Abstract
Double-hit (DH) genetics induces a reduction in the complete remission (CR) and, consequently, in poor overall survival (OS) in diffuse large B-cell lymphoma (DLBCL) patients. Unfortunately, DH identification is time-consuming. Here, we retrospectively reviewed 92 newly diagnosed DLBCL patients, stratified them into the DH (n = 14) and non-DH groups (n = 78), and compared their clinical features and outcomes. The results revealed that the DH group had a higher percentage of bulky disease than the non-DH group (64.3% vs. 28.2%; p = 0.013). More patients in the DH group tested positive for double expresser (DE) (50.0% vs. 21.8%; p = 0.044). The three-year OS rates of patients with and without DH were 33.3% and 52.2%, respectively (p = 0.016). Importantly, advance stage and multiple comorbidities were correlated with a high mortality rate in multivariate analysis. Furthermore, by combining DE and the bulky disease, a specificity of 89.7% for DH prediction was achieved. In summary, DH genetics, not DE immunopositivity, could be a factor for an inferior OS in DLBCL. A combination of bulky disease and a positive DE immunophenotype could facilitate DH genetics prediction in newly diagnosed DLBCL patients.
Keywords: DLBCL, double-hit, immunophenotyped, prognosis, bulky disease
1. Introduction
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma (NHL) in adults, accounting for approximately half of all new cases [1]. Immunochemotherapy with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) approximately cures two-thirds of patients with DLBCL [2,3]. However, in patients with refractory/relapsed lymphoma subjected to R-CHOP treatment, the outcomes remain dismal [3,4]. DLBCL is a heterogeneous disease. The morphology, cell of origin (COO), molecular features, and genetic profiles can differ among different DLBCL types [5]. Although R-CHOP is the standard of care for newly diagnosed DLCBL, intensified chemotherapeutic regimens could improve the outcomes of DLBCL with high-risk features [6,7,8]. Optimal risk stratification according to the nature of the disease could facilitate the development of an appropriate therapeutic strategy for DLBCL patients by balancing the efficacy and treatment-related toxicities.
For decades, the predictive model of DLBCL using the Revised International Prognostic Index (R-IPI) score or Lugano classification has been based on clinical features, and the disease has extended. The purpose of these models is to predict the outcomes of DLBCL patients undergoing R-CHOP treatment by identifying patients with inferior overall survival (OS) [9]. Lugano classification incorporates disease extent and tumor burden to the NHL stage [10]. Regardless of the disease stage, the regimen containing immunochemotherapy is the standard treatment for DLBCL. However, 30–40% of patients eventually relapse after standard treatment and are refractory to immunochemotherapy [11]. Personalized treatment remains the best strategy for DLBCL.
With the improvement in genetic technologies, DLBCL has been discovered to be genetically heterogeneous. MYC rearrangement is one of the most important genetic alterations that have a significant impact on treatment outcomes [12,13]. Consequently, the World Health Organization 2017 Classification defined high-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements among the tumors within DLBCL morphology as double hit (DH) DLBCL [14]. In addition to DH, double expresser (DE) DLBCL, defined as MYC/BCL2 protein co-expression by immunohistochemical (IHC) staining, also has an aggressive clinical course in some reports [15]. However, the impact of DE may not be significant after adjusting for LDH levels [16]. Therefore, DH is a more profound prognostic factor for DLBCL than DE. A study by Riedell et al. [17] showed that DH DLBCL has a lower complete response (CR) rate than the non-DH DLBCL. The inferior CR rate leads to reduced OS.
Some studies have demonstrated that intensified chemotherapy or frontline autologous stem-cell transplantation may improve the outcome of DH DLBCL. However, the optimal frontline treatment strategy remains controversial [18]. Moreover, the results of DH are generally not readily available because of long turnaround times and high costs. We generally stratify the risks of high-grade B-cell lymphoma by clinical profiles, including tumor burden, DE status, R-IPI score, and Lugano staging in our real-world practice. However, the impact of DH requires further investigation. Herein, a retrospective study was conducted to analyze the prognostic impact of DH in DLBCL patients in our institution. This study further attempted to develop an algorithm to predict the DH genetics of DLBCL using clinical parameters.
