Abstract
The response to the COVID-19 epidemic requires people to undertake actions such as mask-wearing or vaccination that also confer benefits to the whole community, and therefore, are akin to public good contributions. This is the case also for participation to the mass testing that took place between November 18th and 25th, 2020 in the South Tyrol region of Italy, where 361,781 out of 500,607 (72.3%) eligible residents volunteered to take a COVID-19 rapid antigen test. We examine the community characteristics that are associated with higher testing rates. Our findings point to a number of key community determinants of people’s willingness to volunteer. Convenience and social capital were important factors. Beyond that, socioeconomic status and religiosity were also both positively related to greater testing, while childhood vaccinations refusal rates show a negative relationship.
Keywords: COVID-19, Testing, Social capital, Religion, Vaccination, Public health
Introduction
During the COVID-19 pandemic, people are asked to take action to protect themselves and others from infection. Wearing masks, for instance, can provide protection to the wearers, as well as reduce outward transmission by infected individuals, therefore, providing protection for others [3, 34]. The same is true regarding vaccination, as the benefits to individuals are combined with benefits to others through community (herd) immunity. Despite the dramatic consequences of COVID-19, however, it cannot be taken for granted that people are keen to undertake these beneficial actions.1
In this paper, we examine the community characteristics that are associated with higher testing rates in a voluntary mass testing scheme implemented in the Italian region of South Tyrol between November 18th and 25th, 2020, where 361,781 out of 500,607 (72.3%) eligible residents were administered a COVID-19 rapid antigen test. 3615 tested positive. While there may be some individual benefits from testing (e.g., reduced anxiety), it is uncontroversial that testing delivers great benefits to others, in particular for the population of asymptomatic that we consider here.2 Therefore, we can consider participation to testing akin to voluntary contributions to a public good, and we examine the relationship between testing rates and characteristics that have been identified in the literature as relevant for contributions to public goods, such as gender and education, as well as a proxy for religiosity and other relevant variables such as age, household size, employment, and past prevalence of the infection.
The willingness to contribute to such public goods is also related to social factors [32, 37]. Hence, we also examine the relationship between testing rates and political participation, a measure of public good contribution that has been used as a proxy for social capital [20, 35]. We also look at vaccinations refusal rates, i.e., the share of children within a village that have not undertaken compulsory vaccinations. This captures the willingness to contribute to a health-related public good, as well as local distrust of medicine.3 Previous work has found that parochialism, i.e., a preference for favoring the members of one’s ethnic, racial or language group, is an important factor behind altruistic behavior [7]. From this point of view, an interesting feature of South Tyrol is the presence of different linguistic groups: German (around 69% of the population), Italian (around 26%), and Ladin (around 5%),4 with a conflictual relationship solved by granting special autonomy to the territory in the early 1970s [30]. For this reason, we explore the role of linguistic diversity, as well as the other factors mentioned above.5
To the best of our knowledge, our paper is the first examining the correlates of voluntary participation in a mass test program. We contribute to a growing literature that identifies community characteristics correlated with various aspects of COVID.6 Borjas [8] and Almagro and Orane-Hutchinson [2], for instance, use data from 177 ZIP codes in NYC to identify the demographic characteristics that correlate with COVID-19 testing and infections across neighborhoods, while Desmet and Wacziarg [14] analyze the correlates of variation in disease severity across US counties, Ginsburgh et al. [19] across French continental departments, and Verwimp [41] across Belgian municipalities.
More specifically, our paper relates to several investigations about the determinants of social distancing during the pandemic [5, 6, 9, 15, 16]. These papers examine US counties or European regions (the only exception is [16], which examines Italian provinces and German districts) and focus on the impact of social capital, measured through trust, electoral participation, or some other measures such as blood donations, newspaper readership, or participation in social activities. These papers find that mobility is reduced more during the COVID outbreak in areas with higher social capital. We also relate to a broader literature analyzing the link between social capital and health (see [27], for an overview). For instance, Hikichi et al. [23] examine the link between community-level social capital and cognitive decline after the 2011 tsunami in Japan.
Our paper also contributes to an emerging literature on vaccine hesitancy. For instance, in a representative survey of 17 countries, Dabla-Norris et al. [13] finds higher hesitancy for women and younger people. For France, Schwarzinger et al. [40] show an association of hesitancy with lower education and females, while Paul et al. [33] uses a large UK sample to show that females, as well as individuals with an ethnic minority background, lower education, and lower income are all more likely to have higher mistrust about vaccines.
The economics benefits of screening tests can be very large [4] and population-scale testing has been proposed as an effective measure to control the pandemic [26] and has already been implemented in several contexts, for instance in the Chinese regions of Wuhan and Qingdao and in Slovakia [24].7 Slovakia, in particular, tested over 3.6 million people—out of a population of almost 5.5 million—and, similarly to South Tyrol, found that around 1% of them were positive.8 Differently from the case studied here, however, non-participants were required to quarantine for ten days, thus providing a strong incentive to participate. While similar incentives could be used also for vaccination, they may prove controversial, and it is, therefore, of great interest to study a context where participation was fully voluntary.
