Abstract
Purpose
Obstructive sleep apnea (OSA) is highly prevalent but mostly undiagnosed in obese patients scheduled for bariatric surgery. To prevent cardiopulmonary complications, many clinics perform preoperative OSA screening. Consequently, adequate adherence to continuous positive airway pressure (CPAP) therapy is essential but challenging. We aimed to evaluate CPAP adherence and its influence on postoperative outcomes.
Methods
In a prospective multicenter cohort study, we compared different perioperative strategies for handling undiagnosed OSA in bariatric patients. In this subgroup analysis, patients newly diagnosed with OSA were compared to those with pre-existing OSA. We assessed inadequate CPAP adherence, defined as < 4 h/night, between the preoperative period and 6 months postoperative. Cardiopulmonary complications and (un)scheduled ICU admissions were also evaluated.
Results
In total, 272 patients with newly diagnosed OSA (67.4%) and 132 patients with pre-existing OSA (32.6%) were included. Before surgery, 41 newly diagnosed patients used CPAP inadequately, compared to 5 patients with pre-existing OSA (15% vs. 4%, p = 0.049). Six months after surgery, inadequate CPAP use increased to 73% for newly diagnosed patients and 39% for patients with pre-existing OSA, respectively (p < 0.001). Incidences of cardiopulmonary complications, scheduled, and unscheduled ICU admissions were similar in the two study groups (p = 0.600, p = 0.972, and p = 0.980, respectively).
Conclusion
Inadequate CPAP adherence is higher in bariatric patients newly diagnosed with OSA when compared to patients with pre-existing OSA. Strategies to increase CPAP adherence may be valuable when considering routine OSA screening and CPAP therapy in patients undergoing bariatric surgery. Further studies are needed to improve current guidelines on perioperative OSA management of obese patients.
Trial registration
POPCORN study, registered at Netherlands Trial Register, https://www.trialregister.nl/trial/6805. ID no: 6805.
Keywords: Obstructive sleep apnea, Obesity, Bariatric surgery, Continuous positive airway pressure, Adherence
Introduction
Obesity has become a health issue of pandemic proportions, with currently 650 million people that are obese worldwide [1]. Treatment of obesity is difficult and initially starts with conservative strategies such as lifestyle interventions, diet, and occasionally drugs. However, as these interventions lack sustainable effectiveness, bariatric surgery can be considered in patients with morbid obesity [2]. Bariatric procedures, such as Roux-en-Y gastric bypass and sleeve gastrectomy, are currently the only treatment options that result in significant weight loss that is sustained during long-term follow-up [3]. In addition, many obesity-related comorbidities are positively affected by weight reduction or even completely resolved.
Obstructive sleep apnea (OSA) is associated with obesity [4]. Obese patients scheduled for bariatric surgery have an excessively high prevalence of OSA compared to the general population (60–83% vs. 1–9%) of which the majority is undiagnosed [5, 6]. Unrecognized and untreated OSA is associated with an increased risk of perioperative cardiopulmonary and thromboembolic complications in patients undergoing surgery [7]. These complications are relatively rare and occur in 1.3% of patients following bariatric surgery. However, these complications can lead to potentially fatal outcomes, which is especially true for major cardiac adverse events, and occur approximately in 0.1% of all bariatric patients [8, 9]. The exact attributable risk for developing these complications due to OSA is unclear, as no randomized studies have been conducted to evaluate this causative link, but observational data show increased odds ratios for these complications in OSA patients compared to those without OSA [10].
To prevent OSA-related complications, guidelines advise to perform preoperative screening in bariatric patients who report symptoms of OSA using questionnaires, polysomnography, or home sleep apnea testing (HSAT) [11, 12]. Patients with a high apnea–hypopnea index (AHI), or in the case of HSAT respiratory event index (REI), indicating moderate or severe disease, should be treated with continuous positive airway pressure (CPAP) [12]. Some studies describing patients undergoing general surgery have shown that adequate CPAP therapy decreases the risk of perioperative complications [13]. Additionally, CPAP therapy may reduce excessive daytime sleepiness, cognitive impairment, and cardiovascular risk profile during the pre-and postoperative months [14]. Although the benefits of CPAP seem apparent, studies describing CPAP adherence and subsequent influence on perioperative outcomes in bariatric patients are scarce.
Data on non-surgical, general OSA patients shows that adherence to CPAP is often poor, with reported adherence rates between 15 and 71% [15, 16]. CPAP is often rejected by patients due to side effects such as nasal congestion, claustrophobia, or mucosal dryness. Although it is unclear if adherence rates differ between the bariatric surgery population and patients with symptomatic OSA, it can be postulated that the latter group is more compliant. Bariatric patients often do not experience symptoms related to OSA, or do not recognize these symptoms as a result of OSA, and therefore may subjectively benefit less from CPAP therapy [14]. Therefore, they could be at risk for poor adherence to CPAP. In addition, many bariatric patients are aware of the effectiveness of bariatric surgery on OSA prevalence, as reduction or complete remission of OSA occurs in 68.4–92.2% [17]. This may also encourage patients to stop CPAP prematurely, before OSA remission is proven by a polysomnography or HSAT. Currently, there is only a consensus-based guideline that recommends postoperative polysomnography to evaluate whether CPAP can be safely discontinued [11]. In this guideline, the timing of postoperative reevaluation is left up to the discretion of the treating physician, based on weight loss and reported symptoms.
The aim of this study was to evaluate CPAP adherence in bariatric patients with newly diagnosed OSA before and after surgery and to compare these results to patients who have been diagnosed with OSA in the past. We hypothesized that newly diagnosed patients might have lower adherence to CPAP, and this could lead to an increased rate of postoperative complications.
