Abstract
Preliminary evidence seems to suggest a reduction in absolute terms of Emergency Department (ED) admissions for an acute psychiatric condition during the first months of the pandemic. The study aimed to test through a long-term time analysis the effect of COVID-19 on changes in ED visits for an acute psychiatric condition.
A quasi-experimental interrupted time series analysis of admissions for acute psychiatric conditions to the Emergency Department of the Merano Hospital (Italy) was performed from January 2017 to August 2021. The main outcome was the monthly rate of ED accesses for an acute psychiatric condition reported per 1000 general admissions. The pandemic outbreak was used as an intervention point.
4398 ED admissions for an acute psychiatric condition were registered. The rate of monthly admissions over total admissions increased from a mean of March 17, 1000 (SD 2.9) admissions per month in the pre-COVID-19 era to September 22, 1000 (SD 4.5) in the pandemic months, p < 0.001. In March 2020, the pandemic outbreak led to a significant increase in ED visits for an acute psychiatric condition (p = 0.013) and suicide attempts (p = 0.029), and to an increased need for pharmacological sedation in ED (p = 0.001). During the pandemic, although admissions and hospitalizations showed a non-significant decreasing trend, suicide attempts increased steadily and significantly.
The outbreak of the COVID-19 pandemic caused a major increase in rates of admission to the ED for an acute psychiatric condition.
Keywords: COVID-19, Suicide, Psychiatric, Acute psychiatric condition, SARS-CoV-2
1. Introduction
Among the adverse side effects of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) pandemic, the increase in mental disorders could be one of the major public health problems in the near future (Fiorillo and Gorwood 2020; Holmes et al., 2020). Lockdowns and restrictions on sociality implemented by governments to contain the rapid spread of the virus have seriously affected mental health, and the long-term effects are still difficult to predict (Fiorillo and Gorwood 2020; Holmes et al., 2020; Kohls et al., 2021).
In the short term, the first limited reports published in the literature seem to unexpectedly suggest a reduction in absolute terms of Emergency Department (ED) admissions for an acute psychiatric condition occurring in both the US and Europe in the first six months after the SARS-CoV-2 outbreak (Flament et al., 2021; Pikkel Pikkel Igal et al., 2021). Home isolation with greater difficulty in reaching health facilities, fear of contagion, and fear of discriminatory acts increased during the pandemic could be some of the reasons behind this decline (Håkansson and Grudet, 2021; Pikkel Pikkel Igal et al., 2021). However, the reduction in ED visits does not seem to be a prerogative of psychiatric pathology alone, as the general decline in visits observed in the immediate onset of the pandemic seems to be between 40 and 70% (Boserup et al., 2020; Mantica et al., 2020).
A recent large US cross-sectional study extending until October 2020 showed that at the outbreak of the pandemic, visits for mental health conditions increased in proportion to the decline in overall visits in the ED (Holland et al., 2021). In addition, considering only the initial months of the pandemic may not be sufficient to provide definitive indications about the impact of SARS-CoV-2 on acute psychiatric pathology, as it is known how disastrous events can cause an increase in mental health problems not only in the short term but especially in the long term (Holland et al., 2021; Kim et al., 2021).
Using the innovative technique of interrupted time series analysis (ITSA), we report an analysis of how the outbreak and sustained occurrence of the SARS-CoV-2 pandemic affected the number of accesses for acute psychiatric disorders in the ED.
2. Methods
2.1. Study design and setting
A quasi-experimental ITSA based on a retrospective review of data from all psychiatric admissions to the ED of the Hospital of Merano (Italy) from January 1, 2017 to August 30, 2021 was conducted. The Merano Hospital is located in an alpine area of Northern Italy, covering a district of 100,000 resident inhabitants and 2.5 million tourist nights per year. The ED of this hospital is open 24 h a day, and remained open even during the entire pandemic period, accepting all patients who requested an evaluation. The Merano Psychiatric Service includes a ten-bed acute hospital ward (Psychiatric Department), two twelve-bed psychiatric residences, a twenty-four-bed therapeutic rehabilitation facility, and a widespread territorial service consisting of three territorial mental health centers open during the week and with direct access. The acute hospital ward is integrated with the community service and operates with a no-restraint methodology with open doors and without the use of mechanical coercion (Colazzi, 2005; Hamlin, 1963).
