Abstract
Objective
To identify factors associated with better or poorer self-reported health status in New Zealand military Veterans.
Design
A cross-sectional survey.
Participants
The participants of interest were the 3874 currently serving Veterans who had been deployed to a conflict zone, but all Veterans were eligible to participate.
Study variables
The EQ-5D-5L, asking about problems across five dimensions (mobility, self-care, usual activities, pain or discomfort and anxiety or depression), with five levels of severity (eg, no, slight, moderate, severe or extreme problems), also containing a Visual Analogue Scale (EQ-VAS) to self-assess health state, scaled from 0 (worst) to 100 (best) imagined health.
Hypothetical relationships with better health were positive social support, sleep and psychological flexibility; with poorer health, post-traumatic stress, exposure to psychological trauma, distress and hazardous drinking.
Results
The EQ5-D-5L was completed by 1767 Veterans, 1009 serving, a response rate of 26% from that group, 1767 completing the EQ5-D, 1458 who had deployed, 288 who had not and the 21 who did not provide deployment data. Of these, 247 were not used in the analysis due to missing values in one or more variables, leaving 1520 for analysis.
A significantly higher proportion of Veterans reported ‘any problems’ rather than ‘no problems’ with four EQ-5D dimensions: mobility, self-care, usual activities and pain or discomfort, but no difference in anxiety or depression. Age, length of service, deployment, psychological flexibility and better sleep quality were associated with higher EQ-VAS scores; distress with lower EQ-VAS scores.
Conclusion
In this sample of New Zealand Veterans, psychological flexibility and good sleep are associated with better self-rated health, and distress and poor sleep with diminished health. These factors might be used as sentinel health indicators in assessing Veteran health status, and cognitive–behavioural therapy encompassing these domains may be useful in improving the health of New Zealand Veterans.
Keywords: epidemiology, occupational & industrial medicine, health & safety, risk management, mental health, musculoskeletal disorders
Strengths and limitations of this study.
Many studies of Veterans have focused on adverse outcomes, but we have been able to focus on a holistic measure of ‘health’.
The study was sufficiently powered to detect important relationships indicating opportunities for intervention.
The exact response rate is unknown, and sampling bias may be a limitation.
The cross-sectional design means that we cannot explore cause and effect relationships.
Introduction
The three major events in the military life course are entry to military service, deployment on active service and transition back to civilian life. On entry, soldiers, sailors and air personnel are subject to a selection process to ensure, as far as possible, good physical and mental health, giving rise to the ‘healthy soldier effect,’ with service personnel being, on average, healthier than the general population.1 However, the physical and psychological stressors of military service have been found to erode this effect.2
The physical stressors have a particular impact on the lower limb, with load carriage, high intensity training and the design of footwear being implicated in injury causation.3 A military career also increases opportunities for psychological trauma, and post-traumatic stress disorder (PTSD) has been identified as the ‘signature injury’ of United States service men and women deployed to Afghanistan and Iraq.4
A focus on adverse health events in the literature5 means that well-being is relatively overlooked. In the long run, military service has been found to have positive effects.6 7 Good health after service does, however, depend on the success of the ‘military civilian transition’, a complex process for which models have been developed.8 Health problems developed in service, difficulty in assuming a post-service identity and many other factors contribute to health and well-being outcomes.8 In New Zealand, military Veterans can only access assistance from New Zealand Veteran’s Affairs (NZVA) if they have undertaken ‘qualifying operational service’ as defined by the Veteran Support Act 2014,9 thus being Veterans in a legal sense. NZVA support some 12 000 Veterans, with an average age of 80 years, 5000 being actively case managed.10 The majority will have seen operational service in Korea, Borneo, Malaya and Vietnam. Post-Vietnam, smaller numbers deployed on United Nations and other missions, but the tempo of operations rose with the deployment to Bosnia in 1992, and some 9000–10 000 ‘legal’ Veterans deployed between then and the withdrawal of New Zealand troops from Afghanistan in 2021. The Ministerial Veteran’s Health Advisory Panel, established under the Veteran Support Act, are specifically charged with funding research on this ‘contemporary Veteran’ group, NZVA acknowledging that they ‘have had different experiences, and have different needs, compared with the older veterans. They are likely to have served in a number of deployments during their career, and come to us with more complex health issues.’10
The aims of this study were therefore to describe self-reported health among these Veterans, and identify factors associated with better or poorer health.
