Abstract
Background:
Men’s alcohol misuse does not occur in a vacuum but has a cascade of consequences for families and children, with ties to violence, poor parenting, and poor partner and child mental health. Despite the intersection of individual and interpersonal problems associated with men’s alcohol use, studies exploring the impact of men’s completion of alcohol misuse treatment on family and family member outcomes are scarce. Here we begin to explore this question.
Methods:
We conducted qualitative interviews (N = 13) with female partners and children (8–17 years) of men with problem drinking who completed individual treatment targeting alcohol misuse, depressed mood, and family-focused efforts in Eldoret, Kenya. Interviews and thematic content analysis were guided by ecological-transactional systems theory.
Results:
Findings highlighted positive perceived changes for men, families, women and children that interacted together in a bi-directional pathway. Partners and children described men’s reduced drinking, reduced spending, increased family-focused effort (e.g., coming home early), as well as increased emotion regulation, and openness to and communication with family. These changes were tied to perceived improvements in the couple and father-child relationship, including improved trust and time together, which were tied to improvements in women and children’s emotional well-being (e.g., hope). Concurrently, reports noted men’s increased effort to share money earned with the family which alleviated financial stress and helped ensure basic needs were met. Results aligned with the ecological transactional systems frame, with individuals in the family, family relationships, and economic climate each dynamically shaping each other.
Conclusions:
Although larger studies are needed, results provide promising signals regarding the potential downstream effects of individual treatment on family systems and members, which may in turn help maintain men’s changes in drinking.
Keywords: Fathers, Family outcomes, Alcohol intervention, Global mental health, Therapeutic change, Kenya
Few studies in low- and middle-income countries (LMICs) take a nuanced exploration of what happens, and how changes unfold, in the family when a family member completes treatment for alcohol use. This is especially true for men who are disproportionately impacted by alcohol use (Rehm et al., 2009), but often missing from family systems literature despite pronounced impacts on family (Panter-Brick et al., 2014). Here we use a qualitative approach to describe changes and pathways to change in the family system, including partner and child well-being, following men’s completion of an individual alcohol use and family engagement intervention in Kenya from the perspective of men’s partners and children. An exploration of how men’s treatment completion does or does not impact family alongside what the family sees as key drivers of change has implications for how to enhance treatment to best leverage downstream family impacts with potential to reinforce and sustain men’s individual substance use changes.
Alcohol misuse, or problem drinking—patterns that put men at risk for adverse health and social consequences (Alcohol & Substance Misuse, 2019) – among men, affects families with serious consequences on relationships and individual safety and mental health (Leonard & Eiden, 2007; Neger & Prinz, 2015; Schacht et al., 2009). When examined within an ecological-transactional framework, men’s drinking impacts, and is affected by, the relationships around him (Bronfenbrenner, 1994; Greenfield et al., 2016; Sundin et al., 2021). The ecological-transactional theory posits that individual well-being is shaped by interacting systems nested around the individual at different levels, such as the cultural climate, family environment, and caregiver well-being (Bronfenbrenner, 1994; Sameroff, 1975). This theory acknowledges the interaction of the environment with both individuals and family systems. For example, economic hardship increases the likelihood of men consuming alcohol to cope, which increases risk of child mental health problems (Gibbs et al., 2018).
We see these pattern with men’s problem drinking. At the individual-level, men’s drinking often co-occurs with depression (Kessler et al., 2011), which can worsen consequences (Orford et al., 2010a; Solis et al., 2012). Men’s problem drinking further places families at risk for intimate partner violence (IPV), child maltreatment, and partner and child mental health problems through longitudinal pathways starting with father alcohol use (Goeke-Morey & Mark Cummings, 2007; Hussong et al., 2012; Jewkes et al., 2011; Leonard & Eiden, 2007). These individual and family consequences are further exacerbated by poverty – widespread in LMICs (Rehm et al., 2009), and in contexts where norms place men in positions of power (Jewkes et al., 2011). Given there may be a ‘domino effect’ of father alcohol use on family systems in which father alcohol use predicts couple conflict, which compromises parenting, and impacts youth adjustment (Goeke-Morey & Mark Cummings, 2007; Schacht et al., 2009), treating father’s alone may have critical downstream influences on family systems.
For women and children in families, mental health problems are already a significant issue (Erskine et al., 2015). Adolescents, for instance, bear the largest burden of mental illness, with the majority of disorders emerging during the transition to adulthood (Kessler et al., 2005; Mokdad et al., 2016). This timing of mental health disorder onset can significantly disrupt a person’s life course, and identifying preventative interventions that can alter this course downstream is critical (Gibb et al., 2010; Kieling et al., 2011). Thus, it is imperative to identify potential pathways through which treatment for men’s alcohol misuse might affect the mental health of family members from family member perspectives, given this is often missing from the literature, especially outside of high-income countries (Cuijpers et al., 2015; Neger & Prinz, 2015; Panter-Brick et al., 2014).
In LMICs, there is a 78% treatment gap for AUD treatment alone (Kohn et al., 2004). Fewer treatments exist that address AUD and family behaviors impacted by drinking such as IPV and poor parenting (Giusto and Puffer, 2018). In Kenya, the need for effective alcohol use treatment is critical. Over 10% of Kenyans aged between 15 and 65 years have an alcohol use disorder (Nationalurv, 2017). In fact, the country has one of the highest total DALYs (54,000) from alcohol use disorders in Africa (orum on alcohol and dru, 2017). Due to this treatment gap in Kenya and other LMICs, little research exists that documents whether men receiving any type of AUD treatment shapes the family system. This has been identified as a critical issue needing attention in global settings (Orford et al., 2010b, 2013).
