Abstract
A health check-up is one of the best ways to prevent diseases and maintain health by screening for risk factors and diagnosing diseases early. As the burden of illness shifts from infectious to chronic diseases, the importance of health check-ups is emphasized. Korean health authorities began the National Health Screening Programs (NHSPs) for public servants and private school staff in 1980. The NHSP is composed of the National Cancer Screening Programs (NCSPs) and general health checkups. NCSPs, started in 1999, included screenings for stomach, liver, colorectal, breast, and uterine cervical cancers, and they may have contributed to the improved cancer survival rate from 42.9% in 1993–1995 to 77.5% in 2013–2017 in Korea. General health check-ups included lifestyle questionnaires, anthropometric measurements; blood pressure measurement; visual acuity test; hearing test; laboratory tests including fasting glucose, lipid profile, liver function tests, creatinine, and urinalysis; and, chest radiography. Additionally, bone density, cognitive function, and depression were assessed. Testing for non-communicable diseases has improved the control rates of chronic diseases such as hypertension and diabetes mellitus. Favorable changes in the risk factors for cardio-cerebrovascular diseases may lead to a decline in age-standardized mortality and heart disease over several decades. However, many areas of the programs need to be improved. NHSPs should be designed on the basis of individual health conditions, medical needs, and scientific evidence. Greater opportunities to receive NHSPs should be provided to socioeconomically vulnerable individuals. In addition, stricter quality control of NHSPs is required. Follow-up management after the NHSPs should be systematized. In conclusion, NHSPs have contributed to the improvement of public health; however, several aspects of these programs must be addressed.
Keywords: Public Health, Mass Screening, Diagnosis, Neoplasms, Noncommunicable Diseases
INTRODUCTION
With improvements in hygiene and nutritional status, human life expectancy has increased. In accordance with these changes in the burden of illness from infectious to non-communicable diseases (NCDs) such as malignant neoplasms, metabolic diseases, and cardiovascular diseases [1-3], the priorities of health policies have shifted to prevention and health promotion. Lifestyle modifications can prevent the development of NCDs as they are closely related to lifestyle and health behaviors. In addition, regular surveillance for and early detection of NCDs through health screening are important and cost-effective from a public health perspective [4-6].
The Korean government enacted “The Basic Health Check-up Act” in 2008 [7]. The purpose of this act was to promote public health and welfare by determining the rights and obligations of citizens and the responsibilities of the government, and stipulating basic matters concerning the planning and implementation of the National Health Screening Program (NHSP). In addition, the Korean government established and announced the third comprehensive Korean NHSP plan to improve the quality of the NHSP, enhance equity, and reduce the burden of disease by 2021. The efforts of the government and medical communities have resulted in the expansion of the screening infrastructure, improvements in the control rates of chronic diseases, and better cancer survival rates [8-10]. The NHSP includes the National Cancer Screening Program (NCSP) to screen for cancer; a general health check-up including anthropometric measurements, chest radiography, oral health assessments, and other tests for variables such as lipid profiles, osteoporosis, and cognitive function; and, health check-ups for infants and adolescents. In this review, we focused on the Korean NHSPs and general health check-ups for adults and described the history, types, and trends in outcome indicators.
HISTORY OF THE NATIONAL HEALTH SCREENING PROGRAM
Although screening for tuberculosis and parasites was initiated in 1950 according to the third comprehensive Korean NHSP plan, health check-ups for public servants and private school staff that were initiated in 1980 are considered the beginning of the NHSP [8]. In 1995, the NHSP was extended to include workplace health insurance subscribers and local subscribers. The NCSPs were implemented for Medicaid beneficiaries in 1999 and expanded to the bottom 50% based on the national health insurance premiums in 2005. The Basic Health Checkup Act was promulgated in 2008. The first comprehensive Korean national health check-up plan was established, and the out-of-pocket fees paid by examinees were lowered to 10% in 2010. The NCSP for uterine cervical cancers began for female Medicaid beneficiaries aged 20 years or older in 2015, which was expanded to non-Medicaid beneficiaries in 2016. The liver cancer screening cycle in the NCSP was changed to twice a year in 2016. In 2017, a hepatitis C virus screening pilot project was initiated. Out-of-pocket expenses for the NCSP for colorectal cancer were exempted in 2018. A lung cancer screening program was implemented in 2019. In 2021, the third comprehensive Korean NHSP plan was released [8]. The main goal was to increase the reliability of the NHSPs and improve the usability of the results.
