Abstract
Background:
Digital Twins (DTs), virtual copies of physical entities, are a promising tool to help manage and predict outbreaks of Covid-19. By providing a detailed model of each patient, DTs can be used to determine what method of care will be most effective for that individual. The improvement in patient experience and care delivery will help to reduce demand on healthcare services and to improve hospital management.
Objectives:
The aim of this study is to address 2 research questions: (1) How effective are DTs in predicting and managing infectious diseases such as Covid-19? and (2) What are the prospects and challenges associated with the use of DTs in healthcare?
Methods:
The review was structured according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) framework. Titles and abstracts of references in PubMed, IEEE Xplore, Scopus, ScienceDirect and Google Scholar were searched using selected keywords (relating to digital twins, healthcare and Covid-19). The papers were screened in accordance with the inclusion and exclusion criteria so that all papers published in English relating to the use of digital twins in healthcare were included. A narrative synthesis was used to analyse the included papers.
Results:
Eighteen papers met the inclusion criteria and were included in the review. None of the included papers examined the use of DTs in the context of Covid-19, or infectious disease outbreaks in general. Academic research about the applications, opportunities and challenges of DT technology in healthcare in general was found to be in early stages.
Conclusions:
The review identifies a need for further research into the use of DTs in healthcare, particularly in the context of infectious disease outbreaks. Based on frameworks identified during the review, this paper presents a preliminary conceptual framework for the use of DTs for hospital management during the Covid-19 outbreak to address this research gap.
Keywords: Digital Twins, healthcare, Covid-19, public health, disease outbreaks
Introduction
Background
The Covid-19 pandemic highlights the need for the ability to predict, and therefore better manage, infectious disease outbreaks. 1 One potential technology that could provide a means of addressing this challenge and improving hospital management and quality of care is a Digital Twin system. Digital Twins (DTs) are virtual representations of physical systems, objects, processes, or services visualising the represented entity.2,3 They learn from continuously updating real-time data and dynamically adapt their insights and recommendations to support improved decision-making. DTs are key to the industry 4.0 transformation, hence, research has been focussed in optimising manufacturing and production.2-5 For example, using DTs in the offshore renewable sector6,7 can reduce operational costs and maximise energy output due to the harshness of the environment where the devices operate. However, the application of DT technology to other sectors is growing, with the use of DTs in ‘smart cities’ offering huge potential.7,8 The potential for DTs to improve healthcare systems is also being increasingly explored,9,10 for example in personalised wellbeing specific to patient-centric dietary requirements 11 as they can be used to model anything from an organ to a patient to a hospital.12,13
DT technology is emerging as a key tool to shift towards a more patient-centric and personalised system of healthcare.9,11 Research on DTs in health and care is gaining momentum in areas such as personalised care, managing chronic conditions, 14 management of severe traumas by integrating DTs with agents and Multi-Agent Systems 12 and improving the management of public health emergencies. 15 DTs are also being used to improve hospital management and demand, with the aim of improving patient experience and care delivery. 16 Another area where this technology could potentially have a significant positive health impact is in the prediction and management of infectious disease outbreaks.
The novel coronavirus has exposed the unpreparedness of nearly every country for a global pandemic and has (as of December 15, 2021) resulted in over 271 million cases and nearly 5.3 million deaths. 17 Due to the global spread of the disease, and the ubiquity of mobile apps and digital technologies, there is a large body of data available about the Covid-19 pandemic. 18 DTs can collect data from a number of sources (such as IoT sensors, mobile apps and healthcare databases) in real time and analyse it to provide clear visualisations and insights. These insights could help hospital administrators and clinicians to better manage the availability of key resources (eg, hospital beds, ventilators, PPE, etc.) and the care of individual patients.
Rationale
There has been limited research on reviewing the applicability of DT in health and care. A search of PROSPERO (using several variations of the keywords ‘covid-19’ and ‘digital twins’) found no reviews registered about the application of DTs to the management of the Covid-19 pandemic. There are also few literature reviews on DTs in healthcare. A systematic review characterising DTs was identified, but although it included healthcare-related DTs, they were not a focus. 19 Additionally, a narrative review was found that provided an overview of DTs in pharmaceutical manufacturing. 20 No systematic reviews evaluating the potential and barriers of applying DTs in healthcare in general were found. However, a small number of companies in the healthcare industry are conducting research on the viability of DTs to optimise patient care and hospital management. 21 The Covid-19 pandemic has highlighted the need to further explore the potential role of DTs in predicting and managing infectious disease outbreaks. The ability to effectively track, trace and isolate positive infectious disease cases will minimise public harm and disruption to the economy. Therefore, there is a need for an overview of the literature concerning the use of DTs in infectious disease outbreaks and the opportunities and challenges associated with their use in healthcare more broadly.
Objectives
The primary objective of this study is to summarise the state of the field of the application of DTs in healthcare, with a focus on the use and effectiveness of DTs for managing infectious disease outbreaks (specifically the Covid-19 pandemic). To achieve this objective, the review will address 2 main research questions:
How effective are DTs in predicting and managing infectious diseases such as Covid-19?
What are the prospects and challenges associated with DTs in healthcare?