In this study, we explored whether men’s completion of treatment for alcohol misuse, low mood, and family problems had downstream effects on family members’ well-being through qualitative interviews with men’s wives/partners and children in Kenya. Interviews were conducted as part of pilot trial of LEAD: Learn, Act, Engage, Dedicate, a treatment developed for Kenya to improve men’s problem drinking, mood, and family interactions delivered by peer-father lay providers (Giusto, Ayuku, & Puffer, 2020). Here, we focus on qualitative data from men’s partners (wives) and children to explore and describe pathways of familial change not captured by quantitative data, identify key drivers of family system change, and elevate the voices of participating women and children affected by men’s alcohol misuse. We were guided by the following questions: Following men’s completion of treatment, how do partners and children: 1) perceive changes in men’s alcohol use and family-directed behaviors? And 2) how do any changes affect family relationships and individual members’ mental health?
1. Methods
1.1. Overview
We report qualitative findings from partners and children of men experiencing problem drinking who received treatment. Results stem from a pilot trial (n = 9 men) that used quantitative and qualitative measures to assess fathers’ alcohol use during and following LEAD, as well as pre-post changes on men’s depression and family outcomes reported on by men, partners, and a child (Giusto et al., 2020). Men also completed qualitative interviews focused on indicators of acceptability, feasibility, satisfaction, and change; the results of which are included elsewhere (Giusto et al., 2020). LEAD, described below, focused on men with problem drinking given this was the reported community need that arose in formative work. LEAD was not designed to target symptoms of dependence that would require medication management given some resources already existed in the area for dependence. Quantitative results, as well as fathers’ interviews, are reported elsewhere (Giusto et al., 2020), though we provide a summary of findings below to complement qualitative findings from partners and youth. Here, we focus on the experiences of women and children.
1.2. Setting
This study took place in the town of Eldoret, Kenya – one of the fastest growing areas in Kenya. Eldoret is a peri-urban community within the Rift Valley Province. The study was conducted in collaboration with Moi Teaching and Referral Hospital. The hospital is a part of the Academic Model Providing Access to Healthcare (AMPATH), a service and research organization including the hospital and a consortium of North American Schools in partnership with the Kenyan Ministry of Health. The hospital provides some psychiatric services, including inpatient care for severe substance use and limited outpatient care for substance use (Jaguga & Kwobah, 2020; Nationalurv, 2017). From a cultural lens, as with most countries worldwide, norms often afford men primary decision-making power within families in the area, and men are typically expected to take on the role of financial provider within the family while women are more often expected to manage the home (Puffer et al., 2019; Wegs et al., 2016). Formative work in the area conducted by our team showed men’s drinking was often tied to a sense of purposelessness or shame due to an inability to “be a man” and fulfill traditional gender roles due to a lack of economic opportunities in the area (Puffer et al., 2020).
1.3. Ethical review and safety considerations
All study procedures were approved by the Institutional Research and Ethics Committee at Moi Teaching and Referral Hospital and the Institutional Review Board at Duke Unicersity. Although this study did not focus on violence as an outcome, we designed procedures to help ensure participant safety, especially among partners and children. To do this, we included protocols, training, and materials that align with WHO recommendations to monitor safety, minimize risk, and respect women’s autonomy in the context of family violence (Ellsberg & Heise, 2005). These included: (1) research assistants trained in safety procedures, including planning and referral processes in ways that maintained privacy and aligned with participant values; (2) a Kenyan psychologist on call and available in case of any safety concern; (3) consenting processes and scripts with women and youth that emphasized privacy, the ability to withdrawal or stop at any point without consequence, and the ways confidentiality would be ensured; (4) no names or identifying information included on materials; (5) qualitative interview materials using open-ended questions aimed at minimizing distress that might be caused by participating in research; and (6) safety monitored with women and children throughout the study with survey measures administered at baseline, weekly during men’s treatment, and post-treatment. Notably, at baseline and during treatment, no female partners or youth reported severe violence indicators on quantitative measures or to research assistants during surveys.
1.4. Learn, engage, Act, Dedicate (LEAD) treatment
LEAD was developed by researchers and clinicians in Kenya and the US using a collaborative, multi-step process to target drinking, depressed-mood, and family-directed effort among men for delivery by lay providers (Giusto et al., 2020). It was developed in response to the lack of relevant services for problem drinking, specifically, as well to address challenges engaging fathers in family-based care due to drinking and gender norms around help-seeking (Giusto et al.). LEAD is 5- session individual treatment anchored in motivational interviewing (MI) and behavioral activation (BA) delivered weekly (Arkowitz et al., 2015; Daughters et al., 2008). It also includes discussions of masculinity and refusal skills training with a focus on applications to family relationships throughout. Session one begins with MI to enhance readiness to change drinking as well as engage men in treatment. Remaining sessions (2–5) use BA to replace drinking and isolating behaviors triggered by negative emotions with healthy, value-based behaviors for self and family; MI-informed strategies are integrated throughout to maintain engagement. In session 2, fathers discuss ‘what it means to be a man’ to expand conceptions of masculinity to include family behaviors aligned with care in order to reduce pressure to be a man in only one way (i.e., provider) and increase motivation to engage in other behaviors aligned with broader conceptions of masculinity (Dworkin et al., 2013). Refusal skills are taught in sessions two through four and are social communication techniques designed to help individuals refuse alcohol and deter urges to drink in social situations (Witkiewitz et al., 2012).
