Abstract
Background:
Cancer-related cognitive impairment (CRCI) is a significant problem for cancer patients, as the number of cancer survivors experiencing cognitive impairments is increasing in the absence of standard treatment. There have been attempts to improve the cognitive function of patients with cancer using acupuncture; however, no studies have been conducted using electroacupuncture. Thus, we designed a preliminary study to investigate the feasibility of a clinical trial using electroacupuncture in CRCI patients.
Methods:
We conducted a single-arm, pilot, clinical trial to investigate the feasibility of a study protocol for further large-scale clinical trials of electroacupuncture in CRCI patients. All participants were treated with electroacupuncture twice a week for 30 minutes at a time, for 8 weeks on acupoints GV20, GV24, EX-HN1, and GB20, HT7, PC6, and KI3. Both subjective and objective outcomes of cognitive function, quality of life (QoL), and psychological factors were measured in all participants at baseline, week 4, 8, and 12. For safety assessment, vital signs, laboratory examinations, and adverse events (AEs) were observed throughout the trial.
Results:
A total of 12 participants were enrolled at Daejeon and Dunsan Korean Medicine Hospital of Daejeon University from 21 April 2017 to 31 January 2018. After 8 weeks of treatment, electroacupuncture significantly improved both subjective and objective cognitive outcomes, including the perceived cognitive impairments scale of the Functional Assessment of Cancer Therapy-Cognitive Function, QoL scale of the European Organization for Research and Treatment of Cancer Quality of Life Core Questionnaire-C30, Korean version of Montreal Cognitive Assessment, Boston Naming Test, Seoul Verbal Learning Test, and Rey Complex Figure Test. During the entire trial period, 19 AEs were observed, with no serious AEs. Additionally, it was found that all feasibility outcomes, including recruitment, completion, and adherence rates, achieved successful results as the ratio exceeded 0.8.
Conclusion:
Our study results revealed that electroacupuncture improved cognitive complaints in cancer patients, and we expect electroacupuncture to be a safe and effective management therapy for CRCI patients. These feasibility trial results will be used as preliminary data for future randomized controlled clinical trials.
Trial registration number:
Korean Clinical Trial Registry (KCT0002168).
Keywords: electroacupuncture, cancer-related cognitive impairment, cancer, integrative medicine, feasibility clinical trial
Background
Advances in cancer treatments, including chemotherapy, radiation therapy, and targeted biological therapies, have greatly improved the overall survival. However, these treatments are often associated with various side effects such as immune dysfunction, fatigue, depression, and cognitive impairment, consequently reducing the quality of life (QoL). 1 Cognitive complaints after cancer and its treatment, also referred to as cancer-related cognitive impairment (CRCI), are among the most frequently reported symptoms in both cancer patients and survivors. 2 As many as 75% of cancer patients have reported problems with memory, executive functioning, attention, or feelings of mental slowness. Current longitudinal studies also indicate that up to 30% of cancer patients have detectable cognitive impairment prior to treatment, up to 75% experience cognitive decline during treatment, and up to 35% exhibit deterioration in cognition several years after the completion of treatment. 3
Cognitive impairment is a complex problem that has been associated with symptoms such as depression, anxiety, and fatigue, which can negatively affect QoL, work ability, self-confidence, and even social relationships. These cognitive deficits may also interfere with adherence to treatment plans, thereby reducing survival rates and increasing other side effects. Additionally, individuals have been reported to experience long-term cognitive alterations for as long as 21 years after cancer treatment. 4
Despite the high prevalence and deleterious side effects of CRCI, no definite treatments for CRCI have been recommended. According to the National Comprehensive Cancer Network guidelines, non-pharmacologic interventions are recommended for CRCI patients, with pharmacologic interventions as a last line of therapy in survivors for whom other interventions have been insufficient. 5 However, non-pharmacologic treatments including cognitive training and physical activity interventions still need additional studies to establish their efficacy 6 and the study results of pharmacologic interventions such as methylphenidate or modafinil are inconsistent. 7
As current treatment approaches for the management of CRCI are limited, there have been attempts to improve the cognitive function of patients with cancer using acupuncture. 8 Acupuncture, an integrative modality that originated from Oriental Medicine, has been used to treat diverse diseases with little risk and rare complications, showing its safety and effectiveness.9,10 A large amount of evidence confirms that acupuncture is safe and effective in treating cancer-related symptoms, including nausea, pain, anxiety, fatigue, and sleep disturbance, 11 as well as mild cognitive impairment (MCI) in Alzheimer’s disease. 12 Moreover, recent studies have also reported the effectiveness of acupuncture in CRCI.13-16
Similarly, several studies of electroacupuncture, which stimulate acupoints by electrical stimulation via inserted acupuncture needles, 17 have shown its efficacy in various neurological diseases, including MCI,18,19 dementia, 20 and Parkinson’s disease. 21 Compared with acupuncture, electroacupuncture has reported to produce a higher intensity of stimulation on acupoints and is progressively being widely used for its adjustable strength, frequency and easy quantification in the clinic. 22 However, studies targeting CRCI treatment using electroacupuncture have not yet been conducted. Thus, we designed a preliminary study to investigate the feasibility of a clinical trial of electroacupuncture for treating CRCI. The aim of this study was to investigate diverse clinical features of CRCI patients, including patient-report complaints, neuropsychological tests, quality of life, and psychological problems as a preliminary clinical study to help design a future confirmatory study.
Methods
Study Design
This study is a single-arm, pilot, clinical trial to investigate the feasibility of planned design, interventions, and outcome measures and to facilitate a power calculation for further large-scale clinical trials of electroacupuncture in CRCI patients. The trial was conducted at Daejeon and Dunsan Korean Medicine Hospital of Daejeon University, from 23 November 2016 to 31 January 2018. A total of 12 out of 15 originally planned patients were enrolled, and 10 completed the trial. The other 2 dropped out during the trial due to the lack of time for 1 participant and the other due to inconvenience of the intervention. Participants who voluntarily signed a written informed consent form were screened for eligibility evaluation based on the inclusion and exclusion criteria. Eligible participants visited the hospital in the next 2 weeks to start administering a total of 16 electroacupuncture treatments twice a week for 8 weeks. Efficacy outcomes were evaluated at baseline (week 0), after 4 weeks, after 8 weeks (end of treatment), and after 12 weeks (follow-up). The feasibility outcomes, recruitment rate, completion rate, and adherence rate were also evaluated. All participant data were coded, and all information was kept confidential.
This study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines and Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) (Table 1). 23 The study protocol was approved by the Institutional Review Board (IRB) of Daejeon and the Dunsan Korean Medicine Hospital of Daejeon University (No. DJOMC-139-1, DJDSKH-17-BMM-05) registered at the Clinical Research Information Service (KCT0002168).
Table 1.
Checklist for Items in STRICTA 2010.
| Item | Detail | Page number |
|---|---|---|
| 1. Acupuncture rationale | (1a) Style of acupuncture (eg, Traditional Chinese Medicine, Japanese, Korean, Western medical, Five Element, ear acupuncture, etc) | p.4 |
| (1b) Reasoning for treatment provided, based on historical context, literature sources, and/or consensus methods, with references where appropriate | p.4 | |
| (1c) Extent to which treatment was varied | p.4 | |
| 2. Details of needling | (2a) Number of needle insertions per subject per session (mean and range where relevant) | p.4 |
| (2b) Names (or location if no standard name) of points used (uni/bilateral) | p.4 | |
| (2c) Depth of insertion, based on a specified unit of measurement, or on a particular tissue level | p.4 | |
| (2d) Response sought (eg, de qi or muscle twitch response) | p.4 | |
| (2e) Needle stimulation (eg, manual, electrical) | p.4 | |
| (2f) Needle retention time | p.4 | |
| (2g) Needle type (diameter, length, and manufacturer or material) | p.4 | |
| 3. Treatment regimen | (3a) Number of treatment sessions | p.4 |
| (3b) Frequency and duration of treatment sessions | p.4 | |
| 4. Other components of treatment | (4a) Details of other interventions administered to the acupuncture group (eg, moxibustion, cupping, herbs, exercises, lifestyle advice) | p.4 |
| 4b) Setting and context of treatment, including instructions to practitioners, and information and explanations to patients | p.4 | |
| 5. Practitioner background | (5) Description of participating acupuncturists (qualification or professional affiliation, years in acupuncture practice, other relevant experience) | p.4 |
| 6. Control or comparator interventions | (6a) Rationale for the control or comparator in the context of the research question, with sources that justify this choice | - |
| (6b) Precise description of the control or comparator. If sham acupuncture or any other type of acupuncture-like control is used, provide details as for Items 1-3 above. | - |
Participants
Screening was conducted considering the inclusion and exclusion criteria, and finally 12 subjects were selected. Subjects were investigated for cancer history, previous anticancer treatment, diagnosis and pre-treatment of CRCI, Eastern Cooperative Oncology Group (ECOG) performance status, Functional Assessment of Cancer Therapy-Cognitive Function-perceived cognitive impairments (FACT-Cog-PCI), and Korean Vision of Mini-Mental State Exam (K-MMSE) to screen for eligibility.
