Abstract
Arthroscopic resection of symptomatic unfused tibial tubercle ossicles causing chronic anterior knee pain due to recalcitrant Osgood-Schlatter disease has been shown to be a reproducible arthroscopic technique. Although a number of other surgical techniques have been described, including ossicle excision and tubercle-plasty, drilling of the tibial tubercle, bone peg insertion to induce fusion, open excision of loose fragments, direct bursoscopic ossicle resection, and closing-wedge tubercle osteotomy, with varied outcomes, this technique offers a minimally invasive approach with low risk. Complications including injury to the patellar tendon and scarring of the anterior fat pad have been previously reported, but this approach can be performed with minimal fat pad debridement and direct visualization of the patellar tendon during all resections. This article presents a technique for arthroscopic resection and debridement of unfused ossicles in patients with chronic anterior knee pain due to Osgood-Schlatter disease by use of minimally invasive arthroscopic techniques that are used in standard knee arthroscopy and should be familiar to most arthroscopists.
Technique Video
Two-portal arthroscopic resection of symptomatic tibial tubercle ossicles in left knee of skeletally mature patient with recalcitrant Osgood-Schlatter disease. First, a 2-portal technique is used for diagnostic arthroscopy, with an anterolateral portal for viewing and an anteromedial portal for instrumentation. Subsequently, the portals are switched for the ossicle excision, with the anteromedial portal used for arthroscopic viewing and the anterolateral portal used for instrumentation.
Osgood-Schlatter disease (OSD) is a common cause of anterior knee pain in children, associated with growth spurts, peaking at the age of 12 to 15 years among boys and 10 to 12 years among girls.1 The male-to-female ratio is 4:1, and 30% f patients present with bilateral disease.1,2 Radiologic and cadaveric studies have led to the theory that OSD is caused by forceful contractions of the quadriceps muscles at the proximal tibial apophysis insertion, resulting in multiple small avulsion fractures.1 Pagenstert et al.3 noted that OSD is a traction apophysitis of the tibial tubercle due to repetitive extensor mechanism strain with resultant chronic avulsion of the secondary ossification center of the tibial tuberosity. Patients typically present with anterior knee pain, swelling, and possible prominence of the tibial tubercle.4 Most symptoms resolve once the patient has reached puberty and physeal closure occurs, but a subset of patients will continue to have chronic insertional patellar tendinopathy. Initial treatment usually involves decreased physical activity, formal physical therapy with specific stretching and strengthening protocols for the quadriceps and hamstring muscles, possible weight-bearing restrictions, and immobilization with a brace or cast.5,6 The goal is to reduce the traction strain on the extensor insertion.3,7,8 Unresolved symptoms are more commonly seen in active patients continuing to participate in competitive sports. In patients in whom conservative treatment fails, consideration of surgical treatment may be necessary when disabling symptoms persist. Different surgical approaches have included fragment excision, endoscopic debridement, needling, and drilling techniques. Debridement approaches involve removal of retained bone to eliminate the chronic mechanical patellar tendon (PT) irritation.9, 10, 11, 12, 13 Bony excision of the retained OSD lesion has been shown to be an effective treatment for resolution of persistent anterior knee pain, and this technique uses standard arthroscopic practices for safe, reproducible bone excision.
Surgical Technique
Video 1 presents a narrated demonstration of the 2-portal surgical technique for arthroscopic resection of symptomatic tibial tubercle ossicles for recalcitrant OSD, as described in this article.
Preoperative Evaluation and Surgical Indications
Preoperative assessment includes a history; physical examination; plain radiographs including anteroposterior, notch, lateral, and sunrise views; and magnetic resonance imaging to assess for the degree of involvement, tibial tubercle location and size, PT involvement with associated tendinopathy, and concomitant pathology. In addition to patellar instability, other causes of anterior knee pain should be excluded. Symptomatic unfused remnant ossicles in chronic OSD can usually be diagnosed with a physical examination and plain radiographs. However, magnetic resonance imaging is recommended to assess the integrity of the PT, evaluate for alternate causes of anterior knee pain, and determine the positioning of the bony fragment prior to arthroscopic resection. Larger intrasubstance fragments may require more extensive open debridement with possible PT insertional repair (Fig 1, Fig 2, Fig 3, Fig 4).
Fig 1.
