Abstract
The kinematic alignment (KA) approach to total knee arthroplasty (TKA) has recently increased in popularity. Accordingly, a number of derivatives have arisen and have caused confusion. Clarification is therefore needed for a better understanding of KA-TKA. Calipered (or true, pure) KA is performed by cutting the bone parallel to the articular surface, compensating for cartilage wear. In soft-tissue respecting KA, the tibial cutting surface is decided parallel to the femoral cutting surface (or trial component) with in-line traction. These approaches are categorized as unrestricted KA because there is no consideration of leg alignment or component orientation. Restricted KA is an approach where the periarthritic joint surface is replicated within a safe range, due to concerns about extreme alignments that have been considered ‘alignment outliers’ in the neutral mechanical alignment approach. More recently, functional alignment and inverse kinematic alignment have been advocated, where bone cuts are made following intraoperative planning, using intraoperative measurements acquired with computer assistance to fulfill good coordination of soft-tissue balance and alignment. The KA-TKA approach aims to restore the patients’ own harmony of three knee elements (morphology, soft-tissue balance, and alignment) and eventually the patients’ own kinematics. The respective approaches start from different points corresponding to one of the elements, yet each aim for the same goal, although the existing implants and techniques have not yet perfectly fulfilled that goal.
Keywords: Knee, Treatment, Arthroplasty, Alignment, Soft-tissue, Mechanical, Kinematic, total knee arthroplasty (TKA), knees, kinematics, soft-tissue balancing, soft-tissue, tibial cutting, cartilage, tibial components, tibial bone, femur
Introduction
Total knee arthroplasty (TKA) has aimed to achieve neutral leg alignment: hip-knee-ankle angle (HKAA) of 0°, both femur and tibial components being perpendicular to the mechanical axes, and parallel and equal bony gaps in extension and flexion. This combination is known as mechanical alignment (MA) TKA. MA-TKA has acquired satisfactory long-term implant survival, accounting for 95% in national registries. 1-3 Nevertheless, 20% of patients after TKA have reported dissatisfaction, 25% of patients do not want to undergo the same operation again, and about 55% of patients have residual symptoms. 4-6 Improved materials, such as vitamin D-containing polyethene bearings, small intervals between component sizes, and sex-specific components, have been introduced with the aim of diminishing dissatisfaction, but there has been little evidence of improvement from the patient’s perspective. 7-9
Neutral leg alignment was shown to be rare in a recent study, even in healthy populations, and constitutional varus is prevalent. 10,11 Soft-tissue release for patients with constitutional varus alignment is therefore necessary to achieve neutral alignment in such patients (Figure 1). 12-14 Moreover, the joint line is not perpendicular to the MA but shows slightly varus obliquity at approximately 3°. 11 Eventually, joint line is inevitably altered, so it might be impossible to achieve perfect replication of the joint line and kinematics (Figure 2). Furthermore, MA-TKA aims to achieve equal and parallel gaps, regardless of the patient’s own soft-tissue balancing and alignment. This ‘one-size-fits-all’ concept of MA-TKA has recently been recognized as a systematic approach. 15-17 As a variation of the systematic approach, anatomical alignment was introduced by Hungerford et al, 18 where the components are implanted in 3° varus considering the joint line obliquity maintaining the leg alignment to be neutral. Due to the difficulty in making an accurate slanted bone cut, however, it has been largely disregarded. 19
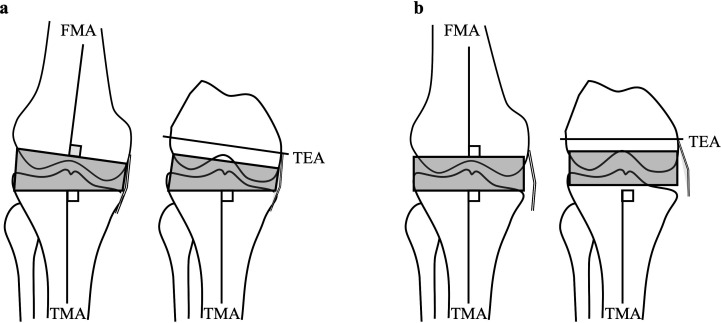
Fig. 1.
a) The mechanical bone cut. The cutting surface is perpendicular to the femoral and tibial mechanical axis (FMA and TMA) and parallel to the transepicondylar axis (TEA). b) Soft-tissue release. Leg alignment is not always neutral and constitutional varus is prevalent, so soft-tissue release is necessary to make the rectangular gap.
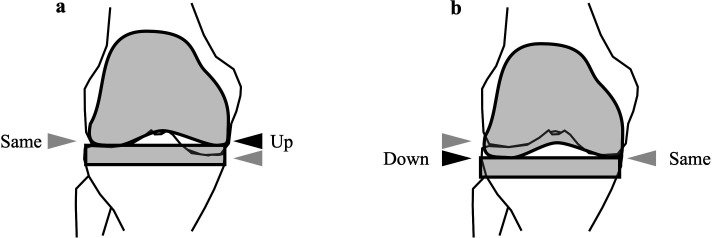
Fig. 2.
The joint line alteration in mechanically aligned total knee arthroplasty. a) As the joint line inclines medially, if the implant is set at the lateral joint line, the medial joint line becomes higher than the native joint line and b) vice versa (right).
A new approach was reported by Howell et al 20 in 2008 as custom-fit positioning TKA, where the component is set along the articular surface. Since then, the approach has developed to become known as kinematic-alignment (KA)-TKA. 21 Unlike the MA approach, the KA approach aims to reform the native (or pre-arthritic) joint line along the three kinematic axes. The goal is eventually different between patients, so it is considered to be a personalized, individualized, or patient-specific approach. 15,22,23 This approach has received a great deal of attention in recent years, and many surgeons have reported good short-term and medium-term clinical results. 24-28
With the spread of KA-TKA, several derivatives with different modifications have been proposed, which has led to some confusion. Therefore, this paper aims to clarify and classify the KA approach and its derivatives for clearer understanding.
