Abstract
Elder abuse is a serious public health concern that increases the risks of negative health outcomes globally. It is well known that abuse in older adults is associated with depression; however, longitudinal studies investigating the causal relationship between these events are scarce. Because the cause precedes the result over time, the temporal relationships between abuse and depression should be verified from each direction. This longitudinal study, therefore, investigated and clarified whether depression causes or results from elder abuse among older Japanese adults. Two longitudinal analyses were conducted using data derived from the Japan Gerontological Evaluation Study. The data were collected in 2010 and 2013 through a mail survey of 1,737 people (983 females, 754 males) across Japan. Of those who did not experience abuse in 2010, 38 (5.0%) males and 53 (5.4%) females newly experienced abuse in 2013. Among respondents who did not have depressive symptoms in 2010, 60 (8.0%) males and 61 (6.2%) females newly reported depressive symptoms in 2013. After adjusting for demographic factors in Analysis 1, people who experienced abuse were 2.28-fold (95% confidence interval [CI] = 1.68–3.09) more likely to have depressive symptoms three years later than those who were not abused. In Analysis 2, respondents who had mild or severe depression in 2010 were 2.23-fold (95% CI = 1.61–3.10) more likely to have experienced abuse after three years than those who did not have depression. After adjusting for several demographic factors, the results showed that abuse can lead to depression and that depression can be a cause of abuse. Therefore, preventing abuse should be considered from both directions.
Keywords: elder abuse, mental health and violence, predicting domestic violence, domestic violence, preventing violence
Introduction
Elder abuse is one of the serious public health issues that increases the risk of negative health outcomes in low-, middle-, and high-income countries (Abdi et al., 2019; Pillemer et al., 2016; World Health Organization (WHO), 2014; Yon et al., 2017). The many risk factors of elder abuse have been categorized in different levels such as individual, perpetrator, individual–perpetrator relationships, and social or community levels (Johannesen & Logiudice, 2013).
In addition, several studies have revealed strong associations between elder abuse and depressive symptoms (Park, 2018; Pillemer et al., 2016; Roepke-Buehler et al., 2015; Santos et al., 2017). Depressive symptoms are known risk factors for many negative health outcomes (Soysal et al., 2017). For example, depressive symptoms are associated with increased rates of morbidity and suicide (Hawton et al., 2013). Therefore, these symptoms represent an urgent issue that must be resolved. However, although several previous studies described the association between elder abuse and depressive symptoms, their causal relationship has not been clarified; that is, it is unclear whether depression is a cause of elder abuse. To date, research has only investigated the correlation between abuse and depression. Although abuse as a cause of depression has been shown, whether depression leads to abuse remains unknown. While it is conceivable that being abused by someone you trust could cause depression, it is also conceivable that weakness caused by depression or other factors results in increased risk of abuse.
Gaining insight into the cause-and-effect relationship between elder abuse and depressive symptom would assist in elucidating the mechanisms of elder abuse and mental illness, which would be useful from a public health perspective considering the implications for treatment of depression and prevention of abuse in older adults in Japan. Because cause precedes result, the temporal relationship between abuse and depression should be verified. Therefore, in this study, we examined the relationship between elder abuse and depressive symptoms from both directions using longitudinal data from independent older people living in Japan.
Methods
Study Design and Respondents
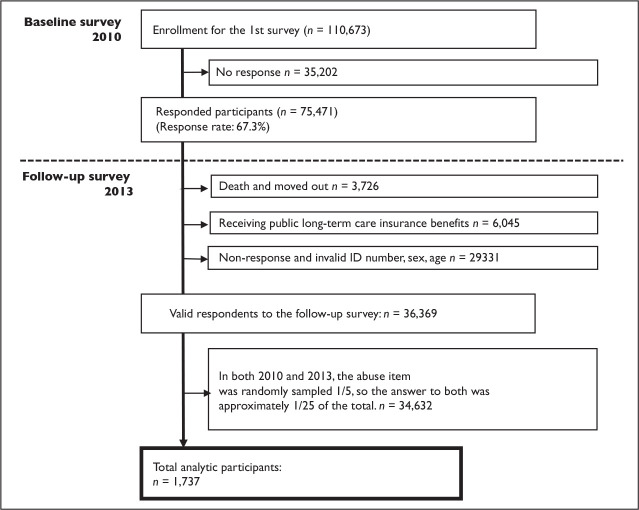
We used a longitudinal data from the Japan Gerontological Evaluation Study (JAGES) collected via mail survey in 2010 and 2013 (Kondo & Rosenberg, 2018). This was a population-based study of independent adults aged 65 years or older who did not have physical or cognitive disabilities and were not eligible for public long-term care insurance benefits. The municipalities included urban, suburban, and rural communities throughout Japan. Although the JAGES respondents were not randomly selected, the data covered a wide range and size of community populations. For the present study, we randomly selected data from one-fifth of the JAGES participants in both 2010 and 2013, totaling 1,737 individuals (Figure 1).
