Abstract
Background and Objectives:
Research provides robust support for an association between traumatic exposure and emotion dysregulation. Less understood is the relation of emotion dysregulation stemming from positive emotions to traumatic exposure, or the extent to which negative and positive emotion dysregulation may be uniquely related to specific trauma types.
Design and Methods:
The present study explored the associations between negative and positive emotion dysregulation and specific trauma types in a community sample of 433 adults (M age = 43.81, 68.4% women).
Results:
Results highlighted three main findings: (1) negative and positive emotion dysregulation were significantly higher among individuals with vs. without exposure to six and nine specific trauma types, respectively; (2) negative and positive emotion dysregulation were significantly and positively related to total number of specific traumatic events; and (3) negative emotion dysregulation was significantly higher among individuals with Victimization Traumas in the overall sample as well as the no-PTSD and no-MDD subsamples, and positive emotion dysregulation was significantly lower among individuals with Accidental/ Injury Traumas and Victimization Traumas in the PTSD subsample.
Conclusions:
Results underscore the relative and unique roles of negative and positive emotion dysregulation in trauma types; these findings may inform future research.
Keywords: traumatic exposure, emotion, dysregulation, emotion, regulation, difficulties, regulating negative, emotions, difficulties, regulating positive emotions
As defined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, a traumatic event involves direct or indirect exposure to actual/threatened death, serious injury, or sexual violence (American Psychiatric Association, 2013). Results from one national survey found that ~90% of adults in the United States experienced one or more traumatic events in their lifetime (Kilpatrick et al., 2013). Traumatic events are associated with a slew of adverse physical (e.g., inflammation, chronic pain, and cardiovascular disease; Kendall-Tackett, 2009), psychological (e.g., major depressive, posttraumatic stress, and generalized anxiety disorders; Grant et al., 2008), and behavioral (e.g., substance use and suicidal behaviors; Carliner et al., 2016; Olshen et al., 2007) health concerns. With the wide array of deleterious costs linked to traumatic experiences, it is imperative that research explicate correlates of trauma as a means of informing targeted interventions aimed at mitigating its deleterious aftereffects.
Theoretical and empirical research highlights the link between emotion dysregulation and traumatic exposure (Ehring & Quack, 2010). Emotion dysregulation involves (a) a lack of awareness, understanding, and acceptance of emotions; (b) the inability to control behaviors when experiencing emotional distress; (c) a lack of access to situationally appropriate strategies for modulating the duration and/or intensity of emotional responses in order to meet individual goals and situational demands; and (d) an unwillingness to experience emotional distress as part of pursuing meaningful activities in life (Gratz & Roemer, 2004; Gratz & Tull, 2010). Intense emotional reactions are common in the aftermath of traumatic experiences (American Psychiatric Association, 2013) and may require substantial effort to modulate, overwhelming the regulatory capacities of trauma-exposed individuals (Tull et al., 2007). As a result, over time, trauma-exposed individuals may rely on maladaptive strategies for regulating their emotions (Weiss, Tull, et al., 2012b). While associated with immediate relief, these strategies may result in a rebound effect (Tull et al., 2010), further taxing emotion regulation capacities (Hayes et al., 1996). In line with theoretical accounts, traumatic exposure has been shown to prospectively predict emotion dysregulation; college students in one study exhibited significant increases in emotion dysregulation from pre- to post-mass school shooting (Bardeen et al., 2013). Providing further support for this association, cross-sectional studies have found evidence for strong positive associations between traumatic exposure and emotion dysregulation in various populations (Buckholdt et al., 2015; Weiss et al., 2013; Weiss, Tull, et al., 2012a).
Less understood is the relation of specific trauma types with emotion dysregulation. One relevant study compared groups that had experienced early-onset interpersonal trauma – sexual or physical violence prior to age 14 – either chronic, lasting one year or more, or non-chronic, lasting less than one year – to groups that had experienced non-interpersonal or late-onset trauma (Ehring & Quack, 2010). The authors found that individuals with a history of early-onset interpersonal trauma reported greater emotion dysregulation (overall as well as for specific dimensions of lack of emotional awareness, lack of emotional clarity, difficulties engaging in goal-directed behavior when distressed, and impulse control difficulties when distressed). Further, those who experienced chronic early-onset interpersonal trauma had more deficits in emotional clarity than all other groups. In another study, Raudales et al. (2019) found that community members with a history of sexual assault experienced greater emotion dysregulation compared to those with a history of combat exposure or non-interpersonal trauma, but did not differ in levels of emotion dysregulation from those with a history of physical assault. Finally, Contractor et al. (2020) found that traumatic experiences characterized by victimization – but not accidental/injury or predominant death threat – were associated with emotion dysregulation.
These early studies suggest that emotion dysregulation may be particularly salient to interpersonal trauma. The unique features of interpersonal trauma – e.g., it is perpetrated by another individual and involves more intense emotional reactions than other traumatic experiences (Amstadter & Vernon, 2008) – may explain its strong relation to emotion dysregulation. Indeed, interpersonal context, such as compromised attachment (Cloitre et al., 2008) and interaction with primary caretaker (Calkins & Hill, 2007), is purported to play an important role in the development of emotion dysregulation. Further, greater intensity of emotional experiences has been shown to be more difficult to regulate (Dixon-Gordon, Aldao, et al., 2015a). Yet, few studies have examined the influence of specific interpersonal trauma types other than sexual or physical assault (e.g., sudden and violent death of a close other) or non-interpersonal trauma types (e.g., natural disaster) on emotion dysregulation. Such research may more precisely identify individuals at risk for emotion dysregulation following trauma.
An additional limitation of the extant research in this area is its exclusive focus on emotion dysregulation stemming from negative emotional experiences. Growing evidence suggests that individuals may also exhibit positive emotion dysregulation, including nonacceptance of positive emotions, difficulties engaging in goal-directed behaviors when experiencing positive emotions, and difficulties controlling impulsive behaviors when experiencing positive emotions (Weiss, Gratz, et al., 2015a). While not directly studied in relation to traumatic types, positive emotion dysregulation has been linked to post-trauma outcomes such as posttraumatic stress disorder (PTSD; Weiss et al., 2018a; Weiss, Darosh, et al., 2019a; Weiss, Nelson, et al., 2019b) and major depressive disorder (MDD; Schick et al., 2019). Explanations as to why positive emotion dysregulation may be elevated post-trauma include that positive emotions may (a) elicit negative secondary emotional responses through negative affect interference (Frewen et al., 2012); (b) not be experienced to their full extent in regard to intensity and duration (i.e., emotional numbing; Feldman et al., 2008); or (c) result in emotion-driven impulsivity (Weiss et al., 2015b). This work underscores the potential for both under- and over-regulation of positive emotional processes among individuals with a history of traumatic exposure. Reflecting under-regulation of positive emotions, traumatic exposure may elicit risky, reward-seeking behavior (Weiss, Tull, et al., 2015b). Conversely, blunting of affect following traumatic exposure may reflect over-regulation of positive emotions (Hopper et al., 2007). It is also possible that individuals with a history of traumatic experiences report an oscillating pattern of both over- and under-regulation of positive emotions (del Río-Casanova et al., 2016). Yet, the relation of positive emotion dysregulation to specific trauma types hasn’t been explored.
To address the above-mentioned gaps in the literature, the current study examined relations between specific trauma types and both negative and positive emotion dysregulation. Consistent with research, we hypothesized that negative and positive emotion dysregulation would be elevated among individuals with versus without a history of traumatic exposure, particularly for the interpersonal trauma types of physical and sexual assault.