2. Materials and Methods
2.1. Patients
The medical records of 126 consecutive DLBCL patients newly diagnosed between January 2018 and July 2020 at Taichung Veterans General Hospital with corresponding clinicopathological data were reviewed. Patients who did not receive FISH because of the inadequate sample size (n = 29), primary central nervous system involvement (n = 3), and no regular follow-up (n = 2) were excluded. Eventually, 92 patients were included in the current study. To investigate the clinical features and prognostic impact of DH genetics, the 92 patients were further stratified into the DH group (n = 14) and the non-DH group (n = 78).
The bulky disease was established when a tumor diameter was ≥6 cm [19]. We measured the maximal standardized uptake values (SUVs) using the [(18)F]-fluoro-2-deoxy-d-glucose positron emission tomography (FDG-PET) with a whole-body acquisition from the groin to the head in 67 of the 92 patients. The general condition of the study cohort was assessed using the Charlson comorbidity index (CCI) score and Eastern Cooperative Oncology Group performance status (PS) [20]. In terms of the initial treatments, 85 patients received intent-to-cure treatments according to the physician’s choice. Treatment regimens were stratified into standard R-CHOP (n = 65), less intensive chemotherapy (R-COP) (n = 7), and more intensive chemotherapy (R-EPOCH or R-hyperCVAD) (n = 13). This study was approved by the Review Board of Taichung Veterans General Hospital (CE21362A) and was conducted following the Declaration of Helsinki. The institutional review board waived the requirement for patients’ informed consent because of the retrospective study design.
2.2. Immunohistochemistry Analysis
The c-Myc, Bcl-2, Bcl-6, CD10, and MUM1 expressions in DLBCL cells were determined by IHC staining. Briefly, the samples were prepared using 3 µm formalin-fixed paraffin-embedded (FFPE) tissue sections. The primary antibody probes utilized were c-myc (clone EP121; Cat# BSB-6580, BioSB, Santa Barbara, CA, USA), Bcl-2 (clone 124; Cat# M0887, DAKO, Santa Clara, CA, USA), Bcl-6 (clone RBT-bcl6; Cat# BSB-5082, BioSB, Santa Barbara, CA, USA), CD10 (clone SP67; Cat# 790-4506, VENTANA, Tucson, AZ, USA), and MUM1 (clone MRQ-43; Cat# 790-4529, VENTANA, Tucson, AZ, USA). We utilized the Ventana benchmark ULTRA IHC staining system for the IHC staining. We defined DE as when ≥40% and ≥50% of DLBCL cells were positive for c-myc and BCL-2, respectively [21]. The cell of origin determination was based on Hans’ algorithm [22].
2.3. Double Hit Analysis
For the DH analysis, we employed FISH to detect MYC, BCL2, or BCL6 translocation. The dual-color break-apart rearrangement probes: SureFISH IGH MYC DF P20 (8q24.21) (G111425), Santa Clara, CA, USA, SureFISH BCL2 P20(18q21.33) (G111421), Santa Clara, CA, USA, and SureFISH BCL6 BA P20(3q27.3) (G111422), Santa Clara, CA, USA, were employed. The probe signals for monolayers of ≥200 DLBCL cell nuclei were counted under a fluorescence microscope at ×100 magnification. Genetic alteration of DH was established to occur when the probe signals exhibited a ≥15% threshold relative to the number of nuclei.
2.4. Statistical Analysis
Continuous and categorical variables between the DH and non-DH groups were compared using the Mann–Whitney U test and the Chi-squared test or Fisher’s exact test, as indicated. Numerical data are presented as the median ± standard deviation. The OS was defined as the period from the first day of treatment to death by any cause or the study censored day (30 June 2021). We performed OS analysis restricted in patient received immunochemotherapy. Patients who underwent palliative care only were excluded (n = 2 in the DH group; n = 5 in the non-DH group). Univariate and multivariate Cox regression models were used to determine the prognostic relevance quantified as hazard ratios (HRs), with 95% confidence intervals (CIs). The Kaplan–Meier survival curve was applied to estimate the OS. Sensitivity and specificity tests were employed to evaluate the DH prediction accuracy. All the tests were analyzed using the Statistical Package for the Social Sciences (IBM SPSS version 22.0; International Business Machines Corp, New York, NY, USA). The statistical significance was set at p < 0.05.