Inclusion criteria were as follows: (1) aged equal to or more than 19 to under 75 years; (2) solid cancer occurred in adult age, 6 months after finishing cancer treatment (hormone therapy is allowed); (3) complaint of cognitive impairment with the FACT-Cog-PCI score <63 24 ; (4) cognitive impairment is supposed to be accompanied with cancer treatment; (5) ECOG performance status 0 to 2; (6) and provided written informed consent.
Subjects who satisfied any of the following criteria were excluded from this trial: (1) currently receiving any of cognitive rehabilitation therapy, herbal medicine, or conventional treatment for cognitive impairment or underwent these treatments within 2 weeks; (2) history of tumor in the central nervous system (CNS), intra-cranial radiotherapy, or intrathecal chemotherapy or history of CNS diseases which can affect cognitive function; (3) recurrence, metastasis, or progression of cancer; (4) history of psychological disorders including alcohol dependence, major depressive disorder, schizophrenia, or bipolar disorder; (5) K-MMSE score <20; (6) score in any field of HADS is equal to or greater than 11; (7) one or more of the following: platelet count ≤60 000/μL, hemoglobin <8 g/dL, or absolute neutrophil count <1000; (8) abnormal liver function test or renal function test values, serious hepatic/renal failure (equal to or more than 2-fold the upper limit of aspartate aminotransferase or alanine aminotransferase or creatinine ≥2.0 mg/dL); (9) suspected clinically significant inflammation with C-reactive protein ≥1.0 mg/L and white blood cell count >10 000/μL; (10) serum albumin value under normal range and poor oral intake; (11) seriously unstable medical condition such as abnormal condition demanding medical intervention or management; (12) life expectancy ≤6 months; (13) planning operation, chemotherapy, or radiotherapy during the clinical trial period; (14) receiving active treatment for anemia (erythropoietin or blood transfusion); (15) history of hypersensitivity reaction to acupuncture or electroacupuncture or difficulty in cooperating for the intervention; (16) inserted prosthesis which is inappropriate for electroacupuncture (pacemaker, a heart-lung machine, an electrocardiograph, etc.), or who has a risk for hypersensitivity reaction to electroacupuncture including epilepsy; (17) currently being enrolled on another clinical trial or 4 weeks have not passed after completion of the previous clinical trial; (18) pregnant women, lactating women, or planning for pregnancy; (19) difficulty in compliance with the treatment, visit, or response to questionnaires etc.
Intervention
All participants were treated with electroacupuncture twice a week for 30 minutes at a time, for 8 weeks. Subjects were needled at GV20, GV24, and EX-HN1, and both sides in GB20, HT7, PC6, and KI3 with a 5 to 20 mm depth of insertion using sterile, stainless steel, and disposable acupuncture needle (0.25 mm × 30 mm; Dongbang Acupuncture Inc., Seoul, Republic of Korea). The acupoint was selected based on previous studies25-28 and consensus among Korean medicine specialists of acupuncture and moxibustion and neuropsychiatry.
The intervention process was initiated with the manipulation of de qi, an irritating feeling of soreness, numbness, and heaviness considered to be indicative of effective needling. The intervention was conducted by licensed Korean medical doctors with more than 2 years of clinical experience. Participants were then treated with an electrostimulator (ES-160, Ito Co. Ltd., Tokyo, Japan) at the acupoint of both sides HT7 and PC6 at a frequency of 2 Hz and 80% intensity for 30 minutes. If needed, practitioners modulated the intensity and depth of acupuncture during treatment, and areas with lymphedema were excluded from the treatment.
Additional treatments for improving cognitive impairment were prohibited during the entire study period. Other medications were permitted at the discretion of the investigators. All drug information (name of product, purpose of administration, dosage, duration of administration, etc.) was recorded on the patient case report form.
Efficacy Outcome Measures
The primary outcome measure to evaluate the efficacy of electroacupuncture on CRCI was FACT-Cog (Version 3) after 8 weeks of treatment compared to the baseline (week 0). The FACT-Cog is a validated self-report questionnaire of perceived cognitive function and impact on QoL over 7 days, consisting of 37 questions on a 5-point Likert-type scale. As subjective complaints are key to the CRCI problem, we tried to evaluate patient-report complaints as our primary outcome measure. The FACT-Cog consists of 4 subscales: perceived cognitive impairments (PCI), perceived cognitive abilities (PCA), impact on quality of life (IQL), and comments from others (CFO). The individual subscale scores are summed to determine the total FACT-Cog score, ranging from 0 to 148, with a higher score indicating better cognitive function. 29
To assess cognitive function, QoL, and psychological problems to investigate various clinical features in cancer survivors with cognitive impairments, we evaluated Korean version of the Montreal Cognitive Assessment (MoCA-K), Seoul Neuropsychological Screening Battery (SNSB), European Organization for Research and Treatment of Cancer Quality of Life Core Questionnaire C30 (EORTC-QLQ-C30), and Hospital Anxiety and Depression Scale (HADS) as secondary outcomes.
To evaluate objective cognitive function in CRCI patients, we assessed MoCA-K and SNSB in all participants. Although it is known that objective neuropsychological tests do not always correlate with subjective complaints, objective outcomes are also important in detecting damage in focal lesions. MoCA-K is a cognitive screening instrument to detect MCI which assesses multiple cognitive domains including memory, language, executive functions, visuospatial skills, calculation, abstraction, attention, concentration, and orientation. 30 Additionally, MoCA-K is recommended for those who are in the normal range on the MMSE. 31 The other neuropsychological battery used in our study was the SNSB, which is also a standardized neuropsychological test battery widely used in Korea. The SNSB is composed of comprehensive cognitive tests evaluating the level of cognitive functioning and impairment of the following cognitive domains: attention, language and related functions, visuospatial functions, memory, frontal/executive functions, and other indexes. 32 It is useful for comparison by domain and for finding changes in cognitive function over time. In particular, it can sensitively evaluate early cognitive decline and estimate the cause of cognitive impairment by analyzing the pattern of cognitive decline. 33 To provide such information about cognitive domains, it contains a variety of subtests in each cognitive domain, including all 3 recommendations of a core set of neuropsychological tests by the International Cognition and Cancer Task Force (ICCTF). 34
All participants were requested to answer the EORTC-QLQ-C30 as a QoL measurement tool in CRCI patients. The EORTC-QLQ-C30 is a 30-item cancer-specific questionnaire assessing the health-related QoL of cancer patients. It comprises the QoL scale, 5 functional scales (physical function, role, emotion, cognition, and social function), 3 symptom scales (fatigue, nausea/vomiting, and pain) and scales for additional symptoms commonly reported in cancer patients (dyspnea, sleep disturbance, appetite loss, constipation, and diarrhea), and financial difficulties. 35 This provides us with more detailed clinical information that affects daily life. The HADS was used in this study to assess psychological symptoms such as anxiety and depression. The HADS is a simple and easy-to-use questionnaire which was developed to identify anxiety and depression among patients in non-psychiatric hospital clinics. It is divided into an anxiety subscale (HADS-A) and a depression subscale (HADS-D), both of which contain 7 items.36,37 As psychological problems are one of the major factors affecting cognitive impairment, it is important to evaluate the participants’ psychological symptoms throughout the trial. 38
Feasibility Outcomes
To test the feasibility of a clinical trial, we assessed the recruitment, completion, and adherence rates. The recruitment rate was defined as the ratio of the number of enrolled subjects to the number of target sample sizes, and the number of enrolled subjects per screening participant was reported together. The completion rate indicates the number of participants who completed the trial without protocol violations. Adherence rates were reported in 3 categories: trial visit (number of visits out of a total of 18 visits), treatment (the number of treatments completed out of a total of 16 treatments), and evaluation (the number of evaluations completed out of a total of 3 evaluations excluding the baseline evaluation of the primary outcome measure).
Safety Assessment
Safety was assessed in terms of vital signs (blood pressure, pulse, body temperature), laboratory examinations (liver function test, routine blood tests, and urine tests), and adverse events (AEs). The vital signs and AEs were evaluated at every visit, and laboratory tests were performed at screening and at week 8.
Sample Size and Statistical Analyses
The sample size calculation was based on previous studies, assuming the mean difference between FACT-Cog-PCI before and after electroacupuncture treatment was 15,39-41 with an SD of 18.2. 41 A total of 15 subjects were required, with a power of 80% and a 2-sided significance level of 5%, allowing a dropout rate of 20%.