Kinematic alignment approaches
In KA-TKA, components are set respecting three kinematic axes: the cylindrical axis (CA), or condylar axis, is the axis between the centres of the estimated circle of medial and lateral condyles. 22 The femur rotates around the CA. The patellar axis is parallel to the CA and located anterior and superior to it. Then, the patella rotates around the patellar axis. The tibial rotation axis locates medial to the centre of the knee, and the tibia locates axially around this axis, producing so-called medial pivot motion. As a result of the restoration of the three kinematic axes, the native articular surface, good soft-tissue balance, and similarity to native kinematics are expected to be restored. The term ‘kinematic’ was intended to express or highlight the implantation following the kinematics of these three axes, but currently many surgeons do not take these axes into account and instead aim to replicate the native joint surface.
Finding the native femoral articular surface
The first step of the KA approach is to restore the native articular surface of the femur by the use of components. The procedure is straightforward; the femoral condyle (distal and posterior) is cut at the same thickness as the component. On the affected condyle, bone resection is made 2 mm thinner than the component thickness, compensating for cartilage wear. Bone resections are made using mechanical instruments, 29,30 or computer-aided instruments. 25,31,32 However, the bone defects have not been considered in this approach and the thickness can vary between patients, the sides, and the site of the condyle. 33-36 More recently, the inversed KA technique has been advocated, in which the femoral cutting plane is decided based on the tibial cutting plane. 37
Tibial cutting concepts
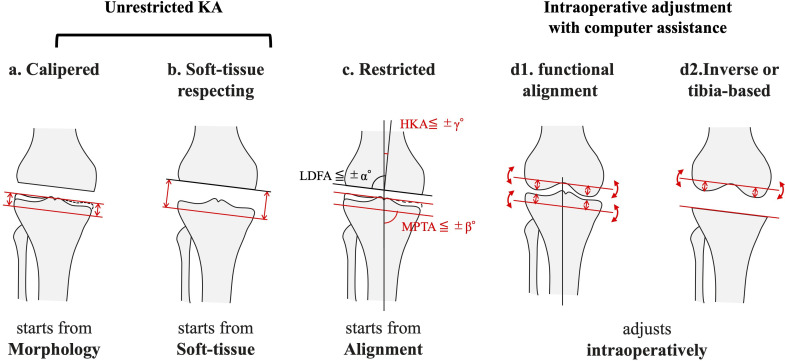
On the tibial side, various methods have been reported to replicate the native joint surface (Figure 3), and this has led to the development of various derivatives.
Fig. 3.
The variation of deciding the tibial cutting surface in the kinematic alignment total knee arthroplasties (KA-TKAs). a) Calipered (or pure, true) KA technique. The tibia is cut parallel to the tibial articular surface, compensating for the cartilage wear, similar to the femoral side. b) Soft-tissue respecting technique. The tibia is cut parallel to the femoral cutting surface under proper traction, parallel to the distal cutting surface of the femur in extension with respect to the trial component, and parallel to the posterior cutting surface of the femur in flexion. The calipered and soft-tissue respecting approaches are categorized as unrestricted KA. c) Restricted KA technique. A similar bone cut is done within the safe range (e.g. < 5° varus); otherwise, the resection is performed at a defined angle. Intraoperative adjustment with computer assistance: d1) Functional alignment. The tibial cutting surface along with the femoral cutting surface is decided based on the intraoperative information, including alignment and gap under computer assistance. d2). Inverse kinematic alignment or tibia-based KA. In this technique, the alignment of tibial component is decided first, followed by that of femoral component. Note that the femoral cutting line can be altered in these techniques. HKA, hip-knee-ankle angle; LDFA, lateral distal femoral angle; MPTA, medial proximal tibial angle.
Calipered technique
The calipered technique (Figure 3a) is an anatomical approach in which the bone cut is made parallel to the articular surface to compensate for the cartilage thickness to replicate the native coronal and sagittal slopes. 29,30,38 This approach is also known as ‘true KA’ 39 or ‘pure KA’. 40 The technique is straightforward and is facilitated using conventional mechanical instruments, 29,30 but there are several concerns. Firstly, the tibial cut is made based on tibial landmarks. Gap imbalance can therefore occur, although it is smaller than that in MA-TKA, 41 and a sophisticated rebalance protocol has been proposed. 30 Secondly, tibial bone defects affect the tibial cutting surface. If bone defects exist on the tibial side, the cutting surface can be more varus than the native surface, and estimating the bone defect is not easy. Intraoperative gap can be helpful for bone defect compensation. 22 The calipered technique is categorized as unrestricted KA-TKA, as neither whole-leg nor component alignment is considered to decide the cutting surface. There is increasing evidence of mid- to long-term survival, and improved clinical outcome and satisfaction, compared with MA-TKA. 24,27,28,42-45
Soft-tissue respecting technique
In the soft-tissue respecting technique (Figure 3b), the tibia is cut parallel to the femoral cutting plane or to the femoral component trial under appropriate in-line traction with the knee in full extension or a slight flexion. 46,47 Similarly, the Zimmer Biomet (USA) operation manual describes the tibial cutting technique in reference to the posterior cutting surface with the knee in 90° flexion. 48 These techniques are based on the assumption that if the components are implanted in the same alignment as the native articular surface, the soft-tissue balance becomes similar to the native pre-disease condition. There is concern, however, that the alignment is decided passively following the soft-tissue envelope, which can result in an extreme alignment. Moreover, soft-tissue abnormality, such as elongated lateral and/or contracted medial structure in medial OA knees, can be observed, 49,50 but the components can be implanted in an altered alignment in such cases. The soft-tissue respecting technique is also categorized as unrestricted KA-TKA because neither whole-leg alignment nor joint line obliquity is considered in deciding the bone cutting surface. Until now, there have been no reports regarding the long-term survival or clinical outcomes of this approach.
