Abstract
Background
Germ cell tumor survival rates have improved over the past few decades. However, there is a lack of data on survival rates and the incidence of female germ cell tumors. This study aims to determine the incidence and survival rates of female germ cell tumors in our institution.
Methodology
This retrospective cross-sectional study was carried out at Shaukat Khanum Memorial Hospital and Research Centre, and the records over 10 years, from January 2010 to December 2020 were examined. The data of 290 females with malignant germ cell tumors were selected from 1387 females with ovarian masses, and their survival records were examined. For statistical analysis, SPSS software (version 24.0; IBM Corp. Armonk, NY) was utilized. The survival analysis was determined using the Kaplan-Meier method.
Results
The mean age of patients was 21.45 ± 9.28 years. The mean duration of diagnosis was 4.53 ± 2.59 years. In 245 (84.5%) patients, ovarian malignancy was involved while uterine malignancy was observed in 44 (15.2%) cases and there was one (0.3%) case of cervical carcinoma. The most common stage at diagnosis of malignancy was IA (96 (33.1%)), followed by IIIC (58 (20.0%)), IV (56 (19.3%)) and IC (26 (9.0%)). Chemotherapy was given in 244 (84.1%) cases. Out of 290 cases, 26 (9.0%) had a recurrence of the tumor while 264 (91.0%) did not have a recurrence of the tumor. Out of 290 cases, 46 (15.9%) died during follow-up, 129 (44.4%) had disease-free survival while 115 (39.7%) were healthy till the end of the study. The mean duration of survival was 3.56 ± 2.33 years. When patients' survival was compared between treatment groups, patients who did not receive chemotherapy fared better than those who did.
Conclusion
Female germ cell tumor patients have a good overall survival rate of more than 20% after 10 years of follow-up with effective adjuvant therapy and conservative surgery. However, more research is needed to determine the long-term effects of chemotherapy on ovarian function.
Keywords: uterine malignancy, survival, ovarian carcinoma, malignant germ cell tumor, chemotherapy
Introduction
Germ cell tumors are heterogeneous benign or malignant neoplasms that arise in the gonadal and midline extragonadal organs [1]. Ovarian germ cell tumors make up 20-25% of all ovarian neoplasms in females, however, only 3-5% of them are cancerous [2-3]. Dysgerminoma, yolk sac tumors, mixed germ cell tumors, and immature teratomas account for more than 90% of all malignant germ cell tumors. The remaining 5-10% of cell types are embryonic cancer, choriocarcinoma, and polyembryoma, which are rarely observed in pure form and have a poor prognosis [3-4].
Seminomas, which include testicular seminomas and ovarian dysgerminomas, and non-seminomas, which include histologic subtypes of yolk sac tumors, teratomas, embryonal carcinomas, and choriocarcinomas, are the two categories of germ cell tumors. Females are more likely than males to develop germ cell tumors, which are normally benign (mature teratomas or "dermoid" tumors) (0.8:1 male-to-female ratio) [5-6].
At the time of diagnosis, ovarian malignant germ cell tumors are typically big and progress quickly. Abdominal pain (87%) and an abdominal mass are the most common symptoms in adolescence (85%). Acute abdomen is seen in about 10% of patients as a result of torsion, bleeding, or tumor rupture. Abdominal distention, fever, and vaginal bleeding are less common symptoms. Symptoms are usually brief, lasting 2-4 weeks on average [7].
Ovarian malignant germ cell tumors are generally unilateral, although, in about 4.3% of patients, they might be bilateral. With pure non-dysgerminoma cell lines, bilaterality is more common in dysgerminomas and mixed germ cell tumors [8-9]. Germ cell tumor survival rates have improved considerably during the last three decades, coinciding with more aggressive surgical staging and combined modality. Germ cell tumors make for a substantially bigger proportion of ovarian neoplasms in Asia and Africa (6% of all cancers) while epithelial ovarian carcinoma is less common [10-12].