Methods
Procedure and participants
Procedures were approved by the University of Rhode Island Institutional Review Board. Community individuals were recruited from Qualtrics Online Panels, an internet-based crowdsourcing platform. Inclusion criteria for the current study were assessed during study screening and included: (1) ages 18 years or older, (2) having a working knowledge of English, (3) residing in North America (because the goal of the larger study was to examine racial and ethnic differences in emotions and the experiences of racial and ethnic groups vary as a function of nationality), and (4) endorsing Asian, Black, Hispanic, or White racial/ethnic background. Recruitment was stratified by race/ethnicity to assure equal representation of individuals from these four racial/ethnic groups (~100 participants per group). Individuals who did not meet inclusion criteria were routed out of the online survey, and thus data for them on the study measures does not exist. Eligible participants who provided informed consent and completed the entire survey without failing validity checks received monetary compensation that varied according to pre-determined Qualtrics sampling and recruitment procedures. Participants completed a battery of questionnaires, which included the measures (Measures section) examined in this study.
Exclusions, missing data, and sample characteristics
A total of 1,160 participants attempted the survey. We excluded participants for the following reasons (more than one reason could be endorsed): being < 18 years (n = 121); not having a working knowledge of English (n = 27); not residing in North America (n = 303); identifying as a race/ethnicity other than Asian, Black or African American, Hispanic or Latino/a, or White (n = 76); failing validity checks inserted to ensure attention and comprehension (n = 380; Meade & Craig, 2012; Oppenheimer et al., 2009; Thomas & Clifford, 2017); and attempting to take the survey more than once (n = 24). The final sample included 434 participants; the age of participants ranged from 18 to 85 years (M = 43.81, SD = 15.23), and 297 were women(68.4%). See Table 1 for demographic data.
Table 1.
Demographic data.
| M (SD) | n (%) | |
|---|---|---|
|
| ||
| Age | 43.81 (15.23) | |
| Gender | 297 (68.4%) | |
| Women | 133 (30.6%) | |
| Men | 1 (0.2%) | |
| Female to Male Transgender | 2 (0.5%) | |
| Male to Female Transgender | 297 (68.4%) | |
| Race | ||
| White | 119 (27.4%) | |
| African American/Black | 105 (24.2%) | |
| Asian | 105 (24.2%) | |
| Hispanic or Latino/a | 105 (24.2%) | |
| Employment Status | ||
| Employed Part-time | 57 (13.4%) | |
| Employed Full-time | 193 (45.3%) | |
| Not in labor force (student, homemaker) | 92 (21.6%) | |
| Unemployed | 84 (19.7%) | |
| Family Annual Income | ||
| < $15,000 | 239 (59.3%) | |
| $15,000–$24,999 | 20 (5.0%) | |
| $25,000–$34,999 | 29 (7.2%) | |
| $35,000–$49,999 | 28 (6.9%) | |
| $50,000–$64,999 | 31 (7.7%) | |
| $65,000–$79,999 | 17 (4.2%) | |
| $80,000 or higher | 39 (9.7%) | |
Measures
Traumatic Exposure.
The Life Events Checklist for DSM-5 (LEC-5; Weathers, Blake, et al., 2013a) is a 17-item self-report measure designed to screen for specific traumatic events in a respondent’s lifetime. It assesses exposure to 16 specific traumatic events. For each event, the respondent is asked to indicate if: (a) it happened to them, (b) they witnessed it, (c) they learned about it, (d) they experienced it as part of their job, (e) they aren’t sure if they experienced it, or (f) they didn’t experience it. Either of the first four response options indicated a positive Criterion A traumatic event endorsement (American Psychiatric Association, 2013); responses for each of the specific trauma types were recoded as “present” vs. “absent.” In addition, the total number of specific traumatic events was calculated by summing dichotomous values (present vs. absent) for the specific trauma types. Finally, consistent with Contractor et al. (2020), trauma type clusters were calculated by summing dichotomous values (present vs. absent) of LEC-5 items within that cluster: Accidental/Injury Traumas (LEC-5 items 1, 2, 3, 4, and 12), Victimization Traumas (LEC-5 items 6, 8, and 9), and Predominant Death Threat Traumas (LEC-5 items 5, 7, 10, 11, 13–16). The LEC has demonstrated convergent validity with measures assessing traumatic exposure and psychopathology related to traumatic exposure (Gray et al., 2004).
Negative Emotion Regulation.
The Difficulties in Emotion Regulation Scale – 16 (DERS-16; Bjureberg et al., 2016) is a 16-item self-report measure developed to assess clinically relevant difficulties in the regulation of negative emotions. Participants rate the extent to which items apply to them using a 5-point Likert-type scale ranging from 1 (almost never) to 5 (almost always). A total score was calculated by summing all the items, with higher scores indicating greater negative emotion dysregulation. The DERS-16 has sound psychometric properties, demonstrating good test-retest reliability, convergent validity, and discriminant validity (Bjureberg et al., 2016). Cronbach’s α was .96 in the current study.
Positive Emotion Regulation.
The Difficulties in Emotion Regulation Scale-Positive (DERS-P; Weiss, Gratz, et al., 2015a) is a 13-item self-report measure developed to assess clinically relevant difficulties in the regulation of positive emotions. Participants rate the extent to which items apply to them using a 5-point Likert-type scale ranging from 1 (almost never) to 5 (almost always). A total score was calculated by summing all the items, with higher scores indicating greater positive emotion dysregulation. The DERS-P has demonstrated good psychometric properties (Weiss, Darosh, et al., 2019a; Weiss, Gratz, et al., 2015a). Cronbach’s α was .96 in the current study.
Posttraumatic Stress Disorder.
The PCL-5 (Weathers, Litz, et al., 2013b) is a 20-item, self-report measure that assesses past 30-day PTSD symptoms stemming from the traumatic event identified as most distressing on the LEC-5. Respondents use a 5-point Likert-type scale ranging from 0 (not at all) to 4 (extremely). A total score was calculated by summing scores for all items. A score of ≥33 indicated a PTSD diagnosis (Blevins et al., 2015). The PCL-5 has demonstrated excellent psychometric properties (Bovin et al., 2016; Wortmann et al., 2016). Internal consistency in the current sample was excellent, Cronbach’s α = .98.
Major Depressive Disorder.
The Patient Health Questionnaire-9 (PHQ-9; Kroenke & Spitzer, 2002) is a 9-item self-report measure assessing past two-week depression symptoms. Respondents answer using a 4-point Likert-type scale ranging from 0 (not at all) to 4 (nearly every day). A total score was calculated by summing scores for all items. A score of ≥10 indicated a MDD diagnosis (Fine et al., 2013). The PHQ-9 has demonstrated excellent psychometric properties (Kroenke & Spitzer, 2002). Internal consistency in the current sample was excellent, Cronbach’s α = .95.
Data analysis
Study variables were assessed for normality using recommendations set by Tabachnick and Fidell (2007). Next, the frequencies of the specific traumatic events on the LEC-5 were calculated. Following this, for the primary analyses, a series of t-tests for independent samples were used to compare levels of negative and positive emotion dysregulation across participants with versus without exposure to each of the specific LEC-5 traumatic events. As noted in Lakens (2013), Cohen’s ds was computed as an index of effect size; a small effect size was indicated by ≥0.20, a medium effect size was indicated by ≥0.50, and a large effect size was indicated by ≥0.80 (Cohen, 1988). A Benjamini-Hochberg adjustment was utilized to minimize both Type I and Type II error (Benjamini & Hochberg, 1995). Specifically, for each model, the p values for these effects were rank ordered by size. Then, each individual p-value’s Benjamini-Hochberg critical value was calculated using the formula (i/m)Q, where i = the individual p-value’s rank, m = the total number of tests, and Q = the p value (.05). Original p-values are then compared to respective Benjamini-Hochberg critical values (based on the p-value’s rank: 1 = .003, 2 = .006, 3 = .009, 4 = .012, 5 = .015, 6 = .018, 7 = .021, 8 = .025, 9 = .028, 10 = .031, 11 = .034, 12 = .037, 13 = .040, 14 = .043, 15 = .046, 16 = .050). This method preserves an overall Type I error without increasing the risk for Type II error and unnecessarily reducing statistical power.
