Abstract
An unexpected increase in gastroenteritis cases was reported by healthcare workers on the KwaZulu-Natal Coast, South Africa, January 2017 with >600 cases seen over a 3-week period. A case–control study was conducted to identify the source and risk factors associated with the outbreak so as to recommend control and prevention measures. Record review identified cases and controls and structured-telephonic interviews were conducted to obtain exposure history. Stool specimens were collected from 20 cases along with environmental samples and both screened for enteric pathogens. A total of 126 cases and 62 controls were included in the analysis. The odds of developing gastroenteritis were 6.0 times greater among holiday makers than residents (95% confidence interval (CI) 2.0–17.7). Swimming in the lagoon increased the odds of developing gastroenteritis by 3.3 times (95% CI 1.06–10.38). Lagoon water samples tested positive for norovirus (NoV) GI.6, GII.3 and GII.6, astrovirus and rotavirus. Eleven (55%) stool specimens were positive for NoV with eight genotyped as GI.1 (n = 2), GI.5 (n = 3), GI.6 (n = 2), and GI.7 (n = 1). A reported sewage contamination event impacting the lagoon was the likely source with person-to-person spread perpetuating the outbreak. Restriction to swimming in the lagoon was apparently ineffective at preventing the outbreak, possibly due to inadequate enforcement, communication and signage strategies.
Key words: Diarrhoea, gastroenteritis, KwaZulu-Natal, lagoon, norovirus, recreational water, waterborne
Introduction
Globally, open water sources such as lakes, rivers, seas and lagoons provide communal recreational resources for swimming and other water sports. While serving as either official or unofficial recreation resources, rivers and lagoons are often also used for personal hygiene in low-resource settings [1]. Inadequate treatment of sewage effluent or leakage of sewage into these water sources leads to the introduction of common waterborne pathogens including enteric viruses [2]. Therefore, many open water sources may pose a considerable health risk to the population utilizing them [3].
A study in the Eastern Cape Province, South Africa (SA), detected rotaviruses (RVs) and enteroviruses in the Buffalo River as well as dams supplied by this river [4]. Enteroviruses, RVs and adenoviruses (AdVs) were also detected in the Umgeni River, KwaZulu Natal (KZN) Province. The majority of these viruses were confirmed through molecular characterisation to be of human origin, suggesting faecal contamination of the river [5].
Although many enteric viruses have been involved in waterborne outbreaks, norovirus (NoV) is a major concern. NoV was implicated in a waterborne gastroenteritis outbreak in China, due to probable sewage contamination of a drinking water well [6].
NoVs have been detected in several rivers in Gauteng [7] and a recent quantitative microbial risk assessment indicated a high risk of NoV infection when swimming in contaminated rivers [8]. These studies highlight the health risk posed by NoVs in open water sources in SA.
In SA, several factors contribute to surface water contamination. These include poor operational state of wastewater treatment infrastructure, inadequate capacity of wastewater treatment facilities especially in rapidly expanding informal settlements or poorly planned towns and insufficient monitoring for wastewater treatment compliance with available guidelines [9, 10].
On 5 January 2017, the Outbreak Response Unit (ORU) of the National Institute for Communicable Diseases (NICD), SA, was alerted to a high number of persons falling ill with gastrointestinal symptoms (diarrhoea and/or vomiting) on the coast of KZN Province. The alert from health authorities in the KZN Province indicated that between 14 December 2016 and 5 January 2017, 690 people presented with gastrointestinal symptoms at a private hospital on the KZN south coast. Over 600 cases were observed while 350 or less were expected for the period. Other surrounding health facilities, including public sector hospitals, did not observe this increase.
Based on the available information at the time, which included local newspaper and online articles that reported a sewage spillage into a nearby lagoon; the investigating team hypothesised that contamination of a coastal lagoon could have led to the outbreak. An epidemiological investigation was conducted to describe the extent of the outbreak, identify the source of the outbreak and identify associated risk factors so as to recommend control and prevention measures.
Materials and methods
Study setting
The outbreak occurred within an urban community on the south coast of KZN Province during December 2016 and January 2017. The community had an estimated population size of 26785 during the 2011 census [11]. However, the population can reportedly double during the festive seasons as inland residents travel to the coast, especially during Christmas holidays in December to January. Along the community beach, there is a lagoon which connects a local river to the Indian ocean (Fig. 1).
Fig. 1.
Satellite image of the beach front, showing the lagoon, beach and the river which connects to the lagoon, KZN, South Africa.
Study design
A case–control study was conducted, with a case defined as a person of any age who presented to the private hospital's emergency department between 19 December 2016 and 6 January 2017 with an acute onset of diarrhoea and/or vomiting. Controls were defined as a person of any age who presented at the same hospital during the same period with acute onset of respiratory illness or musculoskeletal problems, e.g. trauma.
