Abstract
Background:
The use of imaging to diagnose patellofemoral instability is often limited by the inability to dynamically load the joint during assessment. Therefore, the diagnosis is typically based on physical examination using the glide test to assess and quantify lateral patellar translation. However, precise quantification with this technique remains difficult.
Purpose:
To quantify patellar position using ultrasound imaging under dynamic loading conditions to distinguish between knees with and without medial patellofemoral complex (MPFC) injury.
Study Design:
Controlled laboratory study.
Methods:
In 10 cadaveric knees, the medial patellofemoral distance was measured to quantify patellar position from 0° to 40° of knee flexion at 10° increments. Knees were evaluated at each flexion angle under unloaded conditions and with 20 N of laterally directed force on the patella to mimic the glide test. Patellar position measurements were made on ultrasound images obtained before and after MPFC transection and compared for significant differences. To determine the ability of medial patellofemoral measurements to differentiate between MPFC-intact and MPFC-deficient states, area under the receiver operating characteristic (ROC) curve analysis and the Delong test were used. The optimal cutoff value to distinguish between the deficient and intact states was determined using the Youden J statistic.
Results:
A significant increase in medial patellofemoral distance was observed in the MPFC-deficient state as compared with the intact state at all flexion angles (P = .005 to P < .001). When compared with the intact state, MPFC deficiency increased medial patellofemoral distance by 32.8% (6 mm) at 20° of knee flexion under 20-N load. Based on ROC analysis and the J statistic, the optimal threshold for identifying MPFC injury was 19.2 mm of medial patellofemoral distance at 20° of flexion under dynamic loading conditions (area under the ROC curve = 0.93, sensitivity = 77.8%, specificity = 100%, accuracy = 88.9%).
Conclusion:
Using dynamic ultrasound assessment, we found that medial patellofemoral distance significantly increases with disruption of the MPFC.
Clinical Relevance:
Dynamic ultrasound measurements can be used to accurately detect the presence of complete MPFC injury.
Keywords: knee, medial patellofemoral ligament, medial patellofemoral complex, patellar instability, patellar dislocation, patellofemoral, ultrasound, dynamic imaging, stress imaging
Patellar dislocation occurs at a rate of 5.8 to 29 per 100,000 persons and is a common reason for primary care office and emergency department visits. 7,29,37 Overall, 30% to 40% of patients who sustain a patellar dislocation continue to have recurrent instability events or functional limitation, which can lead to significant long-term morbidity without surgical stabilization. 19,31 Injury or insufficiency of the medial patellofemoral complex (MPFC), which consists of the medial patellofemoral ligament (MPFL) and the medial quadriceps tendon–femoral ligament, is the primary factor leading to patellar instability, and assessment of its integrity is crucial in determining the stability of the patella and potential treatment options. 5,8,12 –14,20,32,35
Imaging modalities such as magnetic resonance imaging (MRI) and computed tomography (CT) are commonly utilized in the evaluation of patellar instability. 2,25 MRI has been argued to be the gold standard in evaluating for MPFC injury 5 ; however, as patellar instability is a dynamic process, assessment of the appearance of the MPFC based on static MRI can lead to high false-negative rates and has not been shown to be a reliable predictor of functional patellar instability. 26 CT scanning allows for excellent visualization of patellofemoral joint anatomy and alignment; however, similar to MRI, it is limited by its static nature. While dynamic CT imaging has been applied in the assessment of patellar maltracking during knee range of motion, this imaging technology is not readily accessible at most institutions. 10,33
Currently, imaging techniques are limited in their ability to definitively diagnose and quantify patellar instability; therefore, the detection of MPFC insufficiency relies primarily on dynamic assessment with clinical examination. 24 The patellar glide test allows for the assessment of patellar translation based on a laterally directed force on the patella, 17,18 in which lateral patellar translation of >2 quadrants of patellar width is typically considered to suggest MPFC insufficiency. Increasing increments of lateral translation have been associated with increased risk of patellar instability. 33 While prior studies have attempted to accurately quantify patellar position during the glide test, widespread clinical application of such tools has been limited. 6,9,15,30,36
Portable ultrasound has been increasingly applied in the diagnosis and imaging of musculoskeletal injuries, as it allows for visualization under dynamic conditions. 21 It additionally has the benefit of low cost, no radiation, and almost immediate availability at the point of care, thereby allowing for increased access to diagnostic measures. Prior studies have demonstrated that ultrasound is an accurate and reliable tool for assessing the patellofemoral joint 11 and has been shown to be comparable with MRI in the assessment of patellar tracking. 26 However, these studies have not evaluated its use in assessing patellar instability.
The primary aim of this study was to quantify patellar position using ultrasound imaging under dynamic loading conditions, comparing knees with and without injury to the MPFC. The secondary aim was to establish ultrasound imaging parameters to differentiate knees with MPFC injury from those without injury. We hypothesized that the ultrasound measurements of lateralized patellar position would significantly increase in the MPFC-deficient state when compared with the intact state.
