Abstract
Background
Alanine aminotransferase (ALT) is a marker of hepatic damage and its range can be affected by viral hepatitis, alcoholic hepatitis and non-alcoholic fatty liver diseases. We aimed to study the factors associated with higher ALT level and update the upper limit of normal (ULN) in the Vietnamese population.
Methods
This cross-sectional study enrolled 8383 adults, aged 18 years and older who visited the Medical Center at Ho Chi Minh City for a health check-up. Following the exclusion criteria, 6677 subjects were included in the analysis.
Results
Age ≤40 years, male gender, body mass index >23 kg/m2, diastolic blood pressure >85 mm Hg, cholesterol >5.2 mmol/L, triglyceride >1.7 mmol/L, positivity, anti-hepatitis C virus positivity and fatty liver (p<0.05) were associated with higher ALT level (>40 U/L). Without considering age and gender, healthy group is defined after exclusion of participants with one of the mentioned contributing factors. The median ALT level in the healthy group was 18 in men and 13 in women. The ULN at the 95th percentile of the healthy group was 40 U/L in men and 28 U/L in women.
Conclusion
The ULN for ALT in healthy women was lower than in healthy men. Updated ULN for ALT level can promote the identification of unhealthy subjects. More studies that involve ethnicity and lifestyle factors are needed to confirm the new ULN in the Vietnamese population.
Keywords: chronic hepatitis, chronic liver disease, fatty liver, enzymology
What is already known about this subject?
The upper limit of normal (ULN) for serum alanine aminotransferase (ALT) is generally considered at 40 U/L in different laboratories.
ALT can be affected by various factors such as age, gender, body mass index, strenuous physical exercise, diet, metabolic status, fasting blood glucose, alcohol consumption and drug treatment.
What are the new findings?
The updated ULN for serum ALT in the Vietnamese population is lower than the previous value, estimated at 28 U/L for healthy women and 40 U/L for healthy men.
How might it impact on clinical practice in the foreseeable future?
The updated ULN for serum ALT in the Vietnamese healthy population can promote early diagnosis, treatment follow-up and prognosis of liver injuries.
Introduction
The clinical diagnosis of acute and chronic illnesses is normally made from various basic blood assays. Transaminase blood chemical tests are used to evaluate liver function and for diagnosis and evaluation of outcome, prognosis and follow-up of patients with liver diseases.1 Alanine aminotransferase (ALT) is mainly presented in hepatocytes, and increased ALT level in the blood usually reflects hepatic cellular damage. ALT level has been widely used as a surrogate marker of liver injury and to evaluate therapeutic efficacy or reversal of liver diseases.2 3 Chronic liver diseases such as hepatitis due to various aetiologies, primary biliary cholangitis, non-alcoholic fatty liver disease, and congenital disorders all exhibit increased serum ALT levels.4 Besides diurnal fluctuation, the level of serum ALT can also be affected by age, gender, body mass index (BMI), strenuous physical exercise, diet, metabolic status, fasting blood glucose, alcohol consumption and drug treatment.5–8
Earlier reference ranges for ALT, which had been suggested by Wroblewski in the 1950s and modified in the 1980s, are still widely used despite notable changes in socioeconomic, scientific and health aspects of humans in the past few decades.9 Although the reference range for ALT varies among different laboratories, the current upper limit of normal (ULN) is usually set at 40 U/L.10 This is the threshold for early screening of blood donors with non-A and B hepatitis before anti-hepatitis C virus (anti-HCV) testing.11 12 With the current ULN, there is potential risk of bias since the reference populations are likely to include people with non-alcoholic fatty liver disease or HCV viral hepatitis, which is now one of the most common aetiologies of chronic liver disease.12–14
Several studies have recently questioned the reliability and sensitivity of the established ULN for serum ALT level. In a large-scale study involving blood donors, Piton and colleagues15 suggested an updated ULN for ALT of 42 U/L for men and 31 U/L for women with BMI ≤23. Another Italian study demonstrated an updated ULN for ALT of 30 U/L for men and 19 U/L for women.10 In healthy adults, Israeli data showed that the ULN for ALT was 45 U/L for men and 32 U/L for women, and in an Iranian study the ULN was 34 U/L and 40 U/L for non-overweight women and men, respectively.7 8 Moreover, Asian populations have different ranges for BMI, nutritional diet and lifestyle, as well as different liver-related disease patterns compared with Western populations. It is not clear whether normal ALT ranges among healthy Asians should be derived from Caucasian populations. Several studies have investigated the normal ALT level in Asian populations. In the Korean population, the ULN for ALT for men was 31 U/L and 23 U/L for women.16 In Chinese men and women, the ULN was 22.15 U/L and 22.4 U/L, respectively.17 Although Vietnam is one of the countries with high prevalence of chronic liver diseases (mainly HCV, hepatitis B virus (HBV), and metabolic or alcoholic fatty liver disease), the normal range for ALT is not yet well established.18 19 Therefore, we conducted this study on a large representative group of healthy Vietnamese adult subjects to update the ULN level for ALT and to identify risk factors affecting its level.