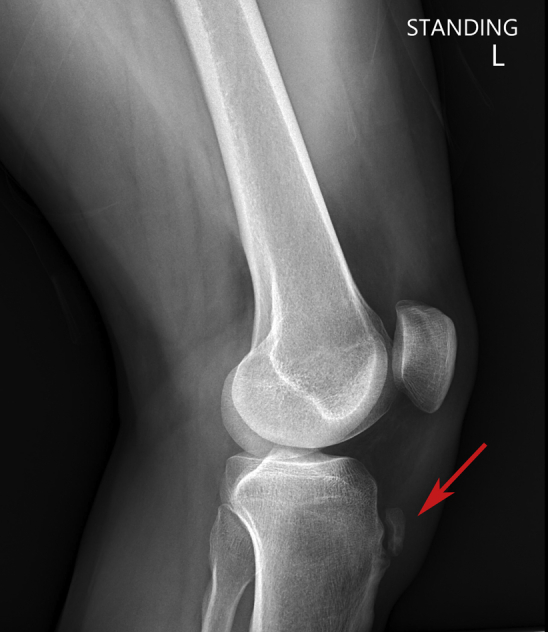
Plain radiographic lateral view left knee showing retained unfused ossicle (red arrow) at tibial tuberosity consistent with Osgood-Schlatter disease.
Fig 2.
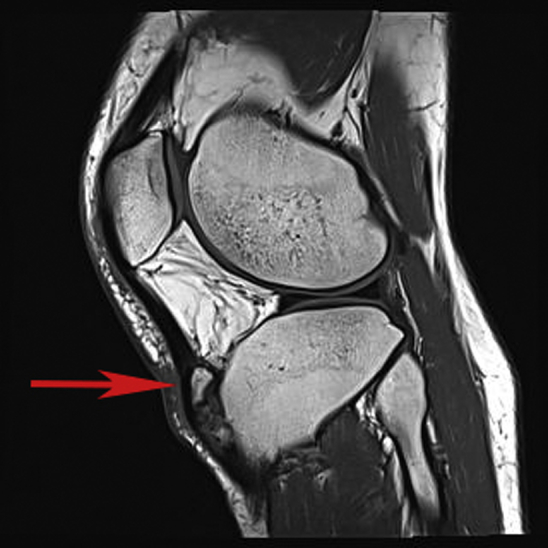
Sagittal T1 magnetic resonance image of left knee showing retained unfused ossicle (arrow) at patellar tendon insertion consistent with Osgood-Schlatter disease.
Fig 3.
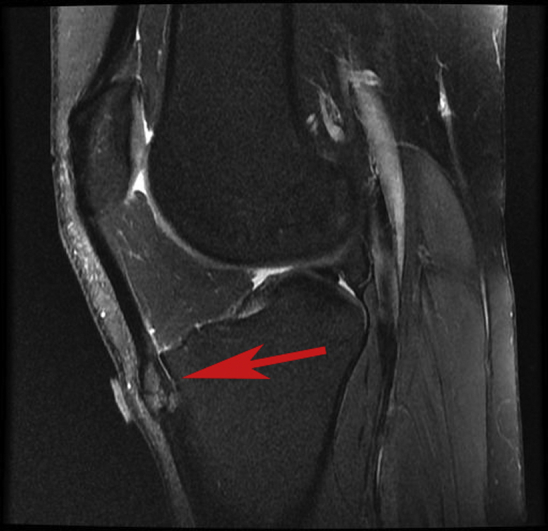
Sagittal T2 magnetic resonance image of left knee showing retained unfused ossicle (arrow) at patellar tendon insertion consistent with Osgood-Schlatter disease.
Fig 4.
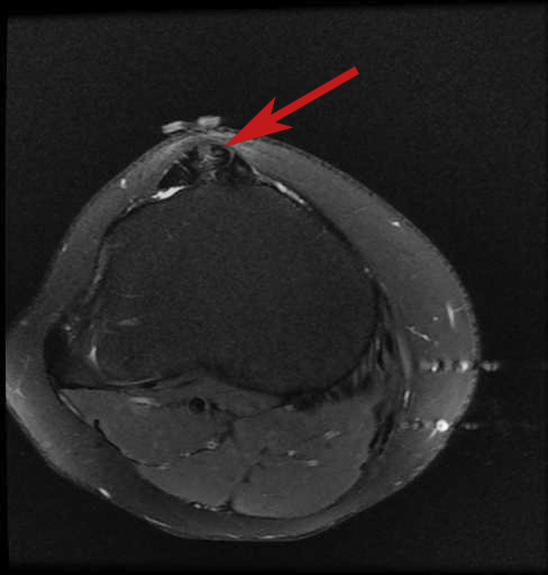
Axial T2 magnetic resonance image of left knee showing retained unfused ossicle (arrow) at patellar tendon insertion consistent with Osgood-Schlatter disease.
