Abstract
Introduction
By identifying drivers of healthcare disparities, providers can better support high-risk patients and develop risk-mitigation strategies. Household income is a social determinant of health known to contribute to healthcare disparities. The present study evaluates the impact of household income on short-term morbidity and mortality following supratentorial meningioma resection.
Methods
A total of 349 consecutive patients undergoing supratentorial meningioma resection over a six-year period (2013-2019) were analyzed retrospectively. Primary outcomes were unplanned hospital readmission, reoperations, emergency department (ED) visits, return to the operating room, and all-cause mortality within 30 days of the index operation. Standardized univariate regression was performed across the entire sample to assess the impact of household income on outcomes. Subsequently, outcomes were compared between the lowest (household income ≤ $51,780) and highest (household income ≥ $87,958) income quartiles. Finally, stepwise regression was executed to identify potential confounding variables.
Results
Across all supratentorial meningioma resection patients, lower household income was correlated with a significantly increased rate of 30-day ED visits (p = 0.002). Comparing the lowest and highest income quartiles, the lowest quartile was similarly observed to have a significantly higher rate of 30-day ED evaluation (p = 0.033). Stepwise regression revealed that the observed association between household income and 30-day ED visits was not affected by confounding variables.
Conclusion
This study suggests that household income plays a role in short-term ED evaluation following supratentorial meningioma resection.
Keywords: social determinants of health, readmissions, outcomes, disparity, brain tumor
Introduction
The social determinants of health (SDOH) refer to the environmental, social, economic, and cultural factors, such as gender, race, socioeconomic status (SES), and education level, outside of the immediate medical setting, which impact a patient’s quality of health. The medical community has increasingly focused on the contribution of SDOH to healthcare disparities. Further, policies have been introduced that emphasize value-based care models, incentivizing the elimination of SDOH-related disparities to reduce avoidable costs.
In the surgical setting, SES has been previously demonstrated to predict postoperative outcomes across a wide range of populations. Within neurosurgery, previous studies have shown that low SES puts patients at risk for complications following multiple different procedures, from brain tumor resection to spinal surgery [1-5]. Given its broad impact, it, therefore, remains important to evaluate SES and identify outcome disparities in specific neurosurgical procedural populations.
Here, we evaluate the impact of SES on outcomes following supratentorial meningioma resection. Supratentorial meningiomas account for nearly half of all primary, non-malignant intracranial lesions [6]. Further, in contrast to other cranial tumors, supratentorial meningiomas have favorable histology and significant long-term survival with maximal safe resection [7-8]. Nonetheless, surgical resection bears an appreciable complication profile, including neurological deficits and seizures [9-10]. As such, the identification of patient characteristics that drive outcome disparities in this population is essential for developing risk-mitigation strategies.
Previous studies in meningioma patients have shown that lower SES is correlated with a decreased likelihood of resection and worse overall survival [11-12]. Further, the present authors observed that meningioma patients with lower household income experienced higher rates of Emergency Department evaluation within 90 days of resection [13]. However, few studies have evaluated morbidity and mortality specifically within the 30-day postoperative window. This time frame is meaningful to consider, as 30-day surgical outcomes are incorporated into multiple hospital grading scales and reimbursement models. The objective of the present study is to assess the effect of SES, specifically household income, on 30-day supratentorial meningioma resection outcomes.
