Abstract
Introduction
When delivered in person, yoga has been shown to be effective in managing irritable bowel syndrome (IBS) symptoms. Research is needed to test the feasibility and effectiveness of yoga as a therapeutic option when delivered virtually. The primary aim of the mind and yoga for IBS randomised controlled trial is to determine the effects of an 8-week virtual meditation and yoga intervention on IBS symptom severity compared with an advice-only active control group.
Methods and analysis
Adults diagnosed with IBS will be randomised to receive either a Upa Yoga intervention or an advice-only control group. The intervention will consist of weekly online classes for 8 weeks delivered by a facilitator using Microsoft Office Teams and daily home practice. Feasibility will be evaluated by examining recruitment and attrition rates, adherence, participant satisfaction with the programme and safety. The primary outcome is IBS symptom severity, and key secondary outcomes include (but not limited to) quality of life, anxiety and depression symptoms, COVID-19-related stress and anxiety, and fatigue. Outcomes will be assessed at baseline, 4 weeks and 8 weeks. An embedded design experimental model substudy will be conducted post intervention using qualitative research methods to identify participants’ experiences in the yoga programme.
Ethics and dissemination
This study has been approved by the Conjoint Health Research Ethics Board (REB ID 20-0084). Findings will be disseminated through peer-reviewed publication, conference presentation and social media.
Trial registration number
Keywords: Clinical trials, Functional bowel disorders, MENTAL HEALTH
Strengths and limitations of this study
Mixed methods study composed of a randomised controlled trial and interviews.
First virtual yoga interventions in irritable bowel syndrome.
Canada-wide recruitment.
Self-reported outcome measures.
Lack of data capture on the frequency of yoga practice in the control group.
Introduction
Stress is a physical, mental or emotional response that causes tension in the mind or the body.1 Altered stress response from psychological and physiological mechanisms may contribute to altered brain–gut signalling patterns and irritable bowel syndrome (IBS) symptoms. Psychological stressors, such as depression and anxiety, may influence gut function (eg, reduced motility). Physiological stressors (eg, infection) in the gut may affect the brain.2 Therapies focusing on mind–body interactions and stress reduction may be adjunctive treatments for IBS. Stress management techniques that include both mind and body interventions such as yoga3 have been effective in improving IBS symptom severity and mental health outcomes.3 4 Mind–body interventions may modulate the brain–gut axis directly by reducing sympathetic activity and increasing parasympathetic activity and the hypothalamus–pituitary–adrenal axis.5
Yoga is a traditional mind–body–breath discipline that includes a triad of postures, structured breathing and meditation.6 Our recent review7 identified four randomised controlled trials that examined traditional yoga practice as therapy for patients with IBS.8–11 These trials demonstrated that yoga was more effective compared with pharmacological treatment and equally effective as dietary interventions or moderate-intensity walking. Physical and mental health improvements included IBS symptom severity, gastric motility and depression.
Research is needed to determine the feasibility and effectiveness of virtual yoga programming as a therapeutic option for patients with IBS. The rationale for virtually delivered interventions to manage IBS is increasing due to rising demand, limited healthcare resources and cost-effectiveness.12 13 A recent review found virtual care tools may be effective in managing disease activity and improving outcomes in patients with digestive diseases.14 This review also highlighted the high acceptability and satisfaction with virtual care among patients with IBS.15–19
The primary objective of the meditation and yoga for irritable bowel syndrome (MY-IBS) study is to explore the feasibility and effectiveness of a virtual yoga programme for patients with IBS. MY-IBS is a mixed-method study including a randomised controlled trial and semistructured interviews. The primary aim of this randomised controlled trial is to determine the effects of an 8-week virtual yoga intervention on IBS symptom severity, measured with the IBS Symptoms Severity Scale, compared with an advice-only control group. Secondary aims are to determine whether (1) a yoga programme delivered virtually is feasible for adults with IBS, (2) improves health outcomes including quality of life (QOL), stress and fatigue and (3) improves mental health outcomes including depression and anxiety symptoms. An embedded design experimental model qualitative substudy using semistructured interviews will explore and describe participants’ experiences in the yoga programme, and its impact. We hypothesise that the programme will be feasible and effective in improving outcomes in the intervention group compared with the control group.