Supplemental analyses were conducted to clarify the relations between trauma types and both negative and positive emotion dysregulation. Pearson correlations examined the associations between total number of specific traumatic events and both negative and positive emotion dysregulation. Then, t-tests for independent samples were conducted to explore the relation of empirically-derived trauma type clusters to both negative and positive emotion dysregulation in the overall sample as well as in subsamples with and without PTSD and MDD.
A priori power analyses with GPower (Faul et al., 2007) indicated that sample sizes of 128 and 84 would be needed to detect medium effects with t-tests and correlations, respectively.
Results
Primary analyses
Most participants (91.1%) reported a history of traumatic exposure. The most commonly experienced traumatic events were transportation accident (75.3%), natural disaster (67.3%), physical assault (56.7%), and fire or explosion (51.6%). See Table 2 for frequencies of specific traumatic events in the overall sample.
Table 2.
Summary of group comparison findings.
| DERS | DERS-P | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Frequencya | t-test | Cohen’s ds | Exposure M(SD) | No Exposure M(SD) | t-test | Cohen’s ds | Exposure M(SD) | No Exposure M(SD) | |
|
| |||||||||
| Natural disaster | 292 (67.3%) | t = 0.36 p = . 72 | 0.03 | 32.42 (15.52) | 31.85 (15.16) | t = 0.12 p = .90 | 0.01 | 17.75 (9.37) | 17.64 (7.61) |
| Fire or explosion | 224 (51.6%) | t = 1.52 p = . 13 | 0.14 | 33.32 (15.74) | 31.08 (15.74) | t = 2.45 p = .01 | 0.23 | 18.73 (10.52) | 16.36 (6.79) |
| Transportation accident | 327 (75.3%) | t = 0.72 p = .47 | 0.08 | 32.54 (15.50) | 31.30 (15.08) | t = 1.04 p = .30 | 0.11 | 17.46 (8.81) | 18.49 (9.41) |
| Serious accident at work, home, or during recreational activity | 208 (47.9%) | t = 2.18 p = .03 | 0.20 | 33.91 (16.37) | 30.70 (14.29) | t = 2.66 p < .001 | 0.25 | 18.90 (10.47) | 16.23 (7.16) |
| Exposure to toxic substance | 126 (29.0%) | t = 2.51 p = . 01 | 0.25 | 35.11 (17.01) | 31.06 (14.54) | t = 4.09 p < .001 | 0.38 | 20.42 (12.11) | 16.61 (7.02) |
| Physical assault | 246 (56.7%) | t = 2.43 p = . 02 | 0.23 | 33.80 (15.73) | 30.20 (14.72) | t = 0.88 p = .38 | 0.08 | 18.04 (9.58) | 17.28 (8.09) |
| Assault with a weapon | 180 (41.4%) | t = 1.95 p = .05 | 0.18 | 33.94 (16.38) | 31.03 (14.56) | t = 2.88 p = .004 | 0.27 | 19.17 (10.76) | 16.68 (7.28) |
| Sexual assault | 200 (46.1%) | t = 2.04 p = .04 | 0.19 | 33.87 (15.78) | 30.85 (14.94) | t = 1.89 p = .06 | 0.18 | 18.59 (9.90) | 16.96 (8.03) |
| Other unwanted or uncomfortable sexual experience | 219b(50.5%) | t = 3.30 p = .001 | 0.36 | 34.63 (16.40) | 29.80 (13.91) | t = 1.11 p = . 27 | 0.10 | 18.19 (9.51) | 17.23 (8.37) |
| Combat or exposure to a war-zone | 127 (29.3%) | t =2.30 p = .02 | 0.23 | 34.87 (16.92) | 31.15 (14.60) | t = 4.32 p < .001 | 0.40 | 20.55 (12.13) | 16.54 (6.97) |
| Captivity | 111 (25.6%) | t = 2.07 p = .04 | 0.21 | 34.84 (17.30) | 31.34 (14.60) | t = 4.32 p < .001 | 0.41 | 20.82 (12.47) | 16.64 (7.10) |
| Life-threatening illness or injury | 212 (48.8%) | t = 2.31 p = .02 | 0.22 | 33.98 (16.07) | 30.58 (14.52) | t = 3.24 p = .001 | 0.30 | 19.12 (10.81) | 16.36 (6.49) |
| Severe human suffering | 179 (41.2%) | t = 1.46 p = .14 | 0.14 | 33.53 (15.94) | 31.33 (14.95) | t = 2.23 p = .03 | 0.21 | 18.85 (10.37) | 16.91 (7.75) |
| Sudden violent death | 178 (41.0%) | t = 2.13 p = .03 | 0.20 | 34.11 (16.33) | 30.93 (14.59) | t = 2.39 p = .02 | 0.22 | 18.94 (10.80) | 16.86 (7.32) |
| Sudden accidental death | 184 (42.4%) | t = 0.98 p = . 33 | 0.09 | 33.08 (15.77) | 31.62 (15.10) | t = 1.87 p = .06 | 0.17 | 18.65 (10.33) | 17.02 (7.76) |
| Serious injury, harm, or death you caused to someone else | 103 (23.7%) | t = 2.56 p = .01 | 0.27 | 35.61 (16.76) | 31.19 (14.81) | t = 4.94 p < .001 | 0.47 | 21.42 (12.53) | 16.56 (7.16) |
Note: Bolded content represents significant findings after the Benjamini-Hochberg adjustment was utilized.
Based on DSM-5 Criterion A for traumatic exposure (i.e., happened to them, they witnessed it, they learned about it, or they experienced it as part of their job).
DERS: Difficulties in Emotion Regulation Scale-16; DERS-P: Difficulties in Emotion Regulation Scale – Positive.