Methods
Study population
This cross-sectional study retrospectively enrolled 8383 consecutive adults, aged 18 years or older who visited the University Medical Center of University of Medicine and Pharmacy at Ho Chi Minh city (Vietnam) for regular health check-up during the period from June 2017 to May 2018. Subjects with incomplete data and laboratory documents as well as pregnant women were excluded from the study.
Collected data included age, sex, BMI, systolic and diastolic blood pressure, biochemical markers (ALT, fasting blood glucose, blood cholesterol, blood high-density lipoprotein cholesterol (HDL-C) and blood triglycerides), serological markers (hepatitis B antigen surface (HBsAg) and anti-HCV) and abdominal ultrasound results.
We set the upper limit of BMI at 23 kg/m2 based on the WHO criteria for Asian population.20 The ULN for systolic and diastolic blood pressure was also set at 130 mm Hg and 85 mm Hg, respectively. Fatty liver diagnosis was established using ultrasonography according to the 2012 guidelines of the American Gastroenterological Association.21
We stored all records of participants in this study confidentially and in private.
Measurement of biochemical and serological markers
Samples from venous blood of participants were collected after an overnight fast. ALT activity was quantitatively determined by the kinetic ultraviolet test on Beckman Coulter Analyzer (Enzyme Commission (EC)2.6.1.2). Electrochemiluminescent immunoassays were carried out to test for serum HBsAg and anti-HCV positivity using ADVIA Centaur HBsAgII Kit and HCV 200T Kit (Siemens, USA), respectively. Serum biochemical tests were measured using Beckman Coulter machine (USA). The upper limit considered for fasting glucose was 100 mg/dL (5.6 mmol/L), 200 mg/dL (5.2 mmol/L) for total cholesterol and 150 mg/dL (1.7 mmol/L) for triglycerides. The lower limits considered for HDL-C were 40 mg/dL for men and 50 mg/dL for women, according to the American Association of Clinical Endocrinologists 2017 guidelines.22
Statistical analysis
All records were stored in Excel. For statistical purposes, all analyses were performed using IBM SPSS Statistics V.20. The assumption of normality was checked by Kolmogorov-Smirnov test. Continuous variables are presented as mean±SD when normally distributed and as median and IQR for variables without normal distribution. Continuous variables with normal distribution are compared by t-test or analysis of variance. On the other hand, Kruskal-Wallis or Mann-Whitney U test was used to compare variables without a normal distribution. A univariable analysis was carried out to test the association of different variables with higher ALT level (>40 U/L). Relevant variables with p value <0.1 by univariable analysis underwent multivariable analysis via the logistic regression model. A p value of less than 0.05 was considered statistically significant. Subjects without risk factors for higher ALT levels constituted the healthy reference population. This healthy population is assumed to possess no factors that might affect serum ALT level. We defined the ULN for ALT at the 95th percentile of the reference healthy population.
Results
Baseline characteristics of all included participants
Out of the 8383 subjects initially enrolled in this study, 1706 were excluded. Figure 1 describes the reasons for exclusion and provides a summary of the steps in our study. The included study population consisted of 6677 subjects, 76.3% of whom were male. The median (IQR) age of the participants was 38 (30–49) years. Moreover, 57.1% of all included participants had a BMI ≥23 kg/m2. Elevated systolic blood pressure was commonly observed in 49.3% of the subjects, while diastolic blood pressure was elevated in 32.8%. HBsAg positivity was detected in 609 subjects, while anti-HCV positivity was present in only 77 individuals. On abdominal ultrasound, 2273 subjects were diagnosed with fatty liver. Increase in triglycerides level, cholesterol level and fasting blood glucose was observed in 47.1%, 29% and 22% of the population, respectively. Moreover, 36.4% of the population had lower HDL-C value. With regard to ALT, 22.7% of the subjects had an ALT level >40 U/L (95% of these participants with high ALT were men). The median (IQR) level of ALT of all participants was 25 (17–39) U/L. On comparing the ALT level based on sex, men had statistically significantly higher ALT level, with a median (IQR) of 29 (20–43) U/L compared with a median (IQR) of 15 (12–21) U/L in women (p<0.001, Mann-Whitney U test).
