Abstract
Background
Severe stress is one of the most common causes of sick leave in Sweden. Previous research has shown that compassion interventions for healthcare professionals can decrease work-related stress through the introduction of self-care, self-awareness, and emotion regulation abilities when experiencing difficult situations. Internet-based stress management interventions have hitherto shown promising results in reducing stress. However, further research is needed to examine the effectiveness of internet-based compassion interventions for healthcare professionals.
Objective
In the present study protocol, a randomised controlled trial is described, aiming to examine the effects of an internet-based compassion course for healthcare professionals on work-related stress and stress of conscience.
Method
Healthcare professionals will be offered an internet-based stress management course of five modules across a period of five weeks. The design is a randomised controlled study consisting of three groups enrolled in one of the following: a compassion course (n = 120), a cognitive behavioural stress management course (n = 120), or placed on a waitlist followed by either the compassion course or the cognitive behavioural stress management course (n = 36). We hypothesise that the internet-based compassion course would reduce the participants’ stress of conscience to a greater degree compared to the other two groups. The secondary hypothesis is that the compassion course would increase the participants’ professional quality of life (i.e., higher job satisfaction and lower empathy fatigue) and self-compassion. In addition, the internet-based compassion course is expected to reduce the participants’ work-related stress and sick leave rates to the same degree (non-inferiority) as the cognitive behavioural stress management course and to a higher degree when compared to the waitlist condition. The primary outcome measure is the Stress of Conscience Questionnaire (SCQ) and the secondary outcome measures are the Professional Quality of Life Scale (PROQOL), the Work-related Stress Copenhagen Psychosocial Questionnaire (COPSOQ), and the Self-compassion Scale (SCS). Assessments will be performed at baseline, four weekly assessments during treatment, post-treatment (5 weeks), and follow-ups at 10 weeks, 15 weeks, and 6 months. The repeated measures data will be analysed using a generalised estimating equation for repeated measurements to examine whether changes over time differ between the groups and whether the improvements persist over time.
Discussion
The clinical trial is expected to provide novel data on the effects of compassion interventions and add to the existing knowledge of internet-based interventions for stress management in healthcare professionals.
Keywords: Compassionate mind training course, Cognitive behavioural therapy, Healthcare professionals, Stress management course, Internet-based intervention, Stress of conscience
Trial registration
ClinicalTrials.gov ID NCT04700878
1. Introduction
In Sweden, sick leave due to work-related stress is higher in the healthcare sector than in any other. More efforts are thus required to prevent mental health problems in this group (Försäkringskassan, 2020a). In the long run, increased stress may lead to fatigue and an increased number of healthcare professionals (HCPs) requesting sick leave, thereby exacerbating the stress levels of those who remain working. The so-called ‘stress of conscience’ phenomenon is common in HCPs. It may occur when they cannot practice their profession according to their values or meet their patients’ physical and psychological needs (Glasberg et al., 2006 Nov 1). Stress of conscience is associated with higher levels of burnout and stress-related issues (Åhlin et al., 2015) and can negatively affect recovery, in turn increasing the risk of burnout and sick leave. In recent years, web and computer-based stress-management interventions have shown promising results in reducing work-related stress (Heber et al., 2017 Feb 17); however, further research is needed to explore whether interventions for HCPs are effective in preventing stress-related health issues, enabling recovery, and reducing mental suffering linked to stressful work situations (Sinclair et al., 2017b).
Compassion is the motivation to reduce suffering in oneself and others—based on wisdom and courage—and is characterised by a warm, understanding, and respectful attitude (Gilbert, 2020). Compassion for oneself (or self-compassion) seems to be associated with lower levels of work-related stress and burnout symptoms in HCPs (Dev et al., 2020 May 1); several interventions with the aim of cultivating compassion have been developed (Kirby et al., 2017). In a meta-analysis of compassion interventions by Kirby et al. (2017), the results showed that compassion interventions seemed to lower levels of depression, anxiety, and perceived stress, as well as increasing levels of well-being compared to waitlist controls. However, the majority of the included randomised controlled trial (RCT) studies involved non-clinical samples with small sample sizes. In addition, the included interventions differed in content and extent and were based on different traditions such as mindfulness interventions, a mix between mindfulness and self-compassion practices, and compassion-based interventions. Overall, compassion interventions for HCPs have shown promising results in lowering the levels of burnout symptoms and work-related stress (Dev et al., 2020 May 1; McVicar et al., 2021 Jan; C Irons C. Heriot-Maitland Compassionate mind training: an 8-week group for the general public. Psychol. Psychother. Theory Res. Pract. [Internet]. [cited, 2020); however, more randomised controlled trials are needed in this area (McVicar et al., 2021 Jan).
One of the most commonly used compassion interventions, Compassionate Mind Training (CMT), a term used in non-clinical populations—or compassion-focused therapy (CFT) in clinical populations (Gilbert, 2005)—was originally developed to reduce levels of self-criticism (Gilbert, 2009). CMT is an emotion-regulation intervention that places particular emphasis on shame and self-criticism; participants learn to increase their self-care abilities instead of resorting to self-criticism during stressful situations (McVicar et al., 2021 Jan; C Irons C. Heriot-Maitland Compassionate mind training: an 8-week group for the general public. Psychol. Psychother. Theory Res. Pract. [Internet]. [cited, 2020; McEwan et al., 2020). People who have greater levels of self-compassion generally seem more supportive of themselves, which has positive effects on their well-being and quality of life (Craig et al., 2020). In contrast, those with high levels of self-criticism tend to judge themselves harshly in stressful situations, thereby increasing their levels of stress and negative emotions. In a systematic review of CFT interventions for clinical populations, 29 studies were included, of which there were nine RCTs, three controlled trials, and 17 observational studies (Craig et al., 2020). Twenty-four of the studies did not make comparisons to an active control group; hence, the evidence base for CMT/CFT interventions remains relatively small. More RCTs with powered sample sizes and active control groups are thus needed.