Data collection
Epidemiological
Hospital patient records were reviewed to identify cases and controls. Due to time constraints of the visit, it was not possible to review patient files for all 760 cases; a decision was made to obtain data from between 30% and 50% of the cases who presented at the hospital between 19 December 2016 and 6 January 2017. With respect to the controls, information regarding the total number of persons presenting on the days between 19 December 2016 and 6 January 2017 was not known. A decision was then made to review 150 patient files of the controls without stratifying by day.
Structured telephonic interviews were conducted to collect the exposure history within the 5 days prior to onset of illness, from both cases and controls using a semi-structured investigation form. Cases and controls who could not be contacted telephonically were sent a Google Form (https://www.google.com/forms/about/) link, which allowed them to complete the investigation form electronically. The investigation form included questions on the demographics of participants, clinical symptoms (if present) and laboratory test results (if known). In addition, questions on exposure variables such as swimming in the sea/lagoon/rivers, ingestion of water and food items from different sources were included.
Laboratory investigations
Clinical specimens
Twenty acute phase stool specimens were collected from cases presenting to the hospital between 6 and 10 January 2017 and sent cooled to the Centre for Enteric Diseases (CED), NICD, for testing. Nucleic acid was extracted from stool specimens with the QIAamp Fast DNA Stool kit (Qiagen, Hilden, Germany) using a modified method and screened using a custom Taqman Array card (Thermo Fischer, Carlsblad, CA, USA) with Ag-Path-ID One-Step RT-PCR reagents [12–14]. The arrays screened for viruses (RV, NoV GI and GII, AdV, astrovirus (AstV), enterovirus, sapovirus (SaV) and oral polio virus 1, 2 and 3), bacteria (Aeromonas spp, Bacteroides fragilis, Clostridium difficile, Campylobacter jejuni and coli, Escherichia coli (E. coli) including enteroaggregative E. coli, enteropathogenic E. coli (EPEC), enterotoxigenic E. coli, enteroinvasive E. coli and Shigella spp., Shiga-toxin producing E. coli (STEC), Helicobacter pylori, Mycobacterium tuberculosis, Salmonella spp. and Vibrio cholerae) and parasites (Ancyclostoma spp., Ascaris lumbricoides, Cryptosporidium spp., Cryptosporidium hominis, Cryptosporidium parvum, Cyclospora cayetanensis, Enterocytozoon bieneusi, Entamoeba histolytica, Encephalitozoon intestinalis, Giardia spp., Giardia A, Giardia B, Isospora belli, Necator americanus, Strongyloides stercoralis, Trichocephalus trichiuris).
Environmental samples
There were reports of a sewage spillage into a local river on the 19 December 2016. Water samples were collected from the lagoon and a nearby wastewater treatment works discharge (final effluent), which drains into a river that flows into the lagoon (Fig. 1). Samples of lagoon water (1 liter and 10 liter) and wastewater discharge (590 ml) were collected on 17 January 2017 and sent, in a cooler box with ice packs, to the Department of Medical Virology, University of Pretoria, for analysis for microbial indicator organisms and enteric viruses. Samples were received and analysed within 48 h of collection (19 January 2017). On arrival, the pH and temperature of the samples were measured and samples were stored at 4 °C until processing.
Microbial indicator analysis
Water samples were analysed >24 and <48 h after collection. The samples were tested for total coliforms, thermotolerant (faecal) coliforms by membrane filtration and selective media, namely m-Endo Les Agar and mFC Agar, as per SANS 5221:2006 Ed 4.2. Samples were tested for E. coli using m-ColiBlue24® broth [15]. Results were expressed as colony forming units (cfu) per 100 ml.
Viral recovery and analysis
Viruses were recovered from the 10 liter lagoon water sample using a glass wool adsorption-elution method followed by secondary concentration [16]. Viruses in the 1 liter lagoon water and 500 ml wastewater discharge (final effluent) sample were concentrated to a final volume of 10 ml using PEG8000/NaCl precipitation [15].
Total nucleic acid was extracted from 1 ml of the virus concentrates using the NucliSENS®EasyMag® instrument (BioMerieux, Marcy, l'Etoile, France) according to the manufacturer's instructions and eluted into 100 µl. Selected enteric viruses were detected in one-step quantitative reverse transcriptase-polymerase chain reaction (qRT-PCR) monoplex assays using the Quantifast® Pathogen RT-PCR + IC Kit (Qiagen), 5 µl nucleic acid and published primers and Taqman probes for AstV, enteroviruses, hepatitis A virus, NoV GI, NoV GII, RV and SaV [17–25]. The molecular amplification and qPCR detection of AdV was done using the TaqMan® Environmental Master Mix 2.0 (Applied Biosystems, Foster City, CA, USA) and primers and Taqman probe [26].
