Abstract
Introduction:
Reperfusion therapy (RT) is a mainstay treatment for acute ischemic stroke (AIS). We aimed to evaluate the impact of a comprehensive national policy (CNP) to improve access to RT for AIS patients across Lithuania.
Patients and methods:
Aggregated anonymized data on AIS cases treated in Lithuanian hospitals between 2006 and 2019 were retrospectively obtained from the Institute of Hygiene and the Stroke Integrated Care Management Committee. Through an interrupted time series analysis, we examined the trends in AIS hospital admissions, RT, and in-hospital case fatality rates prior to the enactment of CNP in 2014, changes immediately after the intervention, and differences in trends between the pre- and post-intervention periods. Mean yearly door-to-needle times were calculated post-intervention.
Results:
114,436 cases were treated for AIS in Lithuanian hospitals before, and 65,084 after the government intervention. We observed a significant decreasing post-intervention trend change in AIS hospital admission rate per 100,000 population (regression coefficient ± standard error: β = –16.47 ± 3.95, p = 0.002) and an increasing trend change in the proportion of AIS patients who received reperfusion treatment: intravenous thrombolysis (β = 1.42 ± 0.96, p < 0.001) and endovascular therapy (β = 0.85 ± 0.05, p < 0.001). The proportion of patients treated in stroke centers increased immediately after the intervention (β = 4.95 ± 1.14, p = 0.001), but the long-term post-intervention trend did not change. In addition, there was a significant decreasing trend in all cause in-hospital case fatality rate within primary and comprehensive stroke centers after the intervention (β = –0.60 ± 0.18, p = 0.008) despite its prompt initial immediate increase (β = 1.68 ± 0.73, p = 0.043). The mean countrywide door-to-needle time decreased from 68 min in 2014 to 43 min in 2019.
Conclusion:
The comprehensive national stroke patient care policy could be associated with an immediate increase in stroke center treatment rate, increased access to RT, and improved stroke care performance measures.
Keywords: Ischemic stroke, implementation, thrombolysis, thrombectomy, interrupted time series, Lithuania
Graphical abstract.
Introduction
Stroke is one of the major causes of death and disability-adjusted life years worldwide.1,2 The incidence of acute ischemic stroke (AIS) and stroke mortality in Lithuania is amongst the highest in the world, 3 in a large part due to a high prevalence and poor control of cardiovascular risk factors (CV RF).4,5 Moreover, the largest increase in the age-adjusted stroke incidence and prevalence rates, as well as the lowest average annual percentage decrease in stroke mortality among all European Union countries are expected in Lithuania. 6
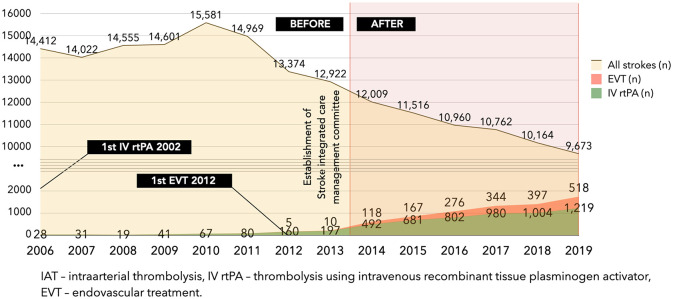
Reperfusion therapy (RT) – thrombolysis using intravenous recombinant tissue plasminogen activator (IV rtPA) and endovascular treatment (EVT), is a widely accepted, safe, and cost-effective method to treat AIS with proven clinical efficacy.7,8 However, its broad implementation in daily clinical practice is challenging.9–12 In Lithuania, the first thrombolysis with IV rtPA was performed after its approval for AIS in 2002, whereas EVT was introduced to clinical practice in 2012. Although IV rtPA was recommended as a first-line treatment for AIS according to national guidelines since 2007, 13 the total annual number of IV rtPA remained low across the country until 2013.
Ever since its establishment in 1997, the Lithuanian Stroke Association (LSA) – a national non-governmental organization uniting stroke care specialists – was one of the leading forces seeking improvement in stroke care quality in Lithuania. Many of the LSA’s objectives came to fruition in 2014, when the Ministry of Health (MoH) of the Republic of Lithuania initiated multiple activities in order to promote and implement modern RT for stroke patients on the national level (see Supplemental Table 1). The integrated government support included ministerial orders on the establishment of a national network of acute stroke centers, the reorganization of AIS patient flow (all acute stroke patients were obliged to be referred to the nearest acute stroke center directly), a coordinated inventory of the AIS diagnostic and management methods, standard requirements for the accreditation of primary stroke centers (PSCs) and comprehensive stroke centers (CSCs), 14 and the creation of the Stroke Integrated Care Management Committee (SICMC) under the MoH. 15 The aim of SICMC was to coordinate new financial incentives, which included a centrally coordinated purchase of rtPA, a retrospective per-case AIS total EVT expense reimbursement to the healthcare providers, and the lift of the budget cap for AIS patients. In addition, it collected and monitored data from stroke treatment sites regarding acute RT, logistics, use of resources and diagnostic investigations, rehabilitation, in-hospital complications, case fatality, and other AIS care performance measures. Quarterly reports were provided to the MoH in order to identify areas that require improvement.