Veteran and public involvement
The Ministerial Veterans Health Advisory Panel10 commissioned the study and advised on the design. We also formed a steering group with representatives from the New Zealand Defence Force (NZDF), NZVA, the Royal New Zealand Returned and Services Association (RSA)11 and No Duff,12 a charity providing first response support to Veterans and their families. We also consulted with the Ngāi Tahu Research Consultation Committee in order to assess the importance of the project to Māori, New Zealand’s indigenous population. During consultation, we undertook to inform the Veteran community before releasing the results, to which end a link to the paper will be posted on the military social media sites where the study was advertised, and to give all NZ Veterans, defined as anyone who had served in the military, an opportunity to participate. Participants were not recruited as patients.
Methods
Participants
Potential participants were currently serving Veterans, as indicated by holding the New Zealand Operational Service Medal at the time of the survey, a total of 3874 personnel at that time; retired ‘legal’ Veterans in the community; and Veterans who had served, but had not deployed to a conflict. Data were collected via an online survey, a postal version being available on request. There is no comprehensive Veteran registry, however in July 2018, a link to the online questionnaire was sent by email to the 3874 currently serving regular and reserve NZDF members registered on the NZDF email system who were ‘legal Veterans’, as indicated by holding the New Zealand Operational Service Medal. An introductory message and link to the questionnaire were also presented on the NZDF ‘intranet landing page’, a secure internal webpage from which all regular force personnel can access relevant work-related content, tools and resources. Retired military personnel were invited to participate through posters distributed to reserve units and the 43 local social clubs identified by the RSA National Office to be ‘Veteran active.’ Paper questionnaires with return postage envelopes were made available at these sites. Announcements were also made on military social media pages, and both retired and currently serving personnel were invited to participate through an announcement on the NoDuff website. The questionnaire was available for completion from June to December 2018.
Questionnaire
Criterion variable
Self-rated health status was assessed using the EuroQol 5D-5L (EQ-5D-5L),13 a short questionnaire asking about the respondent’s health across five dimensions: mobility, self-care, usual activities, pain or discomfort and anxiety or depression, with response options ranging from (eg) ‘no problems’, to ‘extreme problems’. For each dimension, participants were categorised as having ‘any problems’ if they selected any response other than ‘no problems’.
Additionally, the EuroQol Visual Analogue Scale (EQ-VAS) asks the respondent to mark on a vertical VAS how good or bad their health is today, where the endpoints are labelled ‘the best health you can imagine’ (score of 100) and ‘the worst health you can imagine’ (score of 0).
Independent variables
Demographic characteristics included age, sex, ethnicity, service years and past deployment on operational service (yes/no). Ethnicity prioritisation was adopted,14 whereby participants with multiple responses were assigned to one of the categories, in the order of Māori, Pacific Peoples, other and European.
Symptoms of PTS were assessed using the PTSD checklist-military version (PCL-M).15 The PCL-M includes 17 items that ask about Diagnostic and Statistical Manual of Mental Disorders version IV (DSM-IV) symptoms of PTS related to stressful military experiences, with response options ranging from 1 ‘not at all’ to 5 ‘extremely’. A total symptom severity score is calculated by summing responses to each option (range=17–85). While scores of 30–35 indicate significant PTS symptomology and probable cases of PTSD, scores of ≥45 indicate a presumptive PTSD diagnosis.16
General psychiatric morbidity was assessed using the 12-item general health questionnaire (GHQ-12),17 scored using a four point scale (0–3) and summing the 12 items to give a total score, with higher scores indicating elevated distress.
Social support was measured using the social provisions scale,18 with responses made on a four-point Likert-type scale ranging from 1 ‘strongly disagree’ to 4 ‘strongly agree’. The 24 items can be reduced to six subscales (attachment, social integration, reassurance of worth, reliable alliance, social guidance and opportunity for nurturance) or summed to create a total score, with greater scores indicating greater social support.
Alcohol use was measured using the audit alcohol consumption questions(AUDIT-C),19 scaled from 0 to 12. A score of 3+ for women and 4+ for men indicated potentially hazardous drinking behaviour.
Sleep quality was assessed with the sleep condition indicator (SCI),20 assessing insomnia as described in the DSM-V.21 The SCI consists of eight items rated from 0 to 4, the total scores being scaled to a range of 0–10, where higher scores represent better sleep.
Trauma exposure was assessed with the brief trauma questionnaire (BTQ),22 which captures past exposure to situations that were life-threatening or capable of producing serious injury.
Psychological flexibility was measured with the 10-item acceptance and action questionnaire version 2 (AAQ-II), designed as a measure of effectiveness in a particular mode of behavioural intervention, acceptance and commitment therapy.23 Items were answered on a 7-point scale, with options ranging from ‘never true’ to ‘always true’. The items were summed to obtain a total score (possible range 10–70), with higher scores indicative of greater psychological flexibility.