Figure 1.
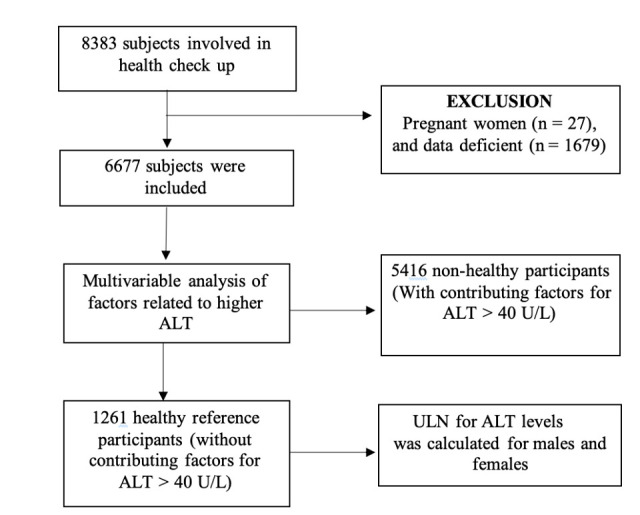
Flow chart of the study design. ALT, alanine aminotransferase, ULN, upper limit of normal.
Factors associated with elevated serum ALT level
The univariable analysis revealed nine factors significantly related to higher ALT level (>40 U/L), namely male sex, BMI ≥23 kg/m2, systolic blood pressure ≥130 mm Hg, diastolic blood pressure ≥85 mm Hg, fasting glucose ≥5.6 mmol/L, cholesterol ≥5.2 mmol/L, triglycerides ≥1.7 mmol/L, HBsAg positivity and fatty liver on ultrasound (p<0.05). Although not statistically significant (p<0.1), higher ALT was associated with younger age (≤40), Low-density lipoprotein cholesterol (LDL-C) <40 mg/dL for men and 50 mg/dL for women, and anti-HCV positivity (table 1).
Table 1.
Univariable and multivariable analyses of factors related to ALT >40 U/L (N=6677)
| Parameters | Univariable analysis | Multivariable analysis | ||||
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Male | 7.6 | 6 to 9.6 | <0.001 | 4.2 | 3.3 to 5.5 | <0.001 |
| Age ≤40 years | 1.1 | 1 to 1.26 | 0.06 | 2.1 | 1.8 to 2.4 | <0.001 |
| BMI ≥23 kg/m2 | 4.34 | 3.8 to 5 | <0.001 | 2.1 | 1.8 to 2.45 | <0.001 |
| Systolic BP ≥130 mm Hg | 2.2 | 2 to 2.5 | <0.001 | 1.09 | 0.9 to 1.26 | 0.28 |
| Diastolic BP ≥85 mm Hg | 2.3 | 2.1 to 2.6 | <0.001 | 1.36 | 1.2 to 1.6 | <0.001 |
| Fasting glucose ≥5.6 mmol/L | 1.75 | 1.5 to 2 | <0.001 | 1.13 | 0.97 to 1.32 | 0.12 |
| Cholesterol ≥5.2 mmol/L | 1.97 | 1.75 to 2.2 | <0.001 | 1.36 | 1.18 to 1.56 | <0.001 |
| Low HDL-C | 1.12 | 1 to 1.26 | 0.053 | 1.02 | 0.9 to 1.17 | 0.78 |
| Triglycerides ≥1.7 mmol/L | 3.33 | 2.94 to 3.76 | <0.001 | 1.65 | 1.4 to 1.9 | <0.001 |
| Fatty liver on abdominal ultrasound | 4.4 | 3.9 to 5 | <0.001 | 2.74 | 2.4 to 3.2 | <0.001 |
| HBsAg positivity | 1.4 | 1.16 to 1.68 | <0.001 | 1.58 | 1.3 to 1.95 | <0.001 |
| Anti-HCV positivity | 1.55 | 0.95 to 2.5 | 0.079 | 1.72 | 1 to 2.95 | 0.051 |
ALT, alanine aminotransferase; BMI, body mass index; BP, blood pressure; HBsAg, hepatitis B antigen surface; HCV, hepatitis C virus; HDL-C, high-density lipoprotein cholesterol.