Restricted KA technique
The unrestricted technique can cause an extreme alignment that has been considered an outlier of MA-TKA. Although an increasing number of reports show that implant failure does not occur regardless of the alignment, 43 adopting the KA technique within a safe alignment range is attractive (Figure 3c). 41,51,52 Satisfactory clinical outcomes have been widely reported, 41,52-54 but the safe range for restriction has not been defined based on scientific evidence. Importantly, the restriction requires computer-assisted technology because it is essential to have precise control of bone cut alignment. Matsumoto et al 55 reported the modified kinematic alignment technique, where the tibial bone cut is made in 3° varus in every case. This approach is also considered to be a kind of restricted KA, but has been labelled as ‘pseudo KA’. 56 It seems reasonable for Asian patients, however, because constitutional varus alignment is common in Asians, and approximately 80% of Japanese knees eventually require restriction using restricted KA protocol. 57
Intraoperative adjustment with computer assistance techniques
Recent computer-assisted technologies, such as navigation and robotics, enable dynamic intraoperative planning based on intraoperative measurements, including alignment, soft-tissue laxity, and joint gaps acquired with computer-assistance (Figure 3d). 25,53,58,59 Further manipulation is possible if the gap balancing is unsatisfactory. Consequently, the component can be set in a well-balanced soft-tissue within the safe alignment. 19,37,59
The functional alignment (FA) introduced by Chang et al 59 is a typical computer-assisted surgery. In the FA technique, the intraoperative manipulation of the femoral and tibial components positions starting from the neutral MA is facilitated based on the intraoperative measurements.
More recently, the inverse kinematic alignment (iKA) technique has been introduced, whereby the tibial cut is made first to restore the periarthritic joint line, and the femoral cutting planes are then decided using intraoperative measurement; this has shown good short-term results. 37 A similar concept of technique is reported as tibia-based functional alignment with favourable results. 60 They are different from most KA approaches, where the femoral periarthritis articular surface is firstly restored prior to the tibial cut.
Is an extreme alignment safe?
Given that the native articular surface is provided and is an extreme alignment in terms of MA-TKA, there should be discussion on whether or not extreme alignment can be accepted. Several reports have shown that the malalignment of the femur, 61-63 tibia, 61,62,64,65 and HKAA 61-64 are associated with the increased failure rate, whereas other reports show no such association. 63,65-69 These results were based on MA-TKA, and so cannot be directly applied to KA-TKA. Regarding unrestricted KA, Howell et al reported six-year 42 and ten-year 43 survival rates of 97.5% (for all causes of revision) and 98.4% (for aseptic loosening) in a single-arm study. More recently, a comparison study of registry data from Australia and New Zealand revealed a cumulative revision rate of 3.1% with unrestricted KA and the rate of 3.0% for all other alignment methods. 44 Furthermore, a radiostereometric study revealed that there was no longitudinal migration between unrestricted KA and MA-TKA. 70 Furthermore, the forces in the medial and lateral compartments were similar in a cadaveric study between outlier and in-range alignment knees in unrestricted KA-TKA. 71 Similar results of intraoperative measurements were reported by Shelton et al, 38 who also reported similarity in the medial and lateral compartmental forces between outlier and in-range alignments. 72
However, most of these studies have been conducted in Western countries and constitutional varus has been reported to be more common in Asian countries. 73,74 Adapting the results to Asian patients should therefore be done with caution, and long-term results of unrestricted KA in Asian patients have not yet been reported. Similarly, patients with excessive alignment or obvious intra- or extra-articular deformities might be out of the range of the unrestricted KA. 22 The restricted KA might therefore be a safe and a promising procedure and there have been reports of satisfactory short-to-midterm clinical results. 17,75 Soft-tissue release is sometimes necessary, however, and it can induce a deterioration of the soft-tissue envelope and a dissimilar restoration of the kinematics. 76 Moreover, up to 3° to 5° for the femoral and tibial component orientations, and up to 3° for the whole leg angle, are used for the safe range. 51,52 There is no evidence, however, that these ranges are appropriate. Evidence-based definitions of the safe range along with long-term results require evaluation.