Statistical analyses
With respect to the calculation of summed scores, if only one item was missing for a particular measure then this was imputed with the mean of the remaining items; if more than one item was missing then the score was set to missing for that participant. Complete-case analysis was used in the remaining analyses. Z tests were used to compare the five dimensions of the EQ-5D-5L to the NZ population normative values.24
Univariate ordinary least-squares linear regression analyses assessed the strength of relationships between each independent variable and EQ-VAS scores, using robust standard errors to account for heteroscedasticity and calculating 95% CIs. Multivariable linear regression was then used to identify the role of the independent variables while adjusting for each other. None of the social support subscales were used in this multivariable model, instead using the social support total score. The model was built using backward variable selection with p<0.10 for variable retention, with the exceptions of age, sex, service years and deployment status which were retained as adjusting variables irrespective of p values. Cronbach’s α (Cα) was used to assess the internal consistency of the scales used.25 A value of alpha greater than 0.7 is considered adequate.26 Collinearity was assessed by calculating the Pearson correlation coefficient (r); if 0<r< 1 there is a positive linear trend.
Results
The EQ-5D-5L was completed by 1767 Veterans, 1009 who were serving (26% of that group), 458 who had retired, 288 who had not deployed and 21 who did not provide deployment data.
There are no reliable denominator data on retired and non-deployed Veterans in New Zealand.
To facilitate a complete case analysis, 247 replies were not used due to missing values in one or more variables, the final sample including 1520 individuals.
Online supplemental table 1 presents the EQ-VAS score according to the sample characteristics.
bmjopen-2021-056916supp001.pdf (95.9KB, pdf)
Figure 1 shows the proportion of EQ-5D-5L dimension responses reporting ‘any problem’ severity level other than ‘no problems’ in comparison to the New Zealand population normative values24 with table 1 showing the 95% CI’s and Z values.
Figure 1.
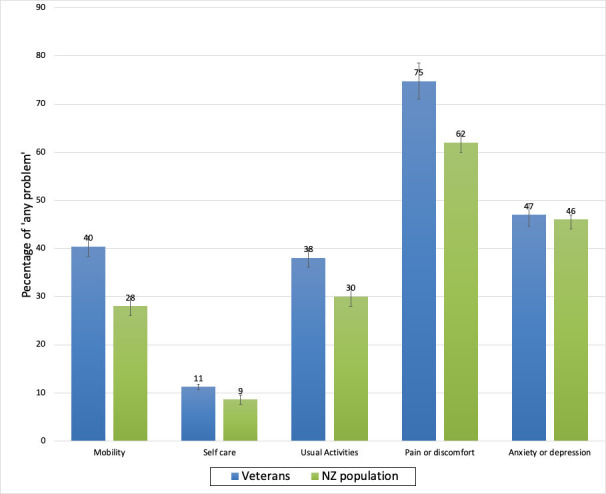
The proportion of Veterans reporting ‘any problem’ with each of the EQ-5D-5L dimension scores compared with the NZ population normative proportions. NZ, New Zealand.
Table 1.
Proportion of ‘any problem’ in EQ-5D-5L domains
| Domain | Veterans | NZ population | Z value (p) |
| Proportion (95% CI) | Proportion (95% CI) | ||
| Mobility | 0.40 (0.38 to 0.43) | 0.28 (0.26 to 0.30) | 8.5 (<0.0001) |
| Self-care | 0.11 (0.10 to 0.13) | 0.09 (0.07 to 0.10) | 2.8 (0.03) |
| Usual activities | 0.38 (0.35 to 0.40) | 0.30 (0.28 to 0.31) | 5.6 (<0.001) |
| Pain/discomfort | 0.75 (0.73 to 0.77) | 0.62 (0.60 to 0.63) | 9.0 (<0.0001) |
| Anxiety/depression | 0.47 (0.44 to 0.49) | 0.46 (0.44 to 0.48) | 0 (1.0) |
NZ, New Zealand.
The results of the univariate analysis are displayed in table 2. Here, for continuous characteristics, the regression coefficient (ß) represents the change in the mean EQ-VAS associated with one unit increase in the characteristic. For categorical characteristics, ß is the change in mean EQ-VAS scores compared with the referent category.
Table 2.
