Abstract
An anterior superior iliac spine avulsion (ASIS) is an injury that is induced by a rapid contraction of the sartorius and tensor fascia lata (TFL) muscles in the thigh. In this technique article, the ASIS is repaired by restoring normal length and tension to the sartorius muscle-tendon unit, which optimizes anatomic healing and function of the hip. We recommend a hybrid fixation strategy. This involved both a tape bridge construct and cannulated compression lag screw fixation. Countersinking the screw below the surface of the ASIS avoids hardware prominence and ensures an impingement-free range of motion. The tape-bridge construct reinforces the lag screw fixation, or can be used as the primary fixation method in the event the fragment is too small to accept a screw. This hybrid technique (tape bridge construct and cannulated screw fixation) is a safe and dependable method of surgically repairing the ASIS, allowing for early mobilization and weight bearing.
Technique Video
This video highlights the specific procedural steps performed for this particular anterior superior iliac spine avulsion (ASIS) fracture repair. The patient’s rehabilitation footage can be found at the conclusion of the video, showing the various fitness protocols in motion.
Introduction
An anterior superior iliac spine avulsion (ASIS) is an injury that is induced by a rapid contraction of the sartorius and tensor fascia lata muscles in the thigh. This type of injury is uncommon; only approximately 1.4 percent of hip and pelvic injuries are ASIS avulsions.1, 2, 3, 4, 5, 6 The majority of these injuries are commonly found in adolescents, mainly athletes. Moreover, soccer players and gymnasts have the highest probability of sustaining an avulsion fracture.1,7 Given the rarity of this injury, there is a high risk for misdiagnosis, as this particular avulsion fracture is oftentimes classified as a mere muscle strain or tendinous injury.8 Many case reports demonstrate various treatment options, ranging from crutch use to bed rest. Conservative treatment consists of a period of relative rest, usually lasting about 3 days, along with protected-weight-bearing with crutch use until the patient does not experience any pain, followed by formal physical therapy.9 Generally, nonoperative treatment can be used for minimally displaced fragments. Various studies state that conservative treatment remains to be the most viable and selected option of treatment.10, 11, 12, 13
Although conservative treatment is the first choice for treatment, depending on the severity of the avulsion fracture, the size of the fragment displacement, or the functional demands of the patient, surgical intervention may be necessary.8 High-level athletes who have sustained this injury may opt for the ASIS surgical repair because of the agility and hip flexor strength necessary for fast-paced sports. Additionally, repetitive hip flexion is common in these sports due to the sudden, swift turns that occur throughout the duration of open play. Thus, surgery may be recommended for high-level athletes with this injury who are planning on competing at the collegiate or professional level. Therefore, it may be warranted to consult with an orthopedic surgeon to consider nonoperative versus operative repair of the ASIS avulsion fracture to avoid any future complications and loss of function. Generally, the surgical techniques for an ASIS avulsion fracture typically involve open reduction and internal fixation. Here, we describe a hybrid technique involving open reduction combined with a tape-bridge fixation construct.
Patient Evaluation
Anterior hip pain and signs of weak hip flexion can be indicative of an ASIS avulsion fracture, especially in the setting of a painful pop during an inciting incident. These symptoms are induced by the rapid, forceful contraction of the sartorius and tensor fascia lata, which commonly occurs during sport activities, such as relay sprints, soccer matches, and gymnastic events. When such symptoms are present, several physical examinations must be conducted to confirm the presence of this type of avulsion fracture. Therefore, inspecting the painful site of the anterior hip and pelvis will determine whether there is any tenderness, edema, or palpable defects near the ASIS. Next, the gait should be observed for any signs of abnormal gait and pelvic tilt. Additionally, hip flexor, hip extensor, abductor, and adductor strength should all be determined. Range of motion of the hip and lumbar spine should also be evaluated. On the basis of the results of these tests, the likelihood of an ASIS avulsion fracture is increased if there is a palpable defect, combined with pain and weakness during resisted hip flexion and resisted straight leg raising. A supine exam and side-lying exam should also be done to further assess any concomitant injury in the hip and pelvic area, including the abductors, glute complex, and proximal hamstring. After conducting these exams, radiographs can be recorded, (X-rays, MRI, CT scan, etc.), which can validate the presence of a suspected ASIS avulsion injury. Depending on the magnitude of the injury, the radiographs can reveal the position and size of the displaced fragment, (if present).
