Abstract
Rab GTPases (Rabs) are small proteins that play crucial roles in vesicle transport and membrane trafficking. Owing to their widespread functions in several steps of vesicle trafficking, Rabs have been implicated in the pathogenesis of several disorders, including cancer, diabetes, and multiple neurodegenerative diseases. As treatments for neurodegenerative conditions are currently rather limited, the identification and validation of novel therapeutic targets, such as Rabs, is of great importance. This review summarises proof-of-concept studies, demonstrating that modulation of Rab GTPases in the context of Alzheimer’s disease (AD) can ameliorate disease-related phenotypes, and provides an overview of the current state of the art for the pharmacological targeting of Rabs. Finally, we also discuss the barriers and challenges of therapeutically targeting these small proteins in humans, especially in the context of AD.
Keywords: Rab GTPases, Alzheimer’s, neurodegeneration
1. Rab GTPases: Function and Biological Roles
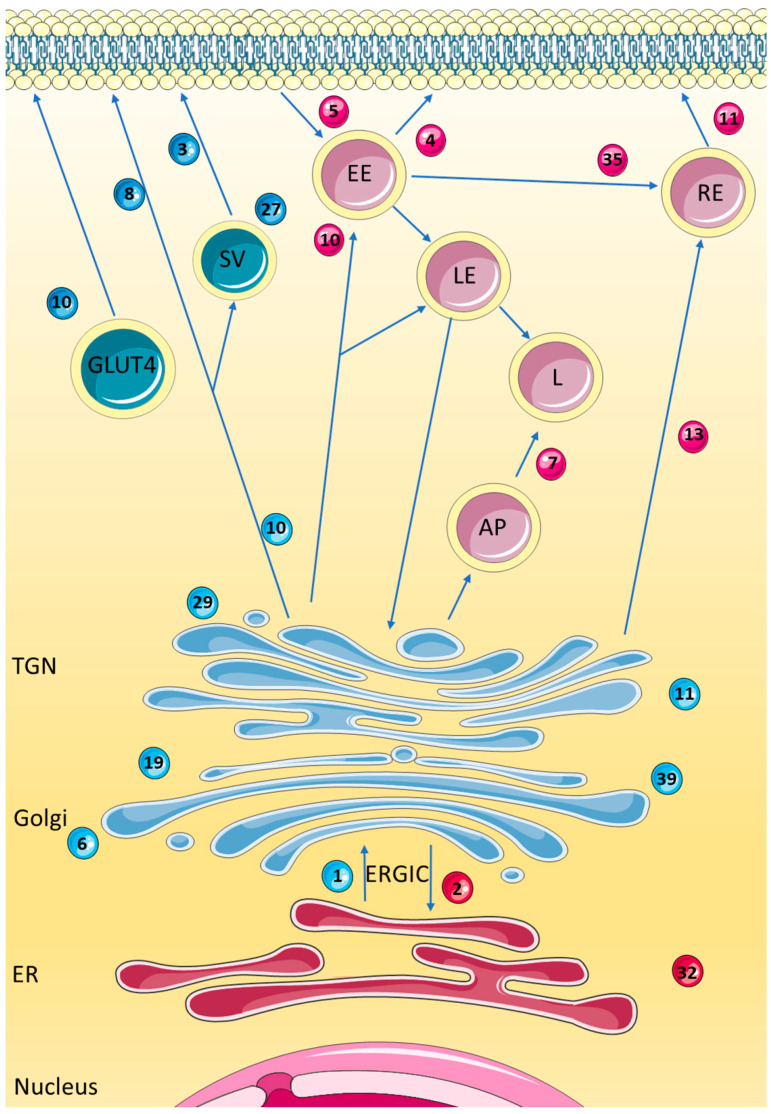
Rab GTPases (Rabs) are a family of small proteins classified within the larger Ras superfamily of guanosine triphosphatase (GTP) binding proteins [1]. Rabs play key roles in vesicle trafficking between different cellular compartments, including the endoplasmic reticulum (ER), Golgi, endosomes, and plasma membrane (Figure 1). There are over 60 mammalian Rabs, with orthologs found in many different species, including D. melanogaster, S. cerevisiae, A. thaliana, and C. elegans [2,3,4,5]. Indeed, several yeast Rab GTPases can be functionally replaced by mammalian homologs as their functions are so highly conserved [6]. Many Rabs are ubiquitously expressed, although some are tissue specific [6].
Figure 1.
The Intracellular pathways and a selected number of Rab GTPases associated with the endoplasmic reticulum (ER), Golgi, trans-Golgi network (TGN), and endosomal pathways. Rab1 and Rab2 are localised to the ER and Golgi, and play a role in the ER to Golgi apparatus trafficking pathway, via the endoplasmic reticulum to Golgi intermediate compartment (ERGIC). Rab3 is localised to synaptic secretory vesicles (SV) and the plasma membrane and is involved in exocytosis and neurotransmitter release. Rab4 has a role in protein recycling and transport to the plasma membrane and is localised to early endosomes (EE). Rab5 is localised to the EE and aids its fusion and formation. Rab6 is involved with regulating intra-Golgi trafficking. Rab7 is localised to the late endosome (LE), lysosome (L), and autophagosomes (AP) and is involved in the maturation and transport between these vesicles. Rab8 is associated with exocytosis from the TGN to the plasma membrane, with localisation to the plasma membrane and SV. Rab10 is localised to the ER, Golgi, endosomes, and GLUT4 vesicles and is involved in ER dynamics, endocytosis, and trafficking to the plasma membrane. Rab11 is also localised to the Golgi, as well as the recycling endosome (RE) and EE. Rab13 is involved in the TGN and RE to plasma membrane transport pathway. Rab19 has been shown to localise to the Golgi, however there is little known about its role. Rab27 is involved in exocytosis, localising to SV. Rab29 and Rab39 are both localised to the Golgi. Rab32 localises to the ER and mitochondria, with a role in mitochondrial dynamics and autophagy. Rab35 localises to the plasma membrane, and is involved in endocytic recycling. Rabs more strongly associated with secretory pathways are shaded in blue while those more strongly associated with endosomal pathways are shown in red. Adapted with permission from Hutagalung et al. 2022, American Physiological Society [7].
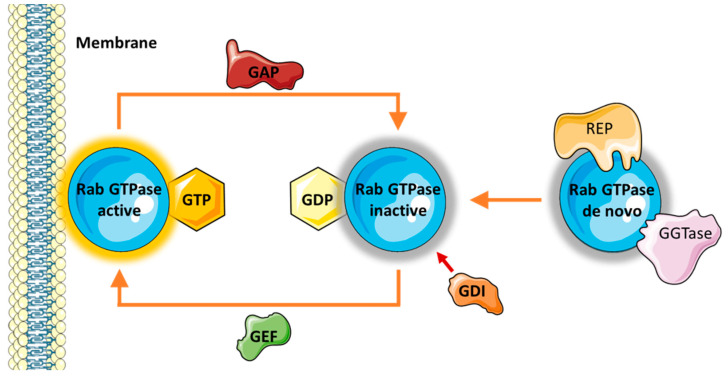
Rabs must be activated in order to function, which occurs through a cycle of GTP and GDP binding controlled by a number of different accessory proteins (Figure 2). Guanine exchange factors (GEFs) are responsible for recruiting the respective Rab to the target membrane, where it becomes active upon GTP binding [8]. Each Rab contains a hypervariable region, which is involved in membrane tethering and is specific to both the Rab and the target membrane where they carry out their function [9,10]. Once associated with the target membrane, the Rab acts as a scaffold protein and interacts with a variety of downstream effectors to complete its function. Following this, hydrolysis of GTP to GDP is driven by GTPase activating proteins (GAPs) to inactivate the small GTPase. GDP dissociation inhibitors (GDIs) then retrieve the GDP-bound Rab from the membrane to solubilise it in the cytosol so that the cycle can begin again. Rabs also undergo the important post-translational modification of prenylation, which controls its membrane association [11]. Prenylation is mediated by the Rab escort protein (REP), which binds to the Rab and presents it to the Rab geranylgeranyltransferase (GGTase) for double prenylation [8].
Figure 2.
The cycle of Rab GTPase activation. Newly synthesised de novo Rab GTPases interact with Rab escort protein (REP), which enables prenylation via geranylgeranyltransferase (GGTase). When active, Rab GTPases are bound to GTP and associated with their target membrane. Following hydrolysis of GTP to GDP, they become inactive and reside in the cytosol. The Rab GTPase activation cycle is aided by a number of effectors. GTPase activating proteins (GAPs) catalyse the hydrolysis of GTP to GDP to inactivate the Rab. GDP dissociation inhibitors (GDIs) retrieve the inactive Rab from the membrane and solubilises it in the cytosol. However, guanine exchange factors (GEFs) catalyse the exchange of GDP with GTP, thus reactivating the Rab [12].
2. Rab GTPases and Neurodegeneration
Rabs have been linked to multiple different diseases including cancer, diabetes, and various genetic disorders such as Griscelli syndrome [13]. Rabs have also been implicated in several neurodegenerative diseases, many of which have aberrant protein folding, vesicle trafficking, and secretion as key molecular pathologies [14,15]. These GTPases could also be involved in the lifecycle of viruses such as the Herpes Simplex Virus (HSV), where there is increasing evidence suggesting that HSV re-activation in the brain could lead to cognitive impairment and the development of AD [16]. Indeed, increasing Rab levels have been found to ameliorate phenotypes in a variety of disease models. For example, overexpression of the yeast Rab1 homolog Ypt1p rescues dopaminergic neuron loss caused by α-synuclein in animal models of Parkinson’s disease (PD) [17], whilst overexpression of Rab1A in rodent models of PD was found to prevent pathological Golgi fragmentation and rescue motor deficits [18]. Similarly, Rab11 overexpression significantly rescues PD- and Huntington’s-disease-related phenotypes in fly models, including neurodegeneration and behavioural deficits [19,20]. Given the localization and physiological function of different Rab GTPases, they are thought to play different roles in disease pathogenesis, thereby having therapeutic relevance (Table 1). This review focuses on the therapeutic targeting of Rab GTPases in AD, owing to promising results from Rab modulation.
Table 1.
Rab GTPases and their known localisations and functions under physiological conditions are summarised here, including their various links with Parkinson’s Disease (PD), Huntington’s Disease (HD), Dementia with Lewy Bodies (DLB), and Alzheimer’s Disease (AD). Endoplasmic reticulum (ER), trans-Golgi network (TGN), endoplasmic reticulum Golgi intermediate compartment (ERGIC), amyloid beta (Aß), amyloid precursor protein (APP), cerebral spinal fluid (CSF), knockdown (KD), huntingtin (Htt), leucine-rich repeat kinase 2 (LRRK), neurofibrillary tangles (NFT), Htt-associated protein 40 (HAP40).
| Rab GTPase | Localisation | Function | Link with Neurodegenerative Diseases | Citations |
|---|---|---|---|---|
| Rab1A/B |
|
|
PD
|
[17,18,21,22,23,24,25,26] |
| Rab2A |
|
|
HD
|
[27,28,29,30,31] |
| Rab3A/B |
|
|
PD
|
[24,32,33,34,35,36,37,38,39,40,41] |
| Rab4A |
|
|
AD
|
[42,43,44,45,46] |
| Rab5 |
|
|
AD
|
[27,44,45,47,48,49,50,51,52,53,54] |
| Rab6A |
|
|
AD
|
[55,56,57,58,59] |
| Rab7 |
|
|
PD
|
[27,31,44,45,49,51,60,61,62,63,64,65] |
| Rab8 |
|
|
PD
|
[24,66,67,68,69,70,71,72] |
| Rab10 |
|
|
AD
|
[73,74,75,76,77,78] |
| Rab11A/B |
|
|
PD
|
[19,20,79,80,81,82,83,84,85,86,87,88,89,90] |
| Rab13 |
|
|
PD
|
[91,92,93] |
| Rab19 |
|
Unknown | HD
|
[31,94] |
| Rab27b |
|
|
PD
|
[45,95,96,97] |
| Rab29 |
|
|
PD
|
[98,99,100] |
| Rab31 |
|
|
PD
|
[71,101,102,103,104] |
| Rab32 |
|
|
PD
|
[62,105,106,107,108] |
| Rab35 |
|
|
AD
|
[109,110,111] |
| Rab39B |
|
|
PD
|
[69,112,113,114,115] |
AD is the most common form of dementia—currently accounting for ~60–70% of cases [116]. Clinical symptoms of AD include gradual memory loss, cognitive decline, and mood changes. AD is characterised by two main neuropathological hallmarks: amyloid-beta (Aβ) plaques, and hyperphosphorylated tau neurofibrillary tangles (NFTs). Currently available treatments can slow the progression, but do not alter the course of the disease. However, the complex pathways leading to Aβ plaque and NFT formation rely heavily on neuronal protein trafficking, processing, and exocytosis. Indeed, several Rab GTPases have been implicated in these pathologies and are thought to play important roles in the aberrant processing pathways that lead to the aggregation and accumulation of these toxic proteins [117].