To date, research has been conducted on the effects of CMT on HCP; however, these studies have been conducted on small non-randomised samples (McVicar et al., 2021 Jan; McEwan et al., 2020; Beaumont et al., 2016). In the study by Beaumont et al. (2016), 15 HCPs participated in a 12-week CMT intervention. The quantitative data showed an increase in self-compassion and a decrease in self-criticism and the qualitative interview data revealed that the CMT intervention helped participants calm down, tolerate distressing emotions rather than acting on them, and shift their thinking in difficult situations from a self-critical stance to a more compassionate and helpful one. The pre-post intervention study by McVicar et al. (2021 Jan) included 26 nursing students who participated in a 12-month training CMT course as part of their specialist community public health nurse training. The study revealed that, following the completion of the course, burnout scores decreased and compassion satisfaction related to work as well as participants’ levels of well-being increased. In another study by McEwan et al. (2020), mental health nurses (n = 17) were interviewed in focus groups one year after they completed a two-day CMT workshop. The participants found CMT helpful and an increase in self-compassion as well as a decrease in self-criticism were noted; however, they also stated that more training would be needed in order to use these skills in relation to their work environments.
Internet-based stress-management interventions have been found to be effective in reducing stress in non-clinical adult samples (Heber et al., 2017 Feb 17). In a systematic review and meta-analysis by Heber et al. (2017 Feb 17), cognitive behavioural therapy (CBT) and the so-called third-wave CBT (which is mindfulness-based CBT and acceptance and commitment therapy, both in many ways similar to CMT) showed small-to-moderate effect sizes. Some internet-based RCTs have focused on compassion, for example, a four-week online loving-kindness meditation intervention for the general population (Galante et al., 2016), an internet-based compassion-focused intervention for high self-criticism (Krieger et al., 2019 Mar 1), and a six-week online self-compassion programme for Australian psychology trainees (Finlay-Jones et al., 2015). However, internet-based CMT interventions are rarely performed (Dhokia et al., 2020 Nov; Halamová et al., 2020 May 29; Lennard et al., 2021). Dhokia et al. (2020 Nov) conducted a pilot RCT on online CMT interventions for people with chronic pain with the aim of helping them avoid analgesic misuse. The participants were randomised to either 20 days CMT or relaxation music, both delivered via the internet. The results indicated that CMT can reduce analgesic use and dependency as well as lower levels of self-criticism. These improvements were maintained at the one-week post-intervention follow-up. In another pilot RCT, perinatal and intending-to-become pregnant women (n = 123) were allocated to either internet-based CMT (n = 61) or internet-based CBT (n = 62) interventions (Kelman et al., 2018). After the two-week course, both CMT and CBT participants showed decreases in self-criticism accompanied by increases in self-compassion and reductions in depression and anxiety. CMT was found to be superior in reducing both depression and anxiety. However, this study did not explore the long-term effects of the course.
Therefore, it appears that CMT seems to increase self-compassion and professional quality of life and decrease work-related stress and burnout symptoms. However, the effects of CMT on stress of conscience have not yet been investigated. Although internet-based stress-management interventions have shown promising results in non-clinical groups of adults, no RCTs have hitherto investigated internet-based CMT interventions in HCPs with active control. In addition, further studies are needed to investigate the link between stress of conscience and sick leave due to stress, as well as what factors may be protective, that is, lowering the risk of burnout and stress-related health issues (Åhlin et al., 2021).
This is a study protocol of an RCT aimed at testing two internet-based stress management courses for HCPs who are recruited on the basis of experiencing work-related stress. The internet-based compassion course (ICOP) is based on CMT and will be compared to an internet-based cognitive behavioural course (ICB), based on cognitive behavioural therapy, for stress-related mental health problems.
1.1. Aims and hypotheses
The aim of this study is to examine whether an internet-based compassion course may be effective in reducing stress of conscience and work-related stress in HCPs. We explore the following hypotheses:
-
1)
The primary hypothesis is that the ICOP course will decrease stress of conscience in HCPs to a greater extent than the ICB course and the waitlist group (superiority) at post-treatment.
-
2)The secondary hypotheses are that the ICOP course will have the following effects:
-
a.increase professional quality of life (higher job satisfaction and lower empathy fatigue) to a greater extent than the other two groups (superiority) at post-treatment;
-
b.increase self-compassion to a greater extent than the other two groups (superiority) at post-treatment;
-
c.decrease work-related stress to the same degree as the ICB course (non-inferiority) but better compared to the waitlist condition (superiority) at post-treatment;
-
d.affect sick leave to the same degree as the ICB course (non-inferiority) but better than the waitlist condition (superiority) at the 6-month follow-up.
-
a.
-
3)
As an active intervention, we hypothesise that, compared to the waitlist condition (superiority), ICB increases professional quality of life (higher job satisfaction and lower empathy fatigue) and self-compassion to a greater extent as well as decreasing work-related stress.
-
4)Further objectives to study are to explore the following:
-
a.the protective factors of burnout and sick leave—for example, what content in the ICOP and ICB courses the participants experience help them reduce work-related stress;
-
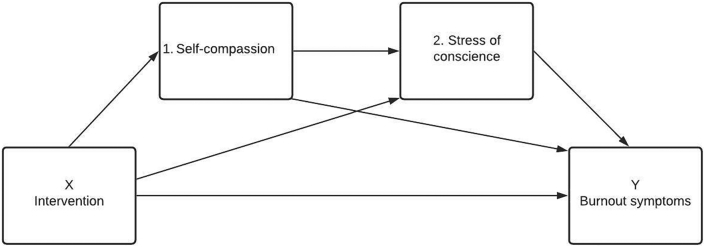
b.whether self-compassion mediates change in stress of conscience; and whether intervention X (ICOP/ICB) affects burnout symptoms (COPSOQ) through four pathways—(1) self-compassion (SCS); (2) stress of conscience (SCQ) (3) through both (1) and (2); or (4) direct from X to Y.
-
c.processes of change and common factors in the two stress-management courses;
-
d.relationships between the participants’ activities on each course module, their experiences of how helpful the modules are regarding stress management, and changes in their perceived stress of conscience and work-related stress.
-
a.
2. Method
2.1. Study design
This study will comprise a single-blind randomised trial comparing a five-module internet-based compassion stress management course (ICOP; n = 120) against an internet-based cognitive behavioural stress management course (ICB; n = 120) and a waitlist group (n = 36). For the primary analysis, only participants with SCQ scores of 45 or higher will be included, and according to the power analysis (see Section 2.10), 100 participants are needed for each active arm (ICOP and ICB). Expecting 20% attrition, we plan to include 240 participants for the primary analysis. Thirty-six participants, including the expected attrition, will be required in the waitlist group. However, as detailed in Section 2.2, we will also include participants with SCQ scores below 45 for secondary analyses, and we estimate there to be as many as the primary participants and thus expect to include 480 participants (ICOP and ICB), with an additional 72 participants in the waitlist group, for a total of 552. Eligible participants will be informed as to which group they are assigned to (either one of the two stress-management courses or the waitlist) but will remain ignorant of the particular conditions. The waitlist group (consisting of ten weeks on the waitlist and thereafter either the ICOP or ICB) will undergo a thorough briefing on the two courses and thereafter rate how attractive they find each course. They will then have the opportunity to choose which course they want to attend most.