Negative emotion dysregulation
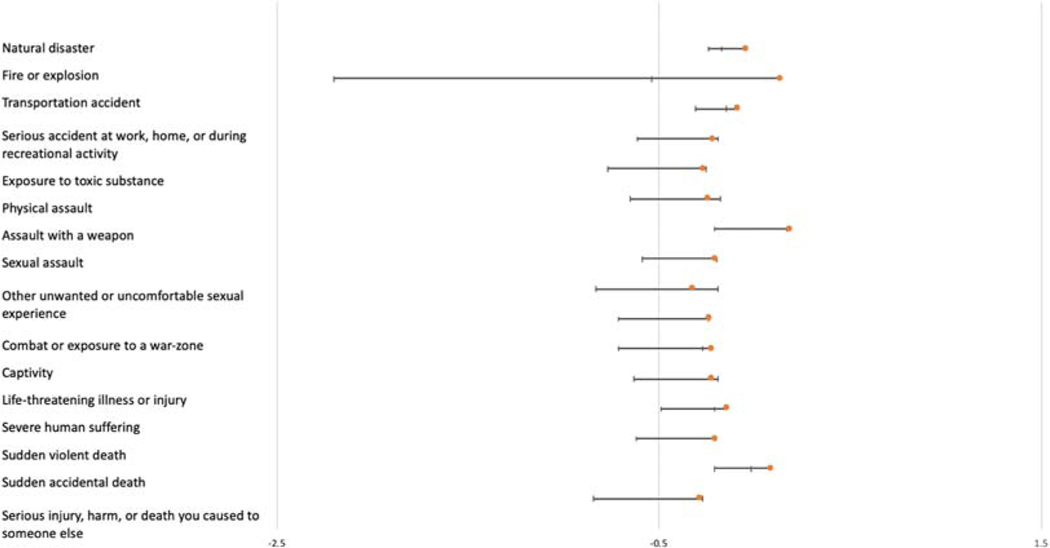
Findings of t-tests (Table 2) showed significant differences in negative emotion dysregulation as a function of exposure to a toxic substance (small effect size), physical assault (small effect size), other unwanted/uncomfortable sexual experience (small-to-medium effect size), combat exposure to a war-zone (small effect size), illness or injury (small effect size), and serious injury, harm, or death caused to someone (small effect size). Levels of negative emotion dysregulation were higher among individuals with versus without exposure to these traumatic events. Summary of unbiased Cohen’s ds values and 95% CI for relations between specific trauma types and negative emotion dysregulation are presented in Table 4 and Figure 1.
Table 4.
Summary of unbiased Cohen’s ds values and 95% confidence intervals (CI) for relations between specific trauma types and negative and positive emotion dysregulation.
| DERS | DERS-P | |||
|---|---|---|---|---|
|
|
|
|||
| dunbiased | 95% CI | dunbiased | 95% CI | |
|
| ||||
| Natural disaster | 0.04 | [−0.20, 0.13] | 0.01 | [−0.18, 0.15] |
| Fire or explosion | 0.14 | [−2.34, 0.68] | 0.27 | [−0.46, −0.08] |
| Transportation accident | 0.08 | [−0.23, 0.07] | 0.11 | [−0.04, 0.27] |
| Serious accident at work, home, or during recreational activity | 0.21 | [−0.40, −0.02] | 0.30 | [−0.49, −0.10] |
| Exposure to toxic substance | 0.26 | [−0.51, −0.01] | 0.38 | [−0.64, −0.14] |
| Physical assault | 0.24 | [−0.41, −0.06] | 0.09 | [−0.26, 0.09] |
| Assault with a weapon | 0.19 | [−040, 0.02] | 0.27 | [−0.48, −0.06] |
| Sexual assault | 0.20 | [−0.39, −0.00] | 0.18 | [−0.38, 0.02] |
| Other unwanted or uncomfortable sexual experience | 0.32 | [−0.51, −0.13] | 0.11 | [−0.30, 0.08] |
| Combat or exposure to a war-zone | 0.23 | [−0.48, 0.01] | 0.04 | [−0.66, −0.16] |
| Captivity | 0.22 | [−0.49, 0.05] | 0.41 | [−0.68, −0.15] |
| Life-threatening illness or injury | 0.22 | [−0.41, −0.03] | 0.31 | [−0.50, −0.12] |
| Severe human suffering | 0.14 | [−0.35, 0.07] | 0.21 | [−0.42, −0.00] |
| Sudden violent death | 0.20 | [−0.42, 0.00] | 0.24 | [−0.46, −0.40] |
| Sudden accidental death | 0.09 | [−0.30, 0.11] | 0.18 | [−0.38, 0.03] |
| Serious injury, harm, or death you caused to someone else | 0.28 | [−0.56, −0.01] | 0.47 | [−0.76, −0.20] |
DERS: Difficulties in Emotion Regulation Scale-16; DERS-P: Difficulties in Emotion Regulation Scale – Positive.
Figure 1.
Graphical depiction of unbiased Cohen’s ds values and 95% confidence intervals for relations between specific trauma types and negative emotion dysregulation.
Positive emotion dysregulation
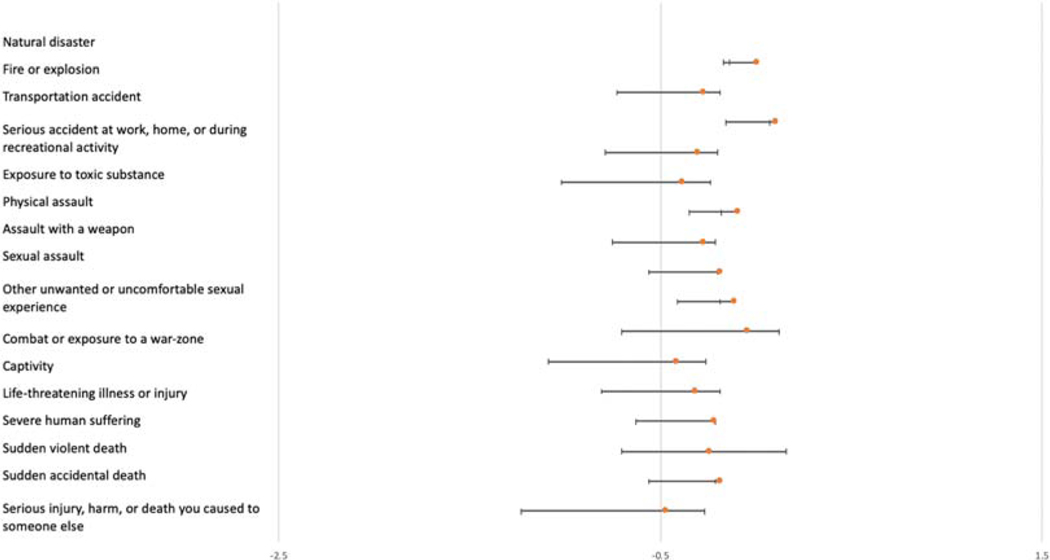
Findings of t-tests (Table 2) showed significant differences in positive emotion dysregulation as a function of exposure to a fire or explosion (small effect size), serious accident at work/home/during recreational (small effect size), exposure to toxic substance (small-to-medium effect size), assault with a weapon (small effect size), combat or exposure to a war-zone (small-to-medium effect size), captivity (small-to-medium effect size), life-threatening illness or injury (small effect size), and serious injury, harm, or death the individual caused to someone else (medium effect size). Levels of positive emotion dysregulation were higher among individuals with versus without exposure to these traumatic events. Summary of unbiased Cohen’s ds values and 95% CI for relations between specific trauma types and positive emotion dysregulation are presented in Table 4 and Figure 2.
Figure 2.
Graphical depiction of unbiased Cohen’s ds values and 95% confidence intervals for relations between specific trauma types and positive emotion dysregulation.
Supplemental analyses
Total number of traumatic events
Total number of specific traumatic events was significantly and positively related to both negative (r = .12, p = .006) and positive (r = .26, p < .001) emotion dysregulation.
Trauma type clusters (Table 3)
Table 3.
