Abstract
Brazil has been severely affected by the COVID-19 pandemic with one of the largest numbers of youth impacted by school closure globally. This longitudinal online survey assessed emotional problems in children and adolescents aged 5–17 years living in Brazil during the COVID-19 pandemic. Recruitment occurred between June to November 2020 and participants were invited for follow-up assessments every 15 days until June 2021. Participants were 5795 children and adolescents living across the country with mean age of 10.7 (SD 3.63) years at recruitment; 50.5% were boys and 69% of white ethnicity. Weighted prevalence rates of anxiety, depressive and total emotional symptoms at baseline were 29.7%, 36.1% and 36%, respectively. Longitudinal analysis included 3221 (55.6%) participants and revealed fluctuations in anxiety and depressive symptoms during one year follow-up, associated with periods of social mobility and mortality. Emotional problems significantly increased in July and September 2020 and decreased from December 2020 to February 2021 and then significantly increased in May 2021 relative to June 2020. Older age, feeling lonely, previous diagnosis of mental or neurodevelopmental disorder, previous exposure to traumatic events or psychological aggression, parental psychopathology, and sleeping less than 8/h a day were associated with increased rates of anxiety and depressive symptoms at baseline and over time. Food insecurity and less social contact with family and peers were associated with baseline anxiety and depressive symptoms, and lowest socio-economic strata, chronic disease requiring treatment and family members physically ill due to COVID-19 were associated with increasing rates over time. The pandemic severely affected youth, particularly those from vulnerable populations and in moments of increased mortality and decreased social mobility. Results underscore the need for allocation of resources to services and the continuous monitoring of mental health problems among children and adolescents.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00787-022-02006-6.
Keywords: COVID-19, Brazil, Anxiety, Depression, Children, Adolescents
Introduction
Brazil has been severely affected by the COVID-19 pandemic, with over 643,000 deaths by mid-February 2022 [1]. In Brazil, schools were fully closed (that is, providing only remote classes or no classes at all) for the fifth longest period of time across all countries in the world between March 2020 and February 2021; Brazil also has the largest number of students impacted by the pandemic globally, with around 44.3 million students having missed almost all classroom instruction time in this period [2]. School restrictions remained from March 2020 to June 2021, which imposed the exposure to a number of risk factors for mental disorders, mainly in vulnerable populations.
School closures have disrupted the routine of children, adolescents and their families, leading to irregular sleep time and more sedentary behavior, increasing screen time and limiting peer interactions. Schools are also a paramount environment for protection and support of children living in poverty. Remote study imposed an extra burden on parents who had to supervise their child's learning, which could have had a negative impact on their relationship [3]. In addition to exposure to these risk situations, a large number of children experienced the illness and death of family members, with estimated rates of 2.4:1000 children experiencing the death of a primary caregiver, one of the highest in the world [4]. This scenario raises concerns about the mental health of youth, especially considering the scarce access to services, with estimates that only 20% of children with mental disorders in urban settings of the most wealthy cities in the country have access to them [4]. Pre-pandemic data indicate that around 13.4% of them have a mental disorder [6], and these numbers might be even higher when considering subthreshold cases [7–10].
To date, evidence regarding mental health during the pandemic is heterogeneous, with some studies suggesting an increase in psychopathology levels, while others document no significant changes [11–19], and is limited in Brazil. It is, therefore, crucial to document the impact of the pandemic on the mental health of children and adolescents in this heavily affected population. We expect children of lower socio-economic status, with greater previous exposure to adversities, with parents presenting higher levels of psychopathology, living in families with more conflict, without structured routines, with previous psychiatric diagnosis, and in families more exposed to COVID to be especially vulnerable [20].
The project Jovens na Pandemia (https://www.jovensnapandemia.com.br/) is a longitudinal online survey that tracked the mental health of children and adolescents living in Brazil during the pandemic. The aim of the study was to estimate the prevalence of emotional (depression and anxiety) problems, to follow the course of the problems during the pandemic, and to identify factors associated with increased risk.
Methods
Design
We conducted a longitudinal online survey assessing a convenience sample of children and adolescents living in Brazil. Recruitment occurred through advertisements on social media and the study website between June to November 2020 and participants were invited for follow-up assessments every 15 days until June 2021 (see supplementary material for further details).
Participants
Parents or legal guardians of children and adolescents between 5 and 17 years living in Brazil during the COVID-19 pandemic were recruited. Eligibility criteria were: individuals aged 5–17 years living in Brazil and parents in contact with their children in the last 15 days. If the parent/guardian had two or more children in this age range, one child was randomly selected in real time using a randomization function written in the Research Electronic Data Capture (RedCap) [21, 22].
Between June and November 2020, 10,226 registries were recorded. After deleting duplicates and incomplete responses on outcome measures, 5795 valid participants remained. The numbers of participants who completed every follow-up assessment are shown in Table S2. Mean age at baseline was 10.7 (SD 3.63) years, 50.5% were boys and 69% of white ethnicity. Participants came from all states of the country, mostly from the Southeast region (63.6%), followed by South (19.3%), Northeast (10.1%), Central-East (5.7%), and North (2.1%). Longitudinal analysis included 3221 (55.6%) participants. Table 1 shows characteristics of the sample.
Table 1.