All statistical analyses were performed by an independent statistician using SAS® (version 9.4, SAS Institute, Cary, North Carolina, USA). Continuous variables are presented as mean (95% confidence interval), and categorical variables are reported as frequencies (percentages). Statistical significance was accepted at a 2-sided test with an α-level of .05. The missing values were handled using a multiple imputation method. For efficacy outcome measures, Student’s paired t-test was used.
Results
Study Participants and Baseline Characteristics
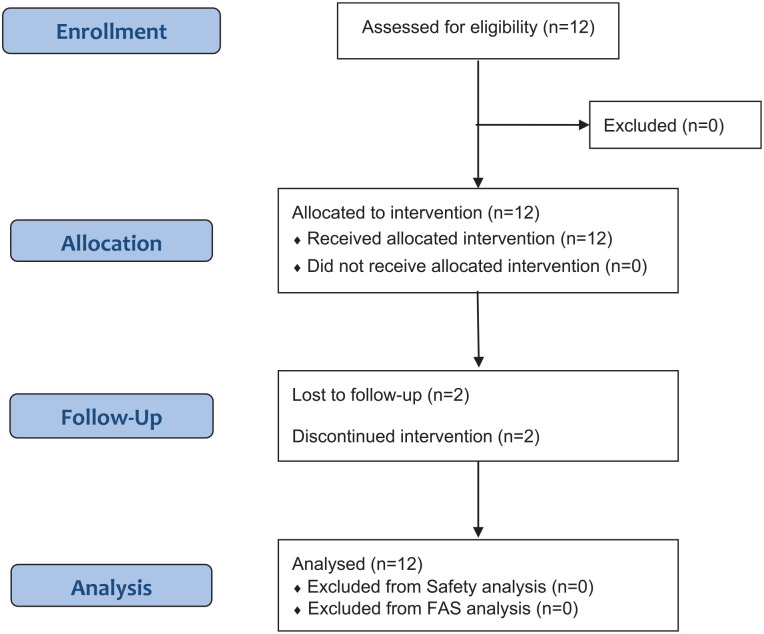
A total of 12 participants were assessed for eligibility, and none were excluded from the study. All 12 subjects were allocated to the treatment group and 10 completed the trial, and the other 2 were dropped out due to the withdrawal of consent inform (Figure 1). All enrolled 12 participants were included in the analysis, both in the safety and full analysis set (FAS).
Figure 1.
Flow chart for the study subjects.
The baseline characteristics of the participants are shown in Table 2. Overall, 10 female and 2 male participants, with an average age of 57.33 years were included in the trial. All except 1 subject were non-smokers and non-alcoho drinkers, and the majority of participants answered that they exercised more than 3 times a week.
Table 2.
Demographics and Baseline Characteristics.
| Characteristic | Electroacupuncture group (n = 12) |
|---|---|
| Gender (M/F) † | 2 (16.7%)/10 (83.3%) |
| Age (year) ‡ | 57.33 (52.40, 62.26) |
| Height (cm) ‡ | 160.43 (155.36, 165.49) |
| Weight (kg) ‡ | 62.47 (56.57, 68.37) |
| Smoking (yes/no) † | 1 (8.3%)/11 (91.7%) |
| Drink (yes/no) † | 1 (8.3%)/11 (91.7%) |
| Exercise (yes/no) † | 11 (91.7%)/1 (8.3%) |
| Exercise frequency, n (%) | |
| None | 1 (8.3%) |
| 1-2 times/week | 1 (8.3%) |
| 3-4 times/week | 5 (41.7%) |
| 5-6 times/week | 2 (16.7%) |
| 7 times/week | 3 (25%) |
| Education, year | 12.83 (11.19, 14.48) |
| Employment, n (%) | |
| Employed | 2 (16.7%) |
| Unemployed | 10 (83.3%) |
| Cancer type, n (%) | |
| Thyroid | 2 (16.7%) |
| Breast | 8 (66.7%) |
| Colon | 1 (8.3%) |
| Kidney | 1 (8.3%) |
| Stage of disease, n (%) | |
| Stage I | 3 (25.0%) |
| Stage II | 4 (33.3%) |
| Stage III | 1 (8.3%) |
| Stage IV | 1 (8.3%) |
| NED a | 3 (25.0%) |
| Prior anticancer treatment, n (%) | |
| Surgery | 12 (100%) |
| Chemotherapy | 9 (75%) |
| Radiotherapy | 3 (25%) |
| Others (hormone therapy) | 6 (50%) |
| ECOG performance status, n (%) | |
| 0 | 12 (100%) |
| Diagnosis of CRCI (yes /no) | 12 (100%)/0 (0%) |
| K-MMSE | 29 (28.25, 29.75) |
| Acupuncture Expectancy Score | 13.67 (11.08, 16.26) |
Abbreviations: ECOG, Eastern Cooperative Oncology Group; CRCI, cancer-related cognitive impairment; K-MMSE, Korean Vision of Mini-Mental State Exam.
NED indicates no evidence of cancer at the time of study entry.
Fisher’s exact test.
Student’s independent t-test.
Among the 12 participants, 8 were diagnosed with breast cancer, 2 with thyroid cancer, 1 with colon cancer, and 1 with kidney cancer, with varied stages in each participants from stage Ⅰ to Ⅳ. All 12 subjects had undergone surgery for cancer treatment, 9 had received chemotherapy, 3 received radiation therapy, and 6 received either hormonal therapy or targeted therapy. The ECOG performance status of all participants was recorded as 0, which means fully active and able to perform all pre-disease performance without restriction. 42 All 12 patients had been diagnosed with CRCI, and only one subject had previously been treated for CRCI. The K-MMSE score of all participants ranged from 27 to 30, with an average of 29. 43
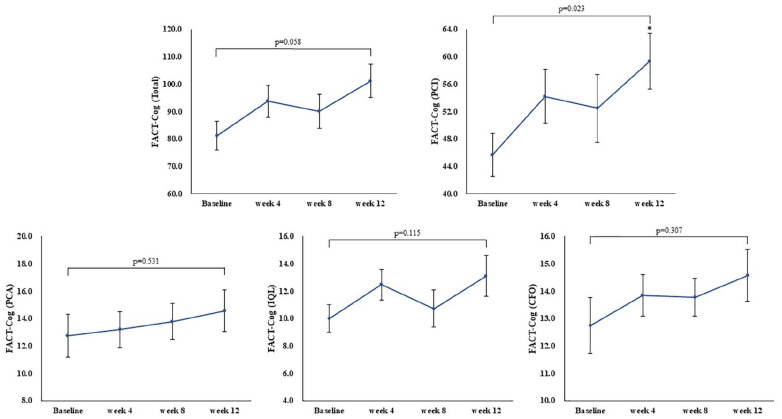
FACT-Cog
At baseline, the average score of FACT-Cog in all cancer participants was found to be 81.17, and scored 45.67, 12.75, 12.75, 10.00 in each subscale of PCI, PCA, CFO, and IQL, respectively. The baseline score of FACT-Cog was included in the lowest quartiles, as the quartile cut-off values of FACT-Cog were reported to be <121 points (lowest), 121 to 134 points, 134 to141 points, and >141 points (highest) in a previous study. 44 In addition, the PCI subscale scored an average of 45.67, exhibiting moderate to severe cognitive problems. 45
After treatment with electroacupuncture, the total FACT-Cog increased from 81.17 points at baseline (week 0) to 93.70 after 4 weeks (P = .145), 90.04 after 8 weeks (P = .326), and 101.14 after 12 weeks (P = .058). As for our primary outcome, the change in FACT-Cog between week 8 and baseline was calculated as 8.87 points which was not a significant difference, but exceeded the minimal clinically important difference (MCID) of FACT-Cog. The previously known MCID for FACT-Cog is 6.9 to 10.6 points, interpreted as an increase of 6.9 to 10.6 points in the FACT-Cog score is the smallest meaningful self-reported cognitive improvement. 46 In addition, the change in FACT-Cog was 12.54 points after 4 weeks and 19.98 points after 12 weeks, both of which also showed clinical improvements in cognitive function in CRCI patients (Figure 2).
Figure 2.
The total score and subscale of FACT-Cog at baseline (week 0), week 4, 8, and 12. All values are mean ± SE.
*Mean statistical significance within-group.
In the subscale analysis, the FACT-Cog-PCI score improved by 45.67 at baseline to 59.33 after 12 weeks of treatment, which demonstrated significant differences between pre- and post-treatment of electroacupuncture (P = .0227). The other subscales of FACT-Cog-PCA increased from 12.75 at baseline to 14.56 on week 12 (P = .531), FACT-Cog-IQL increased by 10.00 to 13.11 (P = .115) and FACT-Cog-CFO from 12.75 to 14.14 (P = .307), not showing significant differences after treatment.