Univariate cross-sectional associations between variables and mean EQ-VAS scores for new Zealand veterans (N=1520)
| Characteristic | Ca* | N | ß | 95% CIs | P value |
| Age† | – | 1520 | −0.18 | −0.24 to −0.12 | <0.01 |
| Sex | |||||
| Female | – | 189 | Ref | ||
| Male | – | 1331 | −0.15 | −2.76 to 2.46 | 0.91 |
| Ethnicity | – |
|
|||
| NZ European | – | 1193 | Ref |
|
0.13 |
| Māori | – | 214 | 0.82 | −1.56 to 3.19 | |
| Other | – | 113 | −3.55 | −7.33 to 0.23 | |
| Service years* | – | 1520 | 0.19 | 0.11 to 0.28 | <0.01 |
| Deployment status | – | ||||
| Not deployed | – | 242 | ref | ||
| Deployed | – | 1278 | 6.56 | 3.85 to 9.26 | <0.01 |
| GHQ-12 score* | 0.89 | 1520 | −1.63 | −1.81 to −1.46 | <0.01 |
| Social support* | 1520 | 2.05 | 1.70 to 2.41 | <0.01 | |
| Attachment | 0.81 | 1520 | 2.47 | 2.02 to 2.92 | <0.01 |
| Social integration | 0.79 | 1520 | 2.49 | 2.08 to 2.91 | <0.01 |
| Reassurance of worth | 0.77 | 1520 | 2.39 | 1.97 to 2.82 | <0.01 |
| Reliable alliance | 0.81 | 1520 | 2.01 | 1.63 to 2.39 | <0.01 |
| Social guidance | 0.84 | 1520 | 0.83 | 0.40 to 1.25 | <0.01 |
| Opportunity fornurturance | 0.75 | 1520 | 0.53 | 0.44 to 0.61 | <0.01 |
| Social support total score | – | 1520 | 0.80 | 0.71 to 0.88 | <0.01 |
| Psychological flexibility* | 0.93 | 1520 | 3.56 | 3.18 to 3.95 | <0.01 |
| Sleep score* | 0.87 | <0.01 | |||
| AUDIT-C | 0.67 | 707 | Ref | ||
| Non-hazardous | 813 | 0.71 | −1.04 to 2.45 | 0.43 | |
| Hazardous | |||||
| Exposure to traumatic events | – | ||||
| Not exposed | 454 | Ref | |||
| Exposed | 1066 | −5.62 | −7.39 to 3.86 | <0.01 | |
| PTSD (PCL-M score)* | 1520 | −0.67 | −0.75 to −0.60 | <0.01 |
*Cronbach’s α.
†Scored as continuous variables, coefficient is per unit increase.
GHQ-12, 12-item General Health Questionnaire; NZ, New Zealand; PTSD PCL-M, Post-Traumatic Stress Disorder Checklist-Military Version.
Of the demographic variables, age was associated with lower EQ-VAS scores, length of service with higher scores. No relationships were apparent for sex or ethnicity. Positive coefficients, indicating better health with presence of the characteristic, were present for the dichotomous variable of deployment, where the mean EQ-VAS score for deployed Veterans was 6.56 VAS units higher than for the non-deployed. The largest negative associations were for exposure to traumatic events, with a mean EQ-VAS score 5.62 lower for those exposed compared with those not exposed. Distress, as measured by the GHQ-12, had a negative association with health state, as did PTSD as measured by the PCL-M. Positive associations with health state were found for psychological flexibility as measured by the AAQ-II, better sleep scores, the total social support score and the individual dimensions of support.
Table 3 shows the results from two multivariable models. The first model is adjusted for the other characteristics, with 12 variables included in the model. All effect sizes were reduced, and the social support and AUDIT-C scores were no longer associated.
Table 3.
Multivariable models of associations between variables and mean EQ-VAS scores for New Zealand veterans
| Characteristic | Adjusted model, N=1520 | Final model, N=1520 | ||||
| ß | 95% CI | P value | ß | 95% CI | P value | |
| Age (years)* | −0.15 | −0.21 to –0.10 | <0.01 | −0.16 | −0.22 to –0.10 | <0.01 |
| Sex | ||||||
| Female | Ref | Ref | ||||
| Male | 0.06 | −0.23 to 2.35 | 0.96 | 0.02 | −2.27 to 2.30 | 0.99 |
| Ethnicity | ||||||
| NZ European | Ref | 0.03 | Ref | 0.03 | ||
| Māori | 0.53 | −1.46 to 2.53 | 0.55 | −1.44 to 2.54 | ||
| Other | −4.04 | −7.12 to –0.95 | −4.07 | −7.16 to –0.99 | ||
| Service years* | 0.16 | 0.09 to 0.24 | <0.01 | 0.17 | 0.09 to 0.24 | <0.01 |
| Deployment status | ||||||
| Not deployed | Ref | Ref | ||||
| Deployed | 3.33 | 1.00 to 5.67 | 0.01 | 3.36 | 1.03 to 5.70 | 0.01 |
| GHQ−12 score* | −0.83 | −1.06 to –0.61 | <0.01 | −0.84 | −1.06 to –0.62 | <0.01 |
| Social support (SPS score)* | 0.02 | −0.07 to 0.11 | 0.65 | – | – | – |
| Psychological Flexibility Score (AAQ−II)* | 0.18 | 0.06 to 0.31 | 0.01 | 0.19 | 0.07 to 0.31 | <0.01 |
| Sleep score (SCI), Range 0–10* | 1.41 | 0.95 to 1.88 | <0.01 | 1.41 | 0.95 to 1.87 | <0.01 |
| AUDIT_C score | ||||||
| Non hazardous | Ref | |||||
| Hazardous | 0.37 | −1.05 to 1.79 | 0.61 | – | – | – |
| Exposure to traumatic events (BTQ) | ||||||
| Not exposed | Ref | Ref | ||||
| Exposed | −1.46 | −3.02 to 0.11 | 0.07 | −1.45 | −3.02 to 0.12 | 0.07 |
| PTSD (PCL−M score)* | −0.14 | −0.25 to –0.04 | 0.01 | −0.15 | −0.25 to –0.04 | 0.01 |
*Scored as continuous variables, coefficient is per unit increase.
