SUMMARY
During the Coronavirus Disease 2019 (COVID-19) pandemic, otolaryngology has been shown to be a high-risk specialty due to the exposure to aerosol-generating physical examinations, procedures and surgical interventions on the head and neck area, both in adult and paediatric patients. This has prompted the issue of updating the guidelines by International Health Authorities in the Ear Nose and Throat (ENT) field and, at the same time, has stimulated engineers and healthcare professionals to develop new devices and technologies with the aim of reducing the risk of contamination for physicians, nurses and patients.
Methods
A review of the literature published on PubMed, Ovid/Medline and Scopus databases was performed from January 01, 2020 to December 31, 2021.
Results
73 articles were eligible to be included, which were subdivided into 4 categories: (“Artificial Intelligence (AI)”; “Personal Protective Equipment (PPE)”; “Diagnostic tools”; “Surgical tools”).
Conclusions
All of the innovations that have been developed during the COVID-19 pandemic have laid the foundation for a radical technological change of society, not only in medicine but also from a social, political and economical points of view that will leave its mark in the coming decades.
KEY WORDS: COVID-19, SARS-CoV-2, otolaryngology, adult, pediatric, technology
RIASSUNTO
Durante la pandemia da COVID-19, l’otorinolaringoiatria ha dimostrato di essere una delle specialità a più alto rischio di contatto con le malattie virali a trasmissione aerea, a causa dell’esposizione a procedure generanti aerosol sul distretto testa-collo, sia sul paziente adulto che pediatrico. Questo ha rappresentato il punto di partenza non solo per l’emanazione di nuove linee guida da parte delle Società scientifiche internazionali, ma ha anche stimolato l’inventiva di tecnici e operatori sanitari nello sviluppare nuovi dispositivi e tecnologie per ridurre il rischio di contaminazione per gli operatori sanitari e per il paziente.
Metodi
È stata eseguita una revisione della letteratura dal giorno 1 gennaio 2020 al 31 dicembre 2021 utilizzando i database di PubMed, Ovid/Medline e Scopus.
Risultati
Sono stati selezionati 73 articoli e raccolti in 4 categorie differenti (“Intelligenza Artificiale”; “Dispositivi di Protezione Individuale”; “Strumenti diagnostici”; “Strumenti chirurgici”).
Conclusioni
Le innovazioni sviluppate durante la pandemia da COVID-19 hanno posto le basi per una trasformazione in ambito tecnologico di tutta la società, non solo da un punto di vista medico ma anche da un punto di vista sociale, politico, ed economico, riflettendosi in una trasformazione che segnerà la mentalità dell’intera popolazione mondiale per i prossimi decenni.
PAROLE CHIAVE: COVID-19, SARS-CoV-2, otorinolaringoiatria, adulto, pediatria, tecnologia
Introduction
Amongst all healthcare specialists, otorhinolaryngologists are especially increased risk of COVID-19 infection 1 due to their exposure to aerosol-generating physical examinations, procedures and surgical interventions on the head and neck area, in both adult and paediatric patients. In addition, while the adult patient is more manageable because of his vaccinated status and general compliance, paediatric patients are even more hazardous to the healthcare worker because they are less compliant and more inclined to cry and cough, and because they may not be wearing face masks 2.
Therefore, in order to minimise the spread of SARS-CoV-2 spread during everyday practice, several protective measures have recently been developed. We conducted a review of the literature with the aim of describing the strategies – especially technological innovations – that have been adopted to mitigate viral trasmission during the COVID-19 pandemic in ENT clinical practice.
Methods
We reviewed the literature to identify innovations that have been developed for the management of the ENT patient during the COVID-19 pandemic era. English-language papers and abstracts published on PubMed, Ovid/Medline and Scopus databases were examined from January 01, 2020 to December 31, 2021, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Fig. 1) 3. Our search was based on the following key-words: “innovations, COVID-19, otolaryngology”; “innovations, COVID-19, ENT”; “COVID-19; otolaryngology”; “COVID-19, ENT”; “COVID-19 pediatric ENT surgery”; “COVID-19, masks”; “otolaryngology, masks”. The latest interventions, techniques, diagnostic and surgical solutions were evaluated according to the Oxford Center for Evidence Based Medicine (EBM) criteria.
Figure 1.
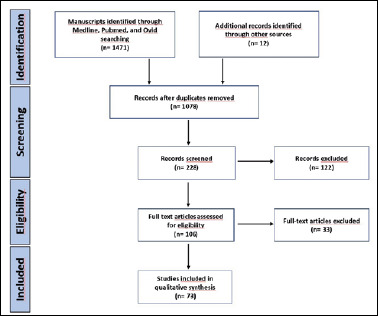
PRISMA diagram (from Liberati et al., 2009 3, mod.).
Results
The search performed on PubMed, Ovid/Medline and Scopus databases has yielded 1483 English-language abstracts and papers. Based on the titles and abstracts, we selected innovations about: upper airways’ Personal Protective Equipment (PPE); diagnostic and surgical devices in laryngology and head and neck surgery, rhinology and skull base surgery, audiology and ear surgery; Artificial Intelligence (AI) related devices employed during the COVID-19 pandemic in the ENT specialty. Therefore, we excluded papers whose title and abstract were unrelated to these topics. After narrowing the search according to our topic of interest, 73 articles were eligible to be included in our review.
These articles were subsequently divided into 4 categories: 4 papers were included in “Artificial Intelligence (AI)”; 26 papers were included in “Personal Protective Equipment (PPE)”; 11 papers were included in “Diagnostic tools”; 33 papers were included in “Surgical tools”. One article was cited twice because it contained some innovations that we selected to be included both in “Personal Protective Equipment (PPE)” plus “Diagnostic tools”.
Discussion
Artificial Intelligence (AI)
During the COVID-19 pandemic, we have witnessed significant development and diffusion of innovative tools – already available to the general population – which have played a positive role in health communication by raising awareness of health status and safety of the healthcare provider and patient. They substantially contributed to behavioural changes, i.e. increasing cognition of seriousness, susceptibility, action clue and self-efficacy. All of this was achieved through the use of social media and videogame platforms.
Jiang 4 conducted a study on college students using “Plague Inc.®”, an infectious disease-themed, simulation game developed in 2012 by Ndemic Creations® for Iphone Operating Systems and Android Systems, based on Centers for Disease Control and Prevention algorithms. He successfully demonstrated how a videogame can help gain deeper understanding of factors influencing infectious disease outbreaks, improve knowledge and educate both healthcare personnels and the general population.
Murri et al. 5 have shown that, as the COVID-19 pandemic unfolded, health professionals turned to rapid communication media (i.e. Facebook groups, Whatsapp and Telegram chats, Twitter feeds) more than to official academic sources in an attempt to seek information and update their scientific knowledge. This has the potential to spread misinformation and distrust towards public health authorities.