Methods
Specimen Preparation
Ten unpaired fresh-frozen human cadaveric knee specimens were utilized in this study. Each knee had been amputated at the mid- to proximal femur and included the foot distally. Specimens were thawed at room temperature for 24 hours before the start of the experiment. Arthroscopic and fluoroscopic evaluation of the lower extremities was performed to assess for osteoarthritis, bony abnormalities, fractures, or evidence of prior surgery, and those with positive findings were excluded.
A fellowship-trained orthopaedic surgeon (M.J.T.) carried out the evaluation of each knee to exclude knees with signs of pre-existing patellar instability, defined as having >2 quadrants of patellar mobility in either direction. Additionally, each knee was assessed for the presence of morphological risk factors that contribute to patellar instability. Fluoroscopic evaluation was performed on each knee before the beginning of the study. Merchant views were performed to assess the morphology of the trochlea, and lateral trochlear inclination was measured as the angle between the slope of the lateral anterior condyle and the posterior condylar axis. On the lateral view, the Caton-Deschamps index was measured using the ratio of the distance from the inferior articular pole to the anterior tibia with the length of the patellar articular surface. Last, at the completion of the study, all knees underwent dissection for manual measurements of tibial tuberosity–trochlear groove distance, using calipers to measure tuberosity offset relative to the deepest point of the trochlear groove. To isolate the effects of MPFC deficiency on patellar position, knees that demonstrated ≥1 risk factors—including trochlear dysplasia (lateral trochlear inclination <11°), patella alta (Caton-Deschamps index <1.2), or malalignment (tibial tuberosity–trochlear groove distance >20 mm)—were excluded from the analysis.
Each knee specimen was positioned with the femur secured in a jig, with the knee joint and lower leg unrestricted to allow for full range of knee motion. To simulate the resting tension of the quadriceps muscle, a traction force of 10 N was placed on the rectus femoris muscle proximally, in line with the muscle vector. 4 A 2.5-mm eyelet screw was placed along the lateral border of the patella at its proximodistal midpoint, perpendicular to its longitudinal axis. An electronic force gauge was attached to the eyelet screw to designate a lateralizing force on the patella, perpendicular to the axis of the extensor mechanism. Two standardized loading conditions were created: unloaded (0 N of force) and loaded with 20 N of laterally directed force on the patella to mimic the patellar glide test, as described in prior studies. 3,4
MPFC Transection and Ultrasound Measurement
The patellofemoral joint was assessed using a portable ultrasound device (2-dimensional grayscale B mode complete ultrasound; Butterfly iQ, Butterfly Network) (Figure 1). The probe was positioned at the medial patella at its widest portion and oriented parallel to the joint line to visualize the medial patellar facet and the medial trochlear facet on 1 image. Images were obtained in the unloaded and loaded conditions from 0° to 40° of knee flexion in 10° increments, during which a handheld goniometer was used to measure knee flexion. Ultrasonographic scanning was performed by an orthopaedic surgeon (R.B.) experienced in utilizing musculoskeletal ultrasound, and the images were saved for analysis.
Figure 1.
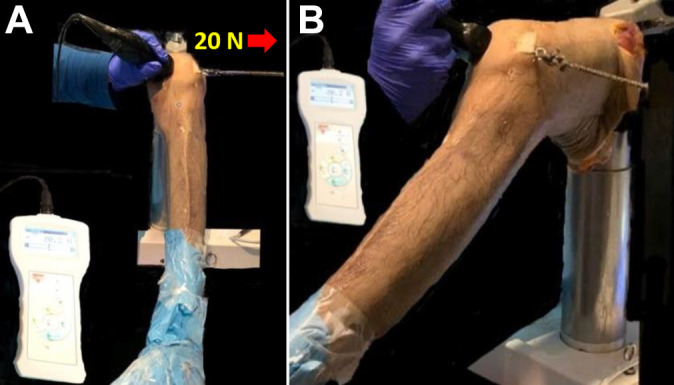
Experimental setup demonstrating probe placement of the portable ultrasound on a left knee. (A) The probe is positioned at the medial patella at its widest portion and oriented parallel to the joint line to visualize the medial patellar facet and the medial trochlear facet on 1 image. Ultrasound images were obtained with and without 20 N of laterally directed force. (B) Setup shown from a different angle.
After ultrasound images were obtained from the intact knees, the MPFC was then arthroscopically transected, using a technique previously described by Tanaka et al. 34 The superomedial border of the patella was visualized with a 30° arthroscope (Synergy 4 K System; Arthrex) through a standard anterolateral portal, and a synovectomy was performed on the medial knee to reveal the MPFC fibers as described by Siebold and Borbon. 28 In each knee, the fibers of the MPFC were visualized inserting on the patella and/or quadriceps tendon. After the proximal and distal boundaries were marked, the fibers were transected using a shaver and arthroscopic biter with care not to extend past the marked boundaries. This was performed by a fellowship-trained orthopaedic surgeon (M.J.T.) with expertise in patellofemoral surgery. The ultrasound was repeated after transecting the medial soft tissue restraints, and images were again captured in the unloaded and loaded states at each flexion angle.
