Abstract
After the Vietnam War, 1.3 million Vietnamese migrated to the U.S. where they are the fourth largest Asian American subgroup. However, little is known about their health compared to other Asian subgroups. As such, we developed the Vietnamese Aging and Care Survey to understand older Vietnamese immigrants’ health in Houston, Texas (N=132). We examined how social support moderated the relationship between their physical disability and mental health (depressive symptoms and loneliness). Most respondents rated their health as fair/poor and more than half lived in extended family households or senior housing in ethnic enclaves. Having more physical disabilities was associated with higher depressive symptoms and loneliness, but higher social support moderated the effect of physical disability on loneliness. Local policymakers and stakeholders might strategize using the existing culturally and linguistically appropriate daycare centers and home and community-based services to mitigate depression and loneliness among older Vietnamese immigrants with physical disabilities.
Keywords: Vietnamese, Immigrants, Social support, Depressive symptoms, Loneliness, Physical disabilities
Introduction
After the end of the Vietnam War in 1975, many Vietnamese immigrants mostly as refugees migrated to the United States (U.S.) where their current population is over 2.2 million.1 Having been exposed to wartime physical and emotional violence, their traumatic escape and relocation to U.S. cities, and their distrust of government, older Vietnamese immigrants are a vulnerable population.2,3 Vietnamese are the fourth largest Asian American subgroup and one of the fastest growing immigrant populations in the U.S.4 However, research on the health of this population is limited compared to other racial/ethnic minorities or other large Asian American groups such as Chinese.5 Vietnamese are rather new immigrants compared to those who have established immigrants such as Chinese and Japanese because their immigration history just started around 1975. They also have a unique immigration history because they not only arrived in the U.S. as refugees with some having spent time in prison or reeducation camp in Vietnam but also with some rejoining family members already in the U.S.6 Those who immigrated to the U.S. around 1975 as middle-aged adults are now older and many have significant physical and mental health problems such as chronic health conditions, post-traumatic stress disorder (PTSD), and depression.7 Many experienced significant physical and mental trauma which may have taken its toll on their health and mental health in their older years. In addition, Vietnamese Americans have not only the lowest socioeconomic and education level among Asian Americans but they also have a low rate of health insurance coverage which compound their health status in their older years.8,9
Vietnamese Americans are susceptible to many most common chronic diseases such as cancer, heart disease stroke, hypertension, and diabetes,10 and older Vietnamese Americans have been found to have the highest Activities of Daily Living (ADL) disability rates among all Asian American populations.5,11–13 Being of female gender, unmarried, having low income with limited education, and immigrating in late life are some of the known factors associated with increased likelihood of poor physical health.14 In addition to low insurance coverage, linguistic and cultural barriers further compromise their access to much needed health care.10,15
Many Asian Americans with mental health problems do not seek professional help due to stigmas associated with mental health problems.7 For example, in the traditional Vietnamese culture, people with mental illnesses such as depression and PTSD are often considered to be crazy, weak, and a curse to the family and ancestors.16–18 Disclosing and sharing your personal problems with individuals outside of the family (i.e., mental health professionals) is not a common practice among Asian Americans.17 However, the prevalence rates of depression among Vietnamese Americans, especially older Vietnamese immigrants have been consistently reported to be high.17,19,20 This is understandable because of their socioeconomic status, linguistic and cultural barriers, as well as different lifestyle in a new host country.
Another common mental health issue in older adults is loneliness. Loneliness is a negative feeling of being alone that occurs irrespective of choice to be alone.21 The experience of loneliness has been associated with older age, female gender, being unmarried, and lower socioeconomic status.22,23 Loneliness has been associated with detrimental physical, mental, and cognitive health in the lives of older adults across different racial/ethnic groups.21,24 Although loneliness has been a public health concern for a while, studies on loneliness in Asian communities have been limited to older Chinese and Korean immigrants.20,25
Many Asian older adults expect to preserve their traditional, collectivistic, family-oriented culture, including the expectation to be cared for by their children during their older years even in a foreign county. However, the reality is often in conflict with such expectations.26 For example, Park and colleagues (2018)20 found that older Chinese and Korean late-life migrants lived either alone or only with their spouses. They tended to experience isolation and loneliness in the host country because, although they wish to connect with their adult children and their families as often as possible, due to the adult children’s work circumstances, they tried not to be a burden to their adult children and maintain a minimum contact. Weng’s study (2019)27 with Asian older immigrants has shared the same sentiments indicating that by depending solely on their adult children and migrating late in life, they lost all the networks and peer relationships that they had established in their home country. Thus, re-establishing the intergenerational relationships is vital to alleviate the loneliness of aging parents.27
Social support is generally defined as reciprocal, accessible, and reliable social relationships that provide needed resources and help with stressors.28 Older adults, especially late-life immigrants, often count on social support from various sources such as family, neighbors, community services, and religious organizations29 and social support has been shown to protect older Asian Americans from negative social stressors.30 Having gone through many traumatic events and experiences, older Vietnamese immigrants are vulnerable to social stressors and are in need of social support from their children and other family members. Given that Vietnamese older adults have the highest disability rates compared to other racial/ethnic groups, social support may play a moderating role between disability and mental health in this population. Except for few older articles (e.g., Gellis, Tran & Wright, Jr.),31,32 the investigation on social support among the Vietnamese population has rarely been explored. The reason could be that compared to other Asian Americans (e.g., Chinese, Japanese), Vietnamese are a more recent immigrant group with a great deal of variation in immigration experiences, with only 35% of them having English language proficiency, 34% living in multigeneration households,1 and only 21% having basic health literacy.33 These characteristics in addition to the limited research about the physical health and mental conditions of Vietnamese older adults emphasize the importance and need of a better understanding of this population, and how social support may facilitate their well-being.