Our study aimed to evaluate the impact of the comprehensive national policy on multiple stroke care performance measures, reflecting access to RT for AIS patients across Lithuania. We analyzed data on cases, treated in acute care hospitals for AIS between 2006 and 2019, using a nationwide public health register and reports supplied to SICMC by all individual stroke-ready hospitals.
Patients and methods
Study design and data collection
Two data sources were used for this study. Firstly, aggregated data on all AIS cases treated in Lithuanian hospitals between 2006 and 2019 were retrospectively obtained from the Institute of Hygiene – an institution, which manages public health registers and is responsible for the monitoring of the Lithuanian population health, health care activities, and resources. 16 The dataset included the total number of AIS (corresponding to the International Statistical Classification of Diseases and Related Health Problems, 10th revision, Australian Modification, code I63), the number of AIS cases treated in Lithuanian CSCs, PSCs, and nonspecialized hospitals (NHs), their gender, age group, place of residence, days spent in hospital, and in-hospital case fatality. The full description of the statistical research methodology of how the dataset was obtained, and how its completeness and patient anonymity were secured is available online. 17
Secondly, the data on the number of RTs performed were collected from the SICMC. Since the establishment of the SICMC in 2014, every quarter all active Lithuanian CSCs and PSCs (see Supplemental Table 2) were obliged to report to it aggregated anonymized data on the predetermined stroke care performance measures, consistent with the information from their hospital information systems. Among others, these include the total number of RT procedures (IV rtPA and EVT) in each hospital and their mean door-to-needle (DTN) time. It should be noted that there are no data on patients who received bridging therapy (IV rtPA in combination with EVT), therefore, a proportion of cases could have received both modes of treatment. The full list of performance measures, developed in accordance with the best practice recommendations of the international guidelines18,19 and adapted to meet the local needs, is shown in Supplemental Table 3.
Our research project was proposed to the MoH and had been designed in accordance with the Declaration of Helsinki. A government advisory committee reviewed our proposal and recommended that the MoH grant us permission to use the required data and perform the study. Data have been collected as part of routine clinical practice, therefore, there was no need for specific informed consent, and approval of the Ethics Committee was not required.
Setting
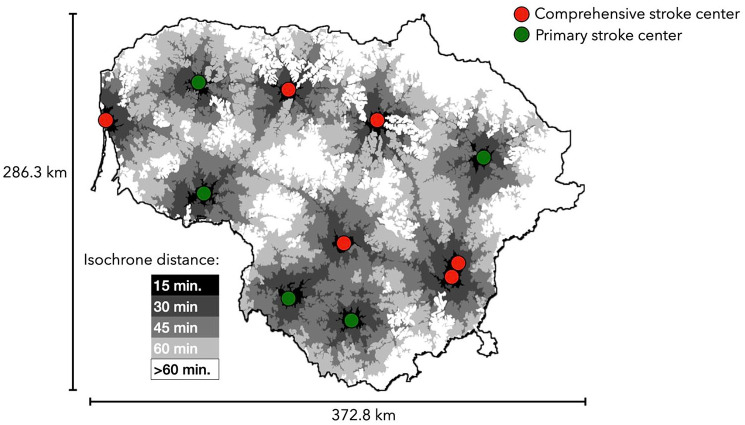
In Lithuania, acute stroke care hospitals are categorized into CSCs, PSCs, and NHs, according to available reperfusion treatment. The distribution of the six Lithuanian CSCs and the five PSCs with isochrone distances of time it takes to reach the closest stroke-ready hospital on a Sunday evening by car is shown in Figure 1. The map was created using publicly available data from Google Maps.
Figure 1.
The distribution of Lithuanian primary and comprehensive stroke centers and isochrone distances to reach them.
As noted above, different actions were taken on a national level in order to encourage the implementation of modern RTs for stroke patients in 2014, marking the introduction of the comprehensive national policy in Lithuania. Thus, we defined the period before 2014 as the pre-intervention period (eight calendar years) and the period from 2014 to 2019 as the post-intervention period (six calendar years).
Outcome measures
The impact of the comprehensive national policy on six different stroke-related outcomes was evaluated. They included the AIS hospital admission rate per 100,000 population, the proportion of patients who received RT, the proportion of cases treated within CSCs and PSCs, and in-hospital case fatality. The in-hospital case fatality was defined as a proportion of all-cause in-hospital AIS patient deaths out of all admitted AIS cases. Since DTN time data were available just for the post-intervention period, only the post-interventional DTN time trend was analyzed. These outcome measures were selected by the authors as they were judged to be most influenced by the changes in the comprehensive national policy.
Statistical analysis
We compared categorical variables using the χ 2 test. Based on their Gaussian distribution, the quantitative variables were compared using the Student’s t-test. Available sociodemographic characteristics were compared before and after the introduction of a comprehensive national policy in Lithuania. The 95% confidence intervals (CI) were calculated, where applicable.