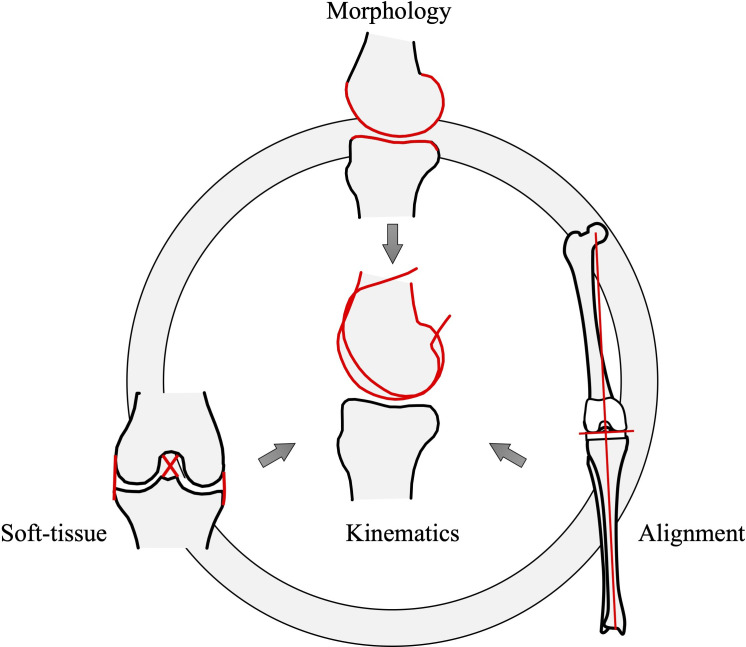
Three key elements
As described in the four-bar linkage model, 77 soft-tissue balancing decides the morphology of the epiphysis, and the morphology determines the alignment. Eventually, three key elements of the knee – morphology, soft-tissue balance, and alignment – form a unique harmony (Figure 4). Each element determines the others and is determined by the others, resulting in individualized kinematics 78 . If one of the three elements is altered from the native configuration, a complete or even satisfactory harmony will not be achieved. The harmony might differ between patients, so individualized goal setting instead of a systematic ‘one-size-fits-all goal’ would be necessary. Each derivative of KA-TKA starts from each element (the calipered KA from the morphology, the soft-tissue respecting KA from the soft-tissue balance, and restricted KA from the alignment and an intraoperative adjustment, stems from each of the three elements at the same time) and aims for the same goal: unique harmony and individual kinematics, with consideration of the other elements. The modern computer-assisted, intraoperative adjustable techniques aim to find the best harmony. However, complete replication of the joint surface and kinematics has not been achieved using current components. 79 An improved component that works well with the KA-TKA technique might be helpful. 22
Fig. 4.
Three fundamental knee elements; morphology, alignment, and soft-tissue. Each element determines and is determined by the other two elements, creating the best harmony on an individual basis. As a result of this harmony, the individualized kinematics are provided. The mechanical approach tends to change all, while the kinematic approach aims to reproduce all. However, the starting point is different among the respective kinematic alignment (KA) approaches. The calipered approach starts from ‘morphology’, focusing on replicating the original articular surface. The soft-tissue respecting approach starts from the soft-tissue balance, and the restricted approach starts from the control of the alignment. All other elements are expected to be eventually overcome and the patients’ original kinematics will be restored. The functional alignment, inverse KA, and other computer-assisted approaches adjust all elements based on intraoperative measurements.
What is ‘alignment’ in KA?
‘Kinematic alignment’ originally referred to the approach that aimed to follow three kinematic axes. More recently, it has evolved to mean recreation of the native articular surface by components, and it is used to refer to a contrast to the MA approach. Furthermore, the alignment seems to be considered as component alignment rather than in reference to the kinematic axes. 15,16 The means of finding the native joint line and whether the joint line can be accepted (unrestricted) or not (restricted or adjusted) remain matters of controversy. Future studies will gain evidence regarding these matters.
KA approaches aim to restore the patients’ best harmony of morphology, soft-tissue balance, alignment, and kinematics similar to that in pre-arthritic knees. All KA approaches aim for the same goal, but the starting point differs between approaches. The calipered approach starts from ‘morphology’, focusing on replicating the original articular surface, the soft-tissue respecting approach starts from the soft tissue balance, and the restricted approach starts with controlling the alignment. All other issues are expected to be eventually overcome and the patients’ original native kinematics might be restored, although the goal has not yet been achieved. ‘Kinematic’ might be used to indicate the goal of the approaches and ‘alignment’ might be considered a means of fulfilling the goal by component alignment. KA has gained in popularity, but there has been confusion about its exact meaning an implications.
KA-TKA aims to restore the patients’ individual harmony of three knee elements (morphology, soft-tissue balance, and alignment) and eventually replicate patients’ own kinematics. The respective approaches start from different points corresponding to one of the three elements, yet aiming for the same goal, although the existing implants and techniques have not yet perfectly fulfilled the goal.
Take home message
- Kinematically aligned total knee arthroplasty aims to restore the patients’ individual harmony of three knee elements (morphology, soft-tissue balance, and alignment) and eventually replicate the patient's own kinematics.
- The respective approaches start from different points corresponding to one of the three elements, yet aim for the same goal, although existing implants and techniques have not yet perfectly fulfilled the goal.
Acknowledgements
The authors thank Benjamin Phillis at the Clinical Study Support Center, Wakayama Medical University, for proofreading and editing.
Footnotes
Author contributions: T. Hiranaka: Conceptualization, Writing – original draft.
Y. Suda: Writing – review and editing.
A. Saitoh: Writing – review and editing.
A. Tanaka: Writing – review and editing.
A. Arimoto: Writing – review and editing.
M. Koide: Writing – review and editing.
T. Fujishiro: Writing – review and editing.
K. Okamoto: Writing – review and editing.
Funding statement: The authors received no financial or material support for the research, authorship, and/or publication of this article.
Open access funding: The open access fee for this study was self-funded.
Contributor Information
Takafumi Hiranaka, Email: takafumi.hiranaka@gmail.com.
Yoshihito Suda, Email: y.suda834@gmail.com.
Akira Saitoh, Email: akira.saitoh0315@gmail.com.
Atsuki Tanaka, Email: atsuki.tanaka1991@gmail.com.
Akihiko Arimoto, Email: ariponanb@yahoo.co.jp.
Motoki Koide, Email: kokokoide4712@yahoo.co.jp.
Takaaki Fujishiro, Email: taka2446@yg8.so-net.ne.jp.
Koji Okamoto, Email: okamoto.kouji@aijinkai-group.com.