Materials and methods
Sample selection
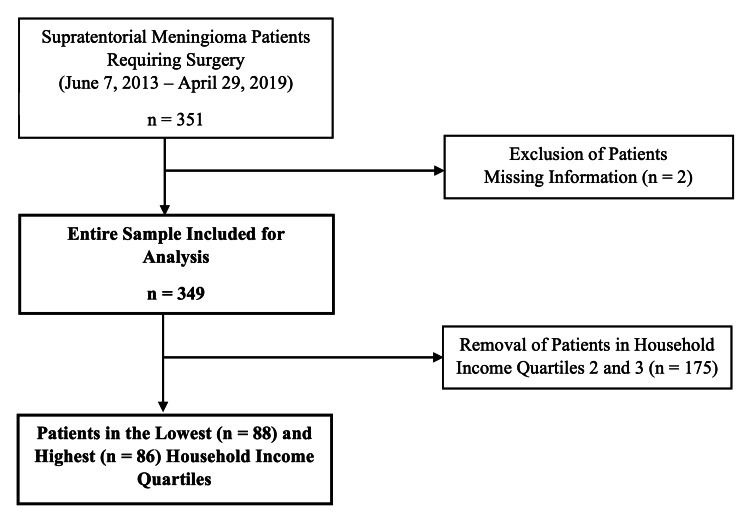
This study retrospectively enrolled 349 consecutive patients with complete health information who underwent supratentorial meningioma resection at a multi-hospital, 1659-bed university health system in Philadelphia, PA, USA, over a six-year period (June 7, 2013 - April 29, 2019) (Figure 1), as previously described by the present authors [13]. Data were acquired using the EpiLog tool - a non-proprietary data acquisition system layered on top of the electronic health record at the present institution to facilitate charting, workflow, quality improvement, and cost reduction initiatives [14].
Figure 1. Patient Selection.
Flowchart describing the selection of supratentorial meningioma cases across a six-year period
Data collection and statistical analysis
Patient characteristics and outcome data were extracted via EpiLog and pushed into defined spreadsheets. Recorded patient characteristics included age, race, gender, body mass index (BMI), zip code, American Society of Anesthesiologists (ASA) score, tobacco use within 12 months prior to surgery, Charlson Comorbidity Index (CCI) score, prior surgical history, total duration of surgery, total cost, and level of education. Household income was determined by cross-referencing patient zip codes with demographic data from the 2012-2016 U.S. Census Bureau 5-Year American Community report [15].
Outcomes included unplanned hospital readmission, reoperations, ED visits, return to the operating room, and all-cause mortality within 30 days of the index operation. Standardized univariate logistic regression was carried out across the entire sample to assess the impact of increasing household income on outcomes. Odds ratio (OR) < 1 indicates that the outcome was more likely with lower household income. Subsequently, patients were separated into quartiles based on household income, and univariate regression was repeated to compare outcomes between the lowest and highest income quartiles. OR < 1 indicates that the outcome was more likely in the lowest income quartile. Finally, a stepwise regression model, incorporating other recorded patient demographic variables, was used to identify potential confounders. For outcomes that had less than 5% of events occur (30-day reoperation and mortality), a Firth correction was applied to eliminate the small sample size bias This statistical analysis has previously been described by the present authors [1,5,13]. Significance for all analyses was set at a p-value < 0.05.
Results
Patient characteristics
Across all patients (n = 349), the mean age was 58.9 ± 14.2 years, mean BMI was 28.9 ± 6.3, and mean CCI score was 2.78 ± 2.33 (Table 1). Further, 63.0% were female and 12.6% reported prior tobacco use. The average household income was $70,608, ranging from $18,119 to $191,354.
Table 1. Patient Characteristics.
Patient demographics and baseline characteristics across the entire sample (n = 349), as well as between the lowest (Q1) and highest (Q4) household income quartiles