Enteric viruses were isolated in cell culture from 4 ml of the virus concentrate as described previously [7, 27]. Briefly, the recovered virus concentrates were treated with antibiotics and antimycotic. Thereafter, monolayers of the human hepatoma cell line PLC/PRF/5 (ECACC 85061113) and an African Green Monkey cell line (BGM: ECACC 90092601) in 25 cm2 cell culture flasks were inoculated, in duplicate, with 1 ml of the virus concentrate and incubated at 37 °C. Seven days post-infection, the cell cultures were blind passaged onto monolayers of the same cell type and incubated at 37 °C for a further 7 days after which the infected cells were harvested for molecular analysis for enteroviruses and AdVs. In addition, the harvested cell cultures were passaged onto monolayers of the Vero African Green Monkey cell line (ECACC 84113001) in cell culture tubes and monitored daily for a cytopathic effect. After a further 7-day incubation, the infected cell cultures, on flying coverslips, were stained with haematoxylin and eosin and examined for virus-specific inclusion bodies.
Irrespective of whether CPE was evident or not, total nucleic acid was extracted from 200 µl of all the harvested cell culture extracts using the NucliSENS®EasyMag® instrument (BioMerieux) according to the manufacturer's instructions and eluted into 50 µl. Enteroviruses were detected in one-step real time RT-PCR monoplex assay using the Quantitect Probe RT-PCR kit (Qiagen), 5 µl nucleic acid and published primers and Taqman probes for enteroviruses [18]. The molecular amplification and real-time PCR detection of AdV was done as described above.
NoV genotyping
NoV GI and GII strains were genotyped based on the partial capsid sequence (320 bp, Region C) [15]. Partial capsid amplicons were cloned in the ClonJET™ vector (Thermo Scientific, Waltham, MA, USA) and randomly selected clones were sequenced using vector-specific primers and the ABI PRISM BigDye1 Terminator v. 3.1 Cycle Sequencing kit (Applied Biosystems). Genotypes were assigned with the online Norovirus Genotyping Tool version 2 [28]. NoV strains from lagoon water and gastroenteritis cases were compared using Neighbour-Joining phylogenetic analysis in MEGA6 [29]. The sequences obtained in the study were submitted to GenBank under the following accession numbers: MG662693–MG662704.
Data analysis
Questionnaire results were exported from Google Forms into MS Excel (Microsoft Corp., Redmond, WA, USA), cleaned and exported into Stata v.14 (StataCorp., USA) for data analysis. The outbreak was described by time, place and person. Characteristics of cases and controls were described and analysed using appropriate significance tests (e.g. χ2 test). The incubation period of the implicated predominant pathogen was calculated by determining the number of hours between peaks on the epidemic curve.
Univariable analysis was conducted using a logistic regression model for each exposure variable and binary outcome variable of cases or controls, thereby enabling calculation of odds ratios (ORs) as a proxy for risk. Stratified analysis was conducted on exposure variables with the largest ORs for illness in the univariable analysis to explore whether other variables were confounding the associations. Variables associated with illness or protection were included at P < 0.2 in a multivariable logistic regression model to derive adjusted ORs.
Results
Epidemiological results
As of 10 January 2017, 760 persons presenting with gastrointestinal symptoms had been seen at the hospital. Historic data of diarrhoeal admissions at the hospital showed that this was above the expected number of admissions for the time period (see Fig. S1).
Descriptive epidemiology
A total of 311 cases and 126 controls were identified. Questionnaire responses were obtained from 157 (50%) cases and 62 (49%) controls. Of the 157 cases, 142 (90%) responded to the telephonic interview and 15 (10%) completed an online investigation form. Responses from controls were obtained through telephonic interview only.
Of the 157 cases, 53% were females. The median age for the cases was 21 years (interquartile range 10–40 years). The age group most affected was <1 to 10 years, with 27% of cases in this age group. There was no significant difference between the cases and controls in terms of age and gender distribution. However, there was a difference in terms of resident type, the control group had more permanent residents than visitors compared with the cases (P = 0.001) (Table 1).
Table 1.
Description of the study participants included in the analysis, KZN 2016/17
| Variables | Cases (%) | Controls (%) | P value* |
|---|---|---|---|
| Age (years) | |||
| 0–10 | 42/157 (27) | 15/61 (25) | 0.802 |
| 11–20 | 35/157 (22) | 17/61 (28) | 0.501 |
| 21–30 | 25/157 (16) | 4/61 (7) | 0.103 |
| 31–40 | 17/157 (11) | 4/61 (7) | 0.380 |
| >40 | 38/157 (24) | 21/61 (34) | 0.256 |
| Gender | |||
| Female | 82/156 (53) | 25/62 (40) | 0.331 |
| Male | 73/156 (47) | 37/62 (58) | 0.333 |
| Resident type | |||
| Permanent | 8/155 (5) | 14/62 (23) | 0.001 |
| Visitor | 147/155 (95) | 48/62 (77) | 0.365 |
Significance of the χ2 Pearson statistic, Significant P value ⩽0.05.