3. Results
3.1. Comparison of Clinical and Biological Features between the DH and Non-DH Groups
The sex, age, performance status, staging, R-IPI score, lactate dehydrogenase (LDH), uric acid, maximal SUV, and cell of origin were not significantly different between the DH and non-DH groups. However, the DH group had more occurrences of bulky diseases than the non-DH group (64.3% vs. 28.2%; p = 0.013). Moreover, more patients in the DH group were DE (+) (50.0% vs. 21.8%; p = 0.044). Concerning the treatments, the initial regimens were similar between groups (Table 1).
Table 1.
Patients’ characteristics and comparison of outcomes.
| All Patients (n = 92) |
Double Hit (n = 14) |
Non-Double Hit (n = 78) |
p-Value | |
|---|---|---|---|---|
| Gender, n (%) | 0.909 a | |||
| Male | 48 (52.2%) | 8 (57.1%) | 40 (51.3%) | |
| Female | 44 (47.8%) | 6 (42.9%) | 38 (48.7%) | |
| Age when diagnosed, n (%) | 0.518 a | |||
| <65 | 50 (54.3%) | 6 (42.9%) | 44 (56.4%) | |
| ≥65 | 42 (45.7%) | 8 (57.1%) | 34 (43.6%) | |
| Performance status, n (%) | 0.060 b | |||
| ≤2 | 81 (88.0%) | 10 (71.4%) | 71 (91.0%) | |
| >2 | 11 (12.0%) | 4 (28.6%) | 7 (9.0%) | |
| Stage, n (%) | 0.134 b | |||
| Limited (Stage 1–2) | 30 (32.6%) | 2 (14.3%) | 28 (35.9%) | |
| Advanced (Stage 3–4) | 62 (67.4%) | 12 (85.7%) | 50 (64.1%) | |
| Bulky disease, n (%) | 0.013 b | |||
| No | 61 (66.3%) | 5 (35.7%) | 56 (71.8%) | |
| Yes | 31 (33.7%) | 9 (64.3%) | 22 (28.2%) | |
| R-IPI score, n (%) | 0.640 a | |||
| Lower risk (0–2) | 48 (52.2%) | 6 (42.9%) | 42 (53.8%) | |
| Higher risk (3–5) | 44 (47.8%) | 8 (57.1%) | 36 (46.2%) | |
| LDH (U/L), median (range) | 315 (111–4461) | 360 (169–1760) | 303 (111–4461) | 0.277 c |
| Uric acid (mg/dL), median (range) | 5.5 (1.5–19.0) | 5.2 (3.5–16.4) | 5.6 (1.5–19.0) | 0.721 c |
| Maximal SUV (/1 h), median (range) | 12.6 (2.5–27.4) | 13.1 (4.1–25.2) | 12.4 (2.5–27.4) | 0.436 c |
| CCI score, median (range) | 4 (2–11) | 5 (2–11) | 4 (2–11) | 0.659 c |
| Double expresser, n (%) | 0.044 b | |||
| No | 68 (73.9%) | 7 (50.0%) | 61 (78.2%) | |
| Yes | 24 (26.1%) | 7 (50.0%) | 17 (21.8%) | |
| Cell of origin, n (%) | 0.122 b | |||
| GCB | 30 (34.1%) | 7 (53.8%) | 23 (30.7%) | |
| Non-GCB | 58 (65.9%) | 6 (46.2%) | 52 (69.3%) | |
| Treatment, n (%) | 0.501 a | |||
| R + intensified chemotherapy | 13 (14.1%) | 2 (14.3%) | 11 (14.1%) | |
| R-CHOP | 65 (70.7%) | 8 (57.1%) | 57 (73.1%) | |
| R-COP | 7 (7.6%) | 2 (14.3%) | 5 (6.4%) | |
| Palliative care | 7 (7.6%) | 2 (14.3%) | 5 (6.4%) | |
| Treatment response, n (%) | 0.687 a | |||
| Non-CR | 31 (36.5%) | 5 (41.7%) | 26 (35.6%) | |
| CR | 54 (63.5%) | 7 (58.3%) | 47 (64.4%) | |
| Mortality, n (%) | 0.028 a | |||
| Alive | 54 (58.7%) | 4 (28.6%) | 50 (64.1%) | |
| Death | 38 (41.3%) | 10 (71.4%) | 28 (35.9%) | |
| Causes of death, n (%) | 0.663 a | |||
| Disease related | 22 (57.9%) | 7 (70.0%) | 15 (53.6%) | |
| Complication | 11 (28.9%) | 2 (20.0%) | 9 (32.1%) | |
| Others | 5 (13.2%) | 1 (10.0%) | 4 (14.3%) |
Data were compared using a Chi-square test, b Fisher’s Exact test, and c Mann–Whitney U test. LDH: lactate dehydrogenase; SUV: standardized uptake value; CCI: Charlson comorbidity index; GCB: germinal center B-cell; R: rituximab; CR: complete remission.