EPIDEMIOLOGY OF THE CAUSES OF DEATH
Cancer is the leading cause of death in Korea [11], followed by cardiocerebrovascular diseases (CCVDs). The top 10 causes of death in 2020 (based on mortality rate per 100,000 individuals) in Korea were as follows, in descending order: malignant neoplasms (160.1), heart diseases (63.0), pneumonia (43.3), cerebrovascular diseases (42.6), suicide (25.7), diabetes mellitus (16.5), Alzheimer’s disease (14.7), liver diseases (13.6), hypertensive diseases (11.9), and sepsis (11.9) [12]. Among these, six were NCDs. Therefore, to reduce the burden of NCDs, it is important to manage the related risk factors to allow for early detection. The Korean National Health Insurance Service (NHIS) provided screening for early detection and diagnosis of common cancers and cardiovascular risk factors.
NATIONAL CANCER SCREENING PROGRAMS
In 2017, 232,255 cases of malignant neoplasms were newly diagnosed and 78,863 individuals with cancer died. The age-standardized cancer incidence and death per 100,000 persons were 254.4 and 76.6, respectively [10]. Although the overall cancer incidence and mortality rates have decreased since 2011 and 2002, respectively, the cancer burden remains high. NCSPs has been used for the early detection of five common cancers since 1999. Cancer screening is one of the most effective methods for the early diagnosis and complete remission of almost all types of cancers, provided there are cost-effective and acceptable screening tests. Therefore, the Korean NHIS provided free NCSPs of the stomach for all individuals aged ≥40 years; liver, high-risk patients aged ≥40 years, such as those infected with hepatitis B or C virus or with liver cirrhosis; colorectum, individuals aged ≥50 years; breast, women aged ≥40 years; and, uterine cervix, women 20 years or older. Since 2019, lung cancer screening has been additionally implemented for high-risk groups aged 54–74 years [13]. The high-risk group for lung cancer included individuals who had a history of 30 pack-years or more, but had not smoked cigarettes for less than 15 years. The screening methods were as follows: stomach cancer, esophagogastroduodenoscopy or upper gastroenterography, biennially; liver cancer, ultrasound and serum α-fetoprotein, every 6 months; colorectal cancer, fecal occult blood test, annually; breast cancer, mammography, biennially; uterine cervical cancer, pap smear test, biennially; and, lung cancer, low-dose lung computed tomography, biennially [13]. However, apart from the current NCSP, the National Cancer Center developed and published recommendations for the seven major cancers including thyroid cancer in 2016 (Table 1) [14]. This vigilant surveillance of common cancers might partly contribute to the improvement of the 5-year relative survival rates at the time of diagnosis, which had increased from 42.9% in 1993–1995 to 77.5% in 2013–2017 (Table 2) [10].
Table 1.
Recommendations to screen seven types of cancers
| Cancer type | Screening target | Examination cycle | Primary screening methods | Secondary screening methods |
|---|---|---|---|---|
| Stomach | Individuals aged 40–74 years | Every 2 years | Esophagogastroduodenoscopy | Gastroenterography |
| Liver | Carriers of hepatitis B or C virus aged 40 years or older | Every 6 months | Alpha-fetoprotein+liver ultrasound | |
| Individuals diagnosed with liver cirrhosis at any age | ||||
| Colorectum | Individuals aged 45–80 years | Every 1–2 years | Fecal occult blood test | Colonoscopy |
| Breast | Women aged 40–69 years | Every 2 years | Mammography | |
| Uterine cervix | Women aged 20 years or older | Every 3 years | Pap smear (or liquid-based cytology) | Pap smear+human papillomavirus test |
| Lung | High-risk group who smoked 30 pack-years or more aged 55–74 years | Every year | Low-dose computed tomography | |
| Thyroid | Not recommended as a routine screening test |
Table 2.