The results of the multivariable analysis found eight remaining factors that had a significant association with higher ALT level (>40 U/L), namely age ≤40 years old, male sex, BMI ≥23 kg/m2, diastolic blood pressure ≥85 mm Hg, cholesterol level ≥5.2 mmol/L, triglyceride level ≥1.7 mmol/L, HBsAg positivity and fatty liver on ultrasound (table 1).
Characteristics of the healthy reference group
Since it was impractical to use age group and sex as criteria for selection, the healthy population was selected based on the six remaining factors that significantly contributed to higher ALT level (>40 U/L) on multivariable analysis, which are BMI ≥23 kg/m2, diastolic blood pressure ≥85 mm Hg, cholesterol ≥5.2 mmol/L, triglycerides ≥1.7 mmol/L, HBsAg positivity and fatty liver on ultrasound. After excluding 5408 subjects who had at least one of these six factors, we categorised the remaining 1269 subjects as the healthy population. In this healthy population we found eight anti-HCV (+) patients; after excluding these eight patients, we defined the remaining 1261 subjects as the healthy reference group.
The median (IQR) age of these healthy subjects was 32 (27–38) years. Men constituted 49.7% (627 of 1261) of the healthy reference group. Mann-Whitney U test was used to compare the characteristics of healthy men and women. Although men had lower HDL-C compared with women, they had higher diastolic blood pressure and higher triglyceride level (p<0.05) (table 2).
Table 2.
Characteristics of male and female healthy participants (n=1269)
| Characteristics | Male (n=632) Median (IQR) |
Female (n=637) Median (IQR) |
P value* |
| Age (years) | 31 (26–39) | 33 (28–38) | 0.022 |
| BMI (kg/m2) | 20.7 (19.4–21.9) | 20.5 (19.4–21.6) | 0.1 |
| Diastolic BP (mm Hg) | 74 (69–79) | 70 (64–75) | <0.001 |
| Fasting glucose (mmol/L) | 4.8 (4.5–5.1) | 4.8 (4.6–5.1) | 0.43 |
| Cholesterol (mmol/L) | 4.5 (4.1–5) | 4.6 (4.1–5) | 0.08 |
| HDL-C (mmol/L) | 1.2 (1.05–1.39) | 1.34 (1.16–1.5) | <0.001 |
| Triglycerides (mmol/L) | 1.05 (0.8–1.3) | 0.8 (0.6–1.06) | <0.001 |
*Mann-Whitney U test.
BMI, body mass index; BP, blood pressure; HDL-C, high-density lipoprotein cholesterol
Distribution of ALT in the healthy population and ULN for ALT
The healthy group still had 3.3% of its subjects (30 men, 11 women) with ALT >40 U/L for undefined causes (ranging from 42 U/L to 206 U/L). The 25th percentile, median, and the 75th and 95th percentiles of ALT in this healthy population were 12 U/L, 16 U/L, 21 U/L and 36 U/L, respectively. The corresponding percentiles in healthy men were 14 U/L, 18 U/L, 25 U/L and 40 U/L. On the other hand, these percentiles were 10 U/L, 13 U/L, 17 U/L and 28 U/L in healthy women. ALT levels were higher in men than in women across different age groups, with the difference statistically significant in every consecutive age group <50 years (figure 2, table 3). ALT was similarly distributed across different age groups of men and women (figure 2, table 3). Therefore, in order to establish the ULN for ALT for each sex, we applied the 95th percentile of ALT in men and women. Based on this healthy population, the ULN for ALT is 40 U/L for men and 28 U/L for women.
Figure 2.