During the first lockdown, between March and May 2021, the territorial services had to suspend their activities in presence but therapeutic assistance was guaranteed by the implementation of telemedicine with remote support. In the following months (June 2020), in-patient activities gradually resumed, with some modifications that probably reduced the number of services per patient but provided therapeutic and rehabilitative assistance. Finally, for patients not known to the service, through planning with general practitioners, it has been possible to guarantee the first assessments at local centers even during the more severe restrictions, allocating the request for assessment at the ED solely to the most serious cases or those not intercepted by the local network, as could have happened even before the pandemic.
The study was approved by the Local Ethics Committee (Comitato etico per la sperimentazione clinica, Azienda Sanitaria dell'Alto Adige, Bolzano, Italia, approval number 57–2020) and was conducted according to the Declaration of Helsinki regarding the Ethical Principles for Medical Research Involving Human Subjects.
2.2. Data collection
The monthly rate of ED accesses for an acute psychiatric condition reported per thousand general accesses was the main outcome of the study. It was derived from the following formula:
An acute psychiatric condition was considered to be any admission to the ED that required an emergency psychiatric assessment or presented a discharge or admission diagnosis with ICD-9 attributable to a psychiatric condition.
Electronic records of admissions for an acute psychiatric condition during the study period and the number of general admissions per month were extracted from the ED's computer database, which has been collecting all ED records since 2012 using QlickView data analysis software (QlikTech, Pennsylvania, PA, US). Non-resident patients (tourists) and patients transferred from other hospitals were excluded. Through manual re-evaluation of extracted records of psychiatric admissions, baseline characteristics of patients were recorded. Additional rates that could serve as surrogates for the impact of psychiatric pathology on ED were also identified: rate of admission for psychiatric pathology from the ED, the rate of monthly ED visits for suicide attempts, and the rate of patients requiring sedation in the ED.
2.3. Statistical analysis
Several quasi-experimental ITSA was conducted by analyzing the time course of different psychiatric indices chosen over the period (Bernal et al., 2017; Biglan et al., 2000). ITSA is a methodological approach recently used to analyze the effects of discrete interventions on longitudinal data and to compare the development of a variable between before and after a specific intervention or condition (Bernal et al., 2017; Biglan et al., 2000). The dependent variable is serially ordered over the number of observations in the time unit to form a time series and multiple observations are compared between before and after the intervention (Bernal et al., 2017; Biglan et al., 2000). The strength of the impact of an intervention is determined by assessing any change in the trend of post-event observations compared to the projected pre-event trend In this case, the intervention was the outbreak of the COVID-19 epidemic (March 2020) which created two time periods, pre-and post-pandemic. The ITSA, performed using the STATA command written by the user “itsa” specifying the prais model that automatically follows a first-order autoregressive process [AR (1)], provided for each time trend of each variable under study the following coefficients including their 95% confidence intervals and their p-values: a) the starting level of the variable; b) the trend before the intervention; c) the modification of the level by the intervention; d) the trend after the intervention.
Categorical variables were expressed as a percentage and number of events out of the total, and univariate comparisons were conducted with Fisher's exact test. Continuous variables were expressed as mean and standard deviation (SD). The univariate comparisons were performed using Student's t-test. Comparisons between variables and pre-post pandemic period were performed with Fisher's exact test. Incidence rate ratios (IRRs) with 95% confidence intervals (CIs) were calculated organizing data into an event-time table and adopting a Poisson regression model. All analyses were carried out with the statistical software STATA 16.1 and a p-value lower than 0.05 was considered significant.
3. Results
Overall, during the period between January 2017 and August 2021, the total number of admissions of patients living in the province in the ED was 235.794 with an average monthly admission of 4.240 (SD 820). The overall average monthly accesses decreased from 4.679 (SD 221) in the pre-COVID-19 era to 3.225 (SD 380), p < 0.001. The count of ED visits for an acute psychiatric condition in absolute terms decreased from a mean of 81 (SD 13) per month in the pre-COVID-19 era to 72 (SD 16) after the pandemic outbreak, p = 0.019. In relative terms compared to general visits, the monthly rate of accesses for an acute psychiatric condition increased from a mean of March 17, 1000 (SD 2.9) in the pre-COVID-19 era to a mean of September 22, 1000 (SD 4.5) after the onset of the pandemic, p < 0.001.