References
- 1. No authors listed . NJR 17th Annual Report 2020. National Joint Registry. 2021. https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2017th%20Annual%20Report%202020.pdf (date last accessed 1 April 2022).
- 2. No authors listed . Australian Orthopaedic Association National Joint Replacement Registry 20th Annual Report 2020. Australian Orthopaedic Association National Joint Replacement Registry. 2020. https://aoanjrr.sahmri.com/documents/10180/668596/Hip%2C+Knee+%26+Shoulder+Arthroplasty/c287d2a3-22df-a3bb-37a2-91e6c00bfcf0 (date last accessed 1 April 2022).
- 3. No authors listed . The New Zealand Joint Registry twenty-one year report January 1999 to December 2019. New Zealand Orthopaedic Association. 2020. https://nzoa.org.nz/sites/default/files/DH8426_NZJR_2020_Report_v5_30Sep.pdf (date last accessed 1 April 2022).
- 4. Lingard EA, Sledge CB, Learmonth ID, Kinemax Outcomes Group . Patient expectations regarding total knee arthroplasty: differences among the United States, United Kingdom, and Australia. J Bone Joint Surg Am. 2006;88-A(6):1201–1207. 10.2106/JBJS.E.00147 [DOI] [PubMed] [Google Scholar]
- 5. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. 10.1007/s11999-009-1119-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nam D, Nunley RM, Barrack RL. Patient dissatisfaction following total knee replacement: a growing concern? Bone Joint J. 2014;96-B(11 Supple A):96–100. 10.1302/0301-620X.96B11.34152 [DOI] [PubMed] [Google Scholar]
- 7. Spece H, Schachtner JT, MacDonald DW, et al. . Reasons for revision, oxidation, and damage mechanisms of retrieved vitamin e-stabilized highly crosslinked polyethylene in total knee arthroplasty. J Arthroplasty. 2019;34(12):3088–3093. 10.1016/j.arth.2019.07.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Flament EM, Berend KR, Hurst JM, Morris MJ, Adams JB, Lombardi AV. Early experience with vitamin E antioxidant-infused highly cross-linked polyethylene inserts in primary total knee arthroplasty. Surg Technol Int. 2016;29:334–340. [PubMed] [Google Scholar]
- 9. Sappey-Marinier E, Swan J, Batailler C, Servien E, Lustig S. No clinical benefit from gender-specific total knee replacement implants: a systematic review. SICOT J. 2020;6:25. 10.1051/sicotj/2020023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res. 2012;470(1):45–53. 10.1007/s11999-011-1936-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thienpont E, Schwab PE, Cornu O, Bellemans J, Victor J. Bone morphotypes of the varus and valgus knee. Arch Orthop Trauma Surg. 2017;137(3):393–400. 10.1007/s00402-017-2626-x [DOI] [PubMed] [Google Scholar]
- 12. Athwal KK, Daou HE, Kittl C, Davies AJ, Deehan DJ, Amis AA. The superficial medial collateral ligament is the primary medial restraint to knee laxity after cruciate-retaining or posterior-stabilised total knee arthroplasty: effects of implant type and partial release. Knee Surg Sports Traumatol Arthrosc. 2016;24(8):2646–2655. 10.1007/s00167-015-3796-0 [DOI] [PubMed] [Google Scholar]
- 13. Rivière C, Vigdorchik JM, Vendittoli P-A. Mechanical alignment: The end of an era! Orthop Traumatol Surg Res. 2019;105(7):1223–1226. 10.1016/j.otsr.2019.07.005 [DOI] [PubMed] [Google Scholar]
- 14. Springer BD, Parratte S, Abdel MP. Measured resection versus gap balancing for total knee arthroplasty. Clin Orthop Relat Res. 2014;472(7):2016–2022. 10.1007/s11999-014-3524-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rivière C, Lazic S, Boughton O, Wiart Y, Vïllet L, Cobb J. Current concepts for aligning knee implants: patient-specific or systematic? EFORT Open Rev. 2018;3(1):1–6. 10.1302/2058-5241.3.170021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rivière C, Villet L, Jeremic D, Vendittoli P-A. What you need to know about kinematic alignment for total knee arthroplasty. Orthop Traumatol Surg Res. 2021;107(1S):102773. 10.1016/j.otsr.2020.102773 [DOI] [PubMed] [Google Scholar]
- 17. Laforest G, Kostretzis L, Kiss M-O, Vendittoli P-A. Restricted kinematic alignment leads to uncompromised osseointegration of cementless total knee arthroplasty. Internet. Knee Surg Sports Traumatol Arthrosc. 2021;30(2):705–712. 10.1007/s00167-020-06427-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hungerford DS, Krackow KA. Total joint arthroplasty of the knee. Clin Orthop Relat Res. 1985;192:23–33. 10.1097/00003086-198501000-00004 [DOI] [PubMed] [Google Scholar]
- 19. Begum FA, Kayani B, Magan AA, Chang JS, Haddad FS. Current concepts in total knee arthroplasty. Bone Jt Open. 2021;2(6):397–404. 10.1302/2633-1462.26.BJO-2020-0162.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Howell SM, Kuznik K, Hull ML, Siston RA. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics. 2008;31(9):857–863. 10.3928/01477447-20080901-15 [DOI] [PubMed] [Google Scholar]
- 21. Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res. 2013;471(3):1000–1007. 10.1007/s11999-012-2613-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rivière C, Harman C, Boughton O, Cobb J. The kinematic alignment technique for total knee arthroplasty. In: Rivière C, Vendittoli P-A. Personalized Hip and Knee Joint Replacement. Cham, Switzerland: Springer, 2020. [PubMed] [Google Scholar]