2.2. Participants and inclusion criteria
HCP participants will be recruited from different healthcare settings such as intensive care units, acute care units, primary care, and residential aged care facilities.
The inclusion criteria will be as follows: the participants work directly with patients full-time or part-time, score 45 points or higher on the primary outcome measure Stress of Conscience Questionnaire (SCQ) (Glasberg et al., 2006 Nov 1), are proficient in Swedish, have the requisite time to attend a digital course, and accept the course's format. All these criteria will be assessed based on an interview conducted telephonically. The exclusion criteria include being partially or fully on sick leave due to stress. The participants will not be informed that our study focuses on stress of conscience nor the cut-off values for inclusion (SCQ ≥ 45). Only participants with SCQ scores greater than or equal to 45 will be included in the primary analysis; however, participants with SCQ scores below 45 will be included for some of the secondary analyses. Including participants with SCS scores below 45 is relevant for exploratory purposes and also makes the study more pertinent for employers since we will include all interested HCPs. It also allows for us to keep the participants unaware of the primary focus of the study, namely studying the effects on SCQ for participants with initial high levels of stress of conscience. In addition, including those who do not experience stress of conscience makes it possible to study the effect of this group and analyse the importance of and relationships between different factors before and after the courses. Finally, more participants would increase statistical power.
2.3. Recruitment and procedure
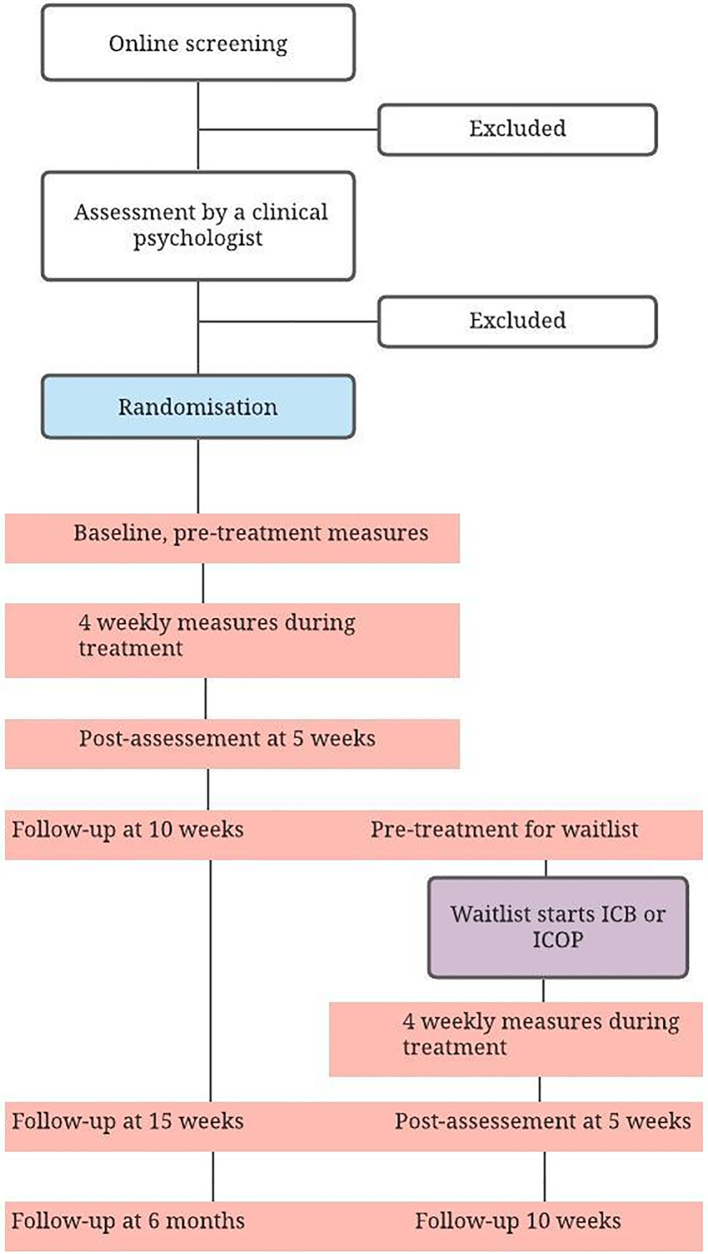
Recruitment will take place via various healthcare settings across Sweden, such as special social media groups for healthcare professionals. Contact information will be presented on the recruitment material and, if interested, potential participants could fill out a screening questionnaire at the BASS-4, a safe and digital platform from Karolinska Core Facilities. Thereafter, the participants will be contacted by a clinical psychologist for telephonic assessment (Fig. 1).
Fig. 1.
Flowchart of participants.
2.4. Timeline
The participants will complete all the outcome measures via the BASS-4 at 0, 5, 10, and 15 weeks and 6 months. In addition, the participants will complete weekly assessments during their courses. The weekly measures (see below) consist of four questions from the SCQ, two questions from the COPSOQ, and two questions from the SCS. The waitlist group will complete all the assessments as well, except for the follow-up at 15 weeks and 6 months. They will be on the waitlist for ten weeks and will thereafter be placed in either the ICOP course or the ICB course.
The RCT is planned to start participant recruitment in September 2021. During February to April 2021, we conducted a feasibility study, and therefore, the status of the trial at clinicaltrials.gov is ‘recruiting’, although the large-scale trial has not yet started. Recruitment is planned to continue during 2022 and 2023, due to the large scale of participants.
