Abstract
The 2015 World Health Organization Global Action Plan and other international policy documents have stressed the need for a 'whole of United Nations approach' in addressing antimicrobial resistance (AMR). As several years have passed, the goal of this paper is to take stock of the current role, mandate, and activities of international organisations and other global stakeholders on AMR. Relevant information is identified through a web-based search and a review of policy documents from international organisations. Based on the assessment of 78 organisations, 21 have AMR-specific activities in the broader sense, although for many of these organisations, their involvement is limited in scope, and 36 have AMR-sensitive activities reflecting the wide scope of AMR. An interdisciplinary framework based on six relevant challenges of global collective actions regarding AMR as well as the main functions of international organisations in global governance is used to organise the findings into several ‘clusters’. AMR is not a priority for many international organisations, but some of them can leverage current efforts to tackle AMR while contributing to their core agenda. Overall, a ‘whole of UN approach’ to AMR within the framework of Sustainable Development Goals is critical to move the global governance of AMR forward.
Keywords: infections, diseases, disorders, injuries; health policies and all other topics
WHAT IS ALREADY KNOWN ON THIS TOPIC
Addressing antimicrobial resistance (AMR) requires an integrated approach across sectors as recognised by the One Health approach.
The 2015 WHO Global Action Plan recognises the need for interorganisational collaboration and specifically identify several international organisations that could contribute to address the topic.
WHAT THIS STUDY ADDS
This study found that, in addition to core international organisations such as the WHO, the World Organization for Animal Health, and the Food and Agriculture Organization of the United Nations, several international organisations have activities that specifically address AMR, and many have activities that relate to AMR.
The findings also identify several collaborations between international organisations.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE AND/OR POLICY
As the global governance of AMR is embedded within wider processes of global health governance, the new findings emphasise the relevance of leveraging existing resources, mechanisms and institutions rather than reshuffling the governance of AMR.
A ‘whole of United Nations approach’ in an essentially polycentric governance system provides a realistic approach to address AMR as part of wider efforts towards sustainable development.
Introduction
Antimicrobial resistance (AMR) represents a formidable challenge for global governance. The cross-border transmission of AMR and the transnational nature of several drivers of antimicrobial use imply that no country can solve the problem on its own. International collaboration including bilateral and multilateral efforts is thus critical to successfully address AMR. In addition, the determinants of AMR are both social and ecological, therefore extending beyond the health sector; they are also related to sustainable development.1 In 2015, the World Health O adopted a Global Action Plan on AMR (WHO GAP AMR).2 This was followed by similar documents by the World Organization for Animal Health (OIE) and the Food and Agriculture Organization of the United Nations (FAO).3 4 In 2016, a political declaration was adopted by Heads of States at the United Nations General Assembly (UNGA).5
The adoption of these soft law instruments marked renewed efforts in terms of increasing the profile of AMR on the global political agenda and addressing AMR from an integrated perspective. Such vision was already present in the 2001 Global Strategy for the containment of AMR.6 However, the 2015 WHO GAP AMR expanded this thinking by framing AMR as a ‘One Health’ issue that cannot be addressed within one sector but requires an ‘all-out effort’ and ‘whole-of-society engagement’.2 The 2015 WHO GAP AMR offers recommendations not only for Member States and the WHO Secretariat but also for other partners/stakeholders. At the global level, several recommendations focus on strengthening the Tripartite collaboration between WHO, OIE and FAO, but others cover the role of other international organisations (IOs) including the United Nations Children's Fund (UNICEF), the United Nations Educational, Scientific and Cultural Organization (UNESCO), the World Bank (WB), the United Nations (UN), Organisation for Economic Co-operation and Development (OECD) and the Codex Alimentarius Commission (CAC).
More than 5 years after the adoption of the 2015 WHO GAP AMR and the subsequent political declaration at the UNGA, it is time to take stock of the progress accomplished in implementing the vision of a 'whole of UN approach' on AMR. In this article, we assess the contribution of different IOs which are part of or related to the UN system to address AMR with a focus on activities undertaken since the 2010s and more specifically in the wake of the adoption of the 2015 WHO GAP AMR. This aligns well with the waves of attention found by Overton et al.7 This assessment is based on an online collection of relevant sources. We report about the level of involvement of IOs in the global governance of AMR and organise these findings in several broad clusters to address AMR. Based on our findings, we discuss the pros and cons about expanding participation of IOs in AMR. We evaluate the potential future involvement of IOs and other global health stakeholders regarding AMR.
Methods
Patient and public involvement
This study is based on online search of publicly available webpages and documents. No patients or members of the public were involved in the design of the study.
Selection of IOs
The UN system, which comprises the UN and several related organisations, is the largest intergovernmental organisation in the world. To select organisations, we used the UN system chart (https://www.un.org/en/pdfs/18-00159e_un_system_chart_17x11_4c_en_web.pdf). From this chart, we extracted the name of 105 organisations and entities in an Excel sheet. We included 78 organisations in the analysis including the 5 principal organs of the UN, the 15 specialised agencies (ie, autonomous organisations whose work is coordinated through Economic and Social Council (ECOSOC) and Chief Executive Board (CEB)), 23 department and offices of secretariat, 11 funds and programmes, 8 related organisations linked to the UNGA or the Security Council, 6 research and training organisations related to ECOSOC and/or the UNGA, 2 subsidiary organs, 6 ‘other entities/bodies’ and 1 mechanism for interorganisational collaboration (CEB). Furthermore, we added manually OIE which is not part of the UN system but is a member of the Tripartite. Because they are already represented by the main organs mentioned above, the subsidiary organs of the Security Council and the UNGA, the functional commissions and other bodies of ECOSOC, and the seven Regional Commissions of ECOSOC/Security Council were not considered for this analysis (some of these bodies are covered in online supplemental material 1). In addition, some other non-UN organisations were assessed but were not integrated in the main analysis (see online supplemental material 2).
bmjgh-2021-008181supp001.pdf (379.4KB, pdf)
Identification of activities
To identify IOs’ activities on AMR, we conducted an online search with AMR and derivatives (eg, antibiotic resistance, antimicrobial resistance, resistant infections) and the name of the IO as the main keywords. As the focus of this article is on the global level, we limited our search to websites associated with global headquarters of each organisation. In addition, we browsed the websites of the relevant organisations to search for activities on AMR. In addition to written information directly available from websites, we downloaded the documents directly linked to the pages we visited. We qualitatively analysed these documents which encompass a wide range of sources such as policy and technical reports, normative guidance (eg, resolutions, action plan, strategy, etc), procedural documents (eg, agenda and meeting reports) with the software ATLAS.ti V.9 (Windows version) for relevant content on AMR activities (cf. the paragraphs below for the categories used). During the analysis, further documents were identified and collected through a snowball approach. In total, we collected 566 documents published by IOs on AMR from 1949 to March 2022 (a list of all documents considered for this analysis is available as a online supplemental material 3). While the core information used in this study was directly extracted from websites and recent documents, the broader information collected from the database of documents provided relevant information about the context of organisations’ engagement in addressing AMR.
We distinguished between activities that are specific to tackle AMR and those that may influence AMR.8 These ‘AMR-sensitive’ activities such as the use of vaccines are not designed to tackle AMR directly but can contribute to address some aspects of the challenge. Because AMR touches on many different sectors, virtually all organisations of the UN system can have AMR-sensitive activities. For example, poverty and security might be upstream drivers of AMR. For this article, we included only AMR-sensitive activities that are related to AMR in terms of six challenges of global collective action. However, to identify organisations that might contribute to tackle AMR through specific and actionable entry points, we assessed the mandate and activities of these organisations in the health, agriculture/food and environmental sectors, all of which are important dimensions of AMR.9 We looked for these activities by searching the name of the organisation and relevant keywords regarding the above-mentioned areas (eg, infectious diseases, malaria, tuberculosis (TB), HIV-AIDS) and by understanding how this relates to the main policy priorities regarding AMR. A summary of activities was created for each organisation.
Analytical framework
To help assess an organisation’s role in tackling AMR, we built a multidimensional framework. First, we drew on the literature to identify six challenges of global collective action regarding AMR.10 11 Accordingly, AMR is not only an issue of classic strategies to tackle infectious diseases, that is, surveillance, prevention, containment, innovation, but also of conservation of a natural resource like several environmental challenges and of access to health technologies (cf. box 1 for definition of these challenges of global collective action). Second, governance covers several functions. Based on the literature in international relations, we distinguished between different types of functions of IOs and other stakeholders in global governance (cf. box 2 for definition of these functions). Third, we defined several sectors that are relevant to address AMR including human health, agriculture, food production and the environment. Fourth, as AMR is pervasive regarding infectious diseases, but with highly variable scope and impact, we included activities to tackle AMR in specific diseases such as HIV-AIDS, malaria and TB in addition to common bacterial, viral and fungal infections. Fifth, we considered the population that can be targeted by different organisations (eg, children, migrants). Taken together, these five dimensions define a framework for evaluation of stakeholders’ action on AMR.
Box 1. Challenges of global collective action related to AMR.
As addressing AMR requires global collective action, evaluating the mandate and activities of IOs requires understanding of strategic approaches and main policy goals. There have been several international policy frameworks to tackle AMR including a comprehensive WHO global strategy for the containment of AMR published in 2001.6 Renewed efforts resulted in the adoption by WHO Member States of the 2015 WHO GAP AMR. The GAP has been legitimised by the UNGA as the main instrument for guiding approaches for tackling AMR. FAO and OIE have published their own action plan based on the 2015 WHO GAP AMR.3 4 IACG-AMR has developed its own framework.50 Based on the literature, one can identify six areas/challenges of global collective action regarding AMR.51 The first is infection prevention which aims to limit infectious diseases in the first place. Relevant interventions include immunisation, sanitation, hygiene as well as infection prevention in healthcare settings. The second corresponds to all surveillance activities related to AMR (human health, animal health and the environment) and antimicrobial use to inform actions based on evidence. The third is conservation of antimicrobial effectiveness that aims to lower selective pressure and in turn reduces the emergence of AMR. This challenge mainly relates to interventions that target overuse and misuse of antibiotics and also limit antibiotic pollution in the environment. As transmission of AMR is an important factor driving the problem,52 the fourth challenge is about containing the different pathways of dissemination of AMR once it has emerged. The fifth is strengthening access to health including but not limited to access to drugs as inequalities are one of the most central challenges regarding AMR policy and global health.53 Strengthening access to health can help not only to reduce the burden of infectious diseases but also improve how we use antibiotics. Finally, a sixth challenge of global collective action is innovation which designates all interventions and policies to support the development of health technologies with the direct goal to address AMR.