- 23. Lustig S, Sappey-Marinier E, Fary C, Servien E, Parratte S, Batailler C. Personalized alignment in total knee arthroplasty: current concepts. SICOT J. 2021;7:19. 10.1051/sicotj/2021021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG. A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J. 2014;96-B(7):907–913. 10.1302/0301-620X.96B7.32812 [DOI] [PubMed] [Google Scholar]
- 25. Hutt JRB, LeBlanc MA, Massé V, Lavigne M, Vendittoli PA. Kinematic TKA using navigation: Surgical technique and initial results. Orthop Traumatol Surg Res. 2016;102(1):99–104. 10.1016/j.otsr.2015.11.010 [DOI] [PubMed] [Google Scholar]
- 26. Matsumoto T, Takayama K, Ishida K, Hayashi S, Hashimoto S, Kuroda R. Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Joint J. 2017;99-B(5):640–646. 10.1302/0301-620X.99B5.BJJ-2016-0688.R2 [DOI] [PubMed] [Google Scholar]
- 27. McEwen PJ, Dlaska CE, Jovanovic IA, Doma K, Brandon BJ. Computer-assisted kinematic and mechanical axis total knee arthroplasty: A prospective randomized controlled trial of bilateral simultaneous surgery. J Arthroplasty. 2020;35(2):443–450. 10.1016/j.arth.2019.08.064 [DOI] [PubMed] [Google Scholar]
- 28. Shelton TJ, Gill M, Athwal G, Howell SM, Hull ML. Outcomes in patients with a calipered kinematically aligned TKA that already had a contralateral mechanically aligned TKA. J Knee Surg. 2021;34(1):87–93. 10.1055/s-0039-1693000 [DOI] [PubMed] [Google Scholar]
- 29. Howell SM. Calipered kinematically aligned total knee arthroplasty: An accurate technique that improves patient outcomes and implant survival. Orthopedics. 2019;42(3):126–135. 10.3928/01477447-20190424-02 [DOI] [PubMed] [Google Scholar]
- 30. Nedopil AJ, Howell SM, Hull ML. Kinematically aligned total knee arthroplasty using calipered measurements, manual instruments, and verification checks. In: Rivière C, Vendittoli P-A. Personalized Hip and Knee Joint Replacement. Cham, Switzerland: Springer, 2020: 279–300. [PubMed] [Google Scholar]
- 31. Woon JTK, Zeng ISL, Calliess T, et al. . Outcome of kinematic alignment using patient-specific instrumentation versus mechanical alignment in TKA: a meta-analysis and subgroup analysis of randomised trials. Arch Orthop Trauma Surg. 2018;138(9):1293–1303. 10.1007/s00402-018-2988-8 [DOI] [PubMed] [Google Scholar]
- 32. Kim KK, Howell SM, Won YY. Kinematically aligned total knee arthroplasty with patient-specific instrument. Yonsei Med J. 2020;61(3):201–209. 10.3349/ymj.2020.61.3.201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Koo S, Gold GE, Andriacchi TP. Considerations in measuring cartilage thickness using MRI: factors influencing reproducibility and accuracy. Osteoarthritis Cartilage. 2005;13(9):782–789. 10.1016/j.joca.2005.04.013 [DOI] [PubMed] [Google Scholar]
- 34. Eckstein F, Cicuttini F, Raynauld J-P, Waterton JC, Peterfy C. Magnetic resonance imaging (MRI) of articular cartilage in knee osteoarthritis (OA): morphological assessment. Osteoarthritis Cartilage. 2006;14 Suppl A:A46-75. 10.1016/j.joca.2006.02.026 [DOI] [PubMed] [Google Scholar]
- 35. Yoon C-H, Kim H-S, Ju JH, Jee W-H, Park S-H, Kim H-Y. Validity of the sonographic longitudinal sagittal image for assessment of the cartilage thickness in the knee osteoarthritis. Clin Rheumatol. 2008;27(12):1507–1516. 10.1007/s10067-008-0956-3 [DOI] [PubMed] [Google Scholar]
- 36. Schmitz RJ, Wang H-M, Polprasert DR, Kraft RA, Pietrosimone BG. Evaluation of knee cartilage thickness: A comparison between ultrasound and magnetic resonance imaging methods. Knee. 2017;24(2):217–223. 10.1016/j.knee.2016.10.004 [DOI] [PubMed] [Google Scholar]
- 37. Winnock de Grave P, Luyckx T, Claeys K, et al. . Higher satisfaction after total knee arthroplasty using restricted inverse kinematic alignment compared to adjusted mechanical alignment. Knee Surg Sports Traumatol Arthrosc. 2022;30(2):488–499. 10.1007/s00167-020-06165-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Shelton TJ, Howell SM, Hull ML. Is there a force target that predicts early patient-reported outcomes after kinematically aligned TKA? Clin Orthop Relat Res. 2019;477(5):1200–1207. 10.1097/CORR.0000000000000600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Huber K, Christen B, Calliess S, Calliess T. True kinematic alignment is applicable in 44% of patients applying restrictive indication criteria-a retrospective analysis of 111 TKA using robotic assistance. J Pers Med. 2021;11(7):662. 10.3390/jpm11070662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Malavolta M, Kley K. Kinematic alignment-management of deformities and flexion contractures. Orthopade. 2021;50(3):173–178. 10.1007/s00132-020-03970-0 [DOI] [PubMed] [Google Scholar]