Methods
The review was structured using the PICO template and the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols Extension for Scoping Reviews) guidelines. 22 Appropriate Medical Subject Headings (MeSH) were selected for the search. The scoping review consists of a literature search, article selection, data extraction, data analysis and a discussion of the implications of the data for the research questions posed.
Eligibility criteria
The research question is based on the Population, Intervention, Comparison and Outcome (PICO) framework shown in Table 1.
Table 1.
PICO (Population, Intervention, Comparison and Outcome) criteria and definitions.
| PICO criteria | Definition |
|---|---|
| Population | Healthcare service (eg, hospital bed management) and patients encountering a DT in a health setting. |
| Intervention | DTs using data collected from all sources eg, sensors, devices and applications. |
| Comparison | No specific comparison is required. |
| Outcomes | ● The potential of DTs in the management of Covid-19 |
| ● Identification of the applications of DTs in health and care and description the technology (eg, DT model) |
Search strategy
A literature review was conducted on 4 academic databases: PubMed, IEEE Xplore, Scopus and ScienceDirect. An initial search was conducted on the 6th and 7th of August and the final search was conducted on the 12th of September, 2020. These 4 databases were chosen to cover the research areas in engineering and healthcare; IEEE Xplore and ScienceDirect comprehensively cover the engineering field, PubMed focuses on healthcare, and Scopus contains a large number of references in a variety of fields, and was included to capture anything missed by the more discipline-specific databases. To identify any relevant papers that are not included in those databases, Google Scholar was also searched. The Google search engine was used to identify grey literature and non-academic publications relevant to the subject and any relevant papers that may have been missed from earlier database searches.
The search terms were grouped into 3 themes and included with the structure: digital technology (MeSH OR Keywords) AND Application (MeSH OR Keywords) AND Covid-19 (MeSH OR Keywords). Keywords were searched for in the titles and abstracts of articles. Table 2 shows the search concept and keywords that were searched for this review. An example sample search string for the IEEE Xplore database is included in Appendix B.
Table 2.
Search terms.
| Category | MeSH | Keywords (in title or abstract) |
|---|---|---|
| Digital technology | Capacity management OR patient centric OR outbreak prediction | digital twin |
| Application | Health management | ‘health’ OR ‘care’ OR ‘healthcare’ OR ‘hospital’ OR ‘patient’ |
| Covid-19 | Covid-19 | ‘2019 novel coronavirus’ OR ‘2019-n-CoV’ OR COVID-19 OR coronavirus OR Covid |
We further conducted search in the Journal of Medical Ethics to capture the papers that discussed the social and ethical challenges of DT. Discussions from these papers are captured in Discussions section later. We used the search terms social OR ethical challenges of DT. The search returned 13 papers.
Inclusion criteria
All papers discussing the use of digital twins in a healthcare setting were eligible for inclusion in the review. There was no limit imposed based on the year of publication because the application of DT in healthcare is relatively new; in initial searches, the earliest relevant paper found was published in 2018.
All papers discussing the ethical and social challenges of DT were included.
Exclusion criteria
Studies that focussed on the application of DTs in non-health settings and that were not published in English were excluded as the search results returned only 3 papers that were not in the English language and the source was not secure. Papers and other grey literature concerning DTs that were published by companies were also excluded. These papers were excluded because the research was focussed on developing DT-based solutions for specific healthcare problems and was not peer reviewed in open access.
All papers that did not explicitly mention DT were excluded from the discussion.
Screening and article selection
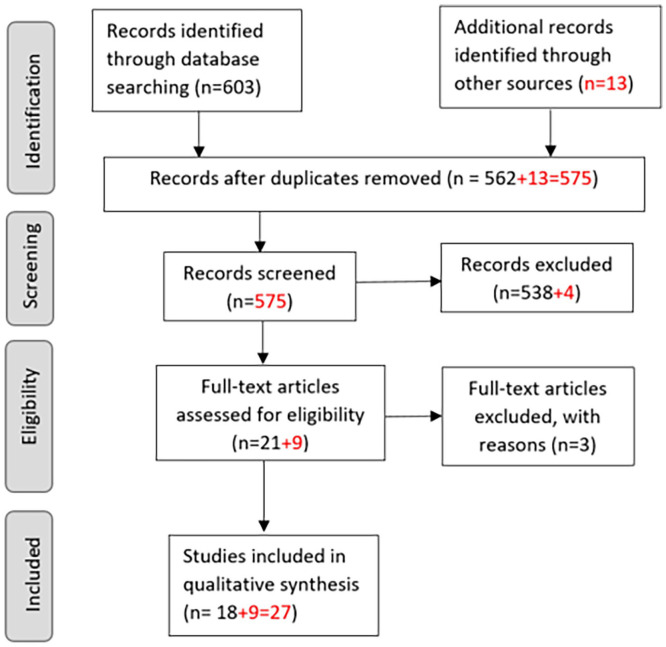
Journal articles, conference papers, non-academic papers and practitioner case reports retrieved by the search were downloaded and duplicates were manually removed. After duplicates were removed, the papers were screened in 3 consecutive phases – title, abstract and full text – based on the pre-specified inclusion and exclusion criteria. Details of the screening and selection process were recorded in a PRISMA flow diagram to ensure reproducibility (Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram of the search strategy.