AMR, antimicrobial resistance; FAO, Food and Agriculture Organization; GAP, Global Action Plan; IACG, Interagency Coordination Group; IOs, international organisations; OIE, World Organization for Animal Health; UNGA, United Nations General Assembly.
Box 2. Functions of IOs and other global health actors.
The IACG-AMR framework identified five levers (eg, awareness and capability building, measurement/surveillance, funding and financial incentives, policy and regulations, championing and piloting)50 while the 2015 WHO GAP AMR does not cover specifically these areas. Based on the academic literature on the functions of IOs, we propose six core functions that form a continuum from purely technical support to countries to more policy-oriented and normative activities.54 55
Knowledge synthesis
IOs often act as a knowledge broker which means that they seek to harness scientific research not only to produce evidence-informed policies, but also to legitimise policy choices, depoliticise action and ensure their institutional survival.56 While the role of IOs in knowledge brokering predominantly involves the synthesis of existing knowledge and the classification of information,57 it also involves the collection and production of new scientific data.58 IOs also create and/or endorse new concepts that are then disseminated in the international community.59 A good example is the coining of the concept of sustainable development by the World Commission on Environment and Development.
Normative and political forum
One of the core functions of IOs is normative.60 This function is facilitated by their unique power for convening people and for providing a forum for negotiations among states. IOs are involved in all steps of the norm cycle: emergence, crystallisation and diffusion of norms.61 The UN system plays a key role in the codification of norms.62 Normative activities in IOs range from the creation of shared technical standards to the making of international law. As IOs have an authoritative role, they are also involved in the formulation of solutions to tackle international challenges.63
Advocacy, awareness raising and capacity building
IOs are often involved in raising awareness about some problems that states are not aware of or insufficiently addressing. The focus here is on the diffusion and dissemination of information rather than the production of new knowledge. When common rules and policies are agreed at the international level, IOs can also play a key role in advocating change to their constituencies either by highlighting best practices or by providing technical guidance to support countries’ implementation. Their capacity to draw on a vast expertise is often call upon to build capacities in countries. This is especially important in LMICs where capacities are often lacking to implement agreed policies. Some IOs specialise in training and capacity building (eg, UNITAR) and many IOs propose training activities.
Funding, procurement and delivery
Some IOs have mechanisms for project funding and delivery. For example, ‘on average, WHO buys approximately US$700 million worth of goods and services every year to maintain operations in the field and to react to upcoming and recurring demands’.64 Funding and procurement activities from IOs and related organisations can be used to advocate changes and orient policies. A relevant example is the structural adjustment programmes conducted by the International Monetary Fund and the World Bank.65
Oversight, monitoring and evaluation
Another function of IOs is to monitor and oversee the implementation of any agreement or shared policies. Monitoring and evaluation are essential to diffuse best practices, to promote learning and to benchmark countries’ performance while oversight is key to foster compliance. Several mechanisms are possible from peer review to self-reporting, to technical experts.66 In some cases, IOs play a key role in devising the oversight instrument through survey/questionnaire and/or in conducting on-site evaluation. A classic example is evaluation conducted by the International Atomic Energy Agency.
Coordination/interplay management
An important function of IOs is to coordinate work across different areas. Traditionally, IOs’ coordination mandate has revolved around specific issues. A good example is the UN Office for the Coordination of Humanitarian Affairs which was created to improve the coordination between several humanitarian actors. In addition, some organs of the UN (eg, ECOSOC, UNGA) have a broader coordination mandate. With the growing interdependence between sectors, a growing coordination role is about the management of interplay between different sectors to improve policy coherence within the context of ‘whole of UN system’ response expressed by the Sustainable Development Goals.67 Organisations that are representative of diverse groups are important.68
AMR, antimicrobial resistance; ECOSOC, Economic and Social Council; GAP, Global Action Plan; IACG, Interagency Coordination Group; IOs, international organisations; LMICs, low/middle-income countries; UN, United Nations; UNGA, United Nations General Assembly; UNITAR, United Nations Institute for Training and Research.
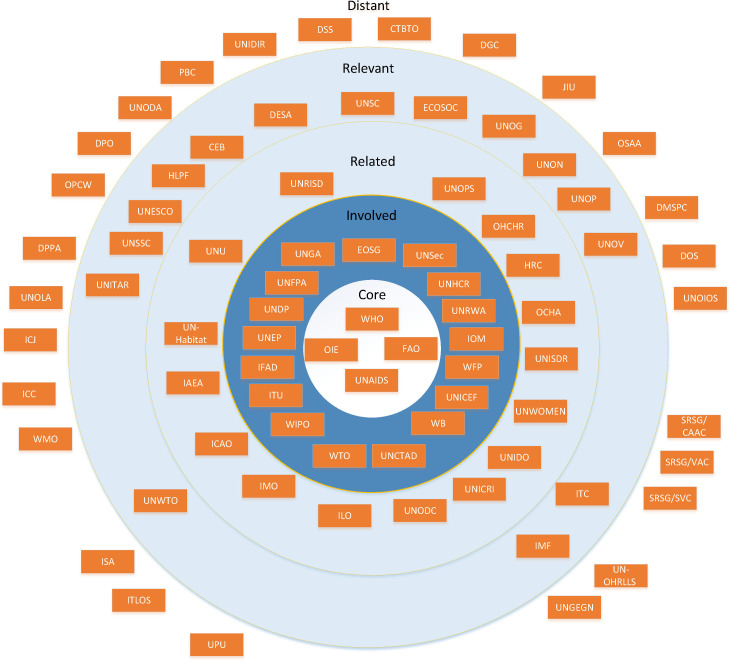
To classify the involvement of IOs in the global governance of AMR, we defined five categories from core to distant organisations. Core organisations have received a mandate on AMR from their Member States. This mandate is associated with both AMR-specific and AMR-sensitive activities. Core organisations have a large scope of activities regarding several of the five parameters above. Involved organisations do not necessarily have a mandate on AMR. However, they have some AMR-specific activities and may also have AMR-sensitive activities. Related organisations have only AMR-sensitive activities which can be related to the six challenges of global collective actions defined above. Relevant organisations have no mandate on AMR but have usually more distant AMR-sensitive activities in areas such as sustainable development, training and coordination. Finally, some organisations are distant as their mandate, priorities and activities are currently far removed from AMR.
Results
Overall results
From the analysis conducted between January and September 2018 and updated in autumn 2021 on 78 international organisations, 21 organisations have AMR-specific activities in the broader sense, although for many of these organisations, their involvement is limited in scope, and 36 have AMR-sensitive activities reflecting the wide scope of AMR (the results based on the identification of relevant AMR activities are summarised in online supplemental material 4). A limited number of organisations have received a direct mandate on AMR from their Member States (WHO, OIE, FAO, the Joint United Nations Programme on HIV/AIDS (UNAIDS)) and more recently the United Nations Environment Programme (UNEP). Among these organisations, we identified WHO, OIE, FAO and UNAIDS as core organisations because they are active on several challenges of global collective action and exert multiple functions in the global governance of AMR. WHO is the main organisation in human health but also develops activities on food safety. OIE is the main organisation in animal health and FAO has an important role regarding AMR in food-producing animals and food systems. UNAIDS’s activities on AMR relate to planning, advocacy, communication and capacity building in HIV-AIDS.
Involved organisations on AMR encompass 17 organisations that have had AMR-specific activities and, for some of them, AMR-sensitive activities. The United Nations Population Fund (UNFPA), the only one which has a primary health mandate, works on infection prevention, access and conservation of antimicrobials mainly in maternal health and HIV-AIDS. UNEP has recently become involved in tackling AMR in the environment. Beyond One Health, finance, trade and intellectual property organisations have been involved to some extent in tackling AMR. These include the WB, the United Nations Conference on Trade and Development (UNCTAD), the World Trade Organization (WTO) and the World Intellectual Property Organization (WIPO). Another relevant area is migration and refugees where the International Organization for Migration (IOM), the United Nations High Commissioner for Refugees (UNHCR), and the United Nations Relief and Works Agency for Palestine Refugees in the Near East (UNRWA) have had AMR-specific activities.
Most organisations in the category ‘involved’ are active in specific challenges of global collective action and/or functions of global governance and/or specific countries/populations. For example, the WB is not only interested in AMR in low/middle-income countries (LMICs) but also covers the economic aspect of AMR. The United Nations Development Programme and UNICEF are involved in access to antimicrobials. This suggests that involved organisations can address important drivers of AMR, but they do so in a way that are generally restricted to one or a few dimensions of the issue (eg, focus on a specific disease or population, functions or limited to one challenge of global collective action). In most cases, we found that IOs work at the project or programme levels without a mandate from their Member States. In some cases, they collaborate directly with an organisation that has a core mandate on AMR. This is for example the case of the International Telecommunication Union with WHO.
Among the 78 organisations assessed, 16 are currently ‘related’. While they have a mandate in different areas including human rights such as the Human Rights Council and the Office of the United Nations High Commissioner for Human Rights, development such as the United Nations Industrial Development Organization (UNIDO) and the United Nations Research Institute for Social Development (UNRISD) or crime such as the United Nations Interregional Crime and Justice Research Institute (UNICRI) and the United Nations Office on Drugs and Crime, they undertake AMR-sensitive activities related to the six challenges of global collective action. Most of them have activities in infection prevention such as immunisation, sanitation, and hygiene and in access to medicines. We identified 15 organisations in the category ‘relevant’. Their mandate includes economic and social development such as the United Nations Department of Economic and Social Affairs and the ECOSOC, education and training, such as UNESCO and the United Nations System Staff College, security such as the United Nations Security Council, or coordination such as the CEB. Lastly, 26 of the 78 organisations assessed are most likely distant from AMR. A quarter of them have a mandate in security, while others have their mandate in different areas such as marine affairs and internal management.
Finally, our analysis of the result led us to identify several mechanisms for intersectoral collaboration between (1) human health, animal health, agriculture and food; (2) human/animal health, food and trade; and (3) public health, intellectual property and trade. The roles of these mechanisms in addressing AMR are summarised in table 1. Some of these mechanisms such as the CAC are old. For several mechanisms, AMR is only part of their mandate. Other mechanisms such as WHO Advisory Group on Integrated Surveillance of Antimicrobial Resistance (AGISAR) were created specifically to address AMR. WHO is engaged in most of these mechanisms for intersectoral collaboration. Overall, the main areas of collaboration within these mechanisms are surveillance, conservation and infection prevention. These mechanisms are mainly dedicated to the management of interplay regarding knowledge synthesis and norms, and, to a lesser extent, policies including support to the development and implementation of national action plans and monitoring and evaluation.