3.2. Outcome Comparison between the DH and Non-DH Groups
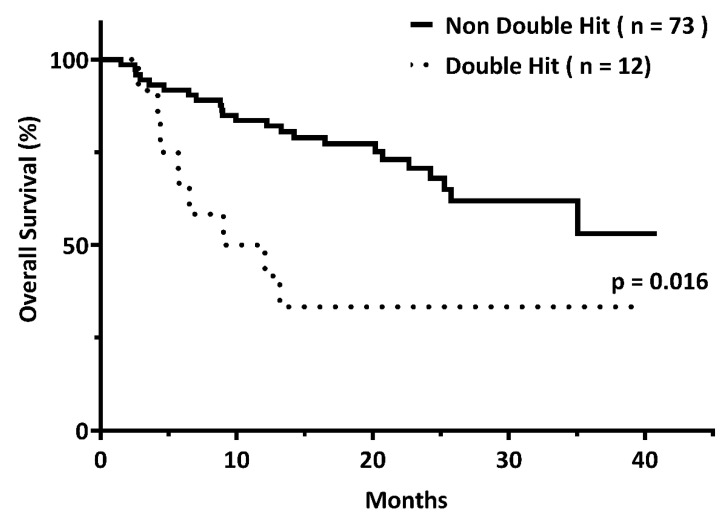
Survival analysis was performed on patients who received immunochemotherapies. The CR rates in the DH and non-DH groups were 58.3% and 64.4%, respectively (p = 0.687). With a median follow-up of 19.2 months (range, 1.5–40.9 months), the three-year OS rates of patients with and without DH were 33.3% and 52.2%, respectively (p = 0.016) (Figure 1).
Figure 1.
The three-year overall survival rates among patients with (n = 12) and without (n = 73) double hit (DH) genetics were 33.3% and 52.2%, respectively (p = 0.016).
Regarding mortality, the two groups had similar causes of death (p = 0.663). Underlying lymphoma remained the leading cause of death in the two groups, accounting for 70.0% and 53.6%, respectively (Table 1).
3.3. DH Genetics as an Independent Factor Associated with Inferior OS
We employed Cox regression analysis to investigate the impact of DH genetics on OS in DLBCL patients receiving immunochemotherapies. The univariate analysis revealed that DH (HR: 2.63; 95% CI: 1.16–5.93; p = 0.020), age ≥ 65 years (HR: 2.74; 95% CI: 1.32–5.67; p = 0.007), a high CCI score (HR: 1.35; 95% CI: 1.13–1.60; p = 0.001), uric acid level (HR: 1.13; 95% CI: 1.02–1.25; p = 0.019), maximal SUV (HR: 1.09; 95% CI: 1.02–1.17; p = 0.016), advanced stage (HR: 6.58; 95% CI: 2.00–21.66; p = 0.002), bulky disease (HR: 2.17; 95% CI: 1.07–4.42; p = 0.032), and poor risk R-IPI score (HR: 3.21; 95% CI: 1.51–6.83; p = 0.002) were significantly associated with an inferior OS (Table 2). Multivariate analysis further validated some of the results, showing advanced stage (HR: 5.00; 95% CI: 1.36–18.35; p = 0.015), and CCI score (HR: 1.30; 95% CI: 1.03–1.63; p = 0.025) were independent factors for mortality. However, DH was not substantially associated with inferior OS in this multivariate analysis (HR: 1.62; 95% CI: 0.65–4.06; p = 0.300) (Table 2).
Table 2.