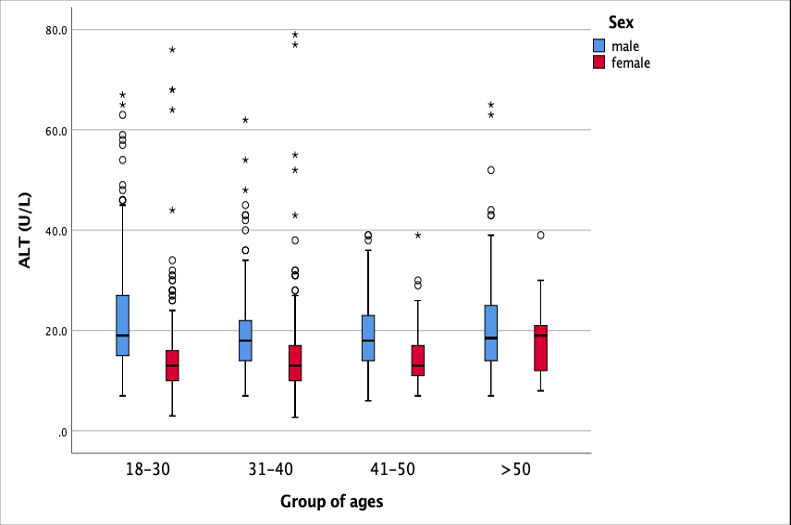
Distribution of serum ALT level across different age groups in healthy men and women (n=1261). ALT, alanine aminotransferase. * data points outside 95% CI
Table 3.
Serum ALT level of the healthy group distributed by sex and age group (n=1269)
| Age group | ALT (U/L) | P value* | |||||
| Male | Female | ||||||
| n | Median | IQR | n | Median | IQR | ||
| 18–30 | 310 | 19 | 15–27 | 249 | 13 | 10–16 | <0.001 |
| 31–40 | 181 | 18 | 14–22 | 281 | 13 | 10–17 | <0.001 |
| 41–50 | 55 | 18 | 14–23 | 85 | 13 | 11–17 | <0.001 |
| >50 | 86 | 19 | 14–25 | 22 | 19 | 12–21 | 0.39 |
*Mann-Whitney U test.
ALT, alanine aminotransferase.
Discussion
Defining the ULN value for blood chemical assays is paramount in clinical decision making. Inappropriate reference ranges can have a negative impact on early diagnosis, treatment and management of patients.23 In a large cohort of healthy subjects at working age, our study redefined the ULN for ALT levels in the Vietnamese population as 40 U/L in men and 28 U/L in women. Furthermore, we identified various risk factors for a higher ALT level (>40 U/L) in the Vietnamese population. Besides HBsAg positivity, factors related to ALT >40 U/L included high BMI (≥23 kg/m2), high cholesterol (≥5.2 mmol/L), high triglycerides (≥1.7 mmol/L) and the presence of fatty liver on abdominal ultrasound. These risk factors have been thoroughly defined in line with obesity, metabolic syndrome, fatty liver and steatosis hepatitis.24 25 A multiethnic cohort study of 392 obese adolescents (14–21 years old and BMI greater than the 85% percentile) revealed an association between modest ALT elevation and metabolism disorders, especially of glucose and lipids.26 Moreover, the growing risk of non-alcoholic fatty liver disease and obesity is commonly diagnosed from abnormal liver function tests.5 27
Male sex significantly contributed to higher ALT in this study (OR=4.2, 95% CI 3.4 to 5.5, p<0.001). In fact, as factors related to high ALT were excluded, the proportion of men in the healthy population descended from 76.3% of overall participants to 49.7% of the healthy population. Our finding is consistent with studies in Taiwan, Japan and Iran.4 8 28 The drinking habit of Vietnamese men might have contributed to this higher ALT level. Unfortunately, data on alcohol intake were not collected on medical health check-up. Age younger than 40 years old significantly contributed to an increased ALT in this study (p<0.001). This finding is inconsistent with studies from Taiwan, Japan and Korea.4 5 16 Elinav et al29 had reported that ALT level increased until the age of 40–50 years and decreased thereafter. The age-related fluctuation and other social factors such as alcohol consumption in young men should be investigated further. Overall, the underlying mechanism beyond age-related changes in ALT remains unclear.
Higher diastolic blood pressure was identified as an independent risk factor for higher ALT. Similar result was reported in two other Asian large-scale studies.4 28 Although the underlying cause remains unclear for this correlation, release of cardiovascular markers is related to increased ALT level in asymptomatic subjects.30 Therefore, various dyslipidaemias, which are also known risk factors for hypertension, might be associated with higher ALT. Further analysis that incorporates more confounding factors is required to clarify the association of high diastolic blood pressure with higher ALT level.