Methods and analysis
Study design overview
The quantitative study is a superiority randomised non-blinded two-group controlled trial. The qualitative study will use semistructured interviews and thematic analysis to explore and describe intervention participant experiences and views of the yoga programme.
Patient involvement
Patients with lived experience were involved in the conduct of this study. During the development stage, patient partners were invited to participate in a series of discussions with the research team to define the study research question, study design, choice of outcome measures and methods of recruitment. Following the completion of the trial, the patient partners will be involved in the dissemination of this research.
Sample and selection
The MY-IBS study will be conducted at the University of Calgary in Alberta, Canada starting March 2021 and ending early 2022. To be eligible in this study, participants must be diagnosed with IBS based on Rome IV criteria by a healthcare professional (eg, physician, nurse, dietician), be 18–70 years old, have an adequate understanding of English, have an ability to provide written informed consent, score at least 75 out 500 points on the IBS Symptoms Severity Scale indicating mild IBS symptoms, and be on stable doses of medications for IBS (including antidepressants) without major changes to diet or physical activity levels for at least 8 weeks prior to starting the intervention. Individuals across Canada are eligible to participate. Exclusion criteria include a major physical impairment that would prevent the individual from doing yoga determined by either the patient or the study coordinator, and diagnosis of any major cognitive, psychological or psychiatric disorder (eg, major depression, schizophrenia) as identified by the treating physician or healthcare practitioner or screened by the study coordinator using the Patient Health Questionnaire-9 (PHQ-9).
Participants will be identified through (1) gastroenterology clinics across Calgary, Alberta; (2) gastroenterologists across Canada who indicated interest in this study for their patients with IBS in a previous survey conducted by our team (not published); (3) participants from the previous survey who indicated interest in this study and have given consent to be contacted; (4) through social media; (5) self-referrals through the study website and the University of Calgary participate in research portal; (6) Canadian Association of Gastroenterologists monthly newsletter; and (7) participants with IBS who are enrolled in the Inflammation, Microbiome and Alimentation Gastro-intestinal and Neuropsychiatric Effects (IMAGINE) cohort study at the University of Calgary and have given their consent to be contacted for future studies.
Participant screening will use the PHQ-9. Individuals who score 20 points or higher on the PHQ-9 indicating severe depression will not be eligible to participate. Reasons for exclusion are lack of compliance in interventional studies among these individuals, potential heterogeneity in the small sample size of participants and skewed results if patients seek treatment for their depression during the trial.
Interventions
Yoga intervention group
Before their first class, the intervention group will receive an introductory video. The video will consist of information on IBS, information on the style of yoga they will be learning, and rationale for yoga as a treatment for IBS. The intervention will be delivered online by a certified yoga facilitator in class sizes of less than 10 participants using the Microsoft Office Teams platform. Classes will be held once per week for the 8-week duration. The first session will be approximately 90 min and subsequent sessions up to 60 min. The introductory session will include the class setup, introductions, teaching poses, corrections and a question and answers period. The yoga facilitator will provide participants with modifications for common challenges to support best practices and ensure safety. Subsequent classes will include a review from the previous week, a question and answer period, individual corrections and modifications and introduce new practices. In addition to the online class component, study staff will ask participants to practice the yoga programme at home every day. They will also have access to the yoga videos, written programme instructions and frequently answered questions accessible through the study website to help support their home practice (https://cumming.ucalgary.ca/research/ascend/resources/patient-resources/my-ibs).
Upa Yoga, developed by the Isha Foundation of Inner Sciences (https://isha.sadhguru.org/us/en), will be promoted. Upa Yoga maintains the ancient principles of Hatha Yoga and will be delivered by a certified yoga facilitator from the Isha Foundation. The Upa Yoga programme will consist of (1) directional movements and neck rotations, (2) hatha yoga-based Yoga Namaskar, (3) breathing practices or alternate nostril breathing, (4) mantra meditation consisting of AUM chanting (OM) and (5) breath watching. Table 1 shows a description of the programme and rationale. Our published prospective study examining the effectiveness of Upa Yoga in patients with inflammatory bowel disease20 shows improvements in mental health scores after an 8-week yoga programme.
Table 1.