The mass test in South Tyrol
The population of South Tyrol was invited to take part in a mass screening using antigen rapid tests, involving a nasal and throat swab. To enable this, authorities set up around 300 testing centers, with each municipality having at least one, where professional health care workers carried out the tests, with the support of volunteers from the civil protection agency, the voluntary fire services, and other organizations for handling the logistics and the administration. All residents were invited to participate, with the exception of children below the age of five, people with COVID-19 symptoms, those on sick leave, those who had tested positive and isolated in the last three months, and those who had recently tested positive or were in quarantine or self-isolating. People with a prior appointment for a PCR test, those regularly tested for work reasons, and individuals in social care were also not tested.
Testing centers generally operated from 8 am till 6 pm from Friday, 20 November to Sunday, 22 November. During this period, people could show up at any of the centers throughout South Tyrol. In some urban municipalities, it was possible to register online, and some published suggested centers and time slots based on the address of residence. This was done to reduce congestion and encourage participation. It was also possible to be tested in some pharmacies and at some GPs in the period 18–25 November. This was mainly done in urban areas to give presumably busier people easier access to testing. People only needed a valid ID, which is a basic requirement for anyone living in or visiting Italy, and a European Health Insurance card. They filled in a form with an email address, where they would receive, generally within a day, an encrypted file with the outcome, and a mobile number, where they would receive an SMS with the code to open the file. In case of a negative result, people were advised to continue following prevention measures such as social distancing and mask-wearing. In case of a positive result, people had to isolate for 10 days if asymptomatic and contact their doctor if they developed symptoms.
Participation in the mass testing was voluntary and encouraged by a massive communication campaign, providing information (with material available also in Albanian, Arabic, English, French and Urdu, as well as in simple language for kids), as well as endorsements by public figures. The headline of the campaign was “Together against coronavirus”, using appeals like “Let’s break the infection wave together and pave the way towards a gradual return to normality!”, thus underlining the importance of common action.
Data and methodology
Data about testing and child immunization rates come from the Health Authority,9 while data about municipality characteristics come from the Provincial Statistical Office, ASTAT,10 the National Statistical Office, ISTAT,11 or the Department of Internal Affairs.12 There are 116 municipalities in the South Tyrol.
Tested individuals are matched by the authorities to their municipality of residence based on their tax identification number and the total number of residents in each municipality is measured using official registration data.13 We define the population eligible for testing as all residents of a municipality age five or higher that are not currently in quarantine either because they have recently tested positive for COVID-19 or have been in close contact with someone that has. The testing rate is then measured as the number of residents of a municipality who volunteered to be tested between November 18th and 25th divided by the population eligible for testing in that municipality. The past COVID-positive rate is similarly calculated as the number of residents in a municipality who previously tested positive but are not currently positive divided by the total number of residents.
Age, gender, employment, immigration status and household size are measured in administrative data and made available at the municipality level. We can also calculate the standard deviation of age within a municipality using the available data. The proportion of individuals with secondary education and higher, and the proportion speaking the three official languages of the region are measured using the 2011 Census. We measure, as a proxy for religiosity, the proportion of religious weddings over total weddings celebrated in a given municipality between 1995 and 2019.14 Vaccination refusal rates refers to the vaccination status regarding the nine compulsory vaccines as of 2019 for the cohorts born 2013–2017. Following Putnam [35] and Guiso et al. [20], we use as a proxy for social capital the average turnout in the European parliament elections of 2019 and the constitutional referendum of 2020, two recent elections that are unrelated to local politics and government.15
In our analysis, we run an OLS regression model of the form:
where Yj is the testing rate in municipality j, Xj is a vector of municipality characteristics and εj is a mean zero error term. In all our models, we calculate robust standard errors that allow for heteroscedasticity. Since the outcome variable is a rate bounded between zero and one, our estimated β coefficients can be interpreted as the percentage point impact on the testing rate of a one-unit difference in the corresponding covariate.
We estimate two specifications. In the first, we include our standard control variables for the characteristics of individuals living in each municipality as well as some information about the municipalities and the availability of testing centers. In the second, we also control for two variables capturing contributions to public goods, namely the vaccination refusal rate and the average share of the eligible population who voted in the 2019 European election and the 2020 constitutional referendum on the number of members of parliament.16
We also estimate three versions of each specification. In the first one, each municipality is given equal weight and hence given an equal importance in estimating the relationship between X and Y. In the second one, the model is estimated using weighted-GLS and the importance of each municipality is determined by its registered population. Here, more populated municipalities are more important in determining the relationship between X and Y. The final specification is similar to the second one, but we drop the five municipalities with population above 15,000, thus focusing on a more homogeneous sample.