Data extraction
Data was extracted from the papers selected for inclusion in the review by one reviewer. An initial review of the literature suggested items to be extracted (Table 3), but other data identified during the review were included if relevant.
Table 3.
Data extraction.
| Article information | Data extracted |
|---|---|
| General study information | Title of publication |
| Year of publication | |
| Authors | |
| Characteristics of digital technology | Digital twin model |
| Intended user/service |
Data analysis and synthesis
It was not feasible to conduct a meta-analysis or statistical analysis due to the variety of source types and reported outcomes. A narrative synthesis was conducted on the extracted data and is summarised in the discussion to provide an overview of the current literature on DTs in healthcare settings, to draw conclusions about their prospects and limitations, and to explore the potential of DTs in managing and predicting infectious disease outbreaks.
Results
Included studies
A total of 603 references were retrieved from the databases. After removing duplicates and screening abstracts and full texts, 18 papers were eligible for the study based on the inclusion and exclusion criteria and were reviewed. A record of the screening process was captured in a PRISMA flow diagram (Figure 1) and the PRISMA-Scr checklist is presented in Appendix A.
Study characteristics
There was a large variety of types of papers included in the review: some presented a review of DTs as applied to the healthcare sector, some papers proposed a framework (without testing it on live data) supporting cloud-based data storage. A further few papers proposed a DT model based on live patient data for specific disease management. Therefore, the papers were split into 3 groups as review papers (4/18),23-26 papers that presented a framework or model (8/18),9,12,15,27-31 and papers that focussed on a specific disease (eg, diabetes or a procedure such as conducting heart surgery, 6/18).14,32-36 The characteristics of the studies and the extracted data are summarised in Table 4.
Table 4.
Components of the review of papers.
| Publication type | Author(s) | Category | Year of publication | Publisher | Digital Twin model | Intended user/service |
|---|---|---|---|---|---|---|
| Journal | Mohapatra and Bose 23 | Review | 2020 | Springer Link Health Technol | A framework for digital twin implementation in the healthcare industry | Service improvement aimed at general public |
| Journal | Corral-Acero et al 24 | Review | 2020 | European Heart Journal | Application of DT to accelerate cardiovascular research and enable the vision of precision medicine | Clinician and patient |
| Chapter | Bagaria et al 25 | Review | 2020 | Springer Nature | DT for personal health and well-being | General public |
| Journal | Bruynseels et al 26 | Review | 2018 | Frontiers in Genetics | Digital twins privacy in healthcare technologies and ethics of biomedical data | General public and clinician |
| Journal | Liu et al 28 | Framework/Model | 2019 | IEEE Access | Cloud-Based Framework for the Elderly Healthcare Services Using Digital Twin | Elderly population |
| Journal | Rodríguez-Aguilar and Marmolejo-Saucedo 15 | Framework/Model | 2020 | EAI Endorsed Transactions on Pervasive Health and Technology | DT of the public emergency system | General public |
| Journal | Laamartet al 29 | Framework/ Model | 2020 | IEEE Access | QoE-based DT framework for health and well-being in smart cities | General public |
| Conference | Rivera et al 27 | Framework/Model | 2019 | ACM Digital Library | A DT reference model in healthcare for decision-making processes when applying medical treatments to patients by healthcare professionals. | General public |
| Conference | Lutze 30 | Framework/Model | 2019 | IEEE | A DT ehealth system focussing on information management | General public |
| PhD thesis | Albraikan 31 | Framework/Model | 2019 | University of Ottawa, Canada | A DT model for emotional well-being | General public/patient with non-clinical mental health issues |
| Journal | Björnsson et al 9 | Framework/Model | 2019 | Genome Med | Personalised medicine framework | General public |
| Journal | Croatti et al 12 | Framework/Model | 2020 | Med Syst. | Agent-based DTs to manage severe traumas | Trauma patient/Clinician |
| Journal | Chakshu et al 32 | Disease improvement | 2019 | Int J Numer Method Biomed Eng. | DT to detect the severity of carotid stenosis from head vibration | Clinician/patient |
| Preprint article | Rao and Mane 33 | Disease improvement | 2019 | Persistent Systems Ltd. | Customised per-patient DT model in liver disease diagnosis using Domain Knowledge and Machine Learning | Clinician/patient |
| Journal | Grosman et al 34 | Disease management | 2020 | Diabetes | DT programme to personalise MiniMed™ 670G settings in Type 1 diabetes patients | Clinician/patient |
| Journal | Walsh et al 14 | Disease improvement | 2020 | bioRxiv | DT for multiple sclerosis using probabilistic neural networks | Clinician/patient |
| Conference | Martinez-Velazquez et al 36 | Disease improvement | 2019 | IEEE | DT for cardiac patients | Clinician/patient |
| Conference | Mazumder et al 35 | Disease improvement | 2019 | IEEE | DT for Cardio-vascular patients | Clinician/patient |
Discussion
Principal findings
No peer reviewed papers were found that specifically addressed the potential of DTs to address the challenge posed by infectious disease outbreaks. Therefore, the review was unable to directly answer the first research question: ‘How effective are DTs in predicting and managing infectious diseases such as Covid-19?’ Potential benefits of DTs for healthcare in general – including increasing patient centricity and improving quality of care – were identified. However, the included studies also described key challenges associated with DTs in healthcare, including: interoperability, data processing, patient confidentiality and data security.
