistical analyses will be performed using SPSS statistics V.25.0. Collected data will be checked for normality of distribution (visually and using the Shapiro-Wilk test). Normally distributed continuous variables will be presented as mean±SD and non-normally variables as median (IQR). Categorical variables will be expressed as numerical values and percentages. Percentages will be calculated on the number of non-missing observations. In all cases the number of missing values will be specified. All statistical tests will be two-sided and p values of <0.05 will be considered statistically significant.
Primary analyses will be performed on an intention-to-treat basis. Descriptive statistics will be used to report patient characteristics. Between-group differences and within-group differences in the primary outcome measures will be evaluated using mixed model analyses using random intercepts. Time will be described as categorical variable. Mixed model analyses are preferred over repeated measures analysis of variance because of their advantage in dealing with missing values. In addition, we will identify patient and disease characteristics that are associated with changes in SB over time by multivariate mixed model analyses. Finally, incidence of clinical outcomes (ie, all-cause mortality, cardiovascular mortality, rehospitalisation and recurrence of acute coronary syndromes) during follow-up will be compared between the intervention and control groups using Kaplan-Meier and Cox proportional hazard analyses.
Discussion
The SIT LESS trial examines the effect of a 12-week, hybrid and personalised behaviour change intervention on SB in patients with CAD participating in CR. We developed a multidisciplinary intervention programme that will be offered alongside usual care CR. Contemporary CR offers the infrastructure to easily incorporate SIT LESS and our intervention fits in perfectly with the holistic approach to promote a healthy lifestyle in patients with CAD across multiple domains (eg, improve physical activity patterns, smoking cessation, stress reduction and weight reduction). Additionally, the preceding cardiovascular event provides the momentum for lifestyle changes, including targeting SB. In face-to-face, motivational interviewing consultations with nurse specialists, patients set their personal SB goals and define a specific plan to reach these goals. The SIT LESS intervention also involves a commercially available activity tracker that provides vibrotactile feedback on prolonged sitting and is connected to a smartphone application and web-based platform to monitor SB and to enable (remote) coaching throughout the intervention programme. We incorporated the staircase approach for our ‘sitting less and moving more strategy’, to achieve more sustainable improvements in movement patterns, especially in this physically inactive, sedentary patient population.26 The first step focuses on reducing and regularly interrupting SB, followed by increasing LIPA throughout the day and ultimately to increase MVPA. We hypothesise that the SIT LESS intervention results in greater reductions in sedentary time compared with the control group, which may ultimately translate into a better disease prognosis.
Previous studies show that most patients with CAD maintain an unhealthy lifestyle, including SB, despite comprehensive exercise-based CR programmes.5 Although many (e-Health) initiatives arose to improve physical activity in patients with CAD, they reported only small-to-medium, non-sustainable effects.27 The COVID-19 pandemic accelerated the adoption of digital health and wearables,28 but worldwide lockdowns further increased SB levels in patients with CAD simultaneously.29 Cardiovascular health benefits can be obtained by reducing total sedentary time, but also through interruption of SB.26 An effective strategy to reduce and regularly interrupt SB within contemporary CR programmes is currently lacking but has significant potential. This highlights the need for well-designed RCTs on SB-related interventions.
Evidence-based behavioural change interventions are strongly recommended for promoting a healthy lifestyle, but implementation is often challenging.30 An important strength of our study is the cumulative development of SIT LESS with valuable input from the advisory boards, using an intervention mapping adaptation framework to adapt a self-management intervention that was previously proven feasible and (cost-)effective.14 We transparently describe all steps of the adaptation process and share the full content of the SIT LESS manual in this manuscript, which facilitates efficient adaptation of our intervention, for example, to other patient populations in the future. Furthermore, the effectiveness of SIT LESS will be tested in a real-world clinical practice, minimising the translational step. Another strength is the objective assessment of SB, making our approach more reliable than self-reported questionnaires to assess SB.31
Limitations
This study also has some limitations. Due to the nature of the intervention, the investigator, nurse specialists and patients are not blinded for the treatment. Nevertheless, our primary outcome is an ambulant and objective measurement, conducted at the patient’s home environment, without interference of research team members. Another limitation is that this study is not designed (and as such not powered) to investigate the relation of SB and the incidence of clinical outcomes. If SIT LESS effectively reduces SB in patients with CAD, larger RCTs are warranted to investigate the impact on clinical outcomes and assess cost-effectiveness. Because SIT LESS is embedded in regular CR, the intervention is provided by the same nurse specialists as the control condition (regular CR). Therefore, contamination related to patient education about the health benefits of sitting less cannot be excluded. This may lead to underestimation of the effectiveness of SIT LESS. Conducting this trial in real-world clinical practice significantly increases the likelihood of future successful implementation on a larger scale.