Overview of the Upa Yoga programme
| Programme component | Description | Rationale |
| Directional movement of the arms | This practice involves extending the arms in four directions (sideways, front, up and down) by rotating the wrists, while consciously focusing on the inhalation and exhalation of breath with each movement. | Studies show that fibromyalgia is common among patients living with IBS.30 This could lead to pain of the muscles and joints, fatigue, and sleep concerns. The principle behind this practice is to lubricate the fluids in the joints, increase circulation and activate the energy nodes in these joints. Doing these practices everyday can relieve muscle and joint stiffness and reduce pain over time. This practice is recommended by the Isha Foundation to increase strengths and flexibility in preparation for Yoga Namaskar. |
| Neck practices | There are five sets of neck practices, each stretching the neck and final one working on the shoulder area. | The main cause of neck pain is usually muscle tension. Perceived stress can increase muscle tension. These neck exercises help relieve stress that can aggravate IBS symptoms. This practice is recommended by the Isha Foundation to increase strengths and flexibility in preparation for Yoga Namaskar. |
| Yoga Namaskar | This practice involves a series of seven consecutive steps of upper body stretching and squatting, aligned with breath. | This practice activates the lumbar region of the spine and strengthens the spinal muscles.31While Yoga Namaskar has not been specifically studied in patients with IBS, yoga squatting postures have been associated with significant decrease in depression among nine individuals with IBD20 and anxiety in a randomised self as control study in 30 healthy subjects.32 |
| Alternate nostril breathing (Nadi Shuddhi) | The participant sits cross-legged with the spine comfortably erect and eyes closed. Closing the right nostril with the thumb, inhaling and exhaling through the left nostril. This is repeated on the right nostril by closing the left nostril with the ring finger. | Alternate nostril breathing is traditionally considered to alleviate mental unrest and promote physical and mental balance.33 34 It has been demonstrated to decrease perceived stress and improve autonomic function in a randomised control trial compared with control subjects in healthy male volunteers, and decreased state anxiety in a prospective study.35 36 |
| Mantra meditation (AUM chanting) | The participants sit cross-legged, and with eyes closed, uttering each of these 3 sounds 7 times. The important aspect to this utterance is the awareness of the reverberations each of the sounds produces in the corresponding parts of the body: a—below the navel, o—mid-point of the chest, m—pit of the throat. | This mantra is thought to facilitate energy flow, and through vibratory mechanisms, creates peace and harmony leading to increased mental alertness and may improve symptoms of depression.37 38 |
| Breath watching | The participants sit cross-legged with eyes closed and hold a hand gesture called the Yoga Mudra (the tips of the thumb and index finger come together forming a circle). They are instructed to maintain a gentle focus on the mid-point between both eyebrows (at the level of the pineal gland), while being conscious of the gentle movement of breath happening in their body. | Breathing in a focused manner can be used as a tool to promote positive changes to the mind, body and emotions.39 Significant reduction in the level of state anxiety was found in a group of healthy male volunteers when they practised breath awareness.16 |
IBS, irritable bowel syndrome.
Advice-only control group
Control participants will receive a video including general education on irritable bowel syndrome (IBS), the mind–gut connection in IBS, and the role of mind–body therapies in the management of IBS. These participants will also receive a list of IBS-related resources from the Canadian Digestive Health Foundation, a link to a patient with IBS support group (www.ibspatient.org), and information about physical activity guidelines from the WHO. Control participants will be eligible to attend a 2-week yoga programme and receive the yoga videos 8 weeks from the time of enrolment. Data on these participants will not be collected as this participation option is for participants who desire to receive the yoga sessions outside of the study.
Outcome measures
Feasibility outcomes
Recruitment, attendance and attrition rates
Recruitment will be calculated by the percentage of participants who complete the eligibility and enrollment phases of the study. Attrition will be calculated by the percentage of participants who complete all study measures at baseline and 8 weeks. A feasible intervention will be defined as class attendance of at least 75% (ie, attendance in 6 out of 8 classes)9 and attrition rate of less than 30%.
Adherence
Adherence will be defined as practicing daily yoga for at least 80% of days for 8 weeks (or 45 out of 56 days minimum). Each week a practice log will be provided to monitor frequency and length of yoga. The yoga facilitator will take attendance during each online class. To increase programme adherence, the study coordinator will email intervention participants weekly. Six months following the completion of the intervention, participants will be asked to report the average frequency (ie, days per month) and duration (ie, minutes) of their yoga practices over the last 7 days to evaluate long-term maintenance.