At the same time, during the pandemic, machine learning and deep learning-based AI technology have improved medical equipment and workflow to minimise contacts with patients 6, enabling healthcare workers to make more efficient and safer clinical decisions. This was implemented thanks to: wearable devices with patients’ GPS data on Wi-Fi, 5G and Bluetooth technologies (cardiac and respiratory wearable sensors); Internet of Things systems-based remote screening (color-coded patient severity identification, facial recognition, smartphone applications for screening); intelligent diagnostic systems for neural networks and digital image processing technology (chest X-rays and CT images); remote intensive care to reduce unnecessary patient-doctor contacts.
Furthermore, Wang has proposed the use of a remotely-controlled, low-cost microrobot for nasopharyngeal swab sample collection 7, replacing medical staff and therefore limiting aerosol and droplet contamination for healthcare workers.
All of these technologies can help solve not only staff shortage, but also limit healthcare-related rising costs and waste, reaching a safety level that may go beyond Personal Protective Equipment (PPE), since they are able to inimize contact with the infected patient (Tab. I).
Table I.
Artificial Intelligence’s core elements.
| Artificial Intelligence (AI) | |
|---|---|
| Innovations | Simulation games |
| Social media | |
| Wearable devices | |
| Internet of Things | |
| Intelligent diagnostic systems | |
| Key point | Platforms and technological devices are able to promote a rapid – often real-time – spread of relevant information and minimize interhuman contacts, thus reducing the contamination risk related to airborne infections during the present and future public-health crises |
Personal Protective Equipment (PPE)
This is the richest chapter of innovations that has been proposed during lockdown and, more extensively, during these two years of the COVID-19 pandemic; it also plays a fundamental role against future airborne infectious disease outbreaks in the field of otolaryngology.
A survey on performing in-office otolaryngology procedures during COVID-19 pandemic 8 showed gloves and masks are the most commonly used types of PPE by ENT specialists. Another international survey noted a significantly higher use of powered air-purifying respirators (PAPRs) in high-risk aerosol.generating medical paediatric procedures 9. In fact, health authorities recommend that every diagnostic procedure needs to be performed on patients who are possibily or certainly infected with COVID-19 should take place in Negative Pressure Rooms (NPRs) wearing full PPE. However, PAPRs and NPRs may not always readily available in healthcare facilities.
To overcome this limitation, Sayin et al. 10 presented a closed chamber unit for ENT examination during aerosol-generating endoscopic examinations, allowing for communication between the examiner and patient to take place thanks to a Bluetooth speaker in the room, with the negative pressure blocking aerosol dissemination. Other authors 11 have modified a liftable, protective methacrylate shield to enclose the whole ENT examination chair, with holes placed in the front, allowing the ENT specialist to introduce his hands and equipment.
A smaller airway-isolating system, called COVID-19 Airway Management Isolation Chamber (CAMIC) 12 covering the patient’s head and chest area, aims at creating an internal negative pressure generated by an aspiration mechanism. This device consists of a polyvinyl chloride hollow frame with fenestrations, with a suction vacuum line and a contralateral air supply line (Fig. 2). Its strong barrier allows the creation of a safer environment for noninvasive upper airway management. A negative-pressure plastic cover with a smoke evacuator and high-efficiency particulate air (HEPA) filtration unit 13 was tested for patients needing tracheostomy. For the same purpose, other authors have developed an external fixator equipment made up of a metal frame wrapped with a sterile plastic cover 14.
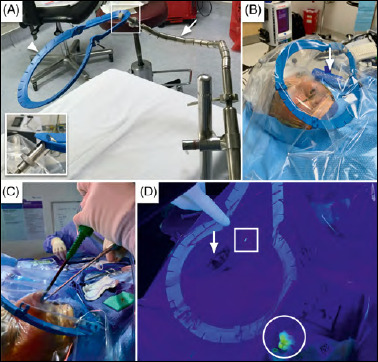
Figure 2.
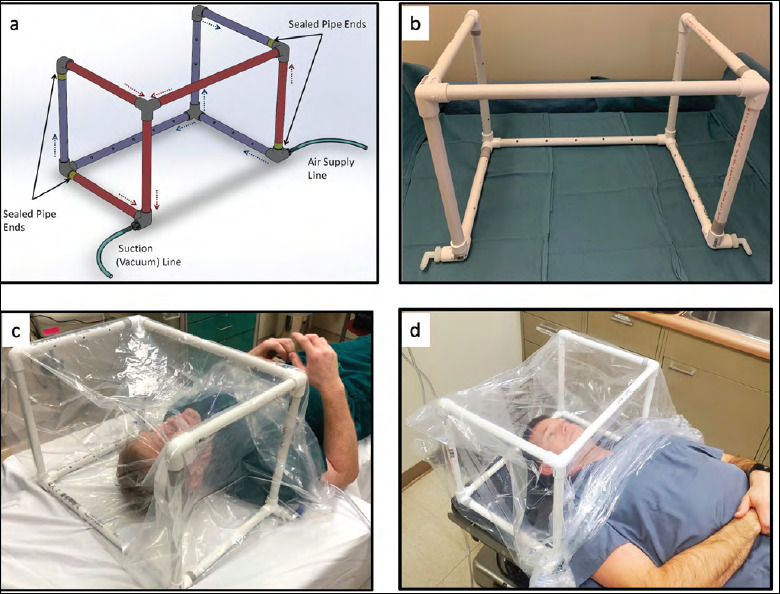
CAMIC polyvinyl chloride hollow frame: (A) CAMIC architecture; (B) CAMIC assembled frame; (C) CAMIC on the surgical bed, viewed from above; (D) CAMIC on the surgical bed, viewed from below (from Blood et al., 2021 12).
For the paediatric patient, protective acrylic boxes have been developed to perform microlaryngoscopy and bronchoscopy, containing aerosolised respiratory secretions with a 3-open-sided suspension covered with a transparent plastic sheet 15.
HEPA filters, PAPRs, N95s and other PPEs used to protect team members during aerosol-generating medical procedures can negatively affect communication, increasing noise levels and listening effort in ENT operative rooms. Therefore, either repurposing operative room team members’ headsets and cellphones towards a conference call or using an in-ear communication device has been shown to be an effective strategy to facilitate communication 16,17.
For in-office examinations, given the potential for airborne conjunctival transmission, wearing enhanced PPE plays a pivotal role in ensuring physicians’ individual safety during the COVID-19 pandemic. Notwithstanding, eye protection may often be neglected by ENT specialists. It has been demonstrated that the addition of either safety goggles or glasses to an upward-facing face shield are able to decrease the risk of eye contamination during cough 18.