The ultrasound images were imported into Image J (National Institutes of Health) to perform the measurements. The magnification scale embedded within the image was used to calibrate each measurement. To quantify patellar position, the distance between the most medial aspect of the articular edge of the medial patellar facet and the apex of the medial trochlear facet was measured on each image and referred to as the medial patellofemoral distance (Figure 2). All measurements were performed by an orthopaedic surgeon trained to perform such measurements (R.B.).
Figure 2.
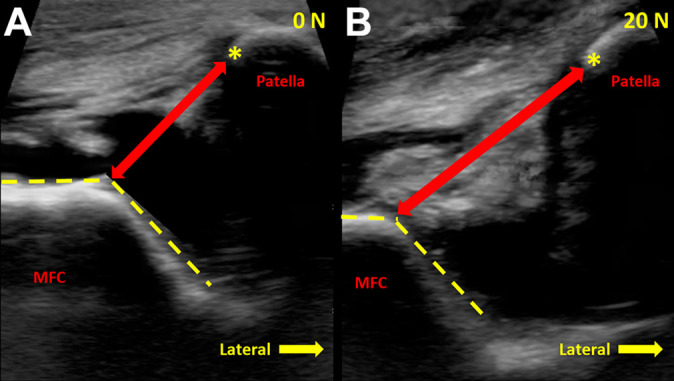
Measurement on ultrasound images of the medial patellofemoral distance, defined as the distance from the apex of the medial trochlea (dashed yellow lines) to the most medial aspect of the patellar articular surface (asterisks). (A) The medial patellofemoral distance between the apex of the medial trochlea and the medial facet of the patella under 0-N force. (B) Increased medial patellofemoral distance under a standardized 20-N laterally directed force. MFC, medial femoral condyle.
Intraclass correlation coefficients (ICCs) were calculated to assess inter- and intrarater reliability. Three observers—2 orthopaedic surgeons (R.B. and S.A.-E.) and a bioengineering graduate student (K.M.)—performed each measurement on 5 knee specimens to assess interrater reliability. A single observer performed each measurement 3 times each on 5 knees to calculate intrarater reliability. The absolute agreement determined how much a measurement of 1 observer varied from that of the other observer. The ICCs were interpreted according to the guidelines provided by Shrout and Fleiss, 27 where values between 0 and 0.10 were considered virtually no agreement; 0.11 and 0.40, slight; 0.41 and 0.60, fair; 0.61 and 0.80, moderate; and 0.81 and 1.0, substantial.
Sample-Size Calculation and Statistical Analysis
In a previous clinical study, Burke et al 1 assessed dynamic patellar position with MRI analysis using continuous real-time radial gradient echo imaging in symptomatic patients and asymptomatic healthy individuals. They found that the lateral patellar position on dynamic MRI was a sensitive measurement for detecting patellar instability. The mean ± SD distance for the symptomatic patients and asymptomatic participants was 4.4 ± 3.7 and 1.5 ± 0.7 mm, respectively. To test the current primary null hypothesis that there was no difference in ultrasound measurements of the lateral patellar position between the MPFC-deficient state and the intact state, we used a paired t test. This parametric test compares 2 dependent samples. To achieve 80% statistical power for detecting a difference of 2.9 mm in lateral patellar tracking between the MPFC-deficient and intact states (4.4 ± 3.7 vs 1.5 ± 0.7 mm; 0.9 correlation) with a 2-tailed type 1 error rate of 5%, we determined that 10 specimens would be needed. The sample-size calculation was performed using G*Power Version 3.1.9.2.
All measurements were reported as percentage or mean and standard deviation. The medial patellofemoral distance was described to the nearest 0.1 mm. The Kolmogorov-Smirnov and Shapiro-Wilk tests were used to test for normality of the data. The paired t test was used to compare the difference in the ultrasound measurements of the medial patellofemoral distance between the MPFC-intact and MPFC-deficient states at each flexion angle. Area under the receiver operating characteristic (ROC) curve analysis and the Delong test were performed to determine the ability of measurements to differentiate between the MPFC-intact and MPFC-deficient states under all testing conditions. An area under the curve (AUC) of 1.0 represents a perfect test, and an area of 0.5 represents a worthless test. The Youden J statistic was calculated to determine the optimal cutoff value to distinguish between the MPFC-intact and MPFC-deficient states. In this study, P <.05 was considered statistically significant. Data analyses were performed using SPSS Version 26.0 (IBM).