Figure 1.
Flow chart showing participants in this study.
Measurements
Elder abuse.
Elder abuse was measured in three dimensions: physical, psychological, and financial abuses in both 2010 and 2013. Questionnaires were designed by the collective effort of several researchers (including medical doctors, social epidemiology researchers, and social workers). Because there is no official and established definition of abuse, clarifying the criteria for judging the type, frequency, and duration of behavior that constitutes elder abuse is difficult. In this study, questionnaires were designed to identify specific actions that respondents had endured, such as being hit, harm to their self-esteem, and taking of their savings/pension benefits to confirm the presence or absence of abuse. Three questions were asked to identify abuses, and integrated them to create a variable abused or not. For physical abuse, respondents were asked, “In the past year, did you ever experience physical violence from your family, such as being hit, kicked, having objects thrown at you, or being shut in a room?” For psychological abuse, they were asked, “In the past year, did you ever experience an act by your family that harmed your self-esteem, such as verbal abuse, cutting remarks, or being ignored for long periods?” Answer options to both questions were on a four-point scale as follows: 1 = never; 2 = once or twice; 3 = occasionally; and 4 = frequently. Those who answered 1 were considered nonabused, whereas those answering from 2 to 4 were considered abused. Concerning financial abuse, respondents were asked, “Do any of your family members take or use your savings or pension benefits without your consent?” The answer was either yes or no, with the former categorized as abuse and the latter as nonabuse. These three variables were then integrated to create a single variable for abuse (Koga et al., 2020).
Depressive symptoms.
Depression symptoms were also measured in both 2010 and 2013 using the 15-item Geriatric Depression Scale, which defines mild depression as >5 points and severe depression as >10 points (Haseda et al., 2017; Saito et al., 2017).
Covariates.
According to previous research, we analyzed basic demographic information, including sex, age (65–69, 70–74, 75–79, 80–84, or ≥85 years), education level (≤9 or ≥10 years), equivalent income (low [≤1,999,999 JPY (100JPY ≈ 1USD)], middle [2,000,000–3,999,999 JPY], or high [≥4,000,000 JPY]), marital status (married, widowed, divorced, unmarried, or other), and living arrangements (living alone, with family members, or other facility) (Dong et al., 2014; Kondo & Rosenberg, 2018; Sooryanarayana et al., 2017; Wu et al., 2012). To assess activity of daily living (ADL) independence, participants were asked, “Do you regularly receive nursing care or assistance for walking, bathing, and/or using a toilet?” Answers options were on a three-point scale as follows: 1 = no need for nursing care or assistance; 2 = requiring but not receiving nursing care or assistance; 3 = needing and receiving nursing care or assistance.
Statistical Analysis
We conducted a descriptive analysis to summarize the characteristics of the participants. In both 2010 and 2013, the abuse item was randomly sampled 1:5, and thus, the answer to both was approximately 1/25th of the total. Therefore, the final analyzed population of this study was 1,737 older adults. Cramér’s V was calculated to confirm that the selected participants comprised a representative sample of the population before random sampling. Previous studies demonstrated that Cramér’s V denotes weak association at the values of 0.1–0.2, whereas values <0.1 indicate negligible association (Lee, 2016). Since variables such as abuse and depressive symptoms in this analysis contained missing data, we performed multiple imputation. In total, 20 multiple imputed datasets including all measurement variables using the multivariate normal imputation method under a “missing at random” assumption were created, and the estimated parameters combined using Rubin’s combination method. Logistic regression analyses were conducted to investigate the causal relationship between abuse and depressive symptoms. Two analysis were performed to investigate each direction of the relationship. In the first analysis (Analysis 1), to investigate the effect of elder abuse on depressive symptoms, respondents without depressive symptoms in 2010 served as the baseline group (abuse in 2010 vs. no abuse in 2010 for predicting depression in 2013). In the second analysis (Analysis 2), which investigated the effect of depressive symptoms on abuse, respondents who had not been abused served as the baseline group (depression in 2010 vs. no depression in 2010 for predicting abuse in 2013). Stata 16/IC (StataCorp, College Station, TX, USA) was used for all statistical analyses.
