Abstract
Background:
Endotracheal tube (ETT) is an important risk factor for the development of Ventilator-associated pneumonia (VAP), as it acts as a reservoir for infectious microorganisms and bypasses the host’s defenses. One of the preventive measures for VAP is endotracheal tube composition. It has been reported that biofilm formation is reduced by using ETTs coated with pure silver or silver compounds. However, noble metal-alloy ETTs have not been adequately studied.
Aims:
To evaluate the efficacy of noble metal alloy ETT (coated Bactiguard Infection Protection ETTs) in preventing VAP compared to standard non-coated ETTs in patients requiring ≥ 48 hours of mechanical ventilation and presenting for coma due to drug intoxication.
Study Design:
Randomized controlled study.
Methods:
Participants were randomized using sealed envelopes with a concealed 1:1 allocation to either the intervention group or the control group. The intervention group used a noble metal–alloy ETT, while the control group received standard ETT. The primary outcomes were the incidence of VAP (per ventilated patients) and the duration of mechanical ventilation.
Results:
Initially, a total of 188 patients were assessed for eligibility, and the final allocation group consisted of 180 patients, who were subsequently randomized into the intervention group (n = 97) and control group (n = 83). The incidence of VAP in the intervention and control groups was 27.83% and 43.16% (P = 0.03), and the VAP ratio per 1000 ventilation days was 51.26/1000 and 83.38/1000 (P = 0.01), respectively. The mean durations of mechanical ventilation were 3.2 ± 0.78 in the intervention group and 5.03 ± 1.88 in the control group (P = 0.22). There was no statistically significant difference between groups in terms of mortality and duration of hospital stay.
Conclusion:
Noble metal-alloy ETT reduces the incidence of VAP, ventilation days, and ICU stay for patients in mechanical ventilation.
INTRODUCTION
Ventilator-associated pneumonia (VAP), a type of nosocomial pneumonia, is the most common infectious complication among patients admitted in the intensive care unit (ICU).1 The United States Centers for Disease Control and Prevention defined VAP as pneumonia occurring 48 h after the initiation of mechanical ventilation, and VAP is associated with increased rates of multidrug-resistant infections, increased antibiotic use, prolonged mechanical ventilation time, and extended ICU and hospital stay.2 Great interest is focused on preventive measures, especially with endotracheal tube (ETT) composition in correlation with VAP incidence. Micro-aspiration is one of the mechanisms involved in bacterial colonization of the lower respiratory tract, and it refers to the migration of bacteria from upper secretions that accumulate above the ETT cuff to the lower parts of bronchial ramifications. In the meantime, biofilm formation provides a network between bacteria and tracheal secretions, facilitating the exposure of the bronchial tree to various pathogens.3 ETT is involved in VAP pathogenesis as a major risk factor because it acts as a reservoir for infected microorganisms and it bypasses the host’s defenses4, including altering the ability to clear secretions adequately. Our interventions involved the prevention of micro-aspiration (through aspiration techniques, cuff pressure, and ETT cuff material) and biofilm formation. Thus far, three randomized controlled trials (RTCs) have reported a significant reduction in biofilm formation using ETTs coated with pure silver or silver compound.5,6,7 However, only a few studies have used noble metal–alloy ETTs.
Objectives
The primary aim of this study was to assess the efficacy of a noble metal–alloy ETT (coated Bactiguard Infection Protection [BIP] ETTs) for VAP prevention in comparison with standard noncoated ETTs in patients who require mechanical ventilation for ≥48 h and admitted for drug poisoning-induced coma. The secondary aim was to evaluate whether noble metal-coated ETTs are effective concerning the duration of intubation, length of hospital and ICU stay, and time to VAP onset.
MATERIALS AND METHODS
Study Design
This RCT was conducted in the Intensive Care Toxicology Unit of Hospital Bucharest Hospital and included adult patients admitted for drug poisoning-induced coma and expected to require orotracheal intubation for > 48 h. The procedures were performed after the informed consent form was signed by the patients or their legal representatives. The study was approved by the Australian New Zealand Clinical Trials Registry and registered on www.anzctr.org.au (ACTRN12618002055280). The Hospital Committee of Ethics approved this trial.