3. Rab GTPases and the APP Processing Pathway
3.1. APP Processing Pathway
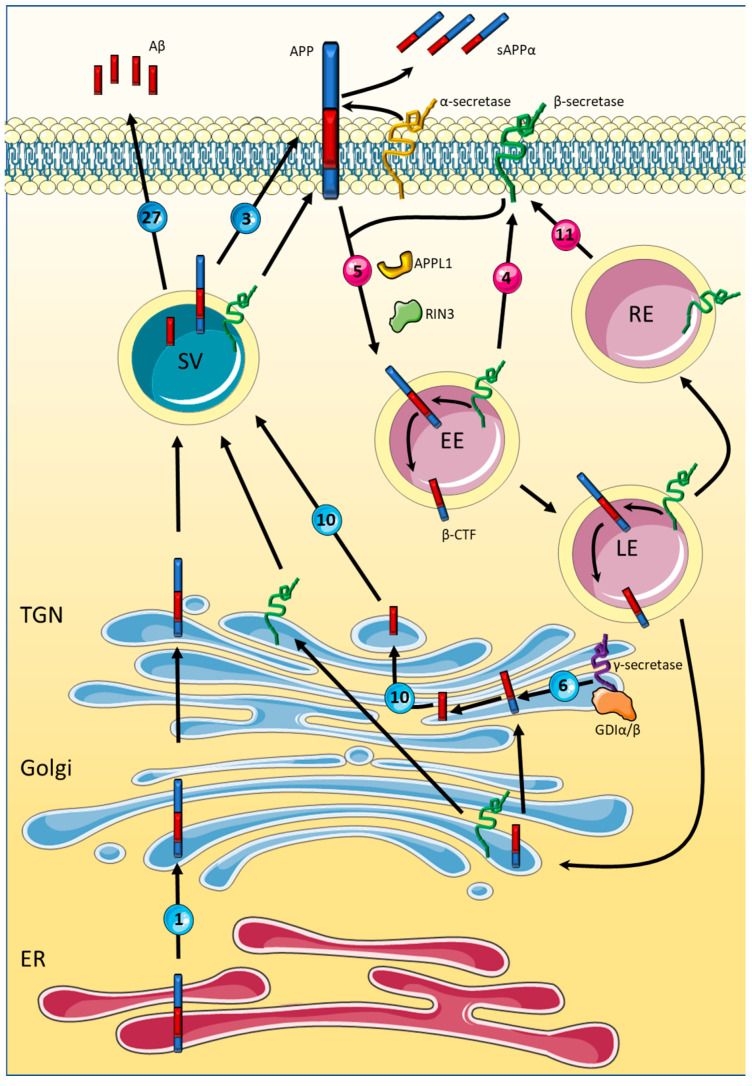
Aβ plaque formation is thought to occur through the progressive aggregation of Aβ peptides, thereby forming oligomers, fibrils, and finally Aβ plaques. Aβ peptides are produced through the sequential cleavage of the amyloid precursor protein (APP). APP has several physiological functions including neuronal survival, synaptogenesis, synaptic plasticity, and neuronal excitability [118], and can be cleaved by two different pathways. The first is considered to be non-amyloidogenic and takes place at the cell surface membrane by an α-secretase. The amyloidogenic pathway requires sequential cleavage by β- and γ-secretases and leads to the production of toxic Aβ peptides. The primary β-secretase responsible for APP cleavage is thought to be Beta-secretase 1 (BACE1) [119], which internalises within endosomes, where it interacts with APP [120]. This accumulation of BACE1 is regulated by the subsequent removal of BACE1 via retrograde endosomal to Golgi transport [121], as well as recycling from the endosomes to the plasma membrane [38]. Following BACE1 cleavage, a γ-secretase protein complex cleaves the APP-produced β-C-terminal fragment (β-CTF) to produce the toxic Aβ peptides [122], which, although largely debated, likely occurs in either the Golgi apparatus [123] or within lysosomes [124]. As the endocytic pathway is essential for the APP amyloidogenic processing pathway, it is therefore unsurprising that several Rab GTPases known to localise and function within the endocytic pathway have been implicated in AD (See Figure 3). Below we discuss several Rabs involved in endocytosis that have been linked to AD, as well as those directly linked to APP processing.
Figure 3.
Rab-mediated amyloid precursor protein metabolism. De novo amyloid precursor protein (APP) is produced with the endoplasmic reticulum (ER) and transported to Golgi for protein maturation via a Rab1 trafficking pathway. Upon passage through the Golgi and trans-Golgi network (TGN), APP resides with the plasma membranes. APP may be processed via the non-amyloidogenic route via α-secretase producing soluble APPα which is released into the extracellular environment. Alternatively, APP along with β-secretases may be internalised via Rab5-dependent endocytosis. Once in the acidic internal compartments of early and late endosomes (EE/LE) the cleavage of APP via β-secretases generates the β-C-terminal fragment (β-CTF). β-secretases is in turn recycled to the plasma membrane either directly via Rab4-mediated traffic, via recycling endosomes (RE) dependent on Rab11 trafficking or trafficking alongside the β-CTF to the Golgi. Within the Golgi and TGN, the γ-secretase complex facilitated by its association with Rab6 processes the β-CTF into β-amyloid (Aβ) which is trafficking into secretary vesicles via Rab10 and released via Rab27/Rab3-dependent process, alongside post Golgi trafficking APP and β-secretase. Also shown is the faciliatory role of Ras and Rab interactor 3 (RIN3) and adaptor protein, phosphotyrosine interacting with PH domain and leucine zipper 1 (APPL1) on Rab5-mediated endocytosis as well as the association of GDP dissociation inhibitors (GDIα/β) with the γ-secretase component presenilin-1. The alternative processing of β-CTF into Aβ within the lysosomes is not shown in this schematic. Rabs more strongly associated with secretory pathways are shaded in blue while those more strongly associated with endosomal pathways are shown in red.
3.2. Rab5
Rab5 is one of the better characterised Rab GTPases and is central to the early endocytic pathway [47,48,49], localising primarily to early endosomes [27]. It is upregulated in several different vulnerable brain areas in AD; the basal forebrain, frontal cortex, and hippocampus in the early stages of AD, and even in mild cognitive impairment (MCI) [44,45]. One of the earliest alterations in AD pathology is the enlargement of Rab5+ early endosomes [50], which can be induced by both APP and β-CTF through the activation of Rab5 [125]. The Rab5 effector APPL1 (adaptor protein, phosphotyrosine interacting with PH domain and leucine zipper 1) is a key protein in β-CTF-dependent endosomal dysfunction and is thought to be recruited by β-CTF to Rab5-positive endosomes where it stabilises the GTP-bound active form of Rab5 associated with the endosome membrane [126]. Through this mechanism, Rab5 becomes overactivated causing pathological endosomal dysfunction and enlargement [126]. Rab5 also upregulates the APP processing pathway when overexpressed in murine cells, significantly increasing the production of both Aβ40 and Aβ42 [52].
These interactions between Rab5 and the APP processing pathway provide a significant therapeutic opportunity and studies have shown benefits from Rab5 modulation. Amyloid precursor protein binding protein 1 (APP-BP1) controls the S to M transition during the cell cycle, and has been shown to bind to APP, inducing neuronal apoptosis [127]. In primary neuronal cultures, exogenous expression of APP-BP1 or APP increases protein levels of Rab5, increasing the number of endosomes and causing endosomal enlargement. Rab5 has been shown to co-localise with and bind to APP-BP1, indicating a possible role in neuronal apoptosis, and subsequent expression of a dominant negative Rab5 further validated this by rescuing apoptosis [128]. Furthermore, a dominant negative Rab5 mutant was able to rescue disrupted axonal transport caused by APP and β-CTF in Drosophila [125]. Taken together, these studies provide evidence that the modulation of Rab5 activity could rescue some of the AD defects caused by endosomal dysfunction.
Additionally, Rab5 effectors also play a role in APP processing and could be targeted. Ras and Rab interactor 3 (RIN3) is a GEF that functions as an effector for Rab5. RIN3 has been identified as a risk factor for both early-onset AD (EOAD) and late-onset AD (LOAD) [129,130]. Using the APP/PS1 mouse model of AD, it was found that RIN3 mRNA and protein levels are increased in the hippocampus and cortex from only 3 months of age, which greatly precedes the formation of Aβ plaques in this model—which usually occurs at ~6–7 months [131]. Overexpression of APP in cultured rat basal forebrain cholinergic neurons (BFCNs) leads to enlarged endosomes and selective upregulation of RIN3 [125], which may indicate a role for RIN3 in this pathology given its links to Rab5 [131]. Notably, RIN3 interacts with the AD risk factor proteins bridging integrator 1 (BIN1) [132] and CD2-associated protein (CD2AP) [133,134], recruiting them to early endosomes. RIN3 and CD2AP function together to increase toxic APP β-CTF production by disrupting BACE1 and APP trafficking [131].
3.3. Other Endosomal Rabs
Additional endosomal Rab GTPases have been implicated in AD. Rab4 is another early endosome Rab upregulated in AD, although not MCI. However, Rab27, which localises to secretory vesicles and the plasma membrane, is upregulated in MCI [45]. Meanwhile, increased levels of Rab6 have been identified in the hippocampus, entorhinal cortex, and temporal cortex during early-stage AD [57], correlating with an increase in binding immunoglobulin protein (BiP), a key marker of ER stress and the unfolded protein response (UPR). Furthermore, Golgi localised Rab6 [55] could play a role in ER stress, increasing retrograde protein transport to the ER, overloading the ER and causing the accumulation of proteins [57]. Indeed, expression of a dominant negative Rab6 mutant increased secretion of the soluble ectodomain s-APPα, which is formed by cleavage of APP by α-secretase, indicating a role for Rab6 in the non-amyloidogenic pathway. It is hypothesised that the dominant negative Rab6 mutant could be facilitating anterograde transport or inhibiting retrograde transport to allow APP to move into the non-amyloidogenic pathway [59]. Rab6 also regulates the membrane association of presenilin 1 [58], mutations of which are common causes of familial AD, suggesting a further pathogenic role for Rab6 in AD.
Rab10 has recently been linked to AD pathology due to its upregulation in the temporal cortex of patient brains [76]. Furthermore, overexpression of Rab10 in mouse neuroblastoma cells significantly increases Aβ production with full length APP levels being unaffected, suggesting that Rab10 function occurs in the later stages of the amyloidogenic pathway [76]. Indeed, levels of sAPP were unaffected in these cells, indicating that Rab10 likely acts after β-secretase cleavage, and instead during γ-secretase cleavage [76]. Importantly, knockdown of Rab10—as well as Rab4 and Rab6A—significantly reduced Aβ levels [38], providing evidence for the therapeutic potential of Rabs in the later stages of Aβ production.
An RNAi screen identified several Rabs as regulators of Aβ and sAPPβ synthesis [38]. When silenced, Rab11A significantly decreased the production of the two proteins. Further experiments identified a crucial role for Rab11 in the recycling of BACE1 through Rab11-positive recycling endosomes [38]. Rab11 also regulates the axonal transport and sorting of BACE1 to presynaptic terminals [135], and contributes to the impaired transcytosis of APP to the soma, a pathology found in familial AD mutant neurons [136]. Critically, in a proteomic study of AD cases, Rab11 expression was notably increased compared to controls [137], consistent with a facilitatory upregulation of the enzyme as part of an overactivation of the amyloidogenic pathways. As Rab11 has shown great potential for other neurodegenerative diseases, these studies suggest that the modulation of Rab11 within the context of AD could have similar benefits.
3.4. ER, Golgi, and Exocytic Rabs
Also involved in the early-stage trafficking of APP is Rab1B, which contributes to protein trafficking between the Golgi and ER [21]. Expression of a GTP-binding defective Rab1B mutant in transformed human embryonic kidney cells inhibited the maturation of APP, thought to occur in the Golgi, providing evidence for the role of Rab1B in the transport of APP from the ER to the Golgi for post-translational modifications [26]. Furthermore, the dominant negative mutant, Rab1BN121I, reduced the secretion of sAPPα from the non-amyloidogenic pathway, and sAPPβ produced by the amyloidogenic pathway, providing further evidence that both pathways are reliant on ER to Golgi transport at an early stage. However, the production of Aβ was also inhibited [26], suggesting another possible therapeutic target (see below for consequences on tau homeostasis). Rab39B is enriched in neuronal cells and localises to the ER, Golgi, and recycling endosomes. Rab39B was shown to co-localise with Aβ plaques in AD cases and Lewy bodies, in dementia with Lewy bodies (DLB) cases, indicating sequestration within these protein aggregates [138]. Whilst there was no change in the cytoplasmic Rab39B levels in AD cases, there was a reduction in DLB cases. This could be due to an increase in active, membrane-associated Rab39B as a compensatory mechanism, or to the sequestration of Rab39B to protein aggregates [138].
Rab3A is also downregulated in AD brains [39], and further work found that Rab3A knockdown decreased the production of Aβ and sAPPβ [38]. Rab3A is involved in exocytosis and is crucial for the formation of vesicles involved in anterograde fast axonal transport of APP to the subsequent cleavage pathways [40]. A study of AD patients identified increased levels of Rab3, and also Rab7, in the CSF, which could indicate a use for them as biomarkers for AD diagnostics, further demonstrating how varied the therapeutic opportunities are for Rabs [41].
In addition to the reported interactions of presenilin 1 with Rab6 [58] and Rab11 [79], the γ-secretase component also directly binds GDIα/β in the ER [58,139]. This association has been speculated to direct GDIs to membranes prior to the recovery of Rab–GDP complexes and thus may serve to prime GDIs for interaction with inactive Rab proteins and subsequently enter them into a reactivation cycle, a process which is anticipated to be enhanced by familial AD presenilin mutations [139]. Furthermore, several proteomic studies have reported the significant upregulation of GDIα and GDIβ in AD brains compared to controls [137,140]. Given that GDIα/β are the predominate regulators for the extraction of Rab–GDP complexes from the membrane prior to reactivation via GEF-mediated GTP exchange [141], such upregulation likely enhances the rate of membrane re-engagement, in turn facilitating the overactivation of membrane trafficking in favour of the amyloidogenic metabolism of APP. Collectively the data highlights GDIs as prominent targets of therapeutic potential.
4. Rab GTPases and Tau Pathology
Intracellular NFTs are another hallmark of AD pathology, caused by the progressive accumulation and aggregation of hyperphosphorylated tau. The occurrence of tau aggregates in AD places this disorder in a family known as tauopathies, which also includes frontotemporal lobar degeneration with tau pathology (FTLD-tau). Although not considered a primary tauopathy, PD also presents with tau pathology. The tau protein is encoded by the MAPT gene, which is located on the long arm of human chromosome 17. Once translated, the mRNA can undergo splicing to form six different isoforms, followed by several different post-translational modifications, including phosphorylation, acetylation, glycosylation, and nitration [142]. Under physiological conditions, approximately 80% of tau in the cell is bound to the microtubules of axons, providing structural integrity and stability [143,144]. The tau protein also plays an important role in regulating axonal transport and cargo shuttling [143]. Pathological hyperphosphorylated tau, as found in tauopathies, dissociates and destabilises microtubules, causing synaptic impairment and subsequent neurodegeneration. Hyperphosphorylated tau can aggregate to form paired helical filaments, which continue to associate in AD to form NFTs. Arguably, tau pathology correlates better with AD-associated disease progression and cognitive decline than Aβ plaques [145,146,147]. Thus, it is possible that targeting tau pathology may provide better clinical outcomes than those obtained with strategies targeting Aβ plaques. Notably, several Rab GTPases have already been implicated in tau pathology.
As tau pathology is present in multiple neurodegenerative diseases, it is not surprising that other proteins linked to tau pathology are common among these disorders. Leucine-rich repeat kinase 2 (LRRK2) mutations are a common genetic cause of PD [148], whilst the R1628P LRRK2 variant increases the risk of AD [149]. Several Rab GTPases, including Rab10, are phosphorylated by LRRK2, which is a member of the leucine-rich repeat kinase family [150]. Furthermore, phosphorylated Rab10 (potentially via LRRK2) has been identified within NFTs, partially co-localising with phosphorylated tau. This suggests that phosphorylated Rab10 may play a role in the pathology and accumulation of NFTs [78], although it is still undetermined if modulation of this Rab could reverse disease phenotypes.