Results
The characteristics of the 1,737 study respondents are shown in Table 1. Among all the respondents, 754 (43.4%) were male, whereas 983 (56.6%) were female. The characteristics of the respondents who were excluded via random sampling (n = 34,632) is presented in the Appendix as a table. The random sampling was considered representative as Cramér’s V was >0.1 for all variables (Lee, 2016). More than half of the subjects were ≤74 years old, 844 (48.6%) had an education level of ≥10 years, 671 (38.6%) were low equivalent income, 1,262 (72.7%) were married, and 1,449 (83.4%) were living with family members in 2010. Among those who did not experience abuse in 2010, 38 (5.0%) males, and 53 (5.4%) females experienced new-onset abuse in 2013. In addition, 60 (8.0%) males and 61 (6.2%) females had depressive symptoms in 2013 but not in 2010.
Table 1.
Characteristics of Respondents.
| All, n = 1,737 | Male, n = 754 | Female, n = 983 | |||||
| n | % | n | % | n | % | ||
| Newly depressed in 2013 | 121 | 7.0 | 60 | 8.0 | 61 | 6.2 | |
| Newly abused in 2013 | 93 | 5.4 | 38 | 5.0 | 53 | 5.4 | |
| Elder abuse | |||||||
| No abuse in 2010 | 1,338 | 77.0 | 594 | 78.8 | 744 | 75.7 | |
| Abused in 2010 | 224 | 12.9 | 92 | 12.2 | 132 | 13.4 | |
| Missing | 175 | 10.1 | 68 | 9.0 | 107 | 10.9 | |
| Elder abuse | |||||||
| No abuse in 2013 | 1,435 | 82.6 | 626 | 83.0 | 809 | 82.3 | |
| Abused in 2013 | 186 | 10.7 | 77 | 10.2 | 109 | 11.1 | |
| Missing | 116 | 6.7 | 51 | 6.8 | 65 | 6.6 | |
| Depression (GDS) | |||||||
| Normal in 2010 | 1,150 | 66.2 | 507 | 67.2 | 643 | 65.4 | |
| Mild or severe depressive in 2010 | 348 | 20.0 | 172 | 22.8 | 176 | 17.9 | |
| Missing | 239 | 13.8 | 75 | 9.9 | 164 | 16.7 | |
| Depression (GDS) | |||||||
| Normal in 2013 | 1,069 | 61.5 | 480 | 63.7 | 589 | 59.9 | |
| Mild or severe depressive in 2013 | 332 | 19.1 | 156 | 20.7 | 176 | 17.9 | |
| Missing | 336 | 19.3 | 118 | 15.6 | 218 | 22.2 | |
| Age (years) | |||||||
| 65–69 | 576 | 33.2 | 270 | 35.8 | 306 | 31.1 | |
| 70–74 | 524 | 30.2 | 215 | 28.5 | 309 | 31.4 | |
| 75–79 | 391 | 22.5 | 169 | 22.4 | 222 | 22.6 | |
| 80–84 | 188 | 10.8 | 79 | 10.5 | 109 | 11.1 | |
| ≥85 | 58 | 3.3 | 21 | 2.8 | 37 | 3.8 | |
| Educational level (years) | |||||||
| ≤9 | 843 | 48.5 | 338 | 44.8 | 505 | 51.4 | |
| ≥10 | 844 | 48.6 | 403 | 53.4 | 441 | 44.9 | |
| Missing | 50 | 2.9 | 13 | 1.7 | 37 | 3.8 | |
| Equivalent income (JPY (100JPY ≈ 1USD)) | |||||||
| Low (≤1,999,999) | 671 | 38.6 | 280 | 37.1 | 391 | 39.8 | |
| Middle (2,000,000–3,999,999) | 576 | 33.2 | 293 | 38.9 | 283 | 28.8 | |
| High (≥4,000,000) | 200 | 11.5 | 98 | 13.0 | 102 | 10.4 | |
| Missing | 290 | 16.7 | 83 | 11.0 | 207 | 21.1 | |
| Marital status | |||||||
| Married | 1,262 | 72.7 | 661 | 87.7 | 601 | 61.1 | |
| Widowed | 377 | 21.7 | 60 | 8.0 | 317 | 32.2 | |
| Divorced | 42 | 2.4 | 14 | 1.9 | 28 | 2.8 | |
| Unmarried | 21 | 1.2 | 5 | 0.7 | 16 | 1.6 | |
| Missing | 35 | 2.0 | 14 | 1.9 | 21 | 2.1 | |
| Living arrangement | |||||||
| Living alone | 161 | 9.3 | 40 | 5.3 | 121 | 12.3 | |
| With family members | 1,449 | 83.4 | 645 | 85.5 | 804 | 81.8 | |
| Other facilities | 107 | 6.2 | 58 | 7.7 | 49 | 5.0 | |
| Missing | 20 | 1.2 | 11 | 1.5 | 9 | 0.9 | |
Odds ratios (ORs) with 95% confidence intervals (CIs) for the causal relationship between elder abuse and depressive symptoms among older Japanese adults from Analyses 1 and 2 are shown in Table 2. After adjusting for demographic factors in analysis 1, subjects who experienced abuse were 2.28 (95% CI = 1.68–3.09) times more likely to have depressive symptoms in 2013 than respondents who did not receive abuse. In contrast, those participants were less likely to have depressive symptoms after three years. Those were female (OR = 0.74, 95% CI = 0.58–0.95), had education level ≥10 years (OR = 0.52, 95% CI = 0.41–0.66), middle (OR = 0.62, 95% CI = 0.47–0.80) or high equivalent income (OR = 0.49, 95% CI = 0.32–0.75). Meanwhile, respondents who are 70–74 years old were 1.37 (95% CI = 1.01–1.85) times, 75–79 years old were 1.51 (95% CI = 1.09–2.09) times, 80–84 years old were 1.87 (95% CI = 1.25–2.80) times, and 85 or older were 1.93 (95% CI = 1.01–3.68) times more likely to have mild or severe depression.