Characteristics of the sample
| Variable | ||||
|---|---|---|---|---|
| Baseline (n = 5795) | Follow-up (n = 3224) | Dropout | ESa | |
| Age, mean (S.D.) | 10.70 (3.63) | 10.6 (3.61) | 10.9 (3.67) | 0.077** |
| Age range (y), n (%) | ||||
| 5–9 years | 2365 (40.81) | 1349 (41.84) | 1016 (39.49) | 0.042** |
| 10–13 years | 1855 (32.01) | 1052 (32.63) | 804 (31.25) | |
| 14–17 years | 1575 (27.18) | 823 (25.53) | 753 (29.26) | |
| Sex, n (%) | ||||
| Male | 2942 (50.77) | 1653 (51.27) | 1288 (50.06) | – |
| Female | 2853 (49.23) | 1571 (48.73) | 1285 (49.94) | |
| Ethnicity, n (%) | ||||
| White | 4010 (69.20) | 2310 (71.65) | 1701 (66.10) | 0.059*** |
| Non-white | 1785 (30.80) | 914 (28.35) | 872 (33.90) | |
| Parental education, n (%) | ||||
| Tertiary education or higher | 3912 (67.51) | 190 (5.89) | 244 (9.48) | 0.168*** |
| Up to upper secondary education | 1449 (25.00) | 630 (19.54) | 820 (31.87) | |
| Up to lower secondary education | 434 (7.49) | 2404 (74.57) | 1509 (58.65) | |
| Monthly income (in BRL), n (%) | ||||
| > 10,000 | 944 (16.29) | 626 (19.42) | 318 (12.36) | 0.175*** |
| 3000–10000 | 2201 (37.99) | 1356 (42.06) | 847 (32.93) | |
| 1000–3000 | 2002 (34.55) | 991 (30.74) | 1013 (39.39) | |
| < 1,000 | 647(11.17) | 251 (7.78) | 394 (15.31) | |
| COVID family exposure, n (%) | ||||
| Suspected or confirmed COVID in child | 457 (7.88) | 256 (7.94) | 200 (7.77) | - |
| Suspected or confirmed COVID in household member19 | 1348 (23.26) | 735 (22.80) | 614 (23.86) | - |
| Family member admitted to hospital due to COVID-19 | 205 (3.53) | 110 (3.41) | 95 (3.69) | - |
| Food insecurity, n (%) | 2254 (38.90) | 1068 (33.15) | 1187 (46.13) | 0.131*** |
| Social contact with peersb, n (%) | ||||
| Daily | 2658 (45.87) | 1061 (32.95) | 988 (38.40) | 0.060*** |
| 3–5 times a week or every 2–3 days | 1085 (18.72) | 650 (20.19) | 436 (16.94) | |
| Less than 3 times per week | 2052 (35.41) | 1509 (46.86) | 1149 (44.66) | |
| How often the child/adolescent felt lonelyb, n(%) | ||||
| Never/almost never | 1854(33.04) | 1020 (32.25) | 832 (34.06) | - |
| A few times | 2980(53.10) | 1675 (52.96) | 1299 (53.17) | |
| Often | 77 (13.86) | 468 (14.79) | 312 (12.77) | |
| The child / adolescent is not studying, n (%) | 528 (9.11) | 231 (11.50) | 296 (7.17) | 0.074*** |
| Hours spent by child / adolescent in digital activities, n (%) | ||||
| Less than 5 h | 1737 (30.48) | 743 (29.38) | 996 (31.47) | - |
| More than 5 h | 3962 (69.52) | 1786 (70.62) | 2169 (68.53) | |
| Absence of structured family routine, n (%) | 1578 (27.23) | 769 (23.91) | 807 (31.64) | 0.082*** |
| Hours of sleep, n (%) | ||||
| More than 10 h /day | 648 (11.18) | 368 (11.45) | 280 (10.88) | 0.049** |
| 8–10 h/day | 3390 (58.50) | 1934 (60.17) | 1450 (56.35) | |
| Less than 8hs/day | 1707 (29.46) | 890 (27.69) | 815 (31.67) | |
| No information | 50 (0.86) | 22 (0.69) | 28 (1.10) | |
| Child victimization, mean (S.D.) | ||||
| Previous exposure to traumatic eventsc | 0.59 (1.12) | 0.634 (1.16) | 0.553 (1.08) | 0.071** |
| Physical maltreatmentd | 0.12 (0.51) | 011(0.47) | 0.14(0.56) | 0.063** |
| Psychological aggressiond | 2.90 (2.13) | 2.88 (2.13) | 2.91 (2.15) | - |
| Neglectd | 2.46 (2.27) | 2.44 (2.23) | 2.48 (2.33) | - |
| Corporal punishmentd | 0.95 (1.73) | 0.86 (1.63) | 1.07 (1.86) | 0.117*** |
| Child’s health, n (%) | ||||
| Chronic disease, needing treatment | 1069 (18.45) | 574 (17.86) | 493 (19.16) | - |
| Previous psychiatric diagnosis | 736 (12.70) | 438 (13.63) | 297 (11.54) | 0.030** |
| Parental psychopathology | ||||
| DASS-21, mean (S.D.) | 16.36 (13.07) | 17.1 (12.5) | 15.4 (13.7) | 0.127*** |
| Parent substance abuse, n(%) | 1060 (18.29) | 629 (19.51) | 431 (16.75) | 0.035*** |
| RCADS, mean (S.D.) | ||||
| Total | 60.07 (14.71) | 60.3 (14.4) | 59.8 (15.1) | - |
| Depression | 60.21 (14.57) | 60.5 (14.5) | 59.9 (14.7) | - |
| Anxiety | 57.14 (13.30) | 57.4 (13.2) | 56.9 (13.4) | - |
DASS-21 = Depression Anxiety Stress Scales (DASS-21)
ES = effect size
aChi-square tests were used for tabular data and t-tests for continuous data. Effect sizes were calculated using Cramer’s V for chi-square test and Cohen’s d for t-tests
bParticipants were asked about the previous 2 weeks. Social contact included internet contact
cTraumatic events include traffic accidents, serious fire, natural disasters, witnessing or suffering a violent crime, physical or sexual abuse
dChild maltreatment was assessed by asking the primary caregiver about the previous two weeks
*p < 0.05
**p < 0.01
***p < 0.001
Measures
Parents or legal guardians completed questionnaires via a secure web-based software platform designed to support data capture and management, RedCap, hosted at the University of São Paulo. At baseline, participants accessed the survey platform through the study website, which contained a detailed description of the study along with a link to access the survey platform. Follow-up assessments were accessed through a link sent by email every 15 days. The contact of the study manager was available for further information if necessary.
Demographic and socio-economic variables collected included age, sex, ethnicity, parental education, income, food insecurity, and previous diagnosis of a chronic or mental health disorder. Risk factors related to the pandemic included contact with peers, loneliness, disruption of daily routine, hours of sleep, study routine, time spent using electronic devices, suspected or confirmed infection by COVID-19, admission to hospital or death in household members due to COVID-19.
Emotional problems were assessed with the 25-item version of the Revised Children's Anxiety and Depression Scale, parents version (RCADS-25-P)[23]. The RCADS is a 25-item scale that measures the frequency of anxiety and low mood symptoms using a 4-point Likert scale (“never”, “sometimes”, “often”, and “always”) based on personal observations from parents or legal guardians. The scale has two subscales assessing Anxiety and Depression, and an overall score. Raw scores are converted to T-scores, with higher scores representing more symptoms. T-scores can also be categorized according to their range, specifically: < 65 (low severity of symptoms, normal); 65–70 (medium severity, borderline clinical threshold), and > 70 (high severity, clinical symptoms).