sd=standard deviation
| Variable | Entire Sample (n = 349) | Q1 (n = 88) | Q4 (n = 86) | Standardized Difference |
| Age, years, mean (sd) | 58.9 (14.2) | 57.0 (15.4) | 60.9 (13.5) | 0.27 |
| Gender, n (%) | 0.11 | |||
| Male | 129 (36.96) | 32 (36.36) | 36 (41.86) | |
| Female | 220 (63.04) | 56 (63.64) | 50 (58.14) | |
| Race, n (%) | 1.26 | |||
| Asian | 8 (2.29) | 2 (2.27) | 2 (2.33) | |
| Black/African American | 63 (18.05) | 38 (43.18) | 3 (3.49) | |
| White | 250 (71.63) | 38 (43.18) | 77 (89.53) | |
| Hispanic/Latino | 10 (2.87) | 5 (5.68) | 2 (2.33) | |
| Other | 18 (5.16) | 5 (5.68) | 2 (2.33) | |
| Tobacco Use within Past 12 Months, n (%) | 0.29 | |||
| Yes | 44 (12.61) | 14 (15.91) | 7 (8.14) | |
| No | 292 (83.67) | 71 (80.68) | 78 (90.70) | |
| Unknown | 13 (3.72) | 3 (3.41) | 1 (1.16) | |
| Body Mass Index, kg/m2, mean (sd) | 28.9 (6.3) | 30.0 (6.8) | 27.5 (5.5) | -0.40 |
| American Society of Anesthesiologists Grade, n (%) | 0.60 | |||
| 1 | 0 (0) | 0 (0) | 0 (0) | |
| 2 | 131 (37.54) | 19 (21.59) | 42 (48.84) | |
| 3 | 209 (59.89) | 66 (75.00) | 42 (48.84) | |
| 4 | 7 (2.01) | 3 (3.41) | 2 (2.33) | |
| Charlson Comorbidity Index Score, mean (sd) | 2.78 (2.33) | 2.88 (2.52) | 2.74 (2.08) | -0.06 |
| Surgeries within 90 Days Prior to Index Operation, n (%) | -0.07 | |||
| 0 | 331 (94.84) | 85 (96.59) | 84 (97.67) | |
| 1 | 17 (4.87) | 3 (3.41) | 2 (2.33) | |
| 2+ | 1 (0.29) | 0 (0) | 0 (0) | |
| Lifetimes Surgeries Prior to Index Operation, n (%) | 0.29 | |||
| 0 | 326 (93.41) | 79 (89.77) | 82 (95.35) | |
| 1 | 13 (3.71) | 5 (5.68) | 3 (3.49) | |
| 2+ | 8 (2.29) | 4 (4.56) | 1 (1.16) | |
| Length of Stay, hours, mean (sd) | 125.1 (133.8) | 150.2 (158.4) | 126.9 (149.1) | -0.15 |
| Total Cost, $, mean (sd) | 3054.37 (1528.88) | 3272.76 (1609.66) | 2940.17 (1373.36) | -0.22 |
| Duration of Surgery, minutes, mean (sd) | 217.1 (117.5) | 241.1 (131.1) | 214.8 (124.3) | -0.21 |
Patients in the lowest income quartile (Q1) had an income range from $18,119 - $51,780, while patients in the highest quartile (Q4) had an income range from $87,958 - $191,354. Additionally, there were more black/African American patients in Q1 (43%) than Q4 (3%) (Table 1).
Patient outcomes
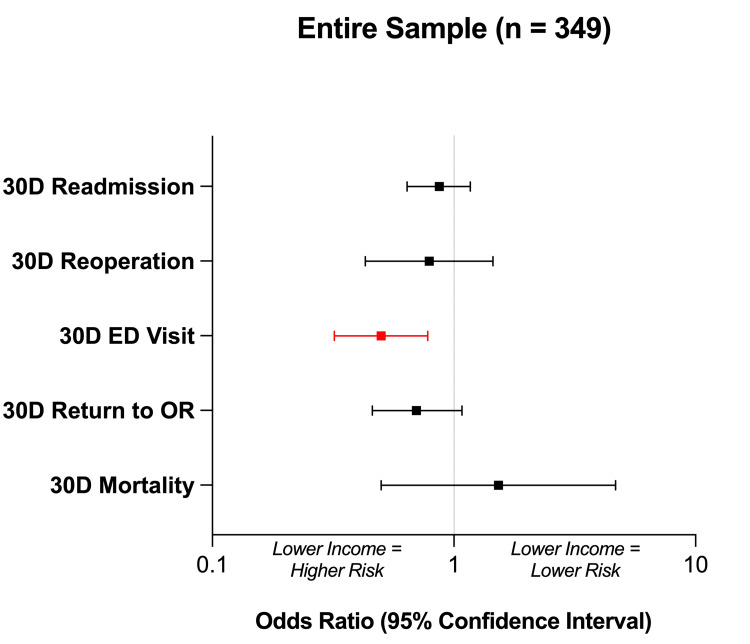
Across all patients (n = 349), univariate analysis revealed a significant, negative correlation between household income and 30-day rate of ED evaluation (p = 0.002, OR = 0.50) (Table 2, Figure 2). Further, a trend was observed between lower household income and increased 30-day return to the operating room; however, this trend was not statistically significant (p = 0.10, OR = 0.70). No associations were seen between household income and 30-day readmission (p = 0.36) or reoperation (p = 0.44). Across all patients, there was only a single recorded mortality event within 30 days (overall rate 0.29%). No correlation was demonstrated between household income and 30-day mortality (p = 0.46).