Table 1.
Mechanisms for intersectoral collaboration
| Acronym of the organisation | Main mandate |
| Human health, animal health, agriculture and food | |
| CAC (FAO and WHO) |
The CAC adopts guidelines and standards regarding the conservation of antimicrobials and the containment of AMR in food products and animal husbandry.20 The main standards on AMR are the 1993 ‘International Code of Practice for Control of the Use of Veterinary Drugs’,69 the 2005 ‘Code of Practice to Minimize and Contain Antimicrobial Resistance’,70 and the 2011 ‘Guidelines for Risk Analysis of Foodborne AMR’.71 These standards are recognised by the Sanitary and Phytosanitary (SPS) Agreement at the WTO. While collaboration was mainly between WHO and FAO through the CAC, OIE was also included in the discussion. The work has been conducted by the ‘Ad hoc Codex Intergovernmental Task Force on AMR’ from 2007 to 2011 and since 2017. |
| Tripartite collaboration 2010 (FAO, OIE and WHO) |
The Tripartite FAO/OIE/WHO Collaboration was created in 2010 and entails a common recognition of the role and functions of each organisation. For example, the standards published for terrestrial and aquatic animals are recognised by WHO.43 Efforts have been done towards better integration between the IHR and PVS instruments, regarding the assessment of national capacities to detect and respond to global health threats.72 In recent years, AMR has become one of the main areas for action of the Tripartite. In 2017, the FAO/OIE/WHO Tripartite Collaboration on AMR renewed their commitment to work together.73In 2019, the Tripartite established a standing Tripartite Joint Secretariat with special governance arrangements. |
| AGISAR (WHO) |
The WHO AGISAR is an expert-based intersectoral AMR-specific mechanism that mainly addresses AMR in food-producing animals. The mission of AGISAR is to support WHO’s effort ‘to minimise the public health impact of AMR associated with the use of antimicrobial agents in all food-producing animals’.74 AGISAR covers surveillance but is also responsible for some aspect of conservation, for example, by establishing the list of critically important antimicrobials. |
| INFOSAN (WHO and FAO) |
Created in 2005 by FAO and WHO, the INFOSAN shares food safety information between human and animal health sectors. INFOSAN has reported on AMR. |
| Human/animal health, food and trade | |
| SPS Agreement (WTO) |
The need to manage the interface between trade and animal health resulted in the adoption of an agreement in 1998 ‘to act in collaboration and to consult each other on questions of mutual interest, in particular those concerning the sanitary aspect of international trade in animals and products of animal origin and zoonoses’.75 The standards adopted by OIE, FAO and the CAC are non-binding but ‘are specifically identified in the WTO Agreement on the Application of Sanitary and Phytosanitary Measures as the international benchmark texts for food’.76 There is no specific mechanism for AMR, but FAO and WTO prepared a joint publication on ‘Trade and food standards’ in which AMR is briefly mentioned.77 |
| Public health, intellectual property and trade | |
| Trilateral Cooperation on Public Health, Intellectual Property and Trade (WHO, WIPO and WTO) |
WHO has a health mandate regarding both access and innovation, which are situated at the interface between the human rights and intellectual property regimes. Following the adoption of the ‘Global Strategy and Plan of Action on Public Health, Innovation and Intellectual Property’, WHO, WTO and the WIPO created the ‘Trilateral Cooperation on Public Health, Intellectual Property and Trade’.25 The topic of AMR has been covered during a technical symposium held in 2016.78 The scope of formal participation remains limited as the WTO Secretariat participates ‘as observers in the WHO Intergovernmental Working Group on Public Health, Innovation and Intellectual Property and in the WHO’s International Medical Products Anti-Counterfeiting Task Force (IMPACT), as well as in the field of technical cooperation’.79 |
| Overall coordination mechanism | |
| IACG-AMR (Convened by the UN Secretariat) |
The adoption of the 2016 Political Declaration by the UNGA led to the creation of the ad hoc IACG-AMR to provide advice on how to make the global AMR agenda move forward.5 IACG-AMR, which is co-chaired by WHO and the UN Secretariat, has a broad membership of IOs and other global health actors. Four objectives have been laid out in its working plan for 2017–2019 and the work has been divided in six subgroups.80 In 2017 and 2018, IACG-AMR commissioned works in several areas and produced its own framework of action which put emphasis on innovation. The final recommendation of IACG-AMR stressed the need for countries’ progress, collaboration, sustainable response and innovation, and mechanisms for global governance (eg, the creation of a Global Leaders Group on Antimicrobial Resistance and an Independent Panel on Evidence for Action Against Antimicrobial Resistance).81 |
| Global framework (WHO, FAO and OIE) |
Following the adoption of WHO Resolution WHA 68.7, and further supported by the 2016 UNGA Political Declaration, an ongoing effort by the FAO/OIE/WHO Tripartite Collaboration on AMR to design an overarching intersectoral mechanism to tackle AMR is the ‘global development and stewardship framework’.76 As the framework aims to balance innovation, access and conservation, ‘[it] is envisaged to form an ‘umbrella’ uniting different instruments’,76 but its legal form still needs to be defined. Several rounds of consultations have been organised with Member States, but it is yet unclear whether this initiative has so far garnered enough support to move to the WHA. |
AGISAR, Advisory Group on Integrated Surveillance of Antimicrobial Resistance; AMR, antimicrobial resistance; CAC, Codex Alimentarius Commission; FAO, Food and Agriculture Organization; IACG, Interagency Coordination Group; IHR, International Health Regulations; INFOSAN, International Food Safety Authorities Network; IOs, international organisations; OIE, World Organization for Animal Health; PVS, Performance of Veterinary Services; UN, United Nations; UNGA, United Nations General Assembly; WHA, World Health Assembly; WIPO, World Intellectual Property Organization; WTO, World Trade Organization.
Results in the six challenges of global collective action
While the findings above provide an overview regarding the work of each organisation or mechanisms for intersectoral organisation, using them in isolation offers limited insights into the global governance of AMR. A relevant approach is thus to understand involvement from these organisations in terms of the six challenges of collective action.
The global responsibility for surveillance of AMR and antimicrobial use is shared between several IOs. In human health, WHO activities on surveillance were already important in the 1960s and again in the 1980s.12 In recent times, WHO set up the Global Antimicrobial Surveillance System in 2015, based on voluntary participation of countries. Several mechanisms are dedicated to pathogens/diseases such as Salmonella spp (‘WHO Global Salm-surv’), Neisseria gonorrhoeae (‘WHO Gonococcal Antimicrobial Surveillance Programme’), malaria (Worldwide Antimalarial Resistance Network) and TB (the Global Project on anti-Tuberculosis drug resistance surveillance). The responsibility for addressing global surveillance of drug resistance in HIV is shared between WHO (‘WHO HIVresnet’) and UNAIDS. Regarding antimicrobial use, WHO has issued technical guidance on surveillance for a long time, but there is currently no global mechanism to monitor antimicrobial use. In animal health and agriculture, OIE and FAO are responsible for global surveillance with activities since the 1960s. OIE has set up an ad hoc group on AMR to develop standards on surveillance and support the collection of data in Member States. FAO created an Assessment Tool for Laboratory and AMR Surveillance Systems, the goal of which is to evaluate surveillance capacities regarding AMR. For a long time, WHO has also been involved in surveillance of AMR in animal health and set up AGISAR in 2008. AGISAR has supported the development of standards regarding the surveillance of AMR but also maintained a list of critically important antimicrobials in human health. In animal health, there is currently no established global surveillance mechanism. In terms of antimicrobial use, activities have been initiated by OIE which collects data on a yearly basis. Finally, there is currently a gap in terms of the surveillance of AMR in the environment.13 Scientific studies are currently the main source of data for environmental surveillance.
Covered by the third objective of the 2015 WHO GAP AMR and relevant for both human and animal health, infection prevention is primarily about AMR-sensitive activities. A variety of activities and collaborations are relevant to AMR including on water sanitation, immunisation, patient safety and biosecurity. In human health, WHO is the main organisation responsible for infection prevention with a dedicated unit and the support of several WHO collaborating centres. In the healthcare setting, the single most effective and inexpensive intervention is hand hygiene, which has been supported by the WHO hand hygiene campaign and other initiatives. There are also targeted activities regarding specific diseases in the community as infection prevention is the basis of public health.14 For example, UNFPA is mainly active on AMR with regard to HIV infection and maternal health. Some organisations are active in infection prevention in specific contexts such as humanitarian crises (United Nations Office for the Coordination of Humanitarian Affairs), maternal health (UN-Women), refugees (UNHCR) or in relation to work activities (International Labour Organization). Other relevant organisations include those active in increasing immunisation such as UNICEF with longstanding collaborations between WHO and UNICEF to improve immunisation coverage in LMICs. UNICEF and UN-Water are the main organisations dedicated to improving sanitation with dedicated programmes in LMICs. UN-Habitat also focuses on infection prevention by working on sanitation, water and urban health. Other organisations are active in infection prevention issues through research and policy analysis (UNRISD) and training (United Nations University). In animal health, core institutions include those with a direct agriculture/animal health mandate (OIE, FAO). However, WHO is also involved in food safety. The CAC, an interorganisational collaboration between FAO/WHO, focuses on internationally recognised food standards. Finally, the WTO rules that govern the standards that are compatible with international trade of animal and food products also impact infection prevention (eg, the agreement on the Application of Sanitary and Phytosanitary Measures (SPS Agreement)).
Conservation corresponds to the fourth objective of the 2015 WHO GAP AMR and combines educational and regulatory strategies to optimise the use of antimicrobials. In human health, WHO provides guidance about the best practices for the rational use of drugs including antimicrobial stewardship. UNAIDS has similar functions for addressing drug resistance in HIV. WHO also raises awareness about AMR including through the provision of education material and the World Antibiotic Awareness Week. AGISAR performed repeated assessments of critically important antimicrobials for human medicine. In 2019, WHO further released a categorisation of antibiotics as access, watch and reserve to maximise their good use.15 In animal health and agriculture, the mandate on conservation is shared between FAO and OIE. OIE set standards through the terrestrial and aquatic animal health codes. With no global mechanism for conservation, OIE reported that 35 countries are allowing antibiotics for growth promotion in 2018.16 WHO has also been involved in non-human use of antimicrobials including regarding foodborne pathogens since the end of the 1990s. WHO collaborates with FAO through the CAC since the 1960s. Several organisations have been involved in some activities related to conservation of antimicrobial effectiveness including UNFPA on TB and HIV, UNICEF in children, UNHCR and UNRWA in refugees. Furthermore, some activities to reduce the issue of counterfeit medicines from UNICRI and United Nations Office for Project Services are indirectly related to the conservation of antimicrobial effectiveness.