More importantly, enhanced PPE devices can successfully be integrated to everyday ENT practice tools, such as headlights. Namely, standard headlights were modified so as to provide better protection for the healthcare provider. Some authors have succeeded in doing so 19 by using a 3D-printed adaptor that is able to generate a protective barrier through a transparent sheet. Another headlight-related innovation is represented by a custom-made clear laminated shield that should be directly fixed to the headlight, functioning as a barrier between the examining ENT specialist and the patient 11.
Despite being less comfortable to wear, face masks remain the first-line defense device for every airborne infection, as they are able to guarantee safety of healthcare personnel and the general population even when facing potential COVID-19 future variants of concern. Convissar et al. 20 assembled a reusable makeshift filter mask, called Modified Airway from VentilatoR Circuit (MAVerIC), starting from an adult anaesthesia breathing circuit with HEPA filters, a facemask and a rubber head strap, with or without an eye protection. MAVerIC is able to filter 99.7% of particles ≥ 0.3 microns.
3D-printed adaptors have represented another great innovation for PPEs, whose potential has been exploited both on their own, as an interface between elastomeric respirators and anaesthesia circuit filters 21 or together with masks. One of the most affordable examples is represented by the use of snorkerling masks (Fig. 3). Thierry et al. tested the EasyBreath snorkeling mask with an upper adaptor connected to a filter, which greatly increased surgeons’ visual comfort and safety 22. Different models of modified full-face snorkeling masks were tested by Vicini et al. during ENT surgical procedures 23.
Figure 3.
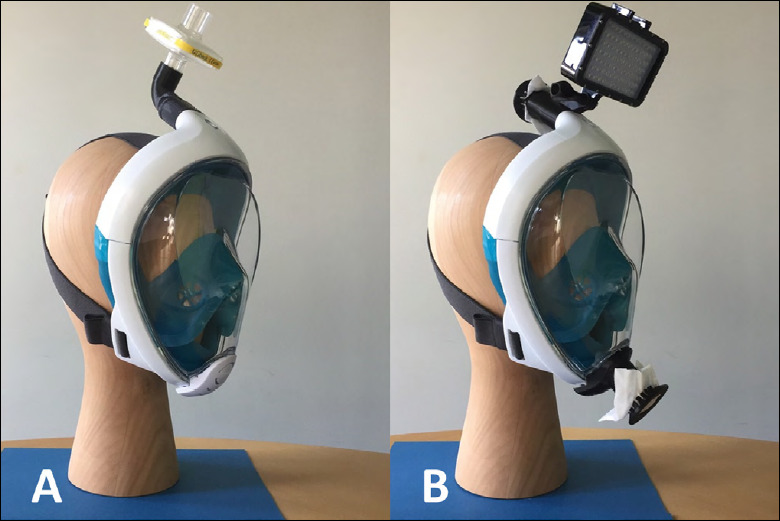
A modified snorkeling mask: (A) EasyBreath® mask with an adaptor and a filter; (B) EasyBreath® mask with dive lights and lower adaptor (from Therry et al., 2020 22).
On the other hand, a cheaper, cost-effective innovation, is represented by a reusable half-face respirator, the Sundstrom SR 100 respirator, routinely used in industrial settings to filter gas and vapour particulates 24.
The COVID-19 pandemic has marked the rise of 3D-printing technology, especially for endoscopy masks, thus allowing ENT specialists to use rigid and flexible endoscopes during in-office evaluations. Davies et al. 25 studied a stereolithographic 3D-printed nasal endoscopy mask with a side port for connection to supplemental oxygen or inline ventilation filter. Two types of endoscopy masks have been tested, both reusable and disposable, which were effective in preventing diffusion of large droplets after a simulated cough.
Another 3D-printed mask was tested – first on mannequins and then on human volunteers – by Ference et al. 26,27 (Fig. 4). It is an Aerosol Containment Mask with an N-95 respirator filter and two frontal ports to support the passage of a rigid or flexible endoscope or suction. Other authors have developed a modified ENVO® mask by SleepNet, which uses suction to create a negative-pressure environment in the nasal and oral cavity of the patient during laryngoscopy 28.
Figure 4.
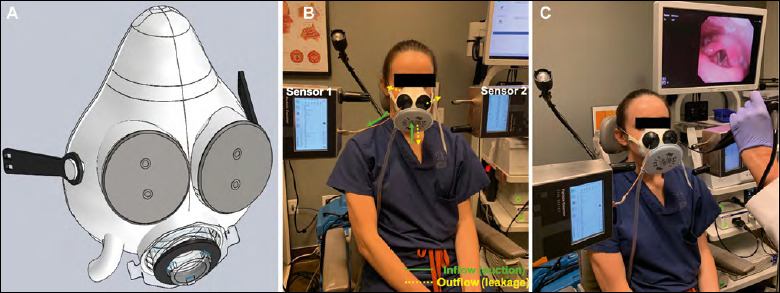
An aerosol containment mask for endoscopy: (A) mask architecture; (B) mask on patient; (C) patient undergoing endoscopy (from Ference et al., 2021 27).
Hoffman et al. 29 proposed a new model for a negative-pressure face shield with controlled access to the nose and mouth. Alternatively, a standard endoscopy face mask has been altered to allow the passage of a flexible laryngoscope by fashioning a 3-mm slit with a scalpel 30. For flexible endoscopy, other authors 31 developed patient-worn enhanced protection face shields. The fibreoptic endoscope was inserted into stellate openings, obtaining a barrier against aerosolised particles. To limit airborne contamination, Curran et al. 32 proposed the use of a low-cost device made up of an anaesthetic closed facemask, anaesthetic filter, and DAR (Covidien) connector with a reusable harness attachment for CPAP.
Lastly, the idea of making a hole in a surgical mask worn by the patient must be limited to children, since according to some authors the use of a pre-prepared modified mask for the paediatric patient with a hole for the scope should also be considered to cover the nose and the mouth during the endoscopy depending on the age and compliance of the patient 33 (Tab. II).
Table II.
Personal Protective Equipment’s core elements.
| Personal Protective Equipment (PPE) | |
|---|---|
| Innovations | Environmental isolation (powered-air purifying respirators, negative pressure rooms, closed chamber examination unit, chair shields) |
| Patient isolation (head and chest shields, face shields, plastic covers and protective boxes with HEPA filters, endoscopy masks) | |
| Healthcare personnel isolation (N95 masks, eye protection, headlight shields, filter masks, snorkeling masks) | |
| Key point | Isolation methods play a fundamental role in the reduction of contamination related to airborne infections |
Diagnostic tools
During lockdowns, some healthcare workers asked parents to monitor their children’s throat using smartphone cameras 34. These digital tools have also been successfully used on adults and were deemed to be convenient by patients and reliable by doctors 35. However, to avoid difficulties in evaluation and diagnostic errors, digital photo shooting must follow strict rules, i.e: the patient needs to position himself in front of the mirror with optimal room lighting and setting flash to forced mode; 16:9 image ratio and highest resolution; horizontal format to cut all unnecessary facial features (nose, eyes, forehead, etc.); use of the back camera without digital zoom and audible indicator when shooting 36.