Summary of trauma cluster comparison findings.
| DERS | DERS-P | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| t-test | Cohen’s ds | No Exposure M(SD) | Exposure M(SD) | t-test | Cohen’s ds | No Exposure M(SD) | Exposure M(SD) | |
|
| ||||||||
| Overall Sample (N = 434) | ||||||||
| Accidental/Injury Traumas | t = 0.13 p = .86 | 0.02 | 32.00 (14.43) | 32.28 (14.43) | t = 1.50 p = .13 | 0.20 | 19.31 (9.47) | 17.45 (8.86) |
| Victimization Traumas | t = 2.70 p = .007 | 0.34 | 29.38 (14.52) | 33.61 (15.63) | t = 0.13 p = .89 | 0.01 | 17.63 (8.78) | 17.75 (9.07) |
| Predominant Death Threat Traumas MDD (n = 119) |
t = 0.56 p = .57 | 0.05 | 31.65 (15.66) | 32.53 (15.27) | t = 0.22 p = .82 | 0.02 | 17.57 (8.41) | 17.78 (9.24) |
| Accidental/Injury Traumas | t = 0.59 p = . 55 | 0.09 | 34.58 (15.63) | 33.00 (16.27) | t = 1.86 p = .06 | 0.29 | 20.41 (10.24) | 17.64 (8.91) |
| Victimization Traumas | t = 1.67 p = .09 | 0.20 | 30.92 (16.06) | 34.21 (16.16) | t = 0.43 p = .67 | 0.05 | 18.35 (9.75) | 17.87 (8.87) |
| Predominant Death Threat Traumas No MDD (n = 314) |
t = 0.06 p = .95 | 0.01 | 33.29 (16.84) | 33.17 (15.87) | t = 0.07 p = .93 | 0.01 | 18.07 (9.13) | 17.99 (9.16) |
| Accidental/Injury Traumas | t = 1.35 p = .18 | 0.39 | 25.83 (8.64) | 30.34 (13.19) | t = 0.15 p = .90 | 0.03 | 16.66 (6.85) | 16.95 (8.78) |
| Victimization Traumas | t = 2.42 p = .01 | 0.48 | 26.13 (9.70) | 31.74 (13.79) | t = 0.83 p = .40 | 0.16 | 16.11 (5.92) | 17.39 (9.71) |
| Predominant Death Threat Traumas PTSD (n = 202) |
t = 1.42 p = .15 | 0.28 | 27.20 (10.86) | 30.89 (13.40) | t = 0.58 p = .59 | 0.12 | 16.23 (5.90) | 17.21 (9.52) |
| Accidental/Injury Traumas | t = 1.81 p = .07 | 0.42 | 42.70 (12.54) | 36.75 (15.39) | t = 2.91 p = .004 | 0.63 | 27.04 (11.01) | 20.08 (10.96) |
| Victimization Traumas | t = 0.47 p = .63 | 0.07 | 38.38 (14.77) | 37.18 (15.33) | t = 2.05 p = .04 | 0.33 | 23.82 (12.00) | 20.03 (10.78) |
| Predominant Death Threat Traumas No PTSD (n = 230) |
t = 1.74 p = .08 | 0.28 | 40.82 (15.11) | 36.44 (15.10) | t = 1.78 p = .07 | 0.29 | 23.44 (11.61) | 20.14 (10.95) |
| Accidental/Injury Traumas | t = 1.29 p = .19 | 0.25 | 25.05 (10.99) | 28.32 (14.60) | t = 0.84 p = .39 | 0.18 | 14.29 (2.55) | 15.06 (5.41) |
| Victimization Traumas | t = 2.63 p = .009 | 0.37 | 24.88 (12.16) | 29.81 (15.04) | t = 1.02 p = .30 | 0.14 | 14.53 (3.94) | 15.22 (5.71) |
| Predominant Death Threat Traumas | t = 0.38 p = .70 | 0.05 | 27.38 (13.99) | 28.10 (14.25) | t = 0.40 p = .68 | 0.05 | 14.78 (4.06) | 15.06 (5.69) |
Note: Bolded content represents significant findings (p < .05).
DERS: Difficulties in Emotion Regulation Scale-16; DERS-P: Difficulties in Emotion Regulation Scale – Positive. MDD: Major Depression; PTSD: Posttraumatic Stress Disorder.
Overall Sample.
Higher levels of negative emotion dysregulation were found among individuals with vs. without Victimization Traumas (small-to-medium effect size).
MDD Status.
In the subgroup without MDD, higher levels of negative emotion dysregulation were found among individuals with vs. without Victimization Traumas (medium effect size).
PTSD Status.
In the subgroup without PTSD, higher levels of negative emotion dysregulation were found among individuals with vs. without Victimization Traumas (small-to-medium effect size). In the subgroup with PTSD, lower levels of positive emotion dysregulation were found among individuals with vs. without Accidental/Injury Traumas (medium-to-large effect size) and Victimization Traumas (small-medium effect size).
Discussion
Past research provides support for an association between emotion dysregulation and traumatic exposure (Bardeen et al., 2013; Weiss et al., 2013). Addressing gaps in these studies, the current investigation examined the relation of specific trauma types to negative and positive emotion dysregulation. In the current study, most participants endorsed traumatic exposure (91.1%), consistent with national estimates of the general population (Kilpatrick et al., 2013). Twelve DSM-5 Criterion A traumatic events were endorsed by greater than 30% of the sample. Regarding the relation between emotion dysregulation and trauma types, results highlighted three main findings: (1) negative and positive emotion dysregulation were significantly higher among individuals with vs. without exposure to six and nine specific trauma types, respectively; (2) negative and positive emotion dysregulation were significantly and positively related to total number of specific traumatic events; and (3) negative emotion dysregulation was significantly higher among individuals with Victimization Traumas in the overall sample as well as the no-PTSD and no-MDD subsamples, and positive emotion dysregulation was significantly lower among individuals with Accidental/Injury Traumas and Victimization Traumas in the PTSD subsample. These findings advance research by clarifying the roles of various indices of traumatic exposure – specific trauma types, cumulative trauma type exposure, and empirically-derived trauma type clusters – in emotion dysregulation.
One important finding was that levels of negative and positive emotion dysregulation were differentially associated with specific trauma types. In particular, levels of positive emotion dysregulation were significantly elevated for a greater number of specific trauma types (n = 9) compared to negative emotion dysregulation (n = 6). One explanation for these findings is that positive emotion dysregulation may be less commonly experienced by individuals compared to negative emotion dysregulation and thus be a stronger indicator of dysfunction. Indeed, negative emotions (e.g., fear, sadness) are frequently experienced as aversive (Watson & Clark, 1984), and efforts to change negative emotions are common (Gross & Thompson, 2007). Conversely, positive emotional states (e.g., happiness, joy) are most often desirable, associated with well-being and life satisfaction (Fredrickson, 2001). In line with these assertions, levels of positive emotion dysregulation (Weiss, Gratz, et al., 2015a) have been found to be lower than those of negative emotion dysregulation (Gratz & Roemer, 2004). Moreover, regarding the consequences of positive emotion dysregulation, in one study, a subgroup of participants characterized by both negative and positive emotion dysregulation reported higher levels of psychopathology and risky behaviors compared to those with negative emotion dysregulation alone (Weiss, Darosh, et al., 2019a). Future research is needed to test the hypothesis that positive emotion dysregulation may be a stronger indicator of more severe clinical outcomes.
Conversely, levels of negative emotion dysregulation were significantly and uniquely associated with exposure to unwanted or uncomfortable sexual experiences and physical assault. This finding is consistent with Raudales et al. (2019) and Contractor et al. (2020) who found that negative emotion dysregulation was most elevated among individuals reporting interpersonal victimization – and exposure to sexual and physical assault specifically – compared to other trauma types (e.g., non-interpersonal traumas). Unique characteristics about sexual and physical traumas may explain why it is related to higher levels of negative (but not positive) emotion dysregulation and with broader detrimental health outcomes (Contractor et al., 2018). For instance, sexual and physical assault is distinct from many other trauma types because it often involves malevolence, betrayal, and immorality (Finkelhor, 2014); subsequently experienced emotions may be particularly difficult to regulate. Alternatively, individuals with heightened levels of negative emotion dysregulation may be at particular risk for experiencing sexual and physical assault, consistent with the high-risk hypothesis (Chilcoat & Menard, 2003).