Although NFTs are an intracellular hallmark of AD, pathological tau is also secreted into the CSF. Whilst this secretion could be viewed as somewhat beneficial, as it is clearing misfolded, toxic proteins from the cell, preventing aggregation, it actually correlates closely with neuronal cell death and cognitive decline in tauopathies [151]. Furthermore, secreted tau has been suggested to propagate through the brain once secreted via a prion-like mechanism, although this is a relatively new concept and somewhat controversial, with more studies required [152]. Regardless, secretion of tau to the CSF has been confirmed and several Rabs have been implicated in this process, which could potentially be targeted.
Golgi fragmentation occurs as a result of AD and contributes to defects in neuronal trafficking [153]. Notably, these alterations correlate well with the accumulation of hyperphosphorylated tau into NFTs. Rab1A is involved in ER to Golgi trafficking [154], and its knockdown significantly increases Golgi fragmentation in primary cortical neurons and HeLa cells, leading to an increase in tau secretion [155]. Tau secretion may also be regulated by Rab7A, which is upregulated in AD and mild cognitive impairment (MCI) [44,45]. Rab7A is localised to late endosomes [27] and lysosomes [60], playing key roles in the progression of endocytosis [49] and lysosomal biogenesis [60]. Rab7A is also involved in the maturation of autophagosomes, essential for autophagy [63]. However, the suspected role of Rab7A in AD is central to tau pathology. Rodriguez et al. demonstrated that overexpression of a dominant negative Rab7A mutant significantly decreased the level of tau secreted from both HeLa cells and primary cortical neurons [65]. This was further validated by overexpression of a constituently active form of Rab7A, which caused an increase in tau secretion [65]. These results demonstrate that Rab7A is crucial to the regulation of tau secretory pathway. The upregulation of Rab7A observed in AD brains [51] could indicate a potential mechanism by which tau secretion is increased, correlating with cell death, toxicity, and further propagation through the brain. Thus, modulation of Rab7A activity could be an interesting and novel therapeutic approach for AD.
Tau accumulation can be triggered by high levels of glucocorticoids, the main stress hormones, resulting in neuronal atrophy, cognitive impairment, and synaptic dysfunction [156,157,158]. This accumulation can occur due to the breakdown and dysfunction of the degradative pathways, preventing the degradation of misfolded, pathological tau and clearance from the cell. Rab35 is involved in endocytic recycling of receptors and other membrane proteins, localising to the plasma membrane [109]. It is a key protein in the endosomal sorting complex required for transport (ESCRT) pathway, which is involved in the degradation of ubiquitylated proteins in multivesicular bodies (MVBs). Tau has been detected in these MVBs and shown to be degraded via lysosomes mediated by the ESCRT pathway. Vaz-Silva and colleagues demonstrated that glucocorticoids suppress Rab35 expression, which in turn inhibits the degradation of tau via the ESCRT pathway, leading to accumulation and toxicity. Importantly, overexpression of Rab35 upregulates the degradation of tau and rescues the associated neuronal atrophy caused by the toxic accumulation of tau [111].
Rab effectors have also been linked to tau pathology. BIN1 is a trafficking protein that has been identified as an AD risk factor [159], in particular, interacting with the processing pathways of tau aggregates [132]. RIN3, a Rab5 guanine exchange factor (GEF), has been shown to recruit BIN1 to the early endosomes, as previously discussed, where it is thought they work together to upregulate levels of hyperphosphorylated tau [131]. However, the exact mechanisms of how these Rab effectors and other trafficking proteins interact with tau pathology still requires further research, although they may provide an interesting therapeutic target that could be used to modulate tau pathology.
Perhaps the most prominent GEF associated with neurodegeneration is Chromosome 9 open reading frame 72 (C9orf72). Familial hexanucleotide GGGGCC repeat expansion in the C9orf72 gene accounts for a third of familial amyotrophic lateral sclerosis and a quarter of frontotemporal dementia (FTD) cases, leading to its haploinsufficiency and inducing the formation of RNA-rich nuclear aggregates [160]. Whilst the association of C9orf72 hexanucleotide expansions with AD is controversial [161,162,163,164], meta-analysis supports an increased risk for AD [165]. In any case, C9orf72 expansion carriers present with robust AD-like tau pathology [166] and in AD, independent of gene mutation, the C9orf72 protein accumulates within hyperphosphorylated tau bearing dystrophic neurites associated with Aβ plaques [167]. Together the studies suggest dysfunction of C9orf72 as being common to AD and likely contributory to the mechanisms leading to the accumulation of tau pathology. Critically, C9orf72 associates with a number of Rab proteins [168] and is an effector of Rab1A [169]. C9orf72 also complexes with SMCR8 and WDR41, for which both Rab8A and Rab39 GEF [69], and Rab8A and Rab11B GAP activity [170] has been reported. Functionally, the modulation of Rab activity via C9orf72 appears to regulate autophagic flux [69,169,171], but also the surface expression of glutamate receptors [172], thus implicating a dysfunction of C9orf72 as contributory to both pathological tau accumulation and disease-mediated changes in neuronal signalling.
5. Pharmacological Targeting of Rab GTPases
As with all central nervous system diseases, the development of effective interventions is challenging. This is, in part, due to the low bioavailability of pharmacological drugs in the brain caused by the impermeably of the blood–brain barrier, but also due to complex issues relating to the targeting of specific brain regions, cell types or even neuronal subtypes. Furthermore, drug development towards the modulation of Rab proteins can be considered additionally problematic due to the largely as yet unresolved nature of their endogenous regulation, in addition to the high degree of homology amongst Rab family members and with other small GTPase families such as Rho and RAS proteins. Yet the integral involvement of Rab proteins in the pathology of, not only AD, but in numerous other diseases, including other neurodegenerative disorders, makes them an enticing target for therapeutics. At a conceptual level, there exist multiple routes in which the activity of Rab proteins can be modulated, including the targeting of (1) Rab protein binding of GTP and subsequent activation, (2) processes underlying Rab prenylation and other post-translational modifications, and (3) Rab effector proteins. Below we highlight several approaches which have yielded relative success and may, in turn, be built upon for future therapeutic development.
5.1. Competitive Antagonists and Allosteric Modulators of Rab Proteins
Of all the mechanisms employed to pharmacologically target enzymatic activity, competitive antagonism of nucleotide engagement is by far the most common. However, small GTPs such as Rhos, RACs, and Rabs have an extremely high affinity for GTP, which has largely ruled out the use of such an approach for Rab-targeted drug design. One exception to this is CID1067700, a small molecule identified from >3000 compounds via high-throughput screening, as the sole candidate capable of competing GTP for Rab binding [173]. This action, although greatest for Rab7, was largely non-specific, with CID1067700 inhibiting other Rabs and the related GTPases Rho and RAC. In addition, the induced antagonism was highly sensitive to GTP concentrations in vitro, raising concerns of efficiency at physiological GTP concentrations. Nevertheless, several studies have reported favourable outcomes of Rab7 inhibition following CID1067700 intervention in rodent models of ischemic stroke [174] and lupus [175]. Given the increased Rab7a expression in AD and its role in the secretion and potential spread of tau pathology, an evaluation of CID1067700 administration in pre-clinical models would seem warranted, with the caveat that inhibition of autophagic flux may negatively impact upon Aβ and, indeed, the viability of pathology-bearing cells. Regardless of the therapeutic relevance of such a compound, these studies nevertheless set a precedent for the effective targeting of specific Rab proteins via competitive GTP antagonism.
Akin to the limited success of direct Rab antagonism, few allosteric modulators of Rab proteins have been reported. Nonetheless, recent structural analyses of the small GTPases RAS, Rab1, and Rab11 have facilitated the identification of allosteric binding sites with the potential for modulating GTP/GDP binding. Whilst structurally conserved, these sites are not identical in sequence and may provide scope for the development of specific ligands for the differential targeting of many of the Rab protein family members [176,177]. Indeed, several small molecules capable of interacting with such sites in Rab11 have been reported, with the drugs displaying preferential binding when Rab11 is in various states of nucleotide association, presumably enabling the potential for allosteric activation or inhibition [177]. Given the multiple roles for Rab11-mediated trafficking in Aβ production, and its upregulated expression in AD (as above), determining the consequence of these drugs on APP metabolism in cellular systems may uncover potential therapeutic benefits.
Different studies report on the potential of small molecules to act as allosteric activators of Rabs, as these compounds act to stabilise the binding of GTP to Rabs and, therefore, can be considered to facilitate prolonged Rab activation. Given that a number of studies appear to a support a protective role for the overexpression of specific Rab proteins in various neurodegenerative diseases, such compounds may hold promise in stimulating Rab proteins reportedly inhibited as a consequence of the AD process. However, to date, work in this line of investigation has been limited and has primarily focused on a small library of compounds, initially identified from a screening of 20,000 molecules [178]. From three chemical families (nicotinic, indole, and salicylic acids) 43 compounds with activation properties across the GTPase families (Rac Rho, Rabs) have been identified, with the salicylic acid compounds CID 3338522, CID 7721337 and CID 1508555, being relatively selective for Rab2 and or Rab7 activation within the nM range [179]. Despite scant research in this area, advances in understanding of the conformational changes in Rab proteins following changes in activation states, and the determination of potential allosteric sites for the stabilisation of such conformations, are likely to bring new renewed potential for the development of selective allosteric activators and inhibitors in the future [180].
5.2. Prenylation Inhibitors
Given that many Rab proteins are reported as dysfunctional and largely overactive in AD, the uses of selective modulators targeting one specific Rab family member may not meaningfully impact their facilitatory role in AD pathogenesis. Therefore, a more broad-spectrum approach may arguably be more beneficial in reducing this pathological overactivation. The generalised downregulation of Rab activity may be achieved by the selective targeting of common modifiers to all Rab proteins. Indeed, there is evidence to justify the targeting of upstream proteins, as elevated levels of the isoprenoids geranylgeranyl diphosphate (GGDP) and farnesylpyrophosphate (FPP)—essential substrates of FTase, GGTaseI, and Rab GGTase II prenylation—have been found in AD brains [181]. In cancers, where the overactivation of small GTPase proteins is also observed, efforts have largely focused on the inhibition of prenylation. However, many of the lead compounds have been developed to inhibit prenylation enzymes such as farnesyl transferase and/or GGTase I and not Rab GGTase II, prioritising the inhibition of Rac and Rho small GTPases, as opposed to Rabs [182,183,184]. Nevertheless, [3-PEHPC 2-(3-pyridinyl)-1-hydroxyethylidene-1,1-phosphonocarboxylic acid] and [3-IPEHPC 2-Hydroxy-3-imidazo [1,2-a]pyridin-3-yl-2-phosphonopropionic acid], as well as psoromic acid, have been identified as specific Rab GGTase inhibitors and have been used in a variety of assays to establish effective inhibitory effects on Rab activity [185,186,187,188]. Despite their proven cellular efficacy, the inhibition of Rab activity via such compounds in AD models remains unexplored. As an alternative to the direct inhibition of Rab GGTases, the upstream inhibition of enzymes responsible for the production of GGDP also offers the potential for broad-spectrum Rab inhibition. Interestingly the depletion of isoprenoid GGDP, and thus Rab inhibition, has been associated with a pleiotropic effect of statins which can reduce Aβ production in cell lines, independent of any effects on cholesterol [189]. Despite evidence for the effectiveness of brain isoprenoid GGDP depletion and small GTPase inhibition in vivo at clinically relevant statin concentrations [189], and early reports of the protective effect of statins against AD [190,191,192], more recent studies have had contradictory outcomes [193]. Notably, specific geranylgeranyl diphosphate synthase inhibitors have recently been developed [194,195]. When tested in AD models, these may prove more readily beneficial in contrast to specific statins which have a range of pharmacological actions and, consequently, may not act via a direct consequence of their efficacy towards Rab inhibition [196].
5.3. Modulators of Rab Effectors
Further potential for Rab protein modulation may lie in the targeting of other Rab effectors such as GEFs, GAPs, and GDIs. Yet, despite the potential for their targeting, the identification of these effectors is generally lacking, particularly for GEFs, for which there exists a significant proportion of Rab family members without a characterised GEF. In recent years, however, progress has been made in identifying proteins with GEF activity, with DENN-domain-containing proteins, by far, forming the major group of GEF proteins within a diverse list of activators [197,198]. In contrast, the prominence of Tre-2/Bub2/Cdc16 (TBC) domains in the majority of GAPs has allowed for a large number of TBC-containing proteins to be screened for GAP activity against many different Rab proteins, enabling a rather comprehensive list of molecules capable of deactivating Rab proteins via the facilitation of GTP hydrolysis [199]. Unfortunately, at present, little is known about the potential modulators of Rab GEF and GAPs. Nevertheless, considerable work has been conducted into RAS and Rho GAP/GEF inhibitors, which have identified a variety of mechanistic approaches for influencing regulatory processes [200] that could, in turn, be translated for Rab modulation in the future.
Instead, targeting upstream regulatory kinases of Rab proteins and their effectors may be more immediately accessible. To date, direct Rab protein phosphorylation has been attributed to cyclin-dependent kinase 1, leucine-enriched kinase 1 and 2, multiple protein kinase C isoforms, TANK-binding kinase 1, transforming growth factor-β-activated kinase-1, and tyrosine kinase Src [198]. Rab phosphorylation typically interferes with their association with particular effectors and, consequently, can facilitate or inhibit Rab-mediated trafficking, depending on the nature of the disrupted interaction. For example, phosphomimetic studies of LRRK2 substrate Rabs demonstrate decreased associations with GDI, which in turn can be anticipated to slow the cycling of membrane-bound Rab–GDP complexes into the cytoplasm for reactivation [201]. Amongst those regulated by LRRK2 are Rab3 and Rab10, which have been highlighted as overactive and facilitatory of Aβ exocytosis and, as such, facilitating LRRK2 phosphorylation may be considered a potential point for pharmacological intervention. However, given the association of LRRK2 mutations with familial PD [202], and its kinases reported overactivity in idiopathic cases [203], establishing a safe therapeutic window for its modulation may not be possible. Alternatively, emerging regulatory pathways for GAP proteins may offer improved potential for exploitation, as highlighted by the recent characterisation of lemur tyrosine kinase 1 (LMTK1). Both Rab11-GAP TBC1D9A and Rab1-GAP TBC1D20 are regulated via LMTK1 interactions with direct phosphorylation of these GAPs assumed responsible for their enhanced functionality and, consequently, the deactivation of Rab proteins [204]. Interestingly, a single nucleotide polymorphism associated with the reduced expression of the LMTK1 gene (AATK1) has been identified as an FTD risk factor within an Italian cohort [205], suggesting that abnormal GAP regulation may be a contributory factor in tau pathology, as well as potentially in the amyloidogenic processing of APP.