Table 2. Patient Outcomes.
Standardized univariate logistic regression was carried out on the entire sample (n = 349) to assess the impact of increasing household income on outcomes (left columns). Subsequently, univariate logistic regression was executed to compare outcomes between the lowest (Q1; n = 88) and highest (Q4; n = 86) household income quartiles (right columns). An odds ratio of < 1 indicates that the outcome was more likely with lower household income. Bolded values denote statistical significance at p < 0.05.
CI=confidence interval, ED=emergency department, OR=odds ratio
| Outcome | Entire Sample | Q1 vs Q4 | |||||
| n (%) | OR (95% CI) | P-value | Q1, n (%) | Q4, n (%) | OR (95% CI) | P-value | |
| 30-Day Readmission | 56 (16.05) | 0.87 (0.64-1.17) | 0.36 | 19 (21.59) | 14 (16.28) | 0.71 (0.33-1.52) | 0.37 |
| 30-Day Reoperation | 12 (3.44) | 0.79 (0.43-1.45) | 0.44 | 4 (4.55) | 2 (2.33) | 0.56 (0.20-1.69) | 0.47 |
| 30-Day ED Visit | 33 (9.46) | 0.50 (0.32-0.78) | 0.002 | 13 (14.77) | 4 (4.65) | 0.28 (0.09-0.90) | 0.033 |
| 30-Day Return to the Operating Room | 29 (8.31) | 0.70 (0.46-1.08) | 0.10 | 10 (11.36) | 6 (6.98) | 0.59 (0.20-1.69) | 0.32 |
| 30-Day Mortality | 1 (0.29) | 1.53 (0.50-4.67) | 0.46 | 0 (0) | 0 (0) | N/A | N/A |
Figure 2. Entire Sample Outcomes.
Forest plot demonstrating standardized univariate logistic regression across the entire sample (n = 349) to assess the impact of increasing household income on outcomes. An odds ratio of < 1 indicates that the outcome was more likely with a lower household income. Red values denote statistical significance at p < 0.05.
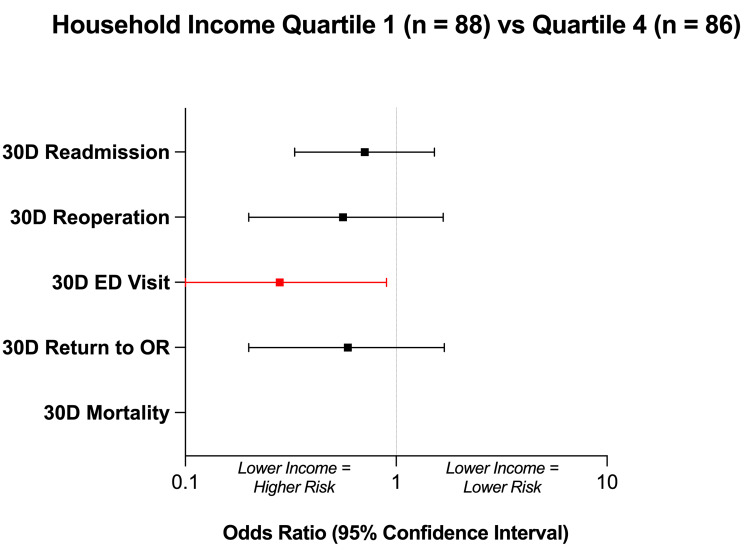
Comparing Q1 and Q4, the lowest income quartile was revealed to have a significantly increased 30-day rate of ED evaluation (p = 0.033, OR = 0.28) (Table 2, Figure 3). However, no differences in 30-day readmission (p = 0.37), reoperation (p = 0.47), or return to the operating room (p = 0.32) rates were observed between Q1 and Q4. No mortality events occurred in Q1 or Q4, so an inter-quartile comparison of 30-day mortality was not conducted.
Figure 3. Household Income Quartile Outcomes.
Forest plot comparing outcomes between the lowest (Quartile 1; n = 88) and highest (Quartile 4; n = 86) household income quartiles. An odds ratio of < 1 indicates that the outcome was more likely in the lowest household income quartile. Red values denote statistical significance at p < 0.05.