Previous child victimization was assessed by questioning if the child had ever suffered or witnessed any traumatic event (such as a traffic accident or severe violence) in any time of their lives. We also assessed child maltreatment in the previous two weeks using an adapted version of the Conflict Tactics Scales: Parent–Child Version (CTSPC). The CTSPC assesses parenting behaviors associated with physical and psychological child maltreatment. The original scale consists of 22 items divided into three dimensions: Nonviolent Discipline, Psychological Aggression, and Physical Aggression (subdivided into corporal punishment, physical maltreatment, and severe physical maltreatment) and has been validated in Brazil [24]. There are also two additional subscales, neglect and sexual abuse [25]. We used questions from the Psychological Aggression and Physical Aggression dimensions and the neglect subscale. Questions on severe physical maltreatment were removed. Parents/Guardians were asked to report how often the cited behavior (eg., "shook him/her") had happened in the previous two weeks ("never", "once", "more than once").
Parental psychopathology was assessed with the Depression, Anxiety and Stress Scale—Short Form (DASS-21) [26] and the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) [27]. The DASS-21 is a 21-item self-report scale covering internalizing symptoms in depressive, anxiety and stress domains. The parent/legal guardian was asked which of 21 statements (e.g., "I found it hard to wind down") applied to them in the past two weeks using a 4-point Likert scale (from 0—"did not apply to me at all" to 3—"applied to me very much or most of the time"). The ASSIST is a 7-item scale developed by the World Health Organization to assess the use of alcohol, tobacco and other psychoactive substances and has been validated for the Brazilian population [27]. Only frequency of use in the previous two weeks was considered. Scores were aggregated as a binary variable (abusive use vs non-abusive). Abusive use was defined as using any substance more than three times in the previous two weeks.
Statistical analysis
Prevalence of emotional problems, measured with the RCADS-P (total, depression, and anxiety scores) at baseline, was estimated using raking ratio to weight raw data based on selected characteristics of the Brazilian population from the last Continuous National Household Sample Survey (PNAD Contínua)[28] (see supplementary material for details). To investigate risk factors for emotional problems at baseline, we ran stepwise logistic regression models with RCADS categorized scores (total, depression, and anxiety) as response variables, and baseline variables as explanatory variables. The RCADS T-scores > 65 (borderline and clinical symptoms) were collapsed into a single category for the baseline analysis. To investigate the effects of time on emotional symptoms, we ran stepwise linear mixed effect models using continuous RCADS T-scores (total, depression, and anxiety) as response variable and baseline variables as explanatory variables. For these longitudinal analyses, time represented the date of assessment, i.e., the time in the pandemic. We included all participants who reported at least one time-point of data using full information maximum likelihood (FIML) estimation. We also compared participants who dropped out of the study after baseline with participants who completed at least one follow-up assessment using Chi-square tests and t-tests, with effect sizes calculated for significant tests using Cramer’s V and Cohen’s d, respectively. The following reference values were used for assessing effect sizes: Cohen’s d: 0.2, 0.5, 0.8 for small, medium, and large, respectively; Cramer’s V: 0.07, 0.21, and 0.35 for small, medium, and large, respectively [29].
All analyses were conducted in R [30] (see supplementary materials for details). Scripts and analysis documentation are available in OSF (https://osf.io/qgb5v/).
Ethics approval and consent
All parents/guardians provided written informed consent. All study procedures were approved by the HCFMUSP ethics committee (CAE 36011120.9.0000.0068).
Results
At baseline, weighted prevalence rates of borderline and clinical emotional problems, anxiety and depressive symptoms only were 36%, 29.7% and 36.1%, respectively.
Characteristics associated with RCADS total, depressive, and anxiety symptoms at baseline are presented in Table 2. The following characteristics were associated with increased rates of anxiety and depressive symptoms: older age, feeling lonely, previous diagnosis of mental or neurodevelopmental disorder, previous exposure to traumatic events or psychological aggression, higher levels of parental psychopathology, sleeping less than 8/h a day, food insecurity, and less social contact with family and peers. Having a member admitted to hospital due to COVID-19 and absence of structured family routine were associated with depressive symptoms only. Having a previous chronic disease requiring treatment was associated with anxiety symptoms only. Female sex was associated with less anxiety symptoms.
Table 2.
Logistic regression models of association between baseline variables and emotional problems measured by the RCDAS
| Variable | RCADS scores [Odds Ratio (95%CI)] | ||
|---|---|---|---|
| Total | Depression | Anxiety | |