Interestingly, after excluding subjects with risk factors for higher ALT level, 3.3% (30 men, 11 women) of our healthy reference group still had a high ALT level of >40 U/L for undefined causes. Possible explanations include alcohol consumption or drug-induced liver injury. Moreover, drinking habits may explain the large number of healthy men with higher ALT compared with healthy women.
The 95th percentile of ALT level (36 U/L) for all healthy participants in our study was similar to the accepted conventional values (<40 U/L). We found eight anti-HCV (+) patients in a healthy population where, after exclusion, the ULN for ALT levels constantly remained at 36 U/L for the healthy population and at 28 U/L for the female healthy population. Moreover, this value slightly decreased from 42 U/L to 40 U/L in the male healthy population. However, comparing our ULN for men (40 U/L) and women (28 U/L) with those reported in several previous studies, there is a varying degree of agreement. The lower female ULN value in our study was approximately similar to other studies worldwide. For example, in Italian blood donors, the ULN for ALT was 30 U/L in men and 19 U/L in women.10 Another study in the USA involving 3747 subjects (negative HCV RNA and hepatitis B surface antigen, low alcohol consumption, no evidence of diabetes, normal BMI and waist circumference) reported the ULN for ALT level as 29 U/L for men and 22 U/L for women.31 Similarly, a study of a healthy reference Taiwanese population reported even lower ULN for both sexes, where the ULN was 21 IU/L for men and 17 IU/L for women.28 On the other hand, other studies had relatively more similar ULN to our results. In a Japanese study of 3508 healthy subjects, the ULN for ALT, defined as the 90th percentile of the ALT level, was 36 U/L for men and 27 U/L for women.4 Similarly, in a Korean cross-sectional study of 411 240 blood donors, the ULN for ALT was 34 U/L in men and 24 U/L in women.16 In addition, in another study of the Chinese Han population which included 13 637 adults after exclusion of any subjects with fatty liver, chronic liver disease, chronic alcohol consumption, HBV, HIV or HCV infection or potentially hepatotoxic medications use, the ULN for ALT from the normal group was 35 U/L in men and 23 U/L in women.32 Studies have found a significant correlation between gender and ALT level; healthy women have lower level of ALT which remained constant throughout their life, while men experience a mild increase until the fifth decade of their life and a gradual decline afterwards. Ultimately it is recommended that both clinicians and laboratories be cautious when interpreting and defining the optimal normal level of serum ALT.15 33 Based on the female ULN for ALT of 28 U/L, we can classify 9.5% more participants with risk factors (16.6% vs 7.1%) that should be screened for liver injury. Further cohort studies are recommended to confirm the validity of this ULN value and identify the appropriate ULN for diagnosis of liver injury in women. In conclusion, we report the new ULN value for ALT is 40 U/L in men and 28 U/L in women in the Vietnamese population. Although we cannot make direct comparisons of our results with those of other studies due to physical, ethnic and lifestyle differences, our results are relatively consistent with other studies in Asia, particularly in women.
While our newly suggested thresholds of ULN for ALT levels might accelerate identification and earlier diagnosis of unhealthy subjects, particularly in women, prospective studies that consider ethnicity and lifestyle factors are required to confirm the new ULN value and prevent overdiagnosis of liver diseases, unnecessary medical investigation costs and personal anxiety, particularly in male patients.
Footnotes
Contributors: NTCH and PTLH developed the idea and conceived the study. NTCH, PTLH and NTT developed the protocol. NTT obtained the ethical approval. NTT, ADNT and HLT recruited patients. SK, NTCH, HNT and PTLH analysed the data and interpreted the results. SK, TTM, GMS and KI drafted the manuscript with all the authors. PTLH, HNT, NTCH and SK edited the final manuscript. HNT and PTLH approved the final version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article.
Ethics statements
Patient consent for publication
Obtained.
Ethics approval
This study involves human participants and was approved by the Ethics Board of Ho Chi Minh City Medicine and Pharmacy University (no 174/ĐHYD-HĐĐĐ, on 19 April 2018). The study complied with the standards of the Declaration of Helsinki. Participants gave informed consent to participate in the study before taking part.