Stepwise regression
The observed association between household income and 30-day ED evaluation was not affected by any confounding variables. Conversely, the 30-day readmission rate was confounded by education level and CCI score. Additionally, the 30-day reoperation rate was confounded by CCI score, and the 30-day rate of return to the operating room was confounded by race, CCI score, and ASA grade. Finally, the 30-day mortality rate was affected by a history of prior surgery within 90 days.
Discussion
In this study, we assessed the impact of household income on short-term morbidity/mortality measures across 349 consecutive supratentorial meningioma resection patients. In both the entire sample and inter-quartile analyses, lower income was significantly correlated with increased ED visits within 30 days of the index operation. No additional associations were observed between household income and our other primary outcomes. Finally, only one mortality event was recorded within the 30-day postoperative window, with no mortalities in either the Q1 or Q4 subgroup, consistent with previously published meningioma outcome data indicating rates of 30-day mortality less than 10% [16-17].
The present authors previously observed that lower household income predicted increased 90-day ED evaluation following supratentorial meningioma resection [13]. In contrast to the previous study, here we focused our analysis on the 30-day window following the index operation. This time frame was an intentional feature of our study design, as outcomes within 30 days of surgery may be factored into surgical reimbursement and hospital ratings. Our study demonstrates that household income independently predicts short-term ED evaluation following meningioma resection. This finding may be explained by several factors, including differences in insurance status, geographic barriers to outpatient care facilities, and social factors (including diet or substance use/abuse) [18-19]. For instance, low-income and uninsured patients often rely on emergency facilities for primary evaluation, which may be reflected in our results [20]. In contrast, household income was not correlated to other adverse events following supratentorial meningioma resection. These negative findings may reflect the comparably low complication rate and favorable long-term prognosis in this population [21-22]. Meningiomas are characterized by their benign pathology and slow progression, which lead to favorable morbidity and mortality postoperatively [23-24].
The results of the present study are immediately applicable to patients, providers, and healthcare systems. Moving forward, strategies are needed to identify and support high-risk meningioma patients. Household income, and other important patient characteristics, may be incorporated into models to predict adverse outcomes [25]. Further, tailored preoperative education, regularly scheduled outpatient visits, and immersive social work involvement may help reduce ED utilization, as well as curb healthcare costs [26-28]. Future, prospective work ought to leverage our findings to mitigate income-related healthcare disparities.
Limitations
One limitation is that this study is retrospective, opening the possibility of sampling bias and data inaccuracies. Further, outcome data were collected via the electronic medical record, potentially underreporting adverse events that occurred outside the primary health system. However, all patients received follow-up beyond the 30-day postoperative window (median follow-up of 700 days), and during each outpatient visit, patients were asked about encounters at other health systems. Also, any discrepancies would be expected to be consistent across all subjects, maintaining the internal validity of our study.
Another limitation is that this study indirectly extracted household income from patient zip code instead of directly recording patient income status. Nonetheless, previous studies have demonstrated that zip-level median household income is effective for detecting health outcome differences [29].
Finally, other important patient characteristics may confound the present results. Here, we utilized stepwise analysis to identify such confounders among multiple recorded patient characteristics known to impact surgical outcomes. We observed that the 30-day rate of ED evaluation was not confounded by any other variables, indicating a robust and independent correlation. Nonetheless, further studies using matched cohorts may better isolate the relationship between income and outcomes to corroborate the present findings.
Conclusions
By identifying patient characteristics that underlie outcome disparities, providers can better support the highest-risk patients. Our results suggest that household income can predict ED utilization within the short-term postoperative window following supratentorial meningioma resection. Future, dedicated studies are needed to examine the impact of income on other neurosurgical populations, as well as to develop interventions that improve patient outcomes and eliminate income-related healthcare disparities.