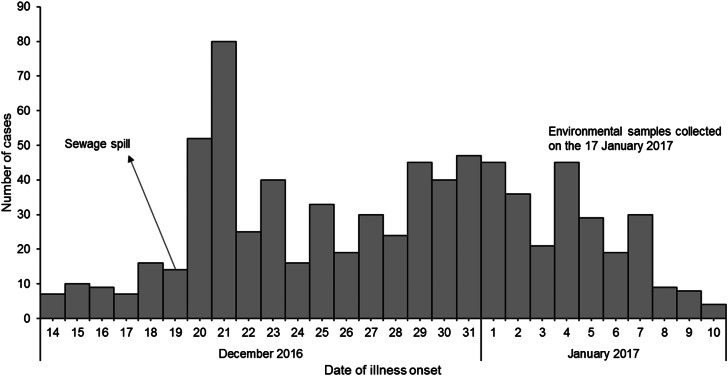
The most common symptoms were vomiting (85%; 133/157), diarrhoea (73%; 115/157) and abdominal cramps (31%; 49/157). The incubation period of the implicated predominant pathogen was 24–72 h. Where data were available on the onset and resolution of gastroenteritis (n = 68), the average duration of illness was 3.6 days (Fig. 2).
Fig. 2.
Epidemic curve showing the number of cases by date of illness onset, KZN 2016/17.
Exposures associated with illness
Four variables were significantly (P ⩽ 0.05) associated with either increased or decreased odds of becoming ill in our univariable analysis. These included being a visitor to the coast (OR 5.3, 95% confidence interval (CI) 2.1–13.5), drinking municipal water at the place of residence (OR 0.5, 95% CI 0.2–0.9), drinking bottled water (OR 2.8, 95% CI 1.4–5.3) and swimming in the lagoon (OR 3.6, 95% CI 1.2–10.9) (Table 2).
Table 2.
Results of the univariate logistic regression analysis of factors potentially associated with illness, KZN 2016/17
| Exposure variables | N | Cases | Controls | OR (95% CI) | P value |
|---|---|---|---|---|---|
| Resident type | |||||
| Permanent | 22 | 8 (36) | 14 (64) | Ref | |
| Visitor | 195 | 147 (75) | 48 (25) | 5.3 (2.1–13.5) | <0.001 |
| Shared a toilet with more than three people | |||||
| No | 9 | 5 (56) | 4 (44) | Ref | |
| Yes | 194 | 150 (77) | 44 (23) | 2.7 (0.7–10.5) | 0.147 |
| Ate at a restaurant | |||||
| No | 123 | 93 (76) | 30 (24) | Ref | |
| Yes | 95 | 63 (66) | 32 (34) | 0.6 (0.3–1.1) | 0.133 |
| Ate at a fast-food outlet | |||||
| No | 181 | 130 (72) | 51 (28) | Ref | |
| Yes | 35 | 24 (69) | 11 (31) | 0.8 (0.3–1.8) | 0.697 |
| Drank municipal water at place of residence | |||||
| No | 147 | 112 (76) | 35 (24) | Ref | |
| Yes | 69 | 42 (61) | 27 (39) | 0.5 (0.2–0.9) | 0.021 |
| Drank bottled water | |||||
| No | 57 | 31 (54) | 26 (46) | Ref | |
| Yes | 157 | 121 (77) | 36 (23) | 2.8 (1.4–5.3) | 0.002 |
| Swam in the lagoon | |||||
| No | 176 | 118 (67) | 58 (33) | Ref | |
| Yes | 34 | 30 (88) | 4 (12) | 3.6 (1.2–10.9) | 0.019 |
OR, odds ratio; CI, confidence interval, significant P value ⩽0.05.
In the final multivariable analysis model, the following positive associations were noted: holiday-makers/visitors had 6.0 times greater odds of developing gastroenteritis than the residents (95% CI 2.0–17.6) and people who swam in the lagoon had 3.3 times greater odds of developing gastroenteritis compared with those who did not swim in the lagoon (95% CI 0.1–10.3). In addition, people who drank bottled water had 2.4 times greater odds of developing gastroenteritis compared with people who drank municipal water (95% CI 1.1–4.8). Conversely, people who ate at restaurants had 0.5 times lesser odds of developing gastroenteritis compared with those who did not eat at restaurants. In our univariable analysis, eating at restaurant was not a significant factor associated with illness (Table 3). The goodness-of-fit test demonstrated that the model-predicted results were not significantly different than the actual observed results, indicating adequate fit (P = 0.65).
Table 3.
Results of the multivariable logistic regression analysis of factors potentially associated with illness, KZN 2016/17
| Variables | Adjusted OR | 95% CI | P value |
|---|---|---|---|
| Resident type | |||
| Permanent | Ref | ||
| Visitor | 6.0 | 2.0–17.6 | 0.001 |
| Ate at a restaurant | |||
| No | Ref | ||
| Yes | 0.5 | 0.2–0.9 | 0.032 |
| Drank bottled water | |||
| No | Ref | ||
| Yes | 2.4 | 1.1–4.8 | 0.015 |
| Swam in the lagoon | |||
| No | Ref | ||
| Yes | 3.3 | 0.1–10.3 | 0.039 |
OR, odds ratio; CI, confidence interval, significant P value ⩽0.05.