| Age | |||
| 5–9 years | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 10–13 years | 1.76 (1.50–2.07)*** | 1.20 (1.02–1.42) | 1.31 (1.11–1.55)** |
| 14–17 years | 1.36 (1.13–1.65)** | 1.33 (1.09–1.61)** | 1.42 (1.18–1.71)*** |
| Sex | |||
| Male | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Female | 1.34 (1.17–1.53)*** | – | 0.83 (0.73–0.95)** |
| Parental education | |||
| Tertiary education or higher | |||
| Up to upper secondary education | – | – | – |
| Up to lower secondary education | |||
| Monthly Income (in BRL) | |||
| > 10,000 | 1 [ Reference] | 1 [Reference] | 1 [Reference] |
| 3000–10,000 | 1.09 (0.89–1.34) | – | 0.98 (0.80–1.21) |
| 1000–3000 | 1.09 (0.88–1.35) | – | 0.90 (0.71–1.13) |
| < 1000 | 1.40 (1.07–1.84)* | – | 1.21 (0.91–1.62) |
| COVID family exposure | |||
| Family member physically ill due to COVID-19 | – | – | – |
| Family member admitted to hospital due to COVID-19 | 1.39 (0.98–1.95) | 1.48 (1.04–2.09)* | 1.31 (0.93–1.83) |
| Food insecurity | 1.22 (1.06–1.40)** | 1.18 (1.01–1.38)* | |
| Social contact with peers in the previous 2 weeks (including through internet) | |||
| Daily | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 3–5 times a week or every 2–3 days | 1.16 (0.97–1.39) | 1.10 (0.91–1.33) | 1.17 (0.97–1.41) |
| Less than 3 times per week | 1.27 (1.08–1.49)** | 1.28 (1.09–1.50)** | 1.28 (1.09–1.50)** |
| How often the child/adolescent felt lonely in the previous 2 weeks | |||
| Never/almost never | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| A few times | 3.50 (2.94–4.19)*** | 3.62 (3.03– 4.33)*** | 2.45 (2.06–2.9)*** |
| Often | 11.55 (9.16–14.61)*** | 14.36 (11.32–18.30)*** | 6.31 (5.07–7.88)*** |
| Absence of structured family routine | 1.41 (1.21–1.64)*** | 1.72 (1.48– 2.00)*** | – |
| Hours of sleep | |||
| More than 10 h /day | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 8–10 h/day | 1.07 (0.86–1.34) | 0.90 (0.73–1.13) | 1.05 (0.85–1.32) |
| Less than 8hs/day | 1.47 (1.17–1.85)** | 1.35 (1.07–1.71)* | 1.26 (1.00–1.59)* |
| No information | 1.69 (0.84–3.38) | 2.01 (0.99–4.11) | 1.58 (0.76–3.15) |
| Child victimization | |||
| Previous exposure to traumatic eventsa | 1.11 (1.05–1.18)*** | 1.10 (1.04– 1.17)** | 1.12 (1.06–1.19)*** |
| Physical maltreatmentb | 1.12 (0.98–1.28) | 1.11 (0.97–1.27) | –- |
| Psychological aggressionb | 1.07 (1.03–1.10)*** | 1.14 (1.10–1.18)*** | 1.05 (1.01–1.08)** |
| Neglectb | 1.06 (1.02–1.09)*** | 1.08 (1.05–1.12)*** | – |
| Child’s health | |||
| Chronic disease, needing treatment | – | – | 1.29 (1.09–1.52)** |
| Previous psychiatric diagnosis | 2.26 (1.87–2.74)*** | 2.48 (2.05–3.02)*** | 1.90 (1.58–2.28)*** |
| Parental psychopathology (DASS-21) | 1.03 (1.02–1.03)*** | 1.02 (1.02– 1.03)*** | 1.02 (1.02–1.03)*** |
Odds Ratio > 1 and < 1 indicate variables associated with increased and decreased risk, respectively
CI = Confidence interval
–Variable dropped after stepwise regression
DASS-21 Depression Anxiety Stress Scales (DASS-21)
aTraumatic events include traffic accidents, serious fire, natural disasters, witnessing or suffering a violent crime, physical or sexual abuse in any period of life
bChild maltreatment by child primary caregiver in the previous two weeks
*p < 0.05
**p < 0.01
***p < 0.001
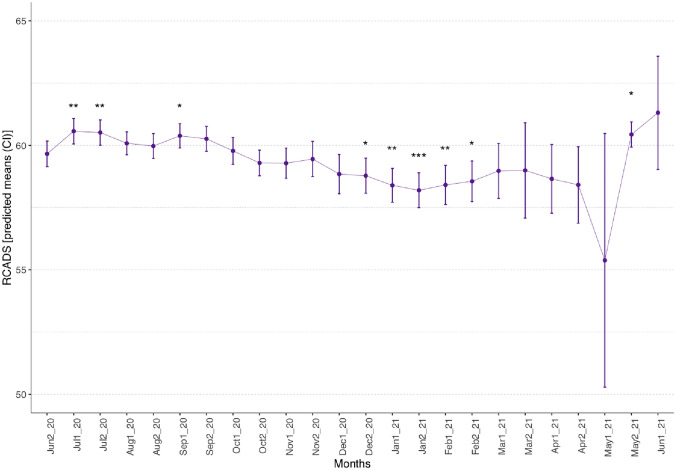
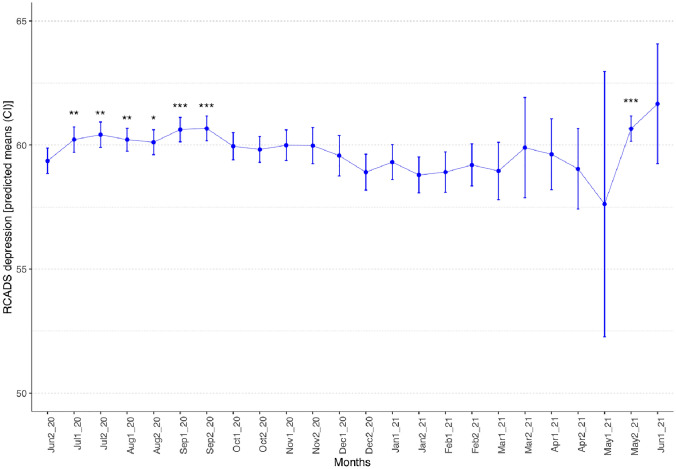
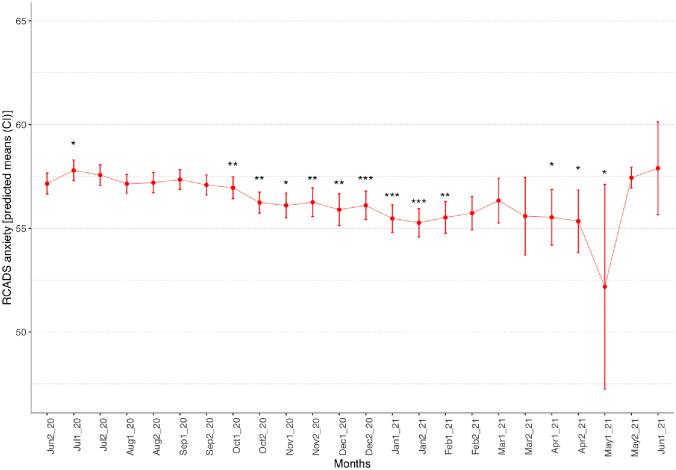
From June 2020 to June 2021, emotional problems significantly increased in July and September 2020 and decreased from December 2020 to February 2021, and then significantly increased in May 2021 (Fig. 1) relative to June 2020. Depressive symptoms significantly increased from July to September 2020, then again significantly increased in May 2021 (Fig. 2) relative to June 2020. Anxiety symptoms significantly increased in July 2020, and significantly decreased from October 2020 to February 2021, and April to May 2021 Fig. 3.
Fig. 1.
Estimated marginal means for emotional problems measured from June 2020 to June 2021 using the RCADS total T-score. Bars represent 95% confidence intervals (CI). *p < 0.05, **p < 0.01, ***p < 0.001
Fig. 2.
Estimated marginal means for depression symptoms measured from June 2020 to June 2021 using the RCADS depression T-score. Bars represent 95% confidence intervals (CI). *p < 0.05, **p < 0.01, ***p < 0.001
Fig. 3.
Estimated marginal means for anxiety symptoms measured from June 2020 to June 2021 using the RCADS anxiety T-score. Bars represent 95% confidence intervals (CI). *p < 0.05, **p < 0.01, ***p < 0.001
Baseline characteristics associated with RCADS total, depressive, and anxiety symptoms during follow-up are presented in Table 3. The following characteristics were associated with increased rates of anxiety and depressive symptoms: older age, feeling lonely, previous diagnosis of mental or neurodevelopmental disorder, lowest socio-economic strata, chronic disease requiring treatment, sleeping less than 8 h per day, exposure to previous traumatic experiences or psychological aggression, higher levels of parental psychopathology, and having a family member physically ill due to COVID-19. Female sex, absence of structured family routine, and physical maltreatment or neglect were associated with depressive symptoms and less formal education and food insecurity were associated with anxiety symptoms only during follow-up.