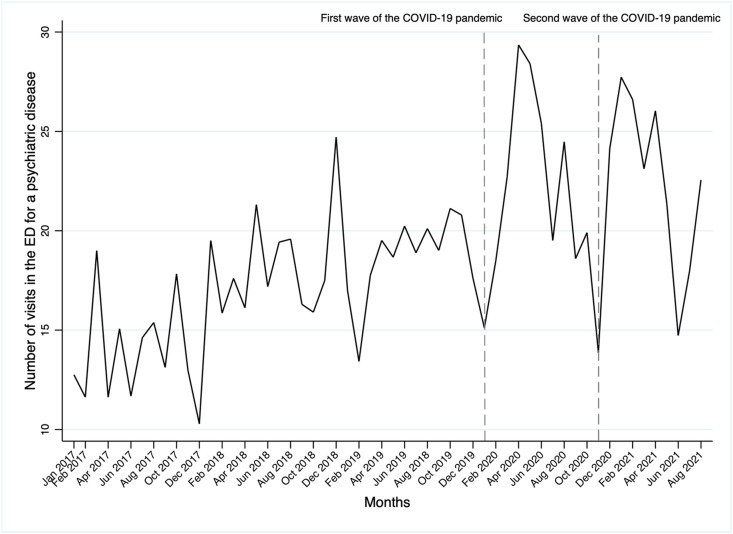
Fig. 1 shows the time series analysis of the monthly rate of visits in the ED for psychiatric conditions during the period 2017–2021. As can be observed, accesses for psychiatric conditions present a steadily increasing trend with unpredictable and non-cyclical seasonalities until the outbreak of the SARS-CoV-2 pandemic.
Fig. 1.
Number of psychiatric admissions in the emergency department from January 2017 to August 2021.
After the start of COVID-19, there is a marked increase in psychiatric accesses with a sustained higher peak until the end of the first wave (May 2020) and a deflation until the start of the second wave (November 2020). During the second pandemic wave (November 2020–May 2020), the increase in psychiatric accesses is concomitant with the resumption of infections and the introduction of new pandemic containment measures, which continue throughout the subsequent months of the pandemic.
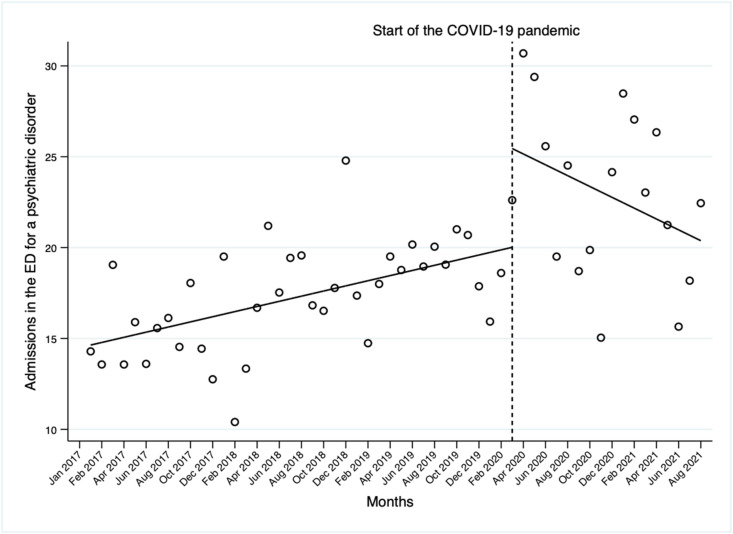
The ITSA shown in Fig. 2 , reported the monthly rate of psychiatric conditions in the ED as June 14, 1000 accesses in the period before the onset of SARS-CoV-2 with a significant increasing trend of 0.14/1000 (CI95% 0.08 to 0.21, p < 0.001) accesses per month until the COVID-19 outbreak. In March 2020, the COVID-19 outbreak led to a significant increase of a further April 5, 1000 (CI95% 1.19 to 9.68, p = 0.013) accesses per month, followed by a non-significant decreasing trend compared to the pre-COVID-19 period of −0.29/1000 accesses per month (CI9% −0.66 to −0.07, p = 0.109) but which seems likely to bring accesses at least to March 2020 levels (Fig. 2).
Fig. 2.
Interrupted time series analysis assessing the rate of psychiatric admissions in the emergency department standardized per 1.000 monthly emergency department visits from January 2017 to August 2021.