GHQ-12, 12-item General Health Questionnaire; NZ, New Zealand; PTSD PCL-M, Post-Traumatic Stress Disorder Checklist-Military Version.
The final model involved backward variable selection setting a p value of 0.10, identifying a smaller subset of variables. Age, sex, service years and deployment status were retained in the model irrespective of their p values, thus adjusting for those variables. Social support and AUDIT-C hazardous drinking were not retained in this final model; other coefficients remaining essentially the same.
Discussion
Principal findings
With the exception of anxiety or depression, Veterans had a significantly greater proportion of ‘any problem’ responses in the EQ-5D-5L dimensions than the general population of New Zealand.
The final model identified variables independently associated with the EQ-VAS score: age, length of service, deployment, the GHQ score, psychological flexibility, the sleep score and exposure to traumatic events. The results make conceptual sense in that distress is associated with reduced EQ-VAS score, and psychological flexibility may have a modest protective effect. Age had a negative association, length of service being positive, most likely due to the ‘healthy soldier’ effect.1 Unusually, social support was dropped, however, the SPS was found to correlate significantly with the GHQ-12 (r=0.47), AAQ-II (r=0.56) and SCI scores (r=0.36), suggesting collinearity. Furthermore, there are known to be many other influences on health, including ‘social well-being’,5 financial status, personality and non-deployment related stressors,27 which we have not measured.
Strengths and weaknesses
Strengths of our study were the relatively large sample size, the inclusion of all Veterans, the assessment of ‘health’, infrequently investigated in Veteran populations, and the inclusion of New Zealand Veterans with a range of characteristics, including ‘deployed’ and ‘non-deployed’ Veterans. As a measure of health, the EQ-5D-5L dimensions and EQ-VAS ask about health on the day that respondents complete the questionnaire, the EQ-VAS end points being, respectively, the ‘best’ and ‘worst’ health they can imagine, so it is a holistic measure of health state.28
The response rate of 26% from serving Veterans, along with the unknown total number of Veterans, raises the question of bias, the direction of which is difficult to assess, as responses may be more likely from either Veterans with good or poor health. The healthy soldier effect is well known, service having a positive effect on well-being, with serving NZ Veterans having good access to primary healthcare through the military system, but the public healthcare system is the primary pathway to care for all Veterans, who are also covered by the ‘no fault’ accident compensation scheme for accidental injuries and occupational diseases.29 Deployed Veterans may be at an advantage, but are covered by NZVA only if their illness or injury is linked to a particular deployment, and the condition is listed on the ‘Statements of Principle’ of the Australian Repatriation Medical Authority.30 We also know that New Zealand Veterans tend to be of stoic disposition, so they might underestimate their health concerns,31 and there are likely to be other personal characteristics that we have not measured. We were, however, able to adjust for deployment status, which did have a positive association with health state. In the interest of minimising responder burden, we used brief scales, which might reduce construct validity. Distress, sleep, psychological flexibility and exposure to traumatic events are likely to be related, so collinearity was difficult to avoid. The effect was greatest for social support, but our finding does not mean that social support is of no importance to Veterans. The precision of the other coefficients may also have been affected. Finally, the cross-sectional design means that we cannot explore cause and effect, so recommendations for future interventions require additional support from longitudinal studies.
Comparison with other studies
We have previously reported factors associated with post-traumatic stress in this group,32 using the PCL-M. Factors associated with higher PCL-M scores were trauma exposure, older age, male gender and being of Māori ethnicity. Factors associated with lower PCL-M scores were greater length of service, psychological flexibility and better quality sleep. Using health as the outcome disclosed that Māori did not have poorer self-reported health compared with non-Māori, that deployment had a positive effect, and in the univariate models, all of the dimensions of social support were associated with improved health. The final model also included good sleep and psychological flexibility, providing most of the explanatory power in the model.