Laboratory results
Stool/clinical specimens
Of the 20 clinical specimens tested, 11 (55%) tested positive for NoV; nine were positive for NoV GI, while two were positive for NoV GII. Aeromonas, enterovirus and EPEC were also detected in one NoV GI-positive specimen and STEC in another NoV GI-positive specimen.
Environmental samples
The total coliform and thermotolerant (faecal) coliform counts in the lagoon water were 2.39 × 104 and 9.5 × 103 cfu/100 ml, respectively. The E. coli level was 1.93 × 103 cfu/100 ml.
Enteric viruses, namely AstV, NoV GI, NoV GII and RV, were detected by direct analysis of the lagoon water, with the wastewater discharge testing positive for NoV GII. After amplification in cell culture, AdVs were detected in the wastewater discharge, by PCR in the infected cell culture extracts. Reoviruses were isolated from, and identified by, typical reovirus eosinophilic cytoplasmic inclusions [28] in cell cultures infected with the wastewater discharge suggesting the presence of potentially infectious viruses.
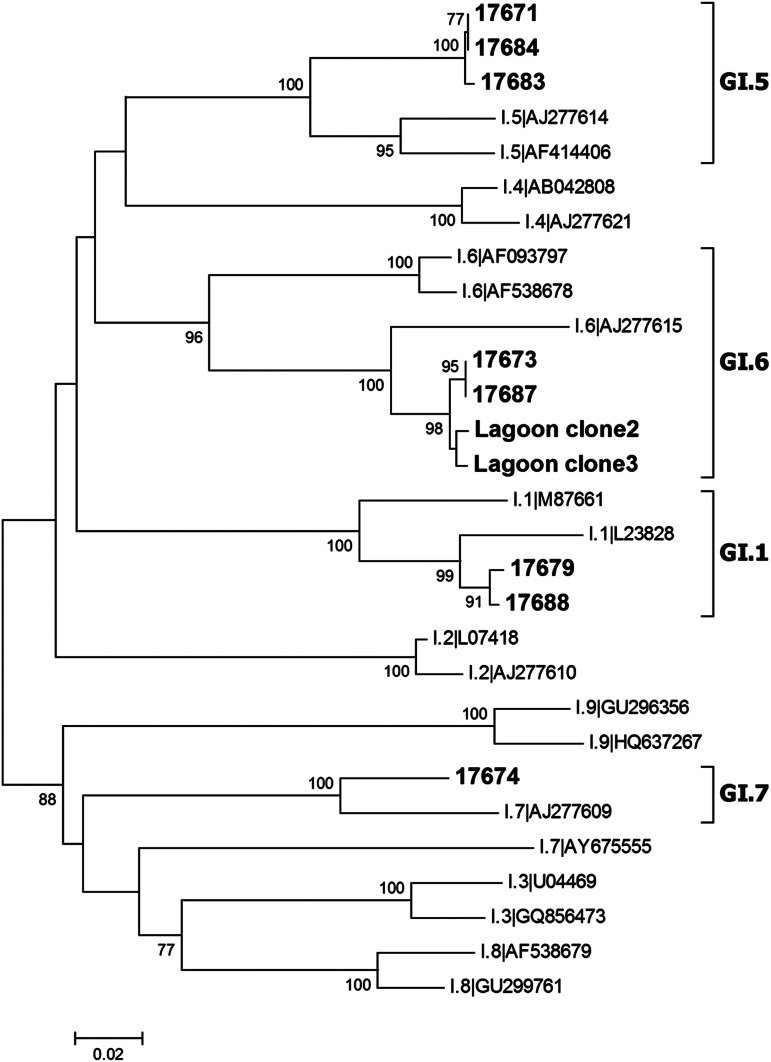
NoV characterisation
Eight NoV GI-positive specimens could be genotyped and GI.1 (n = 2), GI.5 (n = 3), GI.6 (n = 2) and GI.7 (n = 1) strains were detected. Based on BLAST-n analysis, the GI.1 strains were most closely related to strains detected in China (KM246902.1, 100% identity) and Taiwan (KT732279.1, 93% identity) between 2011 and 2015. The GI.5 strains were 97–99% identical to strains that had been detected in surface water and sewage in SA between 2010 [6] and 2015 [13]. The GI.6 viruses were closely related to strains that circulated in China (KU724081, 99% identity) and Russia (KY210910, 99% identity) in 2015/2016. The GI.7 genotype had previously been detected in a child hospitalised with gastroenteritis in Johannesburg, SA in 2011 (KR904267, 96% identity).
NoV genotypes GI.6, GII.3 and GII.6 could be characterised from NoVs detected in the lagoon water samples. The GII.3 strains were closely related to viruses that were detected in children with gastroenteritis in SA in 2013 (KR904473, 97% identity) as well as NoVs detected in wastewater (MF182296, 97% identity) in the Free State Province in 2016. The GII.6 strains in contrast were related to strains that circulated in China (KP3355058, 99% identity) and South Korea (KX764803, 99% identity) in 2014/2016. NoV GI.6, with 99% identity over a 299 nucleotide region of the capsid gene, was identified in both the lagoon and two gastroenteritis cases (Fig. 3).