MoCA-K
The average MoCA-K was 25.50 at baseline and increased to 27.73, 28.40, and 28.90 after 4, 8, and 12 weeks, respectively. Among the 7 subscales, it was found that the study participants scored relatively low on abstraction and delayed recall domains compared with healthy participants. 47
After electroacupuncture treatment, the total MoCA-K score significantly increased at weeks 4, 8, and 12 (P = .0074, .0010, .0003). Notably, the score on the delayed recall section significantly increased at every evaluation visit, beginning at a baseline score of 2.42 to 4.27 at week 4, 4.30 at week 8, and finally 4.40 at week 12 (P = .0007, .0002, .0004, respectively). Other visuospatial and executive sections also showed a significant increase at week 12, from 4.25 at baseline to 4.90 at week 12 (P = .0368). In the abstraction section, the score also increased after electroacupuncture treatment and ranked highest on week 8, demonstrating significant differences compared with baseline (P = .0368). For the other sections of naming, attention, language, and orientation, most participants answered all questions correctly on weeks 4, 8, or 12, and on some of the time period, all subjects scored perfect, as shown in Table 3.
Table 3.
MoCA-K in Electroacupuncture Group at Baseline (Week 0), Week 4, 8, and 12.
| MoCA-K | Visuospatial/executive | Naming | Attention | Language | Abstraction | Delayed recall | Orientation | Total |
|---|---|---|---|---|---|---|---|---|
| Baseline | 4.25 (3.70, 4.80) | 2.92 (2.73, 3.10) | 5.67 (5.25, 6.08) | 2.83 (2.59, 3.08) | 1.50 (1.17, 1.83) | 2.42 (1.84, 2.99) | 5.92 (5.73, 6.10) | 25.50 (24.50, 26.50) |
| Week 4 | 4.18 (3.59, 4.77) | 3.00 (cannot be estimated) | 5.73 (5.29, 6.16) | 2.82 (2.55, 3.09) | 1.73 (1.41, 2.04) | 4.27 (3.67, 4.88) | 6.00 (cannot be estimated) | 27.73 (26.68, 28.77) |
| P-value | .5884 | .3409 | .7787 | .9999 | .0816 | .0007 | .3409 | .0074 |
| Week 8 | 4.60 (4.10, 5.10) | 3.00 (cannot be estimated) | 5.60 (5.10, 6.10) | 3.00 (cannot be estimated) | 1.90 (1.67, 2.13) | 4.30 (3.82, 4.78) | 6.00 (cannot be estimated) | 28.40 (27.71, 29.09) |
| P-value | .5911 | .3409 | .7804 | .1679 | .0368 | .0002 | .3409 | .0010 |
| Week 12 | 4.90 (4.67, 5.13) | 3.00 (cannot be estimated) | 6.00 (cannot be estimated) | 3.00 (cannot be estimated) | 1.70 (1.35, 2.05) | 4.40 (3.80, 5.00) | 5.90 (5.67, 6.13) | 28.90 (28.19, 29.61) |
| P-value | .0368 | .3409 | .1934 | .1679 | .1679 | .0004 | .9999 | .0003 |
Bold values mean statistical significance within-group.
Abbreviation: MoCA-K, Korean version of the Montreal Cognitive Assessment.
SNSB
The study participants were evaluated using the SNSB second edition at baseline, week 8, and week 12. At baseline, we found that the participants had a slight decline in the visuospatial and memory domains. After the participants received treatment, they showed significant improvements in memory and language and related functions, among the domains of attention, language and related functions, visuospatial functions, memory, frontal/executive functions, and others. On the Boston Naming Test (BNT) which aims to evaluate language and related functions, the participants scored 51.70 on baseline, and consequently scored 53.90 on week 8 and 54.90 on week 12, both showing significant improvements (P = .0207, .0003) (Table 4). Additionally, on the Seoul Verbal Learning Test (SVLT) and Rey Complex Figure Test (RCFT) for immediate recall, delayed recall, and recognition, all scores significantly increased after electroacupuncture treatment for either 8 or 12 weeks. In the other domains, the scores were within the normal range at baseline and increased after electroacupuncture treatment, although there were no significant improvements. Moreover, after electroacupuncture treatment, the Short-Geriatric Depression Scale (SGDS), a tool for assessing the symptoms of depression, had shown a decrease by 3.20 at baseline to 1.5 on week 8 and 1.3 week 12, although not significant.
Table 4.
Major Findings in SNSB in Electroacupuncture Group at Baseline (Week 0), Week 8, and Week 12.
| Attention |
Language and related
functions |
Visuospatial functions |
||||
|---|---|---|---|---|---|---|
| Digit span test-forward |
Digit span test-backward |
BNT |
Calculation |
RCFT-copy score |
RCFT-copy time (sec) |
|
| Baseline | 6.60 (5.83, 7.37) | 4.40 (3.80, 5.00) | 51.70 (49.76, 53.64) | 11.20 (10.26, 12.14) | 32.75 (29.69, 35.81) | 131.70 (96.44, 166.96) |
| Week 8 | 6.90 (6.04, 7.76) | 4.70 (3.80, 5.60) | 53.90 (51.84, 55.96) | 11.40 (10.71, 12.09) | 34.40 (33.50, 35.30) | 132.60 (87.14, 178.06) |
| P-value | .4344 | .3434 | .0207 | .5554 | .2155 | .9491 |
| Week 12 | 7.10 (6.24, 7.96) | 4.40 (3.71, 5.09) | 54.90 (53.38, 56.42) | 11.20 (10.46, 11.94) | 34.50 (33.14, 35.86) | 123.30 (75.35, 171.25) |
| P-value | .2126 | .9999 | .0003 | .9999 | .1011 | .6009 |
| Memory | ||||||
| SVLT-immediate recalls | SVLT-delayed recall | SVLT-recognition | RCFT-immediate recalls | RCFT-delayed recall | RCFT-recognition | |
| Baseline | 20.50 (18.71, 22.29) | 6.10 (4.91, 7.29) | 20.50 (19.18, 21.82) | 17.30 (11.02, 23.58) | 18.30 (13.59, 23.01) | 19.60 (18.42, 20.78) |
| Week 8 | 24.30 (22.30, 26.30) | 7.30 (5.04, 9.56) | 22.10 (20.82, 23.38) | 22.70 (17.59, 27.81) | 22.00 (16.46, 27.54) | 21.10 (20.39, 21.81) |
| P-value | .0168 | .3051 | .0487 | .0004 | .0216 | .0258 |
| Week 12 | 26.40 (23.38, 29.42) | 9.40 (8.13, 10.67) | 22.10 (20.73, 23.47) | 24.05 (18.70, 29.40) | 23.60 (18.18, 29.02) | 21.10 (19.91, 22.29) |
| P-value | .0070 | <0.0001 | .0570 | .0005 | .0035 | .0341 |
| Frontal/executive functions | Others | |||||
| COWAT-animal, supermarket | COWAT-phonemic | K-TMT-e (part A) | K-TMT-e (part B) | K-MMSE | SGDS | |
| Baseline | 37.40 (31.24, 43.56) | 27.90 (20.26, 35.54) | 19.10 (14.75, 23.45) | 25.10 (16.97, 33.23) | 29.00 (28.25, 29.75) | 3.20 (0.75, 5.65) |
| Week 8 | 37.60 (33.52, 41.68) | 30.10 (22.60, 37.60) | 16.50 (11.00, 22.00) | 26.10 (16.89, 35.31) | 28.40 (27.43, 29.37) | 1.50 (0.66, 2.34) |
| P-value | .9337 | .2958 | .1233 | .4997 | .1114 | .1125 |
| Week 12 | 39.00 (35.43, 42.57) | 31.30 (26.12, 36.48) | 16.50 (12.38, 20.62) | 22.20 (16.64, 27.76) | 28.30 (27.54, 29.06) | 1.30 (0.47, 2.13) |
| P-value | .5457 | .2397 | .1043 | .2622 | .1727 | .0882 |
Bold values mean statistical significance within-group.
Abbreviations: SNSB, Seoul Neuropsychological Screening Battery; BNT, Boston Naming Test; RCFT, Rey Complex Figure Test; SVLT, Seoul Verbal Learning Test; COWAT, Controlled Oral Word Association Test; K-TMT-e, Korean Trail Making Test for the elderly; K-MMSE, The Korean Mini-Mental State Examination; SGDS, Short version of the Geriatric Depression scale.
EORTC-QLQ-C30
To assess the QoL of CRCI participants, the EORTC-QLQ-C30 was evaluated at baseline, week 4, 8, and 12. The EORTC-QLQ-C30 is divided into 3 sections: QoL scale, functional scale, and symptom scale. At baseline, the study participants showed relatively better functions on most of the scales when compared with the results previously reported for cancer patients in Korea. 35 It was found that the cognitive function was the only scale which had shown lower scores than previous studies, demonstrating that the major complaint affecting the whole QoL of the study participants was the decline of cognitive function.