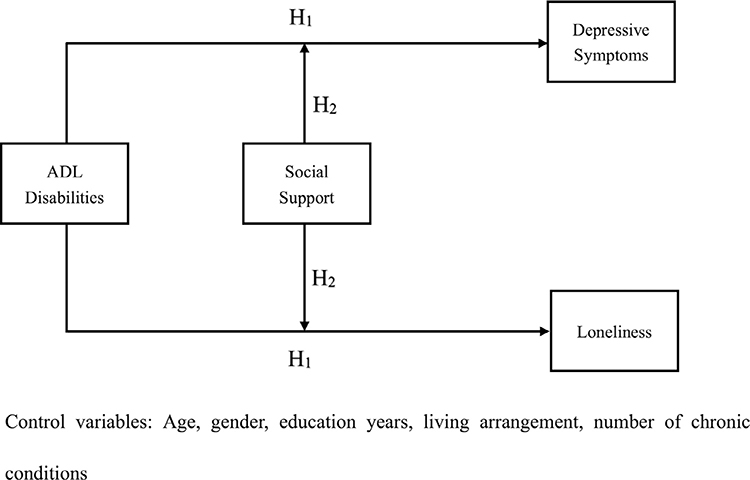
To address the knowledge gap, we developed the Vietnamese Aging and Care Survey (VACS) and collected data on older Vietnamese Americans (65 years and older) and their family caregivers in Houston, Texas in 2017 and 2018.34,35 Vietnamese are the largest Asian American subgroup in Houston and Houston has the third-largest Vietnamese American population in the nation.36 The purpose of this study was three-fold: to report on the health status of older Vietnamese immigrants; to examine the association between having a physical disability (i.e., number of Activities of Daily Living (ADL) disability) and their mental health (depressive symptoms and loneliness); and to test the possible moderating role of social support in the association between ADL disability and mental health. We used Cohen’s stress-buffering model (1985)37 as a conceptual framework. Cohen’s model posits that social support “intervene between the stressful event and a stress reaction by attenuating or preventing a stress appraisal response” and even “intervene between the experience of stress and the onset of the pathological outcome by reducing or eliminating the stress reaction or by directly influencing physiological processes” (p. 312). We hypothesized that older Vietnamese immigrants with more ADL disability would experience more depressive symptoms and loneliness (H1) and social support would moderate the effect of ADL disability on depressive symptoms and loneliness (H2). Figure 1 shows the conceptual model of this study. Since there have been hardly any previous studies on how social support moderates older Vietnamese immigrants’ physical disabilities on depressive symptoms and loneliness (role of social support), this exploratory study is vital in filling the knowledge gap on this understudied but fast-growing population.
Figure 1.
Conceptual Model of the Study
Methods
Study design
Using the Hispanic Established Populations for Epidemiological Studies of the Elderly (H-EPESE) as a model,38 we developed a crosss-ectional care recipient survey in both Vietnamese and English. We selected psychosocial instruments from the H-EPESE and included additional instruments related to the Asian cultural context such as filial responsibility expectation. In this analysis, we used questions on the participants’ sociodemographics, global health, chronic health conditions, ADL and Instrumental Activities of Daily Living (IADL) disability, mental health (depressive symptoms, loneliness), memory-related questions, and receipt of social support.
Sample
Inclusion criteria were self-identification as Vietnamese, who were 65 years and older, spoke English or Vietnamese, and lived in the greater Houston, Texas area at the time of the survey. Exclusion criteria were those who lived in long-term care facilities and were cared for by professional caregivers. We approached 132 potential study participants. All of them (100%) were eligible and consented to participate in the study. The final sample size was 132 participants (N = 132).
Data collection
Data collection took place in November 2017 and April-May 2018. We first reached out to the Executive Directors of the two Vietnamese social service agencies and obtained their support, which was instrumental in introducing us to several Vietnamese community key persons in various organizations (e.g., Vietnamese senior housing, senior center, community centers). We used the English and Vietnamese versions of the study flyer and asked these organizations to disseminate the information about the study to their organization members. Snowball sampling and word-of-mouth were used to identify participants. We hired two bilingual and bicultural Vietnamese Research Assistants (RAs) and trained them in interviewing skills. They interviewed and filled out the surveys on behalf of the participants as many older Vietnamese participants preferred to be interviewed rather than filling out the surveys by themselves. Vietnamese key personnel selected eligible participants and arranged group meeting dates/times. Our research team met these participants in groups and surveyed them in one location. Other potential Vietnamese participants approached RAs by phone. The RAs checked their eligibility, set appointments, and met at the participants’ preferred locations (e.g., home, church, community center, etc.). In order to protect the physical and mental health safety of the participants, the surveys took place primarily at their homes. We were allowed to use a proxy (i.e., family caregiver) in case the participants were unable to answer questions by themselves due to their physical, mental, or cognitive conditions. However, no proxy data were used for this analysis. The survey interview took 20 to 30 minutes, and a $20 store gift card was provided to all the participants at the end of the interview. A written consent form was obtained from all the participants prior to the survey. The study was approved by the PI’s university (STUDY00000419).
Measures
All the existing instruments and sociodemographic questions except the Center for Epidemiologic Studies Depression Scale (CES-D)39 needed to be translated from English to Vietnamese since no Vietnamese versions of these instruments were available. A bilingual, native Vietnamese social worker (Master of Social Work) conducted forward translations from English into Vietnamese. Another bilingual, native Vietnamese medical sociologist (Postdoctoral fellow) conducted backward translation. Our Vietnamese Community Advisory Board consisted of five bilingual Vietnamese professionals (i.e., social workers and counselors) with a licensed Master’s degree in Social Work and currently working with diverse racial/ethnic groups of clients in the Houston community. They provided suggestions on the types of inquires to ask and the instruments to be used in the surveys. They also approved the translation.