Although the procedure for excision of tibial tubercle ossicles with OSD can be considered an endoscopic approach, this technique is considered an arthroscopic approach owing to its access to the ossicles from within the joint. Indications for arthroscopic resection of ossicles for symptomatic OSD include patients in whom initial nonsurgical treatment has failed, including decreased physical activity, formal physical therapy with specific stretching and strengthening protocols for the quadriceps and hamstring muscles, possible weight-bearing restrictions, and immobilization with a brace or cast.5,6
Setup and Positioning
Typical anesthesia for arthroscopic resection of ossicles includes general anesthesia with a supplemental adductor canal block for additional postoperative pain control. After anesthesia and block induction, a standard knee examination with the patient under anesthesia is performed. The patient is positioned supine on the operating table with the operative lower extremity placed in a standard thigh leg holder with the foot of the bed dropped. The nonsurgical leg is held in an abduction stirrup to permit unimpeded motion of the operative leg with the nonoperative extremity well padded, particularly in the region of the peroneal nerve. A proximal thigh tourniquet is placed and inflated for the duration of the procedure with a pressure of 250 mm Hg, but its use is optional for the procedure. The fluoroscopic imager (Fluoroscan InSight-FD; Hologic, Bedford, MA) should be sterilely draped for later use and is accessed from the lateral side of the ipsilateral knee.
Arthroscopic Evaluation
Initial standard 2-portal diagnostic knee arthroscopy is performed. The anterolateral portal (ALP) and anteromedial portal (AMP) are infiltrated with the use of 0.25% bupivacaine without epinephrine. A standard 2-portal diagnostic arthroscopy is performed using an ALP for arthroscopy, created by an outside-in technique, and an AMP for instrumentation, created by spinal needle localization. The portals can be strategically placed to allow for ideal positioning for ease in ossicle excision depending on their locations. Concomitant pathology is addressed as needed.
Next, the portals are switched using the AMP for the arthroscope and the ALP for instrumentation because, in our experience, the ossicles tend to be more easily accessed from the lateral side (Fig 5). An arthroscopic 4.2- or 3.7-mm shaver (Merlin Cuda Shaver, pre-bent 15°; ConMed, Largo, FL) is used to minimally resect the infrapatellar fat pad, extending inferiorly from the inferior pole of the patella at the undersurface of the PT, with exquisite care taken to avoid any injury to the PT itself. As much of the fat pad is maintained to protect the undersurface of the PT but to allow adequate visualization of the ossicles. This is extended inferiorly to the proximal tibia, maintaining the inner meniscal ligament and avoiding the anterior cruciate ligament. Once the proximal tibial plateau is exposed in a centralized position, an arthroscopic shaver is used from the ALP to define the PT anteriorly, and this is avoided. A radiofrequency electrode (VAPR TriPolar 90 Suction Electrode; DePuy Synthes, Raynham, MA) is then used to expose the bony surfaces inferiorly and laterally.
Fig 5.

Operative positioning during arthroscopic resection of ossicles in left knee with Osgood-Schlatter disease using 2-portal technique, with anteromedial portal for arthroscopic viewing and anterolateral portal for instrumentation. The portals have been switched from the initial diagnostic arthroscopy, with the anterolateral portal used for arthroscopic viewing and the anteromedial portal used for instrumentation.
An arthroscopic shaver and ablator are subsequently used to dissect more distally and laterally. Simultaneously, fluoroscopic imaging is used with a lateral view, and spinal needle localization is performed to mark the superior border of the ossicle(s) (Fig 6). The surgeon excavates this area appropriately with the radiofrequency electrode, carefully avoiding the PT by pointing the tip posteriorly rather than anteriorly. Arthroscopic burrs, consisting of 3.5-mm round and oval unhooded burrs (Vortex Router, Two Flutes, and Spherical Bur; ConMed) (Fig 7, Fig 8, Fig 9), are then used to perform a complete resection of the ossicle under direct visualization. A 70° arthroscope and an arthroscopic probe are additionally used for visualization. Secondary visualization with fluoroscopic imaging should be performed to verify complete eradication (Fig 10). Copious irrigation of the joint should be performed using arthroscopic fluid to ensure no loose bodies or debris. If there is any evidence of ossicles within the PT, then consideration can be given to conversion to an open incision to resect additional intratendinous ossicles because this may require more vigorous dissection and potentially repair of the PT as needed to the native tibial tubercle with suture anchors.