Table 3.
RCDAS scores at follow-up (stepwise mixed linear model)
| Variable | RCADS scores [β (95% CI)] | ||
|---|---|---|---|
| Total | Depression | Anxiety | |
| Age | |||
| 5–9 years | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 10–13 years | 3.50 (2.73–4.26)*** | 1.96 (1.27–2.64)*** | 0.73 (0.02–1.45)* |
| 14–17 years | 1.33 (0.44–2.22)** | 1.05 (0.27–1.83)*** | 1.13 (0.33–1.93)** |
| Sex | |||
| Male | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Female | 2.41 (1.79–3.02)*** | 1.19 (0.62–1.76)*** | – |
| Parental education | |||
| Tertiary education or higher | 1 [Reference] | – | 1 [Reference] |
| up to upper secondary education | – 0.78 ( – 1.61 to 0.04) | – | – 0.53 ( – 1.34 to 0.27) |
| up to lower secondary education | 0.89 ( – 0.36 to 2.13) | – | 1.36 (0.14–2.57)* |
| Monthly income (in BRL) | |||
| > 10,000 | 1 [ Reference] | 1 [Reference] | 1 [Reference] |
| 3000–10,000 | 0.66 ( – 0.24 to 1.56) | 0.38 ( – 0.45 to 1.20) | 0.72 ( – 0.16 to 1.60) |
| 1000–3000 | 1.26 (0.26–2.26)** | 1.17 (0.30–2.04)** | 0.83 ( – 0.18 to 1.8) |
| < 1000 | 3.15 (1.80–4.50)*** | 2.07 (0.91–3.24)** | 2.67 (1.30–4.05)*** |
| COVID family exposure | |||
| Family member physically ill due to COVID-19 | 0.91 (0.16–1.67)* | 0.99 (0.32–1.67)** | 0.78 (0.07–1.50)* |
| Family member admitted to hospital due to COVID-19 | 1.77 (0.07–3.48)* | – | – |
| Food insecurity | – | – | 1.01 (0.29–1.73)** |
| Social contact with peers in the previous 2 weeks (including through internet) | |||
| Daily | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 3–5 times a week or every 2–3 days | 0.48 (-0.37–1.33) | – | – |
| Less than 3 times per week | 0.95 (0.20–1.69)* | – | – |
| How often the child/adolescent felt lonely in the previous 2 weeks | |||
| Never/almost never | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| A few times | 6.27 (5.56–6.97)*** | 6.13 (5.48–6.78)*** | 5.03 (4.35–5.71)*** |
| Often | 14.68 (13.61–15.74)*** | 15.21 (14.23–16.20)*** | 11.18 (10.07–12.08)*** |
| Absence of structured family routine | 2.32 (1.57– 3.07)*** | 3.42 (2.72–4.11)*** | −−− |
| Hours of sleep | |||
| More than 10 h /day | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 8–10 h/day | 0.44 ( – 0.57 to 1.44) | – 0.67 ( – 1.61 to 0.26) | 0.29 ( – 0.68 to 1.26) |
| Less than 8hs/day | 2.10 (1.01–3.18)*** | 1.32 (0.32–2.33)* | 1.27 (0.22–2.32)* |
| No information | 2.12 ( – 1.49 to 5.74) | 2.02 ( – 1.35 to 5.40) | – 5.20 ( – 4.04 to 3.01) |
| Child victimizationa | |||
| Previous exposure to traumatic events | 0.82 (0.54–1.10)*** | 0.68 (0.42–0.94)*** | 0.89 (0.61–1.16)*** |
| Physical maltreatment | 0.65 (0.01–1.29) | 0.89 (0.29–1.49)** | – |
| Psychological aggression | 0.53 (0.37–0.69)*** | 0.82 (0.67– 0.97)*** | 0.29 (0.14–0.44)*** |
| Neglect | 0.35 (0.20–0.50)*** | 0.55 (0.41–0.69)*** | – |
| Child’s health | |||
| Chronic disease, needing treatment | 1.47 (0.67–2.26)*** | 1.39 (0.65–2.12)*** | 1.50 (0.72–2.27)*** |
| Previous psychiatric diagnosis | 5.89 (5.96–6.83)*** | 6.69 (5.83–7.56)*** | 4.52 (3.61–5.42)*** |
| Parental psychopathology (DASS-21) | 0.20 (0.18–0.23)*** | 0.19 (0.16–0.21)*** | 0.17 (0.15–0.20)*** |
CI confidence interval
–Coefficients not shown. Variable dropped after stepwise regression
DASS-21 = Depression Anxiety Stress Scales (DASS-21)
Coefficients for time factors not shown
aChild maltreatment by child primary caregiver in the previous two weeks
*p < 0.05
**p < 0.01
***p < 0.001
We performed comparisons between participants who completed only the baseline and participants who completed at least one follow-up assessment (Table 1). Groups were significantly different with small to moderate effect sizes. In the group who dropped out of the study, there was a higher proportion of participants from lower socio-economic strata (V = 0.175), with food insecurity (V = 0.131), exposure to corporal punishment (d = 0.117) but less parental psychopathology (d = 0.127). Moreover, the proportion of participants in this group with tertiary education or up to secondary education was higher relative to participants who completed at least one follow-up (V = 0.168). Differences between groups were also significant for age range, ethnicity, social contact, hours of sleep, physical maltreatment, previous psychiatric diagnosis, parent substance abuse, exposure to previous traumatic events, and parental psychopathology but all of these difference had very small effect sizes (< 0.07 or 0.2 for Cramer’s V and Cohen’s d, respectively).
We analyzed response rates per time-point (Table S2). Response rates decreased throughout the project, with the lowest rate in the first half of May 2021. In the second half of May 2021, we announced to participants that we would conduct one more round of assessments before closing the project, which resulted in the increase of response rate in the second half of May.
We also compared participants whose baseline assessment was conducted early (from June to August 2020) with participants whose baseline was conducted late (from September to November 2020) during the study. In the early phase of the project, 4658 participants completed baseline, and 1137 participants completed baseline at the late stage. Both the prevalences and mean RCDAS scores did not significantly differ between early and late stages (Table S3).
Discussion
Our study assessed 5795 children and adolescents in Brazil and indicated that approximately 1 in 3 presented emotional, depression, or anxiety symptoms from June to November 2020. A number of risk factors associated with higher symptoms at baseline and follow-up were identified. There were slight fluctuations in emotional problems during one year follow-up, but no sustained increase. These are relevant data from an understudied and highly affected population, and underscore a high number of children and adolescents with emotional symptoms during the pandemic.