Depressive symptoms were measured by the 20-item CES-D.39 Scores may range from 0 to 60 with the higher score indicating greater depressive symptoms. A score of 16 or greater has been associated with a risk of clinical depression (high depressive symptoms).40 We used the validated Vietnamese version of the CES-D.41 Cronbach’s alpha was 0.89, which is comparable to other studies with Vietnamese subjects.42
Loneliness was measured by the three-item UCLA Loneliness Scale.43 The three questions measure three dimensions of participants’ loneliness: related connectedness, social connectedness, and self-perceived isolation by asking: “How often do you feel that you lack companionship?” (related connectedness), “How often do you feel left out?” (social connectedness) and “How often do you feel isolated from others?” (self-perceived isolation) respectively. There are three response categories from “hardly ever = 1,” “some of the time = 2,” to “often = 3.” Scores are added together with the possible range of 3 to 9. A higher score indicates a greater feeling of loneliness. Cronbach’s alpha was 0.84, which is higher than that was obtained in the original study of 0.72.43
Receipt of social support was assessed using the 19-item Medical Outcomes Study Social Support Survey (MOS-SS).44 It is a widely used, self-administered survey that measures four major dimensions of social support: tangible, affectionate, and emotional support, and positive social interaction. Participants were asked how often each support was available to them by selecting a choice of “none of the time,” “a little of the time,” “some of the time,” “most of the time,” and “all the time.” For this assessment, we selected a total of nine questions and measured the availability of support such as “Someone to help you if you were confined to bed” (tangible support), “Someone who shows you love and affection” (affectionate support), “Someone to confide in or talk about yourself or your problems” (emotional support), or “Someone to get together with for relaxation” (positive social interaction). We used the answer choice of “1 = none of the time,” “2 = some of the time” and “3 = all the time.” Cronbach’s alpha was 0.95, which is slightly higher than the alpha obtained in the original study.44
Covariates included sociodemographic characteristics: age, gender (0 = male, 1 = female), years of formal education (0 = < 12 years, 1 = ≥12 years), and living arrangements (0 = live alone, 1 = live with others). Health-related characteristics assessed included the number of ADL disabilities: walking across a small room, bathing, grooming, dressing, eating, getting from a bed to a chair, and toileting (1 = need help with; 0 = do not need help with). The presence of chronic health conditions such as arthritis, cancer, heart attack, stroke, high blood pressure, diabetes, liver diseases, lung diseases were coded 1 for yes vs 0 for no.
Data analysis
T-tests and Chi-square (or Fisher’s exact) tests were used to compare continuous and categorical variables between participants who reported high depressive symptoms or loneliness and those who did not. We first examined the crude association between physical disability and depressive symptoms (Model 1), and then the crude association between receipt of social support and depressive symptoms (Model 2) using linear regression models with the depressive symptom outcome treated as a logged score. In the third model, we created an interaction term between physical disability and receipt of social support and tested its significance to examine the moderator role of social support. Lastly, we tested the significance of this interaction term adjusting for covariates (Model 4). Similar models were also performed with the loneliness outcome as a continuous score.
Given the small sample size, we calculated pairwise correlation coefficients and examined collinearity using Collin command in Stata. This command computes several collinearity diagnostic measures including variance inflation factor (VIF) and tolerance. No multicollinearity was found based on a variance inflation factor (VIF) cut-off score of greater than 10 or a tolerance value lower than 0.1. We also conducted sensitivity analyses treating the depressive symptoms and loneliness outcomes as binary variables to ensure the robustness of our results (See Supplemental materials). The post hoc power with the logged depression score as the outcome was 0.79 and the one with the loneliness score as the outcome was 0.83. Person-mean imputation was used for missing data in outcome variables. All the analyses were performed with STATA version 15.0 (StataCorp., 2017).
Results
Participants’ sociodemographic and health characteristics
Table 1 presents the results of the overall characteristics of the respondents (N = 132) by depressive symptoms and loneliness status. Respondents were between 65 and 90 years old (mean=75.4), mostly retired (94%), married (58%) or widowed (21%), and female (55%). They were all born in Vietnam (100%) and immigrated at the mean age of 49 years old (range 21–88). Their mean number of formal education years was eight; however, education years varied widely from no formal education (20%) to more than 12 years with a high school diploma (14%). The vast majority (94%) had annual household income of less than $25,000/year. They lived with their spouse (39%) or other relatives (28%) in ethnic enclaves (48%) (not shown in the table) and spoke only Vietnamese at home (88%). Many (70%) had caregivers, who were family members (67%) living with them (57%) or near-by (32%), and approximately 36% and 15% of them experienced depressive symptoms and feelings of loneliness, respectively (not shown in the table).
Table 1.