- 41. Blakeney W, Beaulieu Y, Kiss M-O, Rivière C, Vendittoli P-A. Less gap imbalance with restricted kinematic alignment than with mechanically aligned total knee arthroplasty: simulations on 3-D bone models created from CT-scans. Acta Orthop. 2019;90(6):602–609. 10.1080/17453674.2019.1675126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Howell SM, Papadopoulos S, Kuznik K, Ghaly LR, Hull ML. Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop. 2015;39(11):2117–2124. 10.1007/s00264-015-2743-5 [DOI] [PubMed] [Google Scholar]
- 43. Howell SM, Shelton TJ, Hull ML. Implant survival and function ten years after kinematically aligned total knee arthroplasty. J Arthroplasty. 2018;33(12):3678–3684. 10.1016/j.arth.2018.07.020 [DOI] [PubMed] [Google Scholar]
- 44. Klasan A, de Steiger R, Holland S, Hatton A, Vertullo CJ, Young SW. Similar risk of revision after kinematically aligned, patient-specific instrumented total knee arthroplasty, and all other total knee arthroplasty: combined results from the Australian and New Zealand joint replacement registries. J Arthroplasty. 2020;35(10):2872–2877. 10.1016/j.arth.2020.05.065 [DOI] [PubMed] [Google Scholar]
- 45. Howell SM, Gill M, Shelton TJ, Nedopil AJ. Reoperations are few and confined to the most valgus phenotypes 4 years after unrestricted calipered kinematically aligned TKA. Knee Surg Sports Traumatol Arthrosc. 2021. 10.1007/s00167-021-06473-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. H M Brown J. Traction during total knee arthroplasty leads to a bone-conserving tibial resection: a retrospective comparative study. International Journal of Orthopaedics. 2020;7(3):1283–1288. 10.17554/j.issn.2311-5106.2020.07.345 [DOI] [Google Scholar]
- 47. Soda Y, Nakamura M, Adachi N. Coronal alignment of three different types of implants in kinematically aligned total knee arthroplasty: a comparative study. OJO. 2021;11(06):183–198. 10.4236/ojo.2021.116018 [DOI] [Google Scholar]
- 48. No authors listed . Persona Kinematically Aligned Total Knee Arthroplasty: Surgical Technique. ZimmerBiomet. 2019. https://www.zimmerbiomet.com/content/dam/zimmer-biomet/medical-professionals/000-surgical-techniques/knee/1578.1-GLBL-en%20Persona%20Kinematically%20Aligned%20TKA%20SurgTech-v3-Final.pdf (date last accessed 1 April 2022).
- 49. Fishkin Z, Miller D, Ritter C, Ziv I. Changes in human knee ligament stiffness secondary to osteoarthritis. J Orthop Res. 2002;20(2):204–207. 10.1016/S0736-0266(01)00087-0 [DOI] [PubMed] [Google Scholar]
- 50. Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Iwamoto Y. Lateral soft tissue laxity increases but medial laxity does not contract with varus deformity in total knee arthroplasty. Clin Orthop Relat Res. 2013;471(4):1334–1342. 10.1007/s11999-012-2745-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Almaawi AM, Hutt JRB, Masse V, Lavigne M, Vendittoli PA. The impact of mechanical and restricted kinematic alignment on knee anatomy in total knee arthroplasty. J Arthroplasty. 2017;32(7):2133–2140. 10.1016/j.arth.2017.02.028 [DOI] [PubMed] [Google Scholar]
- 52. MacDessi SJ, Griffiths-Jones W, Chen DB, et al. . Restoring the constitutional alignment with a restrictive kinematic protocol improves quantitative soft-tissue balance in total knee arthroplasty: A randomized controlled trial. Bone Joint J. 2020;102-B(1):117–124. 10.1302/0301-620X.102B1.BJJ-2019-0674.R2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Clement ND, Calliess T, Christen B, Deehan DJ. An alternative technique of restricted kinematic alignment of the femur and gap balanced alignment of the tibia using computer aided navigation. Bone Joint Res. 2020;9(6):282–284. 10.1302/2046-3758.96.BJR-2020-0119.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Abhari S, Hsing TM, Malkani MM, et al. . Patient satisfaction following total knee arthroplasty using restricted kinematic alignment. Bone Joint J. 2021;103-B(6 Supple A):59–66. 10.1302/0301-620X.103B6.BJJ-2020-2357.R1 [DOI] [PubMed] [Google Scholar]
- 55. Matsumoto T, Takayama K, Ishida K, et al. . Intraoperative soft tissue balance/kinematics and clinical evaluation of modified kinematically versus mechanically aligned total knee arthroplasty. J Knee Surg. 2020;33(8):777–784. 10.1055/s-0039-1688504 [DOI] [PubMed] [Google Scholar]
- 56. Nisar S, Palan J, Rivière C, Emerton M, Pandit H. Kinematic alignment in total knee arthroplasty. EFORT Open Rev. 2020;5(7):380–390. 10.1302/2058-5241.5.200010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Suda Y, Hiranaka T, Kamenaga T, et al. . Approximately 80% of Japanese osteoarthritic patients fall out of the safety range in restricted kinematically-aligned total knee arthroplasty in an analysis of preoperative long-leg radiograms. Knee. 2022;35:54–60. 10.1016/j.knee.2022.02.008 [DOI] [PubMed] [Google Scholar]
- 58. Hutt J, Massé V, Lavigne M, Vendittoli PA. Functional joint line obliquity after kinematic total knee arthroplasty. Int Orthop. 2016;40(1):29–34. 10.1007/s00264-015-2733-7 [DOI] [PubMed] [Google Scholar]
- 59. Chang JS, Kayani B, Wallace C, Haddad FS. Functional alignment achieves soft-tissue balance in total knee arthroplasty as measured with quantitative sensor-guided technology. Bone Joint J. 2021;103-B(3):507–514. 10.1302/0301-620X.103B.BJJ-2020-0940.R1 [DOI] [PubMed] [Google Scholar]