Risk factors for diffuse large B cell lymphoma.
| Clinical Variables | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Age, years | ||||||
| <65 | 1.00 | 1.00 | ||||
| ≥65 | 2.74 | 1.32–5.67 | 0.007 | 1.46 | 0.57–3.71 | 0.432 |
| Gender | ||||||
| Male | 1.00 | |||||
| Female | 0.78 | 0.38–1.59 | 0.489 | |||
| Performance status | ||||||
| ≤2 | 1.00 | |||||
| >2 | 2.17 | 0.76–6.22 | 0.150 | |||
| Stage | ||||||
| Limited (Stage: 1–2) | 1.00 | 1.00 | ||||
| Advanced (Stage: 3–4) | 6.58 | 2.00–21.66 | 0.002 | 5.00 | 1.36–18.35 | 0.015 |
| Bulky, n (%) | ||||||
| No | 1.00 | 1.00 | ||||
| Yes | 2.17 | 1.07–4.42 | 0.032 | 1.80 | 0.78–4.16 | 0.169 |
| R-IPI score | ||||||
| Non-poor risk (0–2) | 1.00 | 1.00 | ||||
| Poor risk (3–5) | 3.21 | 1.51–6.83 | 0.002 | 1.21 | 0.52–2.85 | 0.655 |
| CCI score | 1.35 | 1.13–1.60 | 0.001 | 1.30 | 1.03–1.63 | 0.025 |
| LDH (U/L) | 1.00 | 1.00–1.00 | 0.197 | |||
| Uric acid (mg/dL) | 1.13 | 1.02–1.25 | 0.019 | |||
| Maximal SUV (/1 h) | 1.09 | 1.02–1.17 | 0.016 | |||
| Double hit | ||||||
| No | 1.00 | 1.00 | ||||
| Yes | 2.63 | 1.16–5.93 | 0.020 | 1.62 | 0.65–4.06 | 0.300 |
| Double expresser | ||||||
| No | 1.00 | |||||
| Yes | 1.47 | 0.69–3.12 | 0.320 | |||
| Cell of origin | ||||||
| GCB | 1.00 | |||||
| Non-GCB | 1.11 | 0.51–2.42 | 0.800 | |||
Data analysis by the Cox proportional hazard model. HR: hazard ratio; CI: confidence interval; CCI: Charlson comorbidity index; LDH: lactate dehydrogenase; SUV: standardized uptake value; GCB: germinal center B-cell.
3.4. Clinical Data of DH (+) DLBCL Patients
Since DH genetics could be factor for mortality in DLBCL patients, we analyzed the clinical data of 14 DH (+) DLBCL patients in the study cohort. The CR rate of DH (+) DLBCL after frontline therapy was 58.3% (7/12). The three-year OS rate was 33.3% among patients undergoing immunochemotherapies (4/12). All the DH (+) DLBCL patients that did not achieve CR died of the underlying lymphoma. Table 3 shows the causes of death.
Table 3.
Detailed profile of double hit (+) diffuse large B cell lymphoma patients.
| No. | Age | Stage | R-IPI | Bulky | DE | Frontline Treatment | CR | Alive | Cause of Death | PFS (Days) | OS (Days) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 75 | 4 | 5 | Yes | Yes | Palliative care | No | No | Disease related | 14 | 14 |
| 2 | 64 | 1 | 1 | No | No | R-CHOP × 6 | Yes | Yes | 1203 | 1203 | |
| 3 | 75 | 2 | 2 | Yes | No | R-COP × 8 | No | No | Disease related | 257 | 368 |
| 4 | 67 | 3 | 2 | Yes | No | R-CHOP × 4 | Yes | No | Hepatitis B flare-up | 174 | 174 |
| 5 | 54 | 4 | 2 | No | No | R-CHOP × 8 | Yes | Yes | 1176 | 1176 | |
| 6 | 77 | 3 | 3 | Yes | No | R-COP × 2 | No | No | Disease related | 85 | 85 |
| 7 | 54 | 4 | 2 | No | Yes | (R-CHOP + IT) × 5 | Yes | No | Septic shock | 128 | 128 |
| 8 | 46 | 4 | 2 | No | No | (R-CHOP + IT, R-MA) × 2 | No | No | Disease related | 223 | 275 |
| 9 | 80 | 4 | 4 | Yes | Yes | Palliative care | No | No | Disease related | 43 | 43 |
| 10 | 71 | 3 | 4 | Yes | No | R-CEOP × 5 | No | No | Disease related | 158 | 401 |
| 11 | 48 | 4 | 3 | Yes | Yes | R-CHOP × 1 | No | No | Disease related | 58 | 134 |
| 12 | 70 | 4 | 3 | Yes | Yes | R-CHOP × 6 | Yes | Yes | 866 | 866 | |
| 13 | 66 | 4 | 3 | No | Yes | R-CHOP × 6 | Yes | No | Aortic stenosis with heart failure | 199 | 199 |
| 14 | 41 | 3 | 3 | Yes | Yes | R-EPOCH × 6 | Yes | Yes | 1157 | 1157 |
R-IPI: revised International Prognostic Index; DE: double expresser; CR: complete remission; PFS: progression-free survival; OS: overall survival; IT: intrathecal chemotherapy; R-CHOP: rituximab plus cyclophosphamide, doxorubicin, vincristine, prednisone; R-COP: rituximab, cyclophosphamide, vincristine, prednisone; R-EPOCH: rituximab, etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin; R-MA: rituximab, methotrexate, cytarabine.