Results
Of the 10 unpaired cadaveric knees in the study, 4 were from men and 6 were from women. The mean age at the time of death was 51 ± 11 years (range, 32-70). In all knees, the MPFC was functionally intact upon manual evaluation and anatomically identified during arthroscopy, with fibers attaching to the patella and quadriceps tendon. In the studied knees, lateral trochlear inclination was 25.3° ± 8.2°, Caton-Deschamps index was 0.9 ± 0.2, and tibial tuberosity–trochlear groove distance was 12.2 ± 3.2 mm. The ICCs for intra- and interrater reliability for medial patellofemoral distance were 0.99 (95% CI, 0.99-0.99) and 0.98 (95% CI, 0.94-0.99), respectively, indicating excellent agreement among observers.
In the MPFC-intact and MPFC-deficient conditions, the medial patellofemoral distance increased with knee flexion from 0° to 40°. In the unloaded and loaded conditions, medial patellofemoral distance significantly increased in the MPFC-deficient state at all knee flexion angles when compared with the intact state (P = .005 to P < .001). The results of medial patellofemoral distance measurements are summarized in Table 1. The greatest increase was found at 20° of knee flexion and 20 N of laterally directed force, at which the medial patellofemoral distance increased by 32.8% (an increase of 6 mm) from 18.3 ± 1.9 mm (95% CI, 16.7-19.5 mm) to 24.3 ± 2.7 mm (95% CI, 21.5-26.7 mm) after MPFC transection (P < .001) (Figure 3).
Table 1.
Medial Patellofemoral Distance Between the MPFC-Intact and MPFC-Deficient States as Measured Using Portable Ultrasound a
| MPFC Distance, mm, Mean ± SD | Difference, Intact vs Deficient | ||||
|---|---|---|---|---|---|
| Testing Condition | Intact | Deficient | Mean (95% CI), mm | Change, % | P Value b |
| 0° of flexion | |||||
| 0 N | 13.5 ± 1.8 | 16.4 ± 1.7 | 2.9 (1.1-4.6) | 21.5 | .005 |
| 20 N | 17.2 ± 1.4 | 21.2 ± 2.7 | 4.0 (1.7-6.2) | 23.3 | .004 |
| 10° of flexion | |||||
| 0 N | 13.7 ± 2.2 | 17.3 ± 2.6 | 3.6 (1.5-5.7) | 26.3 | .005 |
| 20 N | 17.7 ± 1.5 | 22.8 ± 3.6 | 5.1 (2.7-7.4) | 28.8 | .001 |
| 20° of flexion | |||||
| 0 N | 13.7 ± 1.6 | 17.8 ± 1.8 | 4.1 (2.3-6.0) | 29.9 | .001 |
| 20 N | 18.3 ± 1.9 | 24.3 ± 2.7 | 6.0 (4.1-7.8) | 32.8 | <.001 |
| 30° of flexion | |||||
| 0 N | 14.6 ± 1.8 | 17.9 ± 1.6 | 3.3 (2.0-4.7) | 22.6 | <.001 |
| 20 N | 18.9 ± 2.3 | 24.4 ± 1.9 | 5.5 (4.2-6.9) | 29.1 | <.001 |
| 40° of flexion | |||||
| 0 N | 14.9 ± 2.2 | 18.8 ± 2.0 | 4.9 (2.9-6.9) | 26.2 | .001 |
| 20 N | 19.1 ± 2.8 | 24.7 ± 2.7 | 5.8 (3.8-7.7) | 30 | <.001 |
a MPFC, medial patellofemoral complex.
b All P values indicate statistically significant difference between the intact and deficient states (P < .05).
Figure 3.
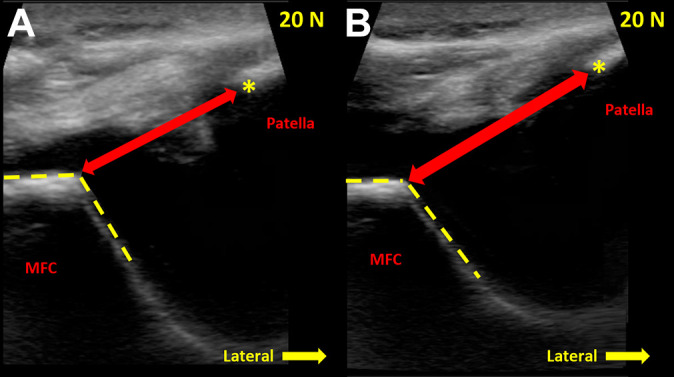
Ultrasound images demonstrating the medial patellofemoral distance between the apex of the medial trochlea (dashed yellow lines) and the medial facet of the patella (asterisks) in MPFC-intact and MPFC-deficient states at 20° of knee flexion under a 20-N load. Ultrasound images showing (A) the medial patellofemoral distance in the intact state and (B) the increased medial patellofemoral distance in the MPFC-deficient state. MFC, medial femoral condyle; MPFC, medial patellofemoral complex.