Intervention and Controls
All patients who gave consent were then randomized using concealed envelopes with an allocation of 1:1 to either the intervention group or the control group. The intervention group used a noble metal–alloy ETT, while the control group received standard ETT. The internal and external surfaces of the device (coated BIP ETT) had Bactiguard® coating (Sweden), which consists of a noble metal–alloy, namely, silver, palladium, and gold. This technology is known to reduce bacterial adhesion in vitro. The proposed ETT is a sterile, single-use, 100% latex-free material, with a beveled tip, Murphy eye, and high-volume low-pressure cuff that will reduce the risk of damage to the trachea and ensure safe usage, without the need for a subglottic drainage secretion system.8
In the control group, patients received standard uncoated ETTs made of polyvinyl chloride that is normally used for intubation. As regards oral care practices, our interventions include daily removal of dental plaques along the gingival margins and the proximal tooth surface. We used the modified Beck oral assessment scale and mucosa–plaque scores to evaluate the severity of dental plaques. The mouth was cleaned with chlorhexidine gluconate 1% gel at an interval of at least 2 h between gel application and tooth brushing with standard toothpaste. Moreover, local VAP prevention techniques included noninvasive positive pressure ventilation, intermittent sedation, weaning trials, avoidance of reintubation, early tracheostomy, head elevation, use of antimicrobial ETTs, and oral decontamination.
Data Collection
The inclusion criteria were as follows: adults aged ≥ 19 years, requiring endotracheal intubation ≥ 48 h, coma due to drug poisoning, and follow-up duration of 18 months. Sample size calculation was not made. The exclusion criteria were as follows: history of a neurologic and psychiatric pathology, transmissible blood disease, and cancer and use of immune-modulating therapies. For all patients, age, sex, weight, major comorbidities, and primary reasons for hospital admission were recorded. Electronic medical records were used to calculate the incidence of VAP, defined by clinical, radiological, and laboratory criteria.9 Follow-up was stopped when one of these events occurred: extubation, tracheostomy, or death. Patients needing reintubation were considered in the initial protocol. We did not assess the ETTs when removed because of bacterial contamination, biofilm accumulation, and qualitative assessment of the inner lumen.
Primary Outcomes
The primary outcomes were the incidence of VAP (per ventilated patients) and the duration of mechanical ventilation. VAP assessment was performed 5 days after the initiation of mechanical ventilation. We routinely obtained bacterial and fungal isolates from each removed ETT and identified and quantified the colonies using tracheal aspirates obtained aseptically with a closed suction device. Resistance testing to major antibiotics was performed.
The diagnosis of VAP was confirmed by imaging and should fulfill at least two of the following criteria: temperature > 38 °C or < 35 °C, white blood cells > 10,000/µL or < 4,000/µL, presence of purulent secretion in the airways, significant quantitative culture of respiratory secretions using tracheal aspirates (> 106 CFU/mL), presence of rales or dullness, and >10% decrease in the arterial oxygen partial pressure.10,11 In this study, we used the definition and diagnosis according to the CDC criteria published in January 2021.
Secondary Outcomes
The secondary outcomes included the length of ICU stay, length of hospital stay, and mortality rate.
Statistical Analysis
The analysis was conducted with SPSS. The normal distribution of variables was assessed using the Shapiro-Wilk test. Data are reported as either mean ± standard deviation (SD) or median [interquartile range, IQR]. Differences between the two groups were analyzed with the Student t-test or the Mann-Whitney U test based on the normality of the distribution. Ratios and proportions between groups were compared using the chi-square test. P-value < 0.05 was considered significant.
RESULTS
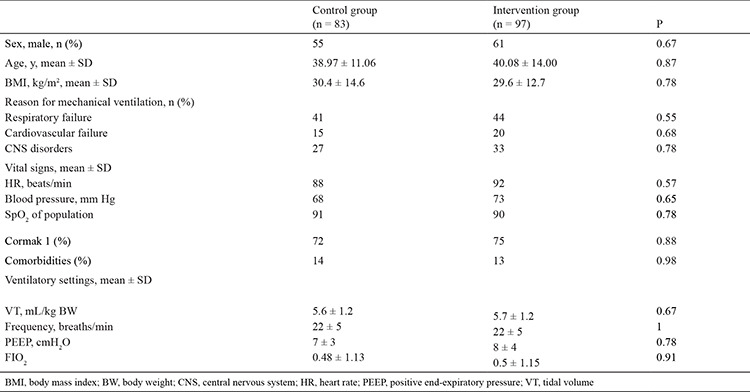
Initially, a total of 188 patients were assessed for eligibility, and the final allocation group consisted of 180 patients, who were then randomized into the intervention group (n = 97) and the control group (n = 8) (in accordance with the available material). We did not include the place and time of intubation because we wanted to evaluate the intrinsic capacity of the device to prevent VAP. Only 30 patients were intubated in the ICU, and we do not have information on the place of intubation in the remaining patients, as some of them were being transferred from all over the country. The mean ages were 38.97 ± 11.06 and 40.08 ± 14.00 years in the control and intervention groups, respectively (P = 0.87). The baseline parameters of the study population are shown in Table 1, and no significant differences were recorded initially between the two groups. The median GCS scores were 7 and 8 in the intervention and control groups, respectively. Moreover, no difference was found in the difficulty of intubation assessed using the Cormack–Lehane classification score.