The primary treatment for most germ cell tumors is surgery. The type of surgery depends on the location and stage of the tumor. In some cases, adjuvant chemotherapy may be recommended. If the tumor has spread to other parts of the body, chemotherapy may be the primary treatment. In some cases, radiation therapy may be used. The survival of these tumors has improved considerably since the introduction of platinum-based chemotherapy in the 1980s, with five-year survival rates of 90% recorded. Gonadal cancers have also been shown to have a better prognosis than extragonadal malignancies [13]. Trends in malignant female germ cell cancers, particularly in Asian races, are poorly understood. The goal of this research was to look at trends in the incidence and survival rates of malignant ovarian germ cell tumors in the South East Asian population. This study aimed to evaluate the 10-year survival of malignant germ cell tumors in the reproductive system of females.
Materials and methods
Study design
This was a retrospective, cross-sectional, single-institution experience.
Study setting
The study was conducted in Shaukat Khanum Memorial Hospital and Research Centre after approval from the institutional review board of Shaukat Khanum Memorial Cancer Hospital and Research Center vide letter no. Ex-17-05-21-01.
Study duration
The data for 10 years, i.e., January 2010 to December 2020, were explored.
Inclusion criteria
Females diagnosed with primary malignant germ cell tumors on histopathology were included.
Exclusion criteria
Females with non-primary malignant germ cell tumors were excluded.
Sample size
The data of 1387 females were included, as it was a time-based retrospective study.
Data collection procedure
The records of 1387 females diagnosed with ovarian masses were explored and 290 females (20.9%) females diagnosed with primary malignant germ cell tumors on histopathology were included. The data of the patients, including age, duration of diagnosis, primary tumor site, histologic subtype, treatment given, and recurrence and survival during follow-up were noted. Five and ten-years survival rates were calculated and disease-free survival was noted as survival without progression, recurrence, and death.
Statistical analysis
The data were entered and analyzed using SPSS software (version 24; IBM Corp., Armonk, IBM). Quantitative variables, i.e., age, duration of disease, and duration of survival, have been presented as mean and standard deviation. Categorical variables, i.e., gender, age groups, year-wise disease distribution, tumor grades, treatment given (chemotherapy given or not), recurrence, and survival of the patient, have been presented as frequency and percentage. Survival rate as determined by using the Kaplan-Meier method. P-value ≤ 0.05 was considered significant.
Results
In this study, the mean age of patients was 21.45 ± 9.28 years. Out of 290 cases, eight (2.8%) were aged <5 years while the maximum numbers of patients fall in the age group 20-40 years, which is the reproductive age group. The mean duration of diagnosis was 4.53 ± 2.59 years. The maximum number of patients were enrolled during the period 2012 to 2018. In 245 (84.5%) patients, ovarian malignancy was involved while uterine malignancy was observed in 44 (15.2%) cases and there was one (0.3%) case of cervical carcinoma. The most common stage at diagnosis of malignancy was IA (96 (33.1%)), followed by IIIC (58 (20.0%)), IV (56 (19.3%)), and IC (26 (9.0%)). Chemotherapy was given in 244 (84.1%) cases while in 46 (15.9%) cases, no chemotherapy was given (Table 1).
Table 1. Baseline characteristics of females.