Conclusion
The SIT LESS RCT is the first study with a primary focus on reducing and interrupting sedentary time in patients with CAD during CR. The results of this study will provide important insights in the effects of a 12-week, hybrid and personalised behaviour change intervention on objectively measured SB. Beyond its impact on time spent sedentary, we will also explore its effect on physical activity levels, quality of life, cardiovascular risk factors and future clinical outcomes. Limitations of this trial include that investigators and patients are not blinded for the treatment due to the nature of the intervention and that this study is not powered to investigate the relation of SB and secondary outcomes. Nevertheless, when confirming our hypothesis, SIT LESS will have major impact on the content and effectiveness of future CR programmes for patients with CAD.
Acknowledgments
We thank Coen Lauwerijssen and Michel Sperling (2M Engineering, Valkenswaard, Netherlands) for their contribution in the developmental process of the Activ8 sit tracker, and Thomas Smit (Appbakkers B.V., Zwolle, Netherlands) for the technical support regarding the RISE application and web-based dashboard. Furthermore, we are indebted to Karin Verhoeven and Myriam Zootjes (nurse specialists, cardiac rehabilitation) and the members of our patient advisory board (Mariëtte Verbakel, Klaas van Winzum and Paul Berens) for their valuable input in the development of the Sedentary Behaviour Intervention as a Personalised Secondary Prevention Strategy (SIT LESS) programme and careful appraisal of the design and content of the SIT LESS manual consisting of educational and coaching components of SIT LESS.
Footnotes
Twitter: @BvBakel
Contributors: BMAvB drafted the manuscript with input from SHK, JD, DHJT and TMHE. All authors were involved in the critical revision of this article for intellectual content and gave the final approval before submission.
Funding: This study was supported by the Dutch Heart Foundation (senior E-Dekker grant #2017T051).
Competing interests: None declared.
Patient and public involvement: Patients and the public were involved in the design, conduct, reporting and dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Data from the Sedentary Behaviour Intervention as a Personalised Secondary Prevention Strategy randomised clinical trial will be available upon reasonable request via the corresponding author.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study protocol was approved by the medical ethics committee of the Radboud University Medical Center (#2020–6101).