Results
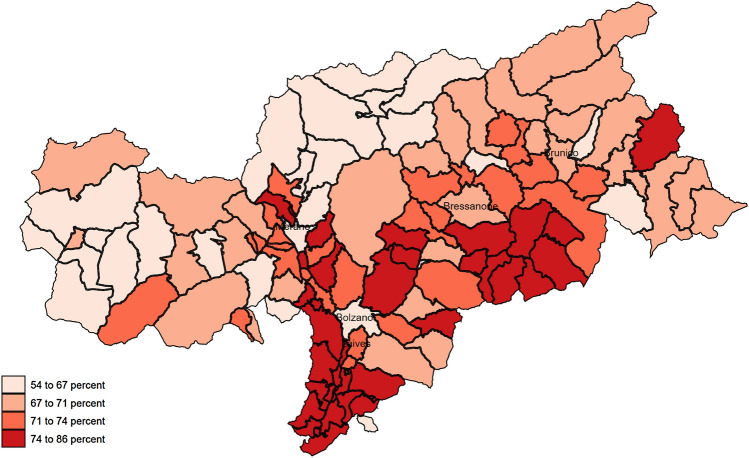
Figure 1 shows the variation in testing rates across the 116 municipalities of the South Tyrol, while Table 1 shows the distribution across the municipalities. Testing rates varied between 54.2 and 85.9% with the interquartile range 67.5–74.5%. Around 71% of eligible individuals volunteered to be tested in the median municipality.17 While we are interested in how community characteristics relate to testing rates and hence have the municipality as unit of observation, there is a large variation in the population of different municipalities (from 200 in the smallest to 108,606 in the largest), hence we also examine how testing rates vary when we weight municipalities by their population. While the most populated municipalities have relatively low testing rates, our weighted estimates look fairly similar with a median testing rate of 68.9% and an interquartile range of 67.0–72.2%. We also present weighted estimates where we drop five municipalities that have a population greater than 15,000.18 The weighted distribution of testing rates is nearly identical in this sample to the unweighted distribution across all municipalities.
Fig. 1.
COVID-19 testing rates across municipalities in the south Tyrol
Table 1.
Testing rates across municipalities
| Unweighted | Weighted by total population | Weighted by population—dropping municipalities > 15 K population | |
|---|---|---|---|
| Mean | 0.711 | 0.697 | 0.711 |
| Standard deviation | 0.059 | 0.045 | 0.051 |
| 1st percentile | 0.552 | 0.621 | 0.576 |
| 5th percentile | 0.621 | 0.637 | 0.633 |
| 10th percentile | 0.638 | 0.651 | 0.638 |
| 25th percentile | 0.675 | 0.670 | 0.677 |
| 50th percentile | 0.712 | 0.689 | 0.715 |
| 75th percentile | 0.745 | 0.722 | 0.745 |
| 90th percentile | 0.782 | 0.757 | 0.775 |
| 95th percentile | 0.816 | 0.781 | 0.793 |
| 99th percentile | 0.847 | 0.826 | 0.840 |
| Municipalities | 116 | 116 | 111 |
Testing rates are out of the share of the population excluding those currently positive or in quarantine
Table 2 presents the mean and standard deviation for all municipality characteristics that we consider in our analysis. On average, municipalities have 4,630 residents and the average population density is 125 inhabitants per KM^2. On average, there were 3 testing centers, 1.5 doctors and 0.3 pharmacies giving tests per municipality, and previously 1.2% of population had tested positive for COVID-19. On average, residents are aged 42, gender balanced, living in a household with 2.5 members. 53% of residents are employed, 41% have secondary education or higher, 6.8% are immigrants, and 83.7% speak German, 9.4% speak Italian and 6.9% speak Ladin as their principal language. On average, 48% of weddings performed recently in each municipality were religious ceremonies, 21% of children did not have the full set of mandatory vaccines and 69% of the eligible population voted, on average, in the European election in 2019 and the constitutional referendum in 2020. We also examine the importance of age heterogeneity; the standard deviation of age within communities is 23.5 on average.
Table 2.