Imaging and Indications
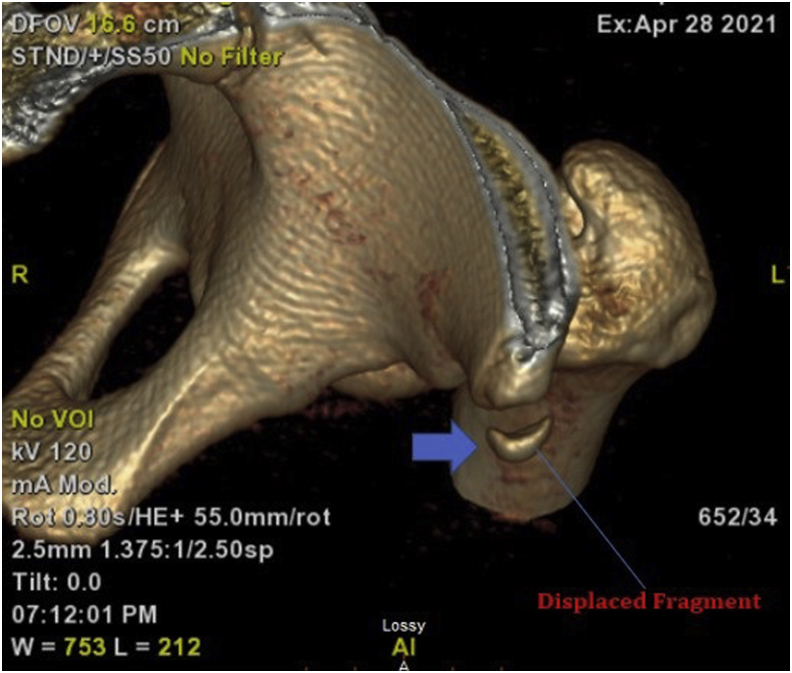
The ASIS repair indications and contraindications are shown in Table 1. Two views of pelvic radiographs (AP Pelvis and False Profile) are often necessary to confirm the presence and displacement of the ASIS fragment. Moreover, a CT scan with three-dimensional reconstructions can also identify missed fracture on plain radiographs, as well as confirm the size and displacement of the fragment. In this instance, the fragment size was displaced by 2 cm inferiorly and .8 cm anteriorly. Because of the magnitude of the displacement, activity profile, and athletic aspirations, surgery was recommended in order to restore normal length and tension to the sartorius muscle, as well as to optimize anatomic healing and function of the hip. The involved rehabilitation was thoroughly explained, as well as the need to protect the repair in the first 4-6 weeks, including limited weight-bearing, the use of a brace while avoiding active hip flexion, or passive hip extension past neutral. The general timelines for return to sport activities were discussed, which would take approximately 3-4 months.
Table 1.
Indications and Contraindications
Indications
|
Surgical Technique
Step 1: Positioning
General anesthesia is administered, and a flattop Jackson table is prepared for supine positioning. The left hip and entire lower extremity are then prepared and draped free in the usual sterile fashion. Next, preoperative intravenous antibiotics are administered.
Step 2: Skin Incision
We mark out the area of the anterior iliac crest and the ASIS. A 4-cm incision is then created longitudinally centered over the ASIS in the area of the palpable defect. Strict hemostasis is maintained, as we dissect down to the fascia of the sartorius and the TFL. Any medial traversing branches of the lateral femoral cutaneous nerve (LFCN) are protected for the balance of the operation. The fascia is split longitudinally along the length of the incision. We then dissect sharply down onto the palpable bony fragment. This dissection is continued subperiosteally proximally, medially, and laterally around the fragment, while ensuring not to transect any of its tendinous attachment of the TFL or the sartorius. If the fragment is not visible or mobile at first sight, measuring 2-3 cm from the ASIS, using radiographic imaging, and palpating known bony landmarks at the ASIS/anterior inferior iliac spine (AIIS) can all be performed to uncover the fragment’s location and enhance its visibility. The bony bed of the fragment is then identified proximally in the dissection. Displacement can be evaluated as shown in Fig 1, Fig 2, Fig 3. The recipient site is then debrided of any intervening fibrous tissue and rasped adequately to give a bony bleeding surface. The fragment is then mobilized circumferentially to give it further excursion. The knee and hip are then flexed in order to allow the fragment and its sartorial attachment to be reduced to its footprint.
