SUMMARY
The Foodborne Diseases Active Surveillance Network (FoodNet) conducts population-based surveillance for Campylobacter infection. For 2010 through 2015, we compared patients with Campylobacter jejuni with patients with infections caused by other Campylobacter species. Campylobacter coli patients were more often >40 years of age (OR = 1·4), Asian (OR = 2·3), or Black (OR = 1·7), and more likely to live in an urban area (OR = 1·2), report international travel (OR = 1·5), and have infection in autumn or winter (OR = 1·2). Campylobacter upsaliensis patients were more likely female (OR = 1·6), Hispanic (OR = 1·6), have a blood isolate (OR = 2·8), and have an infection in autumn or winter (OR = 1·7). Campylobacter lari patients were more likely to be >40 years of age (OR = 2·9) and have an infection in autumn or winter (OR = 1·7). Campylobacter fetus patients were more likely male (OR = 3·1), hospitalized (OR = 3·5), and have a blood isolate (OR = 44·1). International travel was associated with antimicrobial-resistant C. jejuni (OR = 12·5) and C. coli (OR = 12) infections. Species-level data are useful in understanding epidemiology, sources, and resistance of infections.
Key words: Campylobacter, food-borne infections, surveillance
INTRODUCTION
Campylobacter causes an estimated 1·3 million illnesses in the USA each year [1]. Antimicrobial resistance in this pathogen is a serious concern [2]. There are currently 26 Campylobacter species; Campylobacter jejuni accounts for the majority (85–95%) of human infections, followed by C. coli (5–10%), and less commonly C. upsaliensis, C. fetus, C. lari, and other rare species [3].
Speciation is important in understanding the epidemiology of infection because Campylobacter organisms and their reservoirs are diverse. The primary reservoirs are poultry, cattle, and pigs; however, Campylobacter has been isolated from numerous other animal species and the environment, and the prevalence of different Campylobacter species in animals differs. For example, C. coli has been isolated more often than C. jejuni from swine and C. jejuni more often than C. coli from chicken [4]. C. fetus is primarily associated with cattle and sheep [5] but has also been identified in reptiles [6]. C. upsaliensis is frequently isolated from cats and dogs [7]. C. lari has been isolated from a variety of sources including wild birds, seawater, and shellfish [8]. Unpasteurized dairy products, poultry, and drinking water have been sources of Campylobacter outbreaks caused by various species [9]. Antimicrobial susceptibility patterns differ by species, with more erythromycin and ciprofloxacin resistance in C. coli isolates [4]. Differences in demographics of and risk factors for infection with various Campylobacter species have been described in patients in Europe [10, 11].
Few clinical laboratories in the USA routinely perform speciation beyond C. jejuni. Species-level identification of non-C.jejuni is challenging using phenotypic methods and it does not affect clinical treatment nor aid in outbreak detection. In addition, isolation methods are biased toward recovery of C.jejuni. Thus, Campylobacter surveillance data in the USA are typically presented at the genus level. To our knowledge, no comprehensive description of Campylobacter cases at the species level in the USA has been published. We attempt to fill this gap by describing available species-level data from 10 Foodborne Diseases Active Surveillance Network (FoodNet) sites, and comparing characteristics of patients and illnesses by the species causing infection.
METHODS
FoodNet is the foodborne disease component of the Centers for Disease Control and Prevention (CDC)’s Emerging Infections Program, a collaborative project of CDC, 10 state health departments, the United States Department of Agriculture's Food Safety and Inspection Service, and the Food and Drug Administration. Since 2004, the FoodNet catchment area has included the entire states of Connecticut, Georgia, Maryland, Minnesota, New Mexico, Oregon, and Tennessee and selected counties in California, Colorado, and New York. FoodNet conducts surveillance for human Campylobacter infections by routinely contacting clinical laboratories serving the catchment area to compile reports of all culture-confirmed infections. Staff collect patient demographics, hospitalization status, outcome, and specimen information from physicians, laboratory records, or through a patient interview in all sites. Information on international travel in the 7 days before illness onset is recorded from an interview or patient chart when available, and patients with such a history are considered to have travel-associated infections.
In some sites, isolates are sent from clinical laboratories to state public health laboratories (SPHLs) for confirmation and speciation. Between 2010 and 2015, Maryland, Minnesota, and New Mexico required all isolates to be submitted, and New York required submission of isolates from 15 of 34 FoodNet counties; routine submission was requested but not required in Georgia and Tennessee, and routine submission was neither requested nor required in California, Colorado, Connecticut, and Oregon. In addition, all sites forward some isolates to CDC for speciation and antimicrobial susceptibility testing as part of the National Antimicrobial Resistance Monitoring (NARMS) Program. Seven states selected Campylobacter isolates to forward based on a sampling scheme applied to isolates received at SPHLs: Georgia, Maryland, and New York (one forwarded for every two received), Minnesota (1:5), New Mexico (1:3), Oregon and Tennessee (all). In California, Colorado, and Connecticut, isolates are sampled from those received at the SPHL from one participating reference laboratory in each state. Because not all states require isolates to be submitted to the SPHL, the number of isolates sent to CDC is not consistently proportional to the total number of Campylobacter infections reported to FoodNet.