Prospects and challenges of DTs in healthcare
Recent research has proposed a potential role for DT technology in the management of hospital capacity 2 by using data and simulations to offer decision support to help improve the management of patients during public health emergencies. 18 DTs can help in developing patient-centric and personalised care by building a simulation of an individual based on their specific health data and insights from population health data, in improving the management of chronic conditions,11,14 and in guiding complex medical procedures. Moreover, DTs also have potential to help improve mental health and well-being by identifying trigger factors and suggesting coping techniques aimed at improving the quality of life holistically. 31
Recently, there has been emerging discussions on the social and ethical challenges of DT. It has been argued that for an ethically acceptable form of digital twin there are 5 conditions that should be met to avoid mis-representation or bias.37,38 This argument is expanded further to include the potential impact of the system on an individual so as not to inadvertently widen the gap in most vulnerable people and those with less cognitive resources. 39
Braun’s paper 37 has given rise to discussion by a number of researchers. This includes the viewpoint that the discussion on ethics is too early as the technology is not fully developed, 40 as well as concerns around access to the individual’s medical data by the company that developed the DT and hence could have control over.41-43 This argument has been expanded to add concerns around ownership, representation, agency, in addition to control. 44 Lupton 45 takes issue to the terminology ‘Digital Twin’ to be used in a medical care setting for a simulation model. The discussion on ethics is only just starting highlighting the challenges associated and will shape how the technology is embedded in medical care in the future.
Another key challenge for DT technology that was identified during the review is establishing interoperability and trust between different data sources contributing to the DT (eg, high-quality clinical/medical data integration with limited quality biometric and behavioural data from the smart home and wearables). 46 Another key challenge will be to find a way of balancing the cost and benefits of collecting and processing large amounts of data, while ensuring that data security and patient confidentiality are not compromised.
A small number of companies identified in the Google search have started to research the application of DT in managing the coronavirus pandemic.47-49 No peer-reviewed papers by these companies were identified, however, the conceptual case studies presented on these companies’ websites suggest that DTs have the potential to accelerate the vaccine production process 48 and improve hospital capacity, staffing and care delivery models, 47 and patient management (such as critical-care beds availability, ventilator availability, etc). 49 Therefore, DTs appear to have the potential to improve health and wellbeing of patients with novel diseases such as Covid-19 by using patient-specific simulations to trial new treatments and improve hospital management during crises. An established DT system could also potentially use data relating to patients’ symptoms and behaviour, such as the emotion-aware digital twin based on sensor data being developed by one of the papers, 31 to support the management of infectious disease outbreaks. This work can be extended to take account of external factors such as location and number of positive cases from a large sample of the population, collected to predict the next outbreak/hotspot for Covid-19. These simulations could facilitate the prediction of potential risks and provide mechanisms for optimal decision making with regards to hospital preparedness and resource management.
Conceptual DT framework for Covid-19 prediction and hospital management
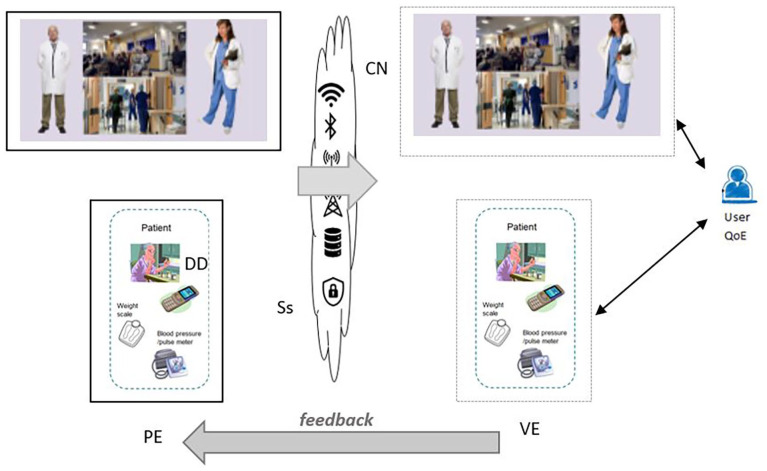
Limitations were identified in some of the models posited by the papers included in the review. For instance, one framework identified in the background research – which focussed on predicting the maintenance of complex equipment, and was not healthcare-specific – limited the development of the DT framework it proposed to five dimensions. 3 This is a limitation for a DT framework in hospital management because it does not sufficiently cover the potential variables or indicators needed to quantify successful management. One of the healthcare-specific DT frameworks included in this review introduced the concept of feedback based on the user’s quality of experience (QoE), 29 which will be an important aspect for a DT framework for hospital management. However, the framework used a very broad definition of health and well-being; data collected from wearable sensors and integrated with other healthcare data was used to suggest activity levels for the patient. The framework was simplistic and did not take into account the interaction of different variables, which would be a necessary component for a framework of hospital management. Although the literature on DTs is limited, both of the frameworks described were found to be useful for their specific applications of wind turbine lifecycle monitoring and increasing physical activity in participants.3,29 However, they are not adequate frameworks for this particular context.