We analyzed the yearly trends of the outcome measures – AIS hospital admission rate, the proportion of patients who received RT, the proportion of cases treated within CSCs and PSCs, and all-cause in-hospital case fatality (overall and within CSCs and PSCs). To calculate the AIS hospital admission rate per 100,000 population, the patient numbers were standardized to the population of Lithuania on the first day of each calendar year. 20 Using an interrupted time series analysis, we evaluated the time trends of the outcome measures before and after the introduction of a comprehensive national policy in 2014.21,22
The analysis was performed using the following regression equation: Yt = β0 + β1Tt + β2Xt + β3Pt + εt, where Yt is the aggregated outcome at time t (year), Tt is the time (years) since the start of the study period, Xt is the dummy variable representing the period after the introduction of a comprehensive national policy, Pt is a continuous variable indicating time (years) since this intervention (Pt is equal to 0 before intervention), β0 is the intercept, β1 is the slope prior to the intervention, β2 is the change in level in the period immediately following the intervention, and β3 is the difference between the pre- and post-intervention slopes. The standard errors (SE) were calculated. p < 0.05 (two-sided) was considered statistically significant. R version 3.6.2 was used for statistical analysis.
Results
Demographic characteristics
Altogether, 114,436 cases were treated for AIS in Lithuanian hospitals before the government intervention, and 65,084 during the study period after it (Table 1). The absolute number of AIS admissions decreased by a striking 25.1% between 2013 and 2019 (Figure 2). As compared with the pre-intervention period, after the introduction of the comprehensive national policy, significantly fewer female patients were diagnosed with AIS (57.2% (95% CI 56.8–57.6) vs 59.0% (58.7–59.3), p < 0.001), there were proportionally fewer individuals under 45 years of age (1.4% (1.3–1.5) vs 1.8% (1.7–1.9), p < 0.001), and significantly fewer patients came from urban areas (64.7% (64.3–65.0) vs 66.5% (66.2–66.8), p < 0.001). In addition, significantly more cases were treated in CSCs and PSCs after the government intervention (54.4% (54.0–54.8) vs 40.3% (40.0–40.5), p < 0.001), and the mean hospital stay decreased significantly (mean ± standard deviation: 10.2 ± 1.7 vs 13.0 ± 0.2 days, p < 0.001).
Table 1.
Demographic characteristics for stroke patients in Lithuania.
| Stroke patients 2006–2013 (n = 114,436) | Stroke patients 2014–2019 (n = 65,084) | p-Value | |
|---|---|---|---|
| Female, n (%) | 67,510 (59.0) | 37,234 (57.2) | <0.001 |
| Age range in years, n (%) | |||
| 0–17 | 27 (0.02) | 34 (0.05) | 0.002 |
| 18–44 | 2001 (1.7) | 866 (1.3) | <0.001 |
| 45–64 | 26,212 (22.9) | 12,958 (19.9) | <0.001 |
| ⩾65 | 86,168 (75.3) | 51,226 (78.7) | <0.001 |
| No data | 28 (0.02) | 0 | |
| Place of residence, n (%) | |||
| Urban | 76,083 (66.5) | 42,089 (64.7) | <0.001 |
| Rural | 37,869 (33.1) | 22,900 (35.2) | <0.001 |
| No data | 484 (0.4) | 95 (0.1) | |
| Treatment place, n (%) | |||
| CSC | 35,584 (31.1) | 27,625 (42.4) | <0.001 |
| PCS | 10,486 (9.2) | 7784 (12.0) | <0.001 |
| Nonspecialized hospital | 68,366 (59.7) | 29,675 (45.6) | <0.001 |
| Days in hospital, mean (SD) | 13.0 (1.7) | 10.2 (0.2) | <0.001 |
CSC: comprehensive stroke center; PSC: primary stroke center; SD: standard deviation.
Figure 2.
The absolute number of ischemic stroke cases and those who received any kind of reperfusion therapy in Lithuania.
Temporal trends in AIS hospital admission rates
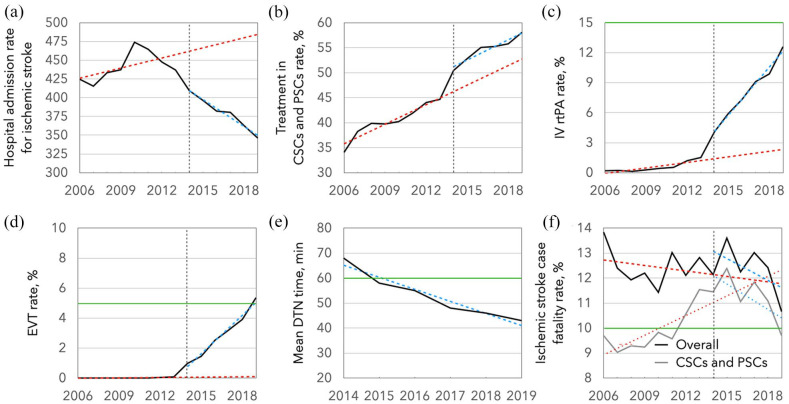
There was no significant AIS hospital admission rate trend during the pre-intervention period (see Supplemental Table 4). In contrast, it decreased significantly immediately after the intervention (regression coefficient ± standard error: β2 = –35.93 ± 15.72, p = 0.045), and continued to consistently decrease throughout the post-intervention period (β3 = –16.47 ± 3.95, p = 0.002) (Figure 3).