The ROC curve analysis revealed that the AUC for predicting MPFC deficiency was greatest at 20° of knee flexion. Results are summarized in Table 2. At 20° of knee flexion without a laterally directed force, AUC was 0.89 (95% CI, 0.65-0.98), indicating a high accuracy of the diagnostic test. Using the Youden J statistic, the optimal threshold of medial patellofemoral distance to distinguish MPFC deficiency from an intact knee in this condition was 14.8 mm (sensitivity = 77.8%; specificity = 100%; accuracy = 88.9%). When loaded with 20 N of laterally directed force at 20° of knee flexion, the AUC for predicting MPFC insufficiency had a score of 0.93 (95% CI, 0.70-0.99) in ROC curve analysis, indicating high accuracy of the diagnostic test. In this condition, the threshold for identifying MPFC insufficiency was a medial patellofemoral distance of 19.2 mm (sensitivity = 77.8%; specificity = 100%; accuracy = 88.9%).
Table 2.
Cutoff Values for Medial Patellofemoral Distance in Each Testing Condition and Their Corresponding Sensitivities and Specificities for the Detection of MPFC Deficiency a
| Testing Condition | Cutoff, mm | AUC (95% CI) | Sensitivity, % | Specificity, % | Accuracy, % | PPV, % | NPV, % |
|---|---|---|---|---|---|---|---|
| 0° of flexion | |||||||
| 0 N | 13.8 | 0.83 (0.58-0.96) | 88.9 | 77.8 | 83.4 | 80 | 87.5 |
| 20 N | 17.6 | 0.78 (0.52-0.94) | 100 | 55.6 | 77.8 | 69.3 | 100 |
| 10° of flexion | |||||||
| 0 N | 14.4 | 0.69 (0.43-0.88) | 100 | 44.4 | 72.2 | 64.3 | 100 |
| 20 N | 18.4 | 0.62 (0.36-0.83) | 88.9 | 55.6 | 72.3 | 66.7 | 83.4 |
| 20° of flexion | |||||||
| 0 N | 14.8 | 0.89 (0.65-0.98) | 77.8 | 100 | 88.9 | 100 | 81.8 |
| 20 N | 19.2 | 0.93 (0.70-0.99) | 77.8 | 100 | 88.9 | 100 | 81.8 |
| 30° of flexion | |||||||
| 0 N | 14.9 | 0.59 (0.34-0.81) | 66.7 | 66.7 | 66.7 | 66.7 | 66.7 |
| 20 N | 20.0 | 0.76 (0.51-0.93) | 77.8 | 77.8 | 77.8 | 77.8 | 77.8 |
| 40° of flexion | |||||||
| 0 N | 15.6 | 0.77 (0.51-0.93) | 66.7 | 88.9 | 77.8 | 85.7 | 72.8 |
| 20 N | 20.7 | 0.87 (0.64-0.98) | 77.8 | 100 | 88.9 | 100 | 81.8 |
a AUC, area under the curve; MPFC, medial patellofemoral complex; NPV, negative predictive value; PPV, positive predictive value.
Discussion
This study demonstrates the utility of dynamic ultrasound imaging to distinguish between intact and MPFC-deficient knees and highlights its potential clinical utility in the evaluation of the patellofemoral joint. We found a significant increase in medial patellofemoral distance when the MPFC fibers were transected as compared with intact knees. Furthermore, measurements of the medial patellofemoral distance could detect MPFC insufficiency with a high level of accuracy.
The MPFC has been described as the primary medial stabilizer to lateral patellar translation, and insufficiency of this complex is associated with patellar dislocations. 8,13,35 MPFC deficiency can be challenging to diagnose, and its assessment requires quantification of patellar mobility during applied stress. Hautamaa et al 9 investigated the role of the medial ligamentous stabilizers of the patella in restraining lateral displacement at 30° of knee flexion under 5 lb of medial and laterally directed force, which is equivalent to 22 N. In their cadaveric study, the authors used a displacement sensor to quantify lateral patellar displacement and reported that the stressed lateral patellar position was 9.3 ± 0.9, 13.8 ± 1.2, and 7.0 ± 1.0 mm in the intact state, after transectioning, and after repair of the MPFL, respectively. They reported a 50% increase in lateral patellar displacement between the MPFL-intact and MPFL-deficient states. In our study, when using a similar laterally directed force of 20 N at 30° of knee flexion, we also found an increase in medial patellofemoral distance from 18.9 ± 2.3 to 24.4 ± 1.9 mm, with a 29.1% increase in lateral patellar position in the MPFC-intact vs MPFC-deficient knees. However, because we did not perform MPFC repair or reconstruction in this study, we were unable to quantify lateral patellar position after repair. In contrast to the use of displacement sensors, ultrasound evaluation can provide a clinical, dynamic, noninvasive tool to evaluate the patellofemoral joint and can occur at the point of care with ease in obtaining comparison images of the uninjured contralateral knee.