Acknowledgments
We would like to thank The EpiLog Project and The Bernadette and Kevin and Bernadette McKenna Family Research Fund.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. IRB at the University of Pennsylvania issued approval 832794. This study was approved by the IRB at the University of Pennsylvania. IRB number for this study is: 832794. A waiver of informed consent was granted by the University of Pennsylvania IRB, as this study was considered to be minimal risk to patients. All ethical guidelines and rules were followed to protect patient privacy
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.The impact of household economics on short-term outcomes in a posterior fossa tumor population. Blue R, Dimentberg R, Detchou DK, Glauser G, Shultz K, McClintock S, Malhotra NR. Cureus. 2020;12:0. doi: 10.7759/cureus.8968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Household income is associated with return to surgery following discectomy for far lateral disc herniation. Borja AJ, Connolly J, Kvint S, et al. J Neurosurg Sci. 2021;[Epub] doi: 10.23736/S0390-5616.21.05246-2. [DOI] [PubMed] [Google Scholar]
- 3.Sociodemographic characteristics predict readmission rates after lumbar spinal fusion surgery. Chen SA, White RS, Tangel V, Nachamie AS, Witkin LR. Pain Med. 2020;21:364–377. doi: 10.1093/pm/pny316. [DOI] [PubMed] [Google Scholar]
- 4.Survival disparity based on household income in 1970 patients following brain tumor surgery. Glauser G, Dimentberg R, Shultz K, McClintock SD, Malhotra NR. World Neurosurg. 2020;143:0–21. doi: 10.1016/j.wneu.2020.07.016. [DOI] [PubMed] [Google Scholar]
- 5.The role of socioeconomic status on outcomes following cerebellopontine angle tumor resection. Huang V, Miranda SP, Dimentberg R, Glauser G, Shultz K, McClintock SD, Malhotra NR. Br J Neurosurg. 2021;[Epub]:1–7. doi: 10.1080/02688697.2020.1866165. [DOI] [PubMed] [Google Scholar]
- 6.CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2010-2014. Ostrom QT, Gittleman H, Liao P, Vecchione-Koval T, Wolinsky Y, Kruchko C, Barnholtz-Sloan JS. Neuro Oncol. 2017;19:0. doi: 10.1093/neuonc/nox158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meningiomas: knowledge base, treatment outcomes, and uncertainties. A RANO review. Rogers L, Barani I, Chamberlain M, et al. J Neurosurg. 2015;122:4–23. doi: 10.3171/2014.7.JNS131644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.An overview of meningiomas. Buerki RA, Horbinski CM, Kruser T, Horowitz PM, James CD, Lukas RV. Future Oncol. 2018;14:2161–2177. doi: 10.2217/fon-2018-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Outcome of elderly patients undergoing intracranial meningioma resection--a systematic review and meta-analysis. Poon MT, Fung LH, Pu JK, Leung GK. Br J Neurosurg. 2014;28:303–309. doi: 10.3109/02688697.2013.841857. [DOI] [PubMed] [Google Scholar]
- 10.Seizures in supratentorial meningioma: a systematic review and meta-analysis. Englot DJ, Magill ST, Han SJ, Chang EF, Berger MS, McDermott MW. J Neurosurg. 2016;124:1552–1561. doi: 10.3171/2015.4.JNS142742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The effect of socioeconomic status on age at diagnosis and overall survival in patients with intracranial meningioma. Brewster R, Deb S, Pendharkar AV, Ratliff J, Li G, Desai A. Int J Neurosci. 2020;[Epub]:1–8. doi: 10.1080/00207454.2020.1818742. [DOI] [PubMed] [Google Scholar]
- 12.Racial and socioeconomic correlates of treatment and survival among patients with meningioma: a population-based study. Bhambhvani HP, Rodrigues AJ, Medress ZA, Hayden Gephart M. J Neurooncol. 2020;147:495–501. doi: 10.1007/s11060-020-03455-2. [DOI] [PubMed] [Google Scholar]
- 13.The effect of household income on outcomes following supratentorial meningioma resection. Spadola M, Farooqi A, Dimentberg R, Blue R, Shultz K, McClintock SD, Malhotra N. Clin Neurol Neurosurg. 2020;195:106031. doi: 10.1016/j.clineuro.2020.106031. [DOI] [PubMed] [Google Scholar]