References
- 1.Suciu A, Abenavoli L, Pellicano R, et al. Transaminases: oldies but goldies. A narrative review. Minerva Gastroenterol Dietol 2020;66:246–51. 10.23736/S1121-421X.20.02660-4 [DOI] [PubMed] [Google Scholar]
- 2.Kallai L, Hahn A, Roeder V, et al. Correlation between histological findings and serum transaminase values in chronic diseases of the liver. Acta Med Scand 1964;175:49–56. 10.1111/j.0954-6820.1964.tb00549.x [DOI] [PubMed] [Google Scholar]
- 3.Pratt DS, Kaplan MM. Evaluation of abnormal liver-enzyme results in asymptomatic patients. N Engl J Med 2000;342:1266–71. 10.1056/NEJM200004273421707 [DOI] [PubMed] [Google Scholar]
- 4.Tanaka K, Hyogo H, Ono M, et al. Upper limit of normal serum alanine aminotransferase levels in Japanese subjects. Hepatol Res 2014;44:1196–207. 10.1111/hepr.12293 [DOI] [PubMed] [Google Scholar]
- 5.Chen C-H, Huang M-H, Yang J-C, et al. Prevalence and etiology of elevated serum alanine aminotransferase level in an adult population in Taiwan. J Gastroenterol Hepatol 2007;22:1482–9. 10.1111/j.1440-1746.2006.04615.x [DOI] [PubMed] [Google Scholar]
- 6.Jamali R, Pourshams A, Amini S, et al. The upper normal limit of serum alanine aminotransferase in Golestan Province, northeast Iran. Arch Iran Med 2008;11:602–7. [PubMed] [Google Scholar]
- 7.Kariv R, Leshno M, Beth-Or A, et al. Re-evaluation of serum alanine aminotransferase upper normal limit and its modulating factors in a large-scale population study. Liver Int 2006;26:445–50. 10.1111/j.1478-3231.2006.01197.x [DOI] [PubMed] [Google Scholar]
- 8.Mohamadnejad M, Pourshams A, Malekzadeh R, et al. Healthy ranges of serum alanine aminotransferase levels in Iranian blood donors. World J Gastroenterol 2003;9:2322–4. 10.3748/wjg.v9.i10.2322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dufour DR, Lott JA, Nolte FS, et al. Diagnosis and monitoring of hepatic injury. I. performance characteristics of laboratory tests. Clin Chem 2000;46:2027–49. 10.1093/clinchem/46.12.2027 [DOI] [PubMed] [Google Scholar]
- 10.Prati D, Taioli E, Zanella A, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med 2002;137:1–10. 10.7326/0003-4819-137-1-200207020-00006 [DOI] [PubMed] [Google Scholar]
- 11.Kim BK, Han K-H, Ahn SH. "Normal" range of alanine aminotransferase levels for Asian population. J Gastroenterol Hepatol 2011;26:219–20. 10.1111/j.1440-1746.2010.06603.x [DOI] [PubMed] [Google Scholar]
- 12.Sheth SG, Gordon FD, Chopra S. Nonalcoholic steatohepatitis. Ann Intern Med 1997;126:137–45. 10.7326/0003-4819-126-2-199701150-00008 [DOI] [PubMed] [Google Scholar]
- 13.Angulo P, Keach JC, Batts KP, et al. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology 1999;30:1356–62. 10.1002/hep.510300604 [DOI] [PubMed] [Google Scholar]
- 14.Daniel S, Ben-Menachem T, Vasudevan G, et al. Prospective evaluation of unexplained chronic liver transaminase abnormalities in asymptomatic and symptomatic patients. Am J Gastroenterol 1999;94:3010–4. 10.1111/j.1572-0241.1999.01451.x [DOI] [PubMed] [Google Scholar]
- 15.Piton A, Poynard T, Imbert-Bismut F, et al. Factors associated with serum alanine transaminase activity in healthy subjects: consequences for the definition of normal values, for selection of blood donors, and for patients with chronic hepatitis C. Hepatology 1998;27:1213–9. 10.1002/hep.510270505 [DOI] [PubMed] [Google Scholar]
- 16.Kang HS, Um SH, Seo YS, et al. Healthy range for serum ALT and the clinical significance of "unhealthy" normal ALT levels in the Korean population. J Gastroenterol Hepatol 2011;26:292–9. 10.1111/j.1440-1746.2010.06481.x [DOI] [PubMed] [Google Scholar]
- 17.Zhang P, Wang C-Y, Li Y-X, et al. Determination of the upper cut-off values of serum alanine aminotransferase and aspartate aminotransferase in Chinese. World J Gastroenterol 2015;21:2419–24. 10.3748/wjg.v21.i8.2419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tran HT-T, Ushijima H, Quang VX, et al. Prevalence of hepatitis virus types B through E and genotypic distribution of HBV and HCV in Ho Chi Minh City, Vietnam. Hepatol Res 2003;26:275–80. 10.1016/S1386-6346(03)00166-9 [DOI] [PubMed] [Google Scholar]