1.5. Pilot procedures and participants
For LEAD, male caregivers were recruited by trained community leaders who invited men to meet with study staff to learn more about the study. Community leaders recruited men for the study; community leaders were chosen as recruiters based on formative work that indicated men most often accepted help from them and men rarely, if ever sought help. For men who expressed an interest, a Kenyan research assistant completed eligibility assessment and informed consent procedures. To be eligible, men needed to meet the following inclusion/exclusion criteria: (a) responsible for the care of at least one child (8- 17); (b) engaged in alcohol misuse indicated by a score of 8–19 on the AUDIT, falling in harmful range (validated in Kenya; Babor et al., 2001; Saunders et al., 1993); (c) alcohol use within the past 2 months; and, (d) agree to have one child and a partner/co-parent participate in assessments. We excluded men who: (a) lived in a home where brewing alcohol occurs; (b) exhibited indicators of dependence and/or scored greater than 19 on the AUDIT (mhGAP, 2016). We excluded these men for a few reasons: (1) this was the first trial of LEAD; (2) LEAD was not designed to treat alcohol dependence, which requires medication management, and (3) LEAD was not designed to target alcohol use in the context of home brewing which would require a structural intervention. Those excluded for dependence were referred to a higher level of care at the local hospital Moi Teaching and Referral Hospital. If the man consented to participate, the research member then explained the study to his partner/co-parent and child to obtain informed consent/assent to participate in assessments. If the man had more than one child aged 8–17 years, we invited the oldest to participate. One month following male caregivers’ completion of treatment, qualitative interviews were conducted individually with men’s partners and with one child per family in a private location in, or surrounding, the family home (i.e., separate room, home when no one else home, outside area not visible to others).
LEAD was piloted using a multiple baseline single case series design, an approach that allows for preliminary inferential conclusions to be made about an intervention on outcomes, even with small samples. This is done through the use of numerous repeated measurements before, during, and, in this case, after the intervention (Hilliard, 1993). Based on the pilot, quantitative improvements were seen in fathers’ drinking as reported on by fathers (Giusto et al., 2020). In the month following treatment, men were 5.1 times more likely not to drink on any given day, and, on days they did drink, they consumed 50% less alcohol as measured with the timeline followback, a calendar-based measure of alcohol use-days drinking and amount drinking. Quantitative improvements also were observed on depression; family interactions; couple and father-child relationship; and father, partner, and child mental health. Qualitative interviews with fathers further complemented men’s quantitative findings, with men reporting high acceptability, feasibility, and satisfaction with treatment, as well as changes in drinking, improved family relationships at the family, couple, and father-child level, and improved well-being and increased enjoyment of their family (Giusto et al., 2020).
1.6. Interview guide
The interviews assessed perceptions of the father, his drinking, depressed mood, and family involvement, and observed changes on his engagement with the family following treatment. We applied the ecological-transactional theory, described above, to guide our investigation. As such, guides were designed to assess individual well-being and relationships surrounding the individual (in this case men) through open-ended questions. Some example questions for partners included the following: [Individual-level]: Tell me what he was like before, what he was like after the program, and what he is like now; [Relational-level] Tell me what it was like between you two before the program, and what it was like between you both after the program. Content was similar for children, but additional time was spent assuring them there were no right or wrong answers and noting that, in general, after parents try things (e.g., like LEAD) that things might stay the same, get better, or get worse; and language was simplified. Interviews were conducted by a trained Kenyan research assistant not involved in treatment. Interviews were administered in Swahili, audio-recorded, and transcribed verbatim into English.
1.7. Analysis
Qualitative interviews with families were analyzed using thematic content analysis using NVivo12 Software (Braun & Clarke, 2006; nternational Pty Ltd, 2018). First, two trained research assistants (one with a bachelor’s in psychology and one completing her master’s degree in global health), familiarized themselves with the transcripts. These team members were familiar with the study but did not conduct any other assessment nor were involved in the direct delivery of treatment. Next, they inductively open coded transcripts line-by-line using thematic analysis. They then deductively coded transcripts guided in part by codes based on ecological-transactional model domains (e.g., individual level, relational level). Together, the inductive and deductive codes were operationalized into a codebook based on initial coding and discussion between open coders and lead author. The coders then double coded five transcripts and were then required to reach 80% agreement on codes using the software. Notably, we opted for percent agreement over a Kappa coefficient because it was unlikely that coders would be “guessing,” and one advantage of Kappa is to account for chance agreement. Further, percent agreement is directly interpretable and does not carry the risk of problematic assumptions about rater independence (McHugh, 2012). After agreement was reached, the remaining transcripts were divided between the coders. Following, themes were generated, reviewed, defined, and summarized.
2. Results
2.1. Participants
In the pilot, eight of the nine men who participated completed LEAD. Seven partners and six children participated in the assessment (n = 13); of those who did not participate, one partner was unavailable to be scheduled, and for youth, two left town for boarding school and one could not be scheduled. The average age of partners was 32 [R: 23–43]; all were married/wives except for one who lived with the participant. For youth, the mean age was 11 [R: 8–15]; half were male, and all were men’s biological children.