After treatment, the QoL score increased from 55.56 at baseline to 61.56 on week 4, 67.58 on week 8, and 66.45 on week 12, indicating significant differences at week 8 (P = .0076) (Table 5). The other functional and symptom scales also improved after treatment with electroacupuncture, although both scale differences were non-significant. In the subtest analysis, there was a significant improvement in appetite loss after 12 weeks of electroacupuncture treatment (P = .0333) (Supplemental Data).
Table 5.
EORTC-QLQ-C30 in electroacupuncture group at baseline, week 4, 8, and 12.
| EORTC-QLQ-C30 | QOL scale |
Functional scale |
Symptom scale |
|||
|---|---|---|---|---|---|---|
| Mean (95% CI) | P-value | Mean (95% CI) | P-value | Mean (95% CI) | P-value | |
| Baseline | 55.56 (44.42, 66.69) | 70.00 (62.49, 77.51) | 21.15 (13.80, 28.51) | |||
| Week 4 | 61.56 (50.51, 72.60) | .2185 | 77.24 (65.01, 89.47) | .2799 | 19.70 (3.67, 35.72) | .8592 |
| Week 8 | 67.58 (58.92, 76.25) | .0076 | 79.39 (62.22, 96.56) | .2849 | 17.50 (0.00, 44.22) | .7865 |
| Week 12 | 66.45 (46.17, 86.73) | .3062 | 76.41 (42.80, 100.0) | .6969 | 17.41 (0.00, 44.90) | .7847 |
Bold values mean statistical significance within-group.
Abbreviations: EORTC-QLQ-C30, European Organization for Research and Treatment of Cancer Quality of Life Core Questionnaire C30; QOL, quality of life.
HADS
The study participants scored 4.75 and 5.42 in HADS-A and HADS-D respectively at baseline, both of which were under the anxiety and depression diagnostic criteria of 9 and 7. After 4, 8, and 12 weeks of treatment, the score slightly decreased to 4.65 and 4.99, indicating that the symptoms were well maintained throughout 12 weeks of the trial period (Table 6).
Table 6.
The Score of HADS in Electroacupuncture Group at Baseline, week 4, 8, and 12.
| HADS | HADS-A (anxiety) |
HADS-D (depression) |
||
|---|---|---|---|---|
| Mean (95% CI) | P-value | Mean (95% CI) | P-value | |
| Baseline | 4.75 (3.24, 6.26) | 5.42 (3.74, 7.10) | ||
| Week 4 | 4.93 (3.20, 6.65) | .7834 | 5.40 (3.24, 7.55) | .9729 |
| Week 8 | 4.50 (3.03, 5.96) | .5244 | 4.37 (2.46, 6.29) | .1635 |
| Week 12 | 4.65 (2.96, 6.33) | .8592 | 4.99 (3.39, 6.60) | .5013 |
Abbreviation: HADS, Hospital Anxiety and Depression Scale.
Feasibility Outcomes
Feasibility evaluations were performed at trial completion to aid in the design of further confirmatory studies. The recruitment rate was calculated as 0.8, as 12 participants were assessed for eligibility compared to the targeted sample size of 15. All 12 screened participants were enrolled in the trial, with no screening failures. The completion rate of this study was 0.83, owing to the 2 dropouts. Finally, the adherence rates of the trial visit, treatment, and evaluation were recorded as 0.84, 0.84, and 0.86, respectively. Over 80% of the subjects visited every planned visit, administered planned treatment, and complied with the planned evaluations. Overall, the recruitment, completion, and adherence rates achieved successful results as the ratio exceeded 0.8 (Table 7).
Table 7.
Feasibility Outcome.
| Recruitment rate | Completion rate | Adherence rate | |||
|---|---|---|---|---|---|
| Trial | Treatment | Evaluation | |||
| Ratio | 0.8 | 0.83 | 0.84 | 0.84 | 0.86 |
Credibility Assessment
The credibility of the electroacupuncture treatment increased after 8 weeks of treatment compared to baseline. The study participants answered more positively after electroacupuncture treatment for the following 4 topics: expectation effectiveness, logicality of treatment, recommendation intention, and chance of success. Notably, the biggest difference in scores was revealed in whether to recommend electroacupuncture to others (Figure 3).
Figure 3.
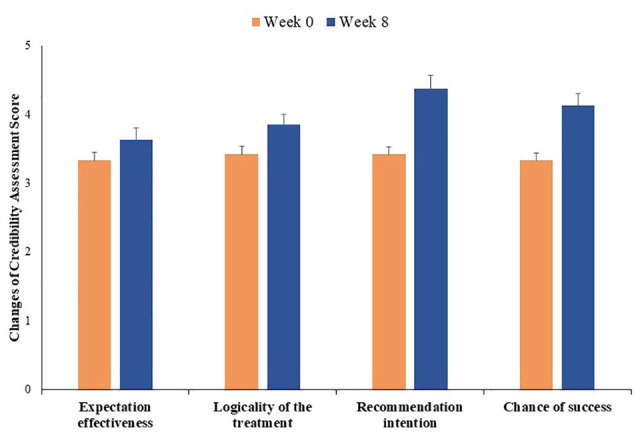
Credibility assessment at week 0 and 8. All values are mean ± SE.
Safety Assessment
A total of 19 AEs were observed during the trial period. The most common AE reported in this study was upper respiratory infection, involving 8 cases among 19 AEs. Other symptoms include dyspepsia, anorexia, enterocolitis, fatigue, insomnia, headache, and skin rash. None of the patients had serious AEs, and all were reported as mild or moderate. All except 1 event was considered irrelevant to the intervention, and 1 case with a complaint of headache, determined as moderate degree, was decided to be possibly related to intervention by investigators as an expected AE when treated with electroacupuncture. All reported AEs disappeared during the study period, and there were no significant differences in vital signs and laboratory examinations throughout the trial.
Discussion
CRCI is a significant problem for cancer patients, as the number of cancer survivors experiencing cognitive impairment is increasing in the absence of standard treatment to manage CRCI. It has been previously acknowledged that chemotherapy induces cognitive impairments, which are also known as chemobrain or chemofog; however, numerous longitudinal studies have suggested that cancer itself and other cancer treatments such as surgery, radiotherapy, targeted therapy, hormonotherapy, and immunotherapy promote biological processes associated with neurological deficits, although the definite mechanism and progression are largely unknown. 48 Nevertheless, some biological factors known to contribute to the development of CRCI are inflammation, neurotoxicity, the hypothalamic-pituitary-adrenal axis, and genetic polymorphisms. 49 To target these diverse factors, a variety of pharmacologic and non-pharmacologic interventions have been studied to manage cognitive alterations, 6 and studies using acupuncture and electroacupuncture have also been conducted to reveal its effectiveness.13-15
Acupuncture has long been shown to be effective in various systems and symptoms by activating neurophysiological effects and modulating the immune system, metabolism, and the gastrointestinal system. 50 In addition, acupuncture and electroacupuncture have shown improvements in cognitive function in Alzheimer’s disease by enhancing cholinergic neurotransmission and trophic factor release, protecting cerebral neurons from apoptosis and oxidative stress, improving synaptic plasticity, and reducing the levels of abnormal proteins. 51 Based on these previous results, we hypothesized that acupuncture and electroacupuncture can improve cognitive function in cancer patients by enhancing neurophysiological pathways and immune functions. As there are no electroacupuncture studies performed before with CRCI, we conducted a feasibility study to investigate the number of participants, outcome measures, and intervention period for further confirmatory studies.
In this study, a total of 12 participants were included, and 10 completed the trial. Both subjective and objective outcomes of cognitive function, QoL, and psychological factors were measured for all participants at baseline, week 4, 8, and 12. Based on our study results at baseline, we found that our study participants included in this trial had a moderate to severe degree of perceived cognitive impairments on subjective outcomes and borderline cognitive functions on neuropsychological tests. Consistent with the results of previous studies, our study results also confirmed that subjective complaints are more severe than objective cognitive tests in CRCI patients. 52 The scores of the PCI subscale were found to be much lower than the inclusion criteria of 63 and the cut-off value of 60, indicating that the cognitive complaints they suffer are above a moderate degree. 24 On evaluation of the objective test, the average MoCA-K score was slightly below the cut-off value for cognitive impairments, and the MMSE-K score was within the normal range. These results explain that our CRCI patients had borderline or normal cognitive function when measured by neuropsychological tests.