Likewise, the upstream regulation of GEFs may be exploitable, as G-protein-coupled-receptor- (GPCR) mediated regulation of Rab39B within striatal neurons has been demonstrated via GPR-52 in a cyclic-AMP-dependent manner [206]. Thus, targeting of GPCRs, and potentially modulation of cAMP levels, may be able to modulate GEF activity, with both inhibitory and excitatory outcomes for selective Rab proteins. Such work suggests the manipulation of upstream receptors, kinase, and/or second messengers as points of potential therapeutic intervention, with the hope that, in the future, further delineation of these regulatory pathways—and potential others related to additional Rab proteins—may expand the scope of approach.
5.4. Pathogen-Secreted Rab Effectors
A final consideration towards identifying approaches for the modulation of Rab activity can be taken from infectious pathogens. In order to maintain their intracellular presence and to avoid degradation, invading bacteria and viruses secrete an array of molecules targeting different molecular components of endosomal trafficking, effectively hijacking these routes to meet their own requirements [207]. Many of these secreted molecules directly interact with Rab proteins and their effectors. For example, Chlamydia trachomatis produce an inclusion membrane protein (CT2999) which binds and sequesters a number of active Rab–GTP complexes, consequently suppressing host cell endosomal trafficking [208]. Likewise, Coxiella burnetiid secrete both a prokaryotic kinase (Coxiella Ser/Thr kinase) which interacts with the Rab7 GAP TBC1D5 to enhance Rab7 activity, which is required for the production of Coxiella-containing vacuoles [209] and also Coxiella vacuolar protein F, which directly associates with Rab26 and consequently enhances host cell autophagic degradation [210]. In fact, various invading pathogens have evolved an arsenal of molecules capable of subverting host Rab-mediated trafficking. For example, Legionella pneumophila secretes molecular mimics of Rab1 GEF and GAPs thus allowing for the modulation of the Rab1 activation/deactivation cycle [211]. Even multiple Rab-interacting non-structural proteins secreted by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have been highlighted as prospects for drug repurposing [212]. Although as yet unexploited, the array of pathogen-generated molecules capable of selectively manipulating intracellular trafficking routes may yield novel and effective means of addressing both the overactivation and suppression of Rab-mediated trafficking as part of the pathology of AD and other diseases.
Collectively, the studies reviewed above suggest that significant progress has been made in targeting the once-thought ‘undruggable’ Rab protein network. In the future, advances in the characterisation of endogenous Rab regulation, the identification of additional Rab interaction partners, and further study of the role of Rabs in infectious diseases may provide a critical insight into targeting Rabs. Ultimately, such work may aid in generating a tool box of compounds with improved specificity for single families of GTPases (Rabs Cf. Rho Cf. RAS GTPases) and the capability of either selectively targeting individual Rab proteins or particular functional trafficking routes (endosomal Cf. exosomal, etc.), which may one day progress to the clinic.
6. Final Considerations
The studies discussed herein provide strong evidence that Rab GTPases are not only heavily involved in AD pathology, but also that modulation of Rab expression and activity could rescue associated defects and toxicity. Focusing on such a large protein family provides many different therapeutic targets that could be exploited at many stages of the disease. It also offers the potential for a multifaceted approach to treatment, incorporating different Rabs to target multiple aspects of AD pathology at once. Although therapeutic targeting and modulation of these small proteins has proven to be difficult in the past, the approaches outlined above, aimed at targeting Rab GTP binding, post-translational modifications, and Rab effectors, have had promising early success and could be developed further into effective therapeutic strategies. Before these strategies can reach the clinic, the common issues with targeting neurodegenerative diseases will need to be addressed, such as the crossing of the blood–brain barrier, as well as more Rab-specific concerns including a lack of specificity and low binding affinities. Whilst the approaches summarised in this review have had success, there is much more research required in pre-clinical models to fully understand potential off-target effects and how these modulations could affect other aspects of AD pathology as a whole. It is vital that research in this field continues to dig deeper into the various pathological roles of Rabs and their effectors in AD, and in the wider context of neurodegeneration, to further elucidate the complex mechanisms involved and discover more potential therapeutic targets.
Author Contributions
Conceptualization, K.L.J., D.J.K., T.F.O. and F.G.; Writing—Original Draft Preparation, K.L.J. and D.J.K.; Writing—Review and Editing, K.L.J., D.J.K., T.F.O. and F.G. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
K.L.J. is funded by a Ph.D. studentship from the College of Life Sciences, University of Leicester, UK. D.K. is funded by the Lewy Body Society (LBS- LBS-0007). F.G. is funded by the Medical Research Council (MR/R011621/1). Open access funding provided by the Leicester Research Archive, University of Leicester.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Colicelli J. Human RAS superfamily proteins and related GTPases. Sci. STKE. 2004;2004:re13. doi: 10.1126/stke.2502004re13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li G., Marlin M.C. Rab family of GTPases. Methods Mol. Biol. 2015;1298:1–15. doi: 10.1007/978-1-4939-2569-8_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang J., Schulze K.L., Hiesinger P.R., Suyama K., Wang S., Fish M., Acar M., Hoskins R.A., Bellen H.J., Scott M.P. Thirty-one flavors of Drosophila rab proteins. Genetics. 2007;176:1307–1322. doi: 10.1534/genetics.106.066761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gallegos M.E., Balakrishnan S., Chandramouli P., Arora S., Azameera A., Babushekar A., Bargoma E., Bokhari A., Chava S.K., Das P., et al. The C. elegans rab family: Identification, classification and toolkit construction. PLoS ONE. 2012;7:e49387. doi: 10.1371/journal.pone.0049387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pereira-Leal J.B., Seabra M.C. Evolution of the rab family of small GTP-binding proteins. J. Mol. Biol. 2001;313:889–901. doi: 10.1006/jmbi.2001.5072. [DOI] [PubMed] [Google Scholar]
- 6.Stenmark H., Olkkonen V.M. The Rab GTPase family. Genome Biol. 2001;2:reviews3007.1. doi: 10.1186/gb-2001-2-5-reviews3007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hutagalung A.H., Novick P.J. Role of Rab GTPases in membrane traffic and cell physiology. Physiol. Rev. 2011;91:119–149. doi: 10.1152/physrev.00059.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Müller M.P., Goody R.S. Molecular control of Rab activity by GEFs, GAPs and GDI. Small GTPases. 2018;9:5–21. doi: 10.1080/21541248.2016.1276999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chavrier P., Gorvel J.P., Stelzer E., Simons K., Gruenberg J., Zerial M. Hypervariable C-terminal domain of rab proteins acts as a targeting signal. Nature. 1991;353:769–772. doi: 10.1038/353769a0. [DOI] [PubMed] [Google Scholar]
- 10.Ueda S., Tamura N., Mima J. Membrane Tethering Potency of Rab-Family Small GTPases Is Defined by the C-Terminal Hypervariable Regions. Front. Cell Dev. Biol. 2020;8:577342. doi: 10.3389/fcell.2020.577342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pereira-Leal J.B., Hume A.N., Seabra M.C. Prenylation of Rab GTPases: Molecular mechanisms and involvement in genetic disease. FEBS Lett. 2001;498:197–200. doi: 10.1016/S0014-5793(01)02483-8. [DOI] [PubMed] [Google Scholar]
- 12.Pfeffer S.R. Rab GTPases: Specifying and deciphering organelle identity and function. Trends Cell Biol. 2001;11:487–491. doi: 10.1016/S0962-8924(01)02147-X. [DOI] [PubMed] [Google Scholar]
- 13.Li G. Rab GTPases, membrane trafficking and diseases. Curr. Drug Targets. 2011;12:1188–1193. doi: 10.2174/138945011795906561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kiral F.R., Kohrs F.E., Jin E.J., Hiesinger P.R. Rab GTPases and Membrane Trafficking in Neurodegeneration. Curr. Biol. 2018;28:R471–R486. doi: 10.1016/j.cub.2018.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arrazola Sastre A., Luque Montoro M., Lacerda H.M., Llavero F., Zugaza J.L. Small GTPases of the Rab and Arf Families: Key Regulators of Intracellular Trafficking in Neurodegeneration. Int. J. Mol. Sci. 2021;22:4425. doi: 10.3390/ijms22094425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bearer E.L., Wu C. Herpes Simplex Virus, Alzheimer’s Disease and a Possible Role for Rab GTPases. Front. Cell Dev. Biol. 2019;7:134. doi: 10.3389/fcell.2019.00134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cooper A.A., Gitler A.D., Cashikar A., Haynes C.M., Hill K.J., Bhullar B., Liu K., Xu K., Strathearn K.E., Liu F., et al. Alpha-synuclein blocks ER-Golgi traffic and Rab1 rescues neuron loss in Parkinson’s models. Science. 2006;313:324–328. doi: 10.1126/science.1129462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coune P.G., Bensadoun J.C., Aebischer P., Schneider B.L. Rab1A over-expression prevents Golgi apparatus fragmentation and partially corrects motor deficits in an alpha-synuclein based rat model of Parkinson’s disease. J. Parkinson’s Dis. 2011;1:373–387. doi: 10.3233/JPD-2011-11058. [DOI] [PubMed] [Google Scholar]
- 19.Breda C., Nugent M.L., Estranero J.G., Kyriacou C.P., Outeiro T.F., Steinert J.R., Giorgini F. Rab11 modulates α-synuclein-mediated defects in synaptic transmission and behaviour. Hum. Mol. Genet. 2014;24:1077–1091. doi: 10.1093/hmg/ddu521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richards P., Didszun C., Campesan S., Simpson A., Horley B., Young K.W., Glynn P., Cain K., Kyriacou C.P., Giorgini F., et al. Dendritic spine loss and neurodegeneration is rescued by Rab11 in models of Huntington’s disease. Cell Death Differ. 2011;18:191–200. doi: 10.1038/cdd.2010.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Plutner H., Cox A.D., Pind S., Khosravi-Far R., Bourne J.R., Schwaninger R., Der C.J., Balch W.E. Rab1b regulates vesicular transport between the endoplasmic reticulum and successive Golgi compartments. J. Cell Biol. 1991;115:31–43. doi: 10.1083/jcb.115.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saraste J., Lahtinen U., Goud B. Localization of the small GTP-binding protein rab1p to early compartments of the secretory pathway. J Cell Sci. 1995;108((Pt 4)):1541–1552. doi: 10.1242/jcs.108.4.1541. [DOI] [PubMed] [Google Scholar]
- 23.Yang X.Z., Li X.X., Zhang Y.J., Rodriguez-Rodriguez L., Xiang M.Q., Wang H.Y., Zheng X.F.S. Rab1 in cell signaling, cancer and other diseases. Oncogene. 2016;35:5699–5704. doi: 10.1038/onc.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gitler A.D., Bevis B.J., Shorter J., Strathearn K.E., Hamamichi S., Su L.J., Caldwell K.A., Caldwell G.A., Rochet J.-C., McCaffery J.M., et al. The Parkinson’s disease protein alpha-synuclein disrupts cellular Rab homeostasis. Proc. Natl. Acad. Sci. USA. 2008;105:145–150. doi: 10.1073/pnas.0710685105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Winslow A.R., Chen C.-W., Corrochano S., Acevedo-Arozena A., Gordon D.E., Peden A.A., Lichtenberg M., Menzies F.M., Ravikumar B., Imarisio S., et al. α-Synuclein impairs macroautophagy: Implications for Parkinson’s disease. J. Cell Biol. 2010;190:1023–1037. doi: 10.1083/jcb.201003122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dugan J.M., deWit C., McConlogue L., Maltese W.A. The Ras-related GTP-binding protein, Rab1B, regulates early steps in exocytic transport and processing of beta-amyloid precursor protein. J. Biol. Chem. 1995;270:10982–10989. doi: 10.1074/jbc.270.18.10982. [DOI] [PubMed] [Google Scholar]
- 27.Chavrier P., Parton R.G., Hauri H.P., Simons K., Zerial M. Localization of low molecular weight GTP binding proteins to exocytic and endocytic compartments. Cell. 1990;62:317–329. doi: 10.1016/0092-8674(90)90369-P. [DOI] [PubMed] [Google Scholar]