Fig. 3.
Neighbour-Joining phylogenetic analysis of partial capsid sequences (299 bp) derived from gastroenteritis cases and lagoon water with norovirus GI reference strains. Strains indicated in bold are from the outbreak investigation. Bootstrap support (1000 replicates) of >70% is shown. The scale bar represents the number of base substitutions per site.
Discussion
In this outbreak, gastroenteritis was associated with swimming in the lagoon, drinking bottled water and being a visitor to the South Coast. Eating at restaurants seemed to be a protective factor against illness. The diverse pathogens and multiple NoV strains detected were consistent with faecal contamination of the water sources [30]. NoV GII was also found in the final effluent from the wastewater treatment works.
Previous studies have suggested an association between gastroenteritis and swimming in recreational water [31–33]. A Danish study showed that healthy athletes who swam in sewage-polluted coastal water were five times more likely to get gastroenteritis compared with those who swam in non-polluted conditions [31]. In the current study, swimming in the lagoon was significantly associated with gastroenteritis. The water was analysed for microbial indicators and despite testing being performed >24 and <48 h after collection, the thermotolerant (faecal coliform) count was >2 × 103. According to the South African Water Quality Guidelines for recreational water, these counts indicate an increased risk of gastrointestinal illness. Likewise, the E. coli detected in the lagoon water was 4.8 times above the recommended <400 cfu/100 ml and indicated an increased risk of health effects [34].
During telephonic interviews, it was established that the residents of the South Coast did not swim in the lagoon as the water was perceived to be contaminated. In fact, of the 34 people who swam in the lagoon, only 1 (3%) was a resident of the South Coast (Table 3). In addition, there were reports of a sewerage spill into the river and warning signs were placed near the lagoon prohibiting people from swimming. These data support the hypothesis that the lagoon was the source of the outbreak among holiday-makers on the KZN Coast.
Sewage waste can harbour several enteric pathogens including NoV, AstV and RV. NoV has been previously implicated in waterborne gastroenteritis outbreaks [30, 31]. Even though the sewage spill occurred almost 1 month before the lagoon was sampled, the flow out of the lagoon into the ocean is limited (see Fig. 1) and NoV has been shown to remain detectable and infectious for at least 61 days in groundwater [35]. It is therefore possible that the pathogens from the spill would still be detectable and infectious after 1 month. Considering that only 16% of the study participants indicated swimming in the lagoon, the outbreak was probably perpetuated by person-to-person transmission [36]. The transmission of NoV occurs through direct person-to-person contact or through indirect contact including contaminated food, water or environment surfaces [37]. At the time of the outbreak, many people were visiting the South Coast for their holidays. As a result, the beach area next to the lagoon, flats, hotels, guest houses, other communal places of residence and recreational places were most likely overcrowded. This would provide a conducive environment for the transmission of NoV.
Activities such as shaking of hands, hugging each other, caring for the sick and preparing food for friends and families can all facilitate the spread of infection. NoV can survive on surfaces such as toilet seats, floors or even walls and remain stable for longer periods, making the spread of infection difficult to prevent [38].
NoV diversity in individuals involved in an outbreak is considered an indication of waterborne exposure [30]. The detection of multiple genotypes provides supporting evidence that the outbreak originated in the contaminated lagoon. Furthermore, NoV GI.6 strains (99% identical) were identified in the lagoon and in two individuals with gastroenteritis providing another potential link between swimming in the lagoon and contracting disease.
NoV has an incubation period of 12–48 h, with the illness duration of 12–72 h [39]. In severe cases, duration of illness can be prolonged; this is commonly seen among the very old and very young [40]. The NoV incubation period and duration of illness are consistent with our findings in this study.
Drinking bottled water was also significantly associated with gastroenteritis during the outbreak. During December 2016, holiday-makers on the KZN Coast generally drank bottled water as there were water shortages at the time. Therefore, drinking bottled water may have been a confounder in this case. If the outbreak was caused by bottled water contamination either at processing or factory level, the outbreak would have affected a larger number of people, including local residents, as supermarkets sell the water on a large scale to consumers. However, sharing bottled water could have facilitated the virus spread.
During the outbreak, eating at a restaurant was significantly associated with not becoming ill. Restaurants are more likely to have policies in place to ensure proper personal hygiene among staffs and in food handling compared with ordinary people. A study in the Netherlands showed that enhanced hygiene practices significantly reduced person-to-person transmission of NoV [36]. This could explain the protective effect associated with eating at restaurants seen during the outbreak.
Limitations encountered in the study included refusal of participation by cases and controls during telephonic interviews. There was a limited number of cases in the study due to lack of or incorrect contact details and recall bias could also not be ruled out. Our control group had more permanent residents than visitors compared with the cases; this may have resulted in an over- or underestimation of the OR. However, despite the bias, results from environmental and clinical investigations support both the source (lagoon) and cause (NoV) of the outbreak. Failure to collect clinical specimens by the healthcare workers from the cases was also a limitation in this study. Municipal drinking water was not tested for bacterial indicators; this is also a limitation in our study.