2.5. Measures
2.5.1. Primary outcome measure: stress of conscience questionnaire
The purpose of the SCQ is to estimate levels of stress related to a troubled conscience (Glasberg et al., 2006 Nov 1; Åhlin et al., 2015). The cut-off value for inclusion of 45 was chosen based on a prior study wherein two groups of HCPs had a mean value of 43.34 and 61.22, respectively, and these values were regarded as high levels of stress of conscience compared to earlier findings (Åhlin et al., 2021). The questionnaire has hitherto shown good internal consistency with a Cronbach's alpha of 0.83 in the original study by Glasberg et al. (2006 Nov 1) and 0.86 in that by Åhlin et al. (2015). The SCQ consists of nine items describing various healthcare situations, each made up of two parts, namely an A question and a B question. Question A concerns how frequently the subject estimates that the situation discussed arises in the workplace. This is assessed on a 6-point Likert scale, where 0 is ‘Never’ and 5 stands for ‘Every day’. For each A question, there is a subsequent B question in which the degree to which one's conscience is troubled by the given situation is estimated on a 10 cm visual analogue scale. The scale ranges from 0 (‘No, it gives me no troubled conscience at all’) to 5 (‘Yes, it gives me a very troubled conscience’).
2.5.2. Secondary outcome measures
2.5.2.1. Professional quality of life scale
Professional quality of life is the quality that an HCP feels in relation to their work as a caregiver (Stamm, 2010). Both the positive and negative aspects of doing one's job exert an influence on one's professional quality of life. The PROQOL has hitherto shown adequate to good reliability from 0.75 to 0.88 (Stamm, 2010; Keesler and Fukui, 2020). Professional quality of life comprises two aspects, namely a positive (compassion satisfaction) and a negative (compassion fatigue) aspect. Compassion fatigue is divided into two parts: the first concerns notions such as exhaustion, frustration, anger, and depression, which are typical of burnout. Secondary traumatic stress is a negative feeling driven by fear and work-related trauma. Trauma at work can be a direct (primary) trauma, and in other cases, it can be a combination of both primary and secondary trauma. The PROQOL consists of 30 questions assessed on a 5-point Likert scale, where 0 stands for ‘Never’ and 5 for ‘Very often’.
2.5.2.2. Work-related stress Copenhagen psychosocial questionnaire
The third version of the COPSOQ includes psychosocial factors at work such as stress and the well-being of employees (Thorsen and Bjorner, 2010; Berthelsen et al., 2020 Jan). The scale has shown adequate or good reliability (ranging from 0.70 to 0.89). The questionnaire can be found in either a long, medium, or short version. The questionnaire can be used as a menu wherein the researcher chooses questions and scales depending on the research questions. In our study, we included questions from the medium version of 89 questions distributed across 27 scales and 33 questions distributed across 11 scales that reflect either work-related stress or general mental health. The questions were assessed on a 5-point Likert scale, measuring either intensity (from ‘To a very large extent’ to ‘To a very small extent’) or frequency (from ‘Always’ to ‘Never/hardly ever’).
2.5.2.3. Self-compassion scale
The SCS includes questions about whether the individual is being kind and understanding rather than self-critical toward themselves when facing difficulties. The 26-item SCS has shown good internal consistency (0.92) (Neff, 2003). It is assessed on a 5-point Likert scale, where 0 corresponds with ‘Almost never’ to 5 for ‘Almost always’.
2.5.2.4. Weekly measures
The participants will answer eight weekly questions after completing each module. Four questions are derived from the SCQ (‘Do you ever find yourself avoiding patients or family members who need help or support?’; ‘Is your work in health care ever so demanding that you don't have the energy to devote yourself to your family as you would like?’; ‘Do you ever feel that you cannot live up to others’ expectations of your work?’; ‘Do you ever lower your aspirations to provide good care?’). Two questions were from the COPSOQ (‘How often have you had problems relaxing?’; ‘How often have you felt stressed?’). The last two questions were from the SCS (‘I'm kind to myself when I'm experiencing suffering’; ‘When something upsets me, I get carried away by my feelings’).
2.5.2.5. Sick leave
Sick leave will be collected from the MIDAS registry of the Swedish Social Insurance Agency. The number of periods of sick leave will be assessed using the registry MiDAS (Mikrodata för analys av. socialförsäkringen; Microdata for Analysis of Social Insurance) from week 5 after baseline until week 52 after baseline.
2.5.2.6. Sociodemographic information
The participants’ age, gender, occupation, workplace, working hours, number of children living at home, and a history of sick leave due to stress will be collected. Furthermore, the participants will be asked to describe what factors they think affect their work-related stress.
2.6. Other measures
2.6.1. Satisfaction with treatment
The participants’ satisfaction with the internet-based courses will be measured using the eight-item version of the Client Satisfaction Questionnaire (Keesler and Fukui, 2020). The total score scale ranges from 8 to 32, where a higher score indicates a higher degree of client satisfaction. Each item is rated on a scale of 1–4. High internal consistency has been found: 0.93 in the original English version (Thorsen and Bjorner, 2010) and 0.93 in the Swedish sample (Berthelsen et al., 2020 Jan). In this study, we will use the same modified version as in Käll et al. (2020).
2.6.2. Treatment credibility scale
The TCS will be used to assess the participants’ credibility of and expectations regarding the courses (Neff, 2003). Cronbach's alpha showed high internal consistency (0.79–0.90 for the expectancy factor and 0.81–0.86 for the credibility factor). The six-item scale uses a 10-point Likert-type scale ranging from 1 ‘Not logical at all’ to 10 ‘Very logical’: ‘How logical does the treatment seem?’; ‘How applicable does the treatment seem applicable to your problems?’; ‘How helpful do you think the treatment will be?’
2.6.3. Evaluation of the courses
The evaluation of the courses will be assessed through 28 questions about the text material, the online platform, support from the course leader, etc.
2.6.4. Adherence to the course
Adherence will be explored by counting the number of modules that the participants complete. In addition, the number of messages sent by the participant and/or phone contact with the course leader will be collected.
2.7. Randomisation
An independent party (Karolinska Trial Alliance) will conduct the randomisation process. Eligible participants will be randomised into ICOP, ICB, or the waitlist in a ratio of 17:17:4.
2.8. Ethical approval and registration
The study protocol was approved by the Swedish Ethical Review Authority (Dnr 2020-05505, Dnr 2021-03415) and registered at ClinicalTrials.gov (ID NCT04700878). All eligible participants will be informed both orally and in writing. Informed written consent to participate will be collected via the secure platform BASS-4. The platform is hosted on an encrypted traffic server and a two-step login with double authentication guarantees participant confidentiality.