3.5. Bulky Disease with DE Immunopositivity for Identifying DH DLBCL
Since DH was associated with a low CR rate and increased mortality in DLBCL patients, a rapid and reliable surrogate marker to predict DH in newly diagnosed DLBCL patients is essential. Our results showed that the sensitivities of DE and the bulky disease for DH prediction were 50.0% and 64.3%, while the specificities were 78.2% and 71.8%, respectively. DE appears more accurate than the bulky disease for predicting DH (73.9% vs. 70.7%). Furthermore, by combining the DE and bulky disease, a specificity of 89.7% for DH prediction was achieved (Table 4).
Table 4.
Prediction of double hit genetics.
| Double Hit | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Yes | No | |||||||
| Double expresser | Yes | 24 | 7 | 17 | 50.0 | 78.2 | 29.2 | 89.7 | 73.9 |
| No | 68 | 7 | 61 | ||||||
| Bulky disease | Yes | 31 | 9 | 22 | 64.3 | 71.8 | 29.0 | 91.8 | 70.7 |
| No | 61 | 5 | 56 | ||||||
| Double expresser + bulky disease | Yes | 13 | 5 | 8 | 35.7 | 89.7 | 38.5 | 88.6 | 81.5 |
| No | 79 | 9 | 70 | ||||||
PPV: positive predictive value; NPV: negative predictive value.
4. Discussion
In the current study, it was found that DH genetics constituted 15.2% of newly diagnosed DLBCL cases. Among DH DLBCL patients, only 50.0% were positive for DE immunophenotype. DH genetics, but not DE immunopositivity, was a factor for inferior OS in terms of survival. However, we established that the positive DE immunophenotype and bulky disease were both indicative of DH genetics. A positive DE immunophenotype and a bulky disease could predict DH genetics with specificities of 78.2% and 71.8%, respectively. Furthermore, a combination of bulky disease and positive DE immunophenotype could achieve a specificity of 89.7% for predicting DH genetics in newly diagnosed DLBCL patients.
The impact of DH genetics on the OS of DLBCL is increasing [23]. Our study showed that DLBCL patients with DH genetics have a shorter OS by three years compared to those without DH genetics (33.3% vs. 52.2%; p = 0.016). The MYC gene alterations may be the primary cause of this. The MYC gene was initially detected in Burkitt lymphoma as a potent oncogene and is associated with aggressive clinical behavior [24]. The role of the MYC gene has been extensively investigated. Not only is it a transcription factor that causes cell proliferation, but also it plays a role in the induction of apoptosis [25]. Aggressive lymphomas appear to have acquired additional oncogenic alterations that cooperate with MYC dysregulation by counteracting its pro-apoptotic function [26]. Moreover, studies have suggested that MYC translocation arises in the germinal center (GC) microenvironment because of the role of massive proliferation and GC phenotype [27]. In the cell of origin model, DH genetics is more frequent in the GCB DLBCL group, while DE immunopositivity is more frequent in the non-GCB subset [28]. However, our study did not reveal the same results, presumably because of the limited number of patients.