It may be something of an understatement, but whenever in-office fibrolaryngoscopic examination is required, it should be performed not by using the endoscope lens, but with a camera and monitor so as to maximise the distance between the patient and examining physician 33. This holds especially true for paediatric patients, given their higher propensity to cough and cry along with less compliance.
As an alternative to the traditional approach, the so-called “back approach to the patient” 37, where during the endoscopic examination the specialist positions himself behind the patient facing the monitor, may represent a simple yet effective solution to decrease healthcare professionals’ exposure to viral particles.
Sciancalepore et al. 38 have tested the accuracy of transcutaneous laryngeal ultrasonography (TLUSG) for vocal fold mobility assessment, which was a noninvasive alternative to fibrolaryngoscopy during COVID-19 pandemic given its ability to screen for vocal fold paralysis without aerosol-generating procedures, especially in patients undergoing thyroidectomy. A further step to this approach may be telerobotic ultrasound examination 39 which, despite being more time-consuming, is safer for healthcare professionals and a valid alternative to diagnose patients who cannot go to the hospital.
Lockdowns have marked the rise of digital USB-otoscopes (DUO), of which different models – even unexpensive ones – have been developed by companies all over the world. They can be connected to smartphones to visualise the auditory canal and tympanic membrane, thus allowing self-monitoring 40, even on children 41. Even though more professional otoscopes have been developed, such as Smartphone-Enabled Wireless Otoscope (SEWO) 42 to be employed during telehealth consultations, and many patients have found these devices ready and easy-to-use, physicians reported that they would not feel comfortable using the images for diagnosis or to defer an in-person examination 43 (Tab. III).
Table III.
Diagnostic tools’ core elements.
| Diagnostic tools | |
|---|---|
| Innovations | Smartphone cameras |
| USB otoscopes | |
| New endoscopic approaches to the patient | |
| Transcutaneous laryngeal ultrasonography | |
| Key point | The use of modern video tools with diagnostic purposes and the adaptation of alternative approaches and diagnostic tools significantly contributes to reduce contact between the healthcare worker and the patient, proving to be effective in minimizing airborne contamination risk |
Surgical tools
During the COVID-19 pandemic, rather than tool-related surgical innovations, we witnessed a rethinking of surgical approaches and choices of techniques and instruments, with the purpose of minimising the risk of contamination. Indeed, health authorities in the ENT field have tried to face the evolving viral outbreak by rapidly developing specific guidelines to ensure the safety of both patients and healthcare professionals. The common ground to all guidelines, both for adult and paediatric patients 44, is to defer to a later date every procedure, except those that are deemed to be emergent and/or whose management and prognosis is time-sensitive, i.e: urgent/emergent cases that could require surgery; surgery for acute airway obstruction; prompt diagnosis of suspected cancer; surgical intervention for sepsis following initial first-line medical management.
Other recommendations include the suggestion of letting procedures to be done by the most skilled surgeons and the use of open approaches rather than endoscopic ones, with the aim of reducing time of exposure both for patients and clinicians 45.
As far as pre-surgical anaesthesia is concerned, general anaesthetic procedures should preferably be switched to local ones. However, when intubation is necessary, shortening peri-procedural aerosolisation and pausing to allow for aerosol dispersion may be useful 45. In addition, as just the act of intubating COVID-19 positive patients is considered to be at high risk of viral transmission; we witnessed the development of innovative devices to protect healthcare professionals from particle aerosolisation.
A tracheostomy should be performed on a careful case-by-case indication, and key technical modifications become necessary. In particular, the use of myorelaxants helps to reduce the risk of cough-generated particle diffusion 46.
Due to the high viral aerosolisation risk, other devices have been developed and can be adapted to the neck and chest of the patient through a plastic envelopment, with holes allowing the specialist to manouver surgical tools 47-49. Other authors 50 have tested a negative airway pressure respirator (NAPR) system to protect health care workers. When suction was applied to the NAPR, no particle escape was noted. Another study tested a specific protocol to avoid droplet contamination during unsecured airway procedures independently from COVID-19 test results, consisting in the use of a surgical tent surrounding the patient. An ultrafiltration smoke evacuator is secured to the drape on the patient’s chest 51. Continuous suction should be placed near the operating field 52.
To reduce the risk of viral transmission, it is advisable to employ viricidal substances perioperatively; in particular, pre-operative hypertonic solution (< 5% NaCl) irrigations have been shown to improve mucociliary clearance 53. Alternatively, 0.23-7% povidone iodine – whose efficacy had already been reported for Severe Acute Respiratory Syndrome Coronavirus 1 (SARS-CoV-1) and Middle East Respiratory Syndrome Coronavirus Infection (MERS-CoV) 54 – was confirmed to be an optimal choice during SARS-CoV-2, even in paediatric patients 55. The use of these substances as nasal and oropharyngeal washings both for the patient and for healthcare professionals has been suggested before and after surgical interventions performed on subjects on patients who are possibily or certainly infected with COVID-19 56. Povidone iodine irrigations have also been suggested for every procedure where drilling is involved, such as mastoidectomies 57.
During surgery, the employment of adhesive dressings on nasal and oral cavities is recommended to reduce particle diffusion 58,59. The same has also been demonstrated for ear surgery: the use of a barrier drape (so-called OtoTent) significantly reduced particulate dispersion 60.
International guidelines also recommend to minimise – whenever possible – the use of surgical electrical instruments, such as drills, electrical and diathermic devices, in order to avoid biological particle aerosolisation. The risk of viral spread following drilling 61-63 or CO2 laser ablation-derived smoke is well estabilished in every ENT surgical subspecialty, i.e. head and neck surgery, nose and skull base surgery and ear surgery 64-69. Therefore, during the COVID-19 pandemic, the use of coarse or cutting burs, irrigation, handheld suction, or additional suction becomes of crucial importance 59.
Among the few truly innovative devices that were conceived during the lockdown, Hoffman et al. tested laser plume containment for diagnostic and operative transnasal potassium-titanyl-phosphate laryngoscopy for biopsy in local anaesthesia 70. The device – developed by the University of Iowa – consists of a negative-pressure face shield installed on a camera stand with two frontal access ports and a lateral suction port. The suction system was a standard wall suction for all the diagnostic laryngoscopies and a portable one for laser and biopsy procedures.