Characteristics of Vietnamese older Immigrants (≥65 years) (N=132)
| All Sample | Depression (n=132) |
Loneliness (n=128) |
|||||
|---|---|---|---|---|---|---|---|
| M±SD, N (%) | Yes (n=47) | No (n=85) | p-value | Yes (n=19) | No (n=109) | p-value | |
| Age (year) Gender | 75.4 ± 6.4 | 76.1 ± 6.7 | 75.0 ± 6.3 | 0.342 | 75.0 ± 6.0 | 75.4 ± 6.5 | 0.785 |
| Female | 72 (54.5%) | 29 (40.3%) | 43 (59.7%) | 0.219 | 14(20.3%) | 55(79.7%) | 0.061 |
| Male | 60 (45.5%) | 18(30.0%) | 42 (70.0%) | 5 (8.8%) | 54(91.5%) | ||
| Marital Status | |||||||
| Married/partnered | 76 (57.6%) | 25 (32.9%) | 51 (67.1%) | 0.449 | 6 (8.2%) | 68(91.9%) | 0.012 |
| Not married | 56 (42.4%) | 22 (39.3%) | 34 (60.7%) | 13 (24.5%) | 41 (75.9%) | ||
| Nativity | |||||||
| Vietnam-Born | 132(100.0%) | ||||||
| Years in the U.S. | 26.9 ± 13.0 | 29.9 ± 12.9 | 25.3 ± 12.9 | 0.067 | 29.6 ± 15.1 | 26.4 ± 12.6 | 0.323 |
| Education | |||||||
| 0 year | 26 (19.7%) | 11 (42.3%) | 15(57.7%) | 0.747 | 6 (23.1%) | 20 (76.9%) | 0.516 |
| 1 to 6 years | 28 (21.2%) | 10(35.7%) | 18(64.3%) | 4(14.8%) | 23 (85.2%) | ||
| 6+ to 12 years | 59 (44.7%) | 21 (35.6%) | 38 (64.4%) | 6 (10.5%) | 51 (89.5%) | ||
| ≥ 12 years | 19(14.4%) | 5 (26.3%) | 14(73.7%) | 3 (16.7%) | 15(83.3%) | ||
| Household Income | |||||||
| < $25,000 | 124(93.9%) | 45 (36.3%) | 79 (63.7%) | 0.518 | 17(14.4%) | 103 (85.8%) | 0.404 |
| ≥ $25,000 Co-Residents | 8(6.1%) | 2 (25.0%) | 6 (75.0%) | 2 (25.0%) | 6 (75.0%) | ||
| Live alone | 24(18.2%) | 8 (33.3%) | 16(66.7%) | 0.797 | 5 (21.7%) | 17(78.3%) | 0.253 |
| Live with other(s) | 108 (81.8%) | 39 (36.1%) | 69 (63.9%) | 14(13.2%) | 92 (86.8%) | ||
| Language spoken at home | |||||||
| Vietnamese | 116(87.9%) | 45 (38.8%) | 71 (61.2%) | 0.039 | 15(13.6%) | 97 (86.6%) | 0.222 |
| Vietnamese & other | 16(12.1%) | 2 (12.5%) | 14(87.5%) | 4 (25.0%) | 12(75.0%) | ||
| Overall Health | |||||||
| Good/Excellent | 32 (24.2%) | 4 (12.5%) | 28 (87.5%) | 0.002 | 3 (9.7%) | 28 (90.3%) | 0.353 |
| Fair/poor | 100(76.8%) | 43(43.0%) | 57 (57.0%) | 16(16.8%) | 81 (83.5%) | ||
| Chronic diseases (yes) | 97(74.1%) | 39 (40.2%) | 58 (59.8%) | 0.039 | 14(15.2%) | 80(85.1%) | 0.979 |
| # of ADL disabilities | 1.3 ± 2.1 | 2.0 ± 2.5 | 0.9 ± 1.7 | 0.002 | 2.3 ± 2.6 | 1.1 ± 2.0 | 0.020 |
| Dementia Status | |||||||
| Yes | 44 (33.3%) | 23 (52.3%) | 21 (47.7%) | 0.005 | 8(18.6%) | 35 (81.4%) | 0.395 |
| No | 88 (66.7%) | 24 (27.3%) | 64 (72.7%) | 11 (12.9%) | 74(87.1%) | ||
| Social Support | 21.4 ± 6.6 | 21.2 ± 7.0 | 21.4 ± 6.4 | 0.876 | 18.1 ± 6.9 | 22.0 ± 6.3 | 0.013 |
Note. M = mean; SD = standard deviation. ADL score ranges: 0–7; Social Support: 9–27
The majority of respondents (77%) reported their health as fair or poor which was associated with high depressive symptoms (p=0.002). Most of them (74%) had at least one chronic health condition including high blood pressure (75%), arthritis (49%), diabetes (41%), and visual impairment (77%) (not shown in the table). Their reported number of ADL disabilities was significantly associated with depressive symptoms (p = 0.002) and loneliness (p = 0.020). Their cognitive status was on average 24.6 out of 30 MMSE points (not shown in the table) with 33% being cognitively impaired (MMSE score of ≤ 23). Their cognitive status was strongly associated with their depressive symptoms (p = 0.005), but it was not with loneliness (p = 0.395). They reported relatively high social support at 21.4 (SD = 6.6) out of 27 points. Receipt of social support was not associated with their depressive symptoms (p = 0.876), but receipt of greater social support was associated with low feelings of loneliness (p = 0.013).
Disabilities and receipt of social support on mental health
Table 2 shows the results of linear regression models predicting depressive symptoms. ADL disabilities showed positive associations in Model 1 (b = 0.067, p = 0.006) and Model 3 (b = 0.213, p = 0.019) and remained positive in Model 4 (b = 0.203, p = 0.030) (H1). But other than that, receipt of social support, as well as any sociodemographic characteristics, had no statistically significant association with depressive symptoms across four models. The interaction term between ADL disabilities and receipt of social support was also insignificant in Model 3 and Model 4 (H2). The results of sensitivity analysis (Supplemental Material Table S1) treating depressive symptoms as binary showed similar patterns.
Table 2.
Linear Regression Analysis Predicting Vietnamese Older Immigrants’ Depressive Symptoms (N = 132)
| Variables | Model 1 |
Model 2 |
Model 3 |
Model 4 |
||||
|---|---|---|---|---|---|---|---|---|
| b (s.e.) | 95% CI | b (s.e.) | 95% CI | b (s.e.) | 95% CI | b (s.e.) | 95% CI | |
| Number of ADL disabilities | 0.067** (.024) | .019,.115 | 0.213* (.089) | .036,.390 | 0.203* (.092) | .020,.386 | ||
| Social support | 0.004 (.008) | −.011,.020 | 0.012 (.009) | −.006,.029 | 0.012 (.009) | −.006, .031 | ||
| ADL disabilities x Social Support | −0.007 (.004) | −.015,.001 | −0.007 (.004) | −.014, .001 | ||||
| Physical Health | ||||||||
| Number of chronic conditions | 0.200 (.117) | −.036, .429 | ||||||
| Sociodemographic Characteristics | ||||||||
| Age (years) | 0.0003 (.008) | −.016, .016 | ||||||
| Gender (ref. male) | 0.117 (.108) | −.097, .332 | ||||||
| Education years | −0.002 (.010) | −.022, .018 | ||||||
| Living arrangement (ref. live alone) | ||||||||
| Live with others | 0.061 (.138) | −.213,.335 | ||||||
Note: s.e. = standard error; CI = Confidence Interval
p< .05
p< .01; all covariates included in the models were presented here.