References
- 1.Visseren FLJ, Mach F, Smulders YM. Esc guidelines on cardiovascular disease prevention in clinical practice: developed by the task force for cardiovascular disease prevention in clinical practice with representatives of the European Society of cardiology and 12 medical societies with the special contribution of the European association of preventive cardiology (EAPC). Eur. Heart J. 2021;2021. [DOI] [PubMed] [Google Scholar]
- 2.Dibben G, Faulkner J, Oldridge N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2021;11:Cd001800. 10.1002/14651858.CD001800.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tremblay MS, Aubert S, Barnes JD, et al. Sedentary Behavior Research Network (SBRN) - Terminology Consensus Project process and outcome. Int J Behav Nutr Phys Act 2017;14:75. 10.1186/s12966-017-0525-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prince SA, Blanchard CM, Grace SL, et al. Objectively-measured sedentary time and its association with markers of cardiometabolic health and fitness among cardiac rehabilitation graduates. Eur J Prev Cardiol 2016;23:818–25. 10.1177/2047487315617101 [DOI] [PubMed] [Google Scholar]
- 5.Kotseva K, De Backer G, De Bacquer D, et al. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: results from the European Society of cardiology ESC-EORP EUROASPIRE V registry. Eur J Prev Cardiol 2019;26:824–35. 10.1177/2047487318825350 [DOI] [PubMed] [Google Scholar]
- 6.Biswas A, Oh PI, Faulkner GE, et al. A prospective study examining the influence of cardiac rehabilitation on the sedentary time of highly sedentary, physically inactive patients. Ann Phys Rehabil Med 2018;61:207–14. 10.1016/j.rehab.2017.06.003 [DOI] [PubMed] [Google Scholar]
- 7.Bakker EA, van Bakel BMA, Aengevaeren WRM, et al. Sedentary behaviour in cardiovascular disease patients: risk group identification and the impact of cardiac rehabilitation. Int J Cardiol 2021;326:194–201. 10.1016/j.ijcard.2020.11.014 [DOI] [PubMed] [Google Scholar]
- 8.Ekelund U, Steene-Johannessen J, Brown WJ, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016;388:1302–10. 10.1016/S0140-6736(16)30370-1 [DOI] [PubMed] [Google Scholar]
- 9.Wu Z, Huang Z, Wu Y, et al. Sedentary time, metabolic abnormalities, and all-cause mortality after myocardial infarction: a mediation analysis. Eur J Prev Cardiol 2019;26:96–104. 10.1177/2047487318804611 [DOI] [PubMed] [Google Scholar]
- 10.Buman MP, Winkler EAH, Kurka JM, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005-2006. Am J Epidemiol 2014;179:323–34. 10.1093/aje/kwt292 [DOI] [PubMed] [Google Scholar]
- 11.Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care 2008;31:661–6. 10.2337/dc07-2046 [DOI] [PubMed] [Google Scholar]
- 12.Sharp P, Spence JC, Bottorff JL, et al. One small step for man, one giant leap for men's health: a meta-analysis of behaviour change interventions to increase men's physical activity. Br J Sports Med 2020;54:1208–16. 10.1136/bjsports-2019-100912 [DOI] [PubMed] [Google Scholar]
- 13.Kok G, Gottlieb NH, Peters G-JY, et al. A taxonomy of behaviour change methods: an intervention mapping approach. Health Psychol Rev 2016;10:297–312. 10.1080/17437199.2015.1077155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Bruin M, Oberjé EJM, Viechtbauer W, et al. Effectiveness and cost-effectiveness of a nurse-delivered intervention to improve adherence to treatment for HIV: a pragmatic, multicentre, open-label, randomised clinical trial. Lancet Infect Dis 2017;17:595–604. 10.1016/S1473-3099(16)30534-5 [DOI] [PubMed] [Google Scholar]
- 15.English C, Wondergem R, Hendrickx W, et al. People with stroke are most sedentary in the afternoon and evening. Cerebrovasc Dis 2022:1–6 (published Online First: 2022/01/05). 10.1159/000521209 [DOI] [PubMed] [Google Scholar]
- 16.Biswas A, Faulkner GE, Oh PI, et al. Patient and practitioner perspectives on reducing sedentary behavior at an exercise-based cardiac rehabilitation program. Disabil Rehabil 2018;40:2267–74. 10.1080/09638288.2017.1334232 [DOI] [PubMed] [Google Scholar]
- 17.Edwardson CL, Rowlands AV, Bunnewell S, et al. Accuracy of posture allocation algorithms for Thigh- and Waist-Worn Accelerometers. Med Sci Sports Exerc 2016;48:1085–90. 10.1249/MSS.0000000000000865 [DOI] [PubMed] [Google Scholar]