Programme satisfaction
Intervention participants will complete a survey regarding overall satisfaction with their programme, including satisfaction with videos and online class instruction. Videos and online classes will be deemed acceptable if at least 70% of participants are at least satisfied (ie, rank classes as either good, great or excellent). Participants will also indicate whether they would recommend the programme to others on a scale from 1 (strongly disagree) to 7 (strongly agree) and provide feedback on how the programme could be improved.
Assessment of harms
The study coordinator will screen potential participants and exclude those with any physical problems that may limit participation with yoga postures. Participants will be asked to report any adverse events experienced during the study period. Participants with adverse events (eg, injury resulting from the programme) will be advised to consult their physician to provide care as appropriate.
Effectiveness outcomes
The primary outcome, IBS symptoms, will be measured using the IBS-Symptom Severity Scale (IBS-SSS). The IBS-SSS is a five-question survey that asks the severity of abdominal pain, frequency of abdominal pain, severity of abdominal distention, dissatisfaction with bowel habits and interference with QOL over the past 10 days. Scores on the IBS-SSS range from 0 to 500 with higher scores indicating more severe symptoms. Participants can be categorised as having mild (75–175), moderate (175–300) or severe (>300) IBS. Symptom reduction of at least 50 points is considered clinically meaningful.
Secondary outcomes (and their measures) include QOL (IBS-QOL), anxiety (Generalised Anxiety Disorder-7), depression (PHQ-9), stress (Perceived Stress Scale), COVID-19 stress (COVID-19 Stress Scale), fatigue (Modified Fatigue Impact Scale-21), somatic Symptoms (PHQ-15) and self-compassion (Self Compassion Scale-Short Form) (1online supplemental table 1). Intention to practice yoga will also be assessed. The intervention and control groups will be assessed on effectiveness outcomes at baseline, 4 and 8 weeks. The intervention group will complete measures of effectiveness outcomes 6 months after the intervention.
bmjopen-2021-059604supp001.pdf (58.4KB, pdf)
Sample size
We will recruit 25 participants per group. However, assuming 30% attrition rate, we will aim to recruit 33 participants per group. Symptom reduction of at least 50 points is considered clinically meaningful; however, a group difference has been shown to represent a considerable self-reported improvement.21 We calculated the sample size using a mean difference of at least 83 points on the IBS-SSS (⍺=0.05, β=0.80, SD of 103.8).9
Randomisation, treatment allocation and blinding
Study flow is shown in figure 1. The study coordinator will obtain consent from participants who will then be enrolled in the study. Participants will be randomised after baseline assessment to either the yoga intervention or the advice-only control group. A statistician blinded to the randomisation key will create a computer-generated REDCap randomised sequence to allocate participants based on gender (1:1:1 male:female:other) and depression (1:1 depression:no depression). Participants will be aware of the group to which they are allocated; however, the principal investigator and data analyst will remain blinded to the randomisation process.
Figure 1.
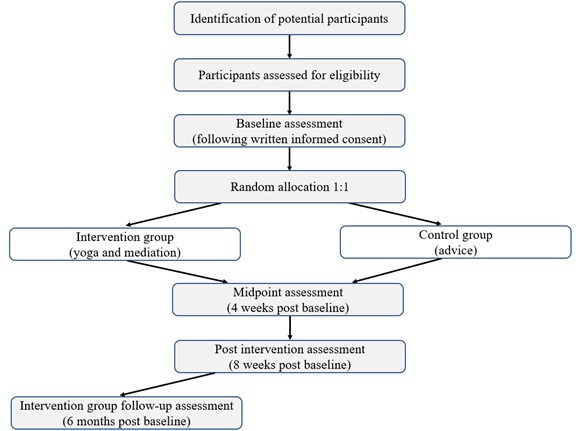
Participant flow chart based on the Consolidated Standards of Reporting Trials guidelines.
Data management
All quantitative data will be entered into a secure REDCap database at the University of Calgary. Effectiveness outcome measures, programme satisfaction, attendance and adherence will be entered by the participants. Recruitment, attrition and safety will be recorded by the study coordinator who is not blinded to the randomisation. After the study, data will be downloaded, and patient identifiers will be removed from the data file. Data will be stored in a password-protected file on a University of Calgary password-protected computer. The interviews will be transcribed, deidentified and uploaded to the University of Calgary’s secure SharePoint site. Only the research team will have access to the data.