In the context of Covid-19, this paper proposes a framework for hospital management that ensures that all of the relevant dimensions can be added in the DT model and that there is a feedback loop in real-time, or near real-time, to ensure that the QoE is maintained at an acceptable level. Based on the frameworks described,3,29 this paper proposes a patient-centric conceptual framework for Covid-19 hospital management based on the healthcare provider’s (the user’s) quality of experience (QoE). The five-dimensional architecture 3 is extended to n-dimensions as shown in equation (1)
| (1) |
where PE are the physical entities, VE are the virtual equivalents, Ss are the services for PE and VE, DD is the DT data and CN are the connections. Additional dimensions (XX1. . .XXn) can be added based on a specific application (eg, number of available beds, number of infected patients, etc). The conceptual DT framework is presented in Figure 2.
Figure 2.
Conceptual patient-centric hospital management DT framework for Covid-19.
In the proposed conceptual framework (Figure 2), the PE is the hospital capacity and VE is the digital replica of PE. DD is collected from a number of sources such as wearable devices, medication and other patient-centric data. Ss and CN information is collected from the network, both fixed and wireless access. The DT framework is predicted in terms of the user’s QoE. Further, we extend the framework to include prediction of the patient’s risk factors of getting Covid-19 based on patient-centric data collected from DD and/or specific questionnaires developed as an app to collect risk factors such as occupation, housing, etc. There is a feedback loop to ensure that the user’s QoE is maintained at an acceptable level.
Limitations
The main limitation of this review is that, given the lack of relevant studies identified in the search, the first research question could not be adequately answered. Although an effort was made to apply the knowledge gained from the included studies to propose a conceptual framework for the use of DTs in hospital management, no conclusions could be drawn about its validity or potential usefulness. Another limitation of this review is that the number of studies identified as eligible for inclusion in the study was relatively small; while this likely reflects the early state of the body of literature regarding DTs in healthcare, it is also possible that relevant articles were missed due to the inclusion of Covid-19 specific keywords in the search string. Therefore, although it was not intended to be the primary focus of this review, the overview of DTs in healthcare in general is likely to be incomplete.
Future directions
As none of the included papers examined the use or effectiveness of DTs in relation to hospital management during the Covid-19 pandemic (or any infectious disease outbreaks), this is clearly a key area for future research. While there are a small number of companies in the healthcare sector that are investigating the potential of DT to provide solutions for the problem of hospital patient capacity and management, there appears to be a lack of academic research developing or evaluating these solutions.
With increased focus on patient-centric care, DTs offer the potential to better predict and manage infectious diseases such as Covid-19. Some patients who have recovered from Covid-19 suffer from long Covid, others have developed severe cardiovascular conditions or other serious diseases.50,51 DTs could aide clinicians in predicting, based on risk factors, if a patient is likely to develop a serious health condition, or the probability that they will suffer from long Covid. This could help the healthcare sector to better manage the resources and provide support and monitoring to those who are at highest risk. There is an urgency to better understand these risk factors post-Covid and propose patient-centric solutions that will improve patients’ quality of life by giving them the appropriate supportive therapy.
Conclusions
The purpose of this scoping review was to examine the prospects and challenges associated with using Digital Twins in healthcare, with a particular focus on their potential to help predict and manage infectious disease outbreaks such as Covid-19. No studies were identified that used DTs for Covid-19 in particular (or infectious disease outbreaks in general), so the potential of DTs for hospital management during an outbreak was explored. This review extended the literature by providing an initial overview of the prospects and challenges of applying DT technology in the healthcare sector. There is a significant lack of research in the examination of DTs’ potential for improving hospital management, particularly in the context of infectious disease outbreaks, and research on the use and effectiveness of DTs in this context is urgently required.
Appendices
Appendix A. PRISMA-ScR checklist
Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist for Khan et al. ‘A Scoping Review of Digital Twins in Healthcare’.