No other studies appear to have used the EQ-VAS as an outcome measure for Veteran health. Barrett et al33 examined well-being among participants in the 2000 Behavioural Risk Factor Surveillance System, describing health-related quality of life by sex and military status, active duty, reservists, Veterans, or no military service. Participants were asked to rate recent physical health, mental health and activity limitation. Active duty men were more likely than men without military service to report 14 or more days of activity limitation, pain and not enough rest in the past 30 days, the mobility and pain findings being similar to our sample. Notably, the predominant reason for medical discharge from the British Armed Forces was musculoskeletal problems.34
Contrary to our finding on deployment, there are reports indicating that non-deployed personnel retain better health than those who have been deployed. Díaz Santana et al35 carried out a cross-sectional survey of 60 000 US Veterans of Afghanistan and Iraq, with 20 563 responses. In contrast to our finding, mental quality of life scores were higher among the non-deployed group compared with the deployed group, though the deployed group reported higher physical quality of life scores compared with the non-deployed. Again in contrast, both mental and physical quality of life were lower among Veterans compared with US population norms.
Both positive and negative consequences of deployment have been described.7 36 In a study of Dutch Veterans,7 two out of three reported a positive effect of deployment on their quality of life at the time of the survey, this being related to positive feelings such as satisfaction or comradeship, but a few expressing emotions such as frustration or shame. As regards tangible effects,36 negative consequences included the military ‘chain of command’, being away from home, and deterioration of marital/significant other relationships. Positive influences include improved financial security, self-improvement and time to reflect.
We found sleep to be associated with better health, sleep difficulties being a common symptom for those with PTSD. McCarthy et al37 reported on the 3157 US military Veterans enrolled in the National Health and Resilience in Veterans Study, in which 27.6% reported poor sleep quality. Path analyses revealed significant associations between poor sleep, severity of PTSD, poorer mental and physical health functioning and lower overall quality of life.
Future directions
The results suggest that distress, psychological flexibility and sleep have an important relationship with self-rated health among Veterans in this study.
Reducing distress through the promotion of psychological flexibility might be possible, although our finding here must be subject to caution as several researchers argue that the AAQ-II may be measuring psychological distress and affect, rather than psychological inflexibility.38
Sleep in military personnel has been recognised as a ‘vital health behaviour’ for which policies and guidelines must be developed.39 Cognitive–behavioural therapy for insomnia is regarded as an effective ‘first-line’ treatment, and a brief intervention has been described for use in Australian general practice.40 Our final model showed that distress had a negative association with health, psychological flexibility a positive relationship, with sleep most likely related to both of these variables. It would seem important to screen for these conditions prior to transition from the military, as well as among retired Veterans, in order to provide targeted support. Further research is needed to examine the potential of cognitive–behavioural therapy to improve Veterans’ well-being.
Supplementary Material
Acknowledgments
We would like to thank Shane Harvey for his input into the initial design, Aidan Smith, previous research advisor to the NZDF, for steering us through the consents process, also the members of our steering group: COL Clare Bennett (NZDF); Ms Marti Eller (New Zealand Veterans Affairs); Mark Compain, Danny Nelson and Richard Terrill (RSA); and NoDuff representatives Aaron Wood and Lars Millar. Finally, a thank you to the New Zealand Veterans who took the time and effort to complete a rather tedious questionnaire. Kia Kaha.
Footnotes
Twitter: @DavidIMcbride, @ehwyeth
Contributors: All the authors have made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content; and final approval of the version to be published; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Specific responsibilites are:
Guarantor: DI. Investigation: AR, EW, SD, DS and DM. Methodology: AR, AS, DG, EW, SD, DM and DS. Project administration: AR. Resources: BdG. Software: BdG. Supervision: AS. Validation: AR. Visualisation: AR. Writing-original draft: DM, AS, DG, EW, SD and DS contributed to the rewrites and final draft.
Funding: This work was supported by a research grant from the Ministerial Veterans Health Advisory Panel, funded through the War Pensions Medical Research Trust Fund (grant number not applicable), also by Lottery Health (grant number LHR-2017-49146) and the Royal New Zealand Returned and Services Association (grant number not applicable).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. Data from this study is unsuitable for public deposition due to the privacy of participant data. Data are anonymised, but contain information on deployments (including location and duration), which could lead to some participants being identified. Furthermore, the participant information sheet, as required by the Northern B Health and Disability Ethics Committee, specifically contains the statement that ‘all study data would be kept strictly confidential to the research team.’ Qualified researchers may apply for data access with the research team at veterans.health@otago.ac.nz and/or hdecs@moh.govt.nz.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethics approval for the study was obtained from the Northern B Health and Disability Ethics Committee, reference 17NTB118.