Figure 3.
Temporal trends in (a) ischemic stroke hospital admission rate per 100,000 population, (b) rate of patient treatment in comprehensive and primary stroke centers (CSCs and PSCs), (c) rate of thrombolysis using intravenous recombinant tissue plasminogen activator (IV rtPA), (d) endovascular treatment (EVT) rate, (e) post-intervention mean door-to-needle (DTN) time, and (f) case fatality from ischemic stroke. The dashed lines represent the regression lines. The green lines represent targets, where applicable. The comprehensive national stroke care policy in Lithuania was implemented in 2014 (vertical dashed line).
The proportion of cases in hospitals, designated as CSCs and PSCs in 2014, had a positive trend for an increase before the intervention (β1 = 1.31 ± 0.002, p < 0.001). Although there was a significant increase in the proportion of CSC and PSC cases immediately after the intervention (β2 = 4.95 ± 1.14, p = 0.001), we observed no significant trend change in the post-intervention period, as the proportion continued to increase to 58.1% in 2019.
Temporal trends in the proportion of AIS patients receiving RT
The proportion of AIS patients, treated with IV rtPA, out of all AIS cases increased from 1.5% (or 197 overall cases) in 2013 to 12.6% (or 1219 overall cases) in 2019 – a sixfold absolute and an eightfold relative increment. Similarly, there was an increase in the number of EVT performed from 10 cases or 0.1% out of all AIS in 2013 to 518 cases or 5.4% out of all AIS in 2019 (Figure 2). Only the proportion of patients treated with IV rtPA increased statistically significantly immediately after the implementation of a comprehensive national policy in Lithuania (β2 = 1.32 ± 0.38, p = 0.006), whereas, a significant change in trend in the period following it was observed for both the proportion of patients treated with IV rtPA (β3 = 1.42 ± 0.96, p < 0.001) and with EVT (β3 = 0.85 ± 0.05, p < 0.001).
In addition, there was a statistically significant decreasing trend in mean DTN time within the Lithuanian CSCs and PSCs since 2014, when it was started to be recorded (β1 = –5.28 ± 0.002, p < 0.001) (Figure 3), by almost 5 min on average annually from 68 min in 2014 to 43 min in 2019.
Temporal trends in case fatality rates for AIS patients
There were no significant changes in the overall all-cause in-hospital AIS case fatality rates during the pre- and post-intervention periods as well as immediately after the intervention. Nevertheless, the in-hospital AIS case fatality rates in CSCs and PSCs increased during the pre-intervention period (β1 = 0.26 ± 0.10, p = 0.024) and immediately following the intervention (β2 = 1.68 ± 0.73, p = 0.043), and decreased significantly during the post-intervention period (β3 = –0.60 ± 0.18, p = 0.008).
Discussion
In our interrupted time series design study on the impact of a comprehensive national policy on improving acute stroke patient care in Lithuania, we observed a significantly decreased AIS hospital admission rate, significant trend improvements in RT rates, and an immediate increase in the proportion of AIS cases treated in CSCs or PSCs after the policy change. In addition, there was a sustained significant decreasing trend of all-cause in-hospital case fatality rates within CSCs and PSCs despite a prompt initial immediate increase. To our knowledge, this is the first study from a very high CV RF region 23 demonstrating that comprehensive changes in national stroke care policy could be associated with substantial improvements in stroke care outcomes.
Lithuania has one of the highest AIS incidences in the world. 2 However, we suspect that a considerable part of the AIS diagnosed in the NHs could have been misdiagnosed cases of peripheral vertigo, 24 sequelae of previous strokes, and other diseases. 25 We speculate that as an increasing proportion of AIS cases have been treated in CSCs and PSCs, more patients received a correct AIS diagnosis. The gradual and significant decrease in the prevalence of CV RFs could have also played a role. 5 Although we assessed AIS hospital admission rather than AIS incidence rate, the actual difference between them may not be large as sudden death from stroke is very uncommon in the pre-hospital setting, 26 and every patient with AIS requires hospital admission by the current guidelines. 27 However, hospital admission rates for AIS in Lithuania in 2019 were still high despite an obvious downward trend from the highest stroke incidence worldwide in 2010.2,28
Ample previous studies have shown a continuous increase in IV rtPA26,29–46 and EVT rates for AIS46–48 in different countries over different study periods. However, our data show that Lithuania experienced a countrywide breakthrough of IV rtPA use only after the introduction of a comprehensive national policy. Similarly, EVT use was in single digits before the government intervention and surged after 2014, although some unmeasured confounders, such as the breakthrough thrombectomy trials in 2015 that increased physicians’ confidence in the safety and efficacy of EVT, might have also contributed. 48 Nevertheless, we believe that retrospective per-case AIS RT expense reimbursement and budget cap removal might have been a more robust incentive to improve RT numbers countrywide. While there is no agreed benchmark for thrombolysis and thrombectomy rates (these were respectively 12.6% and 5.4% in Lithuania in 2019), 10 there is still room for improvement as shown by remarkable nationwide IV tPA administration rates of 23.5% in the Czech Republic and a 5.6% EVT rate in Malta.45,49
Previous research has shown that the development of stroke centers could improve patient outcomes and result in a substantial increase in the proportion of AIS patients receiving IV rtPA.26,50,51 International guidelines recommend the certification of stroke centers by an independent external body, 52 and suggest that 90% or more of stroke patients should be treated in a stroke unit as the first level of care. 53 In our study despite the significant immediate level change, a non-significant slope change for the proportion of cases treated in CSCs or PSCs suggests a lack of effect of this government intervention over time. We contemplate that other types of interventions, such as centralization of AIS care requiring to bypass the NHs, or increase in stroke unit density within the country could have a higher impact on CSC/PSC treatment rate.