- 19.Nguyen VT-T, McLaws M-L, Dore GJ. Highly endemic hepatitis B infection in rural Vietnam. J Gastroenterol Hepatol 2007;22:2093–100. 10.1111/j.1440-1746.2007.05010.x [DOI] [PubMed] [Google Scholar]
- 20.WHO Expert Consultation . Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157–63. 10.1016/S0140-6736(03)15268-3 [DOI] [PubMed] [Google Scholar]
- 21.Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American gastroenterological association, American association for the study of liver diseases, and American College of gastroenterology. Gastroenterology 2012;142:1592–609. 10.1053/j.gastro.2012.04.001 [DOI] [PubMed] [Google Scholar]
- 22.Jellinger PS, Handelsman Y, Rosenblit PD, et al. American association of clinical endocrinologists and American College of endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract 2017;23:1–87. 10.4158/EP171764.APPGL [DOI] [PubMed] [Google Scholar]
- 23.Lu Y, Wang Q, Yu L, et al. Revision of serum ALT upper limits of normal facilitates assessment of mild liver injury in obese children with non-alcoholic fatty liver disease. J Clin Lab Anal 2020;34:e23285. 10.1002/jcla.23285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Petta S, Amato MC, Di Marco V, et al. Visceral adiposity index is associated with significant fibrosis in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther 2012;35:238–47. 10.1111/j.1365-2036.2011.04929.x [DOI] [PubMed] [Google Scholar]
- 25.Anty R, Iannelli A, Patouraux S, et al. A new composite model including metabolic syndrome, alanine aminotransferase and cytokeratin-18 for the diagnosis of non-alcoholic steatohepatitis in morbidly obese patients. Aliment Pharmacol Ther 2010;32:1315–22. 10.1111/j.1365-2036.2010.04480.x [DOI] [PubMed] [Google Scholar]
- 26.Burgert TS, Taksali SE, Dziura J, et al. Alanine aminotransferase levels and fatty liver in childhood obesity: associations with insulin resistance, adiponectin, and visceral fat. J Clin Endocrinol Metab 2006;91:4287–94. 10.1210/jc.2006-1010 [DOI] [PubMed] [Google Scholar]
- 27.Clark JM, Brancati FL, Diehl AM. Nonalcoholic fatty liver disease. Gastroenterology 2002;122:1649–57. 10.1053/gast.2002.33573 [DOI] [PubMed] [Google Scholar]
- 28.Wu W-C, Wu C-Y, Wang Y-J, et al. Updated thresholds for serum alanine aminotransferase level in a large-scale population study composed of 34 346 subjects. Aliment Pharmacol Ther 2012;36:560–8. 10.1111/j.1365-2036.2012.05224.x [DOI] [PubMed] [Google Scholar]
- 29.Elinav E, Ben-Dov IZ, Ackerman E, et al. Correlation between serum alanine aminotransferase activity and age: an inverted U curve pattern. Am J Gastroenterol 2005;100:2201–4. 10.1111/j.1572-0241.2005.41822.x [DOI] [PubMed] [Google Scholar]
- 30.Siddiqui MS, Sterling RK, Luketic VA, et al. Association between high-normal levels of alanine aminotransferase and risk factors for atherogenesis. Gastroenterology 2013;145:1271–9. 10.1053/j.gastro.2013.08.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ruhl CE, Everhart JE. Upper limits of normal for alanine aminotransferase activity in the United States population. Hepatology 2012;55:447–54. 10.1002/hep.24725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zheng M-H, Shi K-Q, Fan Y-C, et al. Upper limits of normal for serum alanine aminotransferase levels in Chinese Han population. PLoS One 2012;7:e43736. 10.1371/journal.pone.0043736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wayne P. Clinical and laboratory Standards Institute. How to define and determine reference intervals in the clinical laboratory: Approved guideline. CLSI Document 2000:C28–A2. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article.