References
- 1.McLaughlin R, Nielsen L, Waller M. An evaluation of the effect of military service on mortality: quantifying the healthy soldier effect. Ann Epidemiol 2008;18:928–36. 10.1016/j.annepidem.2008.09.002 [DOI] [PubMed] [Google Scholar]
- 2.Bollinger MJ, Schmidt S, Pugh JA, et al. Erosion of the healthy soldier effect in veterans of US military service in Iraq and Afghanistan. Popul Health Metr 2015;13:8. 10.1186/s12963-015-0040-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andersen KA, Grimshaw PN, Kelso RM, et al. Musculoskeletal lower limb injury risk in army populations. Sports Med Open 2016;2:22. 10.1186/s40798-016-0046-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13–22. 10.1056/NEJMoa040603 [DOI] [PubMed] [Google Scholar]
- 5.Oster C, Morello A, Venning A, et al. The health and wellbeing needs of veterans: a rapid review. BMC Psychiatry 2017;17:414. 10.1186/s12888-017-1547-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spiro A, Settersten RA, Aldwin CM. Long-Term outcomes of military service in aging and the life course: a positive Re-envisioning. Gerontologist 2016;56:5–13. 10.1093/geront/gnv093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duel J, Reijnen A. The long-term effects of military deployments and their relation with the quality of life of Dutch veterans. Mil Behav Health 2021;9:160–9. 10.1080/21635781.2020.1819488 [DOI] [Google Scholar]
- 8.Pedlar D, Thompson JM, Castro CA, Military Veteran reintegration . Military-to-civilian transition theories and frameworks. In: Castro C, Dursun S, eds. Military veteran reintegration, approach, management, and assessment of military veterans transitioning to civilian life. San Diego: Academic Press, 2019: 257p. [Google Scholar]
- 9.Veterans support act (NZ) 2014. Available: https://www.legislation.govt.nz/act/public/2014/0056/latest/whole.html [Accessed 28 Aug 2020].
- 10.Wellington: New Zealand Veteran’s Affairs; 2020 . New Zealand government. Briefing to the incoming Minister for veterans. Available: https://www.beehive.govt.nz/sites/default/files/2020-12/VeteranAffairs.pdf [Accessed 28 Aug 2020].
- 11.Royal New Zealand Returned and Services Association [internet]. Available: https://www.rsa.org.nz/ [Accessed 02 Feb 2022].
- 12.NoDuff. [Internet]. Available: https://www.noduff.org/ [Accessed 02 Feb 2022].
- 13.EuroQol Research Foundation . EQ-5D-5L User Guide[Internet]. Rotterdam: EuroQol Research Foundation; 2021. Available: https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/ [Accessed 02 Feb 2022].
- 14.Health Information Standards Organisation HISO 10001:2017. Ethnicity data protocols. Wellington: Ministry of health; 2017. [Google Scholar]
- 15.Weathers F, Litz B, Herman D, et al. Ptsd Checklist—Military version for DSM-IV. Boston, MA: National Center for PTSD, Behavioral Sciences Division, 1994. [Google Scholar]
- 16.U.S Department of Veterans Affairs . Using the PTSD checklist (PCL). Veterans Affairs National Center for PTSD 2012. [Google Scholar]
- 17.Goldberg DP. The detection of psychiatric illness by questionnaire. Maudsley monograph No. 21. London: Oxford University Press, 1972. [Google Scholar]
- 18.Barrera M, Ainlay SL. The structure of social support: a conceptual and empirical analysis. J Community Psychol 1983;11:133–43. [DOI] [PubMed] [Google Scholar]
- 19.Bush K, Kivlahan DR, McDonell MB, et al. The audit alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. ambulatory care quality improvement project (ACQUIP). alcohol use disorders identification test. Arch Intern Med 1998;158:1789–95. 10.1001/archinte.158.16.1789 [DOI] [PubMed] [Google Scholar]
- 20.Espie CA, Kyle SD, Hames P, et al. The sleep condition indicator: a clinical screening tool to evaluate insomnia disorder. BMJ Open 2014;4:e004183. 10.1136/bmjopen-2013-004183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Psychiatric Association . Diagnostic and statistical manual of mental disorders (DSM-5). Fifth edition. Washington DC: American Psychiatric Association, 2013: 991p. [Google Scholar]
- 22.Schnurr PP, Spiro III A, Vielhauer MJ, et al. Trauma in the lives of older men: findings from the normative aging study. J Clin Geropsychol 2002;8:175–87. 10.1023/A:1015992110544 [DOI] [Google Scholar]
- 23.Bond FW, Hayes SC, Baer RA, et al. Preliminary psychometric properties of the acceptance and action Questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther 2011;42:676–88. 10.1016/j.beth.2011.03.007 [DOI] [PubMed] [Google Scholar]
- 24.Sullivan T, Hansen P, Ombler F, et al. A new tool for creating personal and social EQ-5D-5L value sets, including valuing 'dead'. Soc Sci Med 2020;246:112707. 10.1016/j.socscimed.2019.112707 [DOI] [PubMed] [Google Scholar]
- 25.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika 1951;16:297–334. 10.1007/BF02310555 [DOI] [Google Scholar]
- 26.Bland JM, Altman DG. Statistics notes: Cronbach’s alpha. BMJ 1997;314:572. 10.1136/bmj.314.7080.572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brooks SK, Greenberg N. Non-deployment factors affecting psychological wellbeing in military personnel: literature review. J Ment Health 2018;27:80–90. 10.1080/09638237.2016.1276536 [DOI] [PubMed] [Google Scholar]
- 28.Feng Y, Parkin D, Devlin NJ. Assessing the performance of the EQ-VAS in the NHS PROMs programme. Qual Life Res 2014;23:977–89. 10.1007/s11136-013-0537-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Accident Compensation Corporation . Homepage [Internet] Wellington: Accident Compensation Corporation; 2022. https://www.acc.co.nz/ [Accessed 16 Feb 2022].