We found declining overall all-cause in-hospital stroke case fatality rates from 13.8% in 2006 to 10.7% in 2019 – comparable to those found in a similar study from neighboring Poland, where in-hospital case fatality rates declined from 13.6% in 2009 to 12.9% in 2013. 26 It was significantly lower in CSCs and PSCs with a sustained significant decreasing trend after the change of government policy. Still, AIS mortality was three times higher in Lithuania than the Organisation for Economic Co-operation and Development (OECD) average (145.08 vs 47.28 per 100,000 population, respectively).2,54
International guidelines recommend developing stroke systems of care so that RT-eligible patients receive treatment in the fastest achievable onset-to-treatment time. 52 We found a statistically significant decreasing trend in the mean DTN time within the Lithuanian hospitals from 68 min in 2014 to 43 min in 2019. We speculate that higher treatment volumes might lead to shorter DTN times – an indicator of experience and confidence.40,55,56 Moreover, quarterly SICMC reports to the MoH, and annual public stroke center progress monitoring may have produced an additional incentive. 27 Astonishingly, recent data from the Czech Republic showed that a national median DTN time of 25 min or less is feasible. 45
Our study has several limitations. First, the interrupted time series design is a quasi-experimental approach used to evaluate the impact of a single intervention, and unmeasured confounders (i.e. decreasing CV RF prevalence) may have affected the results. In addition, we did not investigate the influence of the coronavirus disease 2019 (COVID-19) pandemic on stroke care outcomes, as we have deliberately chosen to conduct our analysis on the pre-pandemic period. Moreover, the breakthrough thrombectomy trials in 2015 might have played a role in the increased thrombectomy rates throughout the country as there was an increase in confidence in the safety and efficacy of EVT among neurologists. 48 Fourth, functional and post-discharge long-term outcomes could not be assessed, due to limited access to such data. Fifth, our analysis is based on the group of hospitalized AIS cases, not overall AIS incidence, but the actual difference between these rates may not be large, since every patient with AIS requires hospital admission by the current guidelines. 27
The strengths of our study are that our nationwide analysis includes all Lithuanian AIS cases, which enables us to elucidate the overall country-wide real-world trends in acute stroke care outcomes. In addition, this is the first study from a very high cardiovascular risk region demonstrating that comprehensive changes in national stroke care policy could be associated with substantial improvements in stroke care outcomes.
Conclusion
We found that a comprehensive national stroke patient care policy in Lithuania was associated with an improvement in a wide array of quality measures both immediately after the intervention and in the period following it. This is the first study from a very high cardiovascular risk region demonstrating how integrated efforts of leading stroke specialists, government support, and a balanced stroke care network could be associated with a breakthrough of modern RTs for AIS patients. Further studies are warranted to elucidate how the use of RT and post-reperfusion functional outcomes change according to time and circumstances in real-world settings.
Supplemental Material
Supplemental material, sj-docx-1-eso-10.1177_23969873221089158 for The impact of a comprehensive national policy on improving acute stroke patient care in Lithuania by Rytis Masiliūnas, Aleksandras Vilionskis, Natan M Bornstein, Daiva Rastenytė and Dalius Jatužis in European Stroke Journal
Supplemental material, sj-docx-2-eso-10.1177_23969873221089158 for The impact of a comprehensive national policy on improving acute stroke patient care in Lithuania by Rytis Masiliūnas, Aleksandras Vilionskis, Natan M Bornstein, Daiva Rastenytė and Dalius Jatužis in European Stroke Journal
Supplemental material, sj-docx-3-eso-10.1177_23969873221089158 for The impact of a comprehensive national policy on improving acute stroke patient care in Lithuania by Rytis Masiliūnas, Aleksandras Vilionskis, Natan M Bornstein, Daiva Rastenytė and Dalius Jatužis in European Stroke Journal
Supplemental material, sj-docx-4-eso-10.1177_23969873221089158 for The impact of a comprehensive national policy on improving acute stroke patient care in Lithuania by Rytis Masiliūnas, Aleksandras Vilionskis, Natan M Bornstein, Daiva Rastenytė and Dalius Jatužis in European Stroke Journal
Acknowledgments
This article/publication is based upon work from IRENE COST Action – Implementation Research Network in Stroke Care Quality (CA18118), supported by COST (European Cooperation in Science and Technology; www.cost.eu). The authors would like to thank all stroke centers, physicians, nurses, CT technicians, coordinators, administrators, and civil servants for contributing to the effort to improve stroke care quality as well as for provision of data from stroke centers and the Institute of Hygiene.