Table 3 presents the associations between ADL disabilities, receipt of social support, and feelings of loneliness. ADL disabilities showed strong positive associations with loneliness in Model 1 (b = 0.183, p = 0.007), Model 3 (b = 0.954, p = 0.001) as well as Model 4 (b = 0.839, p = 0.001) (H1). Receipt of social support had negative associations with feelings of loneliness, but they were not statistically significant. Receipt of social support significantly moderated the relationship between the number of ADL disabilities and feelings of loneliness in Model 3 (b = −0.035, p = 0.001) with its moderating effect remaining strong after adjusting for physical health and sociodemographics (i.e., age, gender, education years, and living arrangements) in Model 4 (b = −0.031, p = 0.004) (H2). When we treated feelings of loneliness as binary (Supplemental Material Table S2), the results were similar.
Table 3.
Linear Regression Analysis Predicting Vietnamese Older Immigrants’ Feeling of Loneliness (N = 128)
| Variables | Model 1 |
Model 2 |
Model 3 |
Model 4 |
||||
|---|---|---|---|---|---|---|---|---|
| b (s.e.) | 95% CI | b (s.e.) | 95% CI | b (s.e.) | 95% CI | b (s.e.) | 95% CI | |
| Number of ADL disabilities | 0.183** (.067) | .050, .317 | 0.954*** (.237) | .485, 1.423 | 0.839** (.245) | .355, 1.323 | ||
| Social support | −0.042 (.022) | −.084, .0009 | −0.001 (.024) | −.048, .045 | −0.014 (.025) | −.062, .034 | ||
| ADL disabilities x Social Support | −0.035*** (.010) | −.056,−.015 | −0.031** (.011) | −.052, −.010 | ||||
| Physical Health | ||||||||
| Number of chronic conditions | −0.156 (.311) | −.772, .460 | ||||||
| Sociodemographic Characteristics | ||||||||
| Age (years) | −0.020 (.022) | −.063, .022 | ||||||
| Gender (ref. male) | 0.073 (.287) | −.495, .642 | ||||||
| Education years | −0.028 (.027) | −.080, .025 | ||||||
| Living arrangement (ref. live alone) | ||||||||
| Live with others | −0.325 (.366) | −1.050, .401 | ||||||
Note: s.e. = standard error; CI = Confidence Interval
p< .05
p< .01
p<.001; all covariates included in the models were presented here.
Discussion
We examined the associations between ADL disabilities and receipt of social support with depressive symptoms and feelings of loneliness in 132 community-dwelling older Vietnamese immigrants in Houston, Texas. Their sociodemographic and health characteristics were similar to older Vietnamese immigrants in the U.S.: low income and fair/poor health. The number of ADL disabilities was significantly associated with high levels of depressive symptoms which is consistent with previous work with both cross-sectional45 and longitudinal studies46,47 across different racial/ethnic groups of older adults.48–50 Our findings are also consistent with those found in older Japanese immigrants for whom ADL disabilities were associated with compromised social opportunities and high depressive symptomatology. Physical disability tends to impede social interaction and may produce changes in older people’s relationships with others thus making them prone to stress and anxiety.
Receipt of social support, however, did not appear to have a strong association with depressive symptoms. This relationship was a surprise because previous studies with older Korean and Japanese immigrants showed that lack of social support was strongly associated with high depressive symptoms48,51 with emotional support moderating the influence of life stress on depressive symptoms.52 Lai and colleagues’ study with older Chinese Americans53 also found similar positive relationships between a feeling of intergenerational closeness and self-rated well-being. Because these older Vietnamese immigrants tended to live with families (82%), their instrumental and emotional support are readily available. Such living arrangements may alleviate their physical disabilities and prevent them from being depressed.
We also found a strong association between the number of ADL disabilities and loneliness: the more disabilities older Vietnamese immigrants had, the higher levels of loneliness they experienced. This relationship has been investigated in various racial/ethnic groups across different countries.54,55 However, the results have been inconsistent with some studies showing similar results with our study while others finding no associations.56 The associations between receipt of social support and the absence of feelings of loneliness in this study was in the expected direction, but it was not statistically significant. However, the interaction term identified receipt of social support as a moderator of the relationship between ADL disabilities and feelings of loneliness: among those who received more social support, ADL disabilities were associated with a lower loneliness score compared to those who received less social support. As previously mentioned, older Vietnamese immigrants tend to live with relatives within ethnic enclaves. They are surrounded by their families living next to each other, interacting, and communicating in their native language daily, and therefore are rarely alone. This living condition is similar to that of older Southeast Asian immigrants in Canada. This arrangement – not being alone in a foreign land - positively influenced a feeling of Southeast Asian elders as they hardly felt lonely.57 Although there are positive and negative intergenerational relationships that may affect their feeling of loneliness,53 social support appears to have a strong effect on loneliness among older Vietnamese immigrants. This is also supported by previous studies that despite their socioeconomic status, living in ethnic enclaves appears to give health advantages among older Hispanic/Latino immigrants in the U.S.58 However, Cela and Fokkema’s study (2017)59 revealed a different scenario experienced by older Albanian and Moroccan immigrants in Italy. Although these older immigrants were surrounded by their immediate and extended families, they still felt lonely because of a lack of meaningful relationships with non-relative, co-ethnic peers. Therefore, acknowledging the familial-focused Vietnamese culture, living in Vietnamese enclaves and having access to their families, relatives, as well as peers can satisfy these older Vietnamese immigrants’ emotional needs and underscore its importance on their mental health.
Limitations
Limitations of the study include a small convenience sample of Vietnamese older adults who lived in the greater Houston area. Many of the participants were interviewed at Vietnamese daycare sites and senior centers and were able to actively participate in their activities, suggesting a certain level of independence. Participation in these activities not only promotes Vietnamese older adults’ independence but also increases socialization opportunities and thus impacts the level of loneliness. It is paramount to also reach out to homebound seniors who are unable to attend daycare or senior centers. There were two large senior housing complexes where many of the respondents were recruited. Others were recruited from Vietnamese churches as well as by word-of-mouth via Vietnamese community key persons. Future research should include a socioeconomically and geographically more diverse sample.