2.2. Qualitative descriptions of change
2.2.1. Overview
Across women and children, overarching findings showed dynamic, bidirectional patterns and improvements in individual family members, family systems (relationships), and household finances that captured overall themes (Fig. 1). The pathway began with men’s reduced drinking, increased positive family-directed behaviors, and reduced spending following LEAD. Family-directed behaviors included increased apologizing to family members for engaging in drinking behaviors, efforts to discuss these behaviors with partners when they occurred, and increased time at home. Notably, these changes were described as happening in tandem with drinking reductions. In other words, family members did not describe alcohol reduction preceding or following changes in family behavior but occurring together. Almost all women and children linked these changes in men to improved family relationships, such as increased trust, and to increased money for basic household needs. In turn, the improved relationships and increased resources for the household were tied to improvements in individual emotional health including increased feelings of safety among wives/partners and reduced fear among children. These changes in the family, and for family members, then seemed to reinforce fathers’ behavior changes, according to participants. Overall, the emergent pattern aligned with the ecological transactional systems frame used to guide the study, with individuals in the family, family relationships, and economic climate each dynamically shaping each other. Below we review the pathway and the relevant subthemes within each change domain.
Fig. 1.
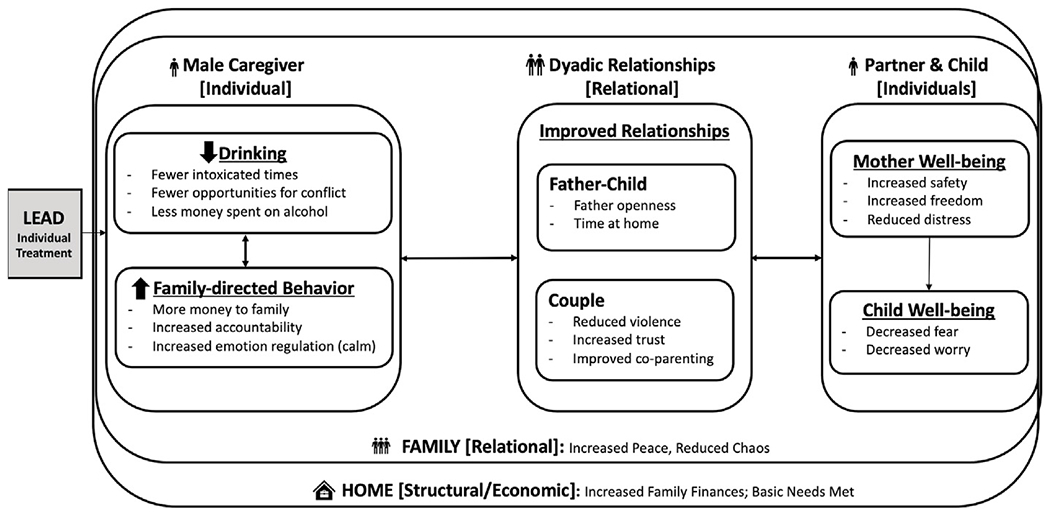
Bidirectional interactions among changes in male caregivers, family system, partners, and children.
Note: This figure depicts overarching pathways that emerged from the data following men’s treatment completion of LEAD: Learn, Act, Dedicate, Engage. The grey box on the left represents the treatment that men completed; each of the constructs that follow, are reported improvements in different ecological domains.
2.2.2. Individual male caregiver change: Partner and child perspectives
All partners reported observing reductions in men’s alcohol use. Prior to treatment, most partners and children described men were drinking alcohol, often causing chaos in the home, and acting inattentive and neglectful of family issues. They described that, as fathers reduced alcohol use they simultaneously showed improved mood and increased positive behaviors towards their family and spent less on alcohol. For all the wives who reported their husbands’ decreased alcohol use but did not abstain, they still described positive changes in men’s behaviors when drinking. These included the father: informing their partner they were going to drink, being more receptive to wives’ questions and requests to come home early, apologizing to family members for drinking or missing family obligations, more openly communicating about drinking, money earned or spent, and remaining calm and “maintaining peace” after drinking. Most youth noticed these changes as well. One daughter (age 10) remarked: “He [my father] can go, then come back in the evening and apologize saying ‘I have drunk a little amount of alcohol,’ so there is no conflict; therefore, we can sleep peacefully, and we all wake up safely and go on with our endeavors for the day.” A few other children noted a similar pattern connected to fathers’ reduced use and apologizing for drinking.
Most partners and children also reported that, after treatment, men began spending less on alcohol use and putting more money towards providing for the household. They suggested that prior to treatment, fathers were “devouring” finances on alcohol. One mother of a 15-year-old son put it succinctly, “he did not bring any money or food home, so we did not have food or even school fees.” Following treatment, women and children reported men shared money they received with the family and helped ensure basic needs were met. This was highlighted by many partners; one noted, “I see the money he earned, unlike before where I never saw any money he earned.” A few fathers even began working in order to provide for the family. One partner (age 32) noted, “He can now work, which he used to not do. He has managed the money well, and he is paying for the children’s education; now the children are in school.” Related, some partners reported improvements in men’s communication and emotion regulation, noting men were calmer and less defensive in interactions, particularly related to money and drinking. Related, one mother (age 26) described, “His bad thoughts have changed, and this made me believe that it was actually possible for a person to change from irrational thinking to rational.”
2.2.3. Relationship changes
All women and children described that fathers reduced drinking, acting in positive ways at home, and sharing money led to improved relationships across the family system including for couples and father-child relationships.