Footnotes
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: RM, AV, and DJ have previously received honoraria payments and travel support from Boehringer-Ingelheim; RM, AV, DJ, and DR are members of Lithuanian Stroke Association. AV, DJ, and DR have been personally involved in the activities of SICMC.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Data have been obtained from an anonymized national public health register and official reports to the MoH from individual stroke-ready hospitals, therefore, there was no need for specific informed consent.
Ethical approval: Because the data have been collected from an anonymized national public health register and official aggregated reports from individual stroke-ready hospitals, approval of Ethics Committees for data collection was not required.
Guarantor: RM.
Author contributions: AV, DJ and DR researched literature and conceived the study. RM, AV and DJ were involved in protocol development and data collection. RM did the data analysis, visualized the data, and wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
ORCID iDs: Rytis Masiliūnas  https://orcid.org/0000-0002-8033-9682
https://orcid.org/0000-0002-8033-9682
Aleksandras Vilionskis  https://orcid.org/0000-0002-8055-3558
https://orcid.org/0000-0002-8055-3558
Supplemental material: Supplemental material for this article is available online.
References
- 1. Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396: 1204–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Feigin VL, Stark BA, Johnson CO, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 2021; 20: 795–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kim J, Thayabaranathan T, Donnan GA, et al. Global stroke statistics 2019. Int J Stroke 2020; 15: 819–838. [DOI] [PubMed] [Google Scholar]
- 4. Stevens E, Emmett E, Wang Y, et al. The burden of stroke in Europe. London: Stroke Alliance for Europe, 2017. [Google Scholar]
- 5. Laucevičius A, Rinkūnienė E, Petrulionienė Ž, et al. Trends in cardiovascular risk factor prevalence among Lithuanian middle-aged adults between 2009 and 2018. Atherosclerosis 2020; 299: 9–14. [DOI] [PubMed] [Google Scholar]
- 6. Wafa HA, Wolfe CDA, Emmett E, et al. Burden of stroke in Europe: Thirty-year projections of incidence, prevalence, deaths, and disability-adjusted life years. Stroke 2020; 51: 2418–2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bluhmki E, Chamorro A, Dávalos A, et al. Stroke treatment with alteplase given 3.0–4.5 h after onset of acute ischaemic stroke (ECASS III): additional outcomes and subgroup analysis of a randomised controlled trial. Lancet Neurol 2009; 8: 1095–1102. [DOI] [PubMed] [Google Scholar]
- 8. National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. New Engl J Med 1995; 333: 1581–1588. [DOI] [PubMed] [Google Scholar]
- 9. Messé SR, Khatri P, Reeves MJ, et al. Why are acute ischemic stroke patients not receiving IV tPA?: results from a national registry. Neurology 2016; 87: 1565–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Paul CL, Ryan A, Rose S, et al. How can we improve stroke thrombolysis rates? A review of health system factors and approaches associated with thrombolysis administration rates in acute stroke care. Implement Sci 2015; 11: 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gonzales S, Mullen MT, Skolarus L, et al. Progressive rural–urban disparity in acute stroke care. Neurology 2017; 88: 441–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stein L, Tuhrim S, Fifi J, et al. National trends in endovascular therapy for acute ischemic stroke: utilization and outcomes. J Neurointerv Surg 2020; 12: 356–362. [DOI] [PubMed] [Google Scholar]
- 13. Barkauskas EV, Bernotas G, Budrys V, et al. Galvos smegenų insulto diagnostikos, gydymo, profilaktikos ir reabilitacijos metodinės rekomendacijos. Neurologijos Seminarai 2007; 3(33): 197–224. [Google Scholar]
- 14. Ministry of Health of the Republic of Lithuania. Asmens sveikatos priežiūros paslaugų įtariant ar diagnozavus ūminį galvos smegenų insultą teikimo tvarkos aprašas [Internet], https://e-seimas.lrs.lt/portal/legalAct/lt/TAD/24591240ff0411e993cb8c8daaf8ff8a?jfwid=-kyrux7o2c (2014, accessed 25 October 2021).
- 15. Ministry of Health of the Republic of Lithuania. Dėl patologijų integruotos sveikatos priežiūros valdymo tarybos, kardiologijos, onkologijos, insulto ir perinatologijos. Integruotos sveikatos priežiūros valdymo komitetų sudarymo [Internet], https://www.hi.lt/uploads/pdf/darbo%20grupes/V-223.pdf (2014, accessed 25 October 2021).
- 16. Institute of Hygiene and Ministry of Health of The Republic of Lithuania. Stacionaro ligonių sudėtis pagal diagnozių grupes ir gydymo rūšis [Internet], https://stat.hi.lt/default.aspx?report_id=224 (2021, accessed 25 October 2021).
- 17. Institute of Hygiene. Statistinių tyrimų metodikos ir rodiklių aprašai. [Internet], https://www.hi.lt/lt/rodikliu_aprasai.html (2021, accessed 07 December 2021).