Fig 6.

Needle localization of superior tip of ossicle using fluoroscopic imaging with lateral view. The needle can be simultaneously visualized arthroscopically to confirm its location.
Fig 7.
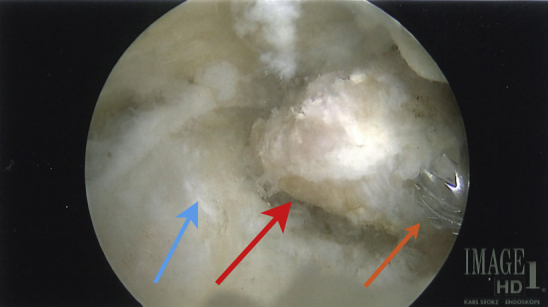
Identification of tibial tubercle ossicle during arthroscopic resection for recalcitrant Osgood-Schlatter disease in left knee using 2-portal technique. Viewing is performed through an anteromedial portal using a 70° arthroscope after arthroscopic shaver and radiofrequency electrode debridement, then looking inferiorly and lateral to the intact and protected patellar tendon (blue arrow). An anterolateral working portal is used to excise the ossicle (red arrow) with an arthroscopic burr (orange arrow) after skeletonization of the ossicle with a shaver and radiofrequency electrode directed away from the patellar tendon.
Fig 8.
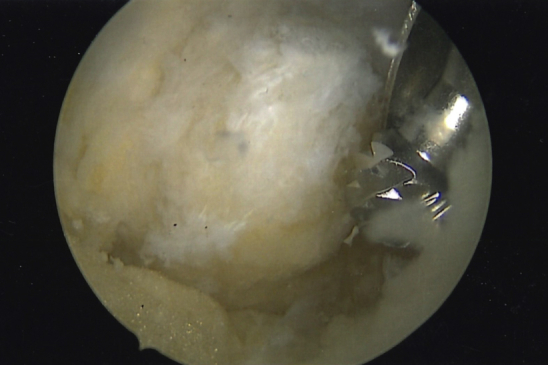
Arthroscopic burr beginning resection of Osgood-Schlatter disease ossicle in left knee with arthroscopic viewing through anteromedial portal and instrumentation through anterolateral portal. An arthroscopic 3.5-mm burr and unhooded burr are used to completely resect the retained tibial tubercle ossicle. The patellar tendon is visualized during resection to ensure that the tendon remains undamaged.
Fig 9.
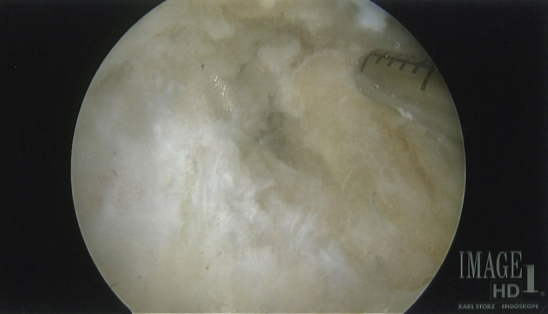
Arthroscopic post-resection image showing eradication of retained tibial tubercle ossicle with intact patellar tendon. Arthroscopic image of left knee with arthroscopic viewing through anteromedial portal and instrumentation through anterolateral portal.
Fig 10.

Post-resection lateral fluoroscopic image confirming complete elimination of tibial tubercle ossicle in knee with Osgood-Schlatter disease.
If desired, at the completion of the resection, the tourniquet can be deflated and the area can be checked for any bleeding about the resection and undergo cauterization with the radiofrequency electrode as needed. Arthroscopic fluid is drained from the knee, and the incisions are closed in standard fashion. The joint can be infiltrated with 0.25% bupivacaine with epinephrine as desired. Dressings are applied, and the operative lower extremity is placed in a hinged knee brace locked in extension.
Postoperative Rehabilitation
As long as no repair of the PT is needed, the patient is allowed full weight bearing with the knee in full extension and the brace locked until the first postoperative visit (1 week). The brace can then be unlocked for sitting with flexion as tolerated. Starting at week 2 or 3, the patient is allowed to discontinue using the brace with full weight bearing as tolerated. The patient is advised to avoid all resisted extension activities for 3 to 4 weeks. Physical therapy is initiated after the first postoperative visit to initiate active and passive quadriceps strengthening exercises. Low-dose aspirin is administered for 3 weeks for deep venous thrombosis prophylaxis.