Fig 1.
Preoperative three-dimensional computed tomography scan, confirming the size, displacement, and orientation of the anterior superior iliac spine avulsion (blue arrow denotes displaced fragment).
Fig 2.
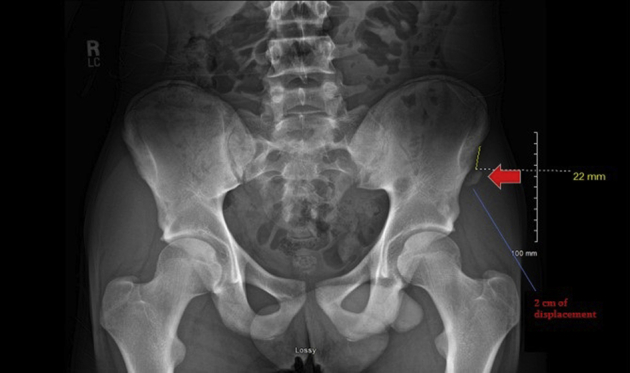
Radiograph of the pelvis. A preoperative radiograph scan of the entire hip shows an avulsion fracture in the left ASIS. (red arrow denotes fragment showing 2 cm of displacement).
Fig 3.
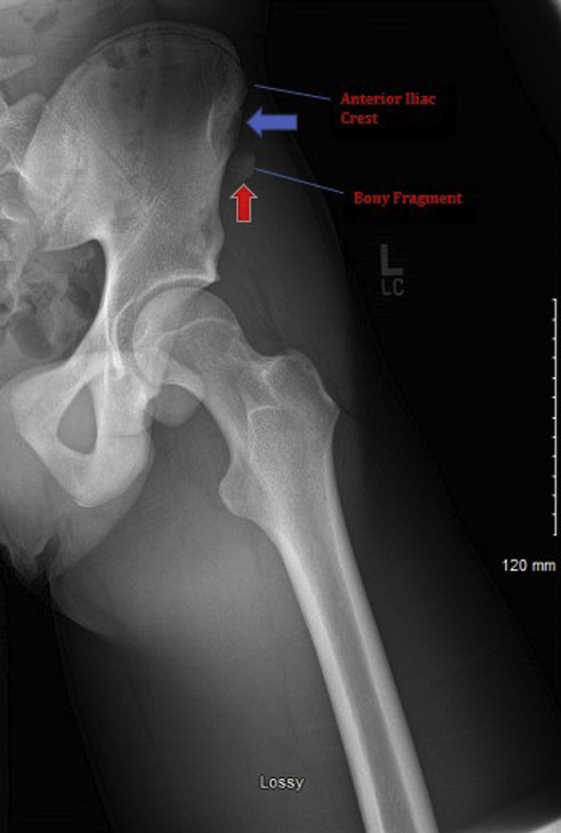
Magnified preoperative radiograph scan of the left pelvis. This scan further reveals the displacement of the bony fragment that lies on the anterior iliac crest (blue arrow denotes anterior iliac crest, and red arrow denotes bony fragment).
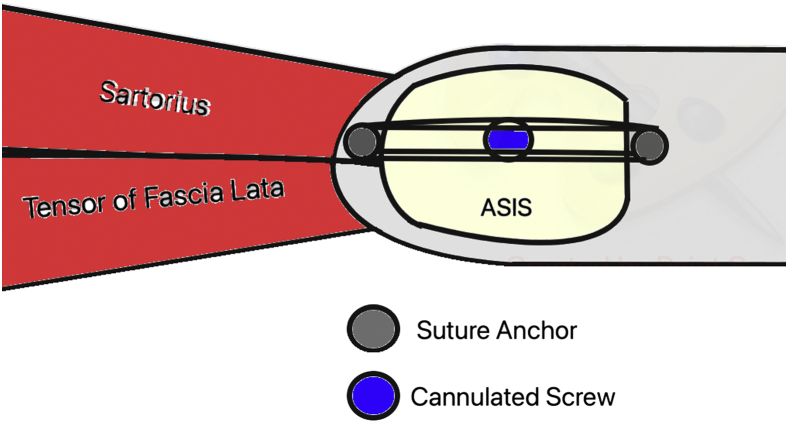
We recommend a hybrid fixation strategy. This involves both a tape bridge construct and cannulated compression screw fixation (Figs 4 and 5).