| Mean ± SD, f (%) | |
| n | 290 |
| Age (years) | 21.45 ± 9.28 |
| Age group | |
| <5 years | 8 (2.8%) |
| 6-10 | 24 (8.3%) |
| 11-19 | 97 (33.4%) |
| 20-40 | 147 (50.7%) |
| 41-55 | 14 (4.8%) |
| Diagnosis of disease | |
| 2010 | 1 (0.3%) |
| 2011 | 20 (6.9%) |
| 2012 | 24 (8.3%) |
| 2013 | 25 (8.6%) |
| 2014 | 36 (12.4%) |
| 2015 | 42 (14.5%) |
| 2016 | 36 (12.4%) |
| 2017 | 37 (12.8%) |
| 2018 | 33 (11.4%) |
| 2019 | 9 (3.1%) |
| 2020 | 27 (9.3%) |
| Mean duration of disease | 4.53 ± 2.59 |
| Site of tumor | |
| Ovary | 245 (84.5%) |
| Uterus | 44 (15.2%) |
| Cervix | 1 (0.3%) |
| Grade of tumor | |
| I | 2 (0.7%) |
| IA | 96 (33.1%) |
| IB | 9 (3.1%) |
| IC | 26 (9.0%) |
| II | 4 (1.4%) |
| IIA | 3 (1.0%) |
| IIB | 3 (1.0%) |
| IIC | 7 (2.4%) |
| III | 19 (6.6%) |
| IIIA | 3 (1.0%) |
| IIIB | 4 (1.4%) |
| IIIC | 58 (20.0%) |
| IV | 56 (19.3%) |
| Treatment given | |
| Chemotherapy | 244 (84.1%) |
| No chemotherapy given | 46 (15.9%) |
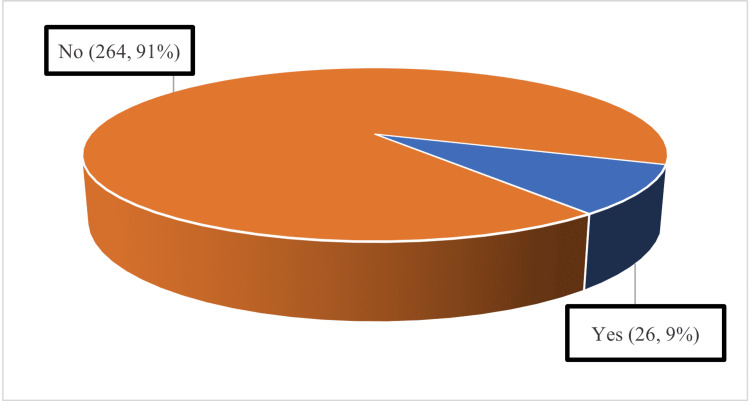
Out of 290 cases, 26 (9.0%) had a recurrence of the tumor while 264 (91.0%) did not have a recurrence of the tumor (Figure 1).
Figure 1. Recurrence of disease after treatment during follow-up.
Out of 290 cases, 46 (15.9%) died during follow-up, 129 (44.4%) had disease-free survival while 115 (39.7%) were fine till the end of the study. The mean duration of survival was 3.56 ± 2.33 years. When the survival of patients was compared in the treatment groups, the survival of patients who did not receive chemotherapy was better than in patients who received chemotherapy (Table 2).
Table 2. Survival of patients during follow-up.
| F (%) | |
| Death | 46 (15.9%) |
| Disease-free survival or Relative survival till the end of the study | 244 (84.1%) |
| Survived up to | |
| 2011 | 1 (0.3%) |
| 2012 | 7 (2.4%) |
| 2013 | 6 (2.1%) |
| 2014 | 6 (2.1%) |
| 2015 | 10 (3.4%) |
| 2016 | 16 (5.5%) |
| 2017 | 23 (7.9%) |
| 2018 | 27 (9.3%) |
| 2019 | 32 (11.0%) |
| 2020 | 32 (11.0%) |
| 2021 | 130 (44.8%) |
| Duration of survival | 3.56 ± 2.33 |
Discussion
Germ cell cancers of the ovary can be cured and treated successfully. Chemotherapy's long-term effects on long-term survivors remain unknown, although these patients can expect to live normally. Early detection and multi-agent chemotherapy are linked to high cure rates of 85.6 percent (range 81.2-90.0%) in female malignant ovarian germ cell tumors [14-15]. Although male germ cell tumors, which are 20 times more common than malignant ovarian germ cell tumors, share many similarities, women who recur with this malignancy have a worse prognosis [16].
Germ cell tumors are more likely to affect adolescents and women of reproductive age [17]. As in our study, we observed that the mean age of patients was 21.45 ± 9.28 years. Out of 290 cases, the maximum number of patients falls in the age group 20-40 years, which is the reproductive age group.
In our study, we observed that ovarian malignancy was involved in 245 (84.5%) patients while uterine malignancy was noted in 44 (15.2%) cases, and there was only one (0.3%) case of cervical carcinoma. The most common stage at diagnosis of malignancy was IA (96 (33.1%)), followed by IIIC (58 (20.0%)), IV (56 (19.3%)), and IC (26 (9.0%)). Chemotherapy was given in 244 (84.1%) cases. Out of 290 cases, 26 (9.0%) had a tumor recurrence, while 264 (91.0%) did not have a recurrence of the tumor. Out of 290 cases, 46 (15.9%) died during follow-up, 129 (44.4%) had disease-free survival, and 115 (39.7%) were fine till the end of the study. The mean duration of survival was 3.56 ± 2.33 years. When the survival of patients was compared in treatment groups, the survival of patients who did not receive chemotherapy was better than patients who received chemotherapy.