Trends in the 5-year relative survival rates (unit, %) at the time of diagnosis between 1993 and 2017 in Korea
| Site | Sex | Year |
|||||
|---|---|---|---|---|---|---|---|
| 1993–1995 | 1996–2000 | 2001–2005 | 2006–2010 | 2011–2015 | 2013–2017 | ||
| All | Both | 42.9 | 45.1 | 54.1 | 65.5 | 70.7 | 70.4 |
| Men | 33.2 | 36.3 | 45.6 | 56.8 | 63.1 | 63.5 | |
| Women | 55.1 | 56.4 | 64.3 | 74.4 | 78.4 | 77.5 | |
| Stomach | Both | 43.9 | 47.3 | 58.0 | 68.4 | 75.9 | 76.5 |
| Men | 43.9 | 47.6 | 58.7 | 69.1 | 76.8 | 77.5 | |
| Women | 43.7 | 46.8 | 56.6 | 67.0 | 74.0 | 74.6 | |
| Colorectum | Both | 56.2 | 58.8 | 66.9 | 73.9 | 76.2 | 75.0 |
| Men | 56.6 | 59.8 | 68.8 | 75.8 | 77.9 | 76.6 | |
| Women | 55.7 | 57.7 | 64.4 | 71.1 | 73.7 | 72.6 | |
| Liver* | Both | 11.7 | 14.1 | 20.5 | 28.2 | 34.3 | 35.6 |
| Men | 10.8 | 13.8 | 20.4 | 28.2 | 34.8 | 36.4 | |
| Women | 15.0 | 15.1 | 20.9 | 28.3 | 32.7 | 33.2 | |
| Breast | Both | 79.2 | 83.6 | 88.6 | 91.2 | 92.7 | 93.2 |
| Men | 77.1 | 84.3 | 87.5 | 89.9 | 89.4 | 94.7 | |
| Women | 79.2 | 83.6 | 88.7 | 91.2 | 92.7 | 93.2 | |
| Uterine cervix | Both | 78.3 | 80.3 | 81.5 | 80.7 | 80.2 | 80.2 |
| Men | - | - | - | - | - | - | |
| Women | 78.3 | 80.3 | 81.5 | 80.7 | 80.2 | 80.2 | |
| Lung† | Both | 12.5 | 13.6 | 16.5 | 20.2 | 27.5 | 30.2 |
| Men | 11.6 | 12.4 | 15.3 | 18.0 | 23.2 | 25.2 | |
| Women | 15.8 | 17.5 | 20.1 | 26.0 | 37.2 | 41.5 | |
Liver cancer includes the liver and intrahepatic bile duct.
Lung cancer includes the lung and bronchus.
The cancer screening rate increased from 12.7% in 2002 to 49.2% in 2020 (Table 3). The individual screening rates of the six types of cancer were as follows: stomach cancer, 12.7% in 2002 to 55.4% in 2020; colorectal cancer, 10.5% in 2004 to 36.9% in 2020; liver cancer, 15.8% in 2003 to 68.4% in 2020; breast cancer, 14.1 % in 2002 to 58.5% in 2020; uterine cervical cancer, 15.4% in 2002 to 54.8% in 2020; and, lung cancer, 33.1% in 2019 to 36.6% in 2020 [15]. Initially, the NCSP began in 1999 for Medicaid beneficiaries. Subsequently, the examinee candidates were expanded to the bottom 20% in 2002 and the bottom 50% in 2005 according to the national health insurance premium. As the number of examinee candidates increased, the number of NCSP examinees continued to increase until 2019 but decreased due to coronavirus disease 2019 in 2020. The cancer screening rates steadily increased; they were the highest in 2019 and then fell in 2020.
Table 3.