We used existing instruments to measure all social and health aspects of the participants. The MOS-SS covers four dimensions of social support, but social support can include broader aspects such as participants’ reciprocal relationships and closeness with their family members and peers. However, that aspect was not included in the question items, and therefore, the measured aspects of social support may be limited.
Associations between ADL and depressive symptoms, as well as loneliness and depressive symptoms, can be bidirectional. We did not investigate these relationships in this study. Nonetheless, this paper contributes to the limited knowledge on the association between older Vietnamese immigrants’ ADL disabilities and receipt of social support and their mental health.
Conclusions
Despite their mid-life migration and refugee experience, Vietnamese older adults in the Houston area are supported by tight family units. By leveraging the family unit as a strength, health-care professionals can facilitate access to more health and social services to benefit Vietnamese older adults’ physical and mental health. Nurses can play an advocacy role by working not only with older adults but also with their family members and encouraging them to use existing social and health services such as senior centers and adult daycare centers that provide congregate meals and group physical activities. It is also critical that service providers consider and meet the expectations of older immigrants and their families by providing culturally and linguistically appropriate services. Positive physical and mental health benefits of ethnically specific senior centers, adult daycare centers, and community group activities for immigrants have been found in different ethnic contexts.58,60–62 Similarly, local policymakers and other stakeholders might need to discuss and strategize how to respond to this physical and mental issue and mitigate depression and loneliness among older Vietnamese people with a higher number of physical disabilities. For example, home and community-based services run by the state may be able to support Vietnamese families by providing professional home care workers to care for their loved ones at home. Since most older Vietnamese adults are mono-lingual Vietnamese, Vietnamese home care workers can be helpful to cook ethnic meals and communicate in their native language. This way, homebound Vietnamese older adults can be cared for while their family members work outside the home. As this segment of the population is increasing rapidly, more needs to be done to maintain and improve the psychosocial status of older Vietnamese immigrants in Houston and elsewhere.
Control variables
Age, gender, education years, living arrangement, number of chronic conditions
Supplementary Material
Acknowledgments
Funding source
Miyawaki was partially funded by the National Institutes of Health (NIH)/National Institute on Aging (NIA) Texas Resource Center for Minority Aging Research (RCMAR) (P30AG059301).
Footnotes
Declaration of Competing Interest
All authors have no competing interests to declare
Submission declaration
This manuscript has not been published previously and is not under consideration for publication elsewhere.
Supplementary materials
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.gerinurse.2022.01.012.
References
- 1.Budiman A Vietnamese in the U.S. fact sheet. Pew Res Center. 2021. Retrieved from; https://www.pewresearch.org/social-trends/fact-sheet/asian-americans-vietnamese-in-the-u-s-fact-sheet/#vietnamese-population-in-the-u-s2000-2019. [Google Scholar]
- 2.Alperin E, Batalova J. Vietnamese immigrants in the United States. Migrat Inf Source. 2018. Retrieved from; https://www.migrationpolicy.org/article/vietnamese-immigrants-united-states-5. [Google Scholar]
- 3.Rkasnuam H, Batalova J. Vietnamese immigrants in the United States. Migrat Inf Source. 2014. Retrieved from; https://www.migrationpolicy.org/article/vietname-seimmigrants-united-states-2. [Google Scholar]
- 4.Budiman A, Ruiz NG. Key facts about Asian origin groups in the U.S. Factank. Pew Res Center. 2021. Retrieved from; https://www.pewresearch.org/fact-tank/2021/04/29/key-facts-about-asian-origin-groups-in-the-u-s/. [Google Scholar]
- 5.Kim G, Chiriboga DA, Jang Y, Lee S, Huang C-H, Parmelee P. Health status of older Asian Americans in California. J Am Geriatr Soc. 2010;58(10):2003–2008. 10.1111/j.1532-5415.2010.03034.x. [DOI] [PubMed] [Google Scholar]
- 6.Pyke K ‘The normal American family’ as an interpretive structure of family life among grown children of Korean and Vietnamese immigrants. J Marriage Family. 2000;62:240–255. [Google Scholar]
- 7.Fancher TL, Ton H, Meyer OL, Ho T, Paterniti DA. Discussing depression with Vietnamese American patients. J Immigrant Minority Health. 2010;12(2):263–266. 10.1007/s10903-009-9234-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen D, Bernstein LJ, Goel M. Asian American elders’ health and physician use: An examination of social determinants and lifespan influences. Health (N. Y). 2012;4:1106–1115. [Google Scholar]
- 9.McCracken M, Olsen M, Chen MS Jr, et al. Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA Cancer J Clin. 2007;57(4):190–205. 10.3322/canjclin.57.4.190. [DOI] [PubMed] [Google Scholar]
- 10.Tran C, Hinton L. Health and health care of Vietnamese American older adults. Ethno Med-Vietnamese. 2010. Stanford School of Medicine. Retrieved from; http://geriatrics.standford.edu/ethnomed/Vietnamese/. [Google Scholar]