Additionally, participants showed a decline, especially in memory function, among the various cognitive domains. Loss of memory often makes it difficult to track dates or events, resulting in patients asking repeated questions, and relying on reminder notes or electrical devices as memory aids, thereby limiting their daily activities. Moreover, memory deficit is a key component in the characterization of MCI and is a strong predictor of the progression of Alzheimer’s disease. 53 In previous studies with CRCI patients, some reported that memory loss is the most commonly observed cognitive domain, while others have reported nonspecific patterns of impairment. 3 In this context, the presence of a decline in memory in our study demonstrates results similar to those of some studies with CRCI and studies with MCI. Thus, it is important to follow up on their cognitive impairments to predict disease progression. In terms of QoL and psychological problems of our study participants, subjects were shown to have a relatively good QoL and had no particular psychological symptoms. Only the QoL related to cognitive function was at a low level compared with other CRCI patients, and fortunately none of our participants had problems with anxiety or depression.
After 8 weeks of electroacupuncture treatment, we found significant improvements in both subjective and objective outcomes of cognitive function compared to baseline. Diverse cognitive outcomes, including FACT-Cog (PCI), EORTC-QLQ-C30 (QoL), MoCA-K, BNT, SVLT, and RCFT, were revealed to have significant changes compared to the baseline either on week 8 or 12. The FACT-Cog and EORTC-QLQ-C30 are self-report questionnaires which represent subjective impairments of cognitive domain and QoL,29,35 while MoCA-K, BNT, SVLR, and RCFT are objective neuropsychological tests for evaluating attention, memory, executive, and visuospatial functions. 30
The primary outcome measure, FACT-Cog, is the most widely used validated patient-report outcome (PRO) to assess cognitive complaints in cancer patients. 54 By using patients’ self-report outcomes, we can detect subtle declines in cognitive function better than neuropsychological testing. 55 In our study, electroacupuncture showed significant improvements on the FACT-Cog-PCI subscale, and no significant change was found in the total score of the FACT-Cog. However, the change in total FACT-Cog score between baseline and weeks 4, 8, and 12 exceeded the MCID, demonstrating its clinical effectiveness in cognitive complaints for cancer patients. Additionally, it is worthwhile to find significant differences in the PCI subscale in that PCI is reported to be the most recommended and preferred outcome among the 4 subscales of FACT-Cog. 24 Many researchers recently identified that PCI relates more to other clinical features such as depression and anxiety than PCA or other subscales 56 and PCI is also being used to identify and diagnose CRCI by developing and validating cut-off points of FACT-Cog-PCI. 24
In the QoL outcome measure of EORTC-QLQ-C30, electroacupuncture showed significant changes in the QoL scale and, unfortunately, not in functional and symptom scales. In the subscale analysis, significant improvements were found in the appetite loss scale after 12 weeks. In other subscales, we found minimal important differences on physical, role, cognitive, and social functions, and on symptoms of dyspnea and constipation. 57 Although significant differences were not observed in the total score of functional and symptom scales, most of the subscales on the functional scale were revealed to have more improvements than MCID in cognitive difficulties after treatment with electroacupuncture. In other words, the overall QoL and symptoms attributed to cancer were well-maintained during the trial, as participants showed good QoL from the baseline. Thus, we can conclude that electroacupuncture can have potential effects in improving the QoL and functional well-being of cancer patients with cognitive impairment.
Among the objective neuropsychological tests measured in our study, MoCA-K, BNT, SVLT, and RCFT showed statistically significant improvement after electroacupuncture treatment. Significant differences in the total score of MoCA-K compared with the baseline could be observed immediately from week 4, and it gradually improved over time, scoring the highest point of 28.90 on week 12. Among the domains in the MoCA-K, electroacupuncture showed the greatest improvement in the delayed recall section, followed by the visuospatial/executive and abstraction domains, indicating that electroacupuncture has the greatest effectiveness in enhancing memory among diverse cognitive functions. SVLT and RCFT are neuropsychological tests for verbal and visuospatial memory, respectively, both of which consist of immediate recall test, delayed recall test after 20 minutes, and recognition test. Electroacupuncture had significantly improved in all 3 of these tests on both SVLT and RCFT, indicating its effectiveness in overall encoding, storage, and retrieval processes of memory performance. 58 However, in the RCFT-copy test which was performed to assess visuospatial function, the copy-score and time did not show significant differences after 8 and 12 weeks. Based on these results, we can also expect that electroacupuncture may be more effective in memory progression than visuospatial function. Lastly, the BNT test for language and related functions showed significant increases after 8 and 12 weeks. Similar results could also be found in the language domain on MoCA-K, as the score of the language domain increased from 2.83 at baseline to 3.0 at week 8 and 12, although the difference was not statistically significant. These results support the evidence that electroacupuncture may be helpful for language-related cognitive functions. Taken together with our neuropsychological test results, we can conclude that electroacupuncture is effective primarily in improving the memory domain and language-related functions.
Overall, in this study, we found the effectiveness of electroacupuncture for CRCI in subjective cognitive measurements and objective neuropsychological tests was mostly due to enhancing the progression of memory. Cancer survivors report both objective and subjective cognitive impairments that range from mild to moderate depending on the type of cancer, stage, and treatment. However, neuropsychological tests that provide objective assessments do not always correlate highly with subjective cognitive complaints, as psychological factors such as anxiety, depression, fatigue, or insomnia affect their discomforts. 1 In our study, we found significant improvements in objective neuropsychological tests as well as subjective outcomes, although we cannot determine whether all of the subjective and objective outcomes evaluated in this study correlate with each other. These results may be due to the baseline characteristic that our study participants did not suffer from psychological problems such as anxiety and depression. Despite the many difficulties in finding effectiveness in objective outcomes for CRCI patients, it is worthwhile to have revealed significant improvements in neuropsychological tests on MoCA-K, BNT, SVLT, and RCFT, as well as subjective complaints. We expect our study results to be valuable in planning future large-scale clinical trials.
As this study is a preliminary trial for confirmatory study, the major goal of this study was to investigate the feasibility of trial design, outcome measures, and calculation of sample size for further confirmatory clinical trials. To determine the feasibility of clinical trials for electroacupuncture, we measured recruitment, completion, and adherence rates, and all 3 outcomes resulted in more than 80% success. Based on these results, we can presume that the overall study design, including inclusion/exclusion criteria, intervention period, visit window, and follow-up period were appropriate for the CRCI participants, and we believe that this trial design can be applied to our next clinical trial.
Despite these successful feasibility results, there are some limitations that we have to complement and revise for our next electroacupuncture clinical trial. First, we have to consider that the study was prematurely terminated as it was difficult to enroll eligible participants, and finally recruited 12 subjects in approximately 9 months. Taking this into account, it is necessary to set a sufficient recruitment period and appropriate number of subjects for the next trial. Second, the cancer type, treatment, and stages of our study participants varied, although most were breast cancer patients. For more delicate and standardized clinical trials to detect effect size and mechanism, it will be better to include specific types of cancer patients, with typical stages or those treated with specific chemotherapy. Third, the outcome measure should be supplemented to detect our intervention and disease conditions best and to gather more information about biomarkers or brain images. Although FACT-Cog is the most commonly used PRO in CRCI, the subscale PCI in FACT-Cog can also be considered as a secondary outcome, as it represents the cognitive complaints well and even better than the total score of FACT-Cog. It is also important to use a suitable battery of neuropsychological tests and self-reporting tools in balance. As we evaluated the SNSB, 3 measures should be included as essential as the ICCTF recommends to least include the following in assessing cognitive function in cancer patients: the Hopkins Verbal Learning Test-Revised, Trail Making Test, and the Controlled Oral Word Association. However, as the SNSB takes over an hour to complete the evaluation, we can also use a short version of SNSB for participants’ convenience and compliance. In addition, biomarkers and brain images can also be used as secondary outcome measures. Biomarkers representing inflammatory status, neurobiological status, and genetic polymorphisms have been investigated recently, although the results are still conflicting. 59 The most reliable biological factors related to CRCI were TNF-α, IL-1β, IL-2, IL-10, IL-6, and IL-860,61 and neurological markers detected during cancer treatments include N-acetylaspartate (NAA)/choline (Cho) and NAA/myo-inositol (myo-I) ratios. 62 Genetic factors such as APOE-4 (rs429358, rs7412), 63 IL-1R1 (rs2287047, rs949963), 64 COMT (rs4680, rs165599), 65 and BDNF (rs6265) 66 have been explored in many studies. These biomarkers will help to understand the mechanisms of electroacupuncture on CRCI, whether it relates with the protection of cerebral neurons or regulation of metabolism or BDNF. Moreover, brain images are usually used to determine changes in brain volume, activity, and metabolism in CRCI patients. 67 Recent studies have reported that chemotherapy reduced the volume or density of gray matter and white matter microstructure, and altered brain activation. 68 In our next study, we will consider the use of these biomarkers and neuroimaging measures as an additional outcome to better understand the possible mechanisms of CRCI. Lastly, our study has limitations as it is a single group, before-after study with a small sample size. We did not compare the intervention and comparison groups, such as the usual care group or the sham group. As our study is a small study, there are limitations in interpreting the effects of electroacupuncture in CRCI and our study results only provide clinical data before and after electroacupuncture treatment. Thus, it is more vulnerable to bias than randomized controlled trials, and the results of this study should be used in consideration of these biases.