As far as nasal and skull base surgery is concerned, other authors have created a modified Vent Mask, using a surgical mask with the finger of a non-latex glove, to allow passage of an endoscope, with significant reduction of aerosolisation. This solution was only tested on a cadaver model 71. In another cadaver model, the authors tested a suction mitigation system of airborne particulate generated during sinonasal drilling and cautery, with a rigid suction placed in the contralateral nostril 72. Another study 73 tested the efficacy of SPIWay® Endonasal sheaths to reduce particle dispersion caused by nasal drilling. When a flexible suction was inserted together with the SPIWays, no aerosols were spread during drilling. Others 74 have introduced the Negative-pressure Otolaryngology Viral Isolation Drape (NOVID) system to reduce the risk of aerosolisation; it consists of a plastic drape suspended above the patient’s head and surgical field with a smoke evacuator suction (Fig. 5). In another study, a low-cost, modifiable and easily producible negative pressure face-mounted antechamber was developed utilising 3D printing and silicone moulding to effectively reduce aerosolisation from endoscopic drilling without disturbing the flow of the operation 75.
Figure 5.
The Negative-pressure Otolaryngology Viral Isolation Drape (NOVID): (A) a holder (arrow) with star ring retractor (arrow-head); (B) HEPA filter (arrow) with suction; (C) endoscope insertion; (D) fluorescein-laden droplets: patient’s nose (arrow), opening of the suction device (square), gauze outside the operating field (circle) (from David et al., 2020 74).
Lastly, in ear surgery, a COVID-19 Airway Management Isolation Chamber (CAMIC) Ear system was tested by using a schedule of Poly-Vinyl Chloride pipes with holes in order to create a hollow frame with fenestrations to facilitate vacuum suction 76 (Fig. 6, Tab. IV).
Figure 6.

CAMIC-Ear system on the microscope drape; microscope handpieces with sterile covers (yellow stars) (from Tolisano et al., 2020 76).
Table IV.
Surgical tools’ core elements.
| Surgical tools | |
|---|---|
| Innovations | Employing surgical tents and drapes |
| Using pre-operative viricidal solutions | |
| Favouring local instead of general anesthesia | |
| Shortening intubation-related aerosolization | |
| Anaesthetic drug choice | |
| Avoiding eletrical instruments | |
| Suctioning near the operating field | |
| Key point | Rethinking of surgical approaches, choices of techniques and instruments can effectively reduce the risk of contamination |
Conclusions
In conclusion, the COVID-19 era has significantly strengthened the application of many innovations that were considered routine in our everyday life, even in the non-medical field. Moreover, it has contributed to empower both patients and healthcare workers on the relevance and correct use of PPEs to such an extent that it represents the most important chapter of the innovations that were developed during these past two years.
Rethinking customary diagnostic and surgical approaches can minimise the risks related to airborne viral transmission. However, these novelties in the diagnosis of upper airway diseases – by reducing interhuman contact – may affect the human dimension of care in the doctor-patient relationship. All these innovations developed during the COVID-19 pandemic represent a true revolution, triggered by the fast-paced evolution of biomedical technology, in an attempt to create something that is able to face the multifaceted challenges in every field of medicine. Consequently, a radical mindset and changes in approach has affected every specialty, and especially in otolaryngology. The pandemic has influenced the development of artificial intelligence-based tools available to the general population, becoming a powerful surge of social, political and administrative change. These are able to influence medicine behind the scenes, while supporting its growth in the coming decades.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributions
PP, EB, CM and MLF: design of the work, data collection, data analysis and interpretation; drafting the article; critical revision of the article, final approval of the version to be published; RA, PIS, ADM, PD, CR, VDC and MM: acquisition of data, analysis and interpretation of data, critical revision of the article.
Ethical consideration
Ethical review and approval was not required for the study. All review procedures have been performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Figures and tables
References
- 1.Mannelli G, Ralli M, Bonali M, et al. Impact of COVID-19 pandemic on Italian Otolaryngology Units: a nationwide study. Acta Otorhinolaryngol Ital 2020;40:325-331. https://doi.org/10.14639/0392-100X-N0832 10.14639/0392-100X-N0832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cho RHW, Yeung ZWC, Ho OYM, et al. Pearls of experience for safe and efficient hospital practices in otorhinolaryngology-head and neck surgery in Hong Kong during the 2019 novel coronavirus disease (COVID-19) pandemic. J Otolaryngol Head Neck Surg 2020;49:30. https://doi.org/10.1186/s40463-020-00427-4 10.1186/s40463-020-00427-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009;62:E1-E34. https://doi.org/10.1016/j.jclinepi.2009.06.006 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 4.Jiang R, Shao B, Si S, et al. Health Communication in games at the early stage of COVID-19 epidemic: a grounded theory study based on Plague, Inc. Games Health J 2021;10:408-419. https://doi.org/10.1089/g4h.2020.0135 10.1089/g4h.2020.0135 [DOI] [PubMed] [Google Scholar]
- 5.Murri R, Segala FV, Del Vecchio P, et al. Social media as a tool for scientific updating at the time of COVID pandemic: results from a national survey in Italy. PLoS One 2020;15:e0238414. https://doi.org/10.1371/journal.pone.0238414 10.1371/journal.pone.0238414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen SW, Gu XW, Wang JJ, et al. AIoT used for COVID-19 pandemic prevention and control. Contrast Media Mol Imaging 2021;2021:3257035. https://doi.org/10.1155/2021/3257035 10.1155/2021/3257035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang S, Wang K, Tang T, et al. Design of a low-cost miniature robot to assist the COVID-19 nasopharyngeal swab sampling. IEEE Transactions on Medical Robotics and Bionics 2021;3:289-293. https://doi.org/10.1109/TMRB.2020.3036461 10.1109/TMRB.2020.3036461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Calcagno H, Anthony BP, Halum SL, et al. Safety practices for in-office laryngology procedures during clinical reintroduction amidst COVID-19. Laryngoscope Investig Otolaryngol 2021;6:780-785. https://doi.org/10.1002/lio2.591 10.1002/lio2.591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim DH, Chadha NK, Nguyen LH, et al. Personal protective equipment availability and usage amongst pediatric otorhinolaryngologists during the COVID-19 pandemic: an international survey. Int J Pediatr Otorhinolaryngol 2020;138:110349. https://doi.org/10.1016/j.ijporl.2020.110349 10.1016/j.ijporl.2020.110349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sayin İ, Devecioğlu İ, Yazıcı ZM. A Closed chamber ENT examination unit for aerosol-generating endoscopic examinations of COVID-19 patients. Ear Nose Throat J 2020;99:594-596. https://doi.org/10.1177/0145561320931216 10.1177/0145561320931216 [DOI] [PubMed] [Google Scholar]