Against the backdrop of globalisation, international dissemination of AMR is an externality of travel and trade.17 Issues related to the containment of AMR are not well developed in recent global policy documents and we found limited activities related to containment. In human health, WHO has issued guidelines for control of some highly drug-resistant bacteria such as carbapenem-resistant Enterobacteriaceae,18 and specific diseases such as HIV-AIDS, malaria and TB.10 11 In addition, it has been argued that the broad scope of the International Health Regulations encompasses AMR, but guidance regarding their applicability has been limited.19 In animal health and food production, some guidelines have been issued by FAO and OIE. Furthermore, any restriction on international trade is governed by the SPS Agreement at WTO which regulates the rules and processes that countries need to respect when adopting standards that might represent barriers to trade. Countries’ policies to restrict imports of products contaminated with AMR appear to have been limited.20 A few activities from the International Civil Aviation Organization and the International Maritime Organization are relevant to the containment of AMR.
The main actors classically dedicated to innovation including research and development of new drugs and other relevant technologies are multinational companies. Given the market failures regarding the development of novel antibiotics,21 22 innovation for technologies to tackle AMR has received growing attention in global governance since the mid-2000s. There has been more emphasis regarding human health than animal health as the latter area is seen as more profitable for pharmaceutical companies. Innovation is well represented in the 2015 WHO GAP AMR (objective 5). Several organisations contribute to this objective at the global level. In 2011, WHO created the ‘Consultative Expert Working Group on Research and Development: Financing and Coordination’ that evaluated innovative approaches to incentivise further the development of new health technologies. This led to the creation of the Global Observatory on Health R&D. In 2017, WHO also issued a list of priority pathogens for the development of new antibiotics.23 Against the background of the development of product development partnerships and several initiatives on AMR, a Global Antibiotic Research & Development Partnership was created in 2016 to address the innovation gap in AMR.24 As intellectual property has been the main mechanism to reward the research and development of new technologies, both WTO and WIPO have an upstream influence on research and development of technologies for AMR. The topic has been discussed within the Trilateral cooperation on public health, intellectual property and trade.25
WHO has historically been the main IO dealing with access to health. Its programme on essential medicines started in 1977.26 Both objectives 4 and 5 of the 2015 WHO GAP AMR cover aspects related to access to medicines. Several global stakeholders contribute to access to medicines with mainly AMR-sensitive activities. While WIPO is responsible for intellectual property, the most important international agreement regarding access is the Agreement on Trade-Related Aspects of Intellectual Property Rights (TRIPS) at WTO. The current regime allows for some flexibilities (eg, compulsory licensing) for drugs of public health importance. UNAIDS has advocated access to antiviral drugs against HIV-AIDS since its creation in 1996. Since 2010, interorganisational collaborations have taken place between WHO, WTO and WIPO under the ‘Trilateral cooperation on public health and intellectual property’ but have not led to the establishment of a specific international mechanism dedicated to improving access to antimicrobials. Other relevant AMR-specific activities to facilitate access have been undertaken at the programme/project level by UNCTAD, UNHCR and UNICEF for specific populations. Finally, the Human Rights Council and UNIDO have activities on access to medicines that indirectly relate to AMR. In 2015, the UN Secretary-General convened a ‘High Level Panel on access to medicine’. In its final report published in 2016, the Panel reiterated the importance of the flexibilities within the TRIPS agreement,27 as did the 2018 UNGA political declaration on TB.28
Discussion
Our assessment provides insights about past and current efforts of IOs to tackle AMR with a focus on activities conducted since the 2010s. First, it suggests that addressing a complex issue such as AMR is shaped by different international actors. While there is a core of IOs with a myriad of activities on AMR, several IOs without a formal mandate on AMR are also contributing to address the challenge, although the respective impact of different regimes on AMR is poorly understood (figure 1 summarises the current levels of involvement from IOs on AMR). Second, despite the call from WHO and the UNGA to expand participation in the global governance of AMR, our assessment reveals a mixed picture. On the one hand, several activities were undertaken over the past years and several IOs have become involved on AMR. The WB and UNEP are the best examples. On the other hand, the level of involvement of other IOs remains often limited to the project level. While the environment is a critical dimension to AMR, it remains under-represented in the global governance of AMR.7 A possible explanation for the growing but still limited involvement of UNEP is that it is faced with several other pressing global challenges. Overall, this suggests a certain amount of ‘output effectiveness’ in current effort to govern AMR. While the goal of this article is not primarily to measure the impact of the current governance system, it appears that the current governance system has managed to raise awareness about AMR and made progress to address several challenges of collective action (eg, surveillance and conservation) and several governance functions (eg, monitoring and evaluation).29
Figure 1.
Current levels of IOs’ involvement on tackling AMR. AMR, antimicrobial resistance; CAAC, Children and Armed Conflict; CEB, Chief Executive Board; CTBTO, Comprehensive Nuclear-Test-Ban Treaty Organization; DESA, Department of Economic and Social Affairs; DGC, United Nations Department of Global Communications; DPPA, United Nations Department of Political Affairs; EOSG, Executive Office of the Secretary-General; DMSPC, Department of Management Strategy, Policy and Compliance; DOS, Department of Operational Support; DPO, Department of Peacekeeping Operations; ECOSOC, Economic and Social Council; FAO, Food and Agriculture Organization; HLPF, High-Level Political Forum on sustainable development; HRC, Human Rights Council; ICAO, International Civil Aviation Organization; IAEA, International Atomic Energy Agency; ICC, International Criminal Court, ICJ, International Court of Justice; IFAD, International Fund for Agricultural Development; ILO, International Labour Organization; IMF, International Monetary Fund; IMO, International Maritime Organization; IOM, International Organization for Migration; ITC, International Trade Center; ITLOS, International Tribunal for the Law of the Sea; ITU, International Telecommunication Union; ISA, International Seabed Authority; JIU, Joint Inspection Unit; OCHA, Office for the Coordination of Humanitarian Affairs; OHCHR, Office of the United Nations High Commissioner for Human Rights; OHRLLS, United Nations Office of the High Representative for the Least Developed Countries, Landlocked Developing Countries and Small Island Developing States OIE, World Organization for Animal Health; OPCW, Organisation for the Prohibition of Chemical Weapons; OSAA, Office of the Special Adviser on Africa; PBC, Peacebuilding Commission; SRSG, Special Representative of the Secretary-General; SVC, Sexual Violence in Conflict; UNAIDS, Joint United Nations Programme on HIV/AIDS; UNCTAD, United Nations Conference on Trade and Development; UNDP, United Nations Development Programme; UNDSS, United Nations Department for Safety and Security; UNEP, United Nations Environment Programme; UNFPA, United Nations Population Fund; UNGA, United Nations General Assembly; UNGEGN, United Nations Group of Experts on Geographical Names; UNHCR, United Nations High Commissioner for Refugees; UNICRI, United Nations Interregional Crime and Justice Research Institute; UNIDIR, United Nations Institute for Disarmament Research; UNIDO, United Nations Industrial Development Organization; UNISDR, United Nations Office for Disaster Risk Reduction; UNITAR, United Nations Institute for Training and Research; UNODA, United Nations Office for Disarmament Affairs; UNODC, United Nations Office on Drugs and Crime; UNOG, United Nations Office at Geneva; UNOIOS, United Nations Office of Internal Oversight Services; UNOLA, United Nations Office of Legal Affairs; UNOP, United Nations Office for Partnerships; UNOPS, United Nations Office for Project Services; UNOV, United Nations Office at Vienna; UPU, Universal Postal Union; UNRISD, United Nations Research Institute for Social Development; UNRWA, United Nations Relief and Works Agency for Palestine Refugees in the Near East; UNSC, United Nations Security Council; UNSec, United Nations Secretariat; UNSSC, United Nations System Staff College; UNU, United Nations University; UNWTO, World Tourism Organization; VAC, Violence against Children WB, World Bank; WFP, World Food Programme; WIPO, World Intellectual Property Organization; WMO, World Meteorological Organization; WTO, World Trade Organization.
Several factors may explain the current situation. From a formal perspective, an important obstacle is that most IOs have not received a formal mandate from their Member States in the respective organisation. So, the lack of engagement primarily reflects the weak will of States, and the current subeffective organisation of the international system when it comes to addressing complex challenges such as AMR. Moreover, the current situation stresses the discrepancy between engagement at the UNGA by Head of States and further engagement in different organisations by ministries. This problem of policy coherence is hampering collective action on AMR.30 Insights on the international policy process suggests that several other factors might play a role in whether an issue get addressed or not by the international community. Getting stakeholders involved require making the issue tractable and actionable.31 32 For example, there is ongoing discussion in the literature about the relevance of developing environmental surveillance of AMR.33 Given the existence of multiple pressing global issues and the competition for attention and resources, one must demonstrate that addressing AMR will reinforce issues that are central to the mandate of organisations whose primary mandate is not AMR.34 For example, organisations working on specific diseases are more likely to provide expertise and logistical support to support broader AMR activities in LMICs (eg, resistance testing for extensively drug-resistant (XDR) TB in remote areas), if these activities do not lead to a reduction of support to their core mandate. More attention is thus needed on the issue of co-benefits to show how AMR can strengthen the core mandate of other organisations.35
Addressing several challenges regarding AMR depends to various extent on the capacity of organisations with different and sometimes conflicting mandate to collaborate. While this stresses the importance of interorganisational collaboration to address AMR,36 37 current efforts take place within ‘a history of heterogeneous, often uncoordinated, and at times conflicting reform efforts, whose legacies remain apparent today’.38 The WHO Secretariat frequently reports to the World Health Assembly about its collaboration within the UN system and with other intergovernmental organisations.39 In addition, specific mechanisms ranging from soft to hard law (eg, an international treaty) are needed in specific areas as it has been discussed in the literature.40–42 While collaboration between human and animal health is not new as illustrated by the CAC, the framing of AMR as a One Health issue in the 2015 WHO GAP AMR has supported collaboration between human, animal and environmental health.43 44 Collaboration ranges from sharing information to avoid surprise, to raising awareness and finally to sharing of resources and decision-making power.45 Moreover, the creation of a Tripartite Joint Secretariat on Antimicrobial Resistance in 2019 signals an impetus to move to joint management of priorities and decision-making. Finally, interorganisational collaboration extends beyond the UN system as demonstrated with Global Antibiotic Research and Development Partnership and other public–private partnerships which have a critical role in funding and delivery of essential medicines in LMICs (table 2 provides an assessment regarding several global health stakeholders). The engagement with global stakeholders is necessary,46 but raises questions regarding transparency and accountability of governance processes.47 Overall, a better understanding of the resources devoted to intersectoral organisation as well as the practical barrier to collaboration is needed. Past experiences in other issues such as HIV-AIDS, tobacco control or climate change suggest that there are potential benefits and costs (eg, increasing conflict) in using a collaborative approach.