Individuals who reported exposure to a toxic substance, combat or exposure to a war-zone, and serious injury/harm/death caused to someone else had higher levels of both negative and positive emotion dysregulation compared to those without exposure to these types of trauma. Given evidence for more negative outcomes among individuals with heightened levels of both negative and positive emotion dysregulation (Weiss et al., 2018b), this finding may suggest that exposure to a toxic substance, combat exposure to a war-zone, and serious injury/harm/death caused to someone else are more severe trauma types. Alternatively, it is possible that severe emotion dysregulation – generalized across both negative and positive emotions – is more salient to perpetration versus victimization, reflected in these trauma types. For instance, guilt – characteristic of perpetration – may be more difficult to regulate (Sharvit & Valetzky, 2019).
Importantly, secondary analyses of PTSD (present/absent) and MDD (present/absent) subsamples suggested that traumatic exposure may be less relevant to emotion dysregulation in the context of psychopathology. Specifically, levels of negative emotion dysregulation were significantly higher among individuals with versus without Victimization Traumas in the overall sample as well as in the no-PTSD and no-MDD subsamples, but not in PTSD and MDD subsamples. PTSD (Tull et al., 2007; Weiss et al., 2013) and MDD (Berking et al., 2014; Dixon-Gordon et al., 2015b) have shown strong and robust relations with negative emotion dysregulation, and thus in the context of PTSD and MDD, type of trauma experienced may play a less critical role in levels of negative emotion dysregulation. Alternatively, among some individuals with Victimization Traumas, factors other than PTSD and MDD may relate to elevations in negative emotion dysregulation, such as traumarelated shame (Amstadter & Vernon, 2008) or substance use patterns (Simpson & Miller, 2002). Lastly, in the subgroup with PTSD, lower levels of positive emotion dysregulation were found among individuals with versus without Accidental/Injury and Victimization Traumas. Future research is needed to better understand these unexpected findings, potentially reflecting interactive effects of trauma and PTSD. Perhaps individuals with PTSD are more likely to experience posttraumatic growth – or positive changes after a challenging event, and related to increases in well-being – after Accidental/Injury and Victimization Traumas (Tedeschi & Calhoun, 2004).
Although the present study adds to the growing body of literature on traumatic exposure and emotion dysregulation, several limitations must be considered. First, the cross-sectional and correlational nature of the data precludes determination of the nature and precise direction of the relations examined. Future research is needed to further investigate the nature and direction of these relations through prospective, longitudinal investigations. A second limitation is an exclusive reliance on a self-report measures, responses to which may be influenced by one’s willingness and ability to report accurately. Future studies may benefit from the use of a multi-method approach (e.g., physiological measures of negative [Vasilev et al., 2009] and positive [Weiss et al., 2021] emotion dysregulation) and inclusion of structured diagnostic interviews. Third, data collection using online resources has some disadvantages that may limit the generalizability of results, such as sample biases (as a result of self-selection) and lack of control over the research environment. Thus, future research that integrates other data collection methods (e.g., face-to-face interviews) is warranted. Relatedly, while using validity checks and excluding individuals missing too much data improves MTurk data quality (Aust et al., 2012; Buhrmester et al., 2011; Oppenheimer et al., 2009) and the extent of our sample truncation (48%) is comparable to other MTurk trauma studies (57%; van Stolk-Cooke et al., 2018), a potential selection bias in our study may limit generalizability. Fourth, while use of a community sample is a strength of the current study, findings may not generalize to other populations. Thus, investigations are needed to replicate these results in larger, more diverse samples, including studies of individuals with different racial and ethnic backgrounds and national origins.
Fifth, Tull and Aldao (2015) distinguished between emotion regulation abilities and strategies. Emotion regulation abilities refer to the typical or dispositional ways in which individuals understand, regard, and respond to their emotional experiences (Gratz & Roemer, 2004), whereas emotion regulation strategies refer to specific tactics that individuals use to influence the experience and expression of their emotions (e.g., reappraisal, suppression; Gross, 2015). The current study only utilized measures of emotion regulation abilities. Thus, future research would benefit from examination of the relation of trauma types to emotion regulation strategies. Sixth, emotion dysregulation can involve both the under- and over-regulation of emotions. However, the measures of emotion dysregulation used in the current study do not distinguish between over- and under-regulation functions. Therefore, studies are needed to examine emotion dysregulation characterized by the under- versus over-regulation of emotions in relation to trauma types. Seventh, the measures of emotion dysregulation utilized here do not assess the regulation of distinct negative (e.g., shame, sadness, fear) and positive (e.g., joy, calm, excitement) emotions. Specific trauma types may be more likely to elicit particular emotional responses (e.g., shame is higher following sexual trauma; Amstadter & Vernon, 2008), and these emotions may be more difficult to regulate (Elison et al., 2014). As such, research that examines the regulation of distinct emotions as a function of specific trauma types is warranted.
Eighth, the version of the LEC-5 used in the current study assessed exposure to types of traumatic events, but did not evaluate specific characteristics of traumatic exposure that might relate to emotion dysregulation (e.g., time since trauma); this is an important consideration for future research. Ninth, existing research indicates that the majority of individuals experience multiple traumas in their lifetime (i.e., polytrauma exposure; Kilpatrick et al., 2013). Thus, excluding individuals with polytrauma exposure would negatively impact the generalizability – and thus clinical utility – of study findings. Nonetheless, it is important to note that not accounting for polytrauma experiences may have impacted results focused on specific trauma types. Future research with larger samples and a longitudinal, prospective design needs to examine the relations between emotion dysregulation and trauma types in samples characterized by single vs. polytrauma exposure. Finally, while sample sizes were considered adequate to detect medium effects in the overall sample and PTSD, no-PTSD, and MDD subsamples, analyses for the no-MDD subsample were not sufficiently powered. Thus, these resulted should be interpreted with caution and require replication in larger samples.
Despite these limitations, results of the current study extend our understanding of the association between traumatic exposure and emotion dysregulation. Specifically, evidence here suggests the importance of considering both negative and positive emotion dysregulation in our understanding of traumatic exposure (across specific types, cumulatively, and for empirically-derived clusters). Future research in this area may inform detection and intervention efforts for reducing negative outcomes among populations characterized by traumatic exposure.