Fig 4.
The orientation of the anchor-suture configuration of the anterior superior iliac spine avulsion (ASIS) repair is shown in this schematic diagram. The anchor-suture configuration appears to be implanted in a linear fashion between the sartorius and the ASIS during the fixation technique. The sartorius muscle, tensor of the fascia lata, ASIS, along with the suture anchors, (Stryker, Kalamazoo, MI), and cannulated screw are shown. The surgical operation is completed correspondingly to this particular diagram.
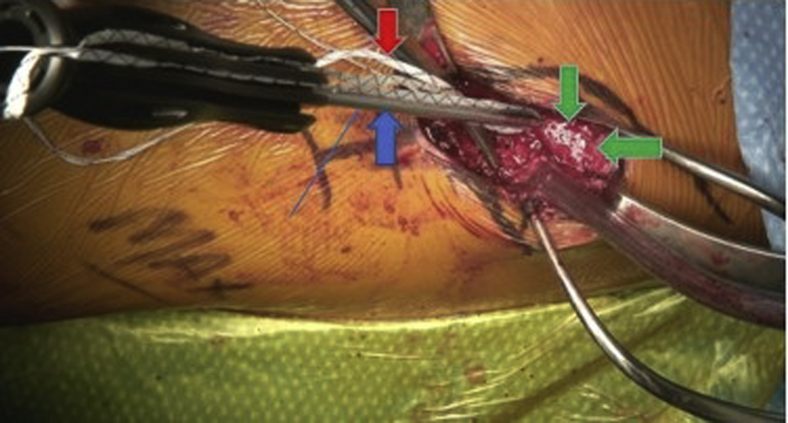
Fig 5.
Patient was placed in a supine position, while a 3.9-mm Omega knotless anchor double-loaded with tape was deployed into the left hemipelvis just beneath the recipient site of the anterior superior iliac spine avulsion bone (blue arrow denotes 3.99-mm Omega knotless anchor, red arrow denotes suture tape, and green arrows recipient site).
We first advance a 3.9-mm omega knotless anchor (Stryker, Kalamazoo, MI) double-loaded with 2.0-mm tape. This anchor is drilled for and advanced just inferior to the recipient site of the ASIS bone.
Using a free needle, the 4 limbs are then passed through at the bone tendon junction of the sartorius and the ASIS and saved for later use.
Step 3: Cannulated Compression Screw Fixation
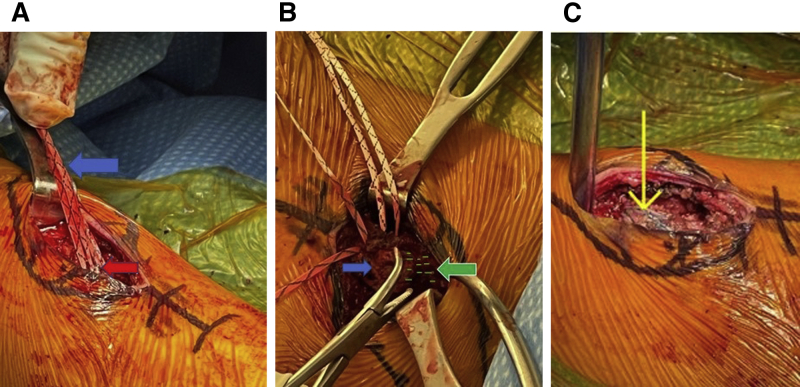
Using reduction forceps, the surgeon pulls the fragment to its bony bed, and anatomic reduction is held with two 1.2-mm K wires provisionally. The reduction is confirmed by a live radiograph, with multiple views of the pelvis and iliac crest. We first drill for and then advance a 3.0-mm cannulated partially threaded screw to achieve compression across the fracture. This is countersunk to avoid future prominence (Fig 6, A-C). Compression and position are once again confirmed on radiograph (Fig 7).
Fig 6.
Intraoperative photographs showing suture tapes crossing over. (A) Suture tapes are secured on a 3.9-mm Omega knotless anchor to allow tapes to cross over (blue arrow denotes suture tape, and red arrow denotes Omega knotless anchor embedded into bony fragment). (B) Aerial view of suture tapes crossing over to complete suture tape-bridge construct near bone tendon junction area, facilitating repair of the anterior superior iliac spine avulsion (ASIS) (blue arrow denotes bony fragment, while green arrow/green markings denote left ASIS). (C) Completed suture-tape fixation of left ASIS, which was completed as per the aforementioned schematic diagram. This allowed for maximum repair, further reinforcing strength and flexion in the pelvis (yellow arrow denotes completed suture tape bridge fixation).