Table 2.
Actors of the global health system and their role on AMR
| Types of actor and examples | Role in the global health system | Role in the global governance of AMR |
|
National governments Bilateral development cooperation agencies; Ministries of Foreign Affairs; Ministries of Health |
Health is primarily a national responsibility; Nation States are the traditional actors in global health. National, and to some extent, international public health depends on Ministries of Health. Donor countries are involved in development assistance for health through their bilateral development cooperation agencies. Recently, as health has gained political prominence as ‘soft’ power, Ministries of Foreign Affairs have been increasingly involved in global health policymaking. | National and subnational governments adopt AMR policies and implement them.6 The responsibility to address AMR usually spans several ministries including health, trade and economy. Since the adoption of the WHO GAP AMR in 2015, national governments have developed national action plans to combat AMR. There is however a gap in implementation. In this regard, national and subnational actors are ultimately the ones that need to be involved and convinced about the need and urgency of implementing AMR policies through a coordinated multisectoral and multilevel approach where authority is increasingly dispersed.49 |
|
Other IOs and mechanisms OECD, ISO, EU, ICRC, TATFAR |
The international system has seen a proliferation of IOs. Among these organisations, some are active at the global level while others work at the regional level (eg, EU which adopted a strategy on global health). | Several non-UN IOs are already involved in tackling AMR. For example, the EU adopted plans on AMR.82 Within the European region, ECDC aggregates data from EU countries on AMR. JPIAMR supports research on AMR. OECD has also published reports on AMR. The International Committee of the Red Cross has been involved in the fight against AMR mainly in conflict areas. TATFAR was created in 2009 to enhance expert transatlantic collaboration on AMR. |
|
Global health initiatives Drugs for Neglected Diseases; Global Fund to Fight AIDS, Tuberculosis, and Malaria; GAVI; Unitaid; GARDP; MPP |
A central innovation in global health governance has been the development of new mechanisms to deliver targeted funding and health technologies in LMICs.83 Global health initiatives are hybrid organisations which mix elements of the private and public sector. They are typically programmes targeted at specific diseases that were created to address major communicable diseases in LMICs. Their number has risen sharply since 2000 with now about 100 organisations active in global health. They take different forms such as a finance mechanism, implementation programme or product development partnership which aims to research and develop new products such as drugs for neglected tropical diseases. These organisations have been endowed with large means and have developed strong expertise in the delivery of health technologies, medications and preventive strategies in LMICs. | Global health initiatives have played a critical role regarding innovation, access to medicines and infection prevention. Organisations such as GAVI have been critical to step immunisation. Regarding access, the main solution has been for HICs to subsidise access to antimicrobials in LMICs through the establishment of funding and procurement organisations (eg, Global Fund or the Medicine Patent Pool, UNITAID). On innovation, several organisations are conducting R&D activities. Recently, efforts have resulted in the creation of GARDP which develops new treatments for drug-resistant infections that pose the most significant threat to health. |
|
Philanthropic organisations Bill and Melinda Gates Foundation, Rockefeller Foundation, Wellcome Trust, Aga Khan Foundation |
Philanthropic organisations have contributed significantly to the increase of funding in global health in the last 20 years. Founded in 2000, the Bill and Melinda Gates Foundation has become a prominent player with total payments of more than US$58.8 billion since inception. With their huge financial means, the largest philanthropies can set priorities and influence the global health agenda. | Philanthropic organisations are contributing to the collaboration between different actors to develop actions and funding programmes against AMR. Through its forums, the World Economic Forum, which included AMR as part of its global risks report, plays a leading role in calling for cooperation between the public and private sectors to develop innovative solutions to combat AMR. |
|
Informal state grouping (quasi-IOs) G7 and G20 |
G7 and G20 are global and informal leadership groups that were primarily created to address financial and macroeconomic issues but have come to cover many pressing issues in global governance. | G8 and G20 have adopted declarations on AMR. These organisations have played a key role in putting AMR on the global political agenda. |
|
Global civil society organisations Care International; Doctors without Borders (Médecins Sans Frontières); OXFAM International; Save the Children; People Health Movement; International Committee of the Red Cross |
Global civil society organisations are non-governmental, non-business organisations or movements that are active across borders. International NGOs have been an important player in global health in implementation programmes as well as in advocacy (eg, the campaign for access to essential medicines by Doctors without Borders, which aims at increasing the availability of drugs in LMICs). Global civil society also encompasses networks such as the People Health Movement, which focuses on health equity and plays a critical role in advocacy and scrutiny of health policy. | Some NGOs have a mandate specifically on AMR while many other NGOs address AMR as part of a wider portfolio of activities on health or humanitarian issues. With a global reach such as Doctors without Borders have been critical in promoting access to medicines as illustrated by the access to medicine campaign which advocates for access to effective drugs for all. |
| Private industry Pharmaceutical companies; biotechnology companies; information and communication companies | The private industry researches, develops and disseminates products such as drugs, diagnostics and technologies through global markets. Some private companies have set up their own foundations and/or participated in public–private partnerships. | To address market failure in the research and development of new drugs, some governments have step up incentives.22 Most research on R&D on new antimicrobials is led by small firms. In addition, big pharmaceutical companies are contributing to global health initiatives and product development partnerships. |
|
Academic institutions and professional associations ReAct |
Academic institutions and networks play an essential role in global health education and research. Professional societies gather members of the same profession such as physicians or nurses and usually set professional standards. In global health, professional societies can enact recommendations for best practices and play a role in global health education. | Academic institutions conduct both fundamental and applied research on AMR including drug discovery, clinical research and wider public health and governance aspects of AMR. Additionally, academic experts contribute to technical meetings from IOs. |
Adapted from ReAct.84
AMR, antimicrobial resistance; ECDC, European Centre for Disease Prevention and Control; EU, European Union; GAP, Global Action Plan; GARDP, Global Antibiotic Research and Development Partnership; GAVI, The Vaccine Alliance; HICs, high-income countries; ICRC, International Committee of the Red Cross; IOs, international organisations; ISO, International Organization for Standardization; JPIAMR, Joint Programming Initiative on Antimicrobial Resistance; LMICs, low/middle-income countries; MPP, Medicine Patent Pool; NGOs, non-governmental organisations; OECD, Organization for Economic Co-operation and Development; R&D, research and development; TATFAR, Transatlantic Taskforce on Antimicrobial Resistance; UN, United Nations.
Our findings contribute to the debate about how to govern AMR globally. Not surprisingly, the analysis of current arrangements for the global governance of AMR reveals that the main responsibilities for addressing AMR fall mainly on a few IOs, whereas several other IOs are involved or simply relate to the governance of AMR. Given their strong mandate on AMR, one can expect that the current core organisations will remain so in the future. However, our assessment suggests several opportunities for further involvement in terms of specific AMR policy goals, functions of IOs, diseases, populations, sectors and regions (these activities are summarised in table 3). We believe that the thematic and functional clusters can further guide institutional involvement in the global governance of AMR. First, organisations within the same cluster do not necessarily all need to be involved or work together. For example, although several UN organisations are specialised in training activities (eg, United Nations Institute for Training and Research, United Nations University, etc), a partnership between the Tripartite and one of those organisations might be sufficient to reach the goal set. Second, organisations can be part of several clusters. This is especially the case of organisations that have a broad mandate on AMR such as WHO. Third, a few organisations such as UNEP might become a core organisation to tackle AMR (Tripartite+). However, the role of most organisations would be limited to some specific aspects of the challenge, functions or populations regarding AMR. Even when limited, involvement can have multiplying effects within a strongly interlinked system.
Table 3.