Identification of C. jejuni was performed by the typical colony and Gram stain morphology, catalase, oxidase, growth at 42 °C, and the hippurate hydrolysis test. Hippurate-positive isolates were identified as C. jejuni. Isolates that were negative for hippurate hydrolysis were further tested with indoxyl acetate. Hippurate-negative isolates were also further characterized by polymerase chain reaction assays with species-specific targets for C. jejuni (mapA or hipO gene), C. coli (ceuE gene or glyA gene), C. fetus (sapD gene), or other species-specific primers [12]. C. jejuni and C. coli isolates were tested for antimicrobial susceptibility using standard NARMS methods [13]. Only resistance to quinolones (ciprofloxacin or nalidixic acid) and macrolides (azithromycin or erythromycin) is included in our analysis because these are the two most important classes for treatment.
We analyzed data from cases of Campylobacter infection reported to FoodNet from 2010 through 2015 that had species results available from a SPHL or CDC. Antimicrobial susceptibility information was available for 2010–2015 from a subset of C. jejuni and C. coli isolates. We performed statistical analyses using SAS version 9.3 (SAS Institute, Cary, NC, USA). Incidence rates were calculated using US census data. C. coli, C. lari, C. fetus, and C. upsaliensis were individually compared with C. jejuni by age (median and in 5-year categories), sex, race, ethnicity, clinical symptoms, hospitalization, outcome, specimen source, international travel, season, and residence in a metro area. Fisher's exact tests were used to compare proportions. The criterion for significance was a 95% confidence interval (CI) excluding 1·0. All variables that showed significant associations were included in species-specific multivariable logistic regression models. Final models were developed using the stepwise option in Proc Logistic SAS Version 9.3. (SAS Institute, Cary, NC, USA). Seasons were defined as follows: winter (December–February), spring (March–May), summer (June–August), and autumn (September–November). FoodNet sites were grouped by US Census Region as follows: northeast (CT, NY); midwest (MN); south (GA, MD, TN); mountain (CO, NM); and Pacific (CA, OR). FoodNet counties were classified as urban, suburban, or rural based on USDA's Economic Research Service 2013 Rural–Urban Continuum Codes [14].
RESULTS
We identified 39 345 culture-confirmed Campylobacter infections in FoodNet sites from 2010 through 2015. We obtained species results for 16 549 (42%) of the isolates; 6971 (42%) were speciated at CDC, and 9578 (58%) were speciated at SPHLs. Forty-four percent of the results from SPHLs came from Minnesota. Of 16 549 isolates with species information, 14 672 (89%) were C. jejuni, 1404 (8%) were C. coli, 333 (2%) were C. upsaliensis, and 140 (1%) were other species, including C. lari (98), C. fetus (35), Campylobacter hyointestinalis (five), Campylobacter curvus (one), and Campylobacter helveticus (one). The percentage of non-C. jejuni species was relatively stable at 10% (259/2673) in 2010 and 12% (336/2784) in 2015.
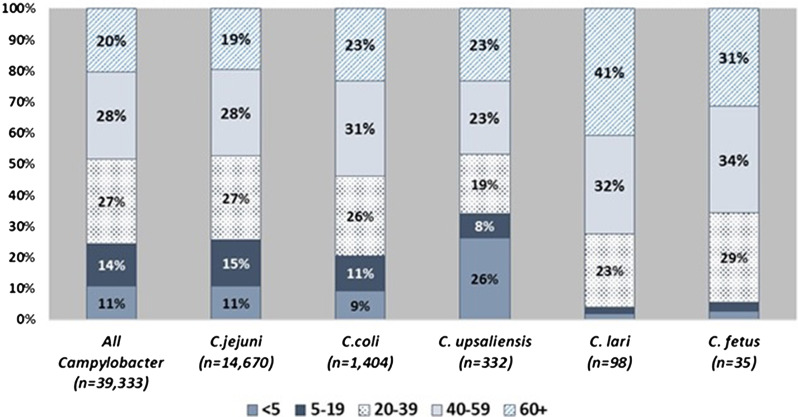
Patient age and sex distributions varied across Campylobacter species (Fig. 1 and Table 1). Patients with C. coli infection tended to be older than C. jejuni patients but had a similar sex distribution, with about 56% of infections in males. C. upsaliensis patients tended to be younger – the proportion of patients <5 years old was higher than for any other species – and a higher percentage (58%) were female. Although few patients with C. fetus and C. lari infection were reported, their age and sex distribution showed patterns similar to but more pronounced than those of C. coli, with even higher median ages (50 and 57 years) and percentages of males (83%, 63%), respectively. The majority of persons with Campylobacter infection identified as white and non-Hispanic, but there were some racial and ethnic differences between patients infected with different species. Thirteen percent of persons with C. fetus cases were Black compared with 8% or less for other species. Nine percent of C. fetus and 6% of C. coli patients were Asian, compared with 5% or less for other species. Sixteen percent of C. upsaliensis patients were Hispanic, compared with 12% or less for other species.
Fig. 1.