Table 2.
Odds Ratios With 95% Confidence Intervals for the Longitudinal Relationship Between Elder Abuse and Depressive Symptoms From Analyses 1 and 2 (n = 1,737).
| Analysis 1: Abuse in 2010 vs. No Abuse in 2010 Predicting Depression in 2013 | Analysis 2: Depression in 2010 vs. No Depression in 2010 Predicting Abuse in 2013 | ||||||||
| Odds Ratio | p | 95% Confidence Interval | Odds Ratio | p | 95% Confidence Interval | ||||
| No abuse in 2010 | 1.00 | Normal in 2010 | 1.00 | ||||||
| Abused in 2010 | 2.28 | <.001 | 1.68 | 3.09 | Mild or severe depressive in 2010 | 2.23 | <.001 | 1.61 | 3.10 |
| Sex | |||||||||
| Male | 1.00 | Male | 1.00 | ||||||
| Female | 0.74 | .017 | 0.58 | 0.95 | Female | 1.40 | .042 | 1.01 | 1.94 |
| Age (years) | |||||||||
| 65–69 | 1.00 | 65–69 | 1.00 | ||||||
| 70–74 | 1.37 | .042 | 1.01 | 1.85 | 70–74 | 1.02 | .916 | 0.71 | 1.47 |
| 75–79 | 1.51 | .013 | 1.09 | 2.09 | 75–79 | 0.79 | .301 | 0.51 | 1.23 |
| 80–84 | 1.87 | .002 | 1.25 | 2.80 | 80–84 | 0.51 | .046 | 0.27 | 0.99 |
| ≥85 | 1.93 | .045 | 1.01 | 3.68 | ≥85 | 0.74 | .535 | 0.28 | 1.94 |
| Educational level | |||||||||
| ≤9 | 1.00 | ≤9 | 1.00 | ||||||
| ≥10 | 0.52 | <.001 | 0.41 | 0.66 | ≥10 | 0.83 | .243 | 0.61 | 1.14 |
| Equivalent income (JPY (100JPY ≈ 1USD)) | |||||||||
| Low (≤1,999,999) | 1.00 | Low (≤1,999,999) | 1.00 | ||||||
| Middle (2,000,000–3,999,999) | 0.62 | <.001 | 0.47 | 0.80 | Middle (2,000,000–3,999,999) | 0.92 | .630 | 0.65 | 1.30 |
| High (≥4,000,000) | 0.49 | <.001 | 0.32 | 0.75 | High (≥4,000,000) | 1.17 | .539 | 0.70 | 1.95 |
| Marital status | |||||||||
| Married | 1.00 | Married | 1.00 | ||||||
| Widowed | 1.27 | .166 | 0.91 | 1.78 | Widowed | 0.62 | .056 | 0.38 | 1.01 |
| Divorced | 1.33 | .454 | 0.63 | 2.78 | Divorced | 1.58 | .326 | 0.64 | 3.91 |
| Unmarried | 2.58 | .058 | 0.97 | 6.85 | Unmarried | 0.51 | .506 | 0.07 | 3.77 |
| Living arrangement | |||||||||
| Living alone | 1.00 | Living alone | |||||||
| With family members | 0.95 | .809 | 0.60 | 1.49 | With family members | 1.95 | .110 | 0.86 | 4.42 |
| Other facilities | 1.41 | .291 | 0.74 | 2.69 | Other facilities | 2.15 | .120 | 0.82 | 5.64 |
In Analysis 2, respondents who had mild or severe depression in 2010 were 2.23 (95% CI = 1.61–3.10) times more likely to have experienced abuse than those who did not have depressive symptoms after three years. Moreover, respondents who were female were 1.40 (95% CI = 1.01–1.94) times more likely to have experienced abuse.