Opportunities for further development of the global governance of AMR based on clusters of competencies and functions
| Cluster of relevant organisations | Addressing gaps in global governance | Potential for further involvement of global stakeholders |
|
Infection prevention DESA, FAO, GAVI, ILO, ISO, OIE, UNISDR, UN-Water, UNICEF, WHO, WTO |
AMR is another strong argument for the implementation of water, sanitation and hygiene (WASH) interventions in LMICs (SDG6) and for better immunisation (SDG3). Synergies between AMR and interventions to tackle infectious diseases and pandemic preparedness should be better assessed. There is currently limited coordination to design intervention based on co-benefits. |
|
|
Surveillance UNEP, WHO, OIE, FAO, IMF |
The Tripartite has strengthened surveillance of AMR but there are gaps in capacities between countries. In addition, there is limited effort for surveillance of antimicrobial use in animal health and a lack of environmental surveillance of AMR. Another need is a better integration/harmonisation of surveillance standards across sectors. |
|
|
Conservation WHO, IFAD, UN-Habitat, ISO, FAO, OIE |
Current global mechanisms for the conservation of antimicrobials rely mainly on the diffusion of information and adoption of standards. Promotion of antimicrobial use is poorly controlled. The responsibility for conservation is shared between different entities. More efforts are needed to translate this into actionable mechanisms, which are currently more developed in human health than in other sectors. An important challenge is to define common standards for the different areas (ban of antibiotics as growth promoters, critically important antibiotics). |
|
|
Containment ICAO, IMO, UNEP, UNWTO, WHO, OIE, FAO, Wellcome Trust, BMGF |
Expansion of containment strategies should be based on the identification of new ways to prevent the dissemination of AMR in different settings, including in the environment. |
|
|
Innovation GARDP, ITU, UNCTAD, Wellcome Trust, WIPO, WHO |
Addressing market failures against AMR requires market incentives and innovative funding mechanisms. Current efforts should build on existing structures that have proven to be effective. |
|
|
Access Doctors without Borders (MSF), Global Fund, HRC, OHCHR, UNAIDS, UNCTAD, UNDP, UNICRI, UNODC, UNOPS, WHO |
Access to antimicrobials has been mainly supported in specific diseases. A current challenge is that access to medicines can conflict with other challenges of global collective action such as conservation. However, enhancing access can also reduce the use of substandard medicines. The report of the UN Secretary-General’s high-level panel on access to medicines stated that an important issue for improved coherence is the diversity of accountability mechanisms between access and innovation.27 |
|
|
Research education and awareness BMGF, ITC, UNCTAD, UNESCO, UNIATF, UNIDO, UNITAR, UNSSC, UNU, UNWTO, UN-Women, WEF, Wellcome Trust |
The Tripartite produces communication material (eg, global campaign) but other IOs with specific commitments and targets are needed to raise awareness and build evidence on AMR, particularly in areas where AMR is not commonly discussed. An important contribution would be to better measure the (cost-)effectiveness of interventions about AMR and understand how to tailor intervention to the context. |
|
|
Specific diseases GFATM, Medicine for Malaria Venture, Medicine Patent Pool, UNAIDS |
AMR has been a growing problem in several specific diseases including TB, malaria and HIV-AIDS. AMR is another strong argument to build the case for tackling these diseases through an intersectoral approach. AMR is an important case for maximising positive synergies in strengthening health system in LMICs.86 |
|
|
AMR in specific and/or discriminated population and conflicted areas CRPD, ICRC, IOM, MSF, OCHA, OSAA, the Tripartite, UNDP, UNFPA, UNHCR, UNIATF, UNICEF, UNRISD, UNRWA, UN-Women, WFP |
Fragile and discriminated people may be more at risk of AMR.89 There is still a lack of empirical evidence on the link between inequalities and AMR but there is a growing sense that AMR can be an obstacle to poverty reduction.8 90 Several IOs may contribute to raise awareness and, in some cases, mitigate the effect of AMR in these populations. |
|
|
Sustainable funding Asian Infrastructure Investment Bank, IMF, World Bank |
Sustainable funding is a key issue for many AMR efforts. A first challenge is funding dedicated to strengthening global governance. Some countries have helped through earmarked funding for AMR. The other is development aid to strengthen capacities in LMICs. While savings regarding One Health approach have been estimated for important components in tackling infectious diseases, more precise assessment and pilot studies are needed regarding AMR.91 |
|
|
Coordination CEB, ECOSOC, JIU, UNGA, UNSG, HLPF |
AMR requires coordination and collaboration across many different areas. In addition to mechanisms specific to AMR, several IOs and mechanisms share a coordination mandate which could provide relevant fora for discussion on AMR. This should facilitate the definition of a common agenda on infectious disease and issue linkages with other pressing global challenges. |
|
AGISAR, Advisory Group on Integrated Surveillance of Antimicrobial Resistance; AMR, antimicrobial resistance; BMGF, Bill and Melinda Gates Foundation; CEB, Chief Executive Board; CRPD, Convention on the Rights of Persons with Disabilities; DESA, Department of Economic and Social Affairs; ECOSOC, Economic and Social Council; EOSG, Executive Office of the Secretary-General; FAO, Food and Agriculture Organization; GARDP, Global Antibiotic Research and Development Partnership; GAVI, The Vaccine Alliance; GFATM, Global Fund to Fight AIDS, Tuberculosis and Malaria; GLASS, Global Antimicrobial Surveillance System; HLPF, High-Level Political Forum on sustainable development; HRC, Human Rights Council; ICAO, International Civil Aviation Organization; ICRC, International Committee of the Red Cross; IFAD, International Fund for Agricultural Development; IHR, International Health Regulations; ILO, International Labour Organization; IMF, International Monetary Fund; IMO, International Maritime Organization; IOM, International Organization for Migration; IOs, international organisations; ISO, International Organization for Standardization; ITC, International Trade Center; ITU, International Telecommunication Union; JIU, Joint Inspection Unit; LMICs, low/middle-income countries; MSF, Médecins Sans Frontières; OCHA, Office for the Coordination of Humanitarian Affairs; OHCHR, Office of the United Nations High Commissioner for Human Rights; OIE, World Organization for Animal Health; OSAA, Office of the Special Adviser on Africa; PVS, Performance of Veterinary Services; SDGs, Sustainable Development Goals; TB, tuberculosis; UN, United Nations; UNAIDS, United Nations Programme on HIV/AIDS; UNCTAD, United Nations Conferences on Trade and Development; UNDP, United Nations Development Programme; UNEP, United Nations Environment Programme; UNFPA, United Nations Population Fund; UNGA, United Nations General Assembly; UNHCR, United Nations High Commissioner for Refugees; UNIATF, United Nations Interagency Task Force on Non-Communicable Diseases; UNICRI, United Nations Interregional Crime and Justice Research Institute; UNIDO, United Nations Industrial Development Organization; UNISDR, United Nations Office for Disaster Risk Reduction; UNITAR, United Nations Institute for Training and Research; UNODC, United Nations Office on Drugs and Crime; UNOPS, United Nations Office for Project Services; UNRISD, United Nations Research Institute for Social Development; UNRWA, United Nations Relief and Works Agency; UNSG, United Nations Secretary-General; UNSSC, United Nations System Staff College; UNU, United Nations University; UNWTO, World Tourism Organization; WEF, World Economic Forum; WFP, World Food Programme; WIPO, World Intellectual Property Organization; WTO, World Trade Organization.
Finally, some limitations can be identified. As data collection was web-based, some activities might have been undertaken without being reported on the internet. In addition, search was more likely to find recent activities than older ones. This is particularly the case before the 1990–2000s, where relevant literature is often accessible through the grey literature. Interviews with key informants could be useful to complement the findings of the web and document searches. Second, while we discussed the overall ‘output effectiveness’, the reported activities are not assessed in terms of ‘outcome/impact effectiveness’ and the capabilities or organisation in terms of know-how, resources and knowledge. Although our search of documents allowed us to provide relevant background about the broader context of engagement of IOs to address AMR, we were not able to evaluate the level of engagement of IOs for each activity. For example, it may be that an organisation published once on AMR but did not sustain any activity through time. Third, the distinction between relevant and distant depends to some extent on what is considered as relevant. Here we considered activities that focus on several challenges of global collective action but there might be other ways to organise results that the ones identified by our interdisciplinary framework. Given the challenge of collecting all relevant documents on AMR-sensitive activities, our assessment of AMR-sensitive activities might be incomplete. Fourth, our assessment focuses on the UN while the global governance of AMR extends to other organisations. In addition, while several entities within a specific IO can be involved in tackling AMR, the analysis did not have such granularity. Internal dynamics of competition may have substantial implications, for example, when specific units within a specific IO seek to secure funding for their own purposes. Another limitation is the focus of the analysis at the global level whereas several IOs work at the regional level (eg, European Union) or at both the international and regional levels (eg, WHO regional offices) where priorities between global and regional activities can differ.48 Finally, our study focuses on the international level but national and subnational actors are ultimately the ones that need to be involved and convinced about the need and urgency of implementing AMR policies through a coordinated multisectoral and multilevel approach where authority is increasingly dispersed.6 49
Conclusion
In conclusion, our assessment demonstrates the complexities of the global governance of AMR within and beyond the UN system. While WHO has been the traditional actor tackling AMR, there is a growing realisation that it is unable to address the problem on its own given the strong intersectoral nature of AMR. This takes place in a broader context of global governance marked by the evolution from the responsibility of one organisation to a network of organisations that seek to achieve common goals. Our assessment demonstrates that the 'whole of UN approach' adopted in the wake of the 2015 WHO GAP AMR has supported increased collaboration in certain areas but that the outcome/impact effectiveness of such approach deserves further attention. In addition, further research is needed to better account for the varying degrees of engagement across time.
Within this deliberate attempt from the World Health Assembly and the UNGA to expand participation in addressing AMR, the key governing principle should be to ensure that the governance system remains fitted to the evolving challenge of AMR. A key strategy for maximising institutional fit is to reflect on the nature of the six challenges of collective action. While some organisations might be more relevant, more willing, and above all, more likely to receive support from their Member States than others to address AMR, our approach by cluster of organisations offers a range of options to consider in seeking to expand and improve AMR governance in relevant areas.
As the global governance of AMR is embedded within wider processes of global (health) governance, these findings emphasise the relevance of leveraging existing resources, mechanisms and institutions rather than reshuffling the governance of AMR. A ‘whole of UN approach’ in an essentially polycentric governance system currently provides a realistic yet underevaluated approach to address AMR. This 'whole of UN approach' should be part of wider efforts towards building more sustainable and resilient societies.
The Tripartite+ constituted of the core organisations (WHO, OIE and FAO + UNEP) should continue to lead the way for developing the AMR agenda. Harnessing the power of the UN system to move the AMR agenda forward can not only help tackle AMR, but it can also contribute to transform the UN system to make it ripe to address the challenges of the 21st century.
Acknowledgments
This work is an expansion of a mandate that was conducted in 2018 for the Interagency Coordination Group on AMR, which released its final recommendations in April 2019. We would like to thank the United Nations Foundation and the Wellcome Trust for support in the research that led to the production of this manuscript. We thank Professor Keiji Fukuda for comments on an earlier version of this work. Furthermore, we thank Ms Elisa Manetti for research assistance on this project.
Footnotes
Handling editor: Stephanie M Topp
Contributors: DW designed the study, collected and analysed the data. DW drafted the paper. SH, NL and DP provided text and edited the manuscript. DW produced the figure, tables and the supplemental material. DW is responsible for the overall content as guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Data about weblinks consulted for the preparation of this manuscript can be provided upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
No ethical approval was sought as per our university requirements.
References
- 1.Jørgensen PS, Aktipis A, Brown Z. Antibiotic and pesticide susceptibility and the Anthropocene operating space. Nature Sustainability 2018;1:632–41. [Google Scholar]
- 2.World Health Organization . Global action plan on antimicrobial resistance. Geneva: World Health Organization, 2015. http://apps.who.int/iris/bitstream/handle/10665/193736/9789241509763_eng.pdf?sequence=1 [DOI] [PubMed] [Google Scholar]
- 3.World Organisation for Animal Health . The OIE strategy on antimicrobial resistance and the prudent use of antimicrobials, 2016. Available: http://www.oie.int/fileadmin/Home/eng/Media_Center/docs/pdf/PortailAMR/EN_OIE-AMRstrategy.pdf [Accessed 18 Mar 2017].