- 28.Lőrincz P., Tóth S., Benkő P., Lakatos Z., Boda A., Glatz G., Zobel M., Bisi S., Hegedűs K., Takáts S., et al. Rab2 promotes autophagic and endocytic lysosomal degradation. J. Cell Biol. 2017;216:1937–1947. doi: 10.1083/jcb.201611027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saraste J. Spatial and Functional Aspects of ER-Golgi Rabs and Tethers. Front. Cell Dev. Biol. 2016;4:28. doi: 10.3389/fcell.2016.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ding X., Jiang X., Tian R., Zhao P., Li L., Wang X., Chen S., Zhu Y., Mei M., Bao S., et al. Rab2 regulates the formation of autophagosome and autolysosome in mammalian cells. Autophagy. 2019;15:1774–1786. doi: 10.1080/15548627.2019.1596478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.White J.A., 2nd, Anderson E., Zimmerman K., Zheng K.H., Rouhani R., Gunawardena S. Huntingtin differentially regulates the axonal transport of a sub-set of Rab-containing vesicles in vivo. Hum. Mol. Genet. 2015;24:7182–7195. doi: 10.1093/hmg/ddv415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Darchen F., Goud B. Multiple aspects of Rab protein action in the secretory pathway: Focus on Rab3 and Rab6. Biochimie. 2000;82:375–384. doi: 10.1016/S0300-9084(00)00219-4. [DOI] [PubMed] [Google Scholar]
- 33.Schlüter O.M., Khvotchev M., Jahn R., Südhof T.C. Localization versus function of Rab3 proteins. Evidence for a common regulatory role in controlling fusion. J. Biol. Chem. 2002;277:40919–40929. doi: 10.1074/jbc.M203704200. [DOI] [PubMed] [Google Scholar]
- 34.Chen R.H.C., Wislet-Gendebien S., Samuel F., Visanji N.P., Zhang G., Marsilio D., Langman T., Fraser P.E., Tandon A. α-Synuclein membrane association is regulated by the Rab3a recycling machinery and presynaptic activity. J. Biol. Chem. 2013;288:7438–7449. doi: 10.1074/jbc.M112.439497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chung C.Y., Koprich J.B., Hallett P.J., Isacson O. Functional enhancement and protection of dopaminergic terminals by Rab3B overexpression. Proc. Natl. Acad. Sci. USA. 2009;106:22474–22479. doi: 10.1073/pnas.0912193106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bereczki E., Francis P.T., Howlett D., Pereira J.B., Höglund K., Bogstedt A., Cedazo-Minguez A., Baek J.H., Hortobágyi T., Attems J., et al. Synaptic proteins predict cognitive decline in Alzheimer’s disease and Lewy body dementia. Alzheimer’s Dement. 2016;12:1149–1158. doi: 10.1016/j.jalz.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 37.Hong Y., Zhao T., Li X.-J., Li S. Mutant Huntingtin Impairs BDNF Release from Astrocytes by Disrupting Conversion of Rab3a-GTP into Rab3a-GDP. J. Neurosci. 2016;36:8790–8801. doi: 10.1523/JNEUROSCI.0168-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Udayar V., Buggia-Prévot V., Guerreiro R.L., Siegel G., Rambabu N., Soohoo A.L., Ponnusamy M., Siegenthaler B., Bali J., Guerreiro R., et al. A paired RNAi and RabGAP overexpression screen identifies Rab11 as a regulator of β-amyloid production. Cell Rep. 2013;5:1536–1551. doi: 10.1016/j.celrep.2013.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reddy P.H., Mani G., Park B.S., Jacques J., Murdoch G., Whetsell W., Jr., Kaye J., Manczak M. Differential loss of synaptic proteins in Alzheimer’s disease: Implications for synaptic dysfunction. J Alzheimer’s Dis. 2005;7:103–117. doi: 10.3233/JAD-2005-7203. [DOI] [PubMed] [Google Scholar]
- 40.Szodorai A., Kuan Y.-H., Hunzelmann S., Engel U., Sakane A., Sasaki T., Takai Y., Kirsch J., Müller U., Beyreuther K., et al. APP anterograde transport requires Rab3A GTPase activity for assembly of the transport vesicle. J. Neurosci. 2009;29:14534–14544. doi: 10.1523/JNEUROSCI.1546-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Armstrong A., Mattsson N., Appelqvist H., Janefjord C., Sandin L., Agholme L., Olsson B., Svensson S., Blennow K., Zetterberg H., et al. Lysosomal network proteins as potential novel CSF biomarkers for Alzheimer’s disease. Neuromolecular Med. 2014;16:150–160. doi: 10.1007/s12017-013-8269-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Van Der Sluijs P., Hull M., Zahraoui A., Tavitian A., Goud B., Mellman I. The small GTP-binding protein rab4 is associated with early endosomes. Proc. Natl. Acad. Sci. USA. 1991;88:6313–6317. doi: 10.1073/pnas.88.14.6313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McCaffrey M.W., Bielli A., Cantalupo G., Mora S., Roberti V., Santillo M., Drummond F., Bucci C. Rab4 affects both recycling and degradative endosomal trafficking. FEBS Lett. 2001;495:21–30. doi: 10.1016/S0014-5793(01)02359-6. [DOI] [PubMed] [Google Scholar]
- 44.Ginsberg S.D., Alldred M.J., Counts S.E., Cataldo A.M., Neve R.L., Jiang Y., Wuu J., Chao M.V., Mufson E.J., Nixon R.A., et al. Microarray analysis of hippocampal CA1 neurons implicates early endosomal dysfunction during Alzheimer’s disease progression. Biol. Psychiatry. 2010;68:885–893. doi: 10.1016/j.biopsych.2010.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ginsberg S.D., Mufson E.J., Alldred M.J., Counts S.E., Wuu J., Nixon R.A., Che S. Upregulation of select rab GTPases in cholinergic basal forebrain neurons in mild cognitive impairment and Alzheimer’s disease. J. Chem. Neuroanat. 2011;42:102–110. doi: 10.1016/j.jchemneu.2011.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.White J.A., 2nd, Krzystek T.J., Hoffmar-Glennon H., Thant C., Zimmerman K., Iacobucci G., Vail J., Thurston L., Rahman S., Gunawardena S. Excess Rab4 rescues synaptic and behavioral dysfunction caused by defective HTT-Rab4 axonal transport in Huntington’s disease. Acta Neuropathol. Commun. 2020;8:97. doi: 10.1186/s40478-020-00964-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bucci C., Parton R.G., Mather I.H., Stunnenberg H., Simons K., Hoflack B., Zerial M. The small GTPase rab5 functions as a regulatory factor in the early endocytic pathway. Cell. 1992;70:715–728. doi: 10.1016/0092-8674(92)90306-W. [DOI] [PubMed] [Google Scholar]
- 48.Gorvel J.-P., Chavrier P., Zerial M., Gruenberg J. rab5 controls early endosome fusion in vitro. Cell. 1991;64:915–925. doi: 10.1016/0092-8674(91)90316-Q. [DOI] [PubMed] [Google Scholar]
- 49.Rink J., Ghigo E., Kalaidzidis Y., Zerial M. Rab conversion as a mechanism of progression from early to late endosomes. Cell. 2005;122:735–749. doi: 10.1016/j.cell.2005.06.043. [DOI] [PubMed] [Google Scholar]
- 50.Cataldo A.M., Barnett J.L., Pieroni C., Nixon R.A. Increased Neuronal Endocytosis and Protease Delivery to Early Endosomes in Sporadic Alzheimer’s Disease: Neuropathologic Evidence for a Mechanism of Increased β-Amyloidogenesis. J. Neurosci. 1997;17:6142. doi: 10.1523/JNEUROSCI.17-16-06142.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ginsberg S.D., Mufson E.J., Counts S.E., Wuu J., Alldred M.J., Nixon R.A., Che S. Regional selectivity of rab5 and rab7 protein upregulation in mild cognitive impairment and Alzheimer’s disease. J. Alzheimer’s Dis. 2010;22:631–639. doi: 10.3233/JAD-2010-101080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Grbovic O.M., Mathews P.M., Jiang Y., Schmidt S.D., Dinakar R., Summers-Terio N.B., Ceresa B.P., Nixon R.A., Cataldo A.M. Rab5-stimulated up-regulation of the endocytic pathway increases intracellular beta-cleaved amyloid precursor protein carboxyl-terminal fragment levels and Abeta production. J. Biol. Chem. 2003;278:31261–31268. doi: 10.1074/jbc.M304122200. [DOI] [PubMed] [Google Scholar]
- 53.Pal A., Severin F., Lommer B., Shevchenko A., Zerial M. Huntingtin-HAP40 complex is a novel Rab5 effector that regulates early endosome motility and is up-regulated in Huntington’s disease. J. Cell Biol. 2006;172:605–618. doi: 10.1083/jcb.200509091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ravikumar B., Imarisio S., Sarkar S., O’Kane C.J., Rubinsztein D.C. Rab5 modulates aggregation and toxicity of mutant huntingtin through macroautophagy in cell and fly models of Huntington disease. J. Cell Sci. 2008;121:1649–1660. doi: 10.1242/jcs.025726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Goud B., Zahraoui A., Tavitian A., Saraste J. Small GTP-binding protein associated with Golgi cisternae. Nature. 1990;345:553–556. doi: 10.1038/345553a0. [DOI] [PubMed] [Google Scholar]
- 56.Grigoriev I., Splinter D., Keijzer N., Wulf P.S., Demmers J., Ohtsuka T., Modesti M., Maly I.V., Grosveld F., Hoogenraad C.C., et al. Rab6 regulates transport and targeting of exocytotic carriers. Dev. Cell. 2007;13:305–314. doi: 10.1016/j.devcel.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 57.Scheper W., Hoozemans J.J., Hoogenraad C.C., Rozemuller A.J., Eikelenboom P., Baas F. Rab6 is increased in Alzheimer’s disease brain and correlates with endoplasmic reticulum stress. Neuropathol. Appl. Neurobiol. 2007;33:523–532. doi: 10.1111/j.1365-2990.2007.00846.x. [DOI] [PubMed] [Google Scholar]
- 58.Scheper W., Zwart R., Baas F. Rab6 membrane association is dependent of Presenilin 1 and cellular phosphorylation events. Mol. Brain Res. 2004;122:17–23. doi: 10.1016/j.molbrainres.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 59.McConlogue L., Castellano F., deWit C., Schenk D., Maltese W. Differential Effects of a Rab6 Mutant on Secretory Versus Amyloidogenic Processing of Alzheimers -Amyloid Precursor Protein. J. Biol. Chem. 1996;271:1343–1348. doi: 10.1074/jbc.271.3.1343. [DOI] [PubMed] [Google Scholar]
- 60.Bucci C., Thomsen P., Nicoziani P., McCarthy J., van Deurs B. Rab7: A key to lysosome biogenesis. Mol. Biol. Cell. 2000;11:467–480. doi: 10.1091/mbc.11.2.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Harrison R.E., Bucci C., Vieira O.V., Schroer T.A., Grinstein S. Phagosomes fuse with late endosomes and/or lysosomes by extension of membrane protrusions along microtubules: Role of Rab7 and RILP. Mol. Cell. Biol. 2003;23:6494–6506. doi: 10.1128/MCB.23.18.6494-6506.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Seto S., Tsujimura K., Koide Y. Rab GTPases regulating phagosome maturation are differentially recruited to mycobacterial phagosomes. Traffic. 2011;12:407–420. doi: 10.1111/j.1600-0854.2011.01165.x. [DOI] [PubMed] [Google Scholar]
- 63.Gutierrez M.G., Munafó D.B., Berón W., Colombo M.I. Rab7 is required for the normal progression of the autophagic pathway in mammalian cells. J. Cell Sci. 2004;117:2687. doi: 10.1242/jcs.01114. [DOI] [PubMed] [Google Scholar]
- 64.Dinter E., Saridaki T., Nippold M., Plum S., Diederichs L., Komnig D., Fensky L., May C., Marcus K., Voigt A., et al. Rab7 induces clearance of α-synuclein aggregates. J. Neurochem. 2016;138:758–774. doi: 10.1111/jnc.13712. [DOI] [PubMed] [Google Scholar]
- 65.Rodriguez L., Mohamed N.-V., Desjardins A., Lippé R., Fon E.A., Leclerc N. Rab7A regulates tau secretion. J. Neurochem. 2017;141:592–605. doi: 10.1111/jnc.13994. [DOI] [PubMed] [Google Scholar]
- 66.Hattula K., Furuhjelm J., Tikkanen J., Tanhuanpää K., Laakkonen P., Peränen J. Characterization of the Rab8-specific membrane traffic route linked to protrusion formation. J. Cell Sci. 2006;119:4866. doi: 10.1242/jcs.03275. [DOI] [PubMed] [Google Scholar]
- 67.Peränen J., Auvinen P., Virta H., Wepf R., Simons K. Rab8 promotes polarized membrane transport through reorganization of actin and microtubules in fibroblasts. J Cell Biol. 1996;135:153–167. doi: 10.1083/jcb.135.1.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pilli M., Arko-Mensah J., Ponpuak M., Roberts E., Master S., Mandell M.A., Dupont N., Ornatowski W., Jiang S., Bradfute S.B., et al. TBK-1 promotes autophagy-mediated antimicrobial defense by controlling autophagosome maturation. Immunity. 2012;37:223–234. doi: 10.1016/j.immuni.2012.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sellier C., Campanari M.L., Julie Corbier C., Gaucherot A., Kolb-Cheynel I., Oulad-Abdelghani M., Ruffenach F., Page A., Ciura S., Kabashi E., et al. Loss of C9ORF72 impairs autophagy and synergizes with polyQ Ataxin-2 to induce motor neuron dysfunction and cell death. EMBO J. 2016;35:1276–1297. doi: 10.15252/embj.201593350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yin G., da Fonseca T.L., Eisbach S.E., Anduaga A.M., Breda C., Orcellet M.L., Szegő É.M., Guerreiro P., Lázaro D.F., Braus G.H., et al. α-Synuclein interacts with the switch region of Rab8a in a Ser129 phosphorylation-dependent manner. Neurobiol. Dis. 2014;70:149–161. doi: 10.1016/j.nbd.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 71.Kumar R., Donakonda S., Müller S.A., Bötzel K., Höglinger G.U., Koeglsperger T. FGF2 Affects Parkinson’s Disease-Associated Molecular Networks Through Exosomal Rab8b/Rab31. Front. Genet. 2020;11:572058. doi: 10.3389/fgene.2020.572058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Delfino L., Mason R.P., Kyriacou C.P., Giorgini F., Rosato E. Rab8 Promotes Mutant HTT Aggregation, Reduces Neurodegeneration, and Ameliorates Behavioural Alterations in a Drosophila Model of Huntington’s Disease. J. Huntingt. Dis. 2020;9:253–263. doi: 10.3233/JHD-200411. [DOI] [PubMed] [Google Scholar]