Material and methods
Study design and subjects
In this multicenter, observational, prospective cohort study, consecutive patients referred for bariatric surgery were recruited from seven centers in the Netherlands between April 2018 and December 2019. Patients with no prior history of OSA were eligible for participating in the POPCORN study, a study that evaluates the cost-effectiveness of two different strategies of perioperative management of OSA in patients undergoing bariatric surgery. This study is registered at the Netherlands Trial Register, https://www.trialregister.nl/trial/6805, and was approved by the Medical Research Ethics Committees United, reference number W17.050 [18]. The primary outcome of the POPCORN study is cost-effectiveness, and these results are not yet complete. In this current paper, we present secondary outcomes in all patients that were diagnosed with OSA. The secondary outcomes are CPAP adherence, reasons to discontinue CPAP, postoperative complications, ICU admissions, outcomes of questionnaires on sleep scores, and sleep-related quality of life. Data on weight loss are presented as a percentage of total body weight loss (%TBWL) and as a percentage excess weight loss (%EWL). Patients undergoing preoperative HSAT were diagnosed with OSA, and CPAP was initiated if they had REI ≥ 15. For some patients with REI 5–15, who reported excessive daytime sleepiness, CPAP treatment was offered too. These patients will be referred to as group A. Four of seven participating hospitals performed HSAT in patients that were pre-selected by STOPBANG-questionnaires, while the higher volume centers screened all consecutive patients eligible for bariatric surgery, regardless of STOPBANG scores. During the same time period, consecutive patients who presented with pre-existing OSA and current CPAP therapy were recruited as controls (group B). Inclusion criteria were (A) eligibility for primary bariatric surgery according to the current IFSO guidelines, (B) age ≥ 18 years, and (C) Dutch language proficiency. Exclusion criteria were (A) absence of OSA on HSAT, (B) OSA treatment other than CPAP, or variable/bilevel positive airway pressure, (C) revisional bariatric procedure, and (D) concomitant procedures that could enhance the risk of (cardiopulmonary) complications, such as repositioning of an intrathoracic stomach. All patients provided either written or digitally-signed informed consent.
Outcomes and data collection
In this current analysis, we aimed to evaluate the prevalence of patients with inadequate adherence to CPAP (defined as < 4 h per night) during the preoperative phase, and during the first 6 months after surgery. We also analyzed the incidence of cardiopulmonary complications, scheduled/unscheduled admissions to the ICU or medium care unit (MCU), and perioperative measures to prevent complications in patients with inadequate CPAP use. Furthermore, reasons to stop CPAP therapy within 6 months after surgery were documented. Predictors to stop CPAP therapy were also analyzed. Data were extracted from hospital files, and telemonitoring of CPAP usage was used to determine adherence to CPAP in terms of hours/night and date of potential discontinuation, if available. Patient-reported outcomes were retrieved from questionnaires: the Epworth Sleepiness Scale (ESS) and the functional outcomes of sleep questionnaire (FOSQ), 10-items edition, and patients were asked whether they still used CPAP treatment, and if not, which data CPAAP was ceased, reasons for discontinuation, and whether they had undergone a new HSAT [19, 20]. Questionnaires were sent to patients preoperatively, and after surgery at 1, 3, and 6 months. Weight at baseline and all other time points was documented, and weight loss was represented as %TBWL, defined as weight loss divided by weight before surgery, and also as %EWL. This percentage was calculated as loss of excess weight (defined as weight above the ideal weight, i.e., = BMI 25 kg/m2) divided by excess weight before surgery.
Statistical analysis
Data are presented as means ± standard deviations (SD) or medians and interquartile ranges (IQR). Comparison of continuous data was performed using independent t-tests or the Mann–Whitney U test. Binary data were analyzed with a chi-square test or a Fishers’ exact test. To identify predicting factors for inadequate use of CPAP, we performed univariable and multivariable logistic regression. Variables in the univariable analysis with a p value under < 0.10 were added to the multivariable model. Risk factors are presented including the odds ratio (OR) and adjusted odds ratio (aOR) with 95% confidence intervals (CI). A p value of < 0.05 was considered as statistically significant. Statistical analyses were performed by using IBM SPSS Statistics, version 25.0 for Windows (SPSS. Chicago, IL).
Results
Of 542 patients that underwent a preoperative HSAT prior to bariatric surgery, 272 patients (50.2%) were diagnosed with OSA and consequently treated with CPAP (group A). In this group, the median time from preoperative HSAT to bariatric surgery was 125 days. During the study period, 132 patients with pre-existing OSA and CPAP therapy were recruited (group B). In this group, the median time between HSAT and bariatric surgery was 1013 days. Patients in group B were more often male, with higher mean REI and lower mean preoperative BMI and higher prevalence of asthma (Table 1).
Table 1.
Baseline characteristics and surgical outcomes
| Total (n = 404) | Group A (newly diagnosed OSA n = 272, 67.4%) | Group B (pre-existing OSA, n = 132, 32.6%) | p | |