- 4.Food and Agriculture Organization of the United Nations . The FAO action plan on antimicrobial resistance 2016-2020, 2016. Available: http://www.fao.org/3/a-i5996e.pdf [Accessed 18 Mar 2017].
- 5.United Nations General Assembly . Resolution 71/3 political Declaration of the high-level meeting of the general assembly on antimicrobial resistance, 2016. Available: http://www.un.org/en/ga/search/view_doc.asp?symbol=A/RES/71/3
- 6.World Health Organization . Anti-Infective drug resistance surveillance and containment team. who global strategy for the containment of antimicrobial resistance. Geneva: World Health Organization, 2001. http://whqlibdoc.who.int/hq/2001/WHO_CDS_CSR_DRS_2001.2.pdf [Google Scholar]
- 7.Overton K, Fortané N, Broom A, et al. Waves of attention: patterns and themes of international antimicrobial resistance reports, 1945-2020. BMJ Glob Health 2021;6:e006909. 10.1136/bmjgh-2021-006909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jonas OB, Irwin A, Berthe FCJ. Drug-resistant infections: a threat to our economic future, 2017. Available: https://documents1.worldbank.org/curated/en/323311493396993758/pdf/final-report.pdf [Accessed 5 May 2022].
- 9.Robinson TP, Bu DP, Carrique-Mas J, et al. Antibiotic resistance is the Quintessential one health issue. Trans R Soc Trop Med Hyg 2016;110:377–80. 10.1093/trstmh/trw048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization . Tuberculosis and air travel: guidelines for prevention and control. 3rd edn. Geneva: World Health Organization, 2008. [PubMed] [Google Scholar]
- 11.World Health Organization . Strategy for malaria elimination in the greater Mekong subregion (2015-2030. Geneva: WHO, 2015. https://apps.who.int/iris/bitstream/handle/10665/208203/9789290617181_eng.pdf?sequence=1&isAllowed=y [Google Scholar]
- 12.Gradmann C. Sensitive matters: the world health organisation and antibiotic resistance testing, 1945-1975. Social History of Medicine 2013;26:555–74. 10.1093/shm/hkt018 [DOI] [Google Scholar]
- 13.United Nations Environment Programme . Environment and health, 2018. Available: https://wedocs.unep.org/bitstream/handle/20.500.11822/30795/UNEA3_4EN.pdf
- 14.World Health Organization, UNICEF . Global action plan for prevention and control of pneumonia (GAPP), 2009. Available: http://whqlibdoc.who.int/hq/2009/WHO_FCH_CAH_NCH_09.04_eng.pdf?ua=1 [DOI] [PMC free article] [PubMed]
- 15.Sharland M, Pulcini C, Harbarth S, et al. Classifying antibiotics in the WHO essential medicines list for optimal use-be aware. Lancet Infect Dis 2018;18:18–20. 10.1016/S1473-3099(17)30724-7 [DOI] [PubMed] [Google Scholar]
- 16.World Organisation for Animal Health . OIE annual report on antimicrobial agents intended for use in animals: better understanding of the global situation, 2020. Available: https://www.oie.int/app/uploads/2021/03/a-fourth-annual-report-amr.pdf
- 17.Frost I, Van Boeckel TP, Pires J, et al. Global geographic trends in antimicrobial resistance: the role of international travel. J Travel Med 2019;26:taz036. 10.1093/jtm/taz036 [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization . Guidelines for the prevention and control of carbapenem-resistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in health care facilities. Geneva: World Health Organization, 2017. [PubMed] [Google Scholar]
- 19.Wernli D, Haustein T, Harbarth S. The European approach to antimicrobial resistance: success stories and challenges. Global Health Europe Issue Briefs 2011. [Google Scholar]
- 20.So AD, Shah TA, Roach S, et al. An integrated systems approach is needed to ensure the sustainability of antibiotic effectiveness for both humans and animals. J Law Med Ethics 2015;43:38–45. 10.1111/jlme.12273 [DOI] [PubMed] [Google Scholar]
- 21.Simpkin VL, Renwick MJ, Kelly R, et al. Incentivising innovation in antibiotic drug discovery and development: progress, challenges and next steps. J Antibiot 2017;70:1087. 10.1038/ja.2017.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Renwick MJ, Brogan DM, Mossialos E. A systematic review and critical assessment of incentive strategies for discovery and development of novel antibiotics. J Antibiot 2016;69:73–88. 10.1038/ja.2015.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tacconelli E, Carrara E, Savoldi A, et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis 2018;18:318–27. 10.1016/S1473-3099(17)30753-3 [DOI] [PubMed] [Google Scholar]
- 24.Balasegaram M, Piddock LJV. The global antibiotic research and development partnership (GARDP) not-for-profit model of antibiotic development. ACS Infect Dis 2020;6:1295–8. 10.1021/acsinfecdis.0c00101 [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization, World Intellectual Property Organization, World Trade Organization . Promoting access to medical technologies and innovation: Intersections between public health, intellectual property and trade. 2nd edn. Geneva: WHO, 2020. https://www.wto.org/english/res_e/booksp_e/who-wipo-wto-2020_e.pdf [Google Scholar]
- 26.Lee K. Global institutions: the world Health organization. Abingdon: Routledge, 2009. [Google Scholar]
- 27.High-Level Panel on Access to Medicines . The report of the UN Secretary-General’s high-level panel on access to medicines: promoting innovation and access to health technologies. United Nations Secretary General, 2016. Available: http://www.unsgaccessmeds.org/final-report/
- 28.United Nations General Assembly . Political declaration of the high-level meeting of the general assembly on the fight against tuberculosis (73/3), 2018. Available: http://www.un.org/en/ga/search/view_doc.asp?symbol=A/RES/73/3
- 29.World Health Organization, Food and Agriculture Organization of the United Nations, World Organisation for Animal Health . Monitoring and evaluation of the global action plan on antimicrobial resistance: framework and recommended indicators. Geneva: World Health Organization, 2019. [Google Scholar]
- 30.Jasovský D, Littmann J, Zorzet A, et al. Antimicrobial resistance-a threat to the world’s sustainable development. Ups J Med Sci 2016;121:159–64. 10.1080/03009734.2016.1195900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shiffman J, Quissell K, Schmitz HP, et al. A framework on the emergence and effectiveness of global health networks. Health Policy Plan 2016;31:i3–16. 10.1093/heapol/czu046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shiffman J, Smith S. Generation of political priority for global health initiatives: a framework and case study of maternal mortality. Lancet 2007;370:1370–9. 10.1016/S0140-6736(07)61579-7 [DOI] [PubMed] [Google Scholar]
- 33.Huijbers PMC, Flach C-F, Larsson DGJ. A conceptual framework for the environmental surveillance of antibiotics and antibiotic resistance. Environ Int 2019;130:104880. 10.1016/j.envint.2019.05.074 [DOI] [PubMed] [Google Scholar]
- 34.United Nations Foundation . Roles, responsibilities and remit of UN organisations in relation to antimicrobial resistance, 2018. Available: https://cdn.who.int/media/docs/default-source/antimicrobial-resistance/amr-gcp-tjs/iacg/other-documents/amr-mapping-synthesis-report-unf.pdf?sfvrsn=4d355fca_5
- 35.World Bank . Pulling together to beat superbugs knowledge and implementation gaps in addressing antimicrobial resistance, 2019. Available: http://documents1.worldbank.org/curated/en/430051570735014540/pdf/Pulling-Together-to-Beat-Superbugs-Knowledge-and-Implementation-Gaps-in-Addressing-Antimicrobial-Resistance.pdf
- 36.Gopinathan U, Watts N, Hougendobler D, et al. Conceptual and institutional gaps: understanding how the WHO can become a more effective cross-sectoral collaborator. Global Health 2015;11:46. 10.1186/s12992-015-0128-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Biermann R, Koops JA. Palgrave handbook of inter-organizational relations in world politics. London: Palgrave Macmillan UK, 2017. [Google Scholar]
- 38.Podolsky SH, Bud R, Gradmann C, et al. History teaches us that confronting antibiotic resistance requires stronger global collective action. J Law Med Ethics 2015;43:27–32. 10.1111/jlme.12271 [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization . Collaboration within the United Nations system and with other intergovernmental organizations, 2018. [Google Scholar]
- 40.Rogers Van Katwyk S, Weldon I, Giubilini A, et al. Making use of existing international legal mechanisms to manage the global antimicrobial commons: identifying legal hooks and institutional mandates. Health Care Anal 2020;105 10.1007/s10728-020-00393-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rogers Van Katwyk S, Giubilini A, Kirchhelle C, et al. Exploring models for an international legal agreement on the global antimicrobial commons: lessons from climate agreements. Health Care Anal 2020:3. 10.1007/s10728-019-00389-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mendelson M, Dar OA, Hoffman SJ, et al. A global antimicrobial conservation fund for low- and middle-income countries. Int J Infect Dis 2016;51:70–2. 10.1016/j.ijid.2016.09.016 [DOI] [PubMed] [Google Scholar]
- 43.World Health Organization, Food and Agriculture Organization of the United Nations, World Organisation for Animal Health, The FAO-OIE-WHO collaboration . Sharing responsibilities and coordinating global activities to address health risks at the animal-human-ecosystems interfaces. A tripartite concept note, 2010. Available: https://cdn.who.int/media/docs/default-source/ntds/neglected-tropical-diseases-non-disease-specific/tripartite_concept_note_hanoi_042011_en.pdf?sfvrsn=8042da0c_1&download=true [Accessed 5 May 2022].