Distribution of patients with Campylobacter infection, by age group and species – FoodNet, 2010–2015.
Table 1.
Characteristics of Campylobacter patients, by five most common species – FoodNet, 2010–2015
| Characteristic | C. jejuni (N = 14 672) | C. coli (N = 1404) | C. upsaliensis (N = 333) | C. lari (N = 98) | C. fetus (N = 35) | Other species (N = 7) | Total (N = 16 549) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n/N | (%) | n/N | (%) | n/N | (%) | n/N | (%) | n/N | (%) | n/N | (%) | n/N | (%) | |
| Sex | ||||||||||||||
| Male | 8043/14 661 | (55) | 785/1401 | (56) | 141/332 | (42) | 62/98 | (63) | 29/35 | (83) | 5/7 | (71) | 9065/16 534 | (55) |
| Median age in years | ||||||||||||||
| All (female; male) | 37 (39; 36) | 43 (42; 44) | 37 (41; 23) | 57 (46; 59) | 50 (55; 49) | 49 (61; 47) | 38 (39; 37) | |||||||
| Race | ||||||||||||||
| Asian | 364/12 939 | (3) | 77/1237 | (6) | 3/299 | (1) | 5/93 | (5) | 3/32 | (9) | 0/6 | (0) | 452/14 606 | (3) |
| Black | 628/12 939 | (5) | 96/1237 | (8) | 15/299 | (5) | 2/93 | (2) | 4/32 | (13) | 3/6 | (50) | 748/14 606 | (5) |
| White | 11 243/12 939 | (87) | 1001/1237 | (81) | 265/299 | (89) | 85/93 | (91) | 24/32 | (75) | 3/6 | (50) | 12 621/14 606 | (86) |
| Other | 704/12 939 | (5) | 63/1237 | (5) | 16/299 | (5) | 1/93 | (1) | 1/32 | (3) | 0/6 | (0) | 785/14 606 | (5) |
| Ethnicity | ||||||||||||||
| Hispanic | 1485/12 682 | (12) | 131/1209 | (11) | 47/298 | (16) | 7/89 | (8) | 3/35 | (9) | 0/6 | (0) | 1673/14 319 | (12) |
| Outcome | ||||||||||||||
| Hospitalized | 2482/14 401 | (17) | 207/1380 | (15) | 52/325 | (16) | 13/97 | (13) | 19/35 | (54) | 3/7 | (43) | 2776/16 245 | (17) |
| Died | 14/14 441 | (0·1) | 2/1379 | (0·1) | 0/327 | (0) | 0/97 | (0) | 0/35 | (0) | 0/7 | (0) | 16/16 286 | (0·1) |
| Specimen source | ||||||||||||||
| Blood | 140/14 656 | (1) | 18/1402 | (1) | 11/332 | (3) | 2/96 | (2) | 16/35 | (46) | 0/7 | (0) | 187/16 528 | (1) |
| International travel | 1965/12 780 | (15) | 263/1197 | (22) | 3/284 | (1) | 6/84 | (7) | 2/31 | (6) | 0/5 | (0) | 2239/14 381 | (16) |
| Live in an urban area | 11 546/14 672 | (79) | 1178/1404 | (84) | 257/333 | (77) | 84/98 | (86) | 28/35 | (80) | 7/7 | (100) | 13 100/16 549 | (79) |
| Occur in autumn or winter | 5984/14 672 | (41) | 634/1404 | (45) | 177/333 | (53) | 53/98 | (54) | 15/35 | (43) | 2/7 | (29) | 6865/16 549 | (41) |
Specimen source and patient outcome also varied by species, especially for C. fetus. The proportion of isolates from blood was highest (46%) for C. fetus infections, and over half of C. fetus patients were hospitalized, compared with ⩽3% bloodstream isolations and ⩽17% hospitalization for most other species.