- 14.Why doctors hate their computers. [ Mar; 2022 ];Gawande A. https://www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers?utm_medium=email&utm_source=transaction 2018 12 [Google Scholar]
- 15.Table B19013. Median household income. [ Mar; 2022 ];https://censusreporter.org/tables/B19013/ IN. 2019
- 16.Outcome following surgery for intracranial meningiomas in the aging. Konglund A, Rogne SG, Lund-Johansen M, Scheie D, Helseth E, Meling TR. Acta Neurol Scand. 2013;127:161–169. doi: 10.1111/j.1600-0404.2012.01692.x. [DOI] [PubMed] [Google Scholar]
- 17.Morbidity and mortality of meningioma resection increases in octogenarians. Steinberger J, Bronheim RS, Vempati P, et al. World Neurosurg. 2018;109:0–23. doi: 10.1016/j.wneu.2017.09.021. [DOI] [PubMed] [Google Scholar]
- 18.Socioeconomic factors are associated with frequency of repeat emergency department visits for pediatric closed fractures. Dy CJ, Lyman S, Do HT, Fabricant PD, Marx RG, Green DW. J Pediatr Orthop. 2014;34:548–551. doi: 10.1097/BPO.0000000000000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. Kangovi S, Barg FK, Carter T, Long JA, Shannon R, Grande D. Health Aff (Millwood) 2013;32:1196–1203. doi: 10.1377/hlthaff.2012.0825. [DOI] [PubMed] [Google Scholar]
- 20.Reducing high-users' visits to the emergency department by a primary care intervention for the uninsured: a retrospective study. Tsai MH, Xirasagar S, Carroll S, Bryan CS, Gallagher PJ, Davis K, Jauch EC. Inquiry. 2018;55:46958018763917. doi: 10.1177/0046958018763917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Epidemiology of brain tumors. Fisher JL, Schwartzbaum JA, Wrensch M, Wiemels JL. Neurol Clin. 2007;25:867-90, vii. doi: 10.1016/j.ncl.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 22.Brain tumor survival: results from the National Cancer Data Base. Surawicz TS, Davis F, Freels S, Laws ER Jr, Menck HR. J Neurooncol. 1998;40:151–160. doi: 10.1023/a:1006091608586. [DOI] [PubMed] [Google Scholar]
- 23.Neurosurgical treatment and outcome patterns of meningioma in Sweden: a nationwide registry-based study. Corell A, Thurin E, Skoglund T, et al. Acta Neurochir (Wien) 2019;161:333–341. doi: 10.1007/s00701-019-03799-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Surgical mortality at 30 days and complications leading to recraniotomy in 2630 consecutive craniotomies for intracranial tumors. Lassen B, Helseth E, Rønning P, et al. Neurosurgery. 2011;68:1259–1268. doi: 10.1227/NEU.0b013e31820c0441. [DOI] [PubMed] [Google Scholar]
- 25.Development and validation of a multivariate prediction model of perioperative mortality in neurosurgery: the New Zealand Neurosurgical Risk Tool (NZRISK-NEURO) Clark S, Boyle L, Matthews P, Schweder P, Deng C, Campbell D. Neurosurgery. 2020;87:0–20. doi: 10.1093/neuros/nyaa144. [DOI] [PubMed] [Google Scholar]
- 26.Effectiveness of case management strategies in reducing emergency department visits in frequent user patient populations: a systematic review. Kumar GS, Klein R. J Emerg Med. 2013;44:717–729. doi: 10.1016/j.jemermed.2012.08.035. [DOI] [PubMed] [Google Scholar]
- 27.Frequent users of US emergency departments: characteristics and opportunities for intervention. Vinton DT, Capp R, Rooks SP, Abbott JT, Ginde AA. Emerg Med J. 2014;31:526–532. doi: 10.1136/emermed-2013-202407. [DOI] [PubMed] [Google Scholar]
- 28.Relationship between office-based provider visits and emergency department encounters among publicly-insured adults with epilepsy. Lekoubou A, Bishu KG, Ovbiagele B. Epilepsy Behav. 2018;80:235–239. doi: 10.1016/j.yebeh.2018.01.030. [DOI] [PubMed] [Google Scholar]
- 29.Evaluating area-based socioeconomic status indicators for monitoring disparities within health care systems: results from a primary care network. Berkowitz SA, Traore CY, Singer DE, Atlas SJ. Health Serv Res. 2015;50:398–417. doi: 10.1111/1475-6773.12229. [DOI] [PMC free article] [PubMed] [Google Scholar]