- 11.Fuller-Thomson E, Brennenstuhl S, Hurd M. Comparison of disability rates among older adults in aggregated and separate Asian American/Pacific Islander subpopulations. Am J Public Health. 2011;101(1):94–100. 10.2105/AJPH.2009.176784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ro A, Gee GC. Disability status differentials among Asian immigrants in the United States: the added dimensions of duration and age. Race Soc Problems. 2012;4:83–92. 10.1007/s12552-012-9069-3. [DOI] [Google Scholar]
- 13.Yang MS, Burr JA, Mutchler JE. The prevalence of sensory deficits, functional limitations, and disability among older Southeast Asians in the United States. J Aging Health. 2012;24(7):1252–1274. 10.1177/0898264312457413. [DOI] [PubMed] [Google Scholar]
- 14.Nkimbeng M, Cudjoe J, Turkson-Ocran RA, Commodore-Mensah Y, Thorpe RJ Jr, Szanton SL. Disparities in the prevalence and correlates of disability in older immigrants in the USA: A systematic review of the literature. J Racial Ethnic Health Disparit. 2019;6(3):552–562. 10.1007/s40615-018-00554-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nguyen GD. Generational conflicts among Vietnamese Americans in the health care decision making process. Online J Health Ethics. 2015;11(2). 10.18785/ojhe.1102.03. [DOI] [Google Scholar]
- 16.Liu D, Hinton L, Tran C, Hinton D, Barker JC. Reexamining the relationships among dementia, stigma, and aging in immigrant Chinese and Vietnamese family caregivers. J Cross Cult Gerontol. 2008;23:283–299. 10.1007/s10823-008-9075-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nguyen QCX, Anderson LP. Vietnamese Americans’ attitudes toward seeking mental health services: Relation to cultural variables. J Commun Psychol. 2005;33 (2):213–231. 10.1002/jcop.20039. [DOI] [Google Scholar]
- 18.Yeo G, UyenTran JN, Hikoyeda N, Hinton L. Conceptions of dementia among Vietnamese American caregivers. J Gerontol Soc Work. 2002;36(1–2):131–152. 10.1300/J083v36n01_08. [DOI] [Google Scholar]
- 19.Do M, McCleary J, Nguyen D, Winfrey K. Mental illness public stigma and generational differences among Vietnamese Americans. Commun Ment Health J. 2020;56:839–853. 10.1007/s10597-019-00545-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park H-J, Morgan T, Wiles J, Gott M. Lonely ageing in a foreign land: Social isolation and loneliness among older Asian migrants in New Zealand. Health Soc Care Commun. 2018;27(3):740–747. 10.1111/hsc.12690. [DOI] [PubMed] [Google Scholar]
- 21.Shorey S, Chan V. The experiences and needs of Asian older adults who are socially isolated and lonely: a qualitative systematic review. Arch. Gerontol. Geriatr. 2021;92: 104254. 10.1016/j.archger.2020.104254. [DOI] [PubMed] [Google Scholar]
- 22.Cohen-Mansfield J, Hazan H, Lerman Y, Shalom V. Correlates and predictors of loneliness in older-adults: a review of quantitative results informed by qualitative insights. Int. Psychogeriatr 2016;28(4):557–576. 10.1017/S1041610215001532. [DOI] [PubMed] [Google Scholar]
- 23.Ong AD, Uchino BN, Wethington E. Loneliness and health in older adults: a minireview and synthesis. Gerontology. 2016;62(4):443–449. 10.1159/000441651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238–249. 10.1177/1745691615570616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kwon S, Min D, Chong S. Asian American older adults and social isolation: a systematic literature review. Innovat Aging. 2020;4(S1):328. [Google Scholar]
- 26.Simon, et al. , et al. The prevalence of loneliness among U.S. Chinese older adults. J Aging Health. 2014;26(7):1172–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weng. An Asian American community intergenerational response. J Intergenerat Relationships. 2019;3:257–272. [Google Scholar]
- 28.Williams P, Barclay L, Schmied V. Defining social support in context: a necessary step in improving research, intervention, and practice. Qual Health Res. 2004;14 (7):942–960. 10.1177/1049732304266997. [DOI] [PubMed] [Google Scholar]
- 29.Wang SC, Creswell JW, Nguyen D. Vietnamese refugee elderly women and their experiences of social support: a multiple case study. J Cross Cult Gerontol. 2017;32:479–496. 10.1007/s10823-017-9338-0. [DOI] [PubMed] [Google Scholar]
- 30.Sangalang CC, Gee GC. Depression and anxiety among Asian Americans: the effects of social support and strain. Soc Work. 2021;57(1):49–60. 10.1093/sw/swr005. [DOI] [PubMed] [Google Scholar]
- 31.Gellis ZD. Kin and nonkin social support in a community sample of Vietnamese immigrants. Soc Work. 2003;48(2):248–258. [DOI] [PubMed] [Google Scholar]
- 32.Tran TV, Wright R Jr Social support and subjective well-being among Vietnamese refugees. Soc Serv Rev. 1986;60(3):449–459. [Google Scholar]
- 33.Dang JK (2011). Vietnamese Americans and health literacy. Vietnam Talking Points. Retrieved from https://talk.onevietnam.org/vietnamese-americans-and-health-literacy-ready/. [Google Scholar]
- 34.Miyawaki CE, Chen N-W, Meyer OL, Tran MT, Markides KS. Vietnamese adult-childand spousal caregivers of older adults in Houston, Texas: Results from the Vietnamese Aging and Care Survey (VACS). J Gerontol Soc Work. 2020;63(1–2):5–18. 10.1080/01634372.2019.1707735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miyawaki CE, Meyer OL, Chen N-W, Markides KS. Health of Vietnamese older adults and caregiver’s psychological status in the United States: Result from the Vietnamese Aging and Care Survey. Clin Gerontol. 2020. 10.1080/07317115.2020.1764157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.U.S. Census Bureau. (2017). American community survey (ACS). American FactFinder 2017. Retrieved from https://data.census.gov/cedsci/table?d=ACS%205-Year%20Estimates%20Data%20Profiles&table=DP05&tid=ACSDP5Y2018.DP05&g=0400000US48_1600000US4835000. [Google Scholar]
- 37.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. [PubMed] [Google Scholar]