Fig 7.
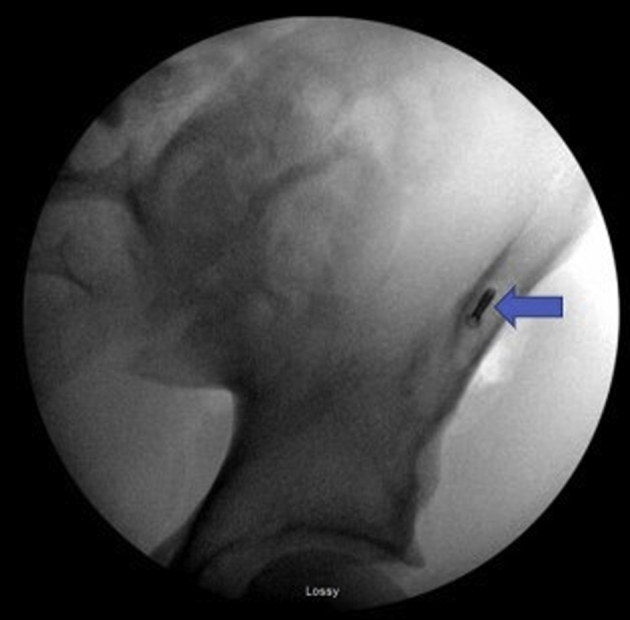
Postoperative radiograph of the left pelvis showing the countersunk screw (blue arrow denotes countersunk screw).
Step 4: Suture-Tape Bridge Construct
We then match two opposing color limbs of tape from the anchor and tie them with a Revo knot with 3 alternating half hitches. This further reinforces the repair at the bone tendon junction area. The remaining 2 limbs of tape are kept free, and now all 4 limbs of tape are crossed over top of the fracture to facilitate further compression. All limbs of tape are subsequently secured onto another 3.9 Omega knotless anchor to give a tape bridge construct, affecting further stability across the fracture and acting as a defunctioning construct.
The hip is taken through some range of motion to confirm excellent stability of the ASIS fragment.
Step 5: Wound Irrigation
The wound is copiously irrigated repeatedly to cleanse and avoid any possible incident of heterotopic ossification (HO). Postoperative Naprosyn (500 mg, twice daily, by mouth) is administered for 2 weeks to minimize the risk of HO.
Rehab Protocol
The surgery resulted in a same-day discharge. For the first 4 weeks, patient should begin with protected 20-lb, flat-touch, weight-bearing in an abductor hip brace locked at 45° flexion (to prevent hip extension and tension on the repair). After the 4-week mark, patient can be transitioned to full weight-bearing, with ROM restrictions lifted. Month 2 involved muscle balance and strengthening. Month 3, patient can be transitioned to functional training of the surgical hip and lower extremity with a gradual return to running. Month 4 and onward focused on advanced training and sport-specific conditioning for football and track and field, including resistance, agility, and aerobic training.
Discussion
ASIS avulsion fractures are rare, with only 1.4% accounting for all pelvic injuries.1, 2, 3, 4, 5 Oftentimes, surgical treatment is used to alleviate pain and allow the avulsion fracture to heal in an anatomic position to optimize tendon-bone attachment and muscle unit function. Depending on the severity of the injury, the majority of the time, the nonoperative treatment produces positive results, allowing for full and comfortable hip flexion with no limitations.10,11,14,15
Fortunately, this hybrid technique (tape bridge construct and cannulated screw fixation) is a safe and dependable method of surgically repairing the ASIS. Countersinking the screw below the surface of the ASIS (Fig 7) avoids hardware prominence and ensures impingement-free range of motion. The tape bridge construct provides two-dimensional compression across the fracture and gives a “belts and suspenders” type backup fixation (Fig 6, A-C). This allows for early passive hip range of motion without further risk of loosening the internal fixation (Fig 4).