- 44.Food and Agriculture Organization of the United Nations, World Organisation for Animal Health, World Health Organization . Providing multi-sectoral, collaborative leadership in addressing health challenges, 2017. Available: http://www.oie.int/fileadmin/Home/eng/Media_Center/docs/pdf/Tripartite_2017.pdf
- 45.Global Health Programme . Good global health begins at home. Geneva, Switzerland: Global Health Programme, 2012. [Google Scholar]
- 46.Held D, Kickbusch I, McNally K, et al. Gridlock, innovation and resilience in global health governance. Glob Policy 2019;10:161–77. 10.1111/1758-5899.12654 [DOI] [Google Scholar]
- 47.Buse K, Hawkes S. Sitting on the FENSA: WHO engagement with industry. Lancet 2016;388:446–7. 10.1016/S0140-6736(16)31141-2 [DOI] [PubMed] [Google Scholar]
- 48.Hanrieder T. The path-dependent design of international organizations: federalism in the world Health organization. Europ J Int Relat 2014. [Google Scholar]
- 49.Schakel AH, Hooghe L, Marks G. Multilevel governance and the state. In: The Oxford Handbook of transformations of the state, 2015: 269–85. [Google Scholar]
- 50.Interagency Coordination Group on Antimicrobial Resistance . AMR framework for action supported by IACG, 2017. Available: https://cdn.who.int/media/docs/default-source/antimicrobial-resistance/amr-gcp-tjs/iacg/other-documents/20170818-amr-ffa-v01.pdf?sfvrsn=796a325e_6
- 51.Dar OA, Hasan R, Schlundt J, et al. Exploring the evidence base for national and regional policy interventions to combat resistance. Lancet 2016;387:285–95. 10.1016/S0140-6736(15)00520-6 [DOI] [PubMed] [Google Scholar]
- 52.Shah NS, Auld SC, Brust JCM, et al. Transmission of extensively drug-resistant tuberculosis in South Africa. N Engl J Med Overseas Ed 2017;376:243–53. 10.1056/NEJMoa1604544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kirchhelle C, Atkinson P, Broom A, et al. Setting the standard: multidisciplinary hallmarks for structural, equitable and tracked antibiotic policy. BMJ Glob Health 2020;5:e003091. 10.1136/bmjgh-2020-003091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Abbott KW, Snidal D. Why states act through formal international organizations. J Conflict Resolut 1998;42:3–32. 10.1177/0022002798042001001 [DOI] [Google Scholar]
- 55.Silberschmidt G. How to set priorities for the world Health organization. Geneva: Global Health Programme, Graduate Institute of International and Development Studies, 2012. [Google Scholar]
- 56.Littoz-Monnet A. The politics of expertise in international organizations : how international bureaucracies produce and mobilize knowledge. Abingdon, Oxon; New York, NY: Routledge, 2017. [Google Scholar]
- 57.Weiss TG, Wilkinson R. International organization and global governance. London; New York: Routledge, Taylor & Francis Group, 2014. [Google Scholar]
- 58.Barkin JS. International organization: theories and institutions. Palgrave Macmillan, 2013. [Google Scholar]
- 59.Nay O. International organisations and the production of Hegemonic knowledge: how the World Bank and the oecd helped invent the fragile state concept. Third World Q 2014;35:210–31. 10.1080/01436597.2014.878128 [DOI] [Google Scholar]
- 60.Kamradt-Scott A. The WHO secretariat, norm entrepreneurship, and global disease outbreak control. J Int Organ Stud 2010;1:72–89. [Google Scholar]
- 61.Finnemore M, Sikkink K. International norm dynamics and political change. Int Organ 1998;52:887–917. 10.1162/002081898550789 [DOI] [Google Scholar]
- 62.Weiss TG. Global governance: why what whither. Polity Press, 2013. [Google Scholar]
- 63.Barnett M, Finnemore M. Rules for the world: international organizations in global politics. Cornell University Press, 2004. [Google Scholar]
- 64.World Health Organization . Procurement at WHO. Available: https://www.who.int/about/accountability/procurement/ [Accessed 21 Jun 2021].
- 65.Kentikelenis AE. Structural adjustment and health: a conceptual framework and evidence on pathways. Soc Sci Med 2017;187:296–305. 10.1016/j.socscimed.2017.02.021 [DOI] [PubMed] [Google Scholar]
- 66.Hoffman SJ, Røttingen J-A. Assessing implementation mechanisms for an international agreement on research and development for health products. Bull World Health Organ 2012;90:854–63. 10.2471/BLT.12.109827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Oberthür S, Stokke OS. Managing institutional complexity: regime interplay and global environmental change. MIT Press, 2011. [Google Scholar]
- 68.Morin J-F, Louafi S, Orsini A, et al. Boundary organizations in regime complexes: a social network profile of IPBES. J Int Relat Dev 2017;20:543–77. 10.1057/s41268-016-0006-8 [DOI] [Google Scholar]
- 69.Codex Alimentarius Commission . International code of practice for control of the use of veterinary drugs (CAC/RCP 38-1993), 1993. [Google Scholar]
- 70.Codex Alimentarius Commission . Code of practice to minimize and contain antimicrobial resistance CAC/RCP 61-2005, 2005. Available: http://www.fao.org/input/download/standards/10213/CXP_061e.pdf
- 71.Codex Alimentarius Commission . Guidelines for risk analysis of foodborne antimicrobial resistance (CAC/GL 77-2011), 2011. Available: http://www.fao.org/input/download/standards/11776/CXG_077e.pdf
- 72.World Health Organization,, World Organisation for Animal Health . WHO-OIE operational framework for good governance at the human-animal interface: bridging WHO and OIE tools for the assessment of national capacities, 2014. Available: https://cdn.who.int/media/docs/default-source/documents/publications/who-oie-framework-for-good-governance-human-animal-interface.pdf?sfvrsn=f9f92e6b_2&download=true
- 73.Food and Agriculture Organization of the United Nations, World organisation for Animal Health, World Health Organization . The Tripartite’s commitment: providing multi-sectoral, collaborative leadership in addressing health challenges, 2017. Available: http://www.oie.int/fileadmin/Home/eng/Media_Center/docs/pdf/Tripartite_2017.pdf
- 74.World Health Organization . Antimicrobial resistance: global report on surveillance. Geneva: World Health Organization, 2014. https://apps.who.int/iris/handle/10665/112642 [Google Scholar]
- 75.World Organisation for Animal Health . Agreement between the world trade organization and the office international des Epizooties, 1998. Available: https://docsonline.wto.org/dol2fe/Pages/FormerScriptedSearch/directdoc.aspx?DDFDocuments/t/WT/L/272.doc
- 76.Food and Agriculture Organization of the United Nations, World Organisation for Animal Health, World Health Organization . Global framework for development & stewardship to combat antimicrobial resistance draft roadmap. Geneva: WHO, 2017. https://cdn.who.int/media/docs/default-source/antimicrobial-resistance/global-framework-for-development-stewardship-to-combat-antimicrobial-resistance-draft-roadmapc7992004-9970-406e-b1f2-515b25c4770b.pdf?sfvrsn=14d8813c_1&download=true [Google Scholar]
- 77.Food and Agriculture Organization of the United Nations, World Trade Organization . Trade and food standards, 2017. Available: http://www.fao.org/3/a-i7407e.pdf
- 78.World Health Organization, World Intellectual Property Organization, World Trade Organization . Antimicrobial resistance – a global epidemic - Background paper for the Technical Symposium on Antimicrobial Resistance: How to Foster Innovation, Access and Appropriate Use of Antibiotics? Prepared by the Secretariats of WHO, WIPO and WTO, 2016. Available: https://www.wipo.int/edocs/mdocs/mdocs/en/wipo_who_wto_ip_ge_16/wipo_who_wto_ip_ge_16_inf_2.pdf
- 79.World Trade Organization . The WTO and the World Health Organization. Available: https://www.wto.org/english/thewto_e/coher_e/wto_who_e.htm [Accessed 27 Oct 2018].
- 80.Interagency Coordination Group on Antimicrobial Resistance . Work plan of the ad-hoc Interagency coordination group on antimicrobial resistance, 2017. Available: https://www.who.int/antimicrobial-resistance/interagency-coordination-group/IACG-AMR_workplan.pdf?ua=1
- 81.Interagency Coordination Group on Antimicrobial Resistance . No time to wait: securing the future from drug-resistant infections: report to the Secretary-General of the United nations, 2019. Available: https://cdn.who.int/media/docs/default-source/documents/no-time-to-wait-securing-the-future-from-drug-resistant-infections-en.pdf?sfvrsn=5b424d7_6&download=true
- 82.European Union . A European one health action plan against antimicrobial resistance, 2017. Available: https://ec.europa.eu/health/sites/default/files/antimicrobial_resistance/docs/amr_2017_action-plan.pdf
- 83.Buse K, Harmer A. Global health partnerships: the mosh pit of global health Governance. In: Buse K, Hein W, Drager N, eds. Making sense of global health governance: a policy perspective. Basingstoke: Palgrave Macmillan, 2009: 366. [Google Scholar]
- 84.ReAct . AMR Stakeholder mapping, 2016. Available: https://www.reactgroup.org/uploads/Stakeholder%20Analysis_ReActForWHO.pdf [Accessed 5 May 2022].
- 85.Sands P, Mundaca-Shah C, Dzau VJ. The neglected dimension of global security - a framework for countering infectious-disease crises. New England Journal of Medicine 2016;374:1281–7. [DOI] [PubMed] [Google Scholar]
- 86., Samb B, Evans T, et al. , World Health Organization Maximizing Positive Synergies Collaborative Group . An assessment of interactions between global health initiatives and country health systems. Lancet 2009;373:2137–69. 10.1016/S0140-6736(09)60919-3 [DOI] [PubMed] [Google Scholar]
- 87.Inoue H, Minghui R. Antimicrobial resistance: translating political commitment into national action. Bull World Health Organ 2017;95:242. 10.2471/BLT.17.191890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Institute of Medicine, National Academies of Sciences/Engineering/Medicine . Global health risk framework: resilient and sustainable health systems to respond to global infectious disease outbreaks: workshop summary. Washington, DC: The National Academies Press, 2016. [PubMed] [Google Scholar]
- 89.Alsan M, Kammili N, Lakshmi J, et al. Poverty and community-acquired antimicrobial resistance with extended-spectrum β-lactamase-producing organisms, Hyderabad, India. Emerg Infect Dis 2018;24:1490–6. 10.3201/eid2408.171030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ahmed SA, Barış E, Go DS, et al. Assessing the global poverty effects of antimicrobial resistance. World Dev 2018;111:148–60. 10.1016/j.worlddev.2018.06.022 [DOI] [Google Scholar]
- 91.Queenan K, Häsler B, Rushton J. A one health approach to antimicrobial resistance surveillance: is there a business case for it? Int J Antimicrob Agents 2016;48:422–7. 10.1016/j.ijantimicag.2016.06.014 [DOI] [PubMed] [Google Scholar]
- 92.Sands P, El Turabi A, Saynisch PA, et al. Assessment of economic vulnerability to infectious disease crises. Lancet 2016;388:2443–8. 10.1016/S0140-6736(16)30594-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Krech R, Kickbusch I, Franz C, et al. Banking for health: the role of financial sector actors in investing in global health. BMJ Glob Health 2018;3:e000597. 10.1136/bmjgh-2017-000597 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2021-008181supp001.pdf (379.4KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Data about weblinks consulted for the preparation of this manuscript can be provided upon reasonable request.