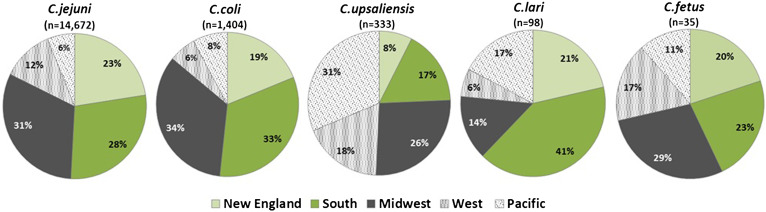
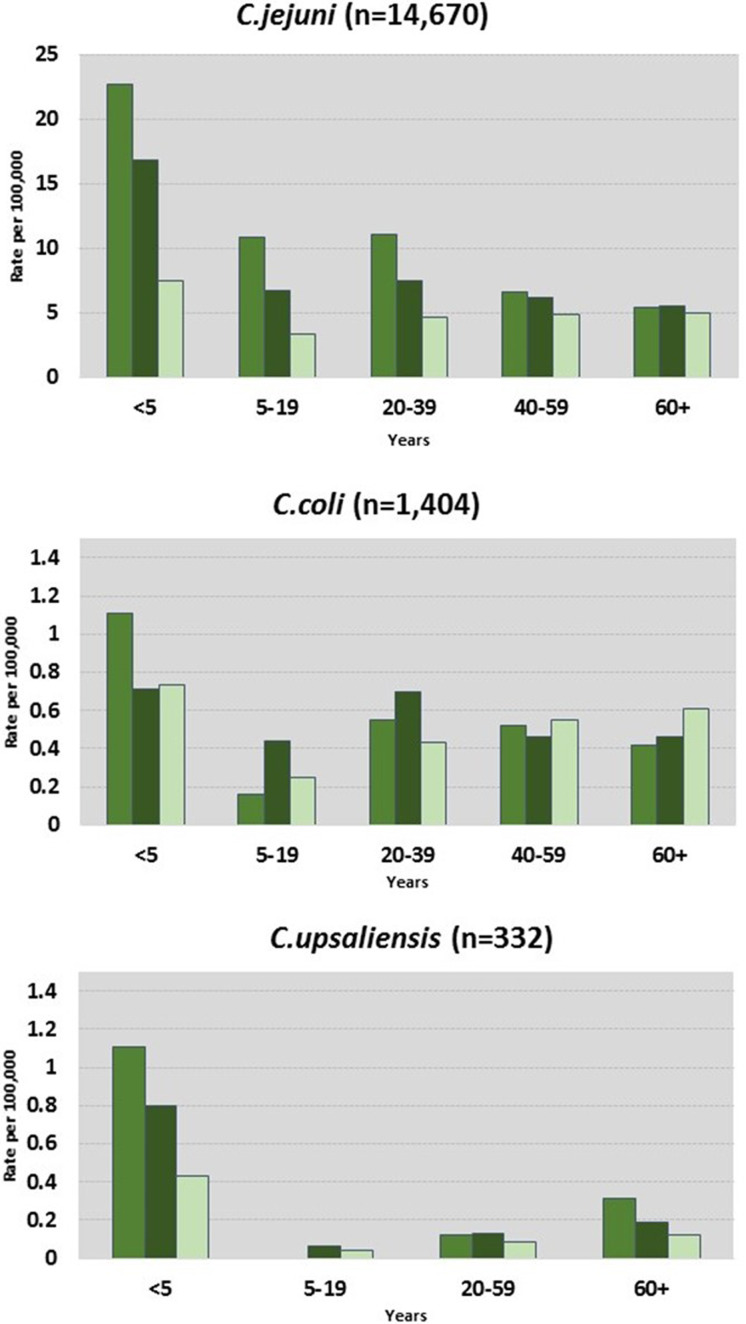
C. jejuni and C. coli infections had similar regional distributions. A higher percentage of C. upsaliensis cases occurred in the Pacific region, C. lari cases in the south, and C. fetus cases in the midwest (Fig. 2). C. jejuni incidence rates were highest in rural areas for persons younger than 60 years and in suburban areas for persons 60 years and older (Fig. 3). C. coli rates were highest in rural areas for children <5 years, in suburban areas for persons aged 5–39 years, and in urban areas for persons 40 years and older. C. upsaliensis rates were highest in rural areas for children <5 years and persons over 60 years. These patterns persisted after excluding travel-associated cases.
Fig. 2.
Distribution of Campylobacter species by geographic region – FoodNet, 2010–2015.
Fig. 3.
Campylobacter infections by species, location, and age group – FoodNet, 2010–2015.
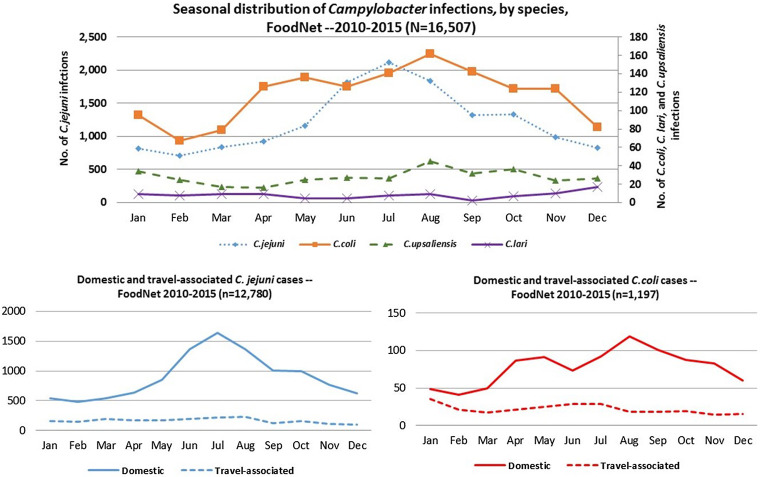
C. jejuni and C. coli infections exhibited strong summer peaks; the peak in C. coli cases occurred slightly later than C. jejuni. C. upsaliensis and C. lari infections predominated in autumn and winter months (Fig. 4). International travel in the 7 days before illness onset was reported by 16% of persons with Campylobacter infection, most commonly among those with C. coli (22%) and rarely among those with C. upsaliensis (1%) infections (Table 1). Travel-associated Campylobacter infections showed little seasonality with the exception of a slight winter peak among C. coli cases (Fig. 4).
Fig. 4.