Although this procedure is minimally invasive, there are several risks of surgery. First and foremost, heterotopic ossification is a possibility; this can be prevented with careful soft-tissue handling, thorough irrigation, and the administration of NSAIDs for a minimum of 2 weeks after surgery. Heterotopic ossification is the emergence of bone in tissue where bones are normally not present. Moreover, stiffness, nonunions, hip flexor weakness, detachment of the sartorius from the ASIS, and nonoptimal function of the pelvis due to discomfort during hip flexion are potential complications that may arise postoperatively. These complications and other pitfalls are listed in Table 2. More importantly, because of the low incidence rate of this injury, ASIS avulsion fractures are oftentimes misdiagnosed because the symptoms that arise are not considered limb-threatening and are, therefore, dismissed as regular musculotendinous injuries, such as tendinitis.8
Table 2.
Pearls and Pitfalls
Pearls
|
Various studies have shown unique approaches to surgically repairing the ASIS avulsion fracture. Generally, the treatment of choice for avulsion fractures is conservative treatment, (rest, analgesia, anti-inflammatories, and rehabilitation).9, 10, 11,14,15 One recent study showed a unique technique involving bone graft harvesting from the anterior iliac spine crest. To successfully repair a displaced fracture, this surgical technique requires the utilization of a special anatomic low-profile lock plate combined with the reconstruction of the bone defect, which was made possible by allograft cancellous bone.16 On the other hand, Kautzner et al. demonstrated a traditional approach: open reduction and lag screw with the washer fixation. In this study, 23 individuals were treated; 19 were male and 4 were female, with a mean age of 15 years. Ten patients were treated conservatively because they had sustained minimally displaced fractures; those with greater displacement fractures were treated surgically, which was 13 patients. Upon radiographic examination, there were 5 minor heterotopic ossifications; however, further treatment was unnecessary.17 Interestingly, Cai et al. compared the patients who were treated conservatively and treated operatively; they were divided into two groups, (Group A: nonsurgical group and Group B: absorbable screws group). Their technique involved the insertion of absorbable screws for fixation of the ASIS. The results showed that absorbable screws are a viable surgical option, which allowed for reduction in recovery time, time to resume sporting activities, and fewer early complications in adolescents. For both groups, callus growth was the only complication that occurred throughout the study. The American Academy of Orthopedic Surgeons (AAOS) lower hip and limb scores were calculated to assess hip function. Between the two groups, the AAOS scores showed a significant difference in the first few months postoperatively. However, after 6 months, there were no significant differences. The significant differences that were analyzed were callus growth, which was determined radiographically, time to return to sports activities, and any other complications that may arise.6
Our technique almost resembled the one discussed in Kautzner et al. except for a major difference; in our scenario, we implemented a hybrid technique (tape bridge construct and cannulated screw compression shown in Figs 5 and 6, A-A). This particular technique provided added reliability of anatomic primary bone healing through screw compression, but also a two-dimensional tape compression that allowed for early loosening-free range of motion. Additionally, our technique differed in two main ways: the size of the fragment and our choice of a small profile cannulated screw. These two differences allowed us to successfully achieve screw fixation. As previously mentioned, countersinking the screw was essential because this helped avoid prominence and future removal of the cannulated screw. This aforementioned technique is the most ideal for adolescent athletes who require high functional demands for sports consisting of versatility and speed.
Footnotes
Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video highlights the specific procedural steps performed for this particular anterior superior iliac spine avulsion (ASIS) fracture repair. The patient’s rehabilitation footage can be found at the conclusion of the video, showing the various fitness protocols in motion.