Nonetheless, our study revealed the safety and effectiveness of electroacupuncture on CRCIs and confirmed the feasibility of the trial design. This trial has valuable findings in designing our next large-scale prospective clinical trial to confirm the efficacy of electroacupuncture in CRCI. Various clinical outcomes of patient-report complaints, neuropsychological tests, QoL, and psychological problems obtained from our study will be used as the basis for designing our next trial. More importantly, we found the value of electroacupuncture in CRCI patients for both subjective and objective measures with a good level of patient satisfaction. Thus, with the application of electroacupuncture in cognitive deficits, a well-designed protocol is needed to confirm its effectiveness.
Conclusion
Our study demonstrated the feasibility of an electroacupuncture clinical trial with successful recruitment, completion, and adherence rates. After 8 weeks of treatment, electroacupuncture significantly improved the subjective cognitive outcomes of the FACT-Cog (PCI scale), EORTC-QLQ-C30 (QoL scale), and objective neuropsychological tests of MoCA-K, BNT, SVLT, and RCFT. These feasibility trial results will be used as preliminary data for future randomized controlled clinical trials to evaluate the safety and efficacy of electroacupuncture for CRCI.
Supplemental Material
Supplemental material, sj-docx-1-ict-10.1177_15347354221098983 for Electroacupuncture for Cancer-Related Cognitive Impairment: A Clinical Feasibility Study by Yee Ran Lyu, Hye-Yoon Lee, Hyo-Ju Park, O-jin Kwon, Ae-Ran Kim, In Chul Jung, Yang-Chun Park, Jung-Hyo Cho, Jung-Eun Kim, Mikyung Kim, Jun-Hwan Lee and Joo-Hee Kim in Integrative Cancer Therapies
Footnotes
Author Contributions: YR: writing of the original draft; HL, JK, MK, JL, and JK: study design; HP and AK: investigation and data collection; OK: statistical analysis; IJ, YP, and JC: investigation; HL and JK: review and supervision. All authors read and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by grants from the Korea Institute of Oriental Medicine (grant numbers: K16122 and KSN2021210).
ORCID iD: Joo-Hee Kim  https://orcid.org/0000-0003-1435-5649
https://orcid.org/0000-0003-1435-5649
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Biegler KA, Alejandro Chaoul M, Cohen L. Cancer, cognitive impairment, and meditation. Acta Oncol. 2009;48:18-26. [DOI] [PubMed] [Google Scholar]
- 2. Ahles TA, Root JC. Cognitive effects of cancer and cancer treatments. Annu Rev Clin Psychol. 2018;14:425-451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wefel JS, Kesler SR, Noll KR, Schagen SB. Clinical characteristics, pathophysiology, and management of noncentral nervous system cancer-related cognitive impairment in adults. CA Cancer J Clin. 2015;65:123-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Koppelmans V, Breteler MMB, Boogerd W, Seynaeve C, Gundy C, Schagen SB. Neuropsychological performance in survivors of breast cancer more than 20 years after adjuvant chemotherapy. J Clin Oncol. 2012;30:1080-1086. [DOI] [PubMed] [Google Scholar]
- 5. Denlinger CS, Ligibel JA, Are M, et al.; National Comprehensive Cancer Network. Survivorship: cognitive function, version 1.2014. J Natl Compr Canc Netw. 2014;12:976-986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chan RJ, McCarthy AL, Devenish J, Sullivan KA, Chan A. Systematic review of pharmacologic and non-pharmacologic interventions to manage cognitive alterations after chemotherapy for breast cancer. Eur J Cancer. 2015;51:437-450. [DOI] [PubMed] [Google Scholar]
- 7. Lv L, Mao S, Dong H, Hu P, Dong R. Pathogenesis, assessments, and management of chemotherapy-related cognitive impairment (CRCI): an updated literature review. J Oncol. 2020;2020:1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Avisar A, River Y, Schiff E, Bar-Sela G, Steiner M, Ben-Arye E. Chemotherapy-related cognitive impairment: does integrating complementary medicine have something to add? Review of the literature. Breast Cancer Res Treat. 2012;136:1-7. [DOI] [PubMed] [Google Scholar]
- 9. Witt CM, Pach D, Brinkhaus B, et al. Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Complement Med Res. 2009;16:91-97. [DOI] [PubMed] [Google Scholar]
- 10. Vincent C. The safety of acupuncture: Acupuncture is safe in the hands of competent practitioners. BMJ. 2001;323:467-468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Garcia MK, McQuade J, Haddad R, et al. Systematic review of acupuncture in cancer care: a synthesis of the evidence. J Clin Oncol. 2013;31:952-960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jia Y, Zhang X, Yu J, et al. Acupuncture for patients with mild to moderate Alzheimer’s disease: a randomized controlled trial. BMC Complement Altern Med. 2017;17:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tong T, Pei C, Chen J, Lv Q, Zhang F, Cheng Z. Efficacy of acupuncture therapy for chemotherapy-related cognitive impairment in breast cancer patients. Med Sci Monit. 2018;24:2919-2927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zeng Y, Cheng ASK, Song T, et al. Effects of acupuncture on cancer-related cognitive impairment in Chinese gynecological cancer patients: a pilot cohort study. Integr Cancer Ther. 2018;17:737-746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liou KT, Garland SN, Li QS, et al. Effects of acupuncture versus cognitive behavioral therapy on brain-derived neurotrophic factor in cancer survivors with insomnia: an exploratory analysis. Acupunct Med. 2021;39:637-645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lee H-Y, Kim J-E, Kim M, Kim J-H. A review of traditional Korean medical treatment for cancer-related cognitive impairment. J Korean Med. 2016;37:74-86. [Google Scholar]
- 17. Lee HG, Jung DJ, Choi YM, et al. A systematic literature review on clinical research in human utilized electroacupuncture in Korea. Acupuncture. 2013;30:139-153. [Google Scholar]
- 18. Zhang H, Zhao L, Yang S, et al. Clinical observation on effect of scalp electroacupuncture for mild cognitive impairment. J Tradit Chin Med. 2013;33:46-50. [DOI] [PubMed] [Google Scholar]
- 19. Kim MW, Yoo JH, Go HJ, et al. Systematic review of acupuncture treatment for mild cognitive impairment. J Acupunct Res. 2019;36:72-79. [Google Scholar]
- 20. Zhao L, Zhang H, Zheng Z, Huang J. Electroacupuncture on the head points for improving gnosia in patients with vascular dementia. J Tradit Chin Med. 2009;29:29-34. [DOI] [PubMed] [Google Scholar]
- 21. Xia Y, Wang H-D, Ding Y, Kang B, Liu W-G. Parkinson’s disease combined with depression treated with electroacupuncture and medication and its effect on serum BDNF. Zhongguo Zhen Jiu. 2012;32:1071-1074. [PubMed] [Google Scholar]
- 22. Ulett GA, Han S, Han JS. Electroacupuncture: mechanisms and clinical application. Biol Psychiatry. 1998;44:129-138. [DOI] [PubMed] [Google Scholar]
- 23. MacPherson H, Altman DG, Hammerschlag R, et al. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. J Altern Complement Med. 2010;16:ST-1-ST-14. [DOI] [PubMed] [Google Scholar]
- 24. Dyk KV, Crespi CM, Petersen L, Ganz PA. Identifying cancer-related cognitive impairment using the FACT-Cog perceived cognitive impairment. JNCI Cancer Spectr. 2020;4:z099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zhang J, Shen Y. [Magnetic resonance spectroscopic study of memory impairment after cerebral infarction treated with electroacupuncture]. Zhongguo Zhen Jiu. 2015;35:657-660. [PubMed] [Google Scholar]
- 26. Bussell J. The effect of acupuncture on working memory and anxiety. J Acupunct Meridian Stud. 2013;6:241-246. [DOI] [PubMed] [Google Scholar]
- 27. Huang J, McCaskey MA, Yang S, et al. Effects of acupuncture and computer-assisted cognitive training for post-stroke attention deficits: study protocol for a randomized controlled trial. Trials. 2015;16:546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chou P, Chu H, Lin J-G. Effects of electroacupuncture treatment on impaired cognition and quality of life in Taiwanese stroke patients. J Altern Complement Med. 2009;15:1067-1073. [PubMed] [Google Scholar]
- 29. Park J-H, Bae SH, Jung YS, Jung Y-M. The psychometric properties of the Korean version of the functional assessment of cancer therapy-cognitive (FACT-Cog) in Korean patients with breast cancer. Support Care Cancer. 2015;23:2695-2703. [DOI] [PubMed] [Google Scholar]