Advantages and disadvantages of the procedure are summarized in Table 1. Pearls and pitfalls of the procedure are outlined in Table 2. The technique is shown in full in Video 1.
Table 1.
Advantages and Disadvantages of Arthroscopic Resection of Ossicles for Recalcitrant Osgood-Schlatter Disease
| Advantages |
| All-arthroscopic approach usually only requiring 2-portal technique |
| No special hardware required with typical shavers, burrs, and radiofrequency electrode use |
| Standard knee arthroscopy approach familiar to most knee arthroscopists |
| Prevention of need for transpatellar tendon approach that may violate patellar tendon and require repair |
| Possible initiation of quicker physical therapy protocol owing to less patellar tendon injury |
| Disadvantages |
| Approach not appropriate for large intra–patellar tendon ossicles |
| Approach not appropriate for concomitant patellar tendinopathy |
| Potential risk of over-resection of prepatellar fat pad |
Table 2.
Pearls and Pitfalls of Arthroscopic Bony Ossicle Resection in Patients With Osgood-Schlatter Disease
| Pearls |
| The surgeon should use a small fluoroscopic lateral view for ossicle identification and perform spinal needle placement at the proximal pole for localization of fragments during debridement. |
| A 70° arthroscope should be used as needed for better visualization. |
| The surgeon should switch portals during debridement and resection as needed for visualization. |
| Full resection of the bony ossicle should be confirmed with fluoroscopy. |
| The surgeon should always visualize the patellar tendon to ensure no damage during the procedure. |
| The surgeon should minimize fat pad debridement and stay on bone. |
| A combination of an arthroscopic radiofrequency electrode and shaver should be used for debridement. |
| The surgeon should ablate the soft tissues off of the ossicle prior to resection. |
| The surgeon should bear in mind that the ossicle tends to sit just posterolateral to the patellar tendon. |
| Pitfalls |
| If the patellar tendon is not visualized, there is a risk of tendon injury. |
| Larger fragments and intrasubstance fragments may require an open procedure and insertional patellar tendon repair. |
| Overly aggressive fat pad debridement can lead to anterior scarring and the potential for continued anterior knee pain. |
| Poorly placed anterolateral and anteromedial portals can restrict visualization. |
Discussion
As a result of recalcitrant OSD, the enlarged and prominent tibial tubercle, in addition to the ununited remnant ossicle after physeal closure, can cause bulging and tilting of the distal PT, which can lead to persistent anterior knee pain.3 Pagenstert et al.,3 who described a closing-wedge tubercle osteotomy approach to the prominent tibial tubercle, noted that isolated fragment excision with prominent debridement is risky because it may disintegrate the residual PT, potentially leading to rupture. Numerous other surgical options have been described in publications, including ossicle excision and tubercle-plasty, drilling of the tibial tubercle, bone peg insertion to induce fusion, open excision of loose fragments, and direct bursoscopic ossicle resection, with varied outcomes.10 An arthroscopic approach has been found to be beneficial compared with an open procedure owing to earlier postoperative recovery, no incisional scar over the anterior tibial tuberosity with the potential for persistent anterior pain, better cosmesis, and the ability to address other intra-articular pathology.14
The goals of surgical management of chronically painful OSD with retained ununited ossicles is to safely remove the offending bone, restore normal function, and allow a rapid return to full activity. Although numerous techniques, both arthroscopic and open, have been described, a gold-standard technique has not been defined. The described arthroscopic approach uses minimally invasive arthroscopic techniques that are used in standard knee arthroscopy and should be familiar to most arthroscopists. This arthroscopic approach for excision of the tibial tubercle ossicles offers a safe and reproducible method for unfused ossicle resection with direct visualization of the PT during all resections and radiographic confirmation during the procedure.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: M.J.R. receives support for attending meetings and/or travel from AANA and has a leadership or fiduciary role in AANA and Arthroscopy. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Two-portal arthroscopic resection of symptomatic tibial tubercle ossicles in left knee of skeletally mature patient with recalcitrant Osgood-Schlatter disease. First, a 2-portal technique is used for diagnostic arthroscopy, with an anterolateral portal for viewing and an anteromedial portal for instrumentation. Subsequently, the portals are switched for the ossicle excision, with the anteromedial portal used for arthroscopic viewing and the anterolateral portal used for instrumentation.