2.9. Interventions
The ICOP and ICB courses will be delivered via BASS-4, a safe digital platform from the Karolinska Core Facilities. Both courses are structured as five-module self-help programs delivered for five weeks with weekly reports to and feedback from a course leader (either a qualified psychologist or psychotherapist) online. The modules in the ICOP and ICB courses will consist of text, reflection exercises, video clips, audio exercises, and homework assignments. The participants will have weekly contact with their course leader via a secure built-in messaging system. The homework assignments for each module are to be completed for each module; however, the participants will be able to continue onto the next module even if they do not complete their homework. The course leaders will provide feedback and encourage the participants in their work; if needed, they could get in contact with the course leaders telephonically.
2.9.1. The ICOP course
The compassion course is designed to motivate participants to care for their well-being by becoming warm and understanding toward themselves when feeling distressed rather than being harsh and judgmental (Gilbert, 2020). The content involves developing key compassionate attributes and skills of compassion through a combination of psychoeducation, emotion-regulation skills, and compassion techniques such as distress tolerance and non-judgement (see Table 1).
Table 1.
Outline of the ICOP course.
| Modules | Content | Exercises and homework |
|---|---|---|
| Module 1 | Psychoeducation about the three-circle model and an exploration into what compassion is | Attention exercise:
|
| Module 2 | Psychoeducation about our “tricky brains”; our compassionate self versus our inner self-critic |
|
| Module 3 | Exploring our emotions and our “multiple parts”; how to develop a compassionate self |
|
| Module 4 | Exploring our inner critics: how to take care of it and be compassionate |
|
| Module 5 | How to use the compassionate mind when facing difficulties in everyday life and how to take a compassionate approach to the future |
|
2.9.2. The ICB course
The ICB course includes CBT for stress-related problems to the same extent as the ICOP course, which consists of five modules for five weeks. The ICB course includes psychoeducation about stress, CBT exercises to cope with work-related stress, and homework assignments and exercises to the same extent as that of the ICOP course (see Table 2).
Table 2.
Outline of the ICB course.
| Modules | Content | Exercises and homework |
|---|---|---|
| Module 1 | Psychoeducation about the cognitive-behavioural perspective and its relation to stress, the effects of long-term stress, and the importance of recovery |
|
| Module 2 | Psychoeducation about the negative effects of non-recovery from stressful situations and activities that help to relieve stress |
|
| Module 3 | Identifying one's core life values and how one wants to live life |
|
| Module 4 | Psychoeducation about emotions and identifying situations where one acts on negative emotions |
|
| Module 5 | Behavioural experiments to strengthen new ways of being |
|
2.9.3. Dropout or attrition
Drop-out rates are often high in internet-based interventions. When participants do not adhere to the courses or answer the questionnaires, they will receive automatic reminders from the BASS-4 platform. If the participants are found to be inactive, the course leaders will contact them telephonically. Although the dropout rates may be high, participants have the option of discontinuing the courses if their own stressful situations become overwhelming. The reasons for any premature termination of the courses will be collected. Following the intention-to-treat principle, this analysis will include data from all of the participants. Those who do not complete the courses will be encouraged to complete the questionnaires at each time point.
2.10. Power analysis
The sample size was determined based on an expected between-group effect size (between ICOP and ICB) of Cohen's d = 0.4 for the primary outcome at the five-week follow-up for the primary analysis for participants with SCQ scores of 45 and higher. To reach 80% power, we need 100 participants in each active arm (ICOP and ICB). Expecting 20% attrition, we will include 120 participants in each active arm for the primary analysis. Thirty participants are required in the waitlist group with an expected between-group effect between the ICOP group and the waitlist of d = 0.8. Including the expected attrition, 36 participants will be required.
Given the 200 participants and a power of 80%, the non-inferiority analysis will provide a minimal clinically important difference (MCID) of roughly d = 0.35. As far as we know, there has been no previous effort to empirically establish an MCID for stress or stress of conscience, but our study is in line with the level recommended or used in intervention studies of mental health conditions (e.g. (Cuijpers et al., 2014; Blom et al., 2015 Jul; Kraepelien et al., 2018 Jul) and is deemed satisfactory due to the secondary nature of the non-inferiority analysis in the current trial.
2.11. Planned analyses
2.11.1. Baseline comparisons
Descriptive statistics will be used to analyse the demographic information and characteristics of the participants (i.e., age, gender, occupation, workplace, working hours, number of children living at home, and a history of sick leave due to stress). Differences in demographic information at baseline between groups will be analysed using the Chi-squared test for categorical variables and analysis of variance (ANOVA) or the t-test for continuous variables.
2.11.2. Effectiveness analyses for primary and secondary outcomes
The intention-to-treat (ITT) approach will be used to test the effectiveness of the ICOP group compared to the ICB group (Tripepi et al., 2020). Repeated-measures data will be analysed using a generalised estimating equation (GEE) for repeated measurements, using data from pre-treatment, post-assessment, and follow-up, to determine whether changes over time differ between the groups and whether the improvements achieved persist over time. For the non-inferiority analyses, estimated means and confidence intervals from the GEE model will be used to establish if the ICOP group is above the threshold determined by the MCID of d = 0.35 and the mean for the ICB group.
Missing data will be managed when using GEE, where the main model will also include baseline factors that correlate with both missingness and outcome as co-variates, and a sensitivity analyses will be conducted without these co-variates. In terms of other analyses, the main analyses will be done using observed data and will be complemented with sensitivity analyses using multiple imputation to handle missing data. The primary measuring point for the primary and secondary outcomes are post-assessments at 5 weeks. Effect sizes as Cohen's d will be calculated, and 95% confidence intervals will be reported. An effect size of 0.20 is considered small, 0.50 moderate, and 0.80 large (Sawilowsky, 2009 Nov 1).
Mediation analyses will be conducted to test whether self-compassion mediates the relationship between stress of conscience and burnout symptoms using PROCESS for SPSS (Hayes, 2017). We will explore whether self-compassion mediates change in stress of conscience using a simple mediation model. In addition, a two-mediator model in which X (intervention ICOP/ICB) affects burnout symptoms Y (COPSOQ) through four pathways—(1) self-compassion (SCS); (2) stress of conscience (SCQ) (3) through both (1) and (2); or (4) direct from X to Y (see Fig. 2)—will be used. Change in self-compassion, stress-of conscience and burnout symptoms will be explored in different models by using both weekly measures, as well as post-assessment of SCS, SCQ, and COPSOQ at 5, 10, and 15 weeks.
Fig. 2.
A two-mediator model of burnout symptoms.