Statistical analysis
Descriptive analysis will summarise participant characteristics and feasibility outcomes. Univariate analysis of variance (ANOVA) will examine baseline differences between groups for variables with continuous data. χ2 tests will examine baseline differences between groups for categorical variables. Unadjusted ANOVA and adjusted analysis of covariance models will compare differences in scores from baseline and postintervention data within and between groups using intent to treat and per-protocol analysis. A logistic regression—model examining determinants of responders (a minimum improvement of at least 50 points on the IBS-SSS scale) versus non-responders will be developed to predict a response to the intervention. This model will consider practice in minutes, baseline depression, anxiety and IBS symptom severity scores. An α of 0.05 will be the threshold for determining statistical significance. If the frequency of missing data is >5%, we will perform additional analyses using imputation methods. Analysis will be conducted using SPSS V.26.
Postintervention interviews
Participants who were randomised to the intervention and did not withdraw from the study will be invited by email to participate in an interview. We aim to recruit men and women and have equal representation of those who benefited from the programme (ie, experienced improvements in their IBS symptom severity) as well as individuals who did not. We anticipate needing to interview between 10 and 15 participants to reach both code and meaning saturation22 aiming for a maximum variation sample.
Semistructured interviews will capture participants’ experiences, programme satisfaction, facilitators and barriers to participation, perceptions of social support and supervised learning, perceived impact on IBS symptoms and overall physical and mental health, and input on improving future programming (box 1). Interviews will happen virtually using Microsoft Office Teams and be approximately 30–45 min in length. The study coordinator will interview the participants, take notes during the interview and reflect following each interview. Interview recordings will be transcribed verbatim without identifying information. Data will be coded and analysed in duplicate using NVivo V.12. Thematic analysis inductively reveals patterns and themes providing an understanding of participant experiences, with the programme and their perspectives on its impact. Thematic analysis is a method for systematically identifying, organising and offering insight into patterns of meaning (themes) across a data set.23 This method makes sense of shared meanings and experiences that allows the researcher to identify what data are important to the research question.24
Box 1. Semistructured interview questions and probes.
1. Whatwhat have you done in the past to manage your irritable bowel syndrome (IBS)?
Have you tried yoga or mediation?
Have you tried exercise?
2. I would like to start by asking you what you were hoping for or expecting from the programme?
Why did you join this study?
Did anyone influence your decision to join?
Did that meet your expectations?
3. Next, I would like to discuss your overall experience in the meditation and yoga for IBS yoga programme in which you participated. Could you describe for me what participating in this programme was like for you?
Subquestions: yoga facilitator/supervision, the timing of sessions/scheduling, length of sessions, attending with other members, online experience vs in-person, social support/other participants.
What did you like most about it?
What didn’t you like?
Did this change over the course of the programme?
What was that like?
What stood out for you?
What emotions were you aware of at the time?
What else do you remember about that experience?
4. How has participating in this programme affected how you manage or live with your IBS?
Subquestions: change in IBS symptoms; physical health, fatigue; mental health—stress, anxiety, depression; feeling better about myself; ability to live with my IBS.
Tell me more about that.
Can you give me an example of what you mean?
How has that affected you?
5. What, if anything, has helped you to do your practices at home?
Subquestions : social support, family support, convenience
Tell me more about that.
Can you give me an example of what you mean?
How has that affected you?
6. What challenges did you have, if any, doing your practices at home?
Subquestions : family, supervision/safety, schedule/time
Are you satisfied with how you did?
Tell me more about that.
Can you give me an example of what you mean?
How has that affected you?
7. What, if anything, has helped you to attend the weekly online class?
Subquestions : social support, family support, HCP support, yoga facilitator, supervision/safety, online classes, schedule/length
Tell me more about that.
Can you give me an example of what you mean?
How has that affected you?
8. What challenges did you have, if any, to attend the weekly online class?
Subquestions : social support, family, yoga facilitator, supervision/safety, online classes, schedule, technical difficulties
Are you satisfied with how you did?
Tell me more about that.
Can you give me an example of what you mean?
How has that affected you?
9. We are interested in any ideas you have about how we might make this programme better. What could we do differently?
Subquestions: content, timing, facilitator, videos, website, delivery, other supports
Would you explain that further?
Can you give me an example of what you mean?