Table 1. Characterization of the Study Population at Baseline.
The overall incidence of VAP was 35.49% according to clinical scoring and bacteriological finding. In this study, 35 (43.16%) patients in the control group and 27 (27.83%) in the intervention group developed VAP. The VAP rate in the control group was 83.38 for 1000 days of ventilation; in the intervention group, it was 51.26 for 1000 ventilation days. Further investigation revealed that VAP was reduced by 67% when the noble metal–alloy ETT was used, and this value was significant. Moreover, 14 patients had more than one intubation attempt (8 in the intervention group and 6 in the control group), and two patients from each group were reintubated twice. The mean durations of mechanical ventilation were 5.03 ± 1.88 in the control group and 3.2 ± 0.78 in the intervention group (P = 0.22).
The median ICU stay decreased from 10.14 ± 2.16 days in the control group and 7.11 ± 2.88 days in the intervention group (Table 2) (P = 0.03). No significant differences were found between the groups regarding tracheostomy or initiation of enteral feeds. The characteristics of the pathogens identified are presented in Table 3.
Table 2. Primary and Secondary Outcomes of the Study.
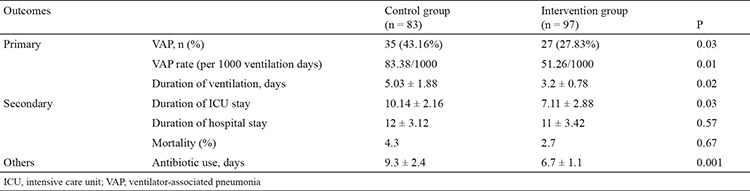
Table 3. Pathogens Detected as Sources of VAP.
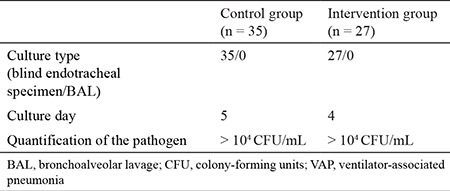
Hospital stay was not influenced by the intervention, as the control group was hospitalized for 12 ± 3.12 days, and the intervention group was discharged after 11 ± 3.42 days (P = 0.57). Gram-negative organisms were the most frequently isolated species from the ETT secretions. One patient had methicillin-resistant Staphylococcus aureus. The mean durations of antibiotic therapy were 9.3 ± 2.4 and 6.7 ± 1.1 days in the control and intervention groups, respectively (P = 0.001). The mortality rates were 2.7% and 4.3% in the intervention and control groups, respectively. Although the mortality rate was low in the intervention group, the difference was not significant (P = 0.67).
DISCUSSION
The prevention of VAP has become the priority of ICUs worldwide. To our knowledge, this single-center RCT was the first in our country to address VAP incidence using coated BIP ETTs in patients admitted for drug poisoning. This is also the first study evaluating the association of noble metal–alloy ETTs with VAP occurrence. Although the exact cause of VAP is not well established, ETT is considered the main risk factor of VAP because of damage against local defense mechanisms, such as the cough reflex and mucociliary clearance, leading to tracheal colonization and pneumonia.12
Some measures are employed in ICUs to prevent VAP, such as placing the patient in a semirecumbent position, elevating the head to 30°–45°13, initiating subglottic secretion drainage, or ETT cuff modifications.12 Other interventions focused directly on ETT innovation, such as using different cuff materials and shapes to prevent microchannel formation.14 Among other interventions, silver-coated ETTs and noble metal–alloy-coated ETTs are seen as viable alternatives, after showing success in the urology area15, because silver is well-known to provide a wide range of antimicrobial properties, from preventing bacterial adherence in vitro to blocking biofilm formation in animal models.16,17 We did not use silver ETTs for comparison because several studies have already evaluated the efficiency of silver ion technology.