The utility of ultrasound in assessing the patellofemoral joint was initially described by Shih et al. 26 In this study, the authors utilized a modified functional knee brace with an ultrasound transducer mounted lateral to the femur in individuals without symptoms of patellar instability. Mediolateral patellar translation was quantified from 0° to 90° of knee flexion while the participants performed sitting, squatting, and stepping tests. The authors reported a linear increase in lateral patellar position with increasing knee flexion from 0° to 50° during activities of standing and stepping. The authors reported this method of ultrasound measurement to have good reproducibility, and the mean error for the accuracy of ultrasound measurements closely matched measurements derived from static MRI, with deviation of only 0.6 ± 1.9 mm. In our study, we similarly identified an increase in lateral patellar position from extension to 40° of flexion, and this pattern was present in the intact and MPFC-deficient states.
Herrington and Pearson 11 described the use of patellofemoral ultrasound by placing the probe on the lateral edge of the superior border of the patella to assess patellar tracking in healthy individuals. They incorporated electrical stimulation of the vastus medialis obliquus and vastus lateralis muscles with the knee in 20° of flexion. They found that contraction of the vastus medialis obliquus resulted in a mean medial displacement of 6.8 ± 2.9 mm at the patella and that contraction of the vastus lateralis resulted in a mean lateral displacement of 5.6 ± 2.7 mm. Therefore, they determined that ultrasound assessment was a reliable technique for dynamically assessing patellar position during muscle contraction. In our study, we placed the ultrasound probe on the medial aspect of the joint, which we found to be not only applicable in assessing greater patellar lateralization in knees that are MPFC deficient but also reproducible in terms of technique (ICCs for intra- and interrater reliability were 0.99 and 0.98, respectively). In addition, we performed dynamic assessment based on an external, laterally directed force of 20 N, which led to a mean medial patellofemoral distance of 18.3 ± 1.9 mm at 20° of flexion in knees with MPFC deficiency. As our in vitro study aimed to find a reproducible method of quantifying patellar motion, further clinical studies are needed to compare the utility and applicability of our ultrasound imaging technique in the clinical setting.
Dynamic imaging of the patellofemoral joint is not routinely utilized to evaluate patellar translation in the setting of MPFC-deficient knees, 11,26 although several prior studies have done so using other imaging modalities, such as radiographs, CT, and MRI. 1,22,23,33,38 Teitge et al 36 investigated lateral patellar translation in patients with unilateral patellar instability using stress radiographs. In this study, the authors performed bilateral axial knee radiographs at 35° of knee flexion under 71 N of laterally directed force. The lateral patellar position was measured by quantifying the distance between the peak of the medial femoral condyle and the medial border of the patella. The authors reported that the stressed lateral patellar position was 21.9 ± 6.20 and 14.4 ± 4.45 mm on the injured and uninjured sides, respectively. In our study, we used similar landmarks for measurement using ultrasound evaluation, and despite using a smaller laterally directed force of 20 N, our findings were similar with 24.4 ± 1.9 and 18.9 ± 2.3 mm in the MPFC-deficient vs MPFC-intact knees at 30° of knee flexion.
Leal et al 16 introduced the Porto Patellofemoral Testing Device (PPTD) and performed MRI-based stress testing of the bilateral patellofemoral joints using PPTD at 0° and 30° of knee flexion. Lateral patellar position was calculated as the distance between a line through the deepest point of the trochlear groove and a line through the center of the patellar ridge, along the axis of the posterior condylar line. The authors reported the device to have a reproducible stress-force application with excellent intrarater agreement on measurements. They also found that PPTD resulted in greater lateral patellar translation with more accurate measurements than manual translation under maximum force, which averaged 30 N of laterally directed force. In our study, we utilized a smaller force of 20 N, which was standardized with a force gauge. Further studies are needed to identify the optimal stress placed on the patella during examination for reproducibility and diagnostic sensitivity while maintaining patient comfort.
Dynamic imaging evaluation of the patellofemoral joint has been shown to be valuable in assessing for patellar instability without the application of an external force. Burke et al 1 dynamically evaluated patellar position on MRI between 0° and 30° of knee flexion, using continuous real-time radial gradient echo in patients with and without patellar instability. They highlighted that lateral patellar maltracking, as defined by >2 mm of patellar lateralization, was the most sensitive parameter to detect patellar instability. They demonstrated that lateral patellar tracking was significantly greater in the symptomatic group (4.4 mm) as compared with healthy volunteers (1.5 mm). Using another modality, Tanaka et al 33 evaluated the utility of dynamic kinetic CT by quantifying patellar lateralization and its correlation with symptoms of patellar instability. They found that severity of patellar lateralization in knee extension correlated with the presence of patellar instability and that >3 quadrants of patellar lateralization in extension had a sensitivity of 93% in detecting patellar instability. While our study was based on cadaveric specimens and did not involve active knee extension, we similarly found that the medial patellofemoral distance, without imparting a lateralizing force, also significantly increased with MPFC injury at all flexion angles and could be used to predict the presence of instability at 20° of knee flexion with a high degree of accuracy.