Conclusion
The outbreak investigation showed that gastroenteritis was associated with swimming in the lagoon. The lagoon was reportedly contaminated by the wastewater treatment works effluent, which drained into the river flowing into the lagoon. Our findings also indicate that the outbreak was further propagated through person-to-person transmission resulting in the high number of cases seen. We recommend that better signage, communication and enforcement should be put in place to restrict swimming in the lagoon in the event of sewage spills. Emphasis should also be put on proper hygiene practices within the residential and recreational areas among holiday-makers. Inspections of the wastewater treatment infrastructures should also be conducted frequently to prevent any leakages of raw sewage into water sources such as rivers.
Acknowledgements
The authors would like to acknowledge the organisations and personnel that played a role in the investigation of the gastroenteritis outbreak: Outbreak Response Unit, Centre for Enteric Diseases, South African Field Epidemiology Training Programme and Centre for Respiratory Diseases and Meningitis – all of the NICD, and the Department of Medical Virology, Faculty of Health Sciences, University of Pretoria. The Communicable Disease Control directorate, Ugu district, KZN, all healthcare facilities and public health professionals that were involved in the outbreak investigations, including the individuals listed below: Ms Premi Govender, Mr Rob Ferreira, Sr Sarah McKaw, Sr Carla Potgieter, Dr Lebo Gumede, Ms Siphumelele Mlambo and Mr Vella Gramoney.
Financial support
This research received no specific grant from any funding agency.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guides on the care and use of laboratory animals. NICD outbreak investigations are approved by the research ethics committee at the University of the Witwatersrand, Johannesburg, South Africa (Clearance certificate number: M160667). All authors vouch for the completeness and accuracy of the data and analyses presented. There was no commercial support for this study.
Conflict of interest
None.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S095026881800122X.
click here to view supplementary material
References
- 1.Elmahdy E et al. (2016) Enteric viruses in surface water and sediment samples from the catchment area of Peri Lagoon, Santa Catarina State, Brazil. Journal of Water and Health 14, 142–154. [DOI] [PubMed] [Google Scholar]
- 2.Aslan A et al. (2011) Occurrence of adenovirus and other enteric viruses in limited-contact freshwater recreational areas and bathing waters. Journal of Applied Microbiology 111, 1250–1261. [DOI] [PubMed] [Google Scholar]
- 3.Hall V et al. (2017) A large outbreak of gastrointestinal illness at an open-water swimming event in the River Thames, London. Epidemiology and Infection 145, 1246–1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chigor VN and Okoh AI (2012) Quantitative RT-PCR detection of hepatitis A virus, rotaviruses and enteroviruses in the Buffalo River and source water dams in the Eastern Cape Province of South Africa. International Journal of Environmental Research and Public Health 9, 4017–4032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin J and Singh A (2015) Detection of human enteric viruses in Umgeni River, Durban, South Africa. Journal of Water and Health 13, 1098–1112. [DOI] [PubMed] [Google Scholar]
- 6.Qin M et al. (2016) A waterborne gastroenteritis outbreak caused by norovirus GII. 17 in a Hotel, Hebei, China, December 2014. Food and Environmental Virology 8, 180–186. [DOI] [PubMed] [Google Scholar]
- 7.Mans J et al. (2013) Diverse norovirus genotypes identified in sewage-polluted river water in South Africa. Epidemiology and Infection 141, 303–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Abel N, Mans J and Taylor MB (2017) Quantitative microbial risk assessment to estimate the health risk from exposure to noroviruses in polluted surface water in South Africa. Journal of Water and Health 15, 908–922. [DOI] [PubMed] [Google Scholar]
- 9.Edokpayi JN, Odiyo JO and Durowoju OS (2017) Impact of wastewater on surface water quality in developing countries: a case study of South Africa. In Tutu H (ed.), Water Quality. London: InTech, pp. 401–416. [Google Scholar]
- 10.Teklehaimanot GZ et al. (2015) Population growth and its impact on the design capacity and performance of the wastewater treatment plants in Sedibeng and Soshanguve, South Africa. Environmental Managemental 56, 984–997. [DOI] [PubMed] [Google Scholar]
- 11.STATSSA. (2011) 2011 Census|Statistics South Africa. Pretoria: STATSSA. [Google Scholar]
- 12.Liu J et al. (2013) A laboratory-developed TaqMan Array Card for simultaneous detection of 19 enteropathogens. Journal of Clinical Microbiology 51, 472–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu J et al. (2016) Use of quantitative molecular diagnostic methods to identify causes of diarrhoea in children: a reanalysis of the GEMS case-control study. The Lancet 388, 1291–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu J et al. (2016) Optimization of quantitative PCR methods for enteropathogen detection. PLoS ONE 11, e0158199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mabasa V et al. (2017) Environmental surveillance for noroviruses in selected South African wastewaters 2015–2016: emergence of the novel GII. 17. Food and Environmental Virology 10, 16–28. [DOI] [PubMed] [Google Scholar]