2.2.3.1. Home system and family.
At home, most mothers and children reported that there was more money for basic needs such as school fees, clothes, food, and activities. Two mothers reported their children were able to enroll in school because of the father’s increased efforts to share money. A few others reported they were able to buy more basic needs for children reporting, “[Before] he wouldn’t bother to buy basic needs. He would leave the house saying that he had gone to buy sugar but then change his mind and decide to drink. Yet, this is not so after the project, because he comes back with the commodity or leaves money so that I can send the child to the shop.”
At the family-level, changes included improvements in an overall feeling of peace and reduced chaos in the household. One woman (age 23) explained, “now … there are no conflicts; he comes home on time … watching his kids. We can even do work together.” Another partner put it clearly saying, “this project has helped him have love for his family because before he loved alcohol a lot but now, he loves his family more than alcohol.”
2.2.3.2. Father-child relationship.
Almost all children said that their relationships with their fathers improved. They described their relationships as more open (i.e., comfortable with father) and feeling less afraid of their father. A few children also reported that their father now made efforts to bring them snacks or treats. One daughter (age 10) relayed: “He can remember about home. He even makes us [the children] happy by bringing us goodies. We get excited and say, “We know dad is going to work so he will bring us something.” Some women also reported increased trust in their partners’ caregiving abilities. One mother (age 42) reported, “Now when my children see their father is sober, they are happy. [This allows] them to have a good relationship. He [also] spends time with them. Even if I leave for work somewhere, I leave them with him and when I return, I find them just fine.” Partners tied changes to fathers’ participation in LEAD and subsequent reductions in drinking and increased commitment to family.
2.2.3.3. Couple relationship.
Most women reported that their husbands now “sit and talk” with them and described improvements in communication, joint decision-making, and trust. When partners described the changes, they often attributed improvements in their relationship to changes in spending, better communication, and, subsequently, improved trust. Prior to treatment, partners described a negative cycle: spending on alcohol led to mistrust and conflict and violence; the conflict then fueled increased drinking and spending, which left no money for basic needs. One partner outlined a typical conflict:
“We would disagree because he would spend his money on alcohol - not on school fees. I would tell him that it was unfair for the children to not attend school and that it’s not good to have them stay at home and miss on the education. I would plead with him to give me little money to take it to school and try to talk to the school administrators to allow the children to continue with education and not neglect the children.”
After treatment, almost all partners reported a shift. They reported more joint planning of spending with their husbands/partners, increased and improved communication and transparency about money. These changes led to fewer fights. A woman from one family described their communication about money alongside her partner’s provision efforts and attitude shifts saying:
“When he wants to drink, he alerts me that he will drink, but just a little. Then I, in return, ask him if he has any money, and he would say yes. Then I would ask him to buy for us food before he goes his way, and he would do that. I would also request him to come back earlier, and he would … So, in general I can say that he is now responding to my opinion unlike before. He would utter words like, ‘We the Nandi people don’t allow women to have any say.‘ He has become very hospitable.”
Regarding violence, three women reported physical violence prior to LEAD during the post-study interviews. Of these three, all reported reductions in physical abuse, as well as harsh verbal treatment after the intervention. A few children noticed these changes as well. One male child (age 12) reported, “They [his parents] used to chase after each other. Father would even throw stones at her, but now it is better, and there is peace in the house.” Related, two partners reported increased freedom and respect within, and outside of, the household. One woman described the following increased economic autonomy:
“Nowadays he lets me go and look for a job, unlike before where if I left to look for a job and returned, it was chaos, violence and abusing me, saying that I had gone to do prostitution and many other things. There was no sleeping in peace. He [would] chase [me] at night because of the job I went to do, saying that I acquired money the wrong way…but nowadays, if I tell him I want to go and look for a job to do, he tells me to go.”
2.2.4. Individual female Partner and child change
Two partners reported experiencing less “psychological hurt” because of their husbands’ positive changes. One woman (age 26) reported the following, connecting the changes described above to her own mental health: “We have been sitting and discussing issues. This has been therapeutic because failure to do so hurt me psychologically. Before, in case of tough issues in the house which needed his attention, he didn’t have time to sit and try to solve it, and most things were left unattended. Lately, we are able to sit and plan with whatever amount of money there is, even if it is little.” Some children also reported increased happiness and hope. One male child (age 10) reported, “I have hope because I have seen some changes in him. Of late he doesn’t drink a lot of alcohol. He remembers about us, and he even makes us [he and his siblings] happy by bringing us goodies.” Some partners and children also reported feeling safer, less worried, and happier due to fathers’ efforts to reduce drinking and fulfill family responsibilities.
3. Discussion
Qualitative exploration into the effects of men’s alcohol use treatment on their families is missing in the literature in LMICs, despite pervasive intersecting risks between male alcohol use and family problems. The current study explored partners’ and children’s perspectives of change in the family and among family members following fathers’ treatment for alcohol misuse and depressed mood. Results illuminate key aspects of men’s change that influenced the family system and partner and child well-being including reduced alcohol use and increased family-directed behavior as a key driver of improved relationships. Findings complemented previous quantitative and qualitative findings from data provided by the men (Giusto et al., 2020).