Limitations
This study has several limitations. First, the cadaveric knees were normal knees that did not have abnormal anatomic risk factors for patellar instability. While this allowed for isolation of the effect of MPFC deficiency on patellar position, our findings may not reflect the measurements of symptomatic knees with this condition that have anatomic risk factors. Second, while resting tension was placed on the rectus femoris muscle, this force may not reflect that of a patient who may have guarding or muscle activation during clinical examination; further evaluation of this measurement in the clinical setting is needed. Finally, although each specimen was evaluated for evidence of previous trauma and arthritic changes, the orthopaedic and clinical history regarding prior knee injury was unavailable for each knee.
Conclusion
Using dynamic ultrasound assessment, we found that medial patellofemoral distance significantly increases with disruption of the MPFC, and such measurements can be used to accurately detect the presence of complete MPFC injury. Dynamic ultrasound allows quantitative assessment of MPFC insufficiency in multiple clinical settings. Future clinical studies are recommended to assess the utility of measurement thresholds in diagnosing and treating patellar instability.
Footnotes
Final revision submitted January 26, 2022; accepted March 8, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: C.W.D. has received education payments from Arthrex; consulting fees from Cartiva, Stryker, Wright Medical, and Zimmer Biomet; speaking fees from Wright Medical; and royalties from Extremity Medical. M.J.T. has received grant support from DJO and education payments from Kairos Surgical and Supreme Orthopedic Systems. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Burke CJ, Kaplan D, Block T, et al. Clinical utility of continuous radial magnetic resonance imaging acquisition at 3 T in real-time patellofemoral kinematic assessment: a feasibility study. Arthroscopy. 2018;34(3):726–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Camp CL, Stuart MJ, Krych AJ, et al. CT and MRI measurements of tibial tubercle–trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med. 2013;41(8):1835–1840. [DOI] [PubMed] [Google Scholar]
- 3. Cancienne JM, Christian DR, Redondo ML, et al. The biomechanical effects of limited lateral retinacular and capsular release on lateral patellar translation at various flexion angles in cadaveric specimens. Arthrosc Sports Med Rehabil. 2019;1(2):e137–e144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Christian DR, Redondo ML, Cancienne JM, et al. Differential contributions of the quadriceps and patellar attachments of the proximal medial patellar restraints to resisting lateral patellar translation. Arthroscopy. 2020;36(6):1670–1676. [DOI] [PubMed] [Google Scholar]
- 5. d’Entremont AG, Nordmeyer-Massner JA, Bos C, Wilson DR, Pruessmann KP. Do dynamic-based MR knee kinematics methods produce the same results as static methods? Magn Reson Med. 2013;69(6):1634–1644. [DOI] [PubMed] [Google Scholar]
- 6. Fithian DC, Mishra DK, Balen PF, Stone ML, Daniel DM. Instrumented measurement of patellar mobility. Am J Sports Med. 1995;23(5):607–615. [DOI] [PubMed] [Google Scholar]
- 7. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114–1121. [DOI] [PubMed] [Google Scholar]
- 8. Fulkerson JP, Edgar C. Medial quadriceps tendon-femoral ligament: surgical anatomy and reconstruction technique to prevent patella instability. Arthrosc Tech. 2013;2(2):e125–e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res. 1998;349:174–182. [DOI] [PubMed] [Google Scholar]
- 10. Heidenreich MJ, Sanders TL, Hevesi M, et al. Individualizing the tibial tubercle to trochlear groove distance to patient specific anatomy improves sensitivity for recurrent instability. Knee Surg Sports Traumatol Arthrosc. 2018;26(9):2858–2864. [DOI] [PubMed] [Google Scholar]
- 11. Herrington L, Pearson S. The applicability of ultrasound imaging in the assessment of dynamic patella tracking: a preliminary investigation. Knee. 2008;15(2):125–127. [DOI] [PubMed] [Google Scholar]
- 12. Huddleston HP, Campbell KJ, Madden BT, et al. The quadriceps insertion of the medial patellofemoral complex demonstrates the greatest anisometry through flexion. Knee Surg Sports Traumatol Arthrosc. 2021;29(3):757–763. [DOI] [PubMed] [Google Scholar]
- 13. Kang HJ, Wang F, Chen BC, et al. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1511–1516. [DOI] [PubMed] [Google Scholar]
- 14. Kruckeberg BM, Chahla J, Moatshe G, et al. Quantitative and qualitative analysis of the medial patellar ligaments: an anatomic and radiographic study. Am J Sports Med. 2018;46(1):153–162. [DOI] [PubMed] [Google Scholar]
- 15. Kujala UM, Osterman K, Kvist M, Aalto T, Friberg O. Factors predisposing to patellar chondropathy and patellar apicitis in athletes. Int Orthop. 1986;10(3):195–200. [DOI] [PubMed] [Google Scholar]