Summary of municipality characteristics
| Unweighted | Weighted by population | Weighted by population—dropping municipalities > 15 K | |
|---|---|---|---|
| Population/1000 | 4.63 (10.9) | 30.23 (41.1) | 4.72 (3.4) |
| Population density (1000 per KM2) | 0.125 (0.254) | 0.657 (0.825) | 0.106 (0.097) |
| Number of testing centers | 2.96 (5.33) | 15.07 (21.47) | 2.74 (1.04) |
| Number of testing doctors | 1.48 (3.11) | 8.26 (10.80) | 1.78 (1.85) |
| Number of testing pharms | 0.29 (1.23) | 3.04 (4.35) | 0.25 (0.60) |
| Past COVID-positive rate | 0.012 (0.009) | 0.013 (0.006) | 0.011 (0.007) |
| Mean age | 41.6 (1.3) | 42.5 (1.6) | 41.5 (1.1) |
| Standard deviation age | 23.5 (0.4) | 23.7 (0.4) | 23.5 (0.4) |
| Share female | 0.495 (0.015) | 0.505 (0.012) | 0.498 (0.010) |
| Mean household size | 2.46 (0.16) | 2.34 (0.18) | 2.44 (0.14) |
| Employment rate | 0.533 (0.055) | 0.536 (0.040) | 0.539 (0.049) |
| Share higher education | 0.407 (0.058) | 0.440 (0.054) | 0.412 (0.051) |
| Share immigrant | 0.068 (0.041) | 0.097 (0.045) | 0.071 (0.033) |
| Share religious weddings | 0.480 (0.135) | 0.404 (0.128) | 0.474 (0.112) |
| Share speaking German | 0.837 (0.265) | 0.680 (0.315) | 0.854 (0.239) |
| Share speaking Italian | 0.094 (0.149) | 0.277 (0.292) | 0.082 (0.113) |
| Share speaking Ladin | 0.069 (0.233) | 0.042 (0.175) | 0.064 (0.221) |
| Vaccination refusal rate | 0.209 (0.075) | 0.189 (0.062) | 0.214 (0.066) |
| Share voting 2019/2020 non-local elections | 0.692 (0.047) | 0.663 (0.045) | 0.683 (0.045) |
| Municipalities | 116 | 116 | 111 |
Standard deviations in parentheses. Share variables are as a proportion of the total or adult population in a municipality
Weighting for population size, the average municipality is much larger with 30,230 residents, a density of 657 inhabitants per KM^2, with 15 testing centers, 8 doctors and 3 pharmacies giving tests. Perhaps surprisingly, most other characteristics of the residents are fairly similar. The main exceptions are that residents of larger areas are more educated, more likely to be immigrants, and more likely to be Italian speakers. In addition, weddings are less likely to be religious. When the larger municipalities are dropped, the characteristics of the weighted sample are nearly identical to those of the unweighted sample in all dimensions.
Table 3 presents our main results. We will focus our discussion on the characteristics of municipalities that are associated with the community testing rate at a minimum 10% significance threshold, but also mention some other interesting relationships. We first discuss the results treating all municipalities with equal weighting. Controlling for population density and the number of testing centers, testing rates are lower in more populated municipalities, but the effect size is fairly small with an additional 1000 people associated with 0.5–0.8 percentage point (pp) lower testing rates. On the other hand, having more testing centers is correlated with higher testing rates, with each additional center associated with 0.6–0.8 pp higher testing rates.
Table 3.
Community characteristics and COVID-19 testing rates
| Unweighted | Weighted by population | Weighted by population—dropping municipalities > 15 K population | ||||
|---|---|---|---|---|---|---|
| Population/1000 | − 0.00802*** (0.00292) | − 0.00519** (0.00257) | − 0.00571*** (0.00171) | − 0.00393** (0.00157) | − 0.00227 (0.00269) | − 0.00183 (0.00198) |
| Population density (1000 per KM2) | 0.0680 (0.0564) | 0.0569 (0.0505) | − 0.0351 (0.0228) | − 0.0101 (0.0194) | 0.172** (0.0820) | 0.139* (0.0741) |
| Number of testing centers | 0.00805** (0.00346) | 0.00580** (0.00288) | 0.00582*** (0.00168) | 0.00349** (0.00152) | 0.00495 (0.00599) | 0.00909* (0.00510) |
| Number of testing doctors | 0.00321 (0.00367) | 0.00204 (0.00371) | 0.00242 (0.00199) | 0.00278 (0.00216) | − 0.000846 (0.00385) | 0.00124 (0.00294) |
| Number of testing pharm | 0.00470 (0.0114) | − 0.00314 (0.0105) | 0.0129 (0.00884) | 0.00583 (0.00741) | 0.00309 (0.0109) | − 0.00324 (0.00916) |
| Past COVID-positive rate | − 0.992 (0.721) | − 0.900 (0.670) | − 0.673 (0.613) | − 0.816 (0.590) | − 0.559 (0.567) | − 0.694 (0.581) |
| Mean age | 0.0168** (0.00651) | 0.0145** (0.00686) | 0.0164** (0.00693) | 0.0102 (0.00669) | 0.0213*** (0.00682) | 0.0158** (0.00647) |
| Standard deviation age | − 0.0315** (0.0147) | − 0.0343** (0.0154) | − 0.0137 (0.0142) | − 0.00972 (0.0130) | − 0.0219 (0.0134) | − 0.0187 (0.0121) |
| Share female | 1.232*** (0.402) | 1.194*** (0.436) | 1.215** (0.523) | 0.850* (0.497) | 1.007* (0.522) | 0.613 (0.499) |
| Mean household size | 0.184*** (0.0639) | 0.148** (0.0741) | 0.123* (0.0666) | 0.0247 (0.0697) | 0.213*** (0.0685) | 0.122* (0.0704) |