Our findings can inform potential hypotheses about what drives change across family systems as perceived by family members; an important consideration for family members and men whose behavior change is more likely to be reinforced through resulting family positive interactions. The reinforcement of individual behavior change by positive interpersonal interactions is a phenomena seen in the literature (O’Farrell et al., 2004). We also observed this in qualitative interviews with men from the study (reported elsewhere) who noted feeling enjoyment, respect, and reduced stress when interacting with family versus drinking (Giusto et al., 2020). Reported perspectives help to better understand distal outcomes and potential pathways for future intervention refinement. Few studies have explored the impact of individual alcohol misuse treatment on family outcomes in LMICs (Giusto and Puffer, 2018) , with exceptions of those who included secondary family outcomes, such as IPV (Nadkarni et al., 2017). Some studies, primarily in the US and HICs, have examined the impact of substance use treatments that include family members (O’Farrell et al., 2004) or explicitly target relationship functioning (Harnett & Dawe, 2008; Stover, 2015) with improvements in use and family relationships. This differs from our approach (individual treatment with an interwoven family focus) but supports the importance of considering relationships in the context of individual disorders.
The qualitative themes fit with broader developmental psychopathology, the guiding framework, and the Family Stress Model. The Family Stress Model presents a multi-step pathway with economic hardship/pressure to provide leading to caregiver mental health problems, which contributes to poor family functioning, including disrupted parenting and couples’ conflict, which in turn impairs children’s well-being (Conger et al., 2002; Masarik & Conger, 2017). We observed these pathways, as well as others described in developmental literature that demonstrate men’s alcohol use predicts poor couple relationships, poor parenting and poor child mental health outcomes (Goeke-Morey & Mark Cummings, 2007; Schacht et al., 2009). The pressure to provide and economic climate associated with male drinking, depressed mood, and family stress, in turn impacted family relationships and women’s and children’s emotional well-being. Women and children reported the importance of not only reduced drinking and increased positive family efforts but the intersecting impact of reduced alcohol spending on the family system. This financial change seemed especially important for rebuilding couple trust and ensuring family basic needs were met; a critical consideration in resource-constrained settings where money often goes to basic needs. In future work, examining these pathways quantitatively can provide clues for how to best intervene with parents to disrupt cycles of risk.
Reported results also highlighted that for women and children, men’s alcohol use reductions, not only abstinence, produced noticeable improvements. Notably, these reductions occurred in tandem with increased family-directed efforts (a treatment target) and improved mood, which added to positive family impacts. These results support harm-reduction efforts (Charlet & Heinz, 2017). They might also have implications for how researchers and clinicians think about alcohol misuse reduction in tandem with increases in other healthy behaviors in treatment as these may be mutually reinforcing (Daughters et al., 2008; Fazzino et al., 2019).
Although reduction results were promising, they also point to areas for further intervention refinement to capitalize on impactful family changes driven by men’s improvements. Example targets might include individual conflict resolution, emotion regulation, and accountability (e.g., verbalizing responsibility for drinking) in interpersonal relationships. Each of these individually driven skills intersected with positive changes that partners and children appreciated. They shared that men spoke more calmly about times they drank, apologized for drinking, and communicated less defensively. Strengthening these skills while emphasizing reduction strategies may create healthy, positive cycles that reinforce themselves over time (Fazzino et al., 2019). Such an approach fits with the broader literature (primarily in the US) that highlights the importance of accountability, communication, and relationship quality in reducing alcohol use within couple relationships, as well as the importance of improved emotion regulation in the context of parenting (Neger & Prinz, 2015; O’Farrell et al., 2004).
Although results provide promising signals of impact in families, limitations exist. First, findings are based on a relatively small sample, which curtails generalizability. Related, although data saturation was reached for overall patterns, a few subthemes, including changes in men’s controlling behavior and experiences of reduced distress, were present only in a few families. This suggests that in a larger trial more interviews would be needed among families presenting with different types of family problems to better understand these experiences. Further, it is important to note that all family members who participated were related to men showing a willingness to receive treatment. These men may display a higher readiness or motivation to engage in treatment compared to other men experiencing problem drinking that could influence effects of treatment on families. Additionally, family members of men who did not complete treatment were not included in the study. There are also two other possible sources of bias. First, family members who did not participate in the assessment due to reported scheduling issues may also have been resistant to participating for other reasons. Next, women and children may have felt pressure to emphasize positive experiences to please the interviewer or possibly to please other family members, even despite privacy measures that were taken.
Overall, our findings highlighted perceived changes for families, women, and children when men complete an individual problem drinking, depressed mood, and family engagement treatment. Men’s reduction in drinking behaviors and increased family engagement improved dyadic relationships between men and their intimate partners as well as children. At the family level, improved relationships were related to decreased chaos and an increased sense of peace in the home. Moreover, families witnessed improved financial situations and more opportunities to provide for basic needs. These changes culminated in improved mental well being in women and children. These results show potential downstream effects of individual treatment and can inform integration of additional treatment components to enhance family effects, which in turn might enhance sustainability of individual change, such as reduced alcohol use.
Acknowledgements
I would like to acknowledge Kathy Sikkema, John Curry, and Brandon Kohrt, for their input, collaboration, and study support; Pryia Sridhar, for her data entry; Wilter Rono, and Franck Makumbi for their coordination, clinical abilities, and attention to detail.
Funding
This work was supported by Duke Global Health Institute, Duke Graduate School [no grant numbers], and National Institute of Health T32MH096724-09 directed by Dr. Milton Wainberg.
Footnotes
Registration
This trial was registered with ISRCTN registry (ID ISRCTN13038027).