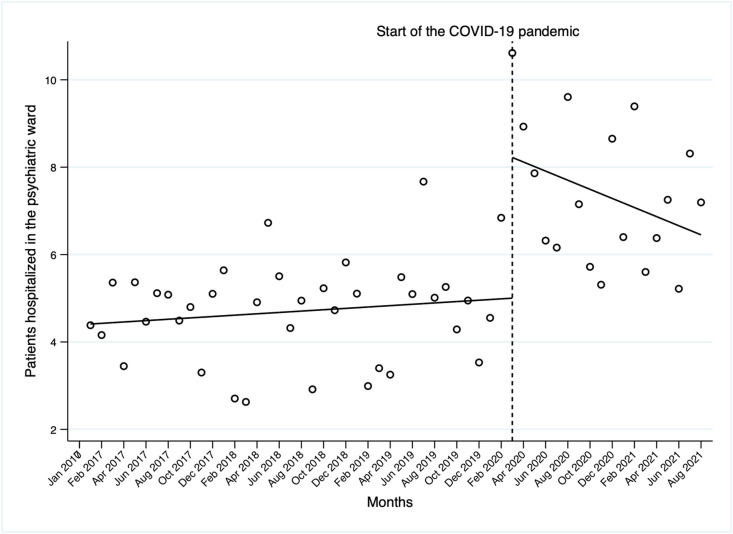
Admissions to the psychiatric department from the ED in the pre-COVID-19 era were stationary at 4.4 per 1000 accesses (CI95% 3.9 to 4.9, p < 0.001) per month with a statistically insignificant incremental trend of January 0, 1000 accesses per month (CI95% −0.01 to 0.04, p = 0.301) until the COVID-19 period. The advent of SARS-CoV-2 led to a marked increase in monthly admissions, with a peak in March 2020 of February 3, 1000 accesses (CI95% 1.6 to 4.9, p < 0.001) and then presenting a slight non-statistically significant decreasing trend compared to the pre-COVID-19 period (−0.1, CI95% −0.24 to 0.03, p = 0.140) but without returning to pre-pandemic levels (Fig. 3 ).
Fig. 3.
Interrupted time series analysis assessing the rate of patients hospitalized in the psychiatric department directly from the emergency department standardized per 1.000 monthly emergency department visits from January 2017 to August 2021.
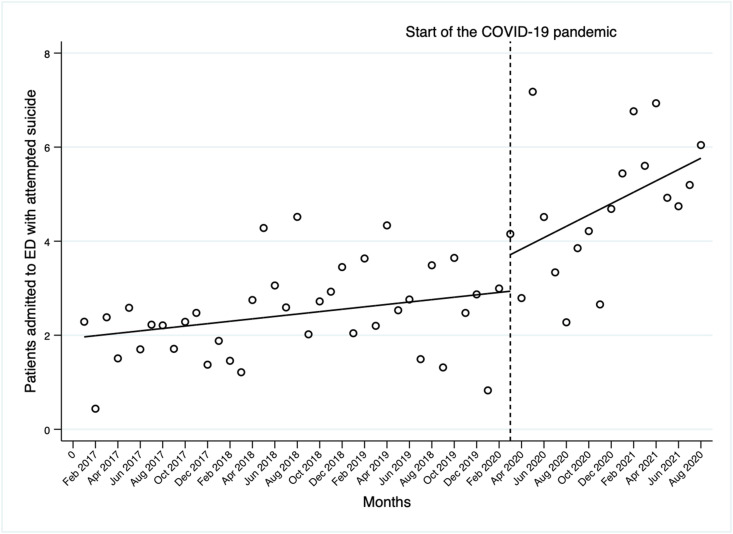
Suicide attempt assessments admitted to the ED were September 1, 1000 accesses in the pre-COVID-19 period (CI95% 1.52 to 2.40, p < 0.001) with a slight but significant steady monthly increase until the pandemic outbreak of February 0, 1000 (CI95 0.00 to 0.4, p = 0.023). SARS-CoV-2 caused a significant increase of December 0, 1000 accesses (CI95% 0.01 to 0.22, p = 0.029) with a steadily increasing trend over the subsequent seventeen months of the pandemic (Fig. 4 ).
Fig. 4.
Interrupted time series analysis assessing the rate of patients admitted to emergency department for an attempted suicide standardized per 1.000 monthly emergency department visits from January 2017 to August 2021.
Table 1 shows the characteristics of patients who accessed or were referred to the ED because they attempted suicide in the pre- and post-pandemic periods. Compared to the pre-pandemic, in the post-pandemic period there was an increase in the incidence rate ratio of ED accesses by patients with a suicide attempt and depression (IRR = 1.089, 95%CI 1.071–1.106, p < 0.001). Moreover, in the post-pandemic period the age of patients evaluated in the ED for suicide attempts was lower (IRR = 0.986, 95%CI 0.974–0.997, p < 0.001).
Table 1.