- 18. Ringelstein EB, Chamorro A, Kaste M, et al. European stroke organisation recommendations to establish a stroke unit and stroke center. Stroke 2013; 44: 828–840. [DOI] [PubMed] [Google Scholar]
- 19. Lindsay P, Furie KL, Davis SM, et al. World Stroke Organization global stroke services guidelines and action plan. Int J Stroke 2014; 9: 4–13. [DOI] [PubMed] [Google Scholar]
- 20. Gaidelytė R, Garbuvienė M, Pošienė A. Lietuvos gyventojų sveikata ir sveikatos priežiūros įstaigų veikla 2019 m [Internet]. Institute of Hygiene, Ministry of Health of The Republic of Lithuania, https://hi.lt/lt/lietuvos-gyventoju-sveikata-ir-sveikatos-prieziuros-istaigu-veikla-2013-m.html (2020, accessed 25 October 2021).
- 21. Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002; 27: 299–309. [DOI] [PubMed] [Google Scholar]
- 22. Kontopantelis E, Doran T, Springate DA, et al. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ 2015; 350: h2750–h2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 2021; 42: 3227–3337. [DOI] [PubMed] [Google Scholar]
- 24. Ulytė A, Valančius D, Masiliūnas R, et al. Diagnosis and treatment choices of suspected benign paroxysmal positional vertigo: current approach of general practitioners, neurologists, and ENT physicians. Eur Arch Otorhinolaryngol 2019; 276: 985–991. [DOI] [PubMed] [Google Scholar]
- 25. Melaika K, Sveikata L, Wiśniewski A, et al. Changes in prehospital stroke care and stroke mimic patterns during the COVID-19 lockdown. Int J Environ Res Public Health 2021; 18: 2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chwojnicki K, Ryglewicz D, Wojtyniak B, et al. Acute ischemic stroke hospital admissions, treatment, and outcomes in Poland in 2009–2013. Front Neurol 2018; 9: 134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jatužis D, Rastenytė D, Vilionskis A. Galvos smegenų insulto diagnostikos, gydymo, profilaktikos ir reabilitacijos metodika. Kaunas: Naujasis lankas, 2014. p.47. [Google Scholar]
- 28. Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 2014; 383: 245–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Maeda M, Fukuda H, Matsuo R, et al. Nationwide temporal trend analysis of reperfusion therapy utilization and mortality in acute ischemic stroke patients in Japan. Medicine 2021; 100: e24145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Eriksson M, Jonsson F, Appelros P, et al. Dissemination of thrombolysis for acute ischemic stroke across a nation: experiences from the Swedish stroke register, 2003 to 2008. Stroke 2010; 41: 1115–1122. [DOI] [PubMed] [Google Scholar]
- 31. Asplund K, Glader E-L, Norrving B, et al. Effects of extending the time window of thrombolysis to 4.5 hours: observations in the Swedish stroke register (Riks-Stroke). Stroke 2011; 42: 2492–2497. [DOI] [PubMed] [Google Scholar]
- 32. Stecksén A, Asplund K, Appelros P, et al. Thrombolytic therapy rates and stroke severity: an analysis of data from the Swedish stroke register (Riks-Stroke) 2007–2010. Stroke 2012; 43: 536–538. [DOI] [PubMed] [Google Scholar]
- 33. Domino JS, Baek J, Meurer WJ, et al. Emerging temporal trends in tissue plasminogen activator use: results from the BASIC project. Neurology 2016; 87: 2184–2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Schwamm LH, Ali SF, Reeves MJ, et al. Temporal trends in patient characteristics and treatment with intravenous thrombolysis among acute ischemic stroke patients at get with the guidelines-stroke hospitals. Circ Cardiovasc Qual Outcomes 2013; 6: 543–549. [DOI] [PubMed] [Google Scholar]
- 35. Messé SR, Fonarow GC, Smith EE, et al. Use of tissue-type plasminogen activator before and after publication of the European Cooperative Acute Stroke Study III in get with the guidelines-stroke. Circ Cardiovasc Qual Outcomes 2012; 5: 321–326. [DOI] [PubMed] [Google Scholar]
- 36. Minnerup J, Wersching H, Ringelstein EB, et al. Impact of the extended thrombolysis time window on the proportion of recombinant tissue-type plasminogen activator-treated stroke patients and on door-to-needle time. Stroke 2011; 42: 2838–2843. [DOI] [PubMed] [Google Scholar]
- 37. Scherf S, Limburg M, Wimmers R, et al. Increase in national intravenous thrombolysis rates for ischaemic stroke between 2005 and 2012: is bigger better? BMC Neurol 2016; 16: 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cheng T-J, Peng G-S, Jhao W-S, et al. Nationwide “hospital emergent capability accreditation by level-stroke” improves stroke treatment in Taiwan. J Stroke 2017; 19: 205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Jeong H-Y, Jung K-H, Mo H, et al. Characteristics and management of stroke in Korea: 2014–2018 data from Korean stroke registry. Int J Stroke 2020; 15: 619–626. [DOI] [PubMed] [Google Scholar]