3. Discussion
The present study protocol has described an RCT with the aim to examine whether an internet-based compassion course may be effective in reducing stress of conscience and work-related stress in HCPs. A single-blind randomised trial will be conducted across three groups: a compassion stress management course (ICOP), a cognitive-behavioural stress management course (ICB), and a waitlist. Stress-related disorders constitute a high proportion of those who are on sick leave due to mental health problems in Sweden, and stress-related exhaustion is an increasing cause of sick leave (Försäkringskassan, 2020a; Försäkringskassan, 2020b). HCPs are at risk for stress-related mental health issues, and factors such as a lack of balance between work and family, being divorced, and working within the healthcare sector are associated with a higher prevalence of sick leave due to stress. Given this situation, there is an urgent need for psychological interventions to prevent stress-related mental health issues. We anticipate that this project can contribute to the well-being of HCPs by lowering levels of stress of conscience and work-related stress and prevent stress-related mental health problems.
The work environment for HCPs is very demanding and stressful with low control, thereby placing them at risk of poor health. Both the ICOP and ICB courses are hypothesised to help participants balance work and private life and reduce stress. While the effects of CBT interventions in reducing stress are proven (Heber et al., 2017 Feb 17), there is still a need for more research on the effects of CMT interventions (Dhokia et al., 2020 Nov; Halamová et al., 2020 May 29; Lennard et al., 2021). Compassion is essential in HCPs’ work. Although compassion stems from an innate human attribute, it is also a skill that can be developed through training (Sinclair et al., 2020 Aug 5). The compassion course includes CMT, which has been found to increase self-compassion, positive emotions, and well-being as well as lower self-criticism and distress in both the general population (C Irons C. Heriot-Maitland Compassionate mind training: an 8-week group for the general public. Psychol. Psychother. Theory Res. Pract. [Internet]. [cited, 2020) and mental health nurses (McEwan et al., 2020). CMT has been developed to help individuals increase their ability to soothe themselves in stressful situations, and regulate negative emotions such as shame (Gilbert, 2010; Gilbert, 2014). Previous studies have revealed that CMT can help participants develop a sense of inner trust and the ability to stand up for themselves and set boundaries in stressful situations (Bratt et al., 2019; Bratt et al., 2020). Therefore, we hypothesise that the ICOP course will be more effective in lowering stress of conscience levels compared to the ICB course, a subject not yet explored in this field. Conscience is an important asset and a driving force for HCPs in their work (Åhlin et al., 2021). However, when an HCP's conscience begins to take a demanding toll and the need to silence or deaden it in order to keep working with a patient arises, what may otherwise be considered an asset becomes a burden (Juthberg, 2008). An important aspect of CMT is balancing self-criticism and improving the ability to support oneself in difficult situations (Beaumont et al., 2021). Women, in particular, struggle with stress of conscience and high levels of self-criticism, which may be one reason for their higher levels of burnout symptoms (Åhlin et al., 2021; Duarte et al., 2016 Aug).
HCPs are continuously exposed to the suffering of those in their care, which can negatively impact their professional ability and personal lives and also lead to exhaustion and compassion fatigue (Delaney, 2018 Nov). Emerging research suggests that compassion training can enhance resilience in nurses; that is, their ability to cope with stress and maintain their well-being despite facing work-related adversity (Delaney, 2018 Nov). Although these results are promising, more studies are needed to replicate these findings in larger samples using RCTs.
Although it is not the focus of this study, it is worth mentioning that in addition to the beneficial effects of HCPs, a compassion-oriented approach has been shown to improve the relationships that exist between patients and staff, increase patient satisfaction with their care, and reduce patient anxiety and stress (Sinclair et al., 2016 Jul 11; Sinclair et al., 2017a). In this regard, compassion, presence, recognition, availability, and mutuality are found to be core components in patient-HCP relationships (Bratt et al., 2020; Juthberg, 2008). Such a relationship may improve the patients’ health and well-being through the HCPs being attuned to the patient's unique experiences.
This study has some notable strengths. Firstly, the RCT results will provide important information regarding stress-management interventions for HCPs. In addition, we expect that HCPs will benefit from the ICOP and ICB courses, namely their stress of conscience and work-related stress will be reduced compared to that of the waitlist controls. A feasibility study has already been conducted in spring 2021 using qualitative data, which considers the views of HCPs regarding both the ICOP and ICB courses, and the courses were adapted accordingly to meet their needs in terms of course content.
The study also has some limitations. Firstly, using self-referrals in RCTs can be problematic since the participants may not represent the general HCP population. Secondly, high levels of stress may be a potential barrier to uptake by HCPs. Time shortage for those who need the stress-management interventions the most may also be a potential problem for participation; in the feasibility study conducted in spring 2021, we noticed time shortage was a problem for participants. Although their employer allowed them to participate in the ICOP or ICB courses during worktime, some participants did not have time for this and instead had to participate during their spare time. Although the stress-management courses were perceived as helpful, finding time for participating in fact caused more stress.
3.1. Conclusions
The present study protocol has described a RCT with the aim to examine whether an internet-based compassion course may be effective in reducing stress of conscience and work-related stress in HCPs. The RCT is planned to start in September 2021, by the ICOP research team at Linnaeus University, Sweden. There is a great need for preventive interventions for stress-related mental health issues in HCPs due to their exposure to work-related stress. We expect that this study will contribute to the development of two effective internet-based psychological interventions that will reduce stress of conscience and work-related stress in HCPs, promoting resilience when faced with suffering.
CRediT authorship contribution statement
AB and VK designed the study. AB wrote the first draft of the manuscript, and VK revised the manuscript critically. All authors have consistently contributed with feedback regarding study design, and have read and revised the manuscript, and approved the final manuscript.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
The authors of the study protocol would like to thank Ludvig Wärnsten, Tilda Widegren, Ida Olsson, Stina Börjesson, Patrik Dahlberg, Sara Nikoo and Cecilia Gunnarsson for their assistance in setting up the modules on the internet platform, and in working as therapists in the feasibility study. The authors would also like to thank Erik Sjöstrand from the BASS-team at Karolinska Institute for all technical support and help in setting up the ICOP and ICB courses.
Funding
This work is supported by The Crafoord Foundation, Sweden [grant number 20210849].