Seasonal distribution of patients with Campylobacter infection by species, overall and by international travel history – FoodNet, 2010–2015.
Data from patients with infections of the more common Campylobacter species were compared with data from C. jejuni patients in multivariate models (Table 2). C. coli patients were more likely than C. jejuni patients to be older than 40 years, be Asian, be Black, have an infection in fall or winter, live in an urban area, and report international travel in the 7 days before infection; and less likely to be hospitalized. C. upsaliensis patients were more likely than C. jejuni patients to be female, be Hispanic, have an isolate from blood and infection in autumn or winter, and less likely to report international travel. C. lari patients were more likely than C. jejuni patients to be older than 40 years and have an infection in autumn or winter. C. fetus cases were more likely than C. jejuni cases to be male, hospitalized, and have an isolate from the blood.
Table 2.
Multivariate analysis of selected Campylobacter species compared with Campylobacter jejuni, FoodNet, 2010–2015
| Campylobacter coli | Campylobacter upsaliensis | Campylobacter lari | Campylobacter fetus | |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Male | n/s | 0·6 (0·5–0·8) | n/s | 3·1 (1·3–7·7) |
| Age | ||||
| ⩾40 (vs. <40 years) | 1·4 (1·2–1·6) | n/s | 2·9 (1·8–4·5) | n/s |
| Race | ||||
| Asian | 2·3 (1·7–3·0) | n/s | n/s | n/s |
| Black | 1·7 (1·3–2·2) | |||
| White | Reference | |||
| Ethnicity | ||||
| Hispanic | n/s | 1·6 (1·1–2·2) | n/s | n/s |
| Hospitalized | 0·8 (0·6–0·9) | n/s | n/s | 3·5 (1·6–7·5) |
| Specimen from blood | n/s | 2·8 (1·4–5·9) | n/s | 44·1 (20·2–96·6) |
| International travel | 1·5 (1·3–1·7) | 0·1 (0·02–0·2) | n/s | n/s |
| Occur in autumn or winter | 1·2 (1·0–1·3) | 1·7 (1·3–2·1) | 1·7 (1·1–2·5) | n/s |
| Live in an urban area | 1·2 (1·0–1·5) | n/s | n/s | n/s |
n/s, not statistically significant.
Antimicrobial susceptibility information was available for 6010 C. jejuni and 665 C. coli isolates. Resistance to quinolones (35% vs. 24%) and macrolides (11% vs. 3%) was higher among C. coli isolates than C. jejuni isolates. Resistance among C. jejuni isolates was higher in the metro (27%) than in suburban and rural (15%) areas (P < 0·0001). Among patients with C. jejuni infection, age >20 years (OR = 1·4; 95% CI 1·1–1·8), Asian race (OR = 2·3; 95% CI 1·4–3·9), and international travel in the 7 days before infection (OR = 12·5; 95% CI 10·0–15·7) was associated with any resistance. Among C. coli patients, international travel in the 7 days before infection (OR = 12; 95% CI 6·4–22·7) was associated with any resistance. Among travelers with either species, the highest percentage of resistant infections was found among persons who visited Asia (18/171 (91%)) or South America (17/83 (83%)).
DISCUSSION
Public health activities to control Campylobacter infections in the USA generally focus at the genus level; speciation of isolates is relatively unusual. Our analysis showed significant demographic and clinical differences between patients infected with different species highlighting the value of examining Campylobacter at the species level. The high burden of Campylobacter infection, its associated sequelae such as Guillain–Barré syndrome, and the potential for treatment failure due to antimicrobial resistance emphasize the urgency of improved control.
C. jejuni is the most common species and provides a good comparison group against which to examine characteristics of other species. In our data, patients with C. jejuni infection were predominately White and non-Hispanic, and a little over half were male. Less than a quarter of patients were hospitalized, and few had invasive infections. Rates of infection were highest in rural areas, particularly among children <5 years old, an association that has been well documented in other countries [15, 16]. C. jejuni infections overall showed a strong summer seasonality consistent with patterns described for other temperate countries [17]. It is well established that poultry is the primary risk factor for sporadic infections [18, 19]. Although poultry is eaten year-round, the seasonality of infections may be explained by studies that have shown that the prevalence of Campylobacter in broiler flocks and poultry at retail varies by season and is highest in warmer months [20, 21]. Exposure to other domestic risk factors common in summer months such as animal contact, raw milk consumption, swimming, eating barbeque-prepared meals, and drinking water from untreated sources likely also influence the summer peak [19, 22].
C. coli is the second most commonly identified species in the USA. Compared with C. jejuni, persons infected with C. coli were more often older than 40 years, Asian, or Black. Nearly a quarter of patients with C. coli reported international travel. Many of these differences are consistent with previous studies [10, 11, 23], but the association with Black race, to our knowledge, has not been previously reported. Mechanisms behind these differences are not known but could reflect occupational or environmental exposures, cultural practices, dietary preferences, or genetic predisposition. The use of proton pump inhibitors has been associated with Campylobacter infection [18, 24], and differential resistance to acid between the two species has been hypothesized to play a role in age differences [23]. C. coli infection has been associated with the consumption of pate and meat pies [10], bottled water [10], undercooked eggs [25], swimming [18], and contaminated surface water [26]. International travel might contribute to the higher rate of C. coli infections in winter months.