- 73.Babbey C.M., Ahktar N., Wang E., Chen C.C.-H., Grant B.D., Dunn K.W. Rab10 regulates membrane transport through early endosomes of polarized Madin-Darby canine kidney cells. Mol. Biol. Cell. 2006;17:3156–3175. doi: 10.1091/mbc.e05-08-0799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cardoso C.M.P., Jordao L., Vieira O.V. Rab10 Regulates Phagosome Maturation and Its Overexpression Rescues Mycobacterium-Containing Phagosomes Maturation. Traffic. 2010;11:221–235. doi: 10.1111/j.1600-0854.2009.01013.x. [DOI] [PubMed] [Google Scholar]
- 75.English A.R., Voeltz G.K. Rab10 GTPase regulates ER dynamics and morphology. Nat. Cell Biol. 2013;15:169–178. doi: 10.1038/ncb2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ridge P.G., Karch C.M., Hsu S., Arano I., Teerlink C.C., Ebbert M.T.W., Gonzalez Murcia J.D., Farnham J.M., Damato A.R., Allen M., et al. Linkage, whole genome sequence, and biological data implicate variants in Rab10 in Alzheimer’s disease resilience. Genome Med. 2017;9:100. doi: 10.1186/s13073-017-0486-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sano H., Roach W.G., Peck G.R., Fukuda M., Lienhard G.E. Rab10 in insulin-stimulated GLUT4 translocation. Biochem. J. 2008;411:89–95. doi: 10.1042/BJ20071318. [DOI] [PubMed] [Google Scholar]
- 78.Yan T., Wang L., Gao J., Siedlak S.L., Huntley M.L., Termsarasab P., Perry G., Chen S.G., Wang X. Rab10 Phosphorylation is a Prominent Pathological Feature in Alzheimer’s Disease. J. Alzheimer’s Dis. 2018;63:157–165. doi: 10.3233/JAD-180023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Dumanchin C., Czech C., Campion D., Cuif M.H., Poyot T., Martin C., Charbonnier F., Goud B., Pradier L., Frebourg T. Presenilins Interact with Rab11, a Small GTPase Involved in the Regulation of Vesicular Transport. Hum. Mol. Genet. 1999;8:1263–1269. doi: 10.1093/hmg/8.7.1263. [DOI] [PubMed] [Google Scholar]
- 80.Li J., Kanekiyo T., Shinohara M., Zhang Y., LaDu M.J., Xu H., Bu G. Differential regulation of amyloid-β endocytic trafficking and lysosomal degradation by apolipoprotein E isoforms. J. Biol. Chem. 2012;287:44593–44601. doi: 10.1074/jbc.M112.420224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Li X., Standley C., Sapp E., Valencia A., Qin Z.-H., Kegel K.B., Yoder J., Comer-Tierney L.A., Esteves M., Chase K., et al. Mutant huntingtin impairs vesicle formation from recycling endosomes by interfering with Rab11 activity. Mol. Cell. Biol. 2009;29:6106–6116. doi: 10.1128/MCB.00420-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Steinert J.R., Campesan S., Richards P., Kyriacou C.P., Forsythe I.D., Giorgini F. Rab11 rescues synaptic dysfunction and behavioural deficits in a Drosophila model of Huntington’s disease. Hum. Mol. Genet. 2012;21:2912–2922. doi: 10.1093/hmg/dds117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Takahashi S., Kubo K., Waguri S., Yabashi A., Shin H.-W., Katoh Y., Nakayama K. Rab11 regulates exocytosis of recycling vesicles at the plasma membrane. J. Cell Sci. 2012;125:4049. doi: 10.1242/jcs.102913. [DOI] [PubMed] [Google Scholar]
- 84.Ullrich O., Reinsch S., Urbé S., Zerial M., Parton R.G. Rab11 regulates recycling through the pericentriolar recycling endosome. J. Cell Biol. 1996;135:913–924. doi: 10.1083/jcb.135.4.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chen S., Yoo H., Li C.H., Park C., Park G., Tan L.Y., Jung S., Park H. Real-time three-dimensional tracking of single vesicles reveals abnormal motion and pools of synaptic vesicles in neurons of Huntington’s disease mice. iScience. 2021;24:103181. doi: 10.1016/j.isci.2021.103181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Elias S., McGuire J.R., Yu H., Humbert S. Huntingtin Is Required for Epithelial Polarity through Rab11A-Mediated Apical Trafficking of PAR3-aPKC. PLoS Biol. 2015;13:e1002142. doi: 10.1371/journal.pbio.1002142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.McClory H., Williams D., Sapp E., Gatune L.W., Wang P., DiFiglia M., Li X. Glucose transporter 3 is a rab11-dependent trafficking cargo and its transport to the cell surface is reduced in neurons of CAG140 Huntington’s disease mice. Acta Neuropathol. Commun. 2014;2:179. doi: 10.1186/s40478-014-0178-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Li X., Valencia A., McClory H., Sapp E., Kegel K.B., Difiglia M. Deficient Rab11 activity underlies glucose hypometabolism in primary neurons of Huntington’s disease mice. Biochem. Biophys. Res. Commun. 2012;421:727–730. doi: 10.1016/j.bbrc.2012.04.070. [DOI] [PubMed] [Google Scholar]
- 89.Li X., Valencia A., Sapp E., Masso N., Alexander J., Reeves P., Kegel K.B., Aronin N., Difiglia M. Aberrant Rab11-dependent trafficking of the neuronal glutamate transporter EAAC1 causes oxidative stress and cell death in Huntington’s disease. J. Neurosci. 2010;30:4552–4561. doi: 10.1523/JNEUROSCI.5865-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Li X., Sapp E., Chase K., Comer-Tierney L.A., Masso N., Alexander J., Reeves P., Kegel K.B., Valencia A., Esteves M., et al. Disruption of Rab11 activity in a knock-in mouse model of Huntington’s disease. Neurobiol. Dis. 2009;36:374–383. doi: 10.1016/j.nbd.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gonçalves S.A., Macedo D., Raquel H., Simões P.D., Giorgini F., Ramalho J.S., Barral D.C., Ferreira Moita L., Outeiro T.F. shRNA-Based Screen Identifies Endocytic Recycling Pathway Components That Act as Genetic Modifiers of Alpha-Synuclein Aggregation, Secretion and Toxicity. PLoS Genet. 2016;12:e1005995. doi: 10.1371/journal.pgen.1005995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Marzesco A.-M., Dunia I., Pandjaitan R., Recouvreur M., Dauzonne D., Benedetti E.L., Louvard D., Zahraoui A. The small GTPase Rab13 regulates assembly of functional tight junctions in epithelial cells. Mol. Biol. Cell. 2002;13:1819–1831. doi: 10.1091/mbc.02-02-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Nokes R.L., Fields I.C., Collins R.N., Fölsch H. Rab13 regulates membrane trafficking between TGN and recycling endosomes in polarized epithelial cells. J. Cell Biol. 2008;182:845–853. doi: 10.1083/jcb.200802176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sinka R., Gillingham A.K., Kondylis V., Munro S. Golgi coiled-coil proteins contain multiple binding sites for Rab family G proteins. J. Cell Biol. 2008;183:607–615. doi: 10.1083/jcb.200808018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fukuda M. Membrane traffic in the secretory pathway. Cell. Mol. Life Sci. 2008;65:2801–2813. doi: 10.1007/s00018-008-8351-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tolmachova T., Anders R., Stinchcombe J., Bossi G., Griffiths G.M., Huxley C., Seabra M.C. A general role for Rab27a in secretory cells. Mol. Biol. Cell. 2004;15:332–344. doi: 10.1091/mbc.e03-07-0452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Underwood R., Wang B., Carico C., Whitaker R.H., Placzek W.J., Yacoubian T.A. The GTPase Rab27b regulates the release, autophagic clearance, and toxicity of α-synuclein. J. Biol. Chem. 2020;295:8005–8016. doi: 10.1074/jbc.RA120.013337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Purlyte E., Dhekne H.S., Sarhan A.R., Gomez R., Lis P., Wightman M., Martinez T.N., Tonelli F., Pfeffer S.R., Alessi D.R. Rab29 activation of the Parkinson’s disease-associated LRRK2 kinase. EMBO J. 2018;37:1–18. doi: 10.15252/embj.201798099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Spanò S., Liu X., Galán J.E. Proteolytic targeting of Rab29 by an effector protein distinguishes the intracellular compartments of human-adapted and broad-host Salmonella. Proc. Natl. Acad. Sci. USA. 2011;108:18418–18423. doi: 10.1073/pnas.1111959108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wang S., Ma Z., Xu X., Wang Z., Sun L., Zhou Y., Lin X., Hong W., Wang T. A Role of Rab29 in the Integrity of the Trans-Golgi Network and Retrograde Trafficking of Mannose-6-Phosphate Receptor. PLoS ONE. 2014;9:e96242. doi: 10.1371/journal.pone.0096242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Rodriguez-Gabin A.G., Cammer M., Almazan G., Charron M., Larocca J.N. Role of rRab22b, an oligodendrocyte protein, in regulation of transport of vesicles from trans Golgi to endocytic compartments. J. Neurosci. Res. 2001;66:1149–1160. doi: 10.1002/jnr.1253. [DOI] [PubMed] [Google Scholar]
- 102.Rodriguez-Gabin A.G., Yin X., Si Q., Larocca J.N. Transport of mannose-6-phosphate receptors from the trans-Golgi network to endosomes requires Rab31. Exp Cell Res. 2009;315:2215–2230. doi: 10.1016/j.yexcr.2009.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ng E.L., Wang Y., Tang B.L. Rab22B’s role in trans-Golgi network membrane dynamics. Biochem. Biophys. Res. Commun. 2007;361:751–757. doi: 10.1016/j.bbrc.2007.07.076. [DOI] [PubMed] [Google Scholar]
- 104.Ng E.L., Ng J.J., Liang F., Tang B.L. Rab22B is expressed in the CNS astroglia lineage and plays a role in epidermal growth factor receptor trafficking in A431 cells. J. Cell Physiol. 2009;221:716–728. doi: 10.1002/jcp.21911. [DOI] [PubMed] [Google Scholar]
- 105.Alto N.M., Soderling J., Scott J.D. Rab32 is an A-kinase anchoring protein and participates in mitochondrial dynamics. J. Cell Biol. 2002;158:659–668. doi: 10.1083/jcb.200204081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bui M., Gilady S.Y., Fitzsimmons R.E.B., Benson M.D., Lynes E.M., Gesson K., Alto N.M., Strack S., Scott J.D., Simmen T. Rab32 modulates apoptosis onset and mitochondria-associated membrane (MAM) properties. J. Biol. Chem. 2010;285:31590–31602. doi: 10.1074/jbc.M110.101584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hirota Y., Tanaka Y. A small GTPase, human Rab32, is required for the formation of autophagic vacuoles under basal conditions. Cell. Mol. Life Sci. 2009;66:2913–2932. doi: 10.1007/s00018-009-0080-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Waschbüsch D., Michels H., Strassheim S., Ossendorf E., Kessler D., Gloeckner C.J., Barnekow A. LRRK2 transport is regulated by its novel interacting partner Rab32. PLoS ONE. 2014;9:e111632. doi: 10.1371/journal.pone.0111632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chua C.E.L., Lim Y.S., Tang B.L. Rab35—A vesicular traffic-regulating small GTPase with actin modulating roles. FEBS Lett. 2010;584:1–6. doi: 10.1016/j.febslet.2009.11.051. [DOI] [PubMed] [Google Scholar]
- 110.Kouranti I., Sachse M., Arouche N., Goud B., Echard A. Rab35 Regulates an Endocytic Recycling Pathway Essential for the Terminal Steps of Cytokinesis. Curr. Biol. 2006;16:1719–1725. doi: 10.1016/j.cub.2006.07.020. [DOI] [PubMed] [Google Scholar]
- 111.Vaz-Silva J., Gomes P., Jin Q., Zhu M., Zhuravleva V., Quintremil S., Meira T., Silva J., Dioli C., Soares-Cunha C., et al. Endolysosomal degradation of Tau and its role in glucocorticoid-driven hippocampal malfunction. EMBO J. 2018;37:e99084. doi: 10.15252/embj.201899084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Giannandrea M., Bianchi V., Mignogna M.L., Sirri A., Carrabino S., D’Elia E., Vecellio M., Russo S., Cogliati F., Larizza L., et al. Mutations in the small GTPase gene Rab39B are responsible for X-linked mental retardation associated with autism, epilepsy, and macrocephaly. Am. J. Hum. Genet. 2010;86:185–195. doi: 10.1016/j.ajhg.2010.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lesage S., Bras J., Cormier-Dequaire F., Condroyer C., Nicolas A., Darwent L., Guerreiro R., Majounie E., Federoff M., Heutink P., et al. Loss-of-function mutations in Rab39B are associated with typical early-onset Parkinson disease. Neurol. Genet. 2015;1:e9. doi: 10.1212/NXG.0000000000000009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mignogna M.L., Giannandrea M., Gurgone A., Fanelli F., Raimondi F., Mapelli L., Bassani S., Fang H., Van Anken E., Alessio M., et al. The intellectual disability protein Rab39B selectively regulates GluA2 trafficking to determine synaptic AMPAR composition. Nat. Commun. 2015;6:6504. doi: 10.1038/ncomms7504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wilson G.R., Sim J.C.H., McLean C., Giannandrea M., Galea C.A., Riseley J.R., Stephenson S.E.M., Fitzpatrick E., Haas S.A., Pope K., et al. Mutations in Rab39B cause X-linked intellectual disability and early-onset Parkinson disease with α-synuclein pathology. Am. J. Hum. Genet. 2014;95:729–735. doi: 10.1016/j.ajhg.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.World Health Organisation Dementia. [(accessed on 29 April 2022)]. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia.