- 11.Farneti P, Sorace F, Tasca I. Personal protective equipment for ENT activity during COVID-19 pandemic. Eur Arch Otorhinolaryngol 2020;277:2933-2935. https://doi.org/10.1007/s00405-020-06177-3 10.1007/s00405-020-06177-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blood TC, Jr, Perkins JN, Wistermayer PR, et al. COVID-19 airway management isolation chamber. Otolaryngol Head Neck Surg 2021;164:74-81. https://doi.org/10.1177/0194599820942500 10.1177/0194599820942500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bertroche JT, Pipkorn P, Zolkind P, et al. Negative-pressure aerosol cover for COVID-19 tracheostomy. JAMA Otolaryngol Head Neck Surg 2020;146:672-674. https://doi.org/10.1001/jamaoto.2020.1081. 10.1001/jamaoto.2020.1081 Erratum in: JAMA Otolaryngol Head Neck Surg 2020;146:678. https://doi.org/10.1001/jamaoto.2020.1370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cordier PY, De La Villeon B, Martin E, et al. Health workers’ safety during tracheostomy in COVID-19 patients: homemade protective screen. Head Neck 2020;42:1361-1362. https://doi.org/10.1002/hed.26222 10.1002/hed.26222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pollaers K, Herbert H, Vijayasekaran S. Pediatric microlaryngoscopy and bronchoscopy in the COVID-19 era. JAMA Otolaryngol Head Neck Surg 2020;146:608-612. https://doi.org/10.1001/jamaoto.2020.1191 10.1001/jamaoto.2020.1191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levin M, Zhou K, Sommer EC, et al. Ambient noise levels and wireless headsets for communication in aerosolizing otolaryngology surgery during COVID-19. Otolaryngol Head Neck Surg 2021;165:528-531. https://doi.org/10.1177/0194599820986584 10.1177/0194599820986584 [DOI] [PubMed] [Google Scholar]
- 17.Nguyen DL, Kay-Rivest E, Tewfik MA, et al. Association of in-ear device use with communication quality among individuals wearing personal protective equipment in a simulated operating room. JAMA Netw Open 2021;4:e216857. https://doi.org/10.1001/jamanetworkopen.2021.6857 10.1001/jamanetworkopen.2021.6857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ng JH, Daniel D, Sadovoy A, et al. Eye protection in ENT practice during the COVID-19 pandemic. OTO Open 2021;5:2473974X211010408. https://doi.org/10.1177/2473974X211010408 10.1177/2473974X211010408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Viera-Artiles J, Valdiande JJ. 3D-printable headlight face shield adapter. Personal protective equipment in the COVID-19 era. Am J Otolaryngol 2020;41:102576. https://doi.org/10.1016/j.amjoto.2020.102576 10.1016/j.amjoto.2020.102576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Convissar D, Berra L, Chang MG, et al. Personal protective equipment N95 facemask shortage quick fix: the modified airway from VEntilatoR Circuit (MAVerIC). Cureus 2020;12:e7914. https://doi.org/10.7759/cureus.7914 10.7759/cureus.7914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu DCY, Koo TH, Wong JKK, et al. Adapting re-usable elastomeric respirators to utilise anaesthesia circuit filters using a 3D-printed adaptor – a potential alternative to address N95 shortages during the COVID-19 pandemic. Anaesthesia 2020;75:1022-1027. https://doi.org/10.1111/anae.15108 10.1111/anae.15108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thierry B, Célérier C, Simon F, et al. How and why use the EasyBreath® surface snorkeling mask as a personal protective equipment during the COVID-19 pandemic? Eur Ann Otorhinolaryngol Head Neck Dis 2020;137:329-331. https://doi.org/10.1016/j.anorl.2020.05.006 10.1016/j.anorl.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vicini C, Cammaroto G, Meccariello G, et al. Overview of different modified full-face snorkelling masks for intraoperative protection. Acta Otorhinolaryngol Ital 2020;40:317-324. https://doi.org/10.14639/0392-100X-N0841 10.14639/0392-100X-N0841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patel B, Hardman JC, Yang W, et al. Reusable respirators as personal protective equipment during ENT surgery. J Laryngol Otol 2020;134:732-734. https://doi.org/10.1017/S0022215120001346 10.1017/S0022215120001346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davies JC, Chan HHL, Gilbert RW, et al. Nasal endoscopy during the COVID-19 pandemic: mitigating risk with 3D printed masks. Laryngoscope 2020;130:2561-2563. https://doi.org/10.1002/lary.29004 10.1002/lary.29004 [DOI] [PubMed] [Google Scholar]
- 26.Ference EH, Kim W, Oghalai JS, et al. COVID-19 in the clinic: aerosol containment mask for endoscopic otolaryngologic clinic procedures. Otolaryngol Head Neck Surg 2021. Jun 22:1945998211024944. https://doi.org/10.1177/01945998211024944. 10.1177/01945998211024944 Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ference EH, Kim W, Oghalai JS, et al. COVID-19 in the clinic: human testing of an aerosol containment mask for endoscopic clinic procedures. Otolaryngol Head Neck Surg 2021. Jun 27:1945998211029184. https://doi.org/10.1177/01945998211029184. 10.1177/01945998211029184 Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCarty EB, Soldatova L, Brant JA, et al. Innovations in otorhinolaryngology in the age of COVID-19: a systematic literature review. World J Otorhinolaryngol Head Neck Surg 2021. Jan 22. https://doi.org/10.1016/j.wjorl.2021.01.001. 10.1016/j.wjorl.2021.01.001 Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hoffman HT, Miller RM, Walsh JE, et al. Negative pressure face shield for flexible laryngoscopy in the COVID-19 era. Laryngoscope Investig Otolaryngol 2020;5:718-726. https://doi.org/10.1002/lio2.437 10.1002/lio2.437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Narwani V, Kohli N, Lerner MZ. Application of a modified endoscopy face mask for flexible laryngoscopy during the COVID-19 pandemic. Otolaryngol Head Neck Surg 2020;163:107-109. https://doi.org/10.1177/0194599820928977 10.1177/0194599820928977 [DOI] [PubMed] [Google Scholar]
- 31.Anon JB, Denne C, Rees D. Patient-worn enhanced protection face shield for flexible endoscopy. Otolaryngol Head Neck Surg 2020;163:280-283. https://doi.org/10.1177/0194599820934777 10.1177/0194599820934777 [DOI] [PubMed] [Google Scholar]