Rates documented in this study are considerably higher than those from a previous estimate of psychiatric disorders in a sample with similar characteristics [31] and the rate of 1 in 6 young people reported in England during the same time-frame [32]. Though we have no pre-pandemic data for comparison, these rates are consistent with recent estimates from the Global Burden of Disease Study that indicates increased risk for depressive and anxiety symptoms among youth and in moments with high rates of infection and reduced human mobility, which corresponds to our study period [33].
Our study identified several risk factors for emotional, depression, and anxiety symptoms both at baseline and follow-up. Loneliness was the predictor with the highest impact, followed by previous psychiatric diagnosis, having a previous chronic disease requiring treatment, higher levels of parental psychopathology, previous exposure to traumatic events, as well as socio-economic disadvantages (lower socio-economic status and lower parental education). Symptomatology was also higher in participants exposed to factors associated with the pandemic, such as absence of structured family routine, sleeping less than 8 h per day, having less contact with family and peers, being exposed to psychological aggression or neglect, having a family member ill or admitted to hospital due to COVID-19, and food insecurity. Being female was protective against anxiety at baseline but not at follow-up.
Risk factors detected in our sample are consistent with the literature [13, 31, 34, 35] and show that there are groups that are at higher risk for developing depression and anxiety symptoms, which should be the focus of interventions. As reported by Loades et al. [36], loneliness is an important predictor of depressive symptomatology in children and adolescents and its effects may last for years. Having a chronic health condition was also associated with increased symptomatology in our sample. Other studies reported similar findings [35, 37–40]. This is not surprising, given that comorbidities represent a risk factor for more severe covid-19 presentations [41] and might be associated with higher levels of distress in both children and parents of those children [42], and more strict social distancing [43].
In our sample, child and parental psychopathology were correlated. This association is observed even in pre-pandemic times [34] due to many factors. Parents and children usually share similar risk factors (both environmental and genetic). Parents are also a coping model for their children, and children of parents with worse coping practices might also lack more adaptive practices [20]. Depressed parents might also perceive their children's behavior as more distressing, thus scoring higher in our caregiver-reported scales [44]. Parental psychopathology is also correlated with harsh or inconsistent parenting [45], another known risk factor for child mental symptoms [46]. Similarly, more severe psychopathology in their children, especially regarding externalizing symptoms, might lead parents to greater distress and disruption of routine, contributing to an increase in their own psychopathology and in less positive parenting practices [47]. It was to be expected then that children and parents' psychopathology were closely interrelated.
Exposure to previous adversities, such as child abuse, is also a possible factor for emergence of psychopathology after another incident [48] or for worse evolution patterns [49], despite some conflicting results [50]. One hypothesis for this association is the “kindling hypothesis”—previous traumatic exposure might lead to a sensitization of mental symptoms, lowering the threshold for their appearance after further events [51, 52]. Those experiences seem to be associated with neurobiological alterations that might underlie the higher susceptibility to psychopathology [53]. Finally, it is also important to consider that at-risk children often have more than one risk factor that might have a cumulative effect, possibly leading to higher levels of symptomatology [54, 55]
There were slight fluctuations in emotional problems during one year follow-up, but no sustained increase. This lack of sustained increase of psychopathology is consistent with a recent cohort study showing no evidence of pandemic-related worsening of psychopathology in Brazilian adults [13] and with a UK convenience sample reporting a stable pattern of emotional symptoms in children and adolescents from March 2020 to March 2021 [11]. In fact, whereas depressive symptoms showed an initial increase during the period between July and September 2020, with another peak in May 2021, anxiety symptoms significantly decreased from October 2020 to February 2021, and April to May 2021. The decrease in symptomatology seen from October to February might be related to a reduction in social distancing requirements that started taking place in late 2020 [56]. It is important to mention, however, that the fluctuation of the number of respondents, especially in May 2021 (table S2), might hinder interpretations regarding this month's data.
This study has limitations. First, data collection started in June 2020, approximately four months after the beginning of the pandemic. Thus, we are not able to characterize the trajectory of symptoms during this period, when an increase from the pre-pandemic period might have happened. Second, due to its design, our sample consisted mainly of participants with a higher educational level, from wealthier regions of the country, and white ethnicity. Given that completion of assessments were online, children living in poverty with no access to the internet were not included in this study. The fact that convenience samples might exclude those who are most in need of help has been a reason for criticism towards the use of online surveys to understand prevalence in the population [57]. To deal with this issue, we employed weighting procedures to account for the population characteristics. Yet, it is possible that the prevalence of emotional problems in the population is higher. It must be acknowledged that there is no representative data on the mental health of children and adolescents in Brazil before the pandemic.
Although most participants were recruited in the first two months of the project, recruitment extended until November 2020, and therefore, not all baseline assessments occurred in the same period. As circumstances and restrictions changed over time, this might have impacted the baseline data. However, we did not find differences between those who completed baseline early (from June to August) from those who completed baseline late (September to November). Moreover, findings regarding risk factors and especially the effects of time might not be generalized to the whole population. As a limitation of online surveys, we could not control the conditions of the moment parents completed the questionnaires. In addition, because of logistical limitations, we did not have reports from children and adolescents [58]. Finally, although differences between participants who dropped out of the study and participants who completed at least one follow-up were small, it must be acknowledged that participants in the follow-up group belonged to the higher socio-economic strata, were less exposed to food insecurity and child maltreatment, but the parents were more likely to have depression and anxiety symptoms. In this context, parental psychopathology is relevant as we used report measures which might be more prone to informant bias [59].
Lessons learned and consequences for the future
Results documented here indicate a high number of children affected by depressive and anxiety symptoms, especially those in more vulnerable situations. This suggests that the toll of the pandemic in severely affected countries goes beyond the number of cases of people infected and heavily affects children and adolescents. Although we did not document a sustained increase in psychopathology, fluctuations associated with moments of increased and decreased mortality and social mobility were detected.
Although it may be difficult to generalize these findings due to the methodological characteristics of our study, these data are concerning, particularly in a country that directs very restricted resources to mental health services, as is the case in a number of countries in the region and across the world. This study underscores the need for allocation of resources and implementation of indicated interventions directed to children and adolescents. Moreover, it indicates the need for continuous monitoring of mental health problems among children and adolescents in the population.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank all participants for their time and engagement in data collection during this challenging period.
Author contributions
Conceptualization: Casella, Fatori, Zuccolo, Polanczyk. Data curation: Teixeira, Argeu, Zuccolo. Formal analysis: Zuccolo. Methodology: all authors. Interpretation of the data: all authors. Project administration: Casella, Zuccolo. Supervision: Polanczyk. Visualization: Zuccolo, Casella, Sugaya. Writing: Casella, Fatori, Shephard, Zuccolo, Polanczyk.