| Employment rate | 0.133 (0.0989) | 0.0652 (0.0981) | 0.163* (0.0919) | 0.0522 (0.0941) | 0.175* (0.0926) | 0.0654 (0.0960) |
| Share higher education | 0.387*** (0.105) | 0.354*** (0.0921) | 0.403*** (0.0960) | 0.337*** (0.0805) | 0.268** (0.111) | 0.270*** (0.0894) |
| Share immigrant | 0.138 (0.196) | 0.0539 (0.211) | 0.0520 (0.182) | − 0.0495 (0.195) | 0.206 (0.180) | 0.0308 (0.190) |
| Share religious weddings | 0.108*** (0.0356) | 0.0672** (0.0334) | 0.118*** (0.0365) | 0.0860*** (0.0310) | 0.113*** (0.0382) | 0.0826** (0.0323) |
| Share speaking Italian | 0.100** (0.0503) | 0.0798 (0.0492) | 0.0960*** (0.0342) | 0.0575 (0.0347) | 0.0648 (0.0592) | 0.0490 (0.0581) |
| Share speaking Ladin | 0.0650*** (0.0189) | 0.0723*** (0.0188) | 0.0650*** (0.0202) | 0.0697*** (0.0182) | 0.0628*** (0.0215) | 0.0674*** (0.0195) |
| Vaccination refusal rate | − 0.104* (0.0585) | − 0.0913* (0.0509) | − 0.119** (0.0510) | |||
| Share voting 2019/2020 non-local elections | 0.310*** (0.0892) | 0.431*** (0.0871) | 0.394*** (0.0817) | |||
| R-squared | 0.507 | 0.572 | 0.558 | 0.662 | 0.506 | 0.619 |
| Municipalities | 116 | 116 | 116 | 116 | 111 | 111 |
Robust standard errors in parentheses. Share variables are as a proportion of the total or adult population in a municipality
***p < 0.01, **p < 0.05, *p < 0.1
Testing rates are higher in municipalities with an older population, less age variation, more women, larger households, and a more educated population. Testing rates are also higher in municipalities with a higher proportion of religious weddings, with communities with a 10 pp higher proportion of religious weddings having 0.7–1.1 pp higher testing rate. Finally, in this specification, municipalities with a larger share of individuals speaking the two minority languages in the region (Italian and Ladin) have higher testing rates.
Turning to our second specification, we see that social capital measured as the vaccination refusal rate (which also is related to skepticism about medicine) and the share voting in non-local elections in 2019/2020 are both strongly predictive of testing rates in a municipality, with the R-squared of our model increasing by 11%, from 0.51 to 0.57. Political participation has a particularly strong relationship, with communities with a 10 pp higher vote share having a 3.1 pp higher testing rate. Interestingly, adding these control variables does not substantively change the estimated relationship between other community characteristics and testing rates indicating that they are capturing something that is unrelated to the sociodemographics of a particular community. The only exception is the effect of the share of Italian speakers, where the coefficient becomes smaller and statistically insignificant.
Our main results are similar if we weight each municipality by its population. In the first specification, the only substantive differences we find are for the population variables. Now, both the negative relationship between population and testing rates and the positive relationship between number of testing centers and testing rates are both about two-thirds their size as in the unweighted estimates. Our additional controls for social capital have an even stronger explanatory power when larger municipalities are given more weight, especially political participation with communities with a 10 pp higher vote share having a 4.3 pp higher testing rate. On the other hand, now some demographic characteristics, e.g., age and household size, are no longer significantly related to testing rates, while others, e.g., share female, have a weaker relationship.
Our main results are qualitatively unaffected if we exclude the larger municipalities. However, population is no longer statistically significantly associated with testing rates, the same is true for the number of testing centers in our first specification, while population density has a positive association with municipalities with an additional 100 people per KM^2 having 1.4–1.7 pp higher testing rates. In addition, the share of Italian speakers is insignificant in both specifications, while the vaccination refusal rate has a stronger negative relationship with test rates once the largest municipalities are dropped from our analysis.
Discussion
Our findings point to a number of key community determinants of people’s willingness to volunteer for the COVID mass testing program in the South Tyrol.
First, it is clear that convenience was an important factor; after controlling for population and population density, individuals were more likely to get tested in communities where there were more centers. We also generally find a positive correlation with the number of doctors and pharmacies doing tests in the community although these relationships are not statistically significant.