- 32.Curran J, Calder N, Yaneza M, et al. Reducing potential aerosol generation in flexible nasolaryngoscopy: a novel method. J Laryngol Otol 2020;134:744-746. https://doi.org/10.1017/S0022215120001413 10.1017/S0022215120001413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leitmeyer K, Felton M, Chadha NK. Strategies for restarting pediatric otolaryngology outpatient clinics after a pandemic-related shutdown such as from COVID-19. Int J Pediatr Otorhinolaryngol 2020;139:110414. https://doi.org/10.1016/j.ijporl.2020.110414 10.1016/j.ijporl.2020.110414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maurrasse SE, Rastatter JC, Hoff SR, et al. Telemedicine during the COVID-19 pandemic: a pediatric otolaryngology perspective. Otolaryngol Head Neck Surg 2020;163:480-481. https://doi.org/10.1177/0194599820931827 10.1177/0194599820931827 [DOI] [PubMed] [Google Scholar]
- 35.Cai Y, Zheng YJ, Gulati A, et al. Patient use of low-cost digital videoscopes and smartphones for remote ear and oropharyngeal examinations. JAMA Otolaryngol Head Neck Surg 2021;147:336-342. https://doi.org/10.1001/jamaoto.2020.5223 10.1001/jamaoto.2020.5223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Maret D, Peters OA, Auria JP, et al. Smartphone oral self-photography in teledentistry: recommendations for the patient. J Telemed Telecare 2021. Jun 23:1357633X211028513. https://doi.org/10.1177/1357633X211028513. 10.1177/1357633X211028513 Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 37.Di Maio P, Traverso D, Iocca O, et al. Endoscopic nasopharyngoscopy and ENT specialist safety in the COVID 19 era: the back endoscopy approach to the patient. Eur Arch Otorhinolaryngol 2020;277:2647-2648. https://doi.org/10.1007/s00405-020-06093-6 10.1007/s00405-020-06093-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sciancalepore PI, Anzivino R, Petrone P, et al. Transcutaneous laryngeal ultrasonography: a promising tool for otolaryngologists during COVID-19. Am J Otolaryngol 2021;42:102772. https://doi.org/10.1016/j.amjoto.2020.102772 10.1016/j.amjoto.2020.102772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ganesh D, Seshadri G, Sokkanarayanan S, et al. AutoImpilo: smart automated health machine using IoT to improve telemedicine and telehealth. In: 2020 International Conference on Smart Technologies in Computing, Electrical and Electronics (ICSTCEE). Bengaloru 2020:487-493. https://doi.org/10.1109/ICSTCEE49637.2020.9277223 10.1109/ICSTCEE49637.2020.9277223 [DOI] [Google Scholar]
- 40.Bayoumy AB, Veugen CCAFM, van Rijssen LB, et al. Self-monitoring of the tympanic membrane: an opportunity for telemedicine during times of COVID-19 and beyond. J Otol 2021;16:120-122. https://doi.org/10.1016/j.joto.2020.12.003 10.1016/j.joto.2020.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jayawardena ADL, Mankarious LA, Keamy DG, Jr, et al. Pediatric, family-centered, “At-Home” otologic physical examination in the COVID-19 era. Otolaryngol Head Neck Surg 2020;163:1061-1063. https://doi.org/10.1177/0194599820934776 10.1177/0194599820934776 [DOI] [PubMed] [Google Scholar]
- 42.Meng X, Dai Z, Hang C, et al. Smartphone-enabled wireless otoscope-assisted online telemedicine during the COVID-19 outbreak. Am J Otolaryngol 2020;4:102476. https://doi.org/10.1016/j.amjoto.2020.102476 10.1016/j.amjoto.2020.102476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ronner EA, Stenerson ME, Goldschmidt NH, et al. Otoendoscopes to enhance telemedicine during the COVID-19 pandemic. Ann Otol Rhinol Laryngol 2021. Nov 2:34894211051810. https://doi.org/10.1177/00034894211051810. 10.1177/00034894211051810 Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 44.Din T, Abdalla T, Chiesa-Estomba C, et al. YO-IFOS Guidelines for pediatric ENT surgery during COVID-19: an overview of recommendations. Laryngoscope 2021;131:1876-1883. https://doi.org/10.1002/lary.29335 10.1002/lary.29335 [DOI] [PubMed] [Google Scholar]
- 45.Elliott D, Ochieng C, Jepson M, et al. ‘Overnight, things changed. Suddenly, we were in it’: a qualitative study exploring how surgical teams mitigated risks of COVID-19. BMJ Open 2021;1:E046662. https://doi.org/10.1136/bmjopen-2020-046662 10.1136/bmjopen-2020-046662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xu K, Lai X, Liu Z. Suggestions on the prevention of COVID-19 for health care workers in department of otorhinolaryngology head and neck surgery. World J Otorhinolaryngol Head Neck Surg 2020;6(Suppl 1):S2-S5. https://doi.org/10.1016/j.wjorl.2020.03.002 10.1016/j.wjorl.2020.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Canelli R, Connor CW, Gonzalez M, et al. Barrier enclosure during endotracheal intubation. N Engl J Med 2020;382:1957-1958. https://doi.org/10.1056/NEJMc2007589 10.1056/NEJMc2007589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kearsley R. Intubation boxes for managing the airway in patients with COVID-19. Anaesthesia 2020;75:969. https://doi.org/10.1111/anae.15081 10.1111/anae.15081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Begley JL, Lavery KE, Nickson CP, et al. The aerosol box for intubation in coronavirus disease 2019 patients: an in-situ simulation crossover study. Anaesthesia 2020;75:1014-1021. https://doi.org/10.1111/anae.15115 10.1111/anae.15115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Khoury T, Lavergne P, Chitguppi C, et al. Aerosolized particle reduction: a novel cadaveric model and a negative airway pressure respirator (NAPR) system to protect health care workers from COVID-19. Otolaryngol Head Neck Surg 2020;163:151-155. https://doi.org/10.1177/0194599820929275 10.1177/0194599820929275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Francom CR, Javia LR, Wolter NE, et al. Pediatric laryngoscopy and bronchoscopy during the COVID-19 pandemic: a four-center collaborative protocol to improve safety with perioperative management strategies and creation of a surgical tent with disposable drapes. Int J Pediatr Otorhinolaryngol 2020;134:110059. https://doi.org/10.1016/j.ijporl.2020.110059 10.1016/j.ijporl.2020.110059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Leboulanger N, Sagardoy T, Akkari M, et al. COVID-19 and ENT pediatric otolaryngology during the COVID-19 pandemic. Guidelines of the French Association of Pediatric Otorhinolaryngology (AFOP) and French Society of Otorhinolaryngology (SFORL). Eur Ann Otorhinolaryngol Head Neck Dis 2020;137:177-181. https://doi.org/10.1016/j.anorl.2020.04.010 10.1016/j.anorl.2020.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Farrell NF, Klatt-Cromwell C, Schneider JS. Benefits and safety of nasal saline irrigations in a pandemic-washing COVID-19 away. JAMA Otolaryngol Head Neck Surg 2020;146:787-788. https://doi.org/10.1001/jamaoto.2020.1622 10.1001/jamaoto.2020.1622 [DOI] [PubMed] [Google Scholar]