Except for dysgerminoma, for which the incidence of bilaterality is 10-15%, bilateral ovarian germ cell tumors are exceedingly rare [18]. In our study, dysgerminoma was detected in 31.7% of cases with choriocarcinoma in 16.2% cases, immature teratoma in 9.7%, and malignant teratoma in 1.0% cases while yolk sac tumor was detected in 22.4% cases. Several studies have shown that normal reproductive function can be maintained without jeopardizing survival [19-20].
While chemotherapy can damage ovarian function and cause ovarian or premature ovarian failure, most women who receive platinum-based therapy for three or four cycles regain normal ovarian function, and fertility is often preserved in this group [21-23]. In another cohort of 71 patients treated with fertility-sparing surgery and combination chemotherapy, the impact of platinum-based chemotherapy on adult women's ovarian function was documented (including cisplatin and bleomycin). Sixty-two (87%) of these women were able to resume regular menstruation, and 24 of them went on to have 37 offspring [24].
The function of vigorous cytoreduction in advanced illness is unclear, and removing both ovaries does not improve the result. Combining bleomycin, etoposide, and cisplatin is considered the gold standard for adjuvant therapy. Studies of ovarian and reproductive ability after conservative surgery and chemotherapy for malignant ovarian germ-cell tumors have repeatedly shown that these women have an excellent prognosis, with regular menstrual function and fertility rates returning with no increased risk of teratogenicity [25]. Because of the physiological similarities between ovarian and testicular germ cell tumors, Tewari claims that the evolution of systemic treatment for ovarian germ cell cancer has matched advances in the treatment of testicular germ cell cancers [26].
Moreover, all data showed that most women with ovarian germ cell cancers have an excellent survival rate of 93% with effective adjuvant therapy (chemotherapy) and conservative surgery [26-27]. After treatment, they will keep their menstruation and reproductive capacity [27]. According to Joliniere et al., the efficacy of chemotherapy allowed for conservative surgery, such as unilateral salpingo-oophorectomy, while preserving fertility. Chemotherapy was indicated for non-dysgerminoma tumors following surgical staging and debulking. The type of tumor and its histological features influenced the treatment options [28].
There were certain limitations to our study. First, this was a retrospective study with a small sample size. Second, we did not have data on the use of fertility-sparing therapy or on the long-term effects of chemotherapy on ovarian function or secondary malignancies. Third, our study was based on a single institution's experience and may not be generalizable to other centers.
Conclusions
Overall survival was good during the 10-year follow-up period, with a rate of over 20%. Chemotherapy has improved the outcome of many carcinomas thanks to advances in research, science, and technology. However, we found contradictory results in this study, which could be due to advanced-stage disease at chemotherapy initiation. Further research with larger sample size and other parameters that may affect female survival should be conducted.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. Institutional Review Board, Shaukat Khanum Memorial Cancer Hospital & Research Center issued approval Ex-17-05-21-01. Institutional Review Board (IRB) of Shaukat Khanum Memorial Cancer Hospital 8 Research Center (SKMCHtRC) has reviewed your application for grant of exempt status to the research study titled, "Incidence and Survival Rates for Female Malignant Germ Cell Tumors: An Institutional Review" IRB assessment: • IRB considers the fact that all clinical information to be studied in this study already exists in medical/hospital records. • IRB further considers that this information will