Funding
Work on this paper was supported by National Institutes of Health Grants K23DA039327 and P20GM125507 awarded to NHW and F31DA051167 awarded to SRF.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed). [Google Scholar]
- Amstadter AB, & Vernon LL (2008). Emotional reactions during and after trauma: A comparison of trauma types. Journal of Aggression, Maltreatment & Trauma, 16(4), 391–408. 10.1080/10926770801926492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aust F, Diedenhofen B, Ullrich S, & Musch J. (2012). Seriousness checks are useful to improve data validity in online research. Behavior Research Methods, 45(2), 527–535. 10.3758/s13428-012-0265-2 [DOI] [PubMed] [Google Scholar]
- Bardeen JR, Kumpula MJ, & Orcutt HK (2013). Emotion regulation difficulties as a prospective predictor of posttraumatic stress symptoms following a mass shooting. Journal of Anxiety Disorders, 27(2), 188–196. 10.1016/j.janxdis.2013.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, & Hochberg Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B (Methodological), 57(1), 289–300. 10.1111/j.2517-6161.1995.tb02031.x [DOI] [Google Scholar]
- Berking M, Wirtz CM, Svaldi J, & Hofmann SG (2014). Emotion regulation predicts symptoms of depression over five years. Behaviour Research and Therapy, 57, 13–20. 10.1016/j.brat.2014.03.003 [DOI] [PubMed] [Google Scholar]
- Bjureberg J, Ljótsson B, Tull MT, Hedman E, Sahlin H, Lundh LG, Bjärehed J, DiLillo D, Messman-Moore T, Gumpert CH, & Gratz KL (2016). Development and validation of a brief version of the difficulties in Emotion Regulation Scale: The DERS-16. Journal of Psychopathology and Behavioral Assessment, 38(2), 284–296. 10.1007/s10862-015-9514-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Buckholdt KE, Weiss NH, Young J, & Gratz KL (2015). Exposure to violence, posttraumatic stress symptoms, and borderline personality pathology among adolescents in residential psychiatric treatment: The influence of emotion dysregulation. Child Psychiatry and Human Development, 46(6), 884–892. 10.1007/s10578-014-0528-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhrmester MD, Kwang T, & Gosling SD (2011). Amazon’s mechanical Turk: A new source of inexpensive, yet highquality, data? Perspectives on Psychological Science, 6, 3–5. [DOI] [PubMed] [Google Scholar]
- Calkins SD, & Hill A. (2007). Caregiver influences on emerging emotion regulation: Biological and environmental transactions in early development. In Gross JJ(Ed.), Handbook of emotion regulation (pp. 229–248). The Guilford Press. [Google Scholar]
- Carliner H, Keyes KM, McLaughlin KA, Meyers JL, Dunn EC, & Martins SS (2016). Childhood trauma and illicit drug use in adolescence: A population-based national comorbidity survey replication-adolescent supplement study. Journal of the American Academy of Child and Adolescent Psychiatry, 55(8), 701–708. 10.1016/j.jaac.2016.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilcoat HD, & Menard C. (2003). Epidemiological investigations: Comorbidity of posttraumatic stress disorder and substance use disorder. In Ouimette P. & Brown PJ(Eds.), Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders (pp. 9–28). American Psychological Association. [Google Scholar]
- Cloitre M, Stovall-Mcclough C, Zorbas P, & Charuvastra A. (2008). Attachment organization, emotion regulation, and expectations of support in a clinical sample of women with childhood abuse histories. Journal of Traumatic Stress, 21 (3), 282–289. 10.1002/jts.20339 [DOI] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Erlbaum. [Google Scholar]
- Contractor AA, Caldas S, Fletcher S, Shea MT, & Armour C. (2018). Empirically-derived lifespan polytraumatization typologies: A systematic review. Journal of Clinical Psychology, 74(7), 1137–1159. 10.1002/jclp.22586 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Weiss NH, Natesan Batley P, & Elhai JD (2020). Clusters of trauma types as measured by the Life Events Checklist for DSM-5. International Journal of Stress Management, 27(4), 380–393. 10.1037/str0000179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Río-Casanova L, González A, Páramo M, Van Dijke A, & Brenlla J. (2016). Emotion regulation strategies in trauma-related disorders: Pathways linking neurobiology and clinical manifestations. Reviews in the Neurosciences, 27(4), 385–395. 10.1515/revneuro-2015-0045 [DOI] [PubMed] [Google Scholar]
- Dixon-Gordon KL, Aldao A, & Reyes ADL (2015a). Emotion regulation in context: Examining the spontaneous use of strategies across emotional intensity and type of emotion. Personality and Individual Differences, 86, 271–276. 10.1016/j.paid.2015.06.011 [DOI] [Google Scholar]
- Dixon-Gordon KL, Weiss NH, Tull MT, DiLillo D, Messman-Moore T, & Gratz KL (2015b). Characterizing emotional dysfunction in borderline personality, major depression, and their co-occurrence. Comprehensive Psychiatry, 62(7), 187–203. 10.1016/j.comppsych.2015.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehring T, & Quack D. (2010). Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy, 41(4), 587–598. 10.1016/j.beth.2010.04.004 [DOI] [PubMed] [Google Scholar]
- Elison J, Garofalo C, & Velotti P. (2014). Shame and aggression: Theoretical considerations. Aggression and Violent Behavior, 19(4), 447–453. 10.1016/j.avb.2014.05.002 [DOI] [Google Scholar]
- Faul F, Erdfelder E, Lang AG, & Buchner A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. 10.3758/BF03193146 [DOI] [PubMed] [Google Scholar]
- Feldman GC, Joormann J, & Johnson SL (2008). Responses to positive affect: A self-report measure of rumination and dampening. Cognitive Therapy and Research, 32(4), 507–525. 10.1007/s10608-006-9083-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine TH, Contractor AA, Tamburrino M, Elhai JD, Prescott MR, Cohen GH, Shirley E, Chan PK, Goto T, Slembarski R, Liberzon I, Galea S, & Calabrese JR (2013). Validation of the telephone-administered PHQ-9 against the in-person administered SCID-I. Journal of Affective Disorders, 150(3), 1001–1007. 10.1016/j.jad.2013.05.029 [DOI] [PubMed] [Google Scholar]
- Finkelhor D. (2014). Childhood victimization: Violence, crime, and abuse in the lives of young people. Oxford University Press. [Google Scholar]
- Fredrickson BL (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56(3), 218–226. 10.1037/0003-066x.56.3.218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen PA, Dean JA, & Lanius RA (2012). Assessment of anhedonia in psychological trauma: Development of the hedonic deficit and interference scale. European Journal of Psychotraumatology, 3(1), 8585. 10.3402/ejpt.v3i0.8585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant DM, Beck JG, Marques L, Palyo SA, & Clapp JD (2008). The structure of distress following trauma: Posttraumatic stress disorder, major depressive disorder, and generalized anxiety disorder. Journal of Abnormal Psychology, 117(3), 662–672. 10.1037/a0012591 [DOI] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. 10.1023/b:joba.0000007455.08539.94 [DOI] [Google Scholar]
- Gratz KL, & Tull MT (2010). Emotion regulation as a mechanism of change in acceptance- and mindfulness-based treatments. In Baer RA (Ed.), Assessing mindfulness and acceptance processes in clients: Illuminating the theory and practice of change (pp. 107–133). New Harbinger Publications. [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, & Lombardo TW (2004). Psychometric properties of the Life Events checklist. Assessment, 11(4), 330–341. 10.1177/1073191104269954 [DOI] [PubMed] [Google Scholar]
- Gross JJ (2015). Emotion regulation: Current status and future prospects. Psychological Inquiry, 26(1), 1–26. [Google Scholar]
- Gross JJ, & Thompson RA (2007). Emotion regulation: Conceptual foundations. In Gross JJ (Ed.), Handbook of emotion regulation (pp. 3–24). Guilford Press. [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VM, & Strosahl K. (1996). Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology, 64(6), 1152–1168. 10.1037/0022-006x.64.6.1152 [DOI] [PubMed] [Google Scholar]