In this study, the overall incidence of VAP was 35.49%, which is a little higher than the rates reported in developing countries, with 15–30%.18 This study also examined the usefulness of noble metal–alloy ETTs in terms of VAP prevention in comparison with conventional ETTs. Among the 97 patients in the intervention group, 27 were considered to have VAP. A reduction in the VAP rate of approximately 67% was noted when the noble metal–alloy ETT was used (P Fisher = 0.02; P difference = 0.01). This finding is consistent with the result of a randomized, large-cohort, multicenter study that reported a reduction in VAP rate, through microbiological studies, in patients intubated with the noble metal–alloy-coated ETT, in comparison with a standard ETT.19
Our study showed a reduction in ICU stay and ventilation days when noble metal–alloy-coated ETT was used. Moreover, microbial analysis of the intestinal tract or any other symbiotic administration was considered.20
A previous study reported a shorter ICU stay in patients using PU-cuffed tubes than in patients who used conventional cuffed tubes (17–11 days).21 Previous studies have suggested that silver-coated ETTs were associated with reduced mortality in patients who developed VAP; however, studies using noble metal–alloy ETTs are limited.
As regards the limitations of this study, it was impossible to analyze biofilm accumulation. This study was performed in a single center providing poisoning-specific services, so the results may not be similar for all ICU patients and units. The incidence of VAP varies in surgical and non-surgical cases and depends on the type of surgery. Moreover, this study did not analyze early and late VAP onset separately.
Thus far, single intervention strategies were not as successful as multiple interventions in VAP prevention or rate reduction. Therefore, next-generation research should improve ETT characteristics to help decrease VAP rates in clinical practice. Multicenter studies are warranted to obtain valuable information about the capabilities of noble metal–alloy ETTs in improving clinical outcomes of patients with intubation.
Footnotes
Ethics Committee Approval: The study was approved by the Australian New Zealand Clinical Trials Registry and registered on www.anzctr.org.au (ACTRN12618002055280). The Hospital Committee of Ethics approved this trial.
Informed Consent: The procedures were performed after the informed consent form was signed by the patients or their legal representatives.
Author Contributions: Concept: R.C.T., I.F.T.; Design: R.C.T., I.F.T.; Analysis or Interpretation: I.F.T.; Supervision: R.A.M.; Literature Search: R.C.T., I.F.T., R.A.M., C.C.; Writing: I.F.T.
Data Sharing Statement: Data available on request from the authors. The data that support the findings of this study are available from the corresponding author.
Conflict of Interest: No conflict of interest was declared by the authors.
Funding: The authors declared that this study received no financial support.
References
- 1.Koenig SM, Truwit JD. Ventilator-associated pneumonia: diagnosis, treatment, and prevention. Clinical Microbiol Rev. 2006;19:637–657. doi: 10.1128/CMR.00051-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buczko W. Ventilator-associated pneumonia among elderly Medicare beneficiaries in long-term care hospitals. Health Care Financ Rev. 2009;31:1–10. [PMC free article] [PubMed] [Google Scholar]
- 3.Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165:867–903. doi: 10.1164/ajrccm.165.7.2105078. [DOI] [PubMed] [Google Scholar]
- 4.Fernandez JF, Levine SM, Restrepo MI. Technologic advances in endotracheal tubes for prevention of ventilator-associated pneumonia. Chest. 2012;142:231–238. doi: 10.1378/chest.11-2420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koerner RJ. Contribution of endotracheal tubes to the pathogenesis of ventilatorassociated pneumonia. J Hosp Infect. 1997;35:83–89. doi: 10.1016/s0195-6701(97)90096-7. [DOI] [PubMed] [Google Scholar]