- 54.Parhar HS, Tasche K, Brody RM, et al. Topical preparations to reduce SARS-CoV-2 aerosolization in head and neck mucosal surgery. Head Neck 2020;42:1268-1272. https://doi.org/10.1002/hed.26200 10.1002/hed.26200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chorney SR, Rizzi MD, Dedhia K. Considerations for povidone-iodine antisepsis in pediatric nasal and pharyngeal surgery during the COVID-19 pandemic. Am J Otolaryngol 2020;41:102737. https://doi.org/10.1016/j.amjoto.2020.102737 10.1016/j.amjoto.2020.102737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mady LJ, Kubik MW, Baddour K, et al. Consideration of povidone-iodine as a public health intervention for COVID-19: utilization as “Personal Protective Equipment” for frontline providers exposed in high-risk head and neck and skull base oncology care. Oral Oncol 2020;105:104724. https://doi.org/10.1016/j.oraloncology.2020.104724 10.1016/j.oraloncology.2020.104724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Khan MM, Parab SR. 0.5% povidone iodine irrigation in otorhinolaryngology surgical practice during COVID 19 pandemic. Am J Otolaryngol 2020;41:102687. https://doi.org/10.1016/j.amjoto.2020.102687 10.1016/j.amjoto.2020.102687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lagos AE, Ramos PH, Andrade T. Protection for otolaryngologic surgery in the COVID-19 pandemic. OTO Open 2020;4:2473974X20934734. https://doi.org/10.1177/2473974X20934734 10.1177/2473974X20934734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Freiser ME, Dharmarajan H, Sri Kavya Boorgu DS, et al. Droplet and aerosol generation with mastoidectomy during the COVID-19 pandemic: assessment of baseline risk and mitigation measures with a high-performance cascade impactor. Otol Neurotol 2021;42:614-622. https://doi.org/10.1097/MAO.0000000000002987 10.1097/MAO.0000000000002987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chen JX, Workman AD, Chari DA, et al. Demonstration and mitigation of aerosol and particle dispersion during mastoidectomy relevant to the COVID-19 era. Otol Neurotol 2020;41:1230-1239. https://doi.org/10.1097/MAO.0000000000002765 10.1097/MAO.0000000000002765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Thamboo A, Lea J, Sommer DD, et al. Clinical evidence based review and recommendations of aerosol generating medical procedures in otolaryngology - head and neck surgery during the COVID-19 pandemic. J Otolaryngol Head Neck Surg 2020;49:28. https://doi.org/10.1186/s40463-020-00425-6 10.1186/s40463-020-00425-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hilal A, Walshe P, Gendy S, et al. Mastoidectomy and trans-corneal viral transmission. Laryngoscope 2005;115:1873-1876. https://doi.org/10.1097/01.mlg.0000177459.80574.2d 10.1097/01.mlg.0000177459.80574.2d [DOI] [PubMed] [Google Scholar]
- 63.Norris BK, Goodier AP, Eby TL. Assessment of air quality during mastoidectomy. Otolaryngol Head Neck Surg 2011;144:408-411. https://doi.org/10.1177/0194599810394967 10.1177/0194599810394967 [DOI] [PubMed] [Google Scholar]
- 64.In SM, Park DY, Sohn IK, et al. Experimental study of the potential hazards of surgical smoke from powered instruments. Br J Surg 2015;102:1581-1586. https://doi.org/10.1002/bjs.9910 10.1002/bjs.9910 [DOI] [PubMed] [Google Scholar]
- 65.Carr MM, Patel VA, Soo JC, et al. Effect of electrocautery settings on particulate concentrations in surgical plume during tonsillectomy. Otolaryngol Head Neck Surg 2020;162:867-872. https://doi.org/10.1177/0194599820914275 10.1177/0194599820914275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Baggish MS, Poiesz BJ, Joret D, et al. Presence of human immunodeficiency virus DNA in laser smoke. Lasers Surg Med 1991;11:197-203. https://doi.org/10.1002/lsm.1900110302 10.1002/lsm.1900110302 [DOI] [PubMed] [Google Scholar]
- 67.Subbarayan RS, Shew M, Enders J, et al. Occupational exposure of oropharyngeal human papillomavirus amongst otolaryngologists. Laryngoscope 2020;130:2366-2371. https://doi.org/10.1002/lary.28383 10.1002/lary.28383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Johnson GK, Robinson WS. Human immunodeficiency virus-1 (HIV-1) in the vapors of surgical power instruments. J Med Virol 1991;33:47-50. https://doi.org/10.1002/jmv.1890330110 10.1002/jmv.1890330110 [DOI] [PubMed] [Google Scholar]
- 69.Patel ZM, Fernandez-Miranda J, Hwang PH, et al. Letter: precautions for endoscopic transnasal skull base surgery during the COVID-19 pandemic. Neurosurgery 2020;87:E66-E67. https://doi.org/10.1093/neuros/nyaa125 10.1093/neuros/nyaa125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hoffman HT, Walsh JE, Pratt A, et al. Laser plume containment during flexible transnasal laryngoscopy. Laryngoscope Investig Otolaryngol 2021;6:234-243. https://doi.org/10.1002/lio2.526 10.1002/lio2.526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Workman AD, Welling DB, Carter BS, et al. Endonasal instrumentation and aerosolization risk in the era of COVID-19: simulation, literature review, and proposed mitigation strategies. Int Forum Allergy Rhinol 2020;10:798-805. https://doi.org/10.1002/alr.22577 10.1002/alr.22577 [DOI] [PubMed] [Google Scholar]
- 72.Workman AD, Xiao R, Feng A, et al. Suction mitigation of airborne particulate generated during sinonasal drilling and cautery. Int Forum Allergy Rhinol 2020;10:1136-1140. https://doi.org/10.1002/alr.22644 10.1002/alr.22644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dharmarajan H, Freiser ME, Sim E, et al. Droplet and aerosol generation with endonasal surgery: methods to mitigate risk during the COVID-19 pandemic. Otolaryngol Head Neck Surg 2021;164:285-293. https://doi.org/10.1177/0194599820949802 10.1177/0194599820949802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.David AP, Jiam NT, Reither JM, et al. Endoscopic skull base and transoral surgery during COVID-19 pandemic: minimizing droplet spread with negative-pressure otolaryngology viral isolation drape. Head Neck 2020;42:1577-1582. https://doi.org/10.1002/hed.26239 10.1002/hed.26239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kim M, Lee M, Schwarz J, et al. A novel negative pressure, face-mounted antechamber to minimize aerosolization of particles during endoscopic skull base surgery. Oper Neurosurg (Hagerstown) 2021;21:131-136. https://doi.org/10.1093/ons/opab173 10.1093/ons/opab173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tolisano AM, Blood TC, Jr, Riley CA, et al. The COVID-19 airway management isolation chamber (CAMIC) for ears. Laryngoscope 2020;130:2690-2692. https://doi.org/10.1002/lary.28942 10.1002/lary.28942 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