|---|---|---|---|---|
| Age (median, IQR) | 51 (45–57) | 51 (45–57) | 51 (46–58) | 0.605 |
| Gender, female (n, %) | 239 (59.2) | 182 (66.9) | 57 (43.2) | < 0.001 |
| BMI in kg/m.2 (mean, SD) | 43.1 ± 6.4 | 43.6 ± 6.3 | 42.3 ± 6.3 | 0.049 |
| Abdominal circumference, in cm (mean, SD) | 132 ± 14.7 | 132 ± 15.0 | 132 ± 13.9 | 0.868 |
| Medical history (n, %) | ||||
| Type 2 diabetes | 111 (27.5) | 70 (25.7) | 41 (31.1) | 0.465 |
| Hypertension | 202 (50) | 139 (51.1) | 63 (47.7) | 0.596 |
| Hypercholesterolemia | 132 (32.7) | 86 (31.6) | 46 (34.8) | 0.572 |
| GERD | 109 (27) | 78 (28.7) | 31 (23.5) | 0.285 |
| Asthma | 60 (14.9) | 28 (10.3) | 32 (24.2) | 0.001 |
| Chronic obstructive pulmonary disease | 17 (4.2) | 9 (3.3) | 8 (6.1) | 0.198 |
| Obesity hypoventilation syndrome | 2 (0.5) | 2 (0.7) | 0 | 0.280 |
| Chronic kidney disease | 17 (4.2) | 12 (4.4) | 5 (3.8) | 0.977 |
| History of psychiatric disorder | 131 (32.4) | 89 (32.7) | 42 (31.8) | 0.910 |
| HSAT outcomes | ||||
| REI (median, IQR) | 25.0 (17.6–40.3) | 23.4 (16.5–36.8) | 34 (20.0–52.4) | 0.001 |
| REI in supine position (median, IQR) | 31.3 (19,0–53.1) | 28.1 (17.9–46.8) | 45.0 (27.0–71.7) | 0.001 |
| ODI (median, IQR) | 25.7 (17.5–43.5) | 24.5 (17.2–39.5) | 34.6 (19.4–52.4) | 0.045 |
| Baseline saturation (median, IQR) | 93.0 (91.3–94.1) | 92.9 (91.2–94.1) | 93.0 (92.0–94.7) | 0.162 |
| Lowest saturation (median, IQR) | 79.0 (73.3–84.0) | 79.0 (73.0–84.2) | 81.5 (74.0–85.8) | 0.400 |
| Smoking (n, %) | ||||
| Current smoking | 19 (4.7) | 14 (5.1) | 5 (3.8) | 0.550 |
| History of smoking | 158 (39.1) | 103 (37.9) | 55 (41.7) | 0.444 |
| Type of Surgery (n, %) | ||||
| LRYGB | 302 (74.8) | 202 (74.3) | 100 (75.8) | 0.746 |
| LSG | 102 (25.2) | 70 (25.7) | 32 (24.2) | 0.747 |
| Complications < 30 days (n, %) | 37 (9.2) | 26 (9.6) | 11 (8.3) | 0.689 |
| Minor* | 21 (5.2) | 14 (5.1) | 7 (5.3) | 0.947 |
| Major * | 15 (3.7) | 12 (4.4) | 3 (2.3) | 0.403 |
| Cardiopulmonary complications | 4 (1) | 2 (0.7) | 2 (1.5) | 0.600 |
| ICU admission (n, %) | 9 (2.2) | 6 (2.2) | 3 (2.3) | 0.788 |
| Scheduled | 6 (1.5) | 4 (1.5) | 2 (1.5) | 0.972 |
| Unscheduled | 3 (0.7) | 2 (0.7) | 1 (0.8) | 0.980 |
| MCU admission (n, %) | 1 (0.2) | 1 (0.4) | 0 | 0.673 |
| Readmission (n, %) | 15 (3.7) | 12 (4.4) | 3 (2.3) | 0.568 |
| Reoperation (n, %) | 6 (1.5) | 6 (2.2) | 0 | 0.186 |
*Based on Clavien-Dindo classification (CDC); minor and major complications were defined as CDC 1–2 and CDC ≥ 3A
BMI body mass index, GERD gastroesophageal reflux disease, LRYGB laparoscopic Roux-en-Y gastric bypass, LSG laparoscopic sleeve gastrectomy, ICU intensive care unit, IQR interquartile range, MCU medium care unit, ODI oxygen desaturation index, OSA obstructive sleep apnea, REI respiratory event index, SD standard deviation
Inadequate CPAP use
Before surgery, 41 patients in group A (15%) used their CPAP device insufficiently, compared to 5 patients (4%) in group B (p = 0.049) (Table 2). The time between the start of CPAP therapy until surgery did not affect CPAP adherence in newly diagnosed patients. One month postoperatively, 43% of patients in group A were inadequate users, compared to 20.5% in group B (p < 0.001). At 3 months after surgery, results similarly differed between groups A and B: 57.7% vs. 37.9% (p < 0.001). At 6 months after surgery, 199 patients in group A (73%) were inadequate CPAP users, compared to 51 (39%) patients in group B (p < 0.001). At that time, six patients were lost to follow-up, and one patient in group A died 156 days after surgery due to a stroke.
Table 2.
Inadequate use of CPAP before and after surgery
| Group A n = 272 |
Group B n = 132 |
p-value | |
|---|---|---|---|
| Before surgery (n, %) | |||
| Inadequate CPAP use | 42 (15.4) | 5 (3.8) | 0.049 |
| - CPAP discontinued | 23 (8.4) | 0 | |
| - CPAP use < 4 h/night | 19 (7.0) | 5 (3.8) | |
| Adequate CPAP use | 230 (84.6) | 127 (96.2) | |
| 1 month postoperative (n, %) | < 0.001 | ||
| Inadequate CPAP use | 117 (43.0) | 27 (20.5) | |
| - CPAP discontinued* | 81 (29.8) | 12 (9.1) | |
| - CPAP use < 4 h/night | 36 (13.2) | 15 (11.4) | |
| Adequate CPAP use | 155 (56.9) | 105 (79.5) | |
| 3 months postoperative (n, %) | < 0.001 | ||
| Inadequate CPAP use | 157 (57.7) | 50 (37.9) | |
| - CPAP discontinued* | 130 (47.8) | 22 (16.7) | |
| - CPAP use < 4 h/night | 27 (9.9) | 28 (21.2) | |
| Adequate CPAP use | 115 (42.3) | 82 (62.1) | |
| 6 months postoperative (n, %) | < 0.001 | ||
| Inadequate CPAP use | 199 (73.2) | 51 (38.6) | |
| - CPAP discontinued* | 180 (66.2) | 45 (34.0) | |
| - CPAP use < 4 h/night | 20 (7.4) | 6 (4.6) | |
| Adequate CPAP use | 71 (26.1) | 76 (57.6) | |
| Missing** | 2 (0.7) | 5 (3.8) |
Group A: newly diagnosed OSA patients, group B: patients with a pre-existent OSA diagnosis
*Cumulative number of patients who discontinued CPAP therapy
**Missing data: 6 lost to FU, 1 fatality (156 days after surgery)
CPAP continuous positive airway pressure, OSA obstructive sleep apnea
Postoperative outcomes
Total postoperative complications were similar in patients with newly diagnosed OSA and patients with pre-existing OSA (9.6% vs. 8.3%, p = 0.689) (Table 1). Cardiopulmonary complications were also similar between study groups (n = 2, 0.7% vs. n = 2, 1.5%, p = 0.600). To analyze the influence of CPAP use on cardiopulmonary complications, we also combined group A and B and made comparisons between adequate and inadequate CPAP users. Complications between these two groups (3/357 vs. 1/47, p = . 212) showed no significant difference.