- 18.Winkler EAH, Bodicoat DH, Healy GN, et al. Identifying adults' valid waking wear time by automated estimation in activPAL data collected with a 24 H wear protocol. Physiol Meas 2016;37:1653–68. 10.1088/0967-3334/37/10/1653 [DOI] [PubMed] [Google Scholar]
- 19.Oldridge N, Höfer S, McGee H, et al. The HeartQoL: Part II. validation of a new core health-related quality of life questionnaire for patients with ischemic heart disease. Eur J Prev Cardiol 2014;21:98–106. 10.1177/2047487312450545 [DOI] [PubMed] [Google Scholar]
- 20.Rademakers J, Maindal HT, Steinsbekk A, et al. Patient activation in Europe: an international comparison of psychometric properties and patients' scores on the short form patient activation measure (PAM-13). BMC Health Serv Res 2016;16:570. 10.1186/s12913-016-1828-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosenberg DE, Norman GJ, Wagner N, et al. Reliability and validity of the sedentary behavior questionnaire (SBQ) for adults. J Phys Act Health 2010;7:697–705. 10.1123/jpah.7.6.697 [DOI] [PubMed] [Google Scholar]
- 22.Wendel-Vos GCW, Schuit AJ, Saris WHM, et al. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity. J Clin Epidemiol 2003;56:1163–9. 10.1016/S0895-4356(03)00220-8 [DOI] [PubMed] [Google Scholar]
- 23.Dorresteijn JAN, Visseren FLJ, Wassink AMJ, et al. Development and validation of a prediction rule for recurrent vascular events based on a cohort study of patients with arterial disease: the smart risk score. Heart 2013;99:866–72. 10.1136/heartjnl-2013-303640 [DOI] [PubMed] [Google Scholar]
- 24.Diaz KM, Howard VJ, Hutto B, et al. Patterns of sedentary behavior and mortality in U.S. middle-aged and older adults: a national cohort study. Ann Intern Med 2017;167:465–75. 10.7326/M17-0212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ter Hoeve N, Sunamura M, van Geffen ME, et al. Changes in physical activity and sedentary behavior during cardiac rehabilitation. Arch Phys Med Rehabil 2017;98:2378–84. 10.1016/j.apmr.2017.05.008 [DOI] [PubMed] [Google Scholar]
- 26.Dunstan DW, Dogra S, Carter SE, et al. Sit less and move more for cardiovascular health: emerging insights and opportunities. Nat Rev Cardiol 2021;18:637–48. 10.1038/s41569-021-00547-y [DOI] [PubMed] [Google Scholar]
- 27.Hodkinson A, Kontopantelis E, Adeniji C, et al. Accelerometer- and Pedometer-Based physical activity interventions among adults with cardiometabolic conditions: a systematic review and meta-analysis. JAMA Netw Open 2019;2:e1912895–e95. 10.1001/jamanetworkopen.2019.12895 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 28.Jensen MT, Treskes RW, Caiani EG, et al. Esc Working group on e-cardiology position paper: use of commercially available wearable technology for heart rate and activity tracking in primary and secondary cardiovascular prevention—in collaboration with the European heart rhythm association, European association of preventive cardiology, association of cardiovascular nursing and allied professionals, patient forum, and the digital health Committee. Eur Heart J 2021;2:49–59. 10.1093/ehjdh/ztab011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Bakel BMA, Bakker EA, de Vries F, et al. Changes in physical activity and sedentary behaviour in cardiovascular disease patients during the COVID-19 Lockdown. Int J Environ Res Public Health 2021;18:11929. 10.3390/ijerph182211929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laddu D, Ma J, Kaar J, et al. Health behavior change programs in primary care and community practices for cardiovascular disease prevention and risk factor management among midlife and older adults: a scientific statement from the American heart association. Circulation 2021;144:e533–49. 10.1161/CIR.0000000000001026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prince SA, Reid RD, Bernick J, et al. Single versus multi-item self-assessment of sedentary behaviour: a comparison with objectively measured sedentary time in nurses. J Sci Med Sport 2018;21:925–9. 10.1016/j.jsams.2018.01.018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2022-001364supp001.pdf (284.5KB, pdf)
bmjsem-2022-001364supp002.pdf (7.7MB, pdf)
bmjsem-2022-001364supp003.pdf (651.5KB, pdf)
bmjsem-2022-001364supp004.pdf (150.8KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Data from the Sedentary Behaviour Intervention as a Personalised Secondary Prevention Strategy randomised clinical trial will be available upon reasonable request via the corresponding author.