References
- 1.Rossi F., Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: Prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol. 2001;30:127–131. doi: 10.1007/s002560000319. [DOI] [PubMed] [Google Scholar]
- 2.Hansson P.G. Bilateral avulsion fracture of the anterior superior iliac spine. Acta Chir Scand. 1970;136:85–86. [PubMed] [Google Scholar]
- 3.Havlas V., Gaheer R.S., Trc T., Anwar F. Simultaneous bilateral avulsion fracture of the anterior superior iliac spine in a young athlete. Inj Extra. 2007;38:352–355. doi: 10.1016/j.injury.2007.01.027. [DOI] [Google Scholar]
- 4.Bendeddouche I., Jean-Luc B.B., Poiraudeau S., Nys A. Anterior superior iliac spine avulsion in a young soccer player. Ann Phys Rehabil Med. 2010;53:584–590. doi: 10.1016/j.rehab.2010.08.030. [DOI] [PubMed] [Google Scholar]
- 5.Naylor J.A., Goffar S.L., Chugg J. Avulsion fracture of the anterior superior iliac spine. J Orthop Sports Phys Ther. 2013;43:195. doi: 10.2519/jospt.2013.0406. [DOI] [PubMed] [Google Scholar]
- 6.Cai W., Xie Y., Su Y. Comparison of non-surgical and surgical treatment using absorbable screws in anterior-superior iliac spine avulsion fractures with over 1.5cm displacement. Orthop Traumatol Surg Res. 2020;106:1299–1304. doi: 10.1016/j.otsr.2020.02.014. [DOI] [PubMed] [Google Scholar]
- 7.Yang T., Li Y., Wang F., He R., He C. Repair of avulsion fracture of the anterior superior iliac spine by knotless suture bridge: Surgical technique and a review of 5 cases. Int J Sports Med Rehab. 2021;4 19: 1-7. [Google Scholar]
- 8.Eberbach H., Hohloch L., Feucht M., et al. Operative versus conservative treatment of apophyseal avulsion fractures of the pelvis in the adolescents: A systematical review with meta-analysis of clinical outcome and return to sports. BMC Musculoskelet Disord. 2017;18:162. doi: 10.1186/s12891-017-1527-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Porr J., Lucaciu C., Birkett S. Avulsion fractures of the pelvis - a qualitative systematic review of the literature. J Can Chiropr Assoc. 2011;55:247–255. [PMC free article] [PubMed] [Google Scholar]
- 10.Kosanovic M., Brilej D., Komadina R., Buhanec B., Pilih I.A., Vlaovic M. Operative treatment of avulsion fractures of the anterior superior iliac spine according to the tension band principle. Arch Orthop Trauma Surg. 2002;122:421–423. doi: 10.1007/s00402-002-0396-5. [DOI] [PubMed] [Google Scholar]
- 11.Beisland C., Maehlumshagen P.M. Avulsion fractures of the anterior superior iliac spine. Lex coincidentia—again. Tidsskr Nor Laegeforen. 1997;117:3366–3367. [PubMed] [Google Scholar]
- 12.Anduaga I., Seijas R., Pérez-Bellmunt A., Casasayas O., Alvarez P. Anterior iliac spine avulsion fracture treatment options in young athletes. J Invest Surg. 2020;33:159–163. doi: 10.1080/08941939.2018.1483447. [DOI] [PubMed] [Google Scholar]
- 13.Yeager K.C., Silva S.R., Richter D.L. Pelvic avulsion injuries in the adolescent athlete. Clin Sports Med. 2021;40:375–384. doi: 10.1016/j.csm.2020.12.002. [DOI] [PubMed] [Google Scholar]
- 14.Dhinsa B.S., Jalgaonkar A., Mann B., Butt S., Pollock R. Avulsion fracture of the anterior superior iliac spine: misdiagnosis of a bone tumour. J Orthop Traumatol. 2011;12:173–176. doi: 10.1007/s10195-011-0153-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boyce S.H., Quigley M.A. Simultaneous bilateral avulsion fractures of the anterior superior iliac spines in an adolescent sprinter. BMJ Case Reports. 2009;2009 doi: 10.1136/bcr.05.2009.1827. bcr05.2009.1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aurich M., Hofmann G.O. Fixation of displaced avulsion fracture of the anterior superior iliac spine (ASIS) after bone graft harvesting using anatomic low-profile locking plate: Case report and surgical technique. Z Orthop Unfall. 2021;159:681–686. doi: 10.1055/a-1192-7544. [DOI] [PubMed] [Google Scholar]
- 17.Kautzner J., Trc T., Havlas V. Comparison of conservative against surgical treatment of anterior-superior iliac spine avulsion fractures in children and adolescents. Int Orthop. 2014;38:1495–1498. doi: 10.1007/s00264-014-2323-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video highlights the specific procedural steps performed for this particular anterior superior iliac spine avulsion (ASIS) fracture repair. The patient’s rehabilitation footage can be found at the conclusion of the video, showing the various fitness protocols in motion.
This video highlights the specific procedural steps performed for this particular anterior superior iliac spine avulsion (ASIS) fracture repair. The patient’s rehabilitation footage can be found at the conclusion of the video, showing the various fitness protocols in motion.