- 117.Zhang X., Huang T.Y., Yancey J., Luo H., Zhang Y.W. Role of Rab GTPases in Alzheimer’s Disease. ACS Chem. Neurosci. 2019;10:828–838. doi: 10.1021/acschemneuro.8b00387. [DOI] [PubMed] [Google Scholar]
- 118.Mattson M.P. Cellular actions of beta-amyloid precursor protein and its soluble and fibrillogenic derivatives. Physiol. Rev. 1997;77:1081–1132. doi: 10.1152/physrev.1997.77.4.1081. [DOI] [PubMed] [Google Scholar]
- 119.Vassar R., Bennett B.D., Babu-Khan S., Kahn S., Mendiaz E.A., Denis P., Teplow D.B., Ross S., Amarante P., Loeloff R., et al. Beta-secretase cleavage of Alzheimer’s amyloid precursor protein by the transmembrane aspartic protease BACE. Science. 1999;286:735–741. doi: 10.1126/science.286.5440.735. [DOI] [PubMed] [Google Scholar]
- 120.Koo E.H., Squazzo S.L. Evidence that production and release of amyloid beta-protein involves the endocytic pathway. J. Biol. Chem. 1994;269:17386–17389. doi: 10.1016/S0021-9258(17)32449-3. [DOI] [PubMed] [Google Scholar]
- 121.Sun M., Zhang H. Par3 and aPKC regulate BACE1 endosome-to-TGN trafficking through PACS1. Neurobiol. Aging. 2017;60:129–140. doi: 10.1016/j.neurobiolaging.2017.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.MacLeod R., Hillert E.-K., Cameron R.T., Baillie G.S. The role and therapeutic targeting of α-, β- and γ-secretase in Alzheimer’s disease. Future Sci. OA. 2015;1:FSO11. doi: 10.4155/fso.15.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Fourriere L., Gleeson P.A. Amyloid β production along the neuronal secretory pathway: Dangerous liaisons in the Golgi? Traffic. 2021;22:319–327. doi: 10.1111/tra.12808. [DOI] [PubMed] [Google Scholar]
- 124.Tam J.H., Seah C., Pasternak S.H. The Amyloid Precursor Protein is rapidly transported from the Golgi apparatus to the lysosome and where it is processed into beta-amyloid. Mol. Brain. 2014;7:54. doi: 10.1186/s13041-014-0054-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Xu W., Weissmiller A.M., White J.A., 2nd, Fang F., Wang X., Wu Y., Pearn M.L., Zhao X., Sawa M., Chen S., et al. Amyloid precursor protein-mediated endocytic pathway disruption induces axonal dysfunction and neurodegeneration. J. Clin. Investig. 2016;126:1815–1833. doi: 10.1172/JCI82409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kim S., Sato Y., Mohan P.S., Peterhoff C., Pensalfini A., Rigoglioso A., Jiang Y., Nixon R.A. Evidence that the rab5 effector APPL1 mediates APP-βCTF-induced dysfunction of endosomes in Down syndrome and Alzheimer’s disease. Mol. Psychiatry. 2016;21:707–716. doi: 10.1038/mp.2015.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Chen Y., Liu W., McPhie D.L., Hassinger L., Neve R.L. APP-BP1 mediates APP-induced apoptosis and DNA synthesis and is increased in Alzheimer’s disease brain. J. Cell Biol. 2003;163:27–33. doi: 10.1083/jcb.200304003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Laifenfeld D., Patzek L.J., McPhie D.L., Chen Y., Levites Y., Cataldo A.M., Neve R.L. Rab5 mediates an amyloid precursor protein signaling pathway that leads to apoptosis. J. Neurosci. 2007;27:7141–7153. doi: 10.1523/JNEUROSCI.4599-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kunkle B.W., Vardarajan B.N., Naj A.C., Whitehead P.L., Rolati S., Slifer S., Carney R.M., Cuccaro M.L., Vance J.M., Gilbert J.R., et al. Early-Onset Alzheimer Disease and Candidate Risk Genes Involved in Endolysosomal Transport. JAMA Neurol. 2017;74:1113–1122. doi: 10.1001/jamaneurol.2017.1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lambert J.C., Ibrahim-Verbaas C.A., Harold D., Naj A.C., Sims R., Bellenguez C., DeStafano A.L., Bis J.C., Beecham G.W., Grenier-Boley B., et al. Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer’s disease. Nat. Genet. 2013;45:1452–1458. doi: 10.1038/ng.2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Shen R., Zhao X., He L., Ding Y., Xu W., Lin S., Fang S., Yang W., Sung K., Spencer B., et al. Upregulation of RIN3 induces endosomal dysfunction in Alzheimer’s disease. Transl. Neurodegener. 2020;9:26. doi: 10.1186/s40035-020-00206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Chapuis J., Hansmannel F., Gistelinck M., Mounier A., Van Cauwenberghe C., Kolen K.V., Geller F., Sottejeau Y., Harold D., Dourlen P., et al. Increased expression of BIN1 mediates Alzheimer genetic risk by modulating tau pathology. Mol. Psychiatry. 2013;18:1225–1234. doi: 10.1038/mp.2013.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Harrison B.J., Venkat G., Lamb J.L., Hutson T.H., Drury C., Rau K.K., Bunge M.B., Mendell L.M., Gage F.H., Johnson R.D., et al. The Adaptor Protein CD2AP Is a Coordinator of Neurotrophin Signaling-Mediated Axon Arbor Plasticity. J. Neurosci. 2016;36:4259–4275. doi: 10.1523/JNEUROSCI.2423-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Vandal M., Gunn C., Bourassa P., Institoris A., Shin S.S., Jiang Y., Tremblay C., Belzil C., Bennett D.A., Gordon G., et al. Defining the role of the Alzheimer disease risk factor CD2AP in brain vascular function. Alzheimer’s Dement. 2020;16:e040566. doi: 10.1002/alz.040566. [DOI] [Google Scholar]
- 135.Buggia-Prévot V., Fernandez C.G., Riordan S., Vetrivel K.S., Roseman J., Waters J., Bindokas V.P., Vassar R., Thinakaran G. Axonal BACE1 dynamics and targeting in hippocampal neurons: A role for Rab11 GTPase. Mol. Neurodegener. 2014;9:1. doi: 10.1186/1750-1326-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Woodruff G., Reyna S.M., Dunlap M., Van Der Kant R., Callender J.A., Young J.E., Roberts E.A., Goldstein L.S.B. Defective Transcytosis of APP and Lipoproteins in Human iPSC-Derived Neurons with Familial Alzheimer’s Disease Mutations. Cell Rep. 2016;17:759–773. doi: 10.1016/j.celrep.2016.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Begcevic I., Kosanam H., Martínez-Morillo E., Dimitromanolakis A., Diamandis P., Kuzmanov U., Hazrati L.N., Diamandis E.P. Semiquantitative proteomic analysis of human hippocampal tissues from Alzheimer’s disease and age-matched control brains. Clin. Proteom. 2013;10:5. doi: 10.1186/1559-0275-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Koss D.J., Bondarevaite O., Adams S., Leite M., Giorgini F., Attems J., Outeiro T.F. Rab39B is redistributed in dementia with Lewy bodies and is sequestered within aβ plaques and Lewy bodies. Brain Pathol. 2021;31:120–132. doi: 10.1111/bpa.12890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Scheper W., Zwart R., van der Sluijs P., Annaert W., Gool W.A., Baas F. Alzheimer’s presenilin 1 is a putative membrane receptor for rab GDP dissociation inhibitor. Hum. Mol. Genet. 2000;9:303–310. doi: 10.1093/hmg/9.2.303. [DOI] [PubMed] [Google Scholar]
- 140.Musunuri S., Wetterhall M., Ingelsson M., Lannfelt L., Artemenko K., Bergquist J., Kultima K., Shevchenko G. Quantification of the brain proteome in Alzheimer’s disease using multiplexed mass spectrometry. J. Proteome Res. 2014;13:2056–2068. doi: 10.1021/pr401202d. [DOI] [PubMed] [Google Scholar]
- 141.Erdman R.A., Maltese W.A. Different Rab GTPases associate preferentially with alpha or beta GDP-dissociation inhibitors. Biochem. Biophys. Res. Commun. 2001;282:4–9. doi: 10.1006/bbrc.2001.4560. [DOI] [PubMed] [Google Scholar]
- 142.Goedert M., Spillantini M.G., Jakes R., Rutherford D., Crowther R.A. Multiple isoforms of human microtubule-associated protein tau: Sequences and localization in neurofibrillary tangles of Alzheimer’s disease. Neuron. 1989;3:519–526. doi: 10.1016/0896-6273(89)90210-9. [DOI] [PubMed] [Google Scholar]
- 143.Arendt T., Stieler J.T., Holzer M. Tau and tauopathies. Brain Res. Bull. 2016;126:238–292. doi: 10.1016/j.brainresbull.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 144.Weingarten M.D., Lockwood A.H., Hwo S.Y., Kirschner M.W. A protein factor essential for microtubule assembly. Proc. Natl. Acad. Sci. USA. 1975;72:1858–1862. doi: 10.1073/pnas.72.5.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Giannakopoulos P., Herrmann F.R., Bussière T., Bouras C., Kövari E., Perl D.P., Morrison J.H., Gold G., Hof P.R. Tangle and neuron numbers, but not amyloid load, predict cognitive status in Alzheimer’s disease. Neurology. 2003;60:1495–1500. doi: 10.1212/01.WNL.0000063311.58879.01. [DOI] [PubMed] [Google Scholar]
- 146.Koss D.J., Dubini M., Buchanan H., Hull C., Platt B. Distinctive temporal profiles of detergent-soluble and -insoluble tau and Aβ species in human Alzheimer’s disease. Brain Res. 2018;1699:121–134. doi: 10.1016/j.brainres.2018.08.014. [DOI] [PubMed] [Google Scholar]
- 147.Koss D.J., Jones G., Cranston A., Gardner H., Kanaan N.M., Platt B. Soluble pre-fibrillar tau and β-amyloid species emerge in early human Alzheimer’s disease and track disease progression and cognitive decline. Acta Neuropathol. 2016;132:875–895. doi: 10.1007/s00401-016-1632-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Henderson M.X., Sengupta M., Trojanowski J.Q., Lee V.M.Y. Alzheimer’s disease tau is a prominent pathology in LRRK2 Parkinson’s disease. Acta Neuropathol. Commun. 2019;7:183. doi: 10.1186/s40478-019-0836-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Zhao Y., Ho P., Yih Y., Chen C., Lee W.L., Tan E.K. LRRK2 variant associated with Alzheimer’s disease. Neurobiol. Aging. 2011;32:1990–1993. doi: 10.1016/j.neurobiolaging.2009.11.019. [DOI] [PubMed] [Google Scholar]
- 150.Rui Q., Ni H., Li D., Gao R., Chen G. The Role of LRRK2 in Neurodegeneration of Parkinson Disease. Curr. Neuropharmacol. 2018;16:1348–1357. doi: 10.2174/1570159X16666180222165418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Blom E.S., Giedraitis V., Zetterberg H., Fukumoto H., Blennow K., Hyman B.T., Irizarry M.C., Wahlund L.O., Lannfelt L., Ingelsson M. Rapid Progression from Mild Cognitive Impairment to Alzheimer’s Disease in Subjects with Elevated Levels of Tau in Cerebrospinal Fluid and the APOEε4/ε4 Genotype. Dement. Geriatr. Cogn. Disord. 2009;27:458–464. doi: 10.1159/000216841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Mudher A., Colin M., Dujardin S., Medina M., Dewachter I., Alavi Naini S.M., Mandelkow E.-M., Mandelkow E., Buée L., Goedert M., et al. What is the evidence that tau pathology spreads through prion-like propagation? Acta Neuropathol. Commun. 2017;5:99. doi: 10.1186/s40478-017-0488-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Antón-Fernández A., Aparicio-Torres G., Tapia S., DeFelipe J., Muñoz A. Morphometric alterations of Golgi apparatus in Alzheimer’s disease are related to tau hyperphosphorylation. Neurobiol Dis. 2017;97:11–23. doi: 10.1016/j.nbd.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Segev N., Mulholland J., Botstein D. The yeast GTP-binding YPT1 protein and a mammalian counterpart are associated with the secretion machinery. Cell. 1988;52:915–924. doi: 10.1016/0092-8674(88)90433-3. [DOI] [PubMed] [Google Scholar]
- 155.Mohamed N.-V., Desjardins A., Leclerc N. Tau secretion is correlated to an increase of Golgi dynamics. PLoS ONE. 2017;12:e0178288. doi: 10.1371/journal.pone.0178288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Pinheiro S., Silva J., Mota C., Vaz-Silva J., Veloso A., Pinto V., Sousa N., Cerqueira J., Sotiropoulos I. Tau Mislocation in Glucocorticoid-Triggered Hippocampal Pathology. Mol. Neurobiol. 2016;53:4745–4753. doi: 10.1007/s12035-015-9356-2. [DOI] [PubMed] [Google Scholar]
- 157.Lopes S., Teplytska L., Vaz-Silva J., Dioli C., Trindade R., Morais M., Webhofer C., Maccarrone G., Almeida O.F.X., Turck C.W., et al. Tau Deletion Prevents Stress-Induced Dendritic Atrophy in Prefrontal Cortex: Role of Synaptic Mitochondria. Cereb. Cortex. 2017;27:2580–2591. doi: 10.1093/cercor/bhw057. [DOI] [PubMed] [Google Scholar]
- 158.Dioli C., Patrício P., Trindade R., Pinto L.G., Silva J.M., Morais M., Ferreiro E., Borges S., Mateus-Pinheiro A., Rodrigues A.J., et al. Tau-dependent suppression of adult neurogenesis in the stressed hippocampus. Mol. Psychiatry. 2017;22:1110–1118. doi: 10.1038/mp.2017.103. [DOI] [PubMed] [Google Scholar]