Discussion
This study investigated the relationship between elder abuse and depressive symptoms from each direction using longitudinal data for independent older people living in Japan. The results illustrate that depressive symptoms are both a cause and consequence of abuse. To the best of our knowledge, this is the first study to investigate the relationship between elder abuse and depressive symptoms from each direction using one dataset.
This study shows that respondents who experienced abuse in 2010 were 2.28 times more likely to have depressive symptoms in 2013. Regarding depression attributable to abuse, violence from family members may lead to anxiety about the future and contribute to the onset of depressive symptoms because of feelings of despair. When older adults have no one with whom to share their abusive experiences, depressive symptoms might develop. Several previous studies have found that social support might be a preventive factor for abuse (Chokkanathan, 2017; Dong & Simon, 2008; Koga et al., 2020). Thus, a lack of expected support from family members or a lack of support itself could also lead to depressive symptoms. Moreover, depressive symptoms may be an intermediate factor between abuse and suicide. Considering a previous study found that abuse is associated with suicide, suicide may occur after depressive symptoms in older adults (Hawton et al., 2013; Luo & Waite, 2011). It is possible that older adults may be in an environment where they are not able to seek help from those around them and develop depressive symptoms because of abuse. In Asia, due to cultural influences, older adults who have been abused are often reluctant to disclose abuse in order to protect the honor and dignity of their families (Moon et al., 2002). This loneliness may increase the risk of developing depressive symptoms.
Moreover, our finding indicates that respondents who have depressive symptoms were 2.23 times more likely to experience abuse three years later. Respondents who already had depressive symptoms may be prone to perceive any aggressive action as abuse, which could lead to exaggeration. For example, previous studies have reported that frailness or functional dependence due to depression can cause people to misinterpret certain situations as abuse (Curcio et al., 2019; Dong, 2017; Soysal et al., 2017). Another study discussed the possibility of abuse associated with chronic pain (Yunus et al., 2018). Based on these findings, depression, which results in emotional and/or physical limitations, may make people more vulnerable to abuse. In addition, people with depression or physical frailty are more easily attacked than their healthy counterparts. This phenomenon is not unique to Japanese or Asian cultures, but is thought to be common.
Abuse typically occurs as part of an ongoing downward spiral (Roepke-Buehler et al., 2015). Thus, subjects could experience abuse and have depressive symptoms almost contemporaneously, and it may be difficult to identify a causal relationship. Some studies have revealed that children tend to be abusers of their parents (Kulakçı Altıntas¸ & Korkmaz Aslan, 2019; Melchiorre et al., 2014; Yan et al., 2015;). Families have long histories, and the relationship between family members might vary over time. To exit this vicious cycle, preventive strategies for abuse and depressive symptoms should be considered from both directions. It has been suggested that social capital may have a preventive and ameliorative effect on both elder abuse and depressive symptoms. Social capital is comprised of the norms, networks, and associations that facilitate actions in the community (Putnam, 1993). For instance, those who have social support have a lower risk of experiencing elder abuse and depressive symptoms (Johannesen & Logiudice, 2013; Sasaki et al., 2019). In addition, another study has shown a relationship between elder abuse and social cohesion (Koga et al., 2020). Because our study confirmed the bidirectional relationship between elder abuse and depressive symptoms, the increased positive aspect of social capital may lead to a break from the downward spiral of abuse and depression, as the causes of abuse and consequences of depression can be efficiently approached.
Several limitations of this study should be mentioned. First, the questionnaires to identify abuse were not validated. Therefore, validation should be performed in future studies. Second, we excluded respondents who were dependent in terms of ADLs and those receiving public long-term care insurance benefits; therefore, the study sample was not nationally representative. Some studies have demonstrated that ADL-dependent respondents are more likely to be abused (Johannesen & Logiudice, 2013). Therefore, the actual incidence of abuse might have been underestimated in this study. Third, to verify the causal relationship, data analysis considering the time until the occurrence of an outcome and Cox proportional hazard analysis are the main methods. Randomized control trials (RCTs) are also recommended to investigate the causal relationship. However, because there was no time or RCT data until the abuse occurred in this study, we considered that time considered using the available data at both time points. Finally, respondents with depressive symptoms may have exaggerated their report of abuse.
Conclusion
The two longitudinal analyses of this study show that depression is both a cause and consequence of elder abuse, illustrating a bidirectional relationship. Prevention strategies from both directions are necessary to avoid a downward spiral of abuse and depression.
Acknowledgment
This study used data from JAGES, conducted by the Nihon Fukushi University Center for Well-Being and Society. We are extremely grateful to all study participants for the use of their personal data. We would like to express our deepest gratitude to everyone who participated and cooperated in the surveys.
Author Biographies
Chie Koga, PhD, is a researcher in the Center for Preventive Medical Sciences, Chiba University, Japan. Her research focuses on preventing elder abuse through environmental factors such as social capital. She is a member of JAGES groups which collaborate with various municipalities in Japan. Through JAGES, she evaluates environmental factors and support policy making of each community.