Second, communities where the population is older, more educated and living in larger households had higher testing rates, consistent with a positive relationship between socioeconomic status and willingness to contribute to public goods and with the emerging literature on vaccine hesitancy surveyed in the introduction. The finding on age could also be related to the increased risk of hospitalization or deaths associated with age.19 Similarly, the finding for household size could occur because large households have increased social contacts and hence are at higher risk.20
Third, we find higher testing rates in communities with a higher female share, consistent with a vast literature showing gender differences in preferences, including altruism [12, 17]. The greater vaccine hesitancy for female suggested instead by the literature so far could be because concerns about safety and, possibly gender-specific, side effects play a big role for COVID-19 vaccination, while being virtually absent for testing [28].
Fourth, we find that more religious communities—proxied by share of religious weddings—have higher testing rates consistent with the literature showing religious rituals being associated with higher degrees of cooperation [39] and, more generally, showing the link between religiosity and civic responsibility [29]. South Tyrol is predominantly catholic. It is important to underline that the impact of religiosity on responses to COVID-19 is likely to vary across denominations and depending on how religion is practiced within communities, something that emerges in the review of early evidence on the nexus between religion and the pandemic by Oman [31].
Fifth, we find higher testing rates in municipalities with a higher share of Ladin speakers, while the positive association with Italian speakers is not significant when controlling for social capital. This occurs because both voting rates and vaccine acceptance are higher in communities with more Italian speakers. One hypothesis for why testing rates were higher in municipalities with a higher share of Ladin speakers is that these individuals are a “minority within a minority”, as they live in a German-majority province within an Italian-majority state. This could create a particularly strong identity at the municipal level.
Finally, we find a strong relationship between social capital, proxied by political participation, and testing. As participation to testing is akin to a contribution to a public good, this is in line with what emerges from a large literature [21, 36]. More specifically, it is also in line with the recent literature on COVID-19 reviewed in the introduction, showing that higher social capital in US counties and European regions is associated with more social distancing. The negative relationship between vaccination refusal rates and testing could also reflect negative attitudes about medicine, possibly fueled by misinformation [10].
Interestingly, we found an insignificant relationship between the past COVID-positive rate in a community and the current testing rate. One could have expected a positive effect of higher previous contagion, as an increased likelihood of knowing people who have had Covid could make the risks loom larger in people’s minds. On the contrary, the insignificant coefficient is consistently negative.
While we focus on a mass testing campaign, we suspect that similar patterns would reveal themselves for vaccination uptake. Hence, these results can be useful for helping guide policies designed to increase vaccine uptake, for example, by making it more convenient, encouraging people to think about the importance of protecting other people and focusing extra resources on lower socioeconomic status communities.
However, an important limitation of our study is that we can only measure the role of community characteristics and it is possible that this hides important heterogeneity across individuals. Individual level data are unfortunately not available, but, even if they were, it would be practically impossible to match them with some of our key variables, e.g., with participation in elections. Beyond this, because individuals typically sort into communities with people with similar characteristics, the correlation between community characteristics and the measured outcome might be stronger at the community than individual level. Furthermore, we can only measure a subset of community characteristics that are related to testing rates and hence we might have not accounted for important unobservable characteristics that could bias the relationships that we currently estimate.
This notwithstanding, our results can be helpful in identifying communities particularly at risk of not adhering to voluntary programs to fight the pandemic, in our case mass tests, but in prospect also vaccination campaigns.
Acknowledgements
We would like to thank Alexia Lochmann for helpful research assistantship.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
See on mask-wearing: https://news.gallup.com/poll/315590/americans-face-mask-usage-varies-greatly-demographics.aspx and on vaccination: https://news.gallup.com/poll/325208/americans-willing-Covid-vaccine.aspx.
The communication campaign related to the mass test made it clear that people with COVID-19 symptoms were not supposed to take part. Moreover, people with symptoms had on-going access to free testing through regular channels (e.g., their GP).
See Kreidl and Morosetti [25] for the importance of the issue of non-vaccination in South Tyrol. See Reich [38] for the relationship between social capital, stigma, and vaccination refusal. In addition, childhood vaccination confers individual benefits, while at the same time greatly contributing to a public good through herd immunity.
Notice that everyone is classified within these three linguistic groups, despite the growing presence of migrants who do not necessarily belong to neither and of bilingual people.
Linguistic fractionalization is common in many countries. In Alesina et al. [1], the sample mean of 185 countries of a fractionalization index going from 0 (for complete homogeneity) to 1 is 0.385.
This relates to the broader economics literature that examines the correlation between community characteristics and important economic and social outcomes. A prominent example is Chetty et al. [11].
Ferrari et al. [18] estimate that the mass test campaign in South Tyrol decreased the growth rate of COVID-19 by 39% which corresponds to a reduction in the total additional cases of 14%, 36% and 66% within 10, 20 and 40 days from the intervention.
https://coronatest.asdaa.it/it/muni (Italian) or https://coronatest.asdaa.it/de/muni (German).