- 159.Tan M.-S., Yang Y.-X., Xu W., Wang H.-F., Tan L., Zuo C.-T., Dong Q., Tan L., Suckling J., Yu J.-T., et al. Associations of Alzheimer’s disease risk variants with gene expression, amyloidosis, tauopathy, and neurodegeneration. Alzheimer’s Res. Ther. 2021;13:15. doi: 10.1186/s13195-020-00755-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Majounie E., Renton A.E., Mok K., Dopper E.G., Waite A., Rollinson S., Chiò A., Restagno G., Nicolaou N., Simon-Sanchez J., et al. Frequency of the C9orf72 hexanucleotide repeat expansion in patients with amyotrophic lateral sclerosis and frontotemporal dementia: A cross-sectional study. Lancet Neurol. 2012;11:323–330. doi: 10.1016/S1474-4422(12)70043-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kohli M.A., John-Williams K., Rajbhandary R., Naj A., Whitehead P., Hamilton K., Carney R.M., Wright C., Crocco E., Gwirtzman H.E., et al. Repeat expansions in the C9ORF72 gene contribute to Alzheimer’s disease in Caucasians. Neurobiol. Aging. 2013;34:1519.e5–1519.e12. doi: 10.1016/j.neurobiolaging.2012.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Beck J., Poulter M., Hensman D., Rohrer J.D., Mahoney C.J., Adamson G., Campbell T., Uphill J., Borg A., Fratta P., et al. Large C9orf72 hexanucleotide repeat expansions are seen in multiple neurodegenerative syndromes and are more frequent than expected in the UK population. Am. J. Hum. Genet. 2013;92:345–353. doi: 10.1016/j.ajhg.2013.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Renton A.E., Majounie E., Waite A., Simón-Sánchez J., Rollinson S., Gibbs J.R., Schymick J.C., Laaksovirta H., van Swieten J.C., Myllykangas L., et al. A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome 9p21-linked ALS-FTD. Neuron. 2011;72:257–268. doi: 10.1016/j.neuron.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Majounie E., Abramzon Y., Renton A.E., Perry R., Bassett S.S., Pletnikova O., Troncoso J.C., Hardy J., Singleton A.B., Traynor B.J. Repeat expansion in C9ORF72 in Alzheimer’s disease. N. Engl. J. Med. 2012;366:283–284. doi: 10.1056/NEJMc1113592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Shu L., Sun Q., Zhang Y., Xu Q., Guo J., Yan X., Tang B. The Association between C9orf72 Repeats and Risk of Alzheimer’s Disease and Amyotrophic Lateral Sclerosis: A Meta-Analysis. Parkinson’s Dis. 2016;2016:5731734. doi: 10.1155/2016/5731734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Bieniek K.F., Murray M.E., Rutherford N.J., Castanedes-Casey M., DeJesus-Hernandez M., Liesinger A.M., Baker M.C., Boylan K.B., Rademakers R., Dickson D.W. Tau pathology in frontotemporal lobar degeneration with C9ORF72 hexanucleotide repeat expansion. Acta Neuropathol. 2013;125:289–302. doi: 10.1007/s00401-012-1048-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Satoh J., Tabunoki H., Ishida T., Saito Y., Arima K. Dystrophic neurites express C9orf72 in Alzheimer’s disease brains. Alzheimer’s Res. 2012;4:33. doi: 10.1186/alzrt136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Tang B.L. C9orf72′s Interaction with Rab GTPases-Modulation of Membrane Traffic and Autophagy. Front. Cell. Neurosci. 2016;10:228. doi: 10.3389/fncel.2016.00228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Webster C.P., Smith E.F., Bauer C.S., Moller A., Hautbergue G.M., Ferraiuolo L., Myszczynska M.A., Higginbottom A., Walsh M.J., Whitworth A.J., et al. The C9orf72 protein interacts with Rab1a and the ULK1 complex to regulate initiation of autophagy. EMBO J. 2016;35:1656–1676. doi: 10.15252/embj.201694401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Tang D., Sheng J., Xu L., Zhan X., Liu J., Jiang H., Shu X., Liu X., Zhang T., Jiang L., et al. Cryo-EM structure of C9ORF72-SMCR8-WDR41 reveals the role as a GAP for Rab8a and Rab11a. Proc. Natl. Acad. Sci. USA. 2020;117:9876–9883. doi: 10.1073/pnas.2002110117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Yang M., Liang C., Swaminathan K., Herrlinger S., Lai F., Shiekhattar R., Chen J.F. A C9ORF72/SMCR8-containing complex regulates ULK1 and plays a dual role in autophagy. Sci. Adv. 2016;2:e1601167. doi: 10.1126/sciadv.1601167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Xiao S., McKeever P.M., Lau A., Robertson J. Synaptic localization of C9orf72 regulates post-synaptic glutamate receptor 1 levels. Acta Neuropathol. Commun. 2019;7:161. doi: 10.1186/s40478-019-0812-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Agola J.O., Hong L., Surviladze Z., Ursu O., Waller A., Strouse J.J., Simpson D.S., Schroeder C.E., Oprea T.I., Golden J.E., et al. A competitive nucleotide binding inhibitor: In vitro characterization of Rab7 GTPase inhibition. ACS Chem. Biol. 2012;7:1095–1108. doi: 10.1021/cb3001099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Qin Y., He Y., Zhu Y.M., Li M., Ni Y., Liu J., Zhang H.L. CID1067700, a late endosome GTPase Rab7 receptor antagonist, attenuates brain atrophy, improves neurologic deficits and inhibits reactive astrogliosis in rat ischemic stroke. Acta Pharm. Sin. 2019;40:724–736. doi: 10.1038/s41401-018-0166-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Lam T., Kulp D.V., Wang R., Lou Z., Taylor J., Rivera C.E., Yan H., Zhang Q., Wang Z., Zan H., et al. Small Molecule Inhibition of Rab7 Impairs B Cell Class Switching and Plasma Cell Survival To Dampen the Autoantibody Response in Murine Lupus. J. Immunol. 2016;197:3792–3805. doi: 10.4049/jimmunol.1601427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Grant B.J., Lukman S., Hocker H.J., Sayyah J., Brown J.H., McCammon J.A., Gorfe A.A. Novel allosteric sites on Ras for lead generation. PLoS ONE. 2011;6:e25711. doi: 10.1371/journal.pone.0025711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Kumar A.P., Lukman S. Allosteric binding sites in Rab11 for potential drug candidates. PLoS ONE. 2018;13:e0198632. doi: 10.1371/journal.pone.0198632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Surviladze Z., Ursu O., Miscioscia F., Curpan R., Halip L., Bologa C., Oprea T., Waller A., Strouse J., Salas V., et al. Probe Reports from the NIH Molecular Libraries Program. National Center for Biotechnology Information (US); Bethesda, MD, USA: 2010. Three small molecule pan activator families of Ras-related GTPases. [PubMed] [Google Scholar]
- 179.Palsuledesai C.C., Surviladze Z., Waller A., Miscioscia T.F., Guo Y., Wu Y., Strouse J., Romero E., Salas V.M., Curpan R., et al. Activation of Rho Family GTPases by Small Molecules. ACS Chem. Biol. 2018;13:1514–1524. doi: 10.1021/acschembio.8b00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Kumar A.P., Verma C.S., Lukman S. Structural dynamics and allostery of Rab proteins: Strategies for drug discovery and design. Brief. Bioinform. 2021;22:270–287. doi: 10.1093/bib/bbz161. [DOI] [PubMed] [Google Scholar]
- 181.Hooff G.P., Wood W.G., Müller W.E., Eckert G.P. Isoprenoids, small GTPases and Alzheimer’s disease. Biochim. Biophys. Acta. 2010;1801:896–905. doi: 10.1016/j.bbalip.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Basso A.D., Kirschmeier P., Bishop W.R. Lipid posttranslational modifications. Farnesyl transferase inhibitors. J. Lipid Res. 2006;47:15–31. doi: 10.1194/jlr.R500012-JLR200. [DOI] [PubMed] [Google Scholar]
- 183.Sebti S.M., Hamilton A.D. Farnesyltransferase and geranylgeranyltransferase I inhibitors and cancer therapy: Lessons from mechanism and bench-to-bedside translational studies. Oncogene. 2000;19:6584–6593. doi: 10.1038/sj.onc.1204146. [DOI] [PubMed] [Google Scholar]
- 184.Sebti S.M., Hamilton A.D. Inhibition of Rho GTPases using protein geranylgeranyltransferase I inhibitors. Methods Enzym. 2000;325:381–388. doi: 10.1016/s0076-6879(00)25459-1. [DOI] [PubMed] [Google Scholar]
- 185.Baron R.A., Tavaré R., Figueiredo A.C., Błazewska K.M., Kashemirov B.A., McKenna C.E., Ebetino F.H., Taylor A., Rogers M.J., Coxon F.P., et al. Phosphonocarboxylates inhibit the second geranylgeranyl addition by Rab geranylgeranyl transferase. J. Biol. Chem. 2009;284:6861–6868. doi: 10.1074/jbc.M806952200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Coxon F.P., Ebetino F.H., Mules E.H., Seabra M.C., McKenna C.E., Rogers M.J. Phosphonocarboxylate inhibitors of Rab geranylgeranyl transferase disrupt the prenylation and membrane localization of Rab proteins in osteoclasts in vitro and in vivo. Bone. 2005;37:349–358. doi: 10.1016/j.bone.2005.04.021. [DOI] [PubMed] [Google Scholar]
- 187.Coxon F.P., Helfrich M.H., Larijani B., Muzylak M., Dunford J.E., Marshall D., McKinnon A.D., Nesbitt S.A., Horton M.A., Seabra M.C., et al. Identification of a Novel Phosphonocarboxylate Inhibitor of Rab Geranylgeranyl Transferase That Specifically Prevents Rab Prenylation in Osteoclasts and Macrophages. J. Biol. Chem. 2001;276:48213–48222. doi: 10.1074/jbc.M106473200. [DOI] [PubMed] [Google Scholar]
- 188.McKenna C.E., Kashemirov B.A., Błazewska K.M., Mallard-Favier I., Stewart C.A., Rojas J., Lundy M.W., Ebetino F.H., Baron R.A., Dunford J.E., et al. Synthesis, chiral high performance liquid chromatographic resolution and enantiospecific activity of a potent new geranylgeranyl transferase inhibitor, 2-hydroxy-3-imidazo [1,2-a]pyridin-3-yl-2-phosphonopropionic acid. J. Med. Chem. 2010;53:3454–3464. doi: 10.1021/jm900232u. [DOI] [PubMed] [Google Scholar]
- 189.Ostrowski S.M., Johnson K., Siefert M., Shank S., Sironi L., Wolozin B., Landreth G.E., Ziady A.G. Simvastatin inhibits protein isoprenylation in the brain. Neuroscience. 2016;329:264–274. doi: 10.1016/j.neuroscience.2016.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Jick H., Zornberg G.L., Jick S.S., Seshadri S., Drachman D.A. Statins and the risk of dementia. Lancet. 2000;356:1627–1631. doi: 10.1016/S0140-6736(00)03155-X. [DOI] [PubMed] [Google Scholar]
- 191.Wolozin B., Kellman W., Ruosseau P., Celesia G.G., Siegel G. Decreased prevalence of Alzheimer disease associated with 3-hydroxy-3-methyglutaryl coenzyme A reductase inhibitors. Arch. Neurol. 2000;57:1439–1443. doi: 10.1001/archneur.57.10.1439. [DOI] [PubMed] [Google Scholar]
- 192.Zamrini E., McGwin G., Roseman J.M. Association between statin use and Alzheimer’s disease. Neuroepidemiology. 2004;23:94–98. doi: 10.1159/000073981. [DOI] [PubMed] [Google Scholar]
- 193.Wolozin B., Manger J., Bryant R., Cordy J., Green R.C., McKee A. Re-assessing the relationship between cholesterol, statins and Alzheimer’s disease. Acta Neurol. Scand. Suppl. 2006;185:63–70. doi: 10.1111/j.1600-0404.2006.00687.x. [DOI] [PubMed] [Google Scholar]
- 194.Reilly J.E., Neighbors J.D., Hohl R.J. Targeting protein geranylgeranylation slows tumor development in a murine model of prostate cancer metastasis. Cancer Biol. Ther. 2017;18:872–882. doi: 10.1080/15384047.2016.1219817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Haney S.L., Wills V.S., Wiemer D.F., Holstein S.A. Recent Advances in the Development of Mammalian Geranylgeranyl Diphosphate Synthase Inhibitors. Molecules. 2017;22:886. doi: 10.3390/molecules22060886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Liao J.K., Laufs U. Pleiotropic effects of statins. Annu. Rev. Pharm. Toxicol. 2005;45:89–118. doi: 10.1146/annurev.pharmtox.45.120403.095748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Yoshimura S., Gerondopoulos A., Linford A., Rigden D.J., Barr F.A. Family-wide characterization of the DENN domain Rab GDP-GTP exchange factors. J. Cell Biol. 2010;191:367–381. doi: 10.1083/jcb.201008051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Homma Y., Hiragi S., Fukuda M. Rab family of small GTPases: An updated view on their regulation and functions. FEBS J. 2021;288:36–55. doi: 10.1111/febs.15453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Fukuda M., Kobayashi H., Ishibashi K., Ohbayashi N. Genome-wide investigation of the Rab binding activity of RUN domains: Development of a novel tool that specifically traps GTP-Rab35. Cell Struct. Funct. 2011;36:155–170. doi: 10.1247/csf.11001. [DOI] [PubMed] [Google Scholar]
- 200.Gray J.L., von Delft F., Brennan P.E. Targeting the Small GTPase Superfamily through Their Regulatory Proteins. Angew. Chem. Int. Ed. Engl. 2020;59:6342–6366. doi: 10.1002/anie.201900585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Steger M., Diez F., Dhekne H.S., Lis P., Nirujogi R.S., Karayel O., Tonelli F., Martinez T.N., Lorentzen E., Pfeffer S.R., et al. Systematic proteomic analysis of LRRK2-mediated Rab GTPase phosphorylation establishes a connection to ciliogenesis. Elife. 2017;6:e31012. doi: 10.7554/eLife.31012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Houlden H., Singleton A.B. The genetics and neuropathology of Parkinson’s disease. Acta Neuropathol. 2012;124:325–338. doi: 10.1007/s00401-012-1013-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Di Maio R., Hoffman E.K., Rocha E.M., Keeney M.T., Sanders L.H., De Miranda B.R., Zharikov A., Van Laar A., Stepan A.F., Lanz T.A., et al. LRRK2 activation in idiopathic Parkinson’s disease. Sci. Transl. Med. 2018;10:eaar5429. doi: 10.1126/scitranslmed.aar5429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Hisanaga S.I., Wei R., Huo A., Tomomura M. LMTK1, a Novel Modulator of Endosomal Trafficking in Neurons. Front. Mol. Neurosci. 2020;13:112. doi: 10.3389/fnmol.2020.00112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Ferrari R., Grassi M., Salvi E., Borroni B., Palluzzi F., Pepe D., D’Avila F., Padovani A., Archetti S., Rainero I., et al. A genome-wide screening and SNPs-to-genes approach to identify novel genetic risk factors associated with frontotemporal dementia. Neurobiol. Aging. 2015;36:2904.e13–2904.e26. doi: 10.1016/j.neurobiolaging.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Yao Y., Cui X., Al-Ramahi I., Sun X., Li B., Hou J., Difiglia M., Palacino J., Wu Z.Y., Ma L., et al. A striatal-enriched intronic GPCR modulates huntingtin levels and toxicity. Elife. 2015;4:e05449. doi: 10.7554/eLife.05449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Yong X., Mao L., Shen X., Zhang Z., Billadeau D.D., Jia D. Targeting Endosomal Recycling Pathways by Bacterial and Viral Pathogens. Front. Cell Dev. Biol. 2021;9:648024. doi: 10.3389/fcell.2021.648024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Faris R., Merling M., Andersen S.E., Dooley C.A., Hackstadt T., Weber M.M. Chlamydia trachomatis CT229 Subverts Rab GTPase-Dependent CCV Trafficking Pathways to Promote Chlamydial Infection. Cell Rep. 2019;26:3380–3390.e3385. doi: 10.1016/j.celrep.2019.02.079. [DOI] [PubMed] [Google Scholar]
- 209.Martinez E., Huc-Brandt S., Brelle S., Allombert J., Cantet F., Gannoun-Zaki L., Burette M., Martin M., Letourneur F., Bonazzi M., et al. The secreted protein kinase CstK from Coxiella burnetii influences vacuole development and interacts with the GTPase-activating host protein TBC1D5. J. Biol. Chem. 2020;295:7391–7403. doi: 10.1074/jbc.RA119.010112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Siadous F.A., Cantet F., Van Schaik E., Burette M., Allombert J., Lakhani A., Bonaventure B., Goujon C., Samuel J., Bonazzi M., et al. Coxiella effector protein CvpF subverts Rab26-dependent autophagy to promote vacuole biogenesis and virulence. Autophagy. 2021;17:706–722. doi: 10.1080/15548627.2020.1728098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Joshi A.D., Swanson M.S. Secrets of a successful pathogen: Legionella resistance to progression along the autophagic pathway. Front. Microbiol. 2011;2:138. doi: 10.3389/fmicb.2011.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Gordon D.E., Hiatt J., Bouhaddou M., Rezelj V.V., Ulferts S., Braberg H., Jureka A.S., Obernier K., Guo J.Z., Batra J., et al. Comparative host-coronavirus protein interaction networks reveal pan-viral disease mechanisms. Science. 2020;370:eabe9403. doi: 10.1126/science.abe9403. [DOI] [PMC free article] [PubMed] [Google Scholar]