C. upsaliensis is the third most commonly identified species in the USA. Compared with C. jejuni, patients with C. upsaliensis infection were more often female and Hispanic. Of all the species we examined, C. upsaliensis infections were least likely to be travel-associated. Female gender has been associated with infection with specific C. coli and C. jejuni strain types found in poultry [27], possibly because women are more likely than men to prepare food, but it is unclear whether this explanation extends to other species. While C. upsaliensis has been isolated from foods such as ground beef [28], the infection has more often been associated with exposure to domestic pets such as dogs and cats. The association with Hispanic ethnicity is unexplained. It could reflect food preferences or be linked to cultural practices and should be further explored, but we do not think it is related to exposures abroad, because the travel-associated proportion is so low. Our finding that C. upsaliensis infections occur more often in autumn or winter months is intriguing but should be interpreted with caution given the small sample size.
We identified a small number of infections with other Campylobacter species. Patients with C. fetus and C. lari infections were predominately male and tended to be older than those with C. jejuni. Older age and male predominance has been previously documented for C. fetus [5, 29] but is not well understood. It is possible that occupational exposure to cattle and sheep plays a role as many sporadic C. fetus cases reported in the literature have occurred among farmers or abattoir workers [5]. Patients with C. fetus infection were much more likely to have bloodstream infections and to be hospitalized than patients infected with any other species. Host factors, pathogen factors, or both may explain this characteristic. C. lari is associated with gastrointestinal infections and bacteremia especially in persons who are immunocompromised. It has been isolated from multiple environmental sources, including surface water, wild birds, and domestic animals [8], and contaminated water has been associated with infection [30].
Consistent with previous studies [31, 32], we found international travel to be a risk factor for antimicrobial-resistant infections, particularly among C. coli patients, and a high percentage of resistant infections occurred among travelers to Asia and South America. Resistance to ciprofloxacin is known to be common in these regions and appears to be increasing [33, 34]. Ciprofloxacin resistance among travelers is a concern because ciprofloxacin is a common treatment for diarrhea in returned travelers [35], although a macrolide is the drug of choice for Campylobacter infections [36]. We also found that a higher percentage of antimicrobial-resistant infections occurred in urban areas. This finding is consistent with reports from the Netherlands; they hypothesized consumption of ready-to-eat foods may be higher in urban areas [31]. It is also possible that persons in urban areas have more severe illness or co-morbidities. Interventions to combat resistance in the USA should focus on targeting domestic food sources, enhancing awareness among healthcare providers and travelers about the increased risk of resistant infections associated with international travel, and promoting appropriate antimicrobial stewardship.
Many factors affect the availability of Campylobacter species data in the USA and these should be taken into account when interpreting our findings. Although infection has been reportable in most states, it did not become a nationally notifiable infection until 2015 [37]. Only 22 (44%) states request or require positive specimens to be sent to SPHL for confirmation and speciation [38], and there are currently no national guidelines for the isolation and speciation of Campylobacter. Only 31% of 403 laboratories serving the FoodNet catchment area routinely speciate Campylobacter [39]. Thus, the process leading to the inclusion of cases in our dataset is complex, and the proportion of cases due to each species is not generalizable to all Campylobacter infection. Nonetheless, the differences we observe between species are unlikely to be due to selection bias, as these pre-speciation biases would be expected to affect all species similarly.
Many laboratories rely on isolation methods and selective media optimized for recovery of C. jejuni from the stool, decreasing the likelihood of recovering many other Campylobacter species. Selective media for isolation of specific non-jejuni species either has not been developed or is not widely available. Isolation methods, such as filtration, that would increase recovery of non-jejuni species are labor-intensive and few laboratories perform them. Traditional phenotypic identification methods [38] are widely performed and accurately identify hippurate-positive C. jejuni. However, these methods do not accurately identify hippurate-negative Campylobacter species or hippurate-negative C. jejuni. A method for species-level identification of Campylobacter using matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF) has been described [40] and is becoming more widely used by clinical laboratories and SPHLs. DNA-based molecular methods can enhance species identification but can be expensive to implement. Since 2010, there has been an increase in the proportion of infections caused by species other than C. jejuni. This could reflect a real change in sources of human Campylobacter infections. Alternatively, it could be due to increased awareness of the non-jejuni species and improved ability to accurately identify these species in the state health departments after the implementation of CDC's quality assurance program for the identification of Campylobacter in 2008 and follow-up training made available to the SPHLs.
The use of culture-independent diagnostic tests (CIDTs) for identification of Campylobacter in FoodNet sites is increasing [41]. Decreasing availability of Campylobacter isolates has important implications for public health surveillance. While CIDTs are quicker and easier to perform, the most commonly used tests at present are limited in the Campylobacter species detected. They do not differentiate between Campylobacter species, nor do they yield an isolate for speciation or antimicrobial susceptibility testing. A strategy for obtaining species information, such as the reflex culture of specimens with a positive CIDT result, reflex culture if medically indicated for patient care, or collection of isolates from sentinel laboratories, is needed to improve understanding of species-related differences and inform source attribution and risk factor studies. Advanced molecular detection methods, such as whole genome sequencing, will greatly facilitate identification and classification of strains and comparison of strains from human, food, animal, and environmental sources, but these methods rely on the availability of isolates to test. Coupled with standardized case exposure data, these approaches offer promise for a clearer understanding of the epidemiology of Campylobacter species in the USA, which in turn can inform prevention strategies.