- 16.Kiulia NM et al. (2014) Norovirus GII.17 predominates in selected surface water sources in Kenya. Food and Environmental Virology 6, 221–231. [DOI] [PubMed] [Google Scholar]
- 17.Le Cann P et al. (2004) Quantification of human astroviruses in sewage using real-time RT-PCR. Research in Microbiology 155, 11–15. [DOI] [PubMed] [Google Scholar]
- 18.Fuhrman JA, Liang X and Noble RT (2005) Rapid detection of enteroviruses in small volumes of natural waters by real-time quantitative reverse transcriptase PCR. Applied and Environmental Microbiology 71, 4523–4530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Costafreda MI, Bosch A and Pintó RM (2006) Development, evaluation, and standardization of a real-time TaqMan reverse transcription-PCR assay for quantification of hepatitis A virus in clinical and shellfish samples. Applied Environmental Microbiology 72, 3846–3855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.da Silva AK et al. (2007) Evaluation of removal of noroviruses during wastewater treatment, using real-time reverse transcription-PCR: different behaviors of genogroups I and II. Applied Environmental Microbiology 73, 7891–7897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Svraka S et al. (2007) Etiological role of viruses in outbreaks of acute gastroenteritis in The Netherlands from 1994 through 2005. Journal of Clinical Microbiology 45, 1389–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kageyama T et al. (2003) Broadly reactive and highly sensitive assay for Norwalk-like viruses based on real-time quantitative reverse transcription-PCR. Journal of Clinical Microbiology 41, 1548–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Loisy F et al. (2005) Real-time RT-PCR for norovirus screening in shellfish. Journal of Virological Methods 123, 1–7. [DOI] [PubMed] [Google Scholar]
- 24.Zeng S-Q et al. (2008) One-step quantitative RT-PCR for the detection of rotavirus in acute gastroenteritis. Journal of Virological Methods 153, 238–240. [DOI] [PubMed] [Google Scholar]
- 25.Chan MC et al. (2006) Sapovirus detection by quantitative real-time RT-PCR in clinical stool specimens. Journal of Virological Methods 134, 146–153. [DOI] [PubMed] [Google Scholar]
- 26.Heim A et al. (2003) Rapid and quantitative detection of human adenovirus DNA by real-time PCR. Journal of Medical Virology 70, 228–239. [DOI] [PubMed] [Google Scholar]
- 27.Vivier JC, Ehlers MM and Grabow WO (2004) Detection of enteroviruses in treated drinking water. Water Research 38, 2699–2705. [DOI] [PubMed] [Google Scholar]
- 28.Kroneman A et al. (2011) An automated genotyping tool for enteroviruses and noroviruses. Journal of Clinical Virology 51, 121–125. [DOI] [PubMed] [Google Scholar]
- 29.Tamura K et al. (2013) MEGA6: molecular evolutionary genetics analysis version 6.0. Molecular Biology and Evolution 30, 2725–2729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nenonen NP et al. (2012) Marked genomic diversity of norovirus genogroup I strains in a waterborne outbreak. Applied Environmental Microbiology 78, 1846–1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harder-Lauridsen NM et al. (2013) Gastrointestinal illness among triathletes swimming in non-polluted versus polluted seawater affected by heavy rainfall, Denmark, 2010–2011. PLoS ONE 8, e78371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Joosten R et al. (2017) Risk factors for gastroenteritis associated with canal swimming in two cities in the Netherlands during the summer of 2015: a prospective study. PLoS ONE 12, e0174732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prüss A (1998) Review of epidemiological studies on health effects from exposure to recreational water. International Journal of Epidemiology 27, 1–9. [DOI] [PubMed] [Google Scholar]
- 34.South African Water Quality Guidelines. Recreational water use. http://www.waternet.co.za/policy/g_wq.html. (Accessed 10 March 2018).
- 35.Seitz SR et al. (2011) Norovirus infectivity in humans and persistence in water. Applied and Environmental Microbiology 77, 6884–6888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heijne JC et al. (2009) Enhanced hygiene measures and norovirus transmission during an outbreak. Emerging Infectious Diseases 15, 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.de Graaf M, Villabruna N and Koopmans MPG (2017) Capturing norovirus transmission. Current Opinion in Virology 22, 64–70. [DOI] [PubMed] [Google Scholar]
- 38.Repp KK, Hostetler TP and Keene WE (2013) A norovirus outbreak related to contaminated surfaces. The Journal of Infectious Diseases 208, 295–298. [DOI] [PubMed] [Google Scholar]
- 39.Lee RM et al. (2013) Incubation periods of viral gastroenteritis: a systematic review. BMC Infectious Diseases 13, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Asten L et al. (2011) Unspecified gastroenteritis illness and deaths in the elderly associated with norovirus epidemics. Epidemiology 22, 336–343. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S095026881800122X.
click here to view supplementary material