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- mhGAP, W. H. O. (2016). Intervention Guide fpr mental, neurological and substance use disorders in non-speacialized health settings. Ve. [Google Scholar]
- Alcohol & Substance Misuse. (2019). Workplace health strategies by condition | workplace health promotion | CDC. https://www.cdc.gov/workplacehealthpromotion/health-strategies/substance-misuse/index.html. [Google Scholar]
- Arkowitz H, Miller W, & Rollnick S (2015). Motivational interviewing in the treatment of psychological problems. Guilford Publications. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, & Monteiro MGA (2001). The alcohol Use Disorders Identification test (AUDIT): guidelines for use in primary care. [Google Scholar]
- Braun V, & Clarke V (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. [Google Scholar]
- Bronfenbrenner U (1994). Ecological models of human development. Readings on the Development of Children, 2, 37–43. [Google Scholar]
- Charlet K, & Heinz A (2017). Harm reduction—a systematic review on effects of alcohol reduction on physical and mental symptoms. Addiction Biology, 22, 1119–1159. [DOI] [PubMed] [Google Scholar]
- Conger RD, et al. (2002). Economic pressure in African American families: A replication and extension of the family stress model. Developmental Psychology, 38, 179–193. [PubMed] [Google Scholar]
- Cuijpers P, Weitz E, Karyotaki E, Garber J, & Andersson G (2015). The effects of psychological treatment of maternal depression on children and parental functioning: A meta-analysis. Eur Child Adolesc Psychiatry, 24, 237–245. [DOI] [PubMed] [Google Scholar]
- Daughters, et al. (2008). Effectiveness of a brief behavioral treatment for inner-city illicit drug users with elevated depressive symptoms: The life enhancement treatment for substance use (LETS Act!). Journal of Clinical Psychiatry, 69, 122. [DOI] [PubMed] [Google Scholar]
- Dworkin SL, Treves-Kagan S, & Lippman SA (2013). Gender-transformative interventions to reduce HIV risks and violence with heterosexually-active men: A review of the global evidence. AIDS and Behavior, 17, 2845–2863. [DOI] [PubMed] [Google Scholar]
- Ellsberg M, & Heise L (2005). Researching violence against women: A practical guide for researchers and activists. (World health Organization ; program for Appropriate Technology in health (PATH). [Google Scholar]
- Erskine HE, et al. (2015). A heavy burden on young minds: The global burden of mental and substance use disorders in children and youth. Psychol Med, 45, 1551–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazzino TL, Bjorlie K, & Lejuez CW (2019). A systematic review of reinforcement-based interventions for substance use: Efficacy, mechanisms of action, and moderators of treatment effects. Journal of Substance Abuse Treatment, 104, 83–96. [DOI] [PubMed] [Google Scholar]
- Gibb SJ, Fergusson DM, & Horwood LJ (2010). Burden of psychiatric disorder in young adulthood and life outcomes at age 30. British Journal of Psychiatry, 197, 122–127. [Google Scholar]
- Gibbs A, Jewkes R, Willan S, & Washington L (2018). Associations between poverty, mental health and substance use, gender power, and intimate partner violence amongst young (18-30) women and men in urban informal settlements in South Africa: A cross-sectional study and structural equation model. PLOS ONE, 13, Article e0204956. [Google Scholar]
- Giusto A et al. Building community-based helping practices by training peer-father counselors: Conducting a Novel intervention to reduce drinking and depressed mood among fathers through a healthy masculinity lens. International Journal of Drug Policy (under review).. [Google Scholar]
- Giusto A, Ayuku D, & Puffer E (2020). An intervention to reduce alcohol use and improve family engagement for fathers in low-resource settings: Development and feasibility testing in Kenya. OSF. [Google Scholar]
- Giusto A, Green EP, Simmons RA, Ayuku D, Patel P, & Puffer ES (2020). A multiple baseline study of a brief alcohol reduction and family engagement intervention for fathers in Kenya. Journal of Consulting and Clinical Psychology, 88(8), 708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giusto A, & Puffer E (2018). A systematic review of interventions targeting men’s alcohol use and family relationships in low-and middle-income countries. Global Mental Health, 5. [Google Scholar]
- Goeke-Morey MC, & Mark Cummings E (2007). Impact of father involvement: A closer look at indirect effects models involving marriage and child adjustment. Applied Development Science, 11, 221–225. [Google Scholar]
- Greenfield TK, Karriker-Jaffe KJ, Kerr WC, Ye Y, & Kaplan LM (2016). Those harmed by others’ drinking in the US population are more depressed and distressed. Drug and Alcohol Review, 35, 22–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harnett PH, & Dawe S (2008). Reducing child abuse potential in families identified by social services: Implications for assessment and treatment. Brief Treatment and Crisis Intervention, 8, 226–235. [Google Scholar]
- Hilliard RB (1993). Single-case methodology in psychotherapy process and outcome research. Journal of Consulting and Clinical Psychology, 61, 373. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Huang W, Serrano D, Curran PJ, & Chassin L (2012). Testing whether and when parent alcoholism Uniquely affects Various Forms of adolescent substance Use. Journal of Abnormal Child Psychology, 40, 1265–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaguga F, & Kwobah E (2020). A review of the public sector substance use disorder treatment and prevention systems in Kenya. Substance Abuse Treatment, Prevention, and Policy, 15, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes R, Sikweyiya Y, Morrell R, & Dunkle K (2011). Gender inequitable masculinity and sexual entitlement in rape perpetration South Africa: Findings of a cross-sectional study. PLoS ONE, 6, Article e29590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, et al. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National comorbidity survey replication. Archives of General Psychiatry, 62, 593–602. [DOI] [PubMed] [Google Scholar]
- Kessler RC, et al. (2011). Development of lifetime comorbidity in the World Health Organization world mental health surveys. Archives of General Psychiatry, 68, 90–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kieling C, et al. (2011). Child and adolescent mental health worldwide: Evidence for action. Lancet, 378, 1515–1525. [DOI] [PubMed] [Google Scholar]
- Kohn R, Saxena S, Levav I, & Saraceno B (2004). The treatment gap in mental health care. Bulletin of the World Health Organization, 82, 858–866. [PMC free article] [PubMed] [Google Scholar]
- Leonard KE, & Eiden RD (2007). Marital and family processes in the context of alcohol use and alcohol disorders. Annu Rev Clin Psychol, 3, 285–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masarik AS, & Conger RD (2017). Stress and child development: A review of the family stress model. Current Opinion in Psychology, 13, 85–90. [DOI] [PubMed] [Google Scholar]
- McHugh ML (2012). Interrater reliability: The kappa statistic. Biochem Med (Zagreb), 22, 276–282. [PMC free article] [PubMed] [Google Scholar]
- Mokdad AH, et al. (2016). Global burden of diseases, injuries, and risk factors for young people’s health during 1990–2013: A systematic analysis for the global burden of disease study 2013. The Lancet, 387, 2383–2401. [Google Scholar]
- NACADA. (2017). National ADA survey report. https://www.nacada.go.ke/sites/default/files/2019-10/National%20ADA%20Survey%20Report%202017_2_2.pdf.