Distribution of minor and major complications based on the Clavien-Dindo Classification [21] did not differ between groups A and B. Scheduled ICU admissions of group A (n = 4) were due to severe chronic obstructive pulmonary disease, non-adherence to CPAP (n = 2), and severe OSA (REI > 100), and in group B (n = 2) due to severe OSA (REI > 80) and congestive heart failure. Unscheduled ICU admissions in group A (n = 2) were anastomotic leakage and diabetic ketoacidosis, and in group B one patient was admitted to the ICU due to severe postoperative desaturations, despite adequate CPAP therapy. Admission to the MCU was required in one patient in group A for postoperative CPAP intolerance, despite adequate preoperative adherence.
Other interventions to prevent OSA-related complications in inadequate CPAP users before surgery mostly consisted of mandatory use of CPAP during hospital admission as a prerequisite to undergo surgery, despite the patients’ inability to adhere to CPAP at home (group A; n = 23, group B; n = 4). The remaining patients that were inadequate CPAP users were all postoperatively monitored with continuous pulse oximetry and received supplemental oxygen as needed (group A, n = 18, group B, n = 1).
CPAP use
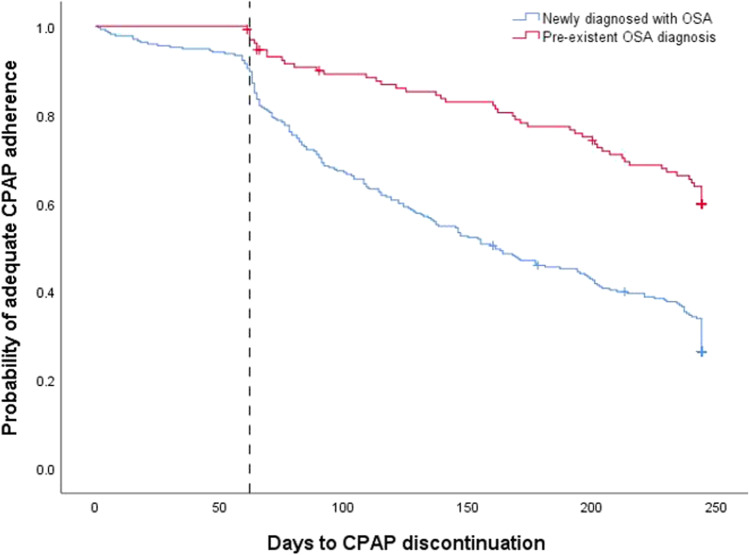
During the preoperative phase, rates of patients who stopped using CPAP differed between the two groups; 8.4% of group A stopped CPAP therapy, while all patients in group B used their CPAP device (Table 2). Six months after surgery, the percentage of patients who stopped CPAP therapy increased to 66.2% and 34.0% in groups A and B, respectively (p < 0.001) (Fig. 1).
Fig. 1.
Kaplan–Meier curve illustrating the time-to-event, i.e., CPAP discontinuation between 2 months before surgery and 6 months after surgery (p < 0.001). Patients newly diagnosed with OSA are indicated in blue. Patients with a pre-existent OSA diagnosis are indicated in red. The day of surgery is indicated by the intermittent line. CPAP continuous positive airway pressure, OSA obstructive sleep apnea
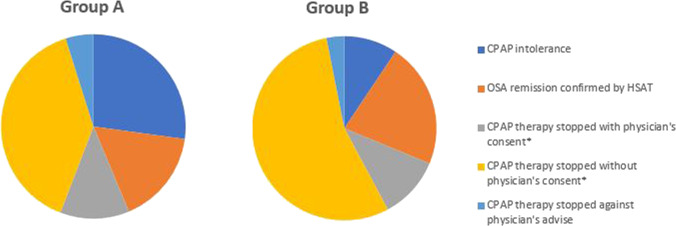
Reasons to stop CPAP therapy also differed between the two study groups (Fig. 2). The majority of patients stopped CPAP therapy without consultation of a physician (group A = 39% vs. group B = 55%, p = 0.004). None of these patients attended a postoperative appointment in an outpatient clinic, either because there were no scheduled appointments or because patients canceled on their own initiative. Another reason to stop CPAP was intolerance to CPAP, which occurred in 23% in group A vs. 9.4% in group B (p = 0.002). In total, 30.5% (n = 83) of group A and 24.2% (n = 32) of group B underwent a postoperative HSAT. All patients underwent HSAT between 3 and 6 months, and an additional 10.3% and 8.3% indicated they had an HSAT scheduled for > 6 months postoperative, respectively. Following these HSATs, remission of OSA proven in 12.5% of group A and 10.6% of group B, and they could cease therapy (p = 0.351). A few patients stopped CPAP therapy despite contrary advice of their physician. In these specific cases, moderate to severe OSA was diagnosed on a postoperative HSAT although patients did not experience any OSA-related symptoms (group A = 4.9% vs. group B = 3.1%, p = 0 0.737). Based on symptom reduction after significant weight loss, 21.9% of group A and 10.9% of group B were advised by their physician to stop therapy without a HSAT was performed (p = 0.497).
Fig. 2.
Motivation to stop CPAP therapy of group A (newly diagnosed OSA patients) and group B (patients with a pre-existent OSA diagnosis). *No postoperative HSAT performed. CPAP continuous positive airway pressure, HSAT home sleep apnea testing, OSA obstructive sleep apnea
A univariable logistic regression was performed to identify predictors to stop CPAP and correct for potential confounders (Table 3). The strongest predictor in the multivariable analysis was the preoperative diagnosis of OSA: aOR 2.9 (p < 0.001). In contrast, patients with preoperative BMI ≥ 45 kg/m2 were less likely to cease CPAP therapy (aOR 0.43, p = 0.003), just like patients with baseline REI ≥ 30 (aOR 0.56, p = 0.029) and type 2 diabetes (aOR 0.55, p = 0.021).
Table 3.