- 30.Repatriation Medical Authority . Statements of Principle [Internet. Canberra ACT: Repatriation Medical Authority; 2022. http://www.rma.gov.au/sops/ [Accessed 16 Feb 2022]. [Google Scholar]
- 31.Austin G, Calvert T, Fasi N, et al. Soldiering on only goes so far: how a qualitative study on veteran loneliness in New Zealand influenced that support during COVID-19 lockdown. J Mil Veteran Fam Health 2020;6:60–9. 10.3138/jmvfh-CO19-0007 [DOI] [Google Scholar]
- 32.Richardson A, Gurung G, Samaranayaka A, et al. Risk and protective factors for post-traumatic stress among New Zealand military personnel: a cross sectional study. PLoS One 2020;15:e0231460. 10.1371/journal.pone.0231460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barrett DH, Boehmer TK, Boothe VL, Flanders WD, et al. Health-Related quality of life of U.S. military personnel: a population-based study. Mil Med 2003;168:941–7. 10.1093/milmed/168.11.941 [DOI] [PubMed] [Google Scholar]
- 34.Williamson V, Diehle J, Dunn R, et al. The impact of military service on health and well-being. Occup Med 2019;69:64–70. 10.1093/occmed/kqy139 [DOI] [PubMed] [Google Scholar]
- 35.Díaz Santana MV, Eber S, Barth S, et al. Health-Related quality of life among U.S. veterans of operation enduring freedom and operation Iraqi Freedom-Results from a population-based study. Mil Med 2017;182:e1885–91. 10.7205/MILMED-D-17-00020 [DOI] [PubMed] [Google Scholar]
- 36.Newby JH, McCarroll JE, Ursano RJ, et al. Positive and negative consequences of a military deployment. Mil Med 2005;170:815–9. 10.7205/MILMED.170.10.815 [DOI] [PubMed] [Google Scholar]
- 37.McCarthy E, DeViva JC, Norman SB, et al. Self-assessed sleep quality partially mediates the relationship between PTSD symptoms and functioning and quality of life in U.S. veterans: results from the National health and resilience in veterans study. Psychol Trauma 2019;11:869–76. 10.1037/tra0000436 [DOI] [PubMed] [Google Scholar]
- 38.Wolgast M. What does the acceptance and action questionnaire (AAQ-II) really measure? Behav Ther 2014;45:831–9. 10.1016/j.beth.2014.07.002 [DOI] [PubMed] [Google Scholar]
- 39.Troxel WM. Sleep in the military: promoting healthy sleep among U.S. Servicemembers. RAND Corporation, 2021. https://www.rand.org/content/dam/rand/pubs/research_reports/RR700/RR739/RAND_RR739.pdf [PMC free article] [PubMed] [Google Scholar]
- 40.Sweetman A, Zwar NA, Grivell N, et al. A step-by-step model for a brief behavioural treatment for insomnia in Australian general practice. Aust J Gen Pract 2021;50:287–93. 10.31128/AJGP-04-20-5391 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-056916supp001.pdf (95.9KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. Data from this study is unsuitable for public deposition due to the privacy of participant data. Data are anonymised, but contain information on deployments (including location and duration), which could lead to some participants being identified. Furthermore, the participant information sheet, as required by the Northern B Health and Disability Ethics Committee, specifically contains the statement that ‘all study data would be kept strictly confidential to the research team.’ Qualified researchers may apply for data access with the research team at veterans.health@otago.ac.nz and/or hdecs@moh.govt.nz.