The cancer screening rates (unit, %) according to cancer type from 2002 to 2020
| Site | Year |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | |
| All | 12.7 | 14.4 | 14.8 | 20.2 | 21.4 | 25.2 | 29.0 | 32.5 | 35.7 | 41.2 | 36.7 | 37.4 | 48.4 | 50.1 | 51.5 | 52.7 | 55.0 | 55.6 | 49.2 |
| Stomach | 11.4 | 13.6 | 15.7 | 20.0 | 21.8 | 25.4 | 29.2 | 34.3 | 37.3 | 44.6 | 43.9 | 43.7 | 55.0 | 56.9 | 59.0 | 59.9 | 61.9 | 62.2 | 55.4 |
| Colorectum | - | - | 10.5 | 15.4 | 15.8 | 18.1 | 21.2 | 26.2 | 30.7 | 33.9 | 25.7 | 27.0 | 34.9 | 36.8 | 38.6 | 40.2 | 43.0 | 43.0 | 36.9 |
| Liver* | - | 15.8 | 23.9 | 26.0 | 26.0 | 28.6 | 32.7 | 38.5 | 42.5 | 46.6 | 40.6 | 44.2 | 59.6 | 60.3 | 66.4 | 68.7 | 71.9 | 73.1 | 68.4 |
| Breast | 14.1 | 16.7 | 18.6 | 24.1 | 26.4 | 30.2 | 34.9 | 40.0 | 43.5 | 49.6 | 49.2 | 48.6 | 60.4 | 61.8 | 63.8 | 64.5 | 65.8 | 66.0 | 58.5 |
| Uterine cervix | 15.4 | 10.6 | 9.9 | 21.3 | 22.1 | 28.0 | 31.9 | 29.7 | 32.3 | 37.4 | 36.3 | 38.5 | 52.1 | 53.9 | 52.8 | 54.6 | 57.3 | 59.8 | 54.8 |
| Lung† | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 33.1 | 36.6 | ||
Liver cancer includes the liver and intrahepatic bile duct.
Lung cancer includes the lung and bronchus.
However, cancer screening rates may differ according to socioeconomic status in Korea. Kim and Kang [16] reported that the overall cancer screening rate within the last 2 years was 56.6% in men and 66.0% in women based on the Korea National Health and Nutrition Examination Survey. Individuals of higher socioeconomic status were more likely to participate in cancer screening programs, including opportunistic cancer screenings and NCSPs, compared to individuals of lower socioeconomic status: 46.7%, 54.4%, 57.6%, and 63.8% in men and 56.4%, 64.7%, 68.8%, and 74.0% in women from the lowest to highest quartile of monthly household income, respectively, participated in cancer screening programs.
GENERAL HEALTH CHECK-UP
General health check-ups were provided biennially for health insurance subscribers aged ≥40 years by the Korean NHIS [17]. However, this check-up program was provided every other year for local subscribers and their dependents aged over 20 years, all job subscribers regardless of age, and Medicaid beneficiaries aged between 19 and 64 years. General health check-ups include lifestyle questionnaires (such as alcohol intake, smoking status, and physical activity), anthropometric measurements (such as height, body weight, and waist circumference), blood pressure measurement, visual acuity and hearing tests, laboratory tests (including hemoglobin, fasting glucose, aspartate transaminase, alanine transaminase, gamma-glutamyl transpeptidase, lipid profile, and creatinine), urinalysis, chest radiography, and oral examinations. In addition, screening for dyslipidemia began at age 24 years in men and 30 years in women. Screening for hepatitis B virus (HBV) was performed at the age of 40 years, except for individuals with immunity against HBV and HBV carriers. Bone densitometry was conducted in women aged 54–66 years. Cognitive function was screened biennially for the elderly population aged ≥66 years. Screening for depression was performed in individuals aged 20, 30, 40, 60, and 70 years.
General health check-up screening rates increased from 65.3% in 2008 to 78.5% in 2017 but slightly decreased to 76.9% in 2018 and 74.1% in 2019 (Figure 1) [18,19]. General health check-up screening rates were calculated by dividing the number of examinees by the number of examinee candidates.
Figure. 1.
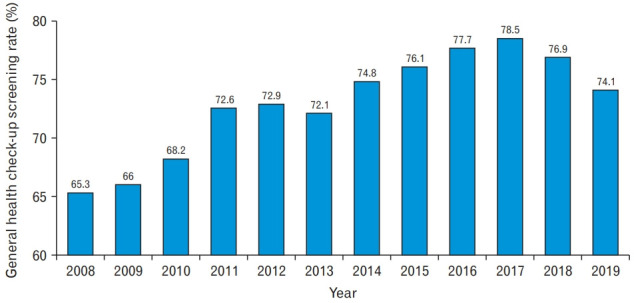
The general health check-up screening rate.
Active screening and treatment of NCDs, such as hypertension and diabetes, may affect their prevalence and control rates [20-22]. The agestandardized prevalence of hypertension and the mean blood pressure decreased [21]. In addition, the control rate of diabetes mellitus increased, even though its prevalence increased [23]. In particular, the prevalence of hypercholesterolemia drastically increased, but the control rates simultaneously improved [9]. Favorable changes in risk factors, such as diabetes mellitus, hypertension, and dyslipidemia, have led to favorable CCVD outcomes. Kim [24] demonstrated that the age-standardized mortalities of cerebrovascular and heart diseases have declined over the last several decades.