References
- Åhlin J., Ericson-Lidman E., Norberg A., Strandberg G. A comparison of assessments and relationships of stress of conscience, perceptions of conscience, burnout and social support between healthcare personnel working at two different organizations for care of older people. Scand. J. Caring Sci. 2015;29(2):277–287. doi: 10.1111/scs.12161. [DOI] [PubMed] [Google Scholar]
- Åhlin J., Ericson-Lidman E., Strandberg G. Assessments of stress of conscience, burnout and social support amongst care providers in home care and residential care for older people. Scand. J. Caring Sci. 2021 doi: 10.1111/scs.12970. http://onlinelibrary.wiley.com/doi/abs/10.1111/scs.12970 (n/a). Available from: [DOI] [PubMed] [Google Scholar]
- Beaumont E., Irons C., Rayner G., Dagnall N. Does compassion-focused therapy training for health care educators and providers increase self-compassion and reduce self-persecution and self-criticism? J. Contin. Educ. Heal. Prof. 2016;36(1):4–10. doi: 10.1097/CEH.0000000000000023. [DOI] [PubMed] [Google Scholar]
- Beaumont E., Bell T., Fairhurst H., McAndrew S. The impact of compassionate mind training on qualified health professionals undertaking a compassion-focused therapy module. Couns. Psychother. Res. 2021 https://onlinelibrary.wiley.com/doi/abs/10.1002/capr.12396 Mar 23];n/a(n/a). Available from: [Google Scholar]
- Berthelsen H., Westerlund H., Bergström G., Burr H. Validation of the Copenhagen psychosocial questionnaire version III and establishment of benchmarks for psychosocial risk Management in Sweden. Int. J. Environ. Res. Public Health. 2020 Jan;17(9):3179. doi: 10.3390/ijerph17093179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blom K., Tarkian Tillgren H., Wiklund T., Danlycke E., Forssén M., Söderström A., et al. Internet-vs. group-delivered cognitive behavior therapy for insomnia: a randomized controlled non-inferiority trial. Behav. Res. Ther. 2015 Jul;1(70):47–55. doi: 10.1016/j.brat.2015.05.002. [DOI] [PubMed] [Google Scholar]
- Bratt A.S., Svensson I., Rusner M. Finding confidence and inner trust as a parent: experiences of group-based compassion-focused therapy for the parents of adolescents with mental health problems. Int. J. Qual. Stud. Health Well Being. 2019;14(1):1684166. doi: 10.1080/17482631.2019.1684166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bratt A.S., Gralberg I.-M., Svensson I., Rusner M. Gaining the courage to see and accept oneself: group-based compassion-focussed therapy as experienced by adolescent girls. Clin. Child Psychol. Psychiatry. 2020;25(4):909–921. doi: 10.1177/1359104520931583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- C Irons C. Heriot-Maitland Compassionate mind training: an 8-week group for the general public. Psychol. Psychother. Theory Res. Pract. [Internet]. [cited 2020 Dec 10];n/a(n/a). Available from: https://bpspsychub.onlinelibrary.wiley.com/doi/abs/10.1111/papt.12320. [DOI] [PubMed]
- Craig C., Hiskey S., Spector A. Compassion focused therapy: a systematic review of its effectiveness and acceptability in clinical populations. Expert. Rev. Neurother. 2020;20(4):385–400. doi: 10.1080/14737175.2020.1746184. (just-accepted) [DOI] [PubMed] [Google Scholar]
- Cuijpers P., Turner E.H., Koole S.L., van Dijke A., Smit F. What is the threshold for a clinically relevant effect? The case of major depressive disorders. Depress. Anxiety. 2014;31(5):374–378. doi: 10.1002/da.22249. [DOI] [PubMed] [Google Scholar]
- Delaney M.C. Caring for the caregivers: evaluation of the effect of an eight-week pilot mindful self-compassion (MSC) training program on nurses’ compassion fatigue and resilience. PLoS One. 2018 Nov;13(11) doi: 10.1371/journal.pone.0207261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dev V., Fernando A.T., Consedine N.S. Self-compassion as a stress moderator: a cross-sectional study of 1700 doctors, nurses, and medical students. Mindfulness. 2020 May 1;11(5):1170–1181. doi: 10.1007/s12671-020-01325-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhokia M., Elander J., Clements K., Gilbert P. A randomized-controlled pilot trial of an online compassionate mind training intervention to help people with chronic pain avoid analgesic misuse. Psychol. Addict. Behav. 2020 Nov;34(7):726–733. doi: 10.1037/adb0000579. [DOI] [PubMed] [Google Scholar]
- Duarte J., Pinto-Gouveia J., Cruz B. Relationships between nurses’ empathy, self-compassion and dimensions of professional quality of life: a cross-sectional study. Int. J. Nurs. Stud. 2016 Aug;1(60):1–11. doi: 10.1016/j.ijnurstu.2016.02.015. [DOI] [PubMed] [Google Scholar]
- Finlay-Jones A.L., Rees C.S., Kane R.T. Self-Compassion, Emotion Regulation and Stress among Australian Psychologists: Testing an Emotion Regulation Model of Self-Compassion Using Structural Equation Modeling. van der Feltz-Cornelis C, editor. PLoS One. 2015;10(7) doi: 10.1371/journal.pone.0133481. Jul 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Försäkringskassan . Uppföljning av sjukfrånvarons utveckling. 2020. p. 143. Report No.: 001382–2020. [Google Scholar]
- Försäkringskassan . A och prognos. Sjukfrånvaro i psykiatriska diagnoser. Vol. 8. 2020. p. 108. Report No. [Google Scholar]
- Galante J., Bekkers M.-J., Mitchell C., Gallacher J. Loving-kindness meditation effects on well-being and altruism: a mixed-methods online RCT. Appl. Psychol. Health Well Being. 2016;8(3):322–350. doi: 10.1111/aphw.12074. [DOI] [PubMed] [Google Scholar]
- Gilbert P. Routledge; 2005. Compassion: Conceptualisations, Research and use in Psychotherapy. 417 p. [Google Scholar]
- Gilbert P. Introducing compassion-focused therapy. Adv. Psychiatr. Treat. 2009;15(3):199–208. [Google Scholar]
- Gilbert P. New Harbinger Publications, Inc.; Oakland, CA: 2010. The Compassionate Mind: A New Approach to Life’s Challenges. [Google Scholar]
- Gilbert P. The origins and nature of compassion focused therapy. Br. J. Clin. Psychol. 2014;53(1):6–41. doi: 10.1111/bjc.12043. [DOI] [PubMed] [Google Scholar]