Taishi Tsuji, PhD, is an assistant professor at the Faculty of Health and Sport Sciences, University of Tsukuba. He is a member of JAGES groups which collaborate with various municipalities in Japan. Through JAGES, he is engaged in social epidemiology and exercise epidemiology.
Masamichi Hanazato, PhD, is an associate professor in the Center for Preventive Medical Sciences, Chiba University, Japan. He is a member of JAGES groups which collaborate with various municipalities in Japan. Through JAGES, he works in analysis of environment and health.
Norimichi Suzuki, PhD, is an associate professor in the Center for Preventive Medical Sciences, Chiba University, Japan. His focus is public health and social medicine from the viewpoint of urban planning. He is a member of JAGES groups which collaborate with various municipalities in Japan. Through JAGES, he works in analysis of social epidemiology and the built environment.
Katsunori Kondo, MD, PhD, is a professor of social epidemiology and health policy at the Center for Preventive Medical Sciences and the Graduate School of Medicine at Chiba University. He is also Head of the Department of Gerontological Evaluation at the Center for Gerontology and Social Science, National Center for Geriatrics and Gerontology.
Appendix.
Comparison Between Analyzed Participants and Others.
| 1/25 (Analyzed Participants) | 24/25 (Before Random Sampling) | |||||
| n = 1,737 | n = 34,632 | Cramer’s V | ||||
| n | % | n | % | |||
| Sex | ||||||
| Male | 754 | 43.4 | 15,894 | 45.9 | ||
| Female | 983 | 56.6 | 18,738 | 54.1 | 0.0106 | |
| Age (years) | ||||||
| 65–69 | 576 | 33.2 | 11,379 | 32.9 | ||
| 70–74 | 524 | 30.2 | 10,435 | 30.1 | ||
| 75–79 | 391 | 22.5 | 7,550 | 21.8 | ||
| 80–84 | 188 | 10.8 | 3,897 | 11.3 | ||
| ≥85 | 58 | 3.3 | 1,371 | 4.0 | 0.0080 | |
| Educational level (years) | ||||||
| ≤9 | 843 | 48.5 | 17,525 | 50.6 | ||
| ≥10 | 844 | 48.6 | 16,403 | 47.4 | ||
| Missing | 50 | 2.9 | 194 | 0.6 | 0.0078 | |
| Equivalent income (JPY (100JPY ≈ 1USD)) | ||||||
| Low (≤1,999,999) | 671 | 38.6 | 14,365 | 41.5 | ||
| Middle (2,000,000–3,999,999) | 576 | 33.2 | 11,310 | 32.7 | ||
| High (≥4,000,000) | 200 | 11.5 | 3,127 | 9.0 | ||
| Missing | 290 | 16.7 | 5,830 | 16.8 | 0.0219 | |
| Marital status | ||||||
| Married | 1,262 | 72.7 | 25,256 | 72.9 | ||
| Widowed | 377 | 21.7 | 7,175 | 20.7 | ||
| Divorced | 42 | 2.4 | 938 | 2.7 | ||
| Unmarried | 21 | 1.2 | 500 | 1.4 | ||
| Missing | 35 | 2.0 | 763 | 2.2 | 0.0078 | |
| Living arrangement | ||||||
| Living alone | 161 | 9.3 | 3,370 | 9.7 | ||
| With family members | 1,449 | 83.4 | 28,836 | 83.3 | ||
| Other facilities | 107 | 6.2 | 1,939 | 5.6 | ||
| Missing | 20 | 1.2 | 487 | 1.4 | 0.0060 | |
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This study was supported by the Ministry of Education, Culture, Sports, Science and Technology-Japan supported Program for the Strategic Research Foundation at Private Universities (20092013), JSPS (Japan Society for the Promotion of Science) KAKENHI (grant Nos. JP22330172, JP22390400, JP23243070, JP23590786, JP23790710, JP24390469, JP24530698, JP24683018, JP25253052, JP25870573, JP25870881, 19K04785 and 20K13721), Health Labor Science Research Grants (H22-Choju-Shitei-008, H24-Junkanki [Seishu]-Ippan-007, H24Chikyukibo-Ippan-009, H24-Cho- ju-Wakate-009, H25-Kenki-Wakate-015, H26-Irryo-Shitei003 [Fukkou], H25-Choju-Ippan-003, and H26-Choju-Ippan-006) from the Ministry of Health, Labor and Welfare, Japan, the Research and Development Grants for Longevity Science from AMED (Japan Agency for Medical Research and Development), a grant from the National Center for Geriatrics and Gerontology, Japan (24-17, 24-23), and a JST-OPERA program grant (JPMJOP1831).