10.Based on your experience with yoga, would you incorporate yoga to help manage your IBS? If so, how?
11.Before we conclude, is this anything else you would like to say about your experience with this programme, that we have not had a chance to talk about yet?
Discussion
The MY-IBS study aims to determine the feasibility and effectiveness of an 8-week virtual yoga and meditation programme combined with home-based practice for patients with IBS. Determining feasibility will be based on study recruitment, adherence, safety and programme satisfaction. Improved IBS symptom management (the primary outcome) will determine intervention effectiveness. Secondary outcomes include QOL, stress, fatigue, depression, anxiety, COVID-19-related stress and anxiety and self-compassion. These findings will inform potential predictors of responders versus non-responders. Predictors may be considered in clinical practice to target the patients with IBS most likely to benefit from the yoga intervention. Interview themes and patterns will refine and inform the development of future virtual yoga programming designed for patients with IBS.
To our knowledge, there are no studies of virtual yoga and meditation in the IBS population. The findings from this study may have implications for the management of IBS. The virtual delivery of yoga represents an opportunity to increase access to effective management therapies for patients with IBS. The COVID-19 pandemic has called for the reorganisation of healthcare including utilisation of virtual care. Nearly 90% of care in the USA has been delivered virtually since the pandemic.25 Due to the COVID-19 pandemic, there is increased psychological distress and gastrointestinal symptoms among individuals with IBS26 27 compared with individuals without IBS.28 The present study offers a unique opportunity to examine prospectively the feasibility and effectiveness of a yoga and meditation programme delivered virtually to individuals living with IBS with the COVID-19 pandemic restrictions taken into consideration. Study findings may aid in developing interventions and services tailored to patients with IBS. New insight into outcomes will be beneficial for healthcare leaders in planning how to allocate existing resources to support these services and potentially lessen the burden of IBS on both the individual and the healthcare system.
Ethics and dissemination
Ethics
The study protocol, informed consent form and other study documents were reviewed and approved by the University of Calgary’s ethics board. All protocol modifications will be submitted for review and approval by the ethics board. The trial participants will be informed of any modifications, and reconsented by the study coordinator, if required. Further, the trial registry for this study will be updated.
Participation is voluntary and will not influence standard clinical care. All participants will provide informed written consent and have the right to withdraw from the study at any time. Pending consent from the participant, all data collected up to the time of withdrawal will be used in the final data analyses as advised by the Consolidated Standards of Reporting Trials guidelines.29
Dissemination
Our targeted knowledge users and audiences will include researchers, healthcare professionals and service providers, persons with lived experiences, community groups and professional organisations (eg, Canadian Association of Gastroenterology). Our goal will be to increase topic area knowledge among these groups and inform future research. Our strategies will include conference presentations, publication in a peer-reviewed journal, social media campaigns, development of virtually delivered tools such as mobile applications to increase accessibility and affordability and educational material distributed through the Digestive Health Foundation, IMAGINE SPOR Chronic Disease Network and Primary Care Networks across Alberta.
Supplementary Material
Footnotes