DISCUSSIONS OF THE KOREAN NATIONAL HEALTH SCREENING PROGRAMS
A report from the Korean National Assembly Budget Office entitled “Evaluation of the National Health Screening Program” was published in 2021 [19]. This report discussed several issues regarding the current NHSP. First, check-up programs should be designed based on individual health conditions, medical needs, and scientific evidence. According to the National Health Screening Statistical Yearbook (2019) published in 2021, more than 20% of the NHSP examinees had known hypertension, diabetes mellitus, dyslipidemia, or pulmonary tuberculosis and were currently being treated [25]. Providing NHSPs for these patients does not conform to the principle of health check-ups, whose purpose is early detection and treatment of undiagnosed diseases. Providing patients with diagnosed hypertension, diabetes mellitus, dyslipidemia, or tuberculosis the same check-up programs is not costeffective. From a financial perspective, health insurance finances are unnecessary. For patients who are diagnosed with and treated for hypertension or diabetes mellitus, it is better to test for complications or provide vouchers for other tests. Second, blind spots for NHSPs should be managed. People of a higher socioeconomic status were associated with a higher rate of participation in general health check-ups and NCSPs [16,26]. People with lower monthly insurance premiums were less likely to participate in the NHSPs. Therefore, improvements are needed so that NHSPs can be more easily provided to those of more vulnerable socioeconomic statuses. In addition, budgeting is also important. The Korean Ministry of Health and Welfare and local governments combine financial resources to provide NHSPs for Medicaid beneficiaries aged ≤64 years, whereas local governments should independently prepare budgets and operate NHSPs for Medicaid beneficiaries aged ≥65 years. For these reasons, only a small number of local governments (64 of 228 local governments) are conducting NHSPs for Medicaid beneficiaries aged 65 years or older. Therefore, the system and laws should be supplemented to provide active and thorough NHSPs to these individuals. Third, stricter quality control is required for NHSPs. The Basic Health Check-up Act sets the application qualifications and standards of personnel, facilities, and equipment for designation as medical institutions for NHSPs to prevent poor health examinations and maintain the quality of the NHSPs [7]. Standards for personnel, facilities, equipment, etc. of the associated medical institutions operating the NHSPs stipulate that, in the case of personnel standards, there should be one doctor for every 25 examinees per day on average per year [27]. The designation of the medical institution can be cancelled if it does not meet the personnel standards. However, many medical institutions designated to perform NHSPs provide several opportunistic health check-up programs along with NHSPs for examinees who undergo NHSPs. These additional opportunistic health check-up programs increase the load of medical doctors in charge of NHSPs and reduce their quality. The Ministry of Health and Welfare should identify information on opportunistic health check-up programs that affect the quality of NHSPs and set appropriate personnel standards based on this information. In addition, unnecessary costs related to opportunistic health check-ups and complications, such as radiation hazards, can occur because opportunistic health check-up programs are being conducted when their necessity or adequacy has not been confirmed. The cost of opportunistic health check-ups by individuals was estimated at 827 billion Korean won in 2019 [28]. Thus, overdiagnosis is an important issue. Overdiagnosis is defined as the identification of abnormal findings that are not harmful, do not progress or progress too slowly to cause symptoms or harm during the individual’s remaining lifetime, or they resolve spontaneously [29]. Overdiagnosis frequently leads to unnecessary medical tests or expenditures that can be harmful. Fourth, follow-up management should be systematized after NHSPs. Compared with the screening rate, the rate of receiving a confirmed test or one leading to treatment was not high. The reason for conducting NHSPs is to detect, treat, and manage health problems at an early stage. Therefore, through follow-up management, such as confirmative tests for individuals with abnormal screening tests and promotion of consultation on the results of the NHSPs, more active management can help prevent disease progression or complications. In addition, an integrative management system must be prepared that can obtain the results of health check-ups performed in the private sector. These integrated management models can maximize the effect of health checkups, regardless of their origin in the national or private sector.