be recorded on the data extra¢tion sheet in such a manner that subjects cannot be identified directly or indirectly through the use of codes. • On the basis of the above, IRB grants you an exemption for the above-mentioned research study. The exemption is limited to activities described in IRB approved proposal. Conditions for the general conduct of human subject research are detailed on the attached sheet. The IRB review process of SKMCH&RC is in compliance with ICH-GCP Guidelines. We appreciate your continued commitment to the protection of human research subjects. • Please be advised that Exemption status is granted as IRB believes that no more than minimal risk is involved since private information of human subjects is recorded without any identifiers and the resulting research data set is completely anonymous (data set cannot be linked back to individuals), hence research would not impact the well-being of research participants. Whereas if by any means the research data can be possibly linked back to individuals, research would not fall in the exempt category. If you feel any difficulty in determining if the data is sufficiently de-identified or not, you are encouraged to contact secretary IRB. IRB also grants you a waiver of informed consent as requested
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Germ cell tumours in children and adolescents. Penn A, Jenney M, Nicholson JC. Paediatr Child Health. 2018;28:169–176. [Google Scholar]
- 2.Ovarian cancer, the revised FIGO staging system, and the role of imaging. Javadi S, Ganeshan DM, Qayyum A, Iyer RB, Bhosale P. AJR Am J Roentgenol. 2016;206:1351–1360. doi: 10.2214/AJR.15.15199. [DOI] [PubMed] [Google Scholar]
- 3.Aggressive neuroendocrine tumor of the ovary with multiple metastases treated with everolimus: a case report. Kaiho-Sakuma M, Toyoshima M, Watanabe M, et al. Gynecol Oncol Rep. 2018;23:20–23. doi: 10.1016/j.gore.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fertility sparing management in non-epithelial ovarian cancer. Which patients, what procedure and what outcome? Thomakos N, Malakasis A, Machairiotis N, Zarogoulidis P, Rodolakis A. J Cancer. 2018;9:4659–4664. doi: 10.7150/jca.26674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epidemiology of childhood cancer. Kaatsch P. Cancer Treat Rev. 2010;36:277–285. doi: 10.1016/j.ctrv.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 6.Childhood cancer burden: a review of global estimates. Bhakta N, Force LM, Allemani C, et al. Lancet Oncol. 2019;20:42–53. doi: 10.1016/S1470-2045(18)30761-7. [DOI] [PubMed] [Google Scholar]
- 7.Ovarian cancer, version 1.2016, NCCN clinical practice guidelines in oncology. Morgan RJ Jr, Armstrong DK, Alvarez RD, et al. J Natl Compr Canc Netw. 2016;14:1134–1163. doi: 10.6004/jnccn.2016.0122. [DOI] [PubMed] [Google Scholar]
- 8.Prognostic impact of laterality in malignant ovarian germ cell tumors. Mahdi H, Kumar S, Seward S, et al. Int J Gynecol Cancer. 2011;21:257–262. doi: 10.1097/IGC.0b013e31820581e5. [DOI] [PubMed] [Google Scholar]
- 9.Ovarian cancer incidence and survival by histologic type in Osaka, Japan. Ioka A, Tsukuma H, Ajiki W, Oshima A. Cancer Sci. 2003;94:292–296. doi: 10.1111/j.1349-7006.2003.tb01435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Histopathological patterns of ovarian tumors at BPKIHS. Pradhan A, Sinha A, Upreti D. Health Renaissance. 2012;10:87–97. [Google Scholar]
- 11.Incidence and outcomes of malignant ovarian germ cell tumors in Korea, 1999-2017. Park M, Lim J, Lee JA, et al. Gynecol Oncol. 2021;163:79–84. doi: 10.1016/j.ygyno.2021.07.037. [DOI] [PubMed] [Google Scholar]
- 12.Adjuvant therapy of completely resected dysgerminoma with carboplatin and etoposide: a trial of the Gynecologic Oncology Group. Williams SD, Kauderer J, Burnett AF, Lentz SS, Aghajanian C, Armstrong DK. Gynecol Oncol. 2004;95:496–499. doi: 10.1016/j.ygyno.2004.07.044. [DOI] [PubMed] [Google Scholar]