| Section | Item | PRISMA-ScR Checklist item | Reported on page # |
|---|---|---|---|
| Title | |||
| Title | 1 | Identify the report as a scoping review. | 1 |
| Abstract | |||
| Structured summary | 2 | Provide a structured summary that includes (as applicable): background, objectives, eligibility criteria, sources of evidence, charting methods, results, and conclusions that relate to the review questions and objectives. | 1 |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. Explain why the review questions/objectives lend themselves to a scoping review approach. | 2-3 |
| Objectives | 4 | Provide an explicit statement of the questions and objectives being addressed with reference to their key elements (e.g., population or participants, concepts, and context) or other relevant key elements used to conceptualize the review questions and/or objectives. | 3 |
| Methods | |||
| Protocol and registration | 5 | Indicate whether a review protocol exists; state if and where it can be accessed (e.g., a Web address); and if available, provide registration information, including the registration number. | N/A |
| Eligibility criteria | 6 | Specify characteristics of the sources of evidence used as eligibility criteria (e.g., years considered, language, and publication status), and provide a rationale. | 3-5 |
| Information sources* | 7 | Describe all information sources in the search (e.g., databases with dates of coverage and contact with authors to identify additional sources), as well as the date the most recent search was executed. | 4 |
| Search | 8 | Present the full electronic search strategy for at least 1 database, including any limits used, such that it could be repeated. | 15 (Appendix B) |
| Selection of sources of evidence † | 9 | State the process for selecting sources of evidence (i.e., screening and eligibility) included in the scoping review. | 4-5 |
| Data charting process ‡ | 10 | Describe the methods of charting data from the included sources of evidence (e.g., calibrated forms or forms that have been tested by the team before their use, and whether data charting was done independently or in duplicate) and any processes for obtaining and confirming data from investigators. | 5 |
| Data items | 11 | List and define all variables for which data were sought and any assumptions and simplifications made. | 5 (Table 3) |
| Critical appraisal of individual sources of evidence § | 12 | If done, provide a rationale for conducting a critical appraisal of included sources of evidence; describe the methods used and how this information was used in any data synthesis (if appropriate). | N/A |
| Synthesis of results | 13 | Describe the methods of handling and summarizing the data that were charted. | 5 |
| Results | |||
| Selection of sources of evidence | 14 | Give numbers of sources of evidence screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally using a flow diagram. | 5-6 |
| Characteristics of sources of evidence | 15 | For each source of evidence, present characteristics for which data were charted and provide the citations. | 6-8 |
| Critical appraisal within sources of evidence | 16 | If done, present data on critical appraisal of included sources of evidence (see item 12). | N/A |
| Results of individual sources of evidence | 17 | For each included source of evidence, present the relevant data that were charted that relate to the review questions and objectives. | 6-8 (included in same table as characteristics) |
| Synthesis of results | 18 | Summarize and/or present the charting results as they relate to the review questions and objectives. | 6 |
| Discussion | |||
| Summary of evidence | 19 | Summarize the main results (including an overview of concepts, themes, and types of evidence available), link to the review questions and objectives, and consider the relevance to key groups. | 8-9 |
| Limitations | 20 | Discuss the limitations of the scoping review process. | 10-11 |
| Conclusions | 21 | Provide a general interpretation of the results with respect to the review questions and objectives, as well as potential implications and/or next steps. | 11 |
| Funding | |||
| Funding | 22 | Describe sources of funding for the included sources of evidence, as well as sources of funding for the scoping review. Describe the role of the funders of the scoping review. | 11 |
Abbreviations: JBI, Joanna Briggs Institute; PRISMA-ScR, Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews.
Where sources of evidence (see second footnote) are compiled from, such as bibliographic databases, social media platforms and Web sites.
A more inclusive/heterogeneous term used to account for the different types of evidence or data sources (eg, quantitative and/or qualitative research, expert opinion and policy documents) that may be eligible in a scoping review as opposed to only studies. This is not to be confused with information sources (see first footnote).
The frameworks by Arksey and O’Malley 52 and Levac et al 53 and the JBI guidance (4,5) refer to the process of data extraction in a scoping review as data charting.
The process of systematically examining research evidence to assess its validity, results, and relevance before using it to inform a decision. This term is used for items 12 and 19 instead of ‘risk of bias’ (which is more applicable to systematic reviews of interventions) to include and acknowledge the various sources of evidence that may be used in a scoping review (eg, quantitative and/or qualitative research, expert opinion, and policy document).
Source: Tricco et al. 22
Appendix B. Sample search strategy
| Database | Search terms |
|---|---|
| IEEE Explore | (((‘Mesh_Terms’:Capacity management OR patient centric OR outbreak prediction) OR ‘Abstract’:digital twin) AND ((‘Mesh_Terms’:Health management) OR ‘Abstract’:”health” OR ‘care’ OR ‘healthcare’ OR ‘hospital’ OR ‘patient’) AND ((‘Mesh_Terms’:Covid-19) AND ‘Abstract’:”‘2019 novel coronavirus’ OR ‘2019-n-CoV’ OR COVID-19 OR coronavirus OR Covid)) |
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: AK conceived the study topic and designed the review methodology. AK executed and wrote the systematic review supported by MMI, with structural comments from EM and revisions from GI, RJ and AJ.