Funding
This study was supported by São Paulo Research Foundation (FAPESP, grant 2016/22455–8) and National Council for Scientific and Technological Development (CNPq, grant 310582/2017–2). The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Declarations
Conflict of interest
GVP has been in the past 3 years a member of advisory board of Shire/Takeda, Aché and Medice and a speaker for Shire/Takeda, Novo Nordisk and Aché. All other authors report no conflicts of interest.
Footnotes
Pedro Fonseca Zuccolo and Caio Borba Casella: Joint first authors
References
- 1.Brazil: WHO Coronavirus Disease (COVID-19) Dashboard with Vaccination Data. https://covid19.who.int. Accessed 22 Feb 2022
- 2.(2021) COVID-19 and School Closures: One year of education disruption. In: UNICEF DATA. https://data.unicef.org/resources/one-year-of-covid-19-and-school-closures/. Accessed 12 Jul 2021
- 3.Almeida M, Challa M, Ribeiro M, et al. Editorial perspective: The mental health impact of school closures during the COVID-19 pandemic. J Child Psychol Psychiatry 10.1111/jcpp.13535 [DOI] [PMC free article] [PubMed]
- 4.Hillis SD, Unwin HJT, Chen Y, et al. Global minimum estimates of children affected by COVID-19-associated orphanhood and deaths of caregivers: a modelling study. The Lancet. 2021;398:391–402. doi: 10.1016/S0140-6736(21)01253-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fatori D, Salum G, Itria A, et al. (2018) The economic impact of subthreshold and clinical childhood mental disorders. J Mental Health. 2018 doi: 10.1080/09638237.2018.1466041. [DOI] [PubMed] [Google Scholar]
- 6.Polanczyk GV, Salum GA, Sugaya LS, et al. Annual Research Review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56:345–365. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- 7.Karande S, Gogtay NJ, Bala N, et al. Anxiety symptoms in regular school students in Mumbai City. India J Postgraduate Med. 2018;64:92. doi: 10.4103/jpgm.JPGM_445_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rao W-W, Xu D-D, Cao X-L, et al. Prevalence of depressive symptoms in children and adolescents in China: A meta-analysis of observational studies. Psychiatry Res. 2019;272:790–796. doi: 10.1016/j.psychres.2018.12.133. [DOI] [PubMed] [Google Scholar]
- 9.Ma L, Gao L, Chiu DT, et al. Depressive symptoms prevalence, associated family factors, and gender differences: A national cohort study of middle school students in China. J Affect Disord. 2020;274:545–552. doi: 10.1016/j.jad.2020.05.128. [DOI] [PubMed] [Google Scholar]
- 10.Wartberg L, Kriston L, Thomasius R. Depressive symptoms in adolescents. Dtsch Arztebl Int. 2018;115:549–555. doi: 10.3238/arztebl.2018.0549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Creswell C, Shum A, Pearcey S, et al. Young people’s mental health during the COVID-19 pandemic. The Lancet Child Adolescent Health. 2021;5:535–537. doi: 10.1016/S2352-4642(21)00177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones EAK, Mitra AK, Bhuiyan AR. Impact of COVID-19 on mental health in adolescents: a systematic review. IJERPH. 2021;18:2470. doi: 10.3390/ijerph18052470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brunoni AR, Suen PJC, Bacchi PS, et al. Prevalence and risk factors of psychiatric symptoms and diagnoses before and during the COVID-19 pandemic: findings from the ELSA-Brasil COVID-19 mental health cohort. Psychol Med. 2021 doi: 10.1017/S0033291721001719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Antiporta DA, Cutipé YL, Mendoza M, et al. Depressive symptoms among Peruvian adult residents amidst a National Lockdown during the COVID-19 pandemic. BMC Psychiatry. 2021;21:111. doi: 10.1186/s12888-021-03107-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Batterham PJ, Calear AL, McCallum SM, et al. Trajectories of depression and anxiety symptoms during the COVID-19 pandemic in a representative Australian adult cohort. Medical J Australia. 2021 doi: 10.5694/mja2.51043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hu Y, Qian Y. COVID-19 and adolescent mental health in the United Kingdom. J Adolesc Health. 2021;69:26–32. doi: 10.1016/j.jadohealth.2021.04.005. [DOI] [PubMed] [Google Scholar]
- 17.Chmielewska B, Barratt I, Townsend R, et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health. 2021;9:e759–e772. doi: 10.1016/S2214-109X(21)00079-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Isumi A, Doi S, Yamaoka Y, et al. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse Negl. 2020;110:104680. doi: 10.1016/j.chiabu.2020.104680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Racine N, McArthur BA, Cooke JE, et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175:1142–1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pfefferbaum B, Jacobs AK, Houston JB, Griffin N. Children’s disaster reactions: the influence of family and social factors. Curr Psychiatry Rep. 2015;17:57. doi: 10.1007/s11920-015-0597-6. [DOI] [PubMed] [Google Scholar]
- 21.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ebesutani C, Korathu-Larson P, Nakamura BJ, et al. The revised child anxiety and depression scale 25–parent version: scale development and validation in a school-based and clinical sample. Assessment. 2017;24:712–728. doi: 10.1177/1073191115627012. [DOI] [PubMed] [Google Scholar]
- 24.Bonfim CB, Santos DN, Menezes IG, et al. Um estudo sobre a validade de construto da Parent-Child Conflict Tactics Scale (CTSPC) em uma amostra populacional urbana do Nordeste brasileiro. Cad Saúde Pública. 2011;27:2215–2226. doi: 10.1590/S0102-311X2011001100015. [DOI] [PubMed] [Google Scholar]
- 25.Straus MA, Hamby SL, Finkelhor D, et al. Identification of child maltreatment with the parent-child conflict tactics scales: development and psychometric data for a national sample of American parents. Child Abuse Negl. 1998;22:249–270. doi: 10.1016/S0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- 26.Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–239. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- 27.Henrique IFS, De Micheli D, de Lacerda RB, et al. Validação da versão brasileira do teste de triagem do envolvimento com álcool, cigarro e outras substâncias (ASSIST) Rev Assoc Med Bras. 2004;50:199–206. doi: 10.1590/S0104-42302004000200039. [DOI] [PubMed] [Google Scholar]
- 28.Sistema IBGE de Recuperação Automática - SIDRA. https://sidra.ibge.gov.br/pesquisa/pnadca/tabelas. Accessed 12 Aug 2021
- 29.FAQ/effectSize - CBU statistics Wiki. https://imaging.mrc-cbu.cam.ac.uk/statswiki/FAQ/effectSize. Accessed 9 Nov 2021
- 30.R Core Team (2020) R: A language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria
- 31.La Maison C, Munhoz TN, Santos IS, et al. Prevalence and risk factors of psychiatric disorders in early adolescence: 2004 Pelotas (Brazil) birth cohort. Soc Psychiatry Psychiatr Epidemiol. 2018;53:685–697. doi: 10.1007/s00127-018-1516-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mental Health of Children and Young People in England, 2020: Wave 1 follow up to the 2017 survey. In: NHS Digital. https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-of-children-and-young-people-in-england/2020-wave-1-follow-up. Accessed 15 Aug 2021
- 33.Santomauro DF, Mantilla Herrera AM, Shadid J, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet. 2021;398:1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li Y, Zhao J, Ma Z, et al. Mental health among college students during the COVID-19 pandemic in China: A 2-wave longitudinal survey. J Affect Disord. 2021;281:597–604. doi: 10.1016/j.jad.2020.11.109. [DOI] [PubMed] [Google Scholar]
- 35.Wu T, Jia X, Shi H, et al. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord. 2021;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59:1218–1239.e3. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Angelina S, Kurniawan A, Agung FH, et al. Adolescents’ mental health status and influential factors amid the Coronavirus Disease pandemic. Clin Epidemiol Glob Health. 2021;12:100903. doi: 10.1016/j.cegh.2021.100903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Burrows AG, Ellis AK. Psychological impacts of coronavirus disease 2019 on people with asthma, allergic rhinitis, and food allergy. Ann Allergy Asthma Immunol. 2021;S1081–1206(21):01310–1317. doi: 10.1016/j.anai.2021.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Samji H, Wu J, Ladak A, et al. Review: Mental health impacts of the COVID-19 pandemic on children and youth – a systematic review. Child and Adolescent Mental Health 10.1111/camh.12501 [DOI] [PMC free article] [PubMed]
- 40.Tso WWY, Wong RS, Tung KTS, et al. Vulnerability and resilience in children during the COVID-19 pandemic. Eur Child Adolesc Psychiatry. 2022;31:161–176. doi: 10.1007/s00787-020-01680-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tsankov BK, Allaire JM, Irvine MA, et al. Severe COVID-19 infection and pediatric comorbidities: a systematic review and meta-analysis. Int J Infect Dis. 2021;103:246–256. doi: 10.1016/j.ijid.2020.11.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wauters A, Vervoort T, Dhondt K, et al. Mental health outcomes among parents of children with a chronic disease during the COVID-19 pandemic: the role of parental burn-out. J Pediatric Psychol. 2021 doi: 10.1093/jpepsy/jsab129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Adepoju OE, Chae M, Woodard L, et al. Correlates of social isolation among community-dwelling older adults during the COVID-19 pandemic. Front Public Health. 2021;9:702965. doi: 10.3389/fpubh.2021.702965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liskola K, Raaska H, Lapinleimu H, et al. The effects of maternal depression on their perception of emotional and behavioral problems of their internationally adopted children. Child Adolesc Psychiatry Ment Health. 2021;15:41. doi: 10.1186/s13034-021-00396-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Park JL, Hudec KL, Johnston C. Parental ADHD symptoms and parenting behaviors: A meta-analytic review. Clin Psychol Rev. 2017;56:25–39. doi: 10.1016/j.cpr.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 46.Wiggins JL, Mitchell C, Hyde LW, Monk CS. Identifying early pathways of risk and resilience: The codevelopment of internalizing and externalizing symptoms and the role of harsh parenting. Dev Psychopathol. 2015;27:1295–1312. doi: 10.1017/S0954579414001412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Allmann AES, Klein DN, Kopala-Sibley DC. Bidirectional and transactional relationships between parenting styles and child symptoms of ADHD, ODD, depression, and anxiety over 6 years. Dev Psychopathol. 2021 doi: 10.1017/S0954579421000201. [DOI] [PubMed] [Google Scholar]
- 48.Cabrera OA, Hoge CW, Bliese PD, et al. Childhood adversity and combat as predictors of depression and post-traumatic stress in deployed troops. Am J Prev Med. 2007;33:77–82. doi: 10.1016/j.amepre.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 49.Kronenberg ME, Hansel TC, Brennan AM, et al. Children of Katrina: lessons learned about postdisaster symptoms and recovery patterns. Child Dev. 2010;81:1241–1259. doi: 10.1111/j.1467-8624.2010.01465.x. [DOI] [PubMed] [Google Scholar]
- 50.Inoue Y, Stickley A, Yazawa A, et al. Adverse childhood experiences, exposure to a natural disaster and posttraumatic stress disorder among survivors of the 2011 Great East Japan earthquake and tsunami. Epidemiol Psychiatr Sci. 2019;28:45–53. doi: 10.1017/S2045796017000233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Monroe SM, Harkness KL. Life stress, the “kindling” hypothesis, and the recurrence of depression: considerations from a life stress perspective. Psychol Rev. 2005;112:417–445. doi: 10.1037/0033-295X.112.2.417. [DOI] [PubMed] [Google Scholar]
- 52.Kendler KS, Thornton LM, Gardner CO. Stressful life events and previous episodes in the etiology of major depression in women: an evaluation of the “kindling” hypothesis. AJP. 2000;157:1243–1251. doi: 10.1176/appi.ajp.157.8.1243. [DOI] [PubMed] [Google Scholar]
- 53.Cacciaglia R, Nees F, Grimm O, et al. Trauma exposure relates to heightened stress, altered amygdala morphology and deficient extinction learning: Implications for psychopathology. Psychoneuroendocrinology. 2017;76:19–28. doi: 10.1016/j.psyneuen.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 54.Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psychol Bull. 2013;139:1342–1396. doi: 10.1037/a0031808. [DOI] [PubMed] [Google Scholar]
- 55.Guo J, Fu M, Liu D, et al. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse Negl. 2020;110:104667. doi: 10.1016/j.chiabu.2020.104667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Plano SP | Governo do Estado de São Paulo. In: Plano SP | Governo do Estado de São Paulo. https://www.saopaulo.sp.gov.br/planosp/. Accessed 22 Feb 2022
- 57.Pierce M, McManus S, Jessop C, et al. Says who? The significance of sampling in mental health surveys during COVID-19. The Lancet Psychiatry. 2020;7:567–568. doi: 10.1016/S2215-0366(20)30237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.De Los RA, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychol Bull. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- 59.Stone AA, Turkkan JS, Bachrach CA, et al. The science of self-report: Implications for research and practice. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers; 2000. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.