- 40. Marko M, Posekany A, Szabo S, et al. Trends of r-tPA (recombinant tissue-type plasminogen activator) treatment and treatment-influencing factors in acute ischemic stroke. Stroke 2020; 51: 1240–1247. [DOI] [PubMed] [Google Scholar]
- 41. Miyamoto Y, Aso S, Iwagami M, et al. Expanded indication for recombinant tissue plasminogen activator from 3 to 4.5 h after onset of stroke in Japan. J Stroke Cerebrovasc Dis 2020; 29: 105341. [DOI] [PubMed] [Google Scholar]
- 42. Kurogi A, Nishimura A, Nishimura K, et al. Temporal trends and geographical disparities in comprehensive stroke centre capabilities in Japan from 2010 to 2018. BMJ Open 2020; 10: e033055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Singer OC, Hamann GF, Misselwitz B, et al. Time trends in systemic thrombolysis in a large hospital-based stroke registry. Cerebrovasc Dis 2012; 33: 316–321. [DOI] [PubMed] [Google Scholar]
- 44. Dequatre-Ponchelle N, Touzani H, Banh A, et al. Rate of intravenous thrombolysis for acute ischaemic stroke in the North-of-France region and evolution over time. J Neurol 2014; 261: 1320–1328. [DOI] [PubMed] [Google Scholar]
- 45. Mikulik R, Bar M, Cernik D, et al. Stroke 20 20: implementation goals for intravenous thrombolysis. Eur Stroke J 2021; 6: 151–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Anand SK, Benjamin WJ, Adapa AR, et al. Trends in acute ischemic stroke treatments and mortality in the United States from 2012 to 2018. Neurosurg Focus 2021; 51: E2. [DOI] [PubMed] [Google Scholar]
- 47. Smith EE, Saver JL, Cox M, et al. Increase in endovascular therapy in get with the guidelines-stroke after the publication of pivotal trials. Circulation 2017; 136: 2303–2310. [DOI] [PubMed] [Google Scholar]
- 48. Atchaneeyasakul K, Liaw N, Lee RH, et al. Patterns of mechanical thrombectomy for stroke before and after the 2015 pivotal trials and US national guideline update. J Stroke Cerebrovasc Dis 2020; 29: 105292. [DOI] [PubMed] [Google Scholar]
- 49. Aguiar de Sousa D, von Martial R, Abilleira S, et al. Access to and delivery of acute ischaemic stroke treatments: a survey of national scientific societies and stroke experts in 44 European countries. Eur Stroke J 2019; 4: 13–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lattimore SU, Chalela J, Davis L, et al. Impact of establishing a primary stroke center at a community hospital on the use of thrombolytic therapy: the NINDS suburban hospital stroke center experience. Stroke 2003; 34: e55–e57. [DOI] [PubMed] [Google Scholar]
- 51. Ganesh A, Lindsay P, Fang J, et al. Integrated systems of stroke care and reduction in 30-day mortality: a retrospective analysis. Neurology 2016; 86: 898–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2019; 50: e344–e418. [DOI] [PubMed] [Google Scholar]
- 53. Norrving B, Barrick J, Davalos A, et al. Action plan for stroke in Europe 2018–2030. Eur Stroke J 2018; 3: 309–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Global Burden of Disease Study 2019 (GBD 2019). Data resources [Internet]. Institute for Health Metrics and Evaluation, University of Washington, https://vizhub.healthdata.org/gbd-compare/ (2020, accessed 25 October 2021). [Google Scholar]
- 55. Bray BD, Campbell J, Cloud GC, et al. Bigger, Faster?: associations between hospital thrombolysis volume and speed of thrombolysis administration in acute ischemic stroke. Stroke 2013; 44: 3129–3135. [DOI] [PubMed] [Google Scholar]
- 56. Groot AE, van Schaik IN, Visser MC, et al. Association between i.v. Thrombolysis volume and door-to-needle times in acute ischemic stroke. J Neurol 2016; 263: 807–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-eso-10.1177_23969873221089158 for The impact of a comprehensive national policy on improving acute stroke patient care in Lithuania by Rytis Masiliūnas, Aleksandras Vilionskis, Natan M Bornstein, Daiva Rastenytė and Dalius Jatužis in European Stroke Journal
Supplemental material, sj-docx-2-eso-10.1177_23969873221089158 for The impact of a comprehensive national policy on improving acute stroke patient care in Lithuania by Rytis Masiliūnas, Aleksandras Vilionskis, Natan M Bornstein, Daiva Rastenytė and Dalius Jatužis in European Stroke Journal
Supplemental material, sj-docx-3-eso-10.1177_23969873221089158 for The impact of a comprehensive national policy on improving acute stroke patient care in Lithuania by Rytis Masiliūnas, Aleksandras Vilionskis, Natan M Bornstein, Daiva Rastenytė and Dalius Jatužis in European Stroke Journal
Supplemental material, sj-docx-4-eso-10.1177_23969873221089158 for The impact of a comprehensive national policy on improving acute stroke patient care in Lithuania by Rytis Masiliūnas, Aleksandras Vilionskis, Natan M Bornstein, Daiva Rastenytė and Dalius Jatužis in European Stroke Journal