ACKNOWLEDGEMENTS
This work was supported by the Centers for Disease Control and Prevention (CDC-RFA-CK17-1701 – Emerging Infections Program).
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Scallan E, et al. Foodborne illness acquired in the United States – major pathogens. Emerging Infectious Diseases 2011; 17(1): 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States, 2013. (http://www.cdc.gov/drugresistance/threat-report-2013/). Accessed 29 August 2014.
- 3.Fitzgerald C. Campylobacter. Clinics in Laboratory Medicine 2015; 35(2): 289–298. [DOI] [PubMed] [Google Scholar]
- 4.FDA. NARMS Integrated Report: 2012–2013. The National Antimicrobial Resistance Monitoring System: Enteric Bacteria (http://www.fda.gov/AnimalVeterinary/SafetyHealth/AntimicrobialResistance/NationalAntimicrobialResistanceMonitoringSystem/ucm059103.htm). Accessed 19 November 2015.
- 5.Wagenaar JA, et al. Campylobacter fetus infections in humans: exposure and disease. Clinical Infectious Diseases 2014; 58(11): 1579–1586. doi: 10.1093/cid/ciu085. Epub 2014 Feb 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gilbert MJ, et al. Occurrence, diversity, and host association of intestinal Campylobacter, Arcobacter, and Helicobacter in reptiles. PLoS ONE 2014; 9(7): e101599. doi: 10.1371/journal.pone.0101599. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Acke E, et al. Prevalence of thermophilic Campylobacter species in household cats and dogs in Ireland. Veterinary Record 2009; 164(2): 44–47. [DOI] [PubMed] [Google Scholar]
- 8.Matsuda M, Moore JE. The epidemiology and zoonotic transmission of thermophilic Campylobacter lari. British Microbiology Research Journal 2011; 1(4): 104–121. [Google Scholar]
- 9.Taylor EV, et al. Common source outbreaks of Campylobacter infection in the USA, 1997–2008. Epidemiology and Infection 2013; 141(5): 987–996. doi: 10.1017/S0950268812001744. Epub 2012 Aug 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gillespie IA, et al. A case-case comparison of Campylobacter coli and Campylobacter jejuni infection: a tool for generating hypotheses. Emerging Infectious Diseases 2002; 8: 937–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bessède E, et al. Comparison of characteristics of patients infected by Campylobacter jejuni, Campylobacter coli, and Campylobacter fetus. Journal of Clinical Microbiology. 2014; 52(1): 328–330. doi: 10.1128/JCM.03029-13. Epub 2013 Nov 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Linton D, et al. PCR detection, identification to species level, and fingerprinting of Campylobacter jejuni and Campylobacter coli direct from diarrheic samples. Journal of Clinical Microbiology 1997; 35: 2568–2572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.CDC. National Antimicrobial Resistance Monitoring System for Enteric Bacteria (NARMS): Human Isolates Final Report, 2013. Atlanta, Georgia: U.S. Department of Health and Human Services, CDC, 2015. [Google Scholar]
- 14.United States Department of Agriculture Economic Research Service (http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx).
- 15.Green CG, Krause DO, Wylie JL. Spatial analysis of Campylobacter infection in the Canadian province of Manitoba. International Journal of Health Geographics 2006; 5: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ethelberg S, et al. Spatial distribution and registry-based case-control analysis of Campylobacter infections in Denmark, 1991–2001. American Journal of Epidemiology 2005; 162(10): 1008–1015. Epub 2005 Oct 5. [DOI] [PubMed] [Google Scholar]
- 17.Nylen G, et al. The seasonal distribution of Campylobacter infection in nine European countries and New Zealand. Epidemiology and Infection 2002; 128(3): 383–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doorduyn Y, et al. Risk factors for indigenous Campylobacter jejuni and Campylobacter coli infections in The Netherlands: a case-control study. Epidemiology and Infection 2010; 138(10): 1391–1404. doi: 10.1017/S095026881000052X. Epub 2010 Mar 12. [DOI] [PubMed] [Google Scholar]
- 19.Friedman CR, et al. Risk factors for sporadic Campylobacter infection in the United States: a case-control study in FoodNet sites. Clinical Infectious Diseases 2004; 38(Suppl. 3): S285–S296. [DOI] [PubMed] [Google Scholar]
- 20.Boysen L, Vigre H, Rosenquist H. Seasonal influence on the prevalence of thermotolerant Campylobacter in retail broiler meat in Denmark. Food Microbiology 2011; 28(5): 1028–1032. doi: 10.1016/j.fm.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 21.Willis WL, Murray C. Campylobacter jejuni seasonal recovery observations of retail market broilers. Poultry Science 1997; 76(2): 314–317. [DOI] [PubMed] [Google Scholar]