Clinical and anamnestic characteristics of patients with attempted suicide, according to ED accesses in pre- and post-pandemic periods. IRR, Incidence rate ratio.
| Variable | Pre-pandemic period | Post-pandemic period | p-value | IRR | p-value |
|---|---|---|---|---|---|
| Patients, n (%) | 401 (64.6) | 220 (35.4) | |||
| Age, years, mean (SD) | 39.9 (19.8) | 36.9 (19.4) | 0.034 | 0.986 (0.974–0.997) | 0.016 |
| Sex, n (%) | 0.554 | ||||
| Male | 178 (44.4) | 92 (41.8) | |||
| Female | 223 (55.6) | 128 (58.2) | |||
| Patients already known to psychiatric service, (%) | 271 (67.6) | 149 (67.7) | 1.000 | ||
| Psychiatric disorder, n (%) | |||||
| Depression | 203 (50.6) | 139 (63.2) | 0.003 | 1.089 (1.071–1.106) | <0.001 |
| Bipolar disorder | 28 (7) | 6 (2.7) | 0.027 | 0.656 (0.321–1.341) | 0.249 |
| Psychotic disorder | 94 (23.4) | 34 (15.5) | 0.022 | 1.086 (1.058–1.103) | <0.001 |
| Borderline personality disorder | 85 (21.3) | 42 (19.1) | 0.535 | ||
| Self-harm, n (%) | 197 (49.1) | 102 (46.4) | 0.557 | ||
| Drugs intoxication, n (%) | 62 (15.5) | 26 (11.8) | 0.231 | ||
| Alcohol abuse, n (%) | 54 (13.5) | 31 (14.1) | 0.903 | ||
| Police intervention, n (%) | 29 (7.2) | 14 (6.4) | 0.743 | ||
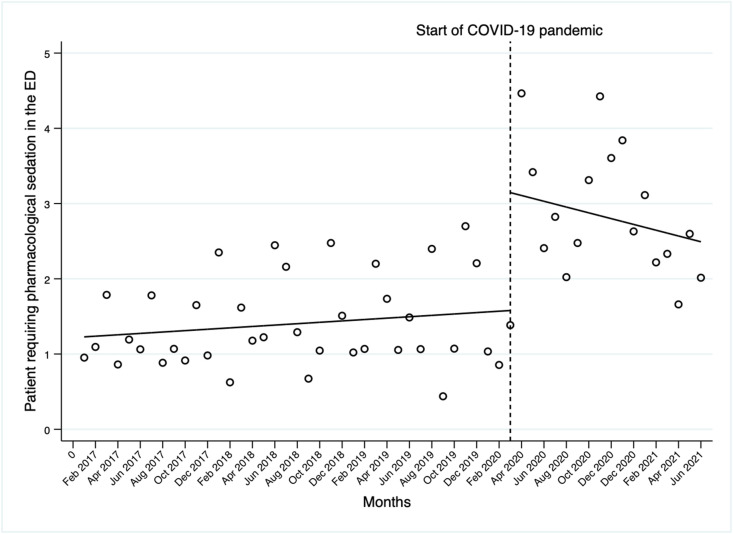
Finally, the need for pharmacological sedation, which in the pre-COVID-19 era was February 1, 1000 accesses per month (CI95% 0.9 to 1.5, p < 0.001) with a stable trend, increased to June 1, 1000 accesses at the outbreak of the pandemic (CI95% 0.6 to 2.5, p = 0.001). In the months following the pandemic, although a non-significant decreasing trend, levels appear to be significantly higher than pre-pandemic rates (Fig. 5 ).
Fig. 5.
Interrupted time series analysis assessing the rate of patients who required pharmacological sedation in the emergency department standardized per 1.000 monthly emergency department visits from January 2017 to August 2021.
4. Discussion
Using the innovative technique of ITSA, the study found that the outbreak of the COVID-19 pandemic caused a significant increase in the incidence of acute psychiatric conditions in relation to total ED visits and that psychiatric conditions remained at higher levels than pre-pandemic in the following months.