ORCID iDs: Asiya Khan  https://orcid.org/0000-0003-3620-3048
https://orcid.org/0000-0003-3620-3048
Madison Milne-Ives  https://orcid.org/0000-0001-7628-882X
https://orcid.org/0000-0001-7628-882X
References
- 1. European Commission | Community Research and Development Information Service (CORDIS). Using prediction models to manage the coronavirus outbreak. Published April 1, 2020. Accessed October 20, 2020. https://cordis.europa.eu/article/id/415792-using-prediction-models-to-manage-the-coronavirus-outbreak
- 2. Ahmadi-Assalemi G, Al-Khateeb H, Maple C, et al. Digital Twins for Precision Healthcare. In: Jahankhani H, Kendzierskyj S, Chelvachandran N, Ibarra J, eds. Cyber Defence in the Age of AI, Smart Societies and Augmented Humanity. Springer; 2020;133-158. [Google Scholar]
- 3. Tao F, Zhang M, Liu Y, Nee AY. Digital twin driven prognostics and health management for complex equipment. CIRP Ann. 2018;67:169-172. [Google Scholar]
- 4. Knapp GL, Mukherjee T, Zuback JS, et al. Building blocks for a digital twin of additive manufacturing. Acta Mater. 2017;135:390-399. [Google Scholar]
- 5. Scharl S, Praktiknjo A. The role of a digital industry 4.0 in a renewable energy system. Int J Energy Res. 2019;43:3891-3904. [Google Scholar]
- 6. Ebrahimi A. Challenges of developing a digital twin model of renewable energy generators. Paper presented at: 2019 IEEE 28th International Symposium on Industrial Electronics (ISIE); June 12-14, 2019:1059-1066; Vancouver, BC. IEEE. [Google Scholar]
- 7. Fuller A, Fan Z, Day C, Barlow C. Digital Twin: Enabling Technologies, challenges and Open Research. IEEE Access. 2020;8:108952-108971. [Google Scholar]
- 8. Ford DN, Wolf CM. Smart cities with Digital Twin Systems for Disaster Management. J Manag Eng. 2020;36:04020027. [Google Scholar]
- 9. Björnsson B, Borrebaeck C, Elander N, et al. Digital twins to personalize medicine. Genome Med. 2019;12:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Erol T, Mendi AF, Doğan D. The digital twin revolution in healthcare. Paper presented at: 2020 4th International Symposium on Multidisciplinary Studies and Innovative Technologies (ISMSIT), October 22-24, 2020:1-7; Istanbul, Turkey. doi: 10.1109/ISMSIT50672.2020.9255249. [DOI] [Google Scholar]
- 11. Gkouskou K, Vlastos I, Karkalousos P, Chaniotis D, Sanoudou D, Eliopoulos AG. The “Virtual Digital Twins” concept in precision nutrition. Adv Nutr. 2020;11:1405-1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Croatti A, Gabellini M, Montagna S, Ricci A. On the integration of agents and Digital Twins in healthcare. J Med Syst. 2020;44:161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Barricelli BR, Casiraghi E, Fogli D. A survey on Digital Twin: definitions, characteristics, applications, and design implications. IEEE Access. 2019;7:167653-167671. [Google Scholar]
- 14. Walsh JR, Smith AM, Pouliot Y, et al. Generating Digital Twins with multiple sclerosis using probabilistic neural networks. bioRxiv. Published online April 19, 2020. doi: 10.1101/2020.02.04.934679 [DOI] [Google Scholar]
- 15. Rodríguez-Aguilar R, Marmolejo-Saucedo J-A. Conceptual framework of Digital Health Public Emergency System: digital twins and multiparadigm simulation. EAI Endorsed Trans Pervasive Health Technol. 2020;6:164261. [Google Scholar]
- 16. Karakra A, Fontanili F, Lamine E, Lamothe J. HospiT’Win: A predictive simulation-based digital twin for patients pathways in hospital. Paper presented at: 2019 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI); May 19-22, 2019; Chicago, IL. IEEE. doi: 10.1109/bhi.2019.8834534. [DOI] [Google Scholar]
- 17. Worldometer. COVID-19 coronavirus pandemic. Accessed October 9, 2020. https://www.worldometers.info/coronavirus/
- 18. Ienca M, Vayena E. On the responsible use of digital data to tackle the COVID-19 pandemic. Nat Med. 2020;26:463-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jones D, Snider C, Nassehi A, Yon J, Hicks B. Characterising the Digital Twin: a systematic literature review. CIRP J Manuf Sci Technol. 2020;29:36-52. [Google Scholar]
- 20. Chen Y, Yang O, Sampat C, Bhalode P, Ramachandran R, Ierapetritou M. Digital Twins in pharmaceutical and biopharmaceutical manufacturing: a literature review. Processes. 2020;8:1088. [Google Scholar]
- 21. Digital Twin. GE Digital. Accessed September 12, 2020. https://www.ge.com/digital/applications/digital-twin?utm_source=Google&utm_medium=Paid%20Search&utm_campaign=2020-08-GLOB-DG-HORZ-MULT-Google_SEM_Dig_Twin-Parent_PDSRCH&gclid=CjwKCAjw4_H6BRALEiwAvgfzq2Fc_-qEimpnWrwKZu4oXQKvPNdF1pUZ6vtCkiN7gv89ojQM_WJn9RoCsJQQAvD_BwE
- 22. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467-473. [DOI] [PubMed] [Google Scholar]
- 23. Mohapatra S, Bose S. An appraisal of literature for design and implementation of developing a framework for digital twin and validation through case studies. Health Technol. 2020;10:1229-1237. [Google Scholar]
- 24. Corral-Acero J, Margara F, Marciniak M, et al. The “Digital Twin” to enable the vision of precision cardiology. Eur Heart J. 2020;41:4556-4564. doi: 10.1093/eurheartj/ehaa159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bagaria N, Laamarti F, Badawi HF, Albraikan A, Velazquez RAM El, Saddik A. Health 4.0: Digital Twins for health and well-being. In: El Saddik A, Hossain M, Kantarci B, eds. Connected Health in Smart Cities. Springer; 2020;143-152. [Google Scholar]