- Nadkarni A, et al. (2017). Counselling for alcohol problems (CAP), a lay counsellor-delivered brief psychological treatment for harmful drinking in men, in primary care in India: A randomised controlled trial. The Lancet, 389, 186–195. [Google Scholar]
- Neger EN, & Prinz RJ (2015). Interventions to address parenting and parental substance abuse: Conceptual and methodological considerations. Clinical Psychology Review, 39, 71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Murphy CM, Stephan SH, Fals-Stewart W, & Murphy M (2004). Partner violence before and after couples-based alcoholism treatment for male alcoholic patients: The role of treatment involvement and abstinence. Journal of Consulting and Clinical Psychology, 72, 202–217. [DOI] [PubMed] [Google Scholar]
- Orford J, Copello A, Velleman R, & Templeton L (2010a). Family members affected by a close relative’s addiction: The stress-strain-coping-support model. Drugs: Education, Prevention and Policy, 17, 36–43. [Google Scholar]
- Orford J, Velleman R, Copello A, Templeton L, & Ibanga A (2010b). The experiences of affected family members: A summary of two decades of qualitative research. Drugs: Education, Prevention and Policy, 17, 44–62. [Google Scholar]
- Orford J, Velleman R, Natera G, Templeton L, & Copello A (2013). Addiction in the family is a major but neglected contributor to the global burden of adult ill-health. Social Science & Medicine, 78, 70–77. [DOI] [PubMed] [Google Scholar]
- Panter-Brick C, et al. (2014). Practitioner Review: Engaging fathers - recommendations for a game change in parenting interventions based on a systematic review of the global evidence. Journal of Child Psychology and Psychiatry, 55, 1187–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puffer ES, Friis-Healy EA, Giusto A, Stafford S, & Ayuku D (2019). Development and implementation of a family therapy intervention in Kenya: A community-embedded lay provider model. Glob Soc Welf. 10.1007/s40609-019-00151-6 [DOI] [Google Scholar]
- Puffer ES, Friis-Healy EA, Giusto A, Stafford S, & Ayuku D (2021). Development and implementation of a family therapy intervention in Kenya: A community-embedded lay provider model. Global Social Welfare, 8(1), 11–28.Chicago. [Google Scholar]
- QRS International Pty Ltd. (2018). NVivo (Version 12).
- Rehm J, et al. (2009). Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet, 373, 2223–2233. [Google Scholar]
- Sameroff A (1975). Transactional models in early social relations. Human Development, 18, 65–79. [Google Scholar]
- Saunders JB, Aasland OG, Amundsen A, & Grant M (1993). Alcohol consumption and related problems among primary health care patients: WHO collaborative project on early detection of persons with harmful alcohol consumption—I. Addiction, 88, 349–362. [DOI] [PubMed] [Google Scholar]
- Schacht PM, Cummings EM, & Davies PT (2009). Fathering in family context and child adjustment: A longitudinal analysis. Journal of Family Psychology, 23, 790–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solis JM, Shadur JM, Burns AR, & Hussong AM (2012). Understanding the diverse needs of children whose parents abuse substances. Current Drug Abuse Reviews, 5, 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stover CS (2015). Fathers for change for substance use and intimate partner violence: Initial community pilot. Family Process, 54, 600–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundin E, Galanti MR, Landberg J, & Ramstedt M (2021). Severe harm from others’ drinking: A population-based study on sex differences and the role of one’s own drinking habits. Drug and Alcohol Review, 40, 263–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegs C, Creanga AA, Galavotti C, & Wamalwa E (2016). Community dialogue to shift social norms and enable family planning: An evaluation of the family planning results initiative in Kenya. PLOS ONE, 11 , Article e0153907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Forum on alcohol, drugs and addictive behaviours. Alcohol and drug use disorders: Global Health Estimates. https://www.who.int/substance_abuse/activities/fadab/msb_adab_2017_GHE_23June2017.pdf, (2017).
- Witkiewitz K, Donovan DM, & Hartzler B (2012). Drink refusal training as part of a combined behavioral intervention: Effectiveness and mechanisms of change. J Consult Clin Psychol, 80, 440–449. [DOI] [PMC free article] [PubMed] [Google Scholar]