Since the beginning of the pandemic, mental health has been seriously affected. The drastic decrease in human contacts, forced isolation, the deconstruction of the day, the loss of active and recognized roles in society have all contributed to an increase in subjective psychological vulnerability and made it difficult to resume a satisfying life (Fountoulakis et al., 2021; Simon et al., 2021). Although the amount of data collected in recent months on various areas of psychiatric pathology seems to agree that the pandemic is causing and will cause an exponential increase in mental disorders in the coming years, the first data on psychiatric admissions to the ED during the first months of the pandemic seems to go against the trend (Fiorillo & Gorwood et al., 2020; Håkansson and Grudet, 2021; Al Majali and Alghazo, 2021; Holland et al., 2021; Holmes et al., 2020). In absolute terms, requests for emergency psychiatric assessments in the ED and psychiatric hospitalization rates have declined in both the US and Europe (Holland et al., 2021; Menculini et al., 2021). Di Lorenzo et al. observed that between March 1, 2020 and August 31, 2020, the request for an urgent psychiatric visit in the ED decreased compared to the same period in 2019 from 602 observations to 476. However, during 2020, a significant increase in patients directed to the ED from psychiatric inpatient facilities was reported compared to the previous year due to an increase in serious conditions that were unmanageable on the territory such as suicidal behavior or maladaptive states with anxiety and aggression (Di Lorenzo et al., 2021). Capuzzi et al. reported that during the first wave of SARS-CoV-2 infection (March–May 2020), 225 emergency psychiatric consultations were performed, slightly more than half (58%) of the corresponding period in 2019 (388 emergency department accesses). Residence in a psychiatric facility (aOR = 1.78, p = 0.031), cannabis dependence (aOR = 1.76, p = 0.028) and diagnosis of obsessive-compulsive disorder (aOR = 10.94, p = 0.003) were all statistically significant predictors of emergency psychiatric consultation during quarantine (Capuzzi et al., 2020). However, both of these studies did not place the decrease in psychiatric admissions in the context of the reduction in general ED admissions observed during the first months of the pandemic, which would appear to be between 30 and 70% according to the different case studies (Boserup et al., 2020; Mantica et al., 2020).
The trend in absolute terms of the reduction of ED visits does not seem to be specific to the psychiatric condition alone (Holland et al., 2021). The pandemic led to a global reduction in ED admissions, especially for minor non-urgent conditions, which were drastically reduced, particularly in European and American EDs (Honeyford et al., 2021; Lucero et al., 2020). Thus, the previously reported data on the reduction of psychiatric accesses in EDs, not taking into account the overall reduction in accesses, do not seem to be able to provide precise indications on the real impact of acute psychiatric pathology collaterally caused by SARS-CoV-2 on EDs. Holland et al. in a study involving several American hospitals, extending the observation period to October 2020 and including nearly 190 million ED visits, noted that the decline in psychiatric visits was smaller than the decline in overall ED visits and that, at their lowest point, psychiatric visit requests were down from the same period in 2019 by “only” 24% compared to a 43% decline in overall ED visits. Similar to our work, when the figure was reported as the rate of visits per 100,000 ED Visits in the US, the rates of ED visits for a psychiatric condition, suicide attempt and drug or opioid overdose exceeded the 2019 average rates and thanks to a significant increase in March 2020, remained higher throughout the study period (Holland et al., 2021). The standardization of psychiatric accesses with general accesses thus seems to suggest that acute psychiatric pathology had a non-negligible impact on EDs involved in fighting the pandemic and may have contributed to the many management and health difficulties experienced by EDs during the most complex moments of the pandemic.
The increase in psychiatric rates in ED at the outbreak of the pandemic, which continued for the following months of the pandemic and was also reported by our study, can be explained by the overall effects of the pandemic on both the psychological and social spheres (Ferrando et al., 2021; Gunnell et al., 2020). Patients with pre-existing bipolar disorders, facilitated by isolation or loss of reference points caused by the reduction of community care activities, may have manifested imbalances and increased suicidal ideation (Gunnell et al., 2020; Vindegaard and Benros, 2020). The occurrence of self-injurious urges may also have occurred in previously unknown patients due mainly to the side effects of the pandemic on work and family status (Chen et al., 2021; Gunnell et al., 2020). As previous research after other human catastrophes has shown, job loss and the inability to plan for the future can cause non-negligible long-term effects on mental health and could explain the increasing trends observed in our study (Holland et al., 2021). The uncertainties created by the pandemic, together with the lack of access to social networks, education, and health services, may have worsened the level of personality functioning. As a consequence, in anxious individuals, this may have been the cause of panic reactions and, in individuals with emotional regulation difficulties, of acting out and aggression reactions with the increased need for sedation in the ED (Al Majali & Alghazo, 2021; Pan et al., 2021). The present study confirms that, compared to the pre-pandemic period, patients with attempted suicide after the COVID-12 outbreak are younger and have a higher rate of depression, as reported in previous studies (Jia et al., 2022; Schwartz-Mette et al., 2022).