Statement of Ethics: The JAGES protocol was reviewed and approved by the Ethics Committee on Research of Human. Ethical approval for the study was obtained from the Ethics Committee at Nihon Fukushi University, Japan (approval No. 10-05) and the Ethics Committee at the Chiba University Faculty of Medicine, Japan (approval No. 2493).
ORCID iDs: Chie Koga  https://orcid.org/0000-0002-1971-4308
https://orcid.org/0000-0002-1971-4308
Taishi Tsuji  https://orcid.org/0000-0002-8408-6619
https://orcid.org/0000-0002-8408-6619
References
- Abdi A., Tarjoman A., & Borji M. (2019). Prevalence of elder abuse in Iran: A Systematic review and meta-analysis. Asian Journal of Psychiatry , 39, 120–127. 10.1016/j.ajp.2018.12.005 [DOI] [PubMed] [Google Scholar]
- Chokkanathan S. (2017). Stressors social support and elder mistreatment. Aging and Mental Health , 21(2), 125–132. 10.1080/13607863.2015.1081151 [DOI] [PubMed] [Google Scholar]
- Curcio C. L., Villamizar C. P., Jiménez A., & Gómez F. (2019). Abuse in Colombian elderly and its association with socioeconomic conditions and functionality. Colombia Medica , 50(2), 77–88. 10.25100/cm.v50i2.4013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X. (2017). The association between physical function and elder mistreatment among community-dwelling Chinese older adults in the Greater Chicago area. Journals of Gerontology: Series A, Biological Sciences and Medical Sciences , 72(suppl_1), S90–S94. 10.1093/gerona/glw238 [DOI] [PubMed] [Google Scholar]
- Dong X., Chen R., Fulmer T., & Simon M. A. (2014). Prevalence and correlates of elder mistreatment in a community-dwelling population of U.S. Chinese older adults. Journal of Aging and Health , 26(7), 1209–1224. 10.1177/0898264314531617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X., & Simon M. A. (2008). Is greater social support a protective factor against elder mistreatment? Gerontology , 54(6), 381–388. 10.1159/000143228 [DOI] [PubMed] [Google Scholar]
- Haseda M., Kondo N., Ashida T., Tani Y., Takagi D., & Kondo K. (2017). Community social capital, built environment, and income-based inequality in depressive symptoms among older people in Japan: An ecological study from the JAGES project. Journal of Epidemiology , 28(3), 108–116. 10.2188/jea.JE20160216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K., Comabella Casañas i, C. Haw K. Saunders K. (2013). Risk factors for suicide in individuals with depression: A systematic review, Journal of Affective Disorders , 147(1–3), pp. 17–28. 10.1016/j.jad.2013.01.004 [DOI] [PubMed] [Google Scholar]
- Johannesen M., & Logiudice D. (2013). Elder abuse: A systematic review of risk factors in community-dwelling elders. Age and Ageing , 42(3), 292–298. 10.1093/ageing/afs195 [DOI] [PubMed] [Google Scholar]
- Koga C., Hanazato M., Tsuji T., Suzuki N., & Kondo K. (2020). Elder abuse and social capital in older adults: The Japan Gerontological Evaluation Study, Gerontology , 66(2), 149–159. 10.1159/000502544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo K., & Rosenberg M. (2018). Advancing universal health coverage through knowledge translation for healthy ageing: Lessons learnt from the Japan Gerontological Evaluation Study . World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/279010/9789241514569-eng.pdf?sequence=1&isAllowed=y. [Google Scholar]
- Kulakçı Altıntas H., & Korkmaz Aslan G. (2020). Prevalence of elder abuse among community-dwelling older adults in Turkey and its associated factors. Psychogeriatrics: The Official Journal of the Japanese Psychogeriatric Society , 20(1), 3–10. 10.1111/psyg.12446 [DOI] [PubMed] [Google Scholar]
- Lee D. K. (2016). Alternatives to P value: Confidence interval and effect size. Korean Journal of Anesthesiology , 69(6), 555–562. 10.4097/kjae.2016.69.6.555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y., & Waite L. J. (2011). Mistreatment and psychological well-being among older adults: Exploring the role of psychosocial resources and deficits. Journals of Gerontology: Series B, Psychological Sciences and Social Sciences , 66(2), 217–229. 10.1093/geronb/gbq096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchiorre M. G., Penhale B., & Lamura G. (2014). Understanding elder abuse in Italy: Perception and prevalence, types and risk factors from a review of the literature. Educational Gerontology , 40(12), 909–931. 10.1080/03601277.2014.912839 [DOI] [Google Scholar]