- 13.Trends in incidence and survival of pediatric and adolescent patients with germ cell tumors in the United States, 1975 to 2006. Poynter JN, Amatruda JF, Ross JA. Cancer. 2010;116:4882–4891. doi: 10.1002/cncr.25454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Survival and reproductive function after treatment of malignant germ cell ovarian tumors. Zanetta G, Bonazzi C, Cantù M, Binidagger S, Locatelli A, Bratina G, Mangioni C. J Clin Oncol. 2001;19:1015–1020. doi: 10.1200/JCO.2001.19.4.1015. [DOI] [PubMed] [Google Scholar]
- 15.Systemic anti-cancer treatment in malignant ovarian germ cell tumours (MOGCTs): current management and promising approaches. Uccello M, Boussios S, Samartzis EP, Moschetta M. Ann Transl Med. 2020;8:1713. doi: 10.21037/atm.2020.04.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malignant ovarian germ cell tumors: identification of novel prognostic markers and long-term outcome after multimodality treatment. Murugaesu N, Schmid P, Dancey G, et al. J Clin Oncol. 2006;24:4862–4866. doi: 10.1200/JCO.2006.06.2489. [DOI] [PubMed] [Google Scholar]
- 17.Ovarian malignant germ cell tumors: cellular classification and clinical and imaging features. Shaaban AM, Rezvani M, Elsayes KM, et al. Radiographics. 2014;34:777–801. doi: 10.1148/rg.343130067. [DOI] [PubMed] [Google Scholar]
- 18.Management of bilateral malignant ovarian germ cell tumors: experience of a single institute. Zhao T, Liu Y, Jiang H, Zhang H, Lu Y. Mol Clin Oncol. 2016;5:383–387. doi: 10.3892/mco.2016.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The influence of conservative surgical practices for malignant ovarian germ cell tumors. Chan JK, Tewari KS, Waller S, Cheung MK, Shin JY, Osann K, Kapp DS. J Surg Oncol. 2008;98:111–116. doi: 10.1002/jso.21079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.An analysis of prognostic factors in patients with ovarian malignant germ cell tumors who are treated with fertility-preserving surgery. Yang ZJ, Liu ZC, Wei RJ, Li L. Gynecol Obstet Invest. 2016;81:1–9. doi: 10.1159/000381771. [DOI] [PubMed] [Google Scholar]
- 21.Germ cell tumors of the ovary: an update. Nogales FF, Dulcey I, Preda O. Arch Pathol Lab Med. 2014;138:351–362. doi: 10.5858/arpa.2012-0547-RA. [DOI] [PubMed] [Google Scholar]
- 22.Reproductive function after conservative surgery and chemotherapy for malignant germ cell tumors of the ovary. Tangir J, Zelterman D, Ma W, Schwartz PE. Obstet Gynecol. 2003;101:251–257. doi: 10.1016/s0029-7844(02)02508-5. [DOI] [PubMed] [Google Scholar]
- 23.Reproduction beyond cancer: a message of hope for young women. Maltaris T, Boehm D, Dittrich R, Seufert R, Koelbl H. Gynecol Oncol. 2006;103:1109–1121. doi: 10.1016/j.ygyno.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 24.Reproductive and sexual function after platinum-based chemotherapy in long-term ovarian germ cell tumor survivors: a Gynecologic Oncology Group Study. Gershenson DM, Miller AM, Champion VL, Monahan PO, Zhao Q, Cella D, Williams SD. J Clin Oncol. 2007;25:2792–2797. doi: 10.1200/JCO.2006.08.4590. [DOI] [PubMed] [Google Scholar]
- 25.Malignant ovarian germ-cell tumours. Low JJ, Ilancheran A, Ng JS. Best Pract Res Clin Obstet Gynaecol. 2012;26:347–355. doi: 10.1016/j.bpobgyn.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 26.Malignant germ cell tumors of the ovary. Tewari K, Cappuccini F, Disaia PJ, Berman ML, Manetta A, Kohler MF. Obstet Gynecol. 2000;95:128–133. doi: 10.1016/s0029-7844(99)00470-6. [DOI] [PubMed] [Google Scholar]
- 27.Management of early ovarian cancer: germ cell and sex cord-stromal tumors. Gershenson DM. Gynecol Oncol. 1994;55:62–72. [PubMed] [Google Scholar]
- 28.Two case reports of a malignant germ cell tumor of ovary and a granulosa cell tumor: interest of tumoral immunochemistry in the identification and management. Bouquet de Jolinière J, Ben Ali N, Fadhlaoui A, et al. Front Oncol. 2014;4:97. doi: 10.3389/fonc.2014.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]