The current study presents some novelties. Similar to the work of Holland et al. the rate of psychiatric conditions in relation to general ED visits, as opposed to absolute trends, would seem to demonstrate a non-negligible role of psychiatric conditions in the ED during the pandemic (Holland et al., 2021). Second, the ITSAs made it possible to quantify acute psychiatric conditions in the ED caused by the pandemic in statistical terms and not only in terms of graphical displays. Third, trend assessments were carried out over the pandemic months allowing initial hypotheses to be drawn on possible future trends.
The study has some limitations. First, its monocentric nature could expose it to some biases related to the territory, the local management of psychiatric pathology, and the type of population considered. Second, no sub-analysis was conducted on the different psychiatric conditions. The study used a priori conditions to analyze the impact on ED, this being the main focus of the analysis. Third, data on the difference between known pre-pandemic and post-pandemic conditions are not available. Fourth, no data are available on the increase or decrease in psychiatric visits in territorial or ambulatory psychiatry services since the outbreak of the COVID-19 pandemic.
In conclusion, this study described changes in ED visit rates for acute psychiatric pathology, psychiatric hospitalizations suicide attempts, and the need for sedation in the ED, demonstrating a non-negligible impact of acute psychiatric pathology during an infectious pandemic phase that saw EDs at the constant forefront of the fight against the virus. However, extending the observation period and considering the deflections observed for other pathological conditions, it appears that COVID-19 has led to a significant increase in the acute psychiatric breakdown and that trends appear to be stable at higher levels than pre-pandemic. The results of this study underline the need for continued longitudinal surveillance to monitor the long-term impacts of COVID-19.
CRediT author statement
Gianni Turcato: Conceptualization, Methodology, Data curation, Investigation, Supervision, Formal analysis Writing- Reviewing and Editing. Arian Zaboli: Methodology, Data curation, Formal analysis, Writing- Reviewing and Editing. Antonio Lucchetti: Investigation. Francesca Sighele: Investigation. Serena Sibilio: Investigation. Candelaria Donato: Investigation. Norbert Pfeifer: Investigation. Francesco Brigo: Conceptualization, Methodology, Data curation, Investigation, Supervision, Writing- Reviewing and Editing.
5. Funding information
No funding was provided for this work.
Declaration of competing interest
There is no conflict of interests.
References
- Al Majali S.A., Alghazo E.M. Mental health of individuals who are deaf during COVID-19: depression, anxiety, aggression, and fear. J. Community Psychol. 2021;49(6):2134–2143. doi: 10.1002/jcop.22539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernal J.L., Cummins S., Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int. J. Epidemiol. 2017;46(1):348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biglan A., Ary D., Wagenaar A.C. The value of interrupted time-series experiments for community intervention research. Prev. Sci. 2000;1(1):31–49. doi: 10.1023/a:1010024016308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boserup B., McKenney M., Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am. J. Emerg. Med. 2020;38(9):1732–1736. doi: 10.1016/j.ajem.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capuzzi E., Di Brita C., Caldiroli A., Colmegna F., Nava R., Buoli M., et al. Psychiatric emergency care during Coronavirus 2019 (COVID 19) pandemic lockdown: results from a Department of Mental Health and Addiction of northern Italy. Psychiatr. Res. 2020;293:113463. doi: 10.1016/j.psychres.2020.113463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Zhu L.J., Fang Z.M., Wu N., Du M., Jiang M., et al. The association of suicidal ideation with family characteristics and social support of the first batch of students returning to a college during the COVID-19 epidemic period: a cross sectional study in China. Front. Psychiatr. 2021;12:653245. doi: 10.3389/fpsyt.2021.653245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colaizzi J. Seclusion & restraint: a historical perspective. J. Psychosoc. Nurs. Ment. Health Serv. 2005;43(2):31–37. doi: 10.3928/02793695-20050201-07. [DOI] [PubMed] [Google Scholar]