Univariable and multivariate logistic regression analysis of predictors for CPAP discontinuation (n = 397*)
| N (%) | Univariable | Multivariable | |||
|---|---|---|---|---|---|
| OR [95% CI] | p value | aOR [95% CI] | p value | ||
| Gender (female) | 239 (59.2) | 0.74 [0.48–1.13] | 0.160 | ||
| Age ≥ 50 years | 238 (58.9) | 0.78 [0.51–1.21] | 0.271 | ||
| Preoperative BMI ≥ 45 kg/m2 | 127 (31.4) | 0.53 [0.34–0.83] | 0.006 | 0.43 [0.25–0.75] | 0.003 |
| Preoperative waist, in cm (mean, SD) | 132 ± 14.7 | 0.99 [0.98–1.00] | 0.165 | ||
| Pre-existing diagnosis of OSA | 272 (67.4) | 3.10 [1.99–4.85] | < 0.001 | 2.93 [1.74–4.92] | < 0.001 |
| Baseline REI ≥ 30 | 161 (42.2) | 0.45 [0.29–0.70] | < 0.001 | 0.59 [0.37–0.95] | 0.029 |
| Asymptomatic before CPAP therapy | 93 (23) | 2.39 [1.28–4.46] | 0.006 | 1.39 [0.74–2.63] | 0.310 |
| ESS ≥ 11** | 111 (27.5) | 1.022 [0.64–1.64] | 0.927 | ||
| Hypertension | 202 (50) | 0.99 [0.65–1.51] | 0.972 | ||
| Type 2 diabetes | 111 (27.5) | 0.58 [0.36–0.91] | 0.018 | 0.55 [0.33–0.91] | 0.021 |
| Hyperlipidemia | 132 (32.7) | 1.30 [0.84–2.03] | 0.245 | ||
| Asthma | 60 (14.9) | 1.60 [0.90–2.82] | 0.109 | ||
| COPD | 17 (4.2) | 1.92 [0.73–5.11] | 0.188 | ||
| History of psychiatric disease | 131 (32.4) | 0.96 [0.61–1.51] | 0.867 | ||
| Current smoking | 19 (4.7) | 0.80 [0.31–2.09] | 0.654 | ||
| EWL ≥ 60%*** | 215 (53.0) | 1.85 [1.20–2.84] | 0.005 | 1.28 [0.66–2.47] | 0.467 |
| TWL ≥ 25%*** | 198 (49.0) | 1.64 [1.07–2.52] | 0.024 | 1.45 [0.79–2.63] | 0.230 |
*7 patients have missing data: 6 lost to follow-up and 1 fatality
**Indicating mild excessive daytime sleepiness
***Measured at six months postoperative
BMI body mass index, CI confidence interval, COPD chronic obstructive pulmonary disease, ESS Epworth Sleepiness Score, %EWL percentage excess weight loss, (a) OR (adjusted) odds Ratio, OSA obstructive sleep apnea, REI respiratory event index, %TWL Percentage Total Weight Loss
Outcomes of questionnaires and weight
All outcomes of questionnaires were evaluated for both groups, with further subdivision based on whether they still used CPAP at the time of the questionnaire (Table 4). There were no significant changes in outcomes of ESS, FOSQ, weight, or BMI between groups A and B, that were consistently observed at all time points. FOSQ scores were significantly lower for group A at baseline and after surgery at 1 and 3 months, while this difference disappeared at 6 months postoperative. The initial BMI of patients newly diagnosed with OSA who used CPAP before surgery was lower compared to patients who did not use their CPAP device, this difference was not seen during all follow-up visits. In patients with pre-existent OSA, no significant distinction could be made between CPAP users and non-user regarding the self-reported outcomes retrieved from questionnaires.
Table 4.
Outcomes of questionnaires and weight loss
| Group A (n = 272) | Group B (n = 132) | p value* | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | CPAP use | No CPAP use | p-value** | Total | CPAP use | No CPAP use | p-value** | ||
| Before surgery (n, %) | |||||||||
| ESS score | 7.6 ± 5.2 | 7.6 ± 5.1 | 7.3 ± 6.1 | 0.723 | 8.4 ± 5.3 | 8.4 ± 5.3 | NA | NA | 0.483 |
| FOSQ score | 20 (19-20) | 20 (19-20) | 20 (19-20) | 0.476 | 19.7 18.3–20) | 19.7 (18.2–20) | NA | NA | 0.013 |
| Weight | 128.7 ± 23.0 | 128.2 ± 22.1 | 136.5 ± 30.5 | 0.009 | 128.8 ± 23.9 | 128.5 ± 23.5 | NA | NA | 0.912 |
| BMI | 43.8 ± 5.8 | 43.6 ± 5.6 | 45.1 ± 7.5 | 0.006 | 41.2 ± 6.6 | 42.3 ± 6.3 | NA | NA | 0.337 |
| 1 month postoperative (n, %) | |||||||||
| ESS score | 5.9 ± 4.9 | 6.5 ± 5.4 | 5.0 ± 3.5 | 0.029 | 6.7 ± 4.6 | 6.7 ± 4.5 | 6.7 ± 5.4 | 0.532 | 0.778 |
| FOSQ score | 20 (19.3–20) | 20 (19.5–20) | 20 (19.3–20) | 0.788 | 20 (18.7–20) | 20 (18.7–20) | 20 (17.4–20) | 0.827 | 0.012 |
| Weight | 116.8 ± 21.9 | 117.4 ± 19.8 | 116.45 ± 23.9 | 0.067 | 116.6 ± 21.9 | 117.6 ± 21.9 | 104.6 ± 18.3 | 0.573 | 0.889 |
| BMI | 39.5 ± 5.9 | 39.8 ± 5.7 | 38.9 ± 6.1 | 0.682 | 37.9 ± 6.3 | 38.2 ± 6.3 | 33.7 ± 4.2 | 0.442 | 0.513 |
| %TWL | 9.8 ± 5.6 | 23.3 ± 15.6 | 26.5 ± 11.4 | 0.831 | 10.2 ± 3.6 | 10.1 ± 3.2 | 12.5 ± 6.0 | 0.015 | 0.263 |
| %EWL | 24.3 ± 14.4 | 20.2 ± 9.5 | 23.5 ± 10.6 | 0.903 | 27.4 ± 12.2 | 26.5 ± 10.7 | 37.8 ± 19.0 | 0.085 | 0.418 |
| 3 months postoperative (n, %) | |||||||||
| ESS score | 4.7 ± 4.7 | 4.7 ± 4.9 | 4.7 ± 4.5 | 0.686 | 6.4 ± 5.0 | 6.0 ± 4.5 | 8.4 ± 6.5 | 0.066 | 0.402 |
| FOSQ score | 20 (20-20) | 20 (20-20) | 20 (19.7–20) | 0.172 | 20 (19-20) | 20 (19.4–20) | 20 (18.7–20) | 0.334 | 0.009 |
| Weight | 105.6 ± 19.7 | 105.7 ± 18.1 | 105.5 ± 23.2 | 0.245 | 105.1 ± 20.7 | 106.7 ± 20.9 | 97.0 ± 17.9 | 0.557 | 0.816 |
| BMI | 35.9 ± 5.5 | 36.1 ± 5.2 | 35.3 ± 6.2 | 0.996 | 34.2 ± 6.0 | 34.8 ± 6.2 | 31.3 ± 4.1 | 0.342 | 0.499 |