Contributors: AD'S is involved in all aspects of protocol design and lead author of the manuscript. DAM, JV, YN, VR and GMK assisted with design of the protocol respective to their expertise. DAM and GMK assisted with the qualitative aspects of the protocol. JKV lead the statistical aspects of the protocol. YN provided their clinical expertise and patient recruitment thought the clinic. VR provided their expertise in yoga therapy. MR is the senior author on the protocol and has guided the work of this research to support AD'S with their training. All authors reviewed the manuscript for study design and provided critical insight into manuscript content and approved the final version for submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: DM receives partial salary support through the Arthur J.E. Child Chair.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Crosswell AD, Lockwood KG. Best practices for stress measurement: how to measure psychological stress in health research. Health Psychol Open 2020;7:205510292093307. 10.1177/2055102920933072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mayer EA, Labus JS, Tillisch K, et al. Towards a systems view of IBS. Nat Rev Gastroenterol Hepatol 2015;12:592–605. 10.1038/nrgastro.2015.121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schumann D, Anheyer D, Lauche R, et al. Effect of Yoga in the Therapy of Irritable Bowel Syndrome: A Systematic Review. Clin Gastroenterol Hepatol 2016;14:1720–31. 10.1016/j.cgh.2016.04.026 [DOI] [PubMed] [Google Scholar]
- 4.Ballou S, Keefer L. Psychological interventions for irritable bowel syndrome and inflammatory bowel diseases. Clin Transl Gastroenterol 2017;8:e214. 10.1038/ctg.2016.69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kavuri V, Raghuram N, Malamud A, et al. Irritable bowel syndrome: yoga as remedial therapy. Evid Based Complement Alternat Med 2015;2015:1–10. 10.1155/2015/398156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brems C, Colgan D, Freeman H, et al. Elements of yogic practice: perceptions of students in healthcare programs. Int J Yoga 2016;9:121. 10.4103/0973-6131.183710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D'Silva A, MacQueen G, Nasser Y, et al. Yoga as a therapy for irritable bowel syndrome. Dig Dis Sci 2020;65:2503-2514. 10.1007/s10620-019-05989-6 [DOI] [PubMed] [Google Scholar]
- 8.Taneja I, Deepak KK, Poojary G, et al. Yogic versus conventional treatment in diarrhea-predominant irritable bowel syndrome: a randomized control study. Appl Psychophysiol Biofeedback 2004;29:19–33. 10.1023/B:APBI.0000017861.60439.95 [DOI] [PubMed] [Google Scholar]
- 9.Kavuri V, Selvan P, Malamud A, et al. Remedial yoga module remarkably improves symptoms in irritable bowel syndrome patients: a 12-week randomized controlled trial. Eur J Integr Med 2015;7:595–608. 10.1016/j.eujim.2015.11.001 [DOI] [Google Scholar]
- 10.Shahabi L, Naliboff BD, Shapiro D. Self-regulation evaluation of therapeutic yoga and walking for patients with irritable bowel syndrome: a pilot study. Psychol Health Med 2016;21:176–88. 10.1080/13548506.2015.1051557 [DOI] [PubMed] [Google Scholar]
- 11.Schumann D, Langhorst J, Dobos G, et al. Randomised clinical trial: yoga vs a low-FODMAP diet in patients with irritable bowel syndrome. Aliment Pharmacol Ther 2018;47:203–11. 10.1111/apt.14400 [DOI] [PubMed] [Google Scholar]
- 12.Hanlon I, Hewitt C, Bell K, et al. Systematic review with meta-analysis: online psychological interventions for mental and physical health outcomes in gastrointestinal disorders including irritable bowel syndrome and inflammatory bowel disease. Aliment Pharmacol Ther 2018;48:244–59. 10.1111/apt.14840 [DOI] [PubMed] [Google Scholar]
- 13.Knowles SR, Mikocka-Walus A. Utilization and efficacy of internet-based eHealth technology in gastroenterology: a systematic review. Scand J Gastroenterol 2014;49:387–408. 10.3109/00365521.2013.865259 [DOI] [PubMed] [Google Scholar]
- 14.Helsel BC, Williams JE, Lawson K, et al. Telemedicine and mobile health technology are effective in the management of digestive diseases: a systematic review. Dig Dis Sci 2018;63:1392–408. 10.1007/s10620-018-5054-z [DOI] [PubMed] [Google Scholar]
- 15.Dorn SD, Palsson OS, Woldeghebriel M, et al. Development and pilot testing of an integrated, web-based self-management program for irritable bowel syndrome (IBS). Neurogastroenterol Motil 2015;27:128–34. 10.1111/nmo.12487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Everitt H, Moss-Morris R, Sibelli A. Management of irritable bowel syndrome in primary care: the results of an exploratory randomised controlled trial of mebeverine, methylcellulose, placebo and a self-management website. BMC Gastroenterol 2012;13:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hunt MG, Moshier S, Milonova M. Brief cognitive-behavioral Internet therapy for irritable bowel syndrome. Behav Res Ther 2009;47:797–802. 10.1016/j.brat.2009.05.002 [DOI] [PubMed] [Google Scholar]