In Italy, all individuals are legally required to register in their municipality of residency and local services, such as education and health care, are only available to those that are registered. 12,971 tested individuals could not be matched to their municipality and are excluded from our analysis (the forms used to indicate personal information could be filled out by hand likely leading to some matching errors). For example, one of the authors of this paper did not receive the code to open his file because his telephone number was illegible. We have no reason to suspect that poor handwriting is correlated with municipality characteristics.
The vast majority of religious weddings in the South Tyrol are catholic.
Unfortunately, other commonly used measures of social capital in Italy (see [16, 22] are either unavailable at the municipality level (blood donations, newspaper readership) or problematic for South Tyrol due to its multilingual environment (cheating on exams is not available for German and Ladin schools). The two measures that we rely on, political participation and vaccination refusals are both highly correlated with blood donations and newspaper readership at the provincial level (political participation has a correlation coefficient of 0.42 with blood donations and 0.30 with newspaper readership, the same numbers for vaccination refusal are − 0.33 and − 0.22, respectively.).
These figures are all lower bounds of the true rate because of the small number of people who were tested and could not be matched to their municipality of residence.
This drops the four ‘cities’ of the South Tyrol, Bolzano-Bozen, Merano-Meran, Brixen-Bressanone and Bruneck-Brunico, and what can be considered the largest suburb of Bolzano, Laives-Leifers.
Supporting this, we also find higher testing rates in communities with more employed people, but this is not usually statistically significant.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Steven Stillman, Email: steven.stillman@unibz.it.
Mirco Tonin, Email: mirco.tonin@unibz.it.
References
- 1.Alesina A, Devleeschauwer A, Easterly W, Kurlat S, Wacziarg R. Fractionalization. J. Econ. Growth. 2003;8(2):155–194. doi: 10.1023/A:1024471506938. [DOI] [Google Scholar]
- 2.Almagro M, Orane-Hutchinson A. JUE Insight: the determinants of the differential exposure to COVID-19 in New York city and their evolution over time. J. Urban Econ. 2021 doi: 10.1016/j.jue.2020.103293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Asadi S, Cappa CD, Barreda S, et al. Efficacy of masks and face coverings in controlling outward aerosol particle emission from expiratory activities. Sci Rep. 2020;10:15665. doi: 10.1038/s41598-020-72798-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Atkeson, A., Droste, M.C., Mina, M. and Stock, J.H.: Economic benefits of COVID-19 screening tests (No. w28031). National Bureau of Economic Research (2020)
- 5.Bargain O, Aminjonov U. Trust and compliance to public health policies in times of COVID-19. J. Public Econ. 2020 doi: 10.1016/j.jpubeco.2020.104316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barrios JM, Benmelech E, Hochberg YV, Sapienza P, Zingales L. Civic capital and social distancing during the COVID-19 pandemic. J. Public Econ. 2021 doi: 10.1016/j.jpubeco.2020.104310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernhard H, Fischbacher U, Fehr E. Parochial altruism in humans. Nature. 2006;442:912–915. doi: 10.1038/nature04981. [DOI] [PubMed] [Google Scholar]
- 8.Borjas, G.J.: Demographic determinants of testing incidence and COVID-19 infections in New York City neighborhoods. National Bureau of Economic Research WP 26952 (2020)
- 9.Brodeur A, Grigoryeva I, Kattan L. Stay-at-home orders, social distancing and trust. J. Popul. Econ. 2021 doi: 10.1007/s00148-021-00848-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carrieri V, Madio L, Principe F. Vaccine hesitancy and (fake) news: quasi-experimental evidence from Italy. Health Econ. 2019;28(11):1377–1382. doi: 10.1002/hec.3937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chetty, R., Friedman, J.N., Hendren, N., Jones, M.R., Porter, S.R.: The opportunity atlas: mapping the childhood roots of social mobility. National Bureau of Economic Research WP 25147 (2018)
- 12.Croson R, Gneezy U. Gender differences in preferences. J. Econ. Lit. 2009;47(2):448–474. doi: 10.1257/jel.47.2.448. [DOI] [Google Scholar]
- 13.Dabla-Norris, E., Khan, H., Lima, F., Sollaci, A.: Who doesn’t want to be vaccinated? Determinants of vaccine hesitancy during COVID-19. International Monetary Fund WP 21/130 (2021)