- 38.Markides K, Chen N-W, Angel R, Palmer R, & Graham J (2016). Hispanic established populations for the epidemiologic study of the elderly (HEPESE) Wave 7, 2010–2011 [Arizona, California, Colorado, New Mexico, and Texas]. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; [distributor], 2016–12-05. doi: 10.3886/ICPSR36537.v2. [DOI] [Google Scholar]
- 39.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Measur. 1977;1(3):385–401. 10.1177/014662167700100306. [DOI] [Google Scholar]
- 40.Windham AM, Rosenberg L, Fuddy L, McFarlane E, Sia C, Duggan AK. Risk of mother-reported child abuse in the first 3 years of life. Child Abuse Negl. 2004;28:645–667. 10.1016/j.chiabu.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 41.Nguyen TH, Le VA, Dunne M. Validity and reliability of the two scales measuring depression and anxiety used in community survey in Vietnamese adolescents. Vietnamese J Public Health. 2007;13(7):25–31. [Google Scholar]
- 42.Ta Park, Ton V, Tiet V, Vuong QQ, Yeo GQ, Gallagher-Thompson D. Promising results from a pilot study to reduce distress in Vietnamese American dementia and memory loss caregivers. Alzheimer’s Dementia: Transl Res Clin Intervent. 2019;5:319–327. 10.1016/j.trci.2019.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Ageing. 2004;26(6):655–672. 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sherbourne CD, Steward AL. The MOS social support survey. Soc Sci Med. 1991;32 (6):705–714. 10.1016/0277-9536(91)90150-B. [DOI] [PubMed] [Google Scholar]
- 45.Song HJ, Meade K, Akobundu U, Sahyoun NR. Depression as a correlate of functional status of community-dwelling older adults: Utilizing a short-version of 5-item Geriatric Depression scale as a screening tool. J Nutr. 2014;18(8):765–770. 10.1007/s12603-014-0542-0. Health & Aging. [DOI] [PubMed] [Google Scholar]
- 46.Chang M, Phillips C, Coppin AK, et al. An association between incident disability and depressive symptoms over 3 years of follow-up among older women: the Women’s Health and Aging Study. Aging Clin Exp Res. 2009;21(2):191–197. 10.1007/BF03325228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Murphy RA, Hagaman AK, Reinders I, et al. Depressive trajectories and risk of disability and mortality in older adults: longitudinal findings from the Health, Aging, and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2016;71(2):228–235. 10.1093/gerona/glv139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim B, Jun H, Lee J, & Kim YM (2020). Social support, activities of daily living, and depression among older Japanese and Korean immigrants in the U.S. Social Work in Public Health, 35(4), 163–176. doi: 10.1080/19371918.2020.1761922. [DOI] [PubMed] [Google Scholar]
- 49.Kim BJ, Liu L, Nakaoka S, Jang S, Browne C. Depression among older Japanese Americans: the impact of functional (ADL & IADL) and cognitive status. Soc Work Health Care. 2018;57(2):109–125. 10.1080/00981389.2017.1397588. [DOI] [PubMed] [Google Scholar]
- 50.Kong D, Solomon P, Dong X. Depressive symptoms and onset of functional disability over 2 years: a prospective cohort study. J Am Geriatric Soc. 2019;67:S538–S544. 10.1111/jgs.15801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee MS, Crittenden KS, Yu E. Social support and depression among elderly Korean immigrants in the United States. Int J Aging Hum Dev. 1996;42(4):313–327. 10.2190/2VHH-JLXY-EBVG-Y8JB. [DOI] [PubMed] [Google Scholar]
- 52.Lai DWL, Lee VWP, Li J, Dong X. The impact of intergenerational relationship onhealth and well-being of older Chinese Americans. J Am Geriatric Soc. 2019;67(S3): S557–S563. 10.1111/jgs.15893. [DOI] [PubMed] [Google Scholar]
- 53.Guo L, An L, Luo F, Yu B. Social isolation, loneliness and functional disability in Chinese older women and men: a longitudinal study. Age Ageing. 2020:1–7. 10.1093/ageing/afaa271Lizhi. [DOI] [PubMed] [Google Scholar]
- 54.Miri K, Bahrami M, Vafainnya R, Gholamzadeh T. Relationship between feeling of loneliness and activities of daily living among the elderly. J Res Health. 2017;7 (3):834–840. [Google Scholar]
- 55.Kuwert P, Knaevelsrud C, Pietrzak RH. Loneliness among older Veterans in the United States: results from the national health and resilience in veterans study. Am J Geriatr Psychiatry. 2014;22(6):564–569. 2014. [DOI] [PubMed] [Google Scholar]
- 56.Guo L, An L, Luo F, Yu B. Social isolation, loneliness and functional disability in Chinese older women and men: a longitudinal study. Age Ageing. 2021;50(4):1222–1228. 10.1093/ageing/afaa271. [DOI] [PubMed] [Google Scholar]
- 57.Nguyen GD. Generational conflicts among Vietnamese Americans in the health care decision making process. Online J Health Ethics. 2015;11(2). 10.18785/ojhe.1102.03. [DOI] [Google Scholar]
- 58.Dane S, Haslam C, Jetten J, Liu S, Gallois C, Tran TLN. The benefits of ethnic activity group participation on older immigrant well-being and host country adjustment. Int J Intercult Relation. 2020;77:119–124. 10.1016/j.ijintrel.2020.05.006. [DOI] [Google Scholar]
- 59.Cela E, Fokkema T. Being lonely later in life: a qualitative study among Albaniansand Moroccans in Italy. Ageing Soc. 2017;37:1197–1226. 10.1019/S0144686X16000209. [DOI] [Google Scholar]
- 60.Kim MK. Effect of Adult Day Health Care (ADHC) on Depression Among Korean Immigrant Older Adults. [Unpublished master’s thesis]. California State University Northridge; 2018. http://hdl.handle.net/10211.3/203999. [Google Scholar]
- 61.Kim J, Kim J. Exploring health benefits through senior center engagement: a qualitative investigation of older Korean immigrants. Activit Adaptat Aging. 2021;45 (1):1–13. 10.1080/01924788.2019.1698121. [DOI] [Google Scholar]
- 62.Miyawaki CE. Generational differences in Japanese Americans’ preferred senior service environments. J Gerontol Soc Work. 2013;56(1):388–406. 10.1080/01634372.2013.791906. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.