- 16. Leal A, Andrade R, Hinckel BB, et al. A new device for patellofemoral instrumented stress-testing provides good reliability and validity. Knee Surg Sports Traumatol Arthrosc. 2020;28(2):389–397. [DOI] [PubMed] [Google Scholar]
- 17. Lester JD, Watson JN, Hutchinson MR. Physical examination of the patellofemoral joint. Clin Sports Med. 2014;33(3):403–412. [DOI] [PubMed] [Google Scholar]
- 18. Lubowitz JH, Bernardini BJ, Reid JB. Current concepts review: comprehensive physical examination for instability of the knee. Am J Sports Med. 2008;36(3):577–594. [DOI] [PubMed] [Google Scholar]
- 19. Magnussen RA, Verlage M, Stock E, et al. Primary patellar dislocations without surgical stabilization or recurrence: how well are these patients really doing? Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2352–2356. [DOI] [PubMed] [Google Scholar]
- 20. Mochizuki T, Nimura A, Tateishi T, et al. Anatomic study of the attachment of the medial patellofemoral ligament and its characteristic relationships to the vastus intermedius. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):305–310. [DOI] [PubMed] [Google Scholar]
- 21. Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364(8):749–757. [DOI] [PubMed] [Google Scholar]
- 22. Nha KW, Papannagari R, Gill TJ, et al. In vivo patellar tracking: clinical motions and patellofemoral indices. J Orthop Res. 2008;26(8):1067–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Niimoto T, Deie M, Adachi N, Usman MA, Ochi M. Quantitative stress radiography of the patella and evaluation of patellar laxity before and after lateral release for recurrent dislocation patella. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2408–2413. [DOI] [PubMed] [Google Scholar]
- 24. Rosa SB, Ewen PM, Doma K, Ferrer JFL, Grant A. Dynamic evaluation of patellofemoral instability: a clinical reality or just a research field? A literature review. Orthop Surg. 2019;11(6):932–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schoettle PB, Zanetti M, Seifert B, et al. The tibial tuberosity–trochlear groove distance; a comparative study between CT and MRI scanning. Knee. 2006;13(1):26–31. [DOI] [PubMed] [Google Scholar]
- 26. Shih YF, Bull AM, McGregor AH, Amis AA. Active patellar tracking measurement: a novel device using ultrasound. Am J Sports Med. 2004;32(5):1209–1217. [DOI] [PubMed] [Google Scholar]
- 27. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420. [DOI] [PubMed] [Google Scholar]
- 28. Siebold R, Borbon CA. Arthroscopic extraarticular reconstruction of the medial patellofemoral ligament with gracilis tendon autograft—surgical technique. Knee Surg Sports Traumatol Arthrosc. 2012;20(7):1245–1251. [DOI] [PubMed] [Google Scholar]
- 29. Sillanpää P, Mattila VM, Iivonen T, Visuri T, Pihlajamäki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40(4):606–611. [DOI] [PubMed] [Google Scholar]
- 30. Skalley TC, Terry GC, Teitge RA. The quantitative measurement of normal passive medial and lateral patellar motion limits. Am J Sports Med. 1993;21(5):728–732. [DOI] [PubMed] [Google Scholar]
- 31. Steensen RN, Bentley JC, Trinh TQ, Backes JR, Wiltfong RE. The prevalence and combined prevalences of anatomic factors associated with recurrent patellar dislocation: a magnetic resonance imaging study. Am J Sports Med. 2015;43(4):921–927. [DOI] [PubMed] [Google Scholar]
- 32. Tanaka MJ, Chahla J, Farr J, et al. Recognition of evolving medial patellofemoral anatomy provides insight for reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2537–2550. [DOI] [PubMed] [Google Scholar]
- 33. Tanaka MJ, Elias JJ, Williams AA, Demehri S, Cosgarea AJ. Characterization of patellar maltracking using dynamic kinematic CT imaging in patients with patellar instability. Knee Surg Sports Traumatol Arthrosc. 2016;24(11):3634–3641. [DOI] [PubMed] [Google Scholar]
- 34. Tanaka MJ, Mirochnik K, Esfahani SA, et al. Arthroscopic patellofemoral measurements can reliably assess patellar instability. Arthroscopy. 2022;38(3):902–910. [DOI] [PubMed] [Google Scholar]
- 35. Tanaka MJ, Voss A, Fulkerson JP. The anatomic midpoint of the attachment of the medial patellofemoral complex. J Bone Joint Surg Am. 2016;98(14):1199–1205. [DOI] [PubMed] [Google Scholar]
- 36. Teitge RA, Faerber WW, Des Madryl P, Matelic TM. Stress radiographs of the patellofemoral joint. J Bone Joint Surg Am. 1996;78(2):193–203. [DOI] [PubMed] [Google Scholar]
- 37. Tsai CH, Hsu CJ, Hung CH, Hsu HC. Primary traumatic patellar dislocation. J Orthop Surg Res. 2012;7:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Williams AA, Elias JJ, Tanaka MJ, et al. The relationship between tibial tuberosity–trochlear groove distance and abnormal patellar tracking in patients with unilateral patellar instability. Arthroscopy. 2016;32(1):55–61. [DOI] [PubMed] [Google Scholar]