- Hopper JW, Frewen PA, van der Kolk BA, & Lanius RA (2007). Neural correlates of reexperiencing, avoidance, and dissociation in PTSD: Symptom dimensions and emotion dysregulation in responses to script-driven trauma imagery. Journal of Traumatic Stress, 20(5), 713–725. 10.1002/jts.20284 [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett K. (2009). Psychological trauma and physical health: A psychoneuroimmunology approach to etiology of negative health effects and possible interventions. Psychological Trauma: Theory, Research, Practice, and Policy, 1 (1), 35–48. 10.1037/a0015128 [DOI] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26 (5), 537–547. 10.1002/jts.21848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, & Spitzer RL (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals, 32 (9), 509–515. 10.3928/0048-5713-20020901-06 [DOI] [Google Scholar]
- Lakens D. (2013). Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Frontiers in Psychology, 4. 10.3389/fpsyg.2013.00863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade AW, & Craig SB (2012). Identifying careless responses in survey data. Psychological Methods, 17(3), 437. 10.1037/a0028085 [DOI] [PubMed] [Google Scholar]
- Olshen E, Mcveigh KH, Wunsch-Hitzig RA, & Rickert VI (2007). Dating violence, sexual assault, and suicide attempts among urban teenagers. Archives of Pediatrics & Adolescent Medicine, 161(6), 539–545. 10.1001/archpedi.161.6.539 [DOI] [PubMed] [Google Scholar]
- Oppenheimer DM, Meyvis T, & Davidenko N. (2009). Instructional manipulation checks: Detecting satisficing to increase statistical power. Journal of Experimental Social Psychology, 45(4), 867–872. 10.1016/j.jesp.2009.03.009 [DOI] [Google Scholar]
- Raudales AM, Short NA, & Schmidt NB (2019). Emotion dysregulation mediates the relationship between trauma type and PTSD symptoms in a diverse trauma-exposed clinical sample. Personality and Individual Differences, 139, 28–33. 10.1016/j.paid.2018.10.033 [DOI] [Google Scholar]
- Schick MR, Weiss NH, Contractor A, Dixon-Gordon KL, & Spillane NS (2019). Depression and risky alcohol use: An examination of the role of difficulties regulating positive emotions in trauma-exposed individuals. The American Journal of Drug and Alcohol Abuse, 45(3), 323–332. 10.1080/00952990.2019.1572759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharvit K, & Valetzky S. (2019). Who wants to be collectively guilty? A causal role for motivation in the regulation of collective guilt. Motivation and Emotion, 43(1), 103–111. 10.1007/s11031-018-9718-y [DOI] [Google Scholar]
- Simpson TL, & Miller WR (2002). Concomitance between childhood sexual and physical abuse and substance use problems: A review. Clinical Psychology Review, 22(1), 27–77. 10.1016/S0272-7358(00)00088-X [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (2007). Using multivariate statistics. Pearson. [Google Scholar]
- Tedeschi RG, & Calhoun LG (2004). Posttraumatic growth: A new perspective on psychotraumatology. Psychiatric Times, 21(4), 58–60. 10.1207/s15327965pli1501_01 [DOI] [Google Scholar]
- Thomas KA, & Clifford S. (2017). Validity and Mechanical Turk: An assessment of exclusion methods and interactive experiments. Computers in Human Behavior, 77, 184–197. 10.1016/j.chb.2017.08.038 [DOI] [Google Scholar]
- Tull MT, & Aldao A. (2015). Editorial overview: New directions in the science of emotion regulation. Current Opinion in Psychology, 3, iv–x. 10.1016/j.copsyc.2015.03.009 [DOI] [Google Scholar]
- Tull MT, Barrett HM, Mcmillan ES, & Roemer L. (2007). A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy, 38(3), 303–313. 10.1016/j.beth.2006.10.001 [DOI] [PubMed] [Google Scholar]
- Tull MT, Jakupcak M, & Roemer L. (2010). Emotion suppression: A preliminary experimental investigation of its immediate effects and role in subsequent reactivity to novel stimuli. Cognitive Behaviour Therapy, 39(2), 114–125. 10.1080/16506070903280491 [DOI] [PubMed] [Google Scholar]
- van Stolk-Cooke K, Brown A, Maheux A, Parent J, Forehand R, & Price M. (2018). Crowdsourcing trauma: Psychopathology in a trauma-exposed sample recruited via Mechanical Turk. Journal of Traumatic Stress, 31(4), 549–557. 10.1002/jts.22303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasilev CA, Crowell SE, Beauchaine TP, Mead HK, & Gatzke-Kopp LM (2009). Correspondence between physiological and self-report measures of emotion dysregulation: A longitudinal investigation of youth with and without psychopathology. Journal of Child Psychology and Psychiatry, 50(11), 1357–1364. 10.1111/j.1469-7610.2009.02172.x [DOI] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1984). Negative affectivity: The disposition to experience aversive emotional states. Psychological Bulletin, 96(3), 465–490. 10.1037/0033-2909.96.3.465 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013a). The Life Events Checklist for DSM-5 (LEC-5). www.ptsd.va.gov. [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013b). The PTSD Checklist for DSM-5 (PCL-5). www.ptsd.va.gov. [Google Scholar]
- Weiss NH, Darosh AG, Contractor AA, Forkus SR, Dixon-Gordon KL, & Sullivan TP (2018a). Heterogeneity in emotion regulation difficulties among women victims of domestic violence: A latent profile analysis. Journal of Affective Disorders, 239, 192–200. 10.1016/j.jad.2018.07.009 [DOI] [PubMed] [Google Scholar]
- Weiss NH, Darosh AG, Contractor AA, Schick MR, & Dixon-Gordon KL (2019a). Confirmatory validation of the factor structure and psychometric properties of the difficulties in Emotion Regulation Scale – positive. Journal of Clinical Psychology, 75(7), 1267–1287. 10.1002/jclp.22768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Dixon-Gordon KL, Peasant C, & Sullivan TP (2018b). An examination of the role of difficulties regulating positive emotions in posttraumatic stress disorder. Journal of Traumatic Stress, 31(5), 775–780. 10.1002/jts.22330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Gratz KL, & Lavender JM (2015a). Factor structure and initial validation of a multidimensional measure of difficulties in the regulation of positive emotions: The DERS-positive. Behavior Modification, 39(3), 431–453. 10.1177/0145445514566504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Nelson RJ, Contractor AA, & Sullivan TP (2019b). Emotion dysregulation and posttraumatic stress disorder: A test of the incremental role of difficulties regulating positive emotions. Anxiety, Stress, & Coping, 32(4), 443–456. 10.1080/10615806.2019.1618842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Schick MR, Waite EE, Haliczer LA, & Dixon-Gordon KL (2021). Association of positive emotion dysregulation to resting heart rate variability: The influence of positive affect intensity. Personality and Individual Differences, 173, 110607. 10.1016/j.paid.2020.110607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Davis LT, Dehon EE, Fulton JJ, & Gratz KL (2012a). Examining the association between emotion regulation difficulties and probable posttraumatic stress disorder within a sample of African Americans. Cognitive Behaviour Therapy, 41(1), 5–14. 10.1080/16506073.2011.621970 [DOI] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Lavender J, & Gratz KL (2013). Role of emotion dysregulation in the relationship between childhood abuse and probable PTSD in a sample of substance abusers. Child Abuse & Neglect, 37(11), 944–954. 10.1016/j.chiabu.2013.03.014 [DOI] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Sullivan TP, Dixon-Gordon KL, & Gratz KL (2015b). Posttraumatic stress disorder symptoms and risky behaviors among trauma-exposed inpatients with substance dependence: The influence of negative and positive urgency. Drug and Alcohol Dependence, 155, 147–153. 10.1016/j.drugalcdep.2015.07.679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Viana AG, Anestis MD, & Gratz KL (2012b). Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders, 26(3), 453–458. 10.1016/j.janxdis.2012.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, Hall-Clark B, Foa EB, Young-McCaughan S, Yarvis JS, Hembree EA, Mintz J, Peterson AL, & Litz BT (2016). Psychometric analysis of the PTSD checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment, 28(11), 1392–1403. 10.1037/pas0000260 [DOI] [PubMed] [Google Scholar]