- Moon A., Tomita S. K., & Jung-Kamei S. (2002). Elder mistreatment among four Asian American groups: An exploratory study on tolerance, victim blaming and attitudes toward third-party intervention. Journal of Gerontological Social Work , 36, 1–2. [Google Scholar]
- Park J.-I. (2018). Relationship between emotional abuse and depression among community-dwelling older adults in Korea. Yonsei Medical Journal , 59(5), 693–697. 10.3349/ymj.2018.59.5.693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pillemer K., Burnes D., Riffin C., & Lachs M. S. (2016. December). Elder abuse: Global situation, risk factors, and prevention strategies. The Gerontologist , 56(Supplement 2), S194–S205. 10.1093/geront/gnw004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam R. D. (1993). Making democracy work: Civic traditions in modern Italy . Princeton University Press. [Google Scholar]
- Roepke-Buehler S. K., Simon M., & Dong X. (2015). Association between depressive symptoms, multiple dimensions of depression, and elder abuse: A cross- sectional, population- based analysis of older adults in urban Chicago. Journal of Aging and Health , 27(6), 1003–1025. 10.1177/0898264315571106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saito M., Kondo N., Aida J., Kawachi I., Koyama S., Ojima T., & Kondo K. (2017). Development of an instrument for community-level health related social capital among Japanese older people: The JAGES project. Journal of Epidemiology , 27(5), 221–227. 10.1016/j.je.2016.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos A. J., Nunes B., Kislaya I., Gil A. P., & Ribeiro O. (2017). Exploring the correlates to depression in elder abuse victims: Abusive experience or individual characteristics. Journal of Interpersonal Violence . 10.1177/0886260517732346 [DOI] [PubMed] [Google Scholar]
- Sasaki Y., Aida J., Tsuji T., Koyama S., Tsuboya T., Saito T., Kondo K., & Kawachi I. (2019). Pre-disaster social support is protective for onset of post-disaster depression: Prospective study from the Great East Japan Earthquake & tsunami. Scientific Reports , 9(1), 19427. 10.1038/s41598-019-55953-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sooryanarayana R., Choo W. Y., Hairi N. N., Chinna K., Hairi F., Ali Mohamad, Z. Nor Ahmad, S. Abdul Razak, I. Abdul Aziz, S. Ramli, R. Mohamad, R. Mohammad, Z. L., Peramalah D. Ahmad N. A., Aris T., & Bulgiba A. (2017). The prevalence and correlates of elder abuse and neglect in a rural community of Negeri Sembilan state: Baseline findings from the Malaysian Elder Mistreatment Project (Maestro)—A population-based survey. BMJ Open , 7(8), e017025. 10.1136/bmjopen-2017-017025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soysal P., Veronese N., Thompson T., Kahl K. G., Fernandes B. S., Prina A. M., Solmi M., Schofield P., Koyanagi A., Tseng P.-T., Lin P.-Y., Chu C.-S., Cosco T. D., Cesari M., Carvalho A. F., & Stubbs B. (2017). Relationship between depression and frailty in older adults: A systematic review and meta-analysis. Ageing Research Reviews , 36, 78–87. 10.1016/j.arr.2017.03.005 [DOI] [PubMed] [Google Scholar]
- (WHO). World Health Organization. (2014). Global status report on violence prevention 2014 (pp. 1–274). https://www.who.int/violence_injury_prevention/violence/status_report/2014/en/ [Google Scholar]
- Wu L., Chen. H., Hu Y., Xiang H., Yu X., Zhang T., Cao Z., & Wang Y. (2012). Prevalence and associated factors of elder mistreatment in a rural community in people’s Republic of China: A cross-sectional study. PLOS ONE , 7(3), e33857. 10.1371/journal.pone.0033857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan E., Chan K. L., & Tiwari A. (2015). A systematic review of prevalence and risk factors for elder abuse in Asia. Trauma, Violence and Abuse , 16(2), 199–219. 10.1177/1524838014555033 [DOI] [PubMed] [Google Scholar]
- Yon Y., Mikton C. R., Gassoumis Z. D., & Wilber K. H. (2017). Elder abuse prevalence in community settings: A systematic review and meta-analysis. The Lancet , 5(2), e147–e156. 10.1016/S2214-109X(17)30006-2 [DOI] [PubMed] [Google Scholar]
- Yunus R. M., Hairi N. N., Choo W. Y., Tan M. P., Hairi F., Sooryanarayana R., Ismail N., Kandiben S., Peramalah D., Ali Z. M., Ahmad S. N., Razak I. A., Othman S., Mydin F. H. M., Chinna K., & Bulgiba A. (2018). Elder abuse and chronic pain: Cross-sectional and longitudinal results from the preventing elder abuse and neglect initiative, Journal of the American Geriatrics Society , 66(6), 1165–1171. 10.1111/jgs.15370 [DOI] [PubMed] [Google Scholar]