| %TWL | 18.3 ± 4.4 | 17.8 ± 3.9 | 18.6 ± 4.9 | 0.006 | 18.4 ± 4.5 | 17.9 ± 4.1 | 20.9 ± 5.3 | 0.137 | 0.828 |
| %EWL | 44.9 ± 14.1 | 42.6 ± 12.1 | 47.5 ± 15.7 | 0.019 | 49.5 ± 17.4 | 47.4 ± 15.8 | 60.2 ± 21.3 | 0.020 | 0.011 |
| 6 months postoperative (n, %) | |||||||||
| ESS score | 4.5 ± 4.5 | 4.6 ± 4.5 | 4.4 ± 4.5 | 0.589 | 5.4 ± 4.1 | 6.0 ± 4.0 | 4.4 ± 4.3 | 0.410 | 0.651 |
| FOSQ score | 20 (19.7–20) | 20 (19.8–20) | 20 (19.7–20) | 0.536 | 20 (19.6–20) | 20 (19.1–20) | 20 (19.9–20) | 0.174 | 0.186 |
| Weight | 96.7 ± 19.4 | 101.1 ± 20.5 | 94.6 ± 18.4 | 0.138 | 96.2 ± 19.1 | 99.1 ± 19.9 | 90.0 ± 14.7 | 0.283 | 0.734 |
| BMI | 32.8 ± 5.3 | 34.2 ± 5.3 | 32.1 ± 5.0 | 0.636 | 31.4 ± 5.4 | 32.4 ± 5.6 | 29.2 ± 3.8 | 0.209 | 0.994 |
| %TWL | 25.2 ± 6.0 | 24.5 ± 6.4 | 25.5 ± 5.8 | 0.504 | 25.3 ± 5.6 | 24.1 ± 5.4 | 27.6 ± 5.5 | 0.303 | 0.451 |
| %EWL | 61.9 ± 18.2 | 57.2 ± 17.1 | 64.2 ± 18.3 | 0.128 | 67.1 ± 20.8 | 62.4 ± 19.2 | 76.5 ± 20.8 | 0.106 | 0.721 |
*P-value of comparison between group A and group B
**P-value of comparison between CPAP users and non-users within group A and group B, respectively
Group A: patients with newly diagnosed OSA, group B: patients with pre-existing OSA
BMI body mass index, CPAP continuous positive airway pressure, %EWL percentage excess weight loss, ESS Epworth Sleepiness Scale, FOSQ functional outcomes of sleep questionnaire, %TWL percentage total weight loss
As sensitivity analyses, we performed subgroup analyses of newly diagnosed patients. We compared patients based on whether preselection for HSAT was performed with STOPBANG-questionnaires or not. We found no difference in CPAP adherence at any time point, neither were any postoperative outcomes different (i.e., all complications, cardiopulmonary complications, or weight loss).
Discussion
Preoperative OSA assessment and subsequent CPAP therapy is perceived to prevent OSA-related complications in obese patients undergoing bariatric surgery, while not conclusively proven. Although 15% of newly diagnosed bariatric patients in this large cohort study did not adequately adhere to CPAP before surgery, this did not lead to an increased number of postoperative complications when compared to patients with pre-existing OSA and CPAP therapy. Six months after surgery, the percentage of patients with inadequate adherence to CPAP increased to 73% in newly diagnosed patients, which was significantly higher than the 39% of patients with pre-existent OSA.
In absence of robust literature on CPAP adherence in bariatric patients who are diagnosed with OSA in the preoperative phase, the true efficacy of routine OSA screening and consequent CPAP therapy remains to be elucidated. In recent years, OSA prevalence in bariatric patients has been extensively reported in studies that performed routine preoperative polysomnography or HSAT [6, 22]. However, limited data is available on consequent perioperative outcomes related to preoperative OSA screening, such as cardiopulmonary complications and related morbidity and mortality [23, 24]. In addition, without accurate data on CPAP adherence and well-designed prospective studies, it seems unjust to assume that CPAP therapy should be applied routinely to prevent postoperative complications. In a study by Guralnick et al., low adherence to CPAP was reported in 104 preoperatively diagnosed patients, as 33% was adherent after 30 days of CPAP therapy [25]. However, it is unclear how many patients in their study failed to adjust to CPAP before hospital admission, as CPAP was initiated only 4 days prior to surgery. In our cohort, we observed that 15% of patients had no or inadequate use of CPAP at the time of surgery. It is important to note that some studies, like ours, perform polygraphy on all patients, instead of pre-selecting patients with a high pre-test probability for OSA, by first applying a screening questionnaire. This means that patients in our cohort are overall less likely to have OSA, and this might negatively influence the adherence rate. To optimize the treatment of OSA and CPAP therapy in bariatric care additional educational, behavioral or troubleshooting interventions should be considered [16, 26]. In addition, postoperative adherence to CPAP might be enhanced by regularly adjusting CPAP pressures, as surgically induced weight loss changes the pressure demand [27]. However, all patients in our cohort used CPAP, while other modalities that also provide positive airway pressure (PAP) may be more suitable for patients with changing pressure demands, such as automated PAP. This potentially increases the ease of continuing CPAP during weight loss. Although these strategies may improve CPAP adherence, they will also require additional time from hospital staff and an increase in costs.