- 14.Desmet K, Wacziarg RT. Understanding spatial variation in COVID-19 across the United States. J. Urban Econ. 2021 doi: 10.1016/j.jue.2021.103332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ding, W., Levine, R., Lin, C., Xie, W.: Social distancing and social capital: why US counties respond differently to COVID-19. National Bureau of Economic Research WP 27393 (2020)
- 16.Durante R, Guiso L, Gulino G. Asocial capital: civic culture and social distancing during COVID-19. J. Public Econ. 2021 doi: 10.1016/j.jpubeco.2020.104342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Falk A, Hermle J. Relationship of gender differences in preferences to economic development and gender equality. Science. 2018;362(6412):eaas9899. doi: 10.1126/science.aas9899. [DOI] [PubMed] [Google Scholar]
- 18.Ferrari, D., Stillman, S., Tonin, M.: Does COVID-19 mass testing work? The importance of accounting for the epidemic dynamics. Mimeo (2021)
- 19.Ginsburgh V, Magerman G, Natali I. COVID-19 and the role of inequality in French regional departments. Eur. J. Health Econ. 2021 doi: 10.1007/s10198-020-01254-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guiso L, Sapienza P, Zingales L. The role of social capital in financial development. Am. Econ. Rev. 2004;94:526–556. doi: 10.1257/0002828041464498. [DOI] [Google Scholar]
- 21.Guiso L, Sapienza P, Zingales L. Civic capital as the missing link. Handb. Soc. Econ. 2011;1:417–480. doi: 10.1016/B978-0-444-53187-2.00010-3. [DOI] [Google Scholar]
- 22.Guiso L, Sapienza P, Zingales L. Long-term persistence. J. Eur. Econ. Assoc. 2016;14(6):1401–1436. doi: 10.1111/jeea.12177. [DOI] [Google Scholar]
- 23.Hikichi H, Aida J, Matsuyama Y, Tsuboya T, Kondo K, Kawachi I. Community-level social capital and cognitive decline after a natural disaster: a natural experiment from the 2011 Great East Japan Earthquake and Tsunami. Soc. Sci. Med. 2020;257:111981. doi: 10.1016/j.socscimed.2018.09.057. [DOI] [PubMed] [Google Scholar]
- 24.Holt E. Slovakia to test all adults for SARS-CoV-2. The Lancet. 2020;396(10260):1386–1387. doi: 10.1016/S0140-6736(20)32261-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kreidl P, Morosetti G. Müssen wir in naher Zukunft mit einer Masernepidemie in Südtirol rechnen? Wien. Klin. Wochenschr. 2003;115:55–60. [PubMed] [Google Scholar]
- 26.Jussi,T., Romer, P., Linnarsson, S.: Population-scale testing can suppress the spread of COVID-19. medRxiv 2020.04.27.20078329. 10.1101/2020.04.27.20078329
- 27.Moore S, Carpiano RM. Introduction to the special issue on "social capital and health: what have we learned in the last 20 Years and where do we go from here?". Soc. Sci. Med. 2020;257:113014. doi: 10.1016/j.socscimed.2020.113014. [DOI] [PubMed] [Google Scholar]
- 28.Moran KR, Del Valle SY. A meta-analysis of the association between gender and protective behaviors in response to respiratory epidemics and pandemics. PLoS ONE. 2016;11(10):e0164541. doi: 10.1371/journal.pone.0164541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Monsma, S.V.: Religion and philanthropic giving and volunteering: Building blocks for civic responsibility. Interdiscip. J. Res. Relig. 3 (2007)
- 30.Niezing J. South Tyrol: A minority conflict of the twentieth century. Routledge; 2017. [Google Scholar]
- 31.Oman D. COVID-19 and religion/spirituality: a global review from a public health perspective. Public Health Rel Spiritual Bull. 2020;3:10–17. [Google Scholar]
- 32.Ostrom E. What is social capital. In: Bartkus VO, Davis JH, editors. Social capital: reaching out, reaching in. Edward Elgar Publishing; 2009. [Google Scholar]
- 33.Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. Lancet Reg Health-Eur. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Prather KA, Wang CC, Schooley RT. Reducing transmission of SARS-CoV-2. Science. 2020 doi: 10.1126/science.abc6197. [DOI] [PubMed] [Google Scholar]
- 35.Putnam R. Making democracy work: civic traditions in modern Italy. Princeton: Princeton University Press; 1993. [Google Scholar]
- 36.Putnam R. Bowling alone. New York: Simon and Schuster; 2000. [Google Scholar]
- 37.Putnam R. Social capital: measurement and consequences. Can. J. Policy Res. 2001;2(1):41–51. [Google Scholar]
- 38.Reich JA. “We are fierce, independent thinkers and intelligent”: social capital and stigma management among mothers who refuse vaccines. Soc. Sci. Med. 2020;257:112015. doi: 10.1016/j.socscimed.2018.10.027. [DOI] [PubMed] [Google Scholar]
- 39.Ruffle, B.J., Sosis, R.: Does it pay to pray? Costly ritual and cooperation. BE J. Econ. Anal. Pol. 7(1) (2007)
- 40.Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6(4):e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Verwimp P. The spread of COVID-19 in Belgium: a municipality-level analysis. ECARES; 2020. [Google Scholar]