- 6.Kollef MH, Afessa B, Anzueto A, et al. Silver-coated endotracheal tubes and incidence of ventilator-associated pneumonia: the NASCENT randomized trial. JAMA. 2008;300:805–813. doi: 10.1001/jama.300.7.805. [DOI] [PubMed] [Google Scholar]
- 7.Rello J, Kollef M, Diaz E, et al. Reduced burden of bacterial airway colonization with a novel silver-coated endotracheal tube in a randomized multiple-center feasibility study. Crit Care Med. 2006;34:2766–2772. doi: 10.1097/01.CCM.0000242154.49632.B0. [DOI] [PubMed] [Google Scholar]
- 8.Berra L, Kolobow T, Laquerriere P, et al. Internally coated endotracheal tubes with silver sulfadiazine in polyurethane to prevent bacterial colonization: a clinical trial. Intensive Care Med. 2008;34:1030–1037. doi: 10.1007/s00134-008-1100-1. [DOI] [PubMed] [Google Scholar]
- 9.Björling G, Johansson D, Bergström L, et al. Tolerability and performance of BIP endotracheal tubes with noble metal alloy coating--a randomized clinical evaluation study. BMC Anesthesiol. 2015;15:174. doi: 10.1186/s12871-015-0156-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lorente L, Lecuona M, Jim´enez A, Mora ML, Sierra A. Influence of an endotracheal tube with polyurethane cuff and subglottic secretion drainage on pneumonia. Am J Respir Crit Care Med. 2007;176:1079–1083. doi: 10.1164/rccm.200705-761OC. [DOI] [PubMed] [Google Scholar]
- 11.Camargo LFA, De Marco FV, Barbas CSV, et al. Ventilator associated pneumonia: comparison between quantitative and qualitative cultures of tracheal aspirates. Crit Care. 2004;8:R422–430. doi: 10.1186/cc2965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mietto C, Pinciroli R, Patel N, Berra L. Ventilator associated pneumonia: Evolving definitions and preventive strategies. Respir Care. 2013;58:990–1007. doi: 10.4187/respcare.02380. [DOI] [PubMed] [Google Scholar]
- 13.Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–332. doi: 10.1016/j.ajic.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Rouzé A, Martin-Loeches I, Nseir S. Improved endotracheal tubes for prevention of ventilator-associated pneumonia: Better than silver and gold? Respir Care. 2019;64:108–109. doi: 10.4187/respcare.06698. [DOI] [PubMed] [Google Scholar]
- 15.Bologna RA, Tu LM, Polansky M, Fraimow HD, Gordon DA, Whitmore KE. Hydrogel/silver ion-coated urinary catheter reduces nosocomial urinary tract infection rates in intensive care unit patients: a multicenter study. Urology. 1999;54:982–987. doi: 10.1016/s0090-4295(99)00318-0. [DOI] [PubMed] [Google Scholar]
- 16.Berra L, De Marchi L, Yu ZX, Laquerriere P, Baccarelli A, Kolobow T. Endotracheal tubes coated with antiseptics decrease bacterial colonization of the ventilator circuits, lungs, and endotracheal tube. Anesthesiology. 2004;100:1446–1456. doi: 10.1097/00000542-200406000-00017. [DOI] [PubMed] [Google Scholar]
- 17.Berra L, Kolobow T, Laquerriere P, et al. Internally coated endotracheal tubes with silver sulfadiazine in polyurethane to prevent bacterial colonization: a clinical trial. Intensive Care Med. 2008;34:1030–1037. doi: 10.1007/s00134-008-1100-1. [DOI] [PubMed] [Google Scholar]
- 18.Gadani H, Vyas A, Kar AK. A study of ventilator-associated pneumonia: Incidence, outcome, risk factors and measures to be taken for prevention. Indian J Anaesth. 2010;54:535–540. doi: 10.4103/0019-5049.72643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kollef MH, Afessa B, Anzueto A, et al. NASCENT Investigation Group Silver-coated endotracheal tubes and incidence of ventilator-associated pneumonia: the NASCENT randomized trial. JAMA. 2008;300:805–813. doi: 10.1001/jama.300.7.805. [DOI] [PubMed] [Google Scholar]
- 20.Becheanu CA, Tincu IF, Smadeanu RE, et al. Benefits of oligofructose and inuline in management of functional diarrhoea in children – interventional study. Farmacia. 2019;67:511–516. [Google Scholar]
- 21.Schweiger J, Karlnoski R, Mangar D, et al. Impact of a low-pressure polyurethane adult endotracheal tube on the incidence of ventilator-associated pneumonia: A before and after concurrence study. ISRN Critical Care. 2013;13:1–6. [Google Scholar]