In the present study, the majority of patients stopped CPAP therapy without consulting their OSA physician and often had no scheduled postoperative follow-up. Postoperative HSATs are important to monitor disease remission, as bariatric patients were often asymptomatic or did not recognize OSA symptoms to begin with. Timmermans et al. showed that remission of OSA (i.e., AHI < 15 events/hour) after bariatric surgery is unrelated to the improvement of sleepiness symptoms, weight loss or even self-initiated discontinuation of CPAP therapy [28]. As our observational study showed, many patients cease their CPAP therapy due to these motives, emphasizing the need for clear guidelines on postoperative follow-up for this patient group to confirm either persistence or remission of OSA. We found that many of our patients did not receive a follow-up appointment or a postoperative polygraphy. As a possible explanation, this may be due to the fact that no guideline recommends a specific timeline in which patients should be re-evaluated [11]. It could also derive from the relatively short follow-up duration that is being investigated in our study; 6 months after surgery might be too short to experience significant weight loss and perform consecutive polygraphy. Additionally, as the follow-up period of this study took place during the COVID-19 pandemic, is it possible that this type of elective care was postponed due to limited resources. In addition, we found that patients with pre-existing OSA were significantly more likely to stop CPAP than newly diagnosed patients without consultation of a physician, which could be explained by the fact that these patients are no longer regularly seen by their OSA physician, and thus, a scheduled postoperative HSAT was omitted. These patients were presumably symptomatic at the time of diagnosis, which may have encouraged them to stop CPAP therapy when their OSA complaints resolved after substantial weight loss.
We acknowledge that our study has several limitations. First, the control group consisted of patients with pre-existing OSA before surgical consultation. These patients differed from newly diagnosed OSA patients in several baseline characteristics and more often reported OSA symptoms before HSAT. Although we aimed to correct for these differences in the logistic regression, it is possible that other factors that were not identified in our cohort also acted as confounders, such as neck circumference, pre- or postmenopausal status. Second, complications related to (untreated) OSA are rare, which is in concordance with the findings in the present study. This is a common finding in bariatric populations that adhere to Enhanced Recovery After Bariatric Surgery, a guideline that promotes bariatric surgery with low administration of drugs that induce breathing cessation, as well as early mobilization for optimal pulmonary recovery [9]. Therefore, it is likely that a clinically relevant impact of CPAP therapy will only be visible in study populations with a much larger sample size. This also makes a future randomized trial that evaluates OSA-related complications quite unlikely or even infeasible, as sample size calculation using previous data of OSA-related complications in a bariatric cohort, i.e., 0.6–0.8% [29], results in group sizes of 27,634 patients, containing 55,268 patients in total. Third, it should be noted that the complication rate is potentially negatively influenced by a specific element of our perioperative strategy, i.e., preoperatively diagnosed OSA patients who did not use CPAP, or used it insufficiently, were advised to use CPAP during the first night postoperatively. Patients that do not tolerate CPAP well are at risk of enhanced sleep deprivation. This fragmentation of sleep can further aggravate the increase of AHI that is observed in the first postoperative week, long after patients are discharged from the hospital [30]. Fourth, the adherence data of this study is partly based on questionnaires outcomes. We tried to refrain from using this data as questionnaires are less objective than data gained from telemonitoring. As we did not have objective quantifiable data through telemonitoring for all patients, this may have influenced our outcomes. Future studies should try to solely use adherence data from telemonitoring, as this is more objective and additionally has the potential to better provide tailored advice for CPAP patients [31].
Rates of inadequate or no adherence in bariatric patients who are newly diagnosed with OSA were high in both the pre- and postoperative periods. Given that routine preoperative OSA screening in all bariatric patients and consequent CPAP implementation is a time-consuming and costly intervention, the percentage of inadequately adherent patients suggests that this approach may not be the most cost-effective modality to prevent OSA-related complications. Future studies should elucidate whether optimization of CPAP use is the best strategy to minimize detrimental effects of untreated OSA in bariatric patients, or if alternative strategies to prevent OSA-related complications (i.e., no preoperative screening but for example intense postoperative monitoring or development of an algorithm that has higher specificity and sensitivity than the existing screening questionnaires) can be used in bariatric practice [32].
Conclusion
Our results indicate that patients who are newly diagnosed with OSA are more likely to stop therapy or inadequately apply CPAP before and after surgery, compared to bariatric patients with pre-existing OSA. Strategies to increase CPAP adherence and scheduled postoperative HSATs may be of value when considering routine HSAT screening and subsequent perioperative CPAP in patients undergoing bariatric surgery. Further studies focusing on efficacy and cost-effectiveness are needed to improve current guidelines on perioperative OSA management in morbidly obese patients.
Acknowledgements
We thank L.J. Hazebroek and A. Hofboer-Kapteijns for data assistance.
Author contribution
All authors declare that they have read and contributed to the final draft.
Funding
This study was funded by ZonMw, grant number “843004110.”
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethical approval
This study was performed in accordance with the 1964 Helsinki declaration and its later amendments and was approved by the medical ethical review board.
Consent Statement
Informed consent was obtained from all participants included in the study.