- Gilbert P. Compassion: from its evolution to a psychotherapy. Front. Psychol. 2020:11. doi: 10.3389/fpsyg.2020.586161. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7762265/ Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasberg A.-L., Eriksson S., Dahlqvist V., Lindahl E., Strandberg G., Söderberg A., et al. Development and initial validation of the stress of conscience questionnaire. Nurs. Ethics. 2006 Nov 1;13(6):633–648. doi: 10.1177/0969733006069698. [DOI] [PubMed] [Google Scholar]
- Halamová J., Kanovský M., Pačutová A., Kupeli N. Randomised controlled trial of an online version of compassion mind training in a nonclinical sample. Eur. J. Psychol. 2020 May 29;16(2):262–279. doi: 10.5964/ejop.v16i2.1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. Guilford Publications; 2017. Introduction to Mediation, Moderation, and Conditional Process Analysis, Second Edition: A Regression-based Approach. 713 p. [Google Scholar]
- Heber E., Ebert D.D., Lehr D., Cuijpers P., Berking M., Nobis S., et al. The benefit of web- and computer-based interventions for stress: a systematic review and meta-analysis. J. Med. Internet Res. 2017 Feb 17;19(2) doi: 10.2196/jmir.5774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juthberg C. Umeå University; Umeå: 2008. Samvetsstress hos vårdpersonal i den kommunala äldreomsorgens särskilda boenden. [Google Scholar]
- Käll A., Jägholm S., Hesser H., Andersson F., Mathaldi A., Norkvist B.T., et al. Internet-based cognitive behavior therapy for loneliness: a pilot randomized controlled trial. Behav. Ther. 2020;51(1):54–68. doi: 10.1016/j.beth.2019.05.001. [DOI] [PubMed] [Google Scholar]
- Keesler J.M., Fukui S. Factor structure of the professional quality of life scale among direct support professionals: factorial validity and scale reliability. J. Intellect. Disabil. Res. 2020;64(9):681–689. doi: 10.1111/jir.12766. [DOI] [PubMed] [Google Scholar]
- Kelman A.R., Evare B.S., Barrera A.Z., Muñoz R.F., Gilbert P. A proof-of-concept pilot randomized comparative trial of brief internet-based compassionate mind training and cognitive-behavioral therapy for perinatal and intending to become pregnant women. Clin. Psychol. Psychother. 2018;25(4):608–619. doi: 10.1002/cpp.2185. [DOI] [PubMed] [Google Scholar]
- Kirby J.N., Tellegen C.L., Steindl S.R. A meta-analysis of compassion-based interventions: current state of knowledge and future directions. Behav. Ther. 2017;48(6):778–792. doi: 10.1016/j.beth.2017.06.003. [DOI] [PubMed] [Google Scholar]
- Kraepelien M., Forsell E., Karin E., Johansson R., Lindefors N., Kaldo V. Comparing individually tailored to disorder-specific internet-based cognitive–behavioural therapy: benchmarking study. BJPsych Open. 2018 Jul;4(4):282–284. doi: 10.1192/bjo.2018.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger T., Reber F., von Glutz B., Urech A., Moser C.T., Schulz A., et al. An internet-based compassion-focused intervention for increased self-criticism: a randomized controlled trial. Behav. Ther. 2019 Mar 1;50(2):430–445. doi: 10.1016/j.beth.2018.08.003. [DOI] [PubMed] [Google Scholar]
- Lennard G.R., Mitchell A.E., Whittingham K. Randomized controlled trial of a brief online self-compassion intervention for mothers of infants: effects on mental health outcomes. J. Clin. Psychol. 2021;77(3):473–487. doi: 10.1002/jclp.23068. [DOI] [PubMed] [Google Scholar]
- McEwan K., Minou L., Moore H., Gilbert P. Engaging with distress: training in the compassionate approach. J. Psychiatr. Ment. Health Nurs. 2020;27(6):718–727. doi: 10.1111/jpm.12630. [DOI] [PubMed] [Google Scholar]
- McVicar A., Pettit A., Knight-Davidson P., Shaw-Flach A. Promotion of professional quality of life through reducing fears of compassion and compassion fatigue: application of the compassionate mind model to specialist community public health nurses (Health Visiting) training. J. Clin. Nurs. 2021 Jan;30(1–2):101–112. doi: 10.1111/jocn.15517. [DOI] [PubMed] [Google Scholar]
- Neff K. The development and validation of a scale to measure self-compassion. Self Identity. 2003;2(3):223–250. [Google Scholar]
- Sawilowsky S.S. New effect size rules of thumb. J. Mod. Appl. Stat. Methods. 2009 Nov 1;8(2):597–599. [Google Scholar]
- Sinclair S., Torres M.-B., Raffin-Bouchal S., Hack T.F., McClement S., Hagen N.A., et al. Compassion training in healthcare: what are patients’ perspectives on training healthcare providers? BMC Med. Educ. 2016 Jul 11;16(1):169. doi: 10.1186/s12909-016-0695-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair S., Kondejewski J., Raffin-Bouchal S., King-Shier K.M., Singh P. Can self-compassion promote healthcare provider well-being and compassionate care to Others? Results of a systematic review. Appl. Psychol. Health Well Being. 2017;9(2):168–206. doi: 10.1111/aphw.12086. [DOI] [PubMed] [Google Scholar]
- Sinclair S., Kondejewski J., Raffin-Bouchal S., King-Shier K.M., Singh P. Can self-compassion promote healthcare provider well-being and compassionate care to others? Results of a systematic review. Appl. Psychol. Health Well Being. 2017 Jul 1;9(2):168–206. doi: 10.1111/aphw.12086. [DOI] [PubMed] [Google Scholar]
- Sinclair S., Hack T.F., McClement S., Raffin-Bouchal S., Chochinov H.M., Hagen N.A. Healthcare providers perspectives on compassion training: a grounded theory study. BMC Med. Educ. 2020 Aug 5;20(1):249. doi: 10.1186/s12909-020-02164-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stamm Hudnall B. ProQOL.org; 2010. The Concise ProQOL Manual. [Google Scholar]
- Thorsen S.V., Bjorner J.B. Reliability of the copenhagen psychosocial questionnaire. Scand. J. Public Health. 2010;38(3_suppl):25–32. doi: 10.1177/1403494809349859. Feb 1. [DOI] [PubMed] [Google Scholar]
- Tripepi G., Chesnaye N.C., Dekker F.W., Zoccali C., Jager K.J. Intention to treat and per protocol analysis in clinical trials. Nephrology. 2020;25(7):513–517. doi: 10.1111/nep.13709. [DOI] [PubMed] [Google Scholar]