CONCLUSION
NHSPs screened for unhealthy lifestyles and provide adequate early diagnosis free of charge or at minimal cost for various diseases such as cancers and NCDs including hypertension, diabetes mellitus, and dyslipidemia. During the last several decades, screening rates have increased, and public awareness has improved. Through vigilant surveillance and early detection systems, a stage shift from advanced to early disease can improve disease outcomes. However, there are many areas for improvement in NHSPs. Appropriate modifications to address these shortcomings can improve public health and increase the costeffectiveness of NHSPs.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (grant no., 2021R1G1A1006485).
REFERENCES
- 1.Yach D, Hawkes C, Gould CL, Hofman KJ. The global burden of chronic diseases: overcoming impediments to prevention and control. JAMA. 2004;291:2616–22. doi: 10.1001/jama.291.21.2616. [DOI] [PubMed] [Google Scholar]
- 2.Global Burden of Disease Cancer Collaboration. Fitzmaurice C, Abate D, Abbasi N, Abbastabar H, Abd-Allah F, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2019;5:1749–68. doi: 10.1001/jamaoncol.2019.2996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2019 Stroke Collaborators Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20:795–820. doi: 10.1016/S1474-4422(21)00252-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee HY, Lee SW, Kim HC, Ihm SH, Park SH, Kim TH. Cost-effectiveness analysis of hypertension screening in the Korea National Health Screening Program. Korean Circ J. 2021;51:610–22. doi: 10.4070/kcj.2021.0051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Go DS, Kim SH, Park J, Ryu DR, Lee HJ, Jo MW. Cost-utility analysis of the National Health Screening Program for chronic kidney disease in Korea. Nephrology (Carlton) 2019;24:56–64. doi: 10.1111/nep.13203. [DOI] [PubMed] [Google Scholar]
- 6.Cho E, Kang MH, Choi KS, Suh M, Jun JK, Park EC. Cost-effectiveness outcomes of the national gastric cancer screening program in South Korea. Asian Pac J Cancer Prev. 2013;14:2533–40. doi: 10.7314/apjcp.2013.14.5.2533. [DOI] [PubMed] [Google Scholar]
- 7.Sejong: The Korean Law Information Center; 2020. The Basic Health Check-up Act, Law No. 17472 (Aug 11, 2020) [Internet] [cited 2022 Mar 30]. Available from: https://law.go.kr/%EB%B2%95%EB%A0%B9/%EA%B1%B4%EA%B0%95%EA%B2%80%EC%A7%84%EA%B8%B0%EB%B3%B8%EB%B2%95. [Google Scholar]
- 8.Ministry of Health and Welfare . Sejong: Ministry of Health and Welfare; 2021. The third comprehensive Korean national health screening program plan [Internet] [cited 2022 Mar 30]. Available from: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=366024&page=1. [Google Scholar]
- 9.Kim Y, Nho SJ, Woo G, Kim H, Park S, Kim Y, et al. Trends in the prevalence and management of major metabolic risk factors for chronic disease over 20 years: findings from the 1998-2018 Korea National Health and Nutrition Examination Survey. Epidemiol Health. 2021;43:e2021028. doi: 10.4178/epih.e2021028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hong S, Won YJ, Park YR, Jung KW, Kong HJ, Lee ES, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2017. Cancer Res Treat. 2020;52:335–50. doi: 10.4143/crt.2020.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Statistics Korea . Daejeon: Statistics Korea; Annual report on the causes of death statistics [Internet] c2022 [cited 2022 Mar 30]. Available from: http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1012. [Google Scholar]
- 12.Statistics Korea . Daejeon: Statistics Korea; Korean report of cause of death in 2020 [Internet] c2022 [cited 2022 Mar 30]. Available from: https://kostat.go.kr/portal/korea/kor_nw/1/1/index.board?bmode=read&aSeq=403046. [Google Scholar]
- 13.National Cancer Center . Goyang: National Cancer Center; 2021. Korean National Cancer Screening Programs [Internet] [cited 2022 Mar 30]. Available from: https://www.ncc.re.kr/main.ncc?uri=manage01_4. [Google Scholar]
- 14.National Cancer Information Center . Goyang: National Cancer Information Center; 2015. Recommendations for the seven major cancers [Internet] [cited 2022 Mar 30]. Available from: https://www.cancer.go.kr/lay1/bbs/S1T261C264/B/36/list.do. [Google Scholar]