- 26. Bruynseels K, Santoni de, Sio F, van den Hoven J. Digital Twins in health care: ethical implications of an emerging engineering paradigm. Front Genet. 2018;9:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rivera LF, Jimenez M, Angara P, Villegas NM, Tamura G, Muller HA. Towards continuous monitoring in personalized healthcare through digital twins. Paper presented at: CASCON ‘19: Proceedings of the 29th Annual International Conference on Computer Science and Software Engineering; November 4-6, 2019:329-335; Toronto, ON. [Google Scholar]
- 28. Liu Y, Zhang L, Yang Y, et al. A novel cloud-based framework for the elderly healthcare services using Digital Twin. IEEE Access. 2019;7:49088-49101. [Google Scholar]
- 29. Laamarti F, Badawi HF, Ding Y, Arafsha F, Hafidh B, El Saddik A. An ISO/IEEE 11073 standardized Digital Twin framework for health and well-being in smart cities. IEEE Access. 2020;8:105950-105961. [Google Scholar]
- 30. Lutze R. Digital Twins in eHealth – : prospects and challenges focussing on information management. Paper presented at: 2019 IEEE International Conference on Engineering, Technology and Innovation (ICE/ITMC); June 17-19, 2019:1-9; Valbonne Sophia-Antipolis, France. IEEE. [Google Scholar]
- 31. Albraikan A. InHarmony: A Digital Twin for emotional well-being, PhD thesis. University of Ottawa; 2019. doi: 10.20381/ruor-23480 [DOI] [Google Scholar]
- 32. Chakshu NK, Carson J, Sazonov I, Nithiarasu P. A semi-active human digital twin model for detecting severity of carotid stenoses from head vibration-A coupled computational mechanics and computer vision method. Int J Numer Methods Biomed Eng. 2019;35:e3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rao DJ, Mane S. Digital Twin approach to Clinical DSS with explainable AI. arXiv. Published online October 22, 2019. Accessed October 9, 2020. http://arxiv.org/abs/1910.13520
- 34. Grosman B, Roy A, Wu D, et al. 1006-P: personalized hybrid closed-loop therapy using a digital twin in patients with Type 1 diabetes: at-home data. Diabetes. 2020;69:1006-P. doi: 10.2337/db20-1006-P [DOI] [Google Scholar]
- 35. Mazumder O, Roy D, Bhattacharya S, Sinha A, Pal A. Synthetic PPG generation from haemodynamic model with baroreflex autoregulation: a digital twin of cardiovascular system. Conf Proc IEEE Eng Med Biol Soc. 2019;2019:5024-5029. [DOI] [PubMed] [Google Scholar]
- 36. Martinez-Velazquez R, Gamez R, Saddik AE. Cardio Twin: a Digital Twin of the human heart running on the edge. Paper presented at: 2019 IEEE International Symposium on Medical Measurements and Applications (MeMeA); İstanbul, Turkey, June 26-28, 2019:1-6. IEEE. [Google Scholar]
- 37. Braun M. Represent me: please! towards an ethics of digital twins in medicine. J Med Ethics. 2021;47:394-400. [DOI] [PubMed] [Google Scholar]
- 38. Braun M. Ethics of digital twins: four challenges. Journal of Medical Ethics. Published Online August 11, 2021. doi: 10.1136/medethics-2021-107675 [DOI] [PubMed] [Google Scholar]
- 39. Krutzinna J. Simulating (some) individuals in a connected world. J Med Ethics. 2021;47:403-404. [DOI] [PubMed] [Google Scholar]
- 40. Mittelstadt B. Near-term ethical challenges of digital twins. J Med Ethics. 2021;47:405-406. [DOI] [PubMed] [Google Scholar]
- 41. Loh J. ‘represent me: please! towards an ethics of digital twins in medicine’: Commentary. J Med Ethics. 2021;47:412. [DOI] [PubMed] [Google Scholar]
- 42. Tretter M. Perspectives on digital twins and the (im)possibilities of control. J Med Ethics. 2021;47:410-411. [DOI] [PubMed] [Google Scholar]
- 43. Tigard DW. Digital twins running amok? Open questions for the ethics of an emerging medical technology. J Med Ethics. 2021;47:407-408. [DOI] [PubMed] [Google Scholar]
- 44. Blumenthal-Barby J. Present and future. J Med Ethics. 2021;47:361-361. [Google Scholar]
- 45. Lupton D. Language matters: the ‘digital twin’ metaphor in health and medicine. J Med Ethics. 2021;47:409. [DOI] [PubMed] [Google Scholar]
- 46. Sun S, Zheng X, Villalba-Díez J, Ordieres-Meré J. Data Handling in Industry 4.0: interoperability based on distributed ledger technology. Sensors. 2020;20:3046. doi: 10.3390/s20113046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. GE Healthcare Command Centers. Digital Twin. Accessed September 27, 2020. https://www.gehccommandcenter.com/digital-twin
- 48. Food D. How does Digital Twin fit into the context of COVID-19? trans.info. Published June 26, 2020. Accessed September 27, 2020. https://trans.info/en/how-does-digital-twin-fit-into-the-context-of-covid-19-189982.
- 49. Thomsen N. The role of digital twins in producing a COVID-19 vaccine. Atos. Published May 18, 2020. Accessed September 27, 2020. https://atos.net/en/blog/the-role-of-digital-twins-in-producing-a-covid-19-vaccine
- 50. Venkatesan P. NICE guideline on long COVID. Lancet Respir Med. 2021;9:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Samidurai A, Das A. Cardiovascular complications associated with COVID-19 and potential therapeutic strategies. Int J Mol Sci. 2020;21:6790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19-32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 53. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implementation Sci. 2010;5. doi: 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]