- Di Lorenzo R., Frattini N., Dragone D., Farina R., Luisi F., Ferrari S. Psychiatric emergencies during the covid-19 pandemic: a 6-month observational study. Neuropsychiatric Dis. Treat. 2021;17:1763–1778. doi: 10.2147/NDT.S307128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrando S.J., Klepacz L., Lynch S., Shahar S., Dornbush R., Smiley A., et al. Psychiatric emergencies during the height of the COVID-19 pandemic in the suburban New York City area. J. Psychiatr. Res. 2021;136:552–559. doi: 10.1016/j.jpsychires.2020.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatr. 2020;63(1):32. doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flament J., Scius N., Zdanowicz N., Regnier M., De Cannière L., Thonon H. Influence of post-COVID-19 deconfinement on psychiatric visits to the emergency department. Am. J. Emerg. Med. 2021;48:238–242. doi: 10.1016/j.ajem.2021.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fountoulakis K.N., Karakatsoulis G., Abraham S., Adorjan K., Ahmed H.U., Alarcòn R.D., et al. Results of the COVID-19 mental health international for the general population (COMET-G) study. Eur. Neuropsychopharmacol. 2021;54:21–40. doi: 10.1016/j.euroneuro.2021.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatr. 2020;7(6):468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Håkansson A., Grudet C. Decreasing psychiatric emergency visits, but stable Addiction emergency visits, during COVID-19-A time series analysis 10 Months into the pandemic. Front. Psychiatr. 2021;12:664204. doi: 10.3389/fpsyt.2021.664204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamlin P.G. John CONOLLY, psychiatric pioneer. Dis. Nerv. Syst. 1963;24:230–233. [PubMed] [Google Scholar]
- Holland K.M., Jones C., Vivolo-Kantor A.M., Idaikkadar N., Zwald M., Hoots B., et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatr. 2021;78(4):372–379. doi: 10.1001/jamapsychiatry.2020.4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatr. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honeyford K., Coughlan C., Nijman R.G., Expert P., Burcea G., et al. Changes in emergency department activity and the first COVID-19 lockdown: a cross-sectional study. West. J. Emerg. Med. 2021;22(3):603–607. doi: 10.5811/westjem.2021.2.49614. Published 2021 May 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia R., Ayling K., Chalder T., Massey A., Gasteiger N., Broadbent E., et al. The prevalence, incidence, prognosis and risk factors for symptoms of depression and anxiety in a UK cohort during the COVID-19 pandemic. BJPsych Open. 2022;8(2):e64. doi: 10.1192/bjo.2022.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H.K., Carvalho A.F., Gratzer D., Wong A.H.C., Gutzin S., Husain M.I., et al. The impact of COVID-19 on psychiatric emergency and inpatient services in the first month of the pandemic in a large urban mental health hospital in Ontario, Canada. Front. Psychiatr. 2021;12:563906. doi: 10.3389/fpsyt.2021.563906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohls E., Baldofski S., Moeller R., Klemm S.L., Rummel-Kluge C. Mental health, social and emotional well-being, and perceived burdens of university students during COVID-19 pandemic lockdown in Germany. Front. Psychiatr. 2021;12:643957. doi: 10.3389/fpsyt.2021.643957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucero A.D., Lee A., Hyun J., Lee C., Kahwaji C., Miller G., et al. Underutilization of the emergency department during the COVID-19 pandemic. West. J. Emerg. Med. 2020;21(6):15–23. doi: 10.5811/westjem.2020.8.48632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantica G., Riccardi N., Terrone C., Gratarola A. Non-COVID-19 visits to emergency departments during the pandemic: the impact of fear. Publ. Health. 2020;183:40–41. doi: 10.1016/j.puhe.2020.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menculini, G., Tortorella, A., Albert, U., Carmassi, C., Carrà, G., Cirulli, F., et al. Access to mental health care during the first wave of the COVID-19 pandemic in Italy: results from the COMET multicentric study. Brain Sci.. 11(11):1413. [DOI] [PMC free article] [PubMed]
- Pan K.Y., Kok A.A.L., Eikelenboom M., Horsfall M., Jörg F., Luteijn R.A., et al. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. Lancet Psychiatr. 2021;8(2):121–129. doi: 10.1016/S2215-0366(20)30491-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pikkel Igal Y., Meretyk I., Darawshe A., Hayek S., Givon L., Levy A., et al. Trends in psychiatric emergency department visits in northern Israel during the COVID-19 outbreak. Front. Psychiatr. 2021;12:603318. doi: 10.3389/fpsyt.2021.603318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz-Mette R.A., Duell N., Lawrence H.R., Balkind E.G. COVID-19 distress impacts adolescents' depressive symptoms, NSSI, and suicide risk in the Rural, Northeast US. J. Clin. Child Adolesc. Psychol. 2022;1–14 doi: 10.1080/15374416.2022.2042697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon J., Helter T.M., White R.G., van der Boor C., Łaszewska A. Impacts of the Covid-19 lockdown and relevant vulnerabilities on capability well-being, mental health and social support: an Austrian survey study. BMC Publ. Health. 2021;21(1):314. doi: 10.1186/s12889-021-10351-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]