- 30. Julayanont P, Nasreddine ZS. Montreal Cognitive Assessment (MoCA): concept and clinical review. In: AJ Larner, ed. Cognitive Screening Instruments. A Practical Approach. 2nd ed. Springer; 2017:139-195. [Google Scholar]
- 31. Chertkow H, Nasreddine Z, Joanette Y, et al. Mild cognitive impairment and cognitive impairment, no dementia: part A, concept and diagnosis. Alzheimer Dement. 2007;3:266-282. [DOI] [PubMed] [Google Scholar]
- 32. Kang Y, Na D. Seoul Neuropsychological Screening Battery. Human Brain Research & Consulting Co.; 2003. [Google Scholar]
- 33. Lee AY, Lee J, Oh E, Yoon SJ, Yoon B, Yu SD. Clinical utility of Seoul neuropsychological screening battery-core for dementia management project in the community. J Korean Neurol Assoc. 2019;37:277-283. [Google Scholar]
- 34. Wefel JS, Vardy J, Ahles T, Schagen SB. International Cognition and Cancer Task Force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncol. 2011;12:703-708. [DOI] [PubMed] [Google Scholar]
- 35. Yun YH, Park YS, Lee ES, et al. Validation of the Korean version of the EORTC QLQ-C30. Qual Life Res. 2004;13:863-868. [DOI] [PubMed] [Google Scholar]
- 36. Oh SM, Min KJ, Park DB. A study on the standardization of the hospital anxiety and depression scale for Koreans: a comparison of normal, depressed and anxious groups. J Korean Neuropsychiatr Assoc. 1999;38:289-296. [Google Scholar]
- 37. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-370. [DOI] [PubMed] [Google Scholar]
- 38. Ganz PA, Kwan L, Castellon SA, et al. Cognitive complaints after breast cancer treatments: examining the relationship with neuropsychological test performance. J Natl Cancer Inst. 2013;105:791-801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. King S, Green HJ. Psychological intervention for improving cognitive function in cancer survivors: a literature review and randomized controlled trial. Front Oncol. 2015;5:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Schuurs A, Green HJ. A feasibility study of group cognitive rehabilitation for cancer survivors: enhancing cognitive function and quality of life. Psychooncology. 2013;22:1043-1049. [DOI] [PubMed] [Google Scholar]
- 41. Milbury K, Chaoul A, Biegler K, et al. Tibetan sound meditation for cognitive dysfunction: results of a randomized controlled pilot trial. Psychooncology. 2013;22:2354-2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649-655. [PubMed] [Google Scholar]
- 43. Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997;15:300-308. [Google Scholar]
- 44. Kobayashi LC, Cohen HJ, Zhai W, et al. Cognitive function prior to systemic therapy and subsequent well-being in older breast cancer survivors: longitudinal findings from the Thinking and Living with Cancer Study. Psychooncology. 2020;29:1051-1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lawrence JA, Griffin L, Balcueva EP, et al. A study of donepezil in female breast cancer survivors with self-reported cognitive dysfunction 1 to 5 years following adjuvant chemotherapy. J Cancer Surviv. 2016;10:176-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cheung YT, Foo YL, Shwe M, et al. Minimal clinically important difference (MCID) for the functional assessment of cancer therapy: cognitive function (FACT-Cog) in breast cancer patients. J Clin Epidemiol. 2014;67:811-820. [DOI] [PubMed] [Google Scholar]
- 47. Nasreddine ZS, Phillips NA, Bã©dirian V, et al. The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695-699. [DOI] [PubMed] [Google Scholar]
- 48. Janelsins MC, Kesler SR, Ahles TA, Morrow GR. Prevalence, mechanisms, and management of cancer-related cognitive impairment. Int Rev Psychiatry. 2014;26:102-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Chung N-C, Walker AK, Dhillon HM, Vardy JL. Mechanisms and treatment for cancer- and chemotherapy-related cognitive impairment in survivors of non-CNS malignancies. Oncology. 2018;32:591-598. [PubMed] [Google Scholar]
- 50. Cabýoglu MT, Ergene N, Tan U. The mechanism of acupuncture and clinical applications. Int J Neurosci. 2006;116:115-125. [DOI] [PubMed] [Google Scholar]
- 51. Zeng B-Y, Salvage S, Jenner P. Effect and mechanism of acupuncture on Alzheimer’s disease. Int Rev Neurobiol. 2013;111:181-195. [DOI] [PubMed] [Google Scholar]
- 52. Horowitz TS, Suls J, Treviño M. A call for a neuroscience approach to cancer-related cognitive impairment. Trends Neurosci. 2018;41:493-496. [DOI] [PubMed] [Google Scholar]
- 53. Belleville S, Sylvain-Roy S, de Boysson C, Ménard M-C. Characterizing the memory changes in persons with mild cognitive impairment. Prog Brain Res. 2008;169:365-375. [DOI] [PubMed] [Google Scholar]
- 54. Wagner LI, Sweet J, Butt Z, Lai J-S, Cella D. Measuring patient self-reported cognitive function: development of the functional assessment of cancer therapy-cognitive function instrument. J Support Oncol. 2009;7:W32-W39. [Google Scholar]
- 55. Jean-Pierre P. Management of cancer-related cognitive dysfunction-conceptualization challenges and implications for clinical research and practice. US Oncol. 2010;6:9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lai JS, Wagner LI, Jacobsen PB, Cella D. Self-reported cognitive concerns and abilities: two sides of one coin? Psychooncology. 2014;23:1133-1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Musoro JZ, Coens C, Fiteni F, et al. Minimally important differences for interpreting EORTC QLQ-C30 scores in patients with advanced breast cancer. JNCI Cancer Spectr. 2019;3:z037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. McDermott KB, Roediger HL. ESRMemory (encoding, storage, retrieval). General Psychology FA2018 Noba Project. 2018:117-153. [Google Scholar]
- 59. Ahles TA, Li Y, McDonald BC, et al. Longitudinal assessment of cognitive changes associated with adjuvant treatment for breast cancer: the impact of APOE and smoking. Psychooncology. 2014;23:1382-1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Pomykala KL, Ganz PA, Bower JE, et al. The association between pro-inflammatory cytokines, regional cerebral metabolism, and cognitive complaints following adjuvant chemotherapy for breast cancer. Brain Imaging Behav. 2013;7:511-523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lyon DE, Cohen R, Chen H, et al. Relationship of systemic cytokine concentrations to cognitive function over two years in women with early stage breast cancer. J Neuroimmunol. 2016;301:74-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kesler SR, Watson C, Koovakkattu D, et al. Elevated prefrontal myo-inositol and choline following breast cancer chemotherapy. Brain Imaging Behav. 2013;7:501-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Koleck TA, Bender CM, Sereika SM, et al. GCFPWWESBC Apolipoprotein E genotype and cognitive function in postmenopausal women with early-stage breast cancer. Oncol Nurs Forum. 2014:41:E313-E325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Merriman JD, Aouizerat BE, Cataldo JK, et al. Association between an interleukin 1 receptor, type I promoter polymorphism and self-reported attentional function in women with breast cancer. Cytokine. 2014;65:192-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Cheng H, Li W, Gan C, Zhang B, Jia Q, Wang K. The COMT (rs165599) gene polymorphism contributes to chemotherapy-induced cognitive impairment in breast cancer patients. Am J Transl Res. 2016;8:5087-5097. [PMC free article] [PubMed] [Google Scholar]
- 66. Ng T, Teo SM, Yeo HL, et al. Brain-derived neurotrophic factor genetic polymorphism (rs6265) is protective against chemotherapy-associated cognitive impairment in patients with early-stage breast cancer. Neuro Oncol. 2016;18:244-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Janelsins MC, Kohli S, Mohile SG, Usuki K, Ahles TA, Morrow GR. An update on cancer- and chemotherapy-related cognitive dysfunction: current status. Semin Oncol. 2011;38:431-438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Deprez S, Kesler SR, Saykin AJ, Silverman DHS, de Ruiter MB, McDonald BC. International cognition and cancer task force recommendations for neuroimaging methods in the study of cognitive impairment in non-CNS cancer patients. J Natl Cancer Inst. 2018;110:223-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-ict-10.1177_15347354221098983 for Electroacupuncture for Cancer-Related Cognitive Impairment: A Clinical Feasibility Study by Yee Ran Lyu, Hye-Yoon Lee, Hyo-Ju Park, O-jin Kwon, Ae-Ran Kim, In Chul Jung, Yang-Chun Park, Jung-Hyo Cho, Jung-Eun Kim, Mikyung Kim, Jun-Hwan Lee and Joo-Hee Kim in Integrative Cancer Therapies