- 15.Statistics Korea . Daejeon: Statistics Korea; Cancer screening rates in national cancer screening programs [Internet] c2022 [cited 2022 Mar 30]. Available from: https://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1440. [Google Scholar]
- 16.Kim JY, Kang HT. Association between socioeconomic status and cancer screening in Koreans over 40 years in age based on the 2010-2012 Korean National Health and Nutrition Examination Survey. Korean J Fam Med. 2016;37:287–92. doi: 10.4082/kjfm.2016.37.5.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Health Insurance Service . Wonju: National Health Insurance Service; Introduction of Korean national health screening programs [Internet] [date unknown] [cited 2022 Mar 30]. Available from: https://www.nhis.or.kr/nhis/policy/wbhada19600m01.do. [Google Scholar]
- 18.Korea Health Promotion Institute . Seoul: Korea Health Promotion Institute; General health check-up screening rates [Internet] [date unknown] [cited 2022 Mar 30]. Available from: https://www.khealth.or.kr/hpl/hplIdx/idxPopup.do?pop=Y&idx_ix=89. [Google Scholar]
- 19.National Assembly Budget Office . Seoul: National Assembly Budget Office; 2021. Evaluation of the national health screening program [Internet] [cited 2022 Mar 30]. Available from: https://www.nabo.go.kr/Sub/01Report/01_02_Board.jsp. [Google Scholar]
- 20.Kim KI, Ji E, Choi JY, Kim SW, Ahn S, Kim CH. Ten-year trends of hypertension treatment and control rate in Korea. Sci Rep. 2021;11:6966. doi: 10.1038/s41598-021-86199-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim TJ, Lee JW, Kang HT, Cho MC, Lim HJ, Kim JY, et al. Trends in blood pressure and prevalence of hypertension in Korean adults based on the 1998-2014 KNHANES. Yonsei Med J. 2018;59:356–65. doi: 10.3349/ymj.2018.59.3.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee JW, Kang HT, Lim HJ, Park B. Trends in diabetes prevalence among Korean adults based on Korean National Health and Nutrition Examination Surveys III-VI. Diabetes Res Clin Pract. 2018;138:57–65. doi: 10.1016/j.diabres.2018.01.013. [DOI] [PubMed] [Google Scholar]
- 23.Shin JY. Trends in the prevalence and management of diabetes in Korea: 2007-2017. Epidemiol Health. 2019;41:e2019029. doi: 10.4178/epih.e2019029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim HC. Epidemiology of cardiovascular disease and its risk factors in Korea. Glob Health Med. 2021;3:134–41. doi: 10.35772/ghm.2021.01008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Health Insurance Service . Wonju: National Health Insurance Service; 2019. Guide for National Health Screening Statistical Yearbook (2019) [Intenet] [cited 2022 Mar 30]. Available from: https://www.nhis.or.kr/nhis/together/wbhaec07000m01.do?mode=view&articleNo=10806637&article.offset=0&articleLimit=10. [Google Scholar]
- 26.Shin HY, Kang HT, Lee JW, Lim HJ. The association between socioeconomic status and adherence to health check-up in Korean adults, based on the 2010-2012 Korean National Health and Nutrition Examination Survey. Korean J Fam Med. 2018;39:114–21. doi: 10.4082/kjfm.2018.39.2.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sejong: The Korean Law Information Center; 2007. Standards for Personnel, Facilities, Equipment, etc. of the Medical Institutions Operating the National Health Screening Programs, Ministry of Health and Welfare No. 131 (Dec 27, 2007) [cited 2022 Mar 30]. Available from: https://www.law.go.kr/LSW/admRulInfoP.do?admRulSeq=6401#AJAX. [Google Scholar]
- 28.Statistics Korea . Daejeon: Statistics Korea; 2021. National health account statistical information report [Internet] [cited 2022 Mar 30]. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=117&tblId=DT_11768_2009NN3&vw_cd=MT_ZTITLE&list_id=F_18&seqNo=&lang_mode=ko&language=kor&obj_var_id=&itm_id=&conn_path=MT_ZTITLE. [Google Scholar]
- 29.Brodersen J, Schwartz LM, Woloshin S. Overdiagnosis: how cancer screening can turn indolent pathology into illness. APMIS. 2014;122:683–9. doi: 10.1111/apm.12278. [DOI] [PubMed] [Google Scholar]