- 60. Zambianchi F, Bazzan G, Marcovigi A, et al. . Joint line is restored in robotic-arm-assisted total knee arthroplasty performed with a tibia-based functional alignment. Arch Orthop Trauma Surg. 2021;141(12):2175–2184. 10.1007/s00402-021-04039-z [DOI] [PubMed] [Google Scholar]
- 61. Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am. 2011;93-A(17):1588–1596. 10.2106/JBJS.J.00772 [DOI] [PubMed] [Google Scholar]
- 62. Kim Y-H, Park J-W, Kim J-S, Park S-D. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop. 2014;38(2):379–385. 10.1007/s00264-013-2097-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Lee BS, Cho HI, Bin SI, Kim JM, Jo BK. Femoral component varus malposition is associated with tibial aseptic loosening after TKA. Clin Orthop Relat Res. 2018;476(2):400–407. 10.1007/s11999.0000000000000012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Arsoy D, Pagnano MW, Lewallen DG, Hanssen AD, Sierra RJ. Aseptic tibial debonding as a cause of early failure in a modern total knee arthroplasty design. Clin Orthop Relat Res. 2013;471(1):94–101. 10.1007/s11999-012-2467-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Karas V, Calkins TE, Bryan AJ, et al. . Total knee arthroplasty in patients less than 50 years of age: results at a mean of 13 years. J Arthroplasty. 2019;34(10):2392–2397. 10.1016/j.arth.2019.05.018 [DOI] [PubMed] [Google Scholar]
- 66. Hooper G, Rothwell A, Frampton C. The low contact stress mobile-bearing total knee replacement: a prospective study with a minimum follow-up of ten years. J Bone Joint Surg Br. 2009;91-B(1):58–63. 10.1302/0301-620X.91B1.20484 [DOI] [PubMed] [Google Scholar]
- 67. Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92-A(12):2143–2149. 10.2106/JBJS.I.01398 [DOI] [PubMed] [Google Scholar]
- 68. Matziolis G, Adam J, Perka C. Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg. 2010;130(12):1487–1491. 10.1007/s00402-010-1064-9 [DOI] [PubMed] [Google Scholar]
- 69. Abdel MP, Ollivier M, Parratte S, Trousdale RT, Berry DJ, Pagnano MW. Effect of postoperative mechanical axis alignment on survival and functional outcomes of modern total knee arthroplasties with cement: a concise follow-up at 20 years. J Bone Joint Surg Am. 2018;100-A(6):472–478. 10.2106/JBJS.16.01587 [DOI] [PubMed] [Google Scholar]
- 70. Laende EK, Richardson CG, Dunbar MJ. A randomized controlled trial of tibial component migration with kinematic alignment using patient-specific instrumentation versus mechanical alignment using computer-assisted surgery in total knee arthroplasty. Bone Joint J. 2019;101-B(8):929–940. 10.1302/0301-620X.101B8.BJJ-2018-0755.R3 [DOI] [PubMed] [Google Scholar]
- 71. Roth JD, Howell SM, Hull ML. Kinematically aligned total knee arthroplasty limits high tibial forces, differences in tibial forces between compartments, and abnormal tibial contact kinematics during passive flexion. Knee Surg Sports Traumatol Arthrosc. 2018;26(6):1589–1601. 10.1007/s00167-017-4670-z [DOI] [PubMed] [Google Scholar]
- 72. Shelton TJ, Nedopil AJ, Howell SM, Hull ML. Do varus or valgus outliers have higher forces in the medial or lateral compartments than those which are in-range after a kinematically aligned total knee arthroplasty? Limb and joint line alignment after kinematically aligned total knee arthroplasty. Bone Joint J. 2017;99-B(10):1319–1328. 10.1302/0301-620X.99B10.BJJ-2017-0066.R1 [DOI] [PubMed] [Google Scholar]
- 73. Hovinga KR, Lerner AL. Anatomic variations between Japanese and Caucasian populations in the healthy young adult knee joint. J Orthop Res. 2009;27(9):1191–1196. 10.1002/jor.20858 [DOI] [PubMed] [Google Scholar]
- 74. Tang Q, Zhou Y, Yang D, Xu H, Liu Q. The offset of the tibial shaft from the tibial plateau in Chinese people. J Bone Joint Surg Am. 2010;92-A(10):1981–1987. 10.2106/JBJS.I.00969 [DOI] [PubMed] [Google Scholar]
- 75. Vendittoli P-A, Martinov S, Blakeney WG. Restricted kinematic alignment, the fundamentals, and clinical applications. Front Surg. 2021;8:697020. 10.3389/fsurg.2021.697020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Hunt NC, Ghosh KM, Athwal KK, Longstaff LM, Amis AA, Deehan DJ. Lack of evidence to support present medial release methods in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22(12):3100–3112. 10.1007/s00167-014-3148-5 [DOI] [PubMed] [Google Scholar]
- 77. Muller M. The angles of femoral and tibial axes with respect to the cruciate ligament four-bar system in the knee joint. J Theor Biol. 1993;161(2):221–230. 10.1006/jtbi.1993.1051 [DOI] [PubMed] [Google Scholar]
- 78. Hiranaka T, Suda Y, Saitoh A, et al. . Infographic: Three key elements of kinematic alignment total knee arthroplasty for clarified understanding of its approaches. Bone Joint Res. 2022;226–228. 10.1302/2046-3758.114.BJR-2021-0543.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Rivière C, Dhaif F, Shah H, et al. . Kinematic alignment of current TKA implants does not restore the native trochlear anatomy. Orthop Traumatol Surg Res. 2018;104(7):983–995. 10.1016/j.otsr.2018.05.010 [DOI] [PubMed] [Google Scholar]