- 18.Ljótsson B, Andersson G, Andersson E, et al. Acceptability, effectiveness, and cost-effectiveness of Internet-based exposure treatment for irritable bowel syndrome in a clinical sample: a randomized controlled trial. BMC Gastroenterol 2011;11:110. 10.1186/1471-230X-11-110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ljótsson B, Falk L, Vesterlund AW, et al. Internet-delivered exposure and mindfulness based therapy for irritable bowel syndrome--a randomized controlled trial. Behav Res Ther 2010;48:531–9. 10.1016/j.brat.2010.03.003 [DOI] [PubMed] [Google Scholar]
- 20.Kaur S, D'Silva A, Rajagopalan V, et al. Evaluation of an integrated yoga program in patients with inflammatory bowel disease: a pilot study. Explore 2022;18:335–41. 10.1016/j.explore.2021.04.006 [DOI] [PubMed] [Google Scholar]
- 21.Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther 1997;11:395–402. 10.1046/j.1365-2036.1997.142318000.x [DOI] [PubMed] [Google Scholar]
- 22.Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation: how many interviews are enough? Qual Health Res 2017;27:591–608. 10.1177/1049732316665344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 24.Braun V, Clarke V. Can I use TA? Should I use TA? Should I not use TA? Comparing reflexive thematic analysis and other pattern‐based qualitative analytic approaches. Couns Psychother Res 2021;21:37–47. 10.1002/capr.12360 [DOI] [Google Scholar]
- 25.Kendzerska T, Zhu DT, Gershon AS, et al. The effects of the health system response to the COVID-19 pandemic on chronic disease management: a narrative review. Risk Manag Healthc Policy 2021;14:575–84. 10.2147/RMHP.S293471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kamp KJ, Levy RL, Munson SA. Impact of COVID-19 on individuals with irritable bowel syndrome and comorbid anxiety and/or depression. J Clin Gastroenterol 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oshima T, Siah KTH, Yoshimoto T. Impacts of the COVID2019 pandemic on functional dyspepsia and irritable bowel syndrome: a population-based survey. J Gastroenterol Hepatol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sabate J-M, Deutsch D, Melchior C, et al. COVID-19 pandemic and lockdown stress consequences in people with and without irritable bowel syndrome. Ethics Med Public Health 2021;18:100660. 10.1016/j.jemep.2021.100660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 2010;63:e1–37. 10.1016/j.jclinepi.2010.03.004 [DOI] [PubMed] [Google Scholar]
- 30.Erdrich S, Hawrelak JA, Myers SP, et al. A systematic review of the association between fibromyalgia and functional gastrointestinal disorders. Therap Adv Gastroenterol 2020;13:1756284820977402. 10.1177/1756284820977402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vasudev SJ. Benefits of yoga Namaskar, 2021. Available: https://isha.sadhguru.org/ca/en/yoga-meditation/yoga-program-for-beginners/yoga-for-overall-wellbeing2021
- 32.Chandrasekeran A, Rajesh SK, Srinivasan T. Effect of repetitive yogic squats with specific hand position (Thoppukaranam) on selective attention and psychological states. Int J Yoga 2014;7:76–9. 10.4103/0973-6131.123497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cramer H, Lauche R, Klose P, et al. Yoga for schizophrenia: a systematic review and meta-analysis. BMC Psychiatry 2013;13:32. 10.1186/1471-244X-13-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saraswati SMS. S.S. Hatha yoga Pradipika. Munger, India, Bihar: Bihar School of Yoga, 1985. [Google Scholar]
- 35.Naik GS, Gaur GS, Pal GK. Effect of modified slow breathing exercise on perceived stress and basal cardiovascular parameters. Int J Yoga 2018;11:53–8. 10.4103/ijoy.IJOY_41_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Telles S, Vishwakarma B, Gupta RK, et al. Changes in shape and size discrimination and state anxiety after Alternate-Nostril yoga breathing and breath awareness in one session each. Med Sci Monit Basic Res 2019;25:121–7. 10.12659/MSMBR.914956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Telles S, Nagarathna R, Nagendra HR. Autonomic changes during "OM" meditation. Indian J Physiol Pharmacol 1995;39:418–20. [PubMed] [Google Scholar]
- 38.Rao NP, Deshpande G, Gangadhar KB, et al. Directional brain networks underlying OM chanting. Asian J Psychiatr 2018;37:20–5. 10.1016/j.ajp.2018.08.001 [DOI] [PubMed] [Google Scholar]
- 39.Arch JJ, Craske MG. Mechanisms of mindfulness: emotion regulation following a focused breathing induction. Behav Res Ther 2006;44:1849–58. 10.1016/j.brat.2005.12.007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-059604supp001.pdf (58.4KB, pdf)