References
- 1.Weiler R., Ingram M., Wolman R. 10-Minute consultation. Osgood-Schlatter disease. BMJ. 2021;343:d4534. doi: 10.1136/bmj.d4534. [DOI] [PubMed] [Google Scholar]
- 2.Ross M.D., Villard D. Disability levels of college-aged men with a history of Osgood-Schlatter disease. J Strength Cond Res. 2003;17:659–663. doi: 10.1519/1533-4287(2003)017<0659:dlocmw>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 3.Pagenstert G., Wurm M., Gehmert S., Egloff C. Reduction osteotomy of the prominent tibial tubercle after Osgood-Schlatter disease. Arthroscopy. 2017;33:1551–1557. doi: 10.1016/j.arthro.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 4.Krause B.L., Williams J.P., Catterall A. Natural history of Osgood-Schlatter disease. J Pediatr Orthop. 1990;10:65–68. [PubMed] [Google Scholar]
- 5.Gholve P.A., Scher D.M., Khakharia S., Widmann R.F., Green D.W. Osgood Schlatter syndrome. Curr Opin Pediatr. 2007;19:44–50. doi: 10.1097/MOP.0b013e328013dbea. [DOI] [PubMed] [Google Scholar]
- 6.Baltaci G., Özer H., Tunay V.B. Rehabilitation of avulsion fracture of the tibial tuberosity following Osgood-Schlatter disease. Knee Surg Sports Traumatol Arthrosc. 2004;12:115–118. doi: 10.1007/s00167-003-0383-6. [DOI] [PubMed] [Google Scholar]
- 7.Frank J.B., Jarit G.J., Bravman J.T., Rosen J.E. Lower extremity injuries in the skeletally immature athlete. J Am Acad Orthop Surg. 2007;15:356–366. doi: 10.5435/00124635-200706000-00005. [DOI] [PubMed] [Google Scholar]
- 8.OrthoInfo, American Academy of Orthopaedic Surgeons Osgood-Schlatter disease (knee pain) https://www.orthoinfo.org/en/diseases--conditions/osgood-schlatter-disease-knee-pain/
- 9.Beyzadeoglu T., Inan M., Bekler H., Altintas F. Arthroscopic excision of an ununited ossicle due to Osgood-Schlatter disease. Arthroscopy. 2008;24:1081–1083. doi: 10.1016/j.arthro.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 10.Eun S.S., Lee S.A., Kumar R., et al. Direct bursoscopic ossicle resection in young and active patients with unresolved Osgood-Schlatter disease. Arthroscopy. 2015;31:416–421. doi: 10.1016/j.arthro.2014.08.031. [DOI] [PubMed] [Google Scholar]
- 11.DeBerardino T.M., Branstetter J.G., Owens B.D. Arthroscopic treatment of unresolved Osgood-Schlatter lesions. Arthroscopy. 2007;23:1127.e1–1127.e3. doi: 10.1016/j.arthro.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 12.El-Husseini T.F., Abdelgawad A.A. Results of surgical treatment of unresolved Osgood-Schlatter disease in adults. J Knee Surg. 2010;23:103–107. doi: 10.1055/s-0030-1267474. [DOI] [PubMed] [Google Scholar]
- 13.Pihlajamäki H.K., Visuri T.I. Long-term outcome after surgical treatment of unresolved Osgood-Schlatter disease in young men: Surgical technique. J Bone Joint Surg Am. 2010;92:258–264. doi: 10.2106/JBJS.J.00450. (suppl 1, pt 2) [DOI] [PubMed] [Google Scholar]
- 14.Circi E., Atalay Y., Beyzadeoglu T. Treatment of Osgood-Schlatter disease: Review of the literature. Musculoskelet Surg. 2017;101:195–200. doi: 10.1007/s12306-017-0479-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Two-portal arthroscopic resection of symptomatic tibial tubercle ossicles in left knee of skeletally mature patient with recalcitrant Osgood-Schlatter disease. First, a 2-portal technique is used for diagnostic arthroscopy, with an anterolateral portal for viewing and an anteromedial portal for instrumentation. Subsequently, the portals are switched for the ossicle excision, with the anteromedial portal used for arthroscopic viewing and the anterolateral portal used for instrumentation.
Two-portal arthroscopic resection of symptomatic tibial tubercle ossicles in left knee of skeletally mature patient with recalcitrant Osgood-Schlatter disease. First, a 2-portal technique is used for diagnostic arthroscopy, with an anterolateral portal for viewing and an anteromedial portal for instrumentation. Subsequently, the portals are switched for the ossicle excision, with the anteromedial portal used for arthroscopic viewing and the anterolateral portal used for instrumentation.