Competing interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
S. L. van Veldhuisen, Email: svanveldhuisen@rijnstate.nl
E. J. Hazebroek, Email: ehazebroek@rijnstate.nl
References
- 1.WHO (2018) Obesity and overweight; Fact sheet
- 2.Fried M, Hainer V, Basdevant A, Buchwald H, Deitel M, Finer N, et al. Interdisciplinary European guidelines on surgery of severe obesity. Obes Facts. 2008;1(1):52–59. doi: 10.1159/000113937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sjostrom L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–2693. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 4.Veasey SC, Rosen IM. Obstructive sleep apnea in adults. N Engl J Med. 2019;380(15):1442–1449. doi: 10.1056/NEJMcp1816152. [DOI] [PubMed] [Google Scholar]
- 5.Tishler PV, Larkin EK, Schluchter MD, Redline S. Incidence of sleep-disordered breathing in an urban adult population: the relative importance of risk factors in the development of sleep-disordered breathing. JAMA. 2003;289(17):2230–2237. doi: 10.1001/jama.289.17.2230. [DOI] [PubMed] [Google Scholar]
- 6.Ravesloot MJ, van Maanen JP, Hilgevoord AA, van Wagensveld BA, de Vries N. Obstructive sleep apnea is underrecognized and underdiagnosed in patients undergoing bariatric surgery. Eur Arch Otorhinolaryngol. 2012;269(7):1865–1871. doi: 10.1007/s00405-012-1948-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hai F, Porhomayon J, Vermont L, Frydrych L, Jaoude P, El-Solh AA. Postoperative complications in patients with obstructive sleep apnea: a meta-analysis. J Clin Anesth. 2014;26(8):591–600. doi: 10.1016/j.jclinane.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 8.Khorgami Z, Jackson TN, Aminian A, Sahawneh JM, Sclabas GM, Chow GS. Early cardiac complications after bariatric surgery: does the type of procedure matter? Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery. 2019;15(7):1132–1137. doi: 10.1016/j.soard.2019.03.030. [DOI] [PubMed] [Google Scholar]
- 9.Malczak P, Pisarska M, Piotr M, Wysocki M, Budzynski A, Pedziwiatr M. Enhanced recovery after bariatric surgery: systematic review and meta-analysis. Obes Surg. 2017;27(1):226–235. doi: 10.1007/s11695-016-2438-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mokhlesi B, Hovda MD, Vekhter B, Arora VM, Chung F, Meltzer DO. Sleep-disordered breathing and postoperative outcomes after bariatric surgery: analysis of the nationwide inpatient sample. Obes Surg. 2013;23(11):1842–1851. doi: 10.1007/s11695-013-0991-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Raaff CAL, Gorter-Stam MAW, de Vries N, Sinha AC, Jaap Bonjer H, Chung F, et al. Perioperative management of obstructive sleep apnea in bariatric surgery: a consensus guideline. Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery. 2017;13(7):1095–1109. doi: 10.1016/j.soard.2017.03.022. [DOI] [PubMed] [Google Scholar]
- 12.Di Lorenzo N, Antoniou SA, Batterham RL, Busetto L, Godoroja D, Iossa A, et al. Clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) on bariatric surgery: update 2020 endorsed by IFSO-EC. EASO and ESPCOP Surgical endoscopy. 2020;34(6):2332–2358. doi: 10.1007/s00464-020-07555-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Proczko MA, Stepaniak PS, de Quelerij M, van der Lely FH, Smulders JF, Kaska L, et al. STOP-Bang and the effect on patient outcome and length of hospital stay when patients are not using continuous positive airway pressure. J Anesth. 2014;28(6):891–897. doi: 10.1007/s00540-014-1848-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jonas DE, Amick HR, Feltner C, Weber RP, Arvanitis M, Stine A, et al. Screening for obstructive sleep apnea in adults: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2017;317(4):415–433. doi: 10.1001/jama.2016.19635. [DOI] [PubMed] [Google Scholar]
- 15.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173–178. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wozniak DR, Lasserson TJ, Smith I. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. The Cochrane database of systematic reviews. 2014(1):CD007736. [DOI] [PubMed]
- 17.Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–1737. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 18.van Veldhuisen SL, Kuppens K, de Raaff CAL, Wiezer MJ, de Castro SMM, van Veen RN, et al. Protocol of a multicentre, prospective cohort study that evaluates cost-effectiveness of two perioperative care strategies for potential obstructive sleep apnoea in morbidly obese patients undergoing bariatric surgery. BMJ Open. 2020;10(10):e038830. doi: 10.1136/bmjopen-2020-038830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 20.Chasens ER, Ratcliffe SJ, Weaver TE. Development of the FOSQ-10: a short version of the Functional Outcomes of Sleep Questionnaire. Sleep. 2009;32(7):915–919. doi: 10.1093/sleep/32.7.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peromaa-Haavisto P, Tuomilehto H, Kossi J, Virtanen J, Luostarinen M, Pihlajamaki J et al (2016) Prevalence of obstructive sleep apnoea among patients admitted for bariatric surgery. a prospective multicentre trial. Obes Surg 26(7):1384–90 [DOI] [PubMed]
- 23.O’Reilly E, Doherty L, O’Boyle C (2019) How relevant is pre-operative obstructive sleep apnoea in the asymptomatic bariatric surgery patient? Obes Surg [DOI] [PubMed]
- 24.Jensen C, Tejirian T, Lewis C, Yadegar J, Dutson E, Mehran A. Postoperative CPAP and BiPAP use can be safely omitted after laparoscopic Roux-en-Y gastric bypass. Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery. 2008;4(4):512–514. doi: 10.1016/j.soard.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 25.Guralnick AS, Pant M, Minhaj M, Sweitzer BJ, Mokhlesi B. CPAP adherence in patients with newly diagnosed obstructive sleep apnea prior to elective surgery. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2012;8(5):501–506. doi: 10.5664/jcsm.2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine Systematic Review, Meta-Analysis, and GRADE Assessment. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2019;15(2):301–334. doi: 10.5664/jcsm.7638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lankford DA, Proctor CD, Richard R. Continuous positive airway pressure (CPAP) changes in bariatric surgery patients undergoing rapid weight loss. Obes Surg. 2005;15(3):336–341. doi: 10.1381/0960892053576749. [DOI] [PubMed] [Google Scholar]
- 28.Timmerman M, Basille D, Basille-Fantinato A, Baud ME, Rebibo L, Andrejak C, et al. Short-term assessment of obstructive sleep apnea syndrome remission rate after sleeve gastrectomy: a cohort study. Obes Surg. 2019;29(11):3690–3697. doi: 10.1007/s11695-019-04110-0. [DOI] [PubMed] [Google Scholar]
- 29.van Veldhuisen SL, Arslan I, Deden LN, Aarts EO, Hazebroek EJ. Safety of continuous postoperative pulse oximetry monitoring without obstructive sleep apnea screening in > 5000 patients undergoing bariatric surgery. Obes Surg. 2020;30(3):1079–1085. doi: 10.1007/s11695-019-04297-2. [DOI] [PubMed] [Google Scholar]
- 30.Chung F, Liao P, Yegneswaran B, Shapiro CM, Kang W. Postoperative changes in sleep-disordered breathing and sleep architecture in patients with obstructive sleep apnea. Anesthesiology. 2014;120(2):287–298. doi: 10.1097/ALN.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 31.Dusart C, Andre S, Mettay T, Bruyneel M (2022) Telemonitoring for the follow-up of obstructive sleep apnea patients treated with CPAP: accuracy and impact on therapy. Sensors (Basel) 22(7) [DOI] [PMC free article] [PubMed]
- 32.Berends F, Aarts EO (2020) Preoperative screening and treatment of OSA is like using a sledgehammer for cracking nuts. Obes Surg [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.