- 22.Schonberg-Norio D, et al. Swimming and Campylobacter infections. Emerging Infectious Diseases 2004; 10: 1474–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roux F, et al. Elucidating the aetiology of human Campylobacter coli infections. PLoS ONE 2013; 8(5): e64504. doi: 10.1371/journal.pone.0064504. Print 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Neal KR, et al. Omeprazole as a risk factor for Campylobacter gastroenteritis: case-control study. British Medical Journal 1996; 312: 414–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sopwith W, et al. Investigation of food and environmental exposures relating to the epidemiology of Campylobacter coli in humans in Northwest England. Applied and Environmental Microbiology 2010; 76(1): 129–135. doi: 10.1128/AEM.00942-09. Epub 2009 Oct 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zeigler M, et al. Outbreak of campylobacteriosis associated with a long-distance obstacle adventure race – Nevada, October 2012. MMWR Morbidity and Mortality Weekly Report 2014; 63(17): 375–378. [PMC free article] [PubMed] [Google Scholar]
- 27.Bessell PR, et al. Using sequence data to identify alternative routes and risk of infection: a case-study of Campylobacter in Scotland. BMC Infectious Diseases 2012; 12: 80. doi: 10.1186/1471-2334-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Trokhymchuk A, et al. Prevalence and diversity of Campylobacter species in Saskatchewan retail ground beef. Journal of Food Protection 2014; 77(12): 2106–2110. doi: 10.4315/0362-028X.JFP-14-247. [DOI] [PubMed] [Google Scholar]
- 29.Gazaigne L, et al. Campylobacter fetus bloodstream infection: risk factors and clinical features. European Journal of Clinical Microbiology and Infectious Diseases 2008; 27(3): 185–189. Epub 2007 Nov 13. [DOI] [PubMed] [Google Scholar]
- 30.Broczyk A, et al. Water-borne outbreak of Campylobacter laridis-associated gastroenteritis. Lancet 1987; 1(8525): 164–165. PMID:2880002. [DOI] [PubMed] [Google Scholar]
- 31.Van Hees BC, et al. Regional and seasonal differences in incidence and antibiotic resistance of Campylobacter from a nationwide surveillance study in The Netherlands: an overview of 2000–2004. Clinical Microbiology and Infection 2007; 13(3): 305–310. [DOI] [PubMed] [Google Scholar]
- 32.Kassenborg HD, et al. Fluoroquinolone-resistant Campylobacter infections: eating poultry outside of the home and foreign travel are risk factors. Clinical Infectious Diseases 2004; 38(Suppl. 3): S279–S284. [DOI] [PubMed] [Google Scholar]
- 33.Pollett S, et al. Campylobacter antimicrobial resistance in Peru: a ten-year observational study. BMC Infectious Diseases 2012; 12: 193–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Post A, et al. Antibiotic susceptibility profiles among Campylobacter isolates obtained from international travelers between 2007 and 2014. European Jounal of Clinical Microbiology and Infectious Diseases 2017. doi: 10.1007/s10096-017-3032-6. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Steffen R, Hill DR, DuPont HL. Traveler's diarrhea: a clinical review. Journal of the American Medical Association 2015; 313(1): 71–80. doi: 10.1001/jama.2014.17006. Review. [DOI] [PubMed] [Google Scholar]
- 36.Allos BM, Blaser M. Campylobacter jejuni and related species. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, 7th edn. Churchill, Livingstone: Elsevier Press, Philadelphia, PA, 2010, p. 2799. [Google Scholar]
- 37.Council of State and Territorial Epidemiologists. Standardized Surveillance for Campylobacteriosis and Addition to the Nationally Notifiable Condition List. Atlanta, GA: Council of State and Territorial Epidemiologists, 2003. (http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/2014PS/14_ID_09upd.pdf). Accessed 15 June 2015. [Google Scholar]
- 38.CSTE. State legal requirements for submission of isolates and other clinical materials by clinical laboratories: a review of state approaches (https://www.aphl.org/aboutAPHL/publications/Documents/StateRequirements_Appendix_v6.pdf) Accessed 15 May 2017.
- 39.Hurd S, et al. Clinical laboratory practices for the isolation and identification of Campylobacter in Foodborne Diseases Active Surveillance Network (FoodNet) sites: baseline information for understanding changes in surveillance data. Clinical Infectious Diseases 2012; 54(Suppl. 5): S440–S445. doi: 10.1093/cid/cis245. [DOI] [PubMed] [Google Scholar]
- 40.Mandrell RE, et al. Speciation of Campylobacter coli, C. jejuni, C. helveticus, C. lari, C. sputorum, and C. upsaliensis by matrix-assisted laser desorption ionization-time of flight mass spectrometry. Applied and Environmental Microbiology 2005; 71(10): 6292–6307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iwamoto M, et al. Bacterial enteric infections detected by culture-independent diagnostic tests – FoodNet, United States, 2012–2014. MMWR Morbidity and Mortality Weekly Report 2015; 64(9): 252–257. [PMC free article] [PubMed] [Google Scholar]