Additionally, the current study analyzed the correlation between DH genetics and DE immunophenotype. A study by Scott et al. [14] showed that 75.0% of DLBCL patients with DH genetics had a positive DE immunophenotype; however, the reverse was not necessarily true. Our results showed that only 50.0% of DLBCL patients with DH genetics were positive for the DE immunophenotype, which was lower than that reported by Scott et al. More than existing DH genetics, chromosomal translocations, MYC gene amplification, and post-translational processes could be the potential mechanisms leading to increased MYC protein expression [29]. Moreover, various genetic backgrounds in different cohorts may also be one of the reasons for this difference. Further studies are required to validate this discrepancy.
Regarding survival, the current study found that DH DLBCL patients had a lower OS rate than non-DH DLBCL patients. Interestingly, the CR rates between the two groups were not substantially different. A previous study revealed that DH DLBCL might benefit more from intensified chemotherapy [30]. Therefore, we examined the disease course of each DH DLBCL in our study cohort. We established that only two (cases 8 and 14) of the 14 patients received chemotherapeutic regimens that are more intense than R-CHOP as their frontline treatment. This reflects the fact that the early identification of DH DLBCL remains a challenge. Thus, the identification of potential DLBCLs using surrogate markers is crucial.
DH genetics has been associated with elevated LDH, high-risk IPI scores, and advanced stages [7]. Our analyses showed that DLBCL patients with DH genetics were more likely to have the bulky disease. Although the prognostic value of the bulky disease appears to be less prominent in the era of rituximab [31], we attempted to utilize bulky disease and DE immunophenotype as surrogate markers to predict DH genetics in DLBCL. With a specificity of 89.7%, the findings suggested that DLBCL patients without the bulky disease and DE immunophenotype were less likely to harbor DH genetics. Thus, standard R-CHOP treatment may be appropriate for these patients.
The small number of patients and the retrospective nature of the study were the primary limitations of the current research. Although our retrospective cohort showed that DH genetics were associated with bulky disease and an inferior OS in DLBCL patients, studies with more patients and prospective design are needed to validate our results. In summary, our study demonstrated that DH genetics, not DE immunophenotype, could be a factor for an inferior OS in DLBCL. The combination of a positive DE immunophenotype and bulky disease simultaneously could achieve a specificity of 89.7% for predicting DH genetics in newly diagnosed DLBCL patients. Intensified chemotherapeutic regimens or frontline autologous stem cell transplantation may be considered for fit DLBCL patients with these two features.
Acknowledgments
We thank the technical services provided by the hematological laboratory of Division of Hematology/Medical Oncology, Department of Medicine, Taichung Veterans General Hospital, Taiwan.
Author Contributions
C.-H.W. and T.-C.C. wrote the paper and analyzed the data. R.-C.W. reviewed and interpreted the tissue sections. C.-L.J.T. and T.-C.C. planned, designed, coordinated the research. J.-P.G., Y.-H.S. and Y.-C.S. provided important materials and help in the study. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was approved by the Review Board of Taichung Veterans General Hospital (CE21362A, approved on 14 September 2021) and was conducted following the Declaration of Helsinki.
Informed Consent Statement
The institutional review board waived the requirement for patients’ informed consent because of the retrospective study design.
Data Availability Statement
Not applicable.
Conflicts of Interest
Chieh-Lin Jerry Teng received an honorarium and consulting fees from Novartis, Roche, Takeda, Johnson & Johnson, Amgen, BMS Celgene, Kirin, AbbVie, and MSD. The other authors declare that they have no conflicts of interest.
Funding Statement
This research was partially supported by the grant from TCVGH-1103701A.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2019. CA Cancer J. Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.Bartlett N.L., Wilson W.H., Jung S.H., Hsi E.D., Maurer M.J., Pederson L.D., Polley M.C., Pitcher B.N., Cheson B.D., Kahl B.S., et al. Dose-Adjusted EPOCH-R Compared with R-CHOP as Frontline Therapy for Diffuse Large B-Cell Lymphoma: Clinical Outcomes of the Phase III Intergroup Trial Alliance/CALGB 50303. J. Clin. Oncol. 2019;37:1790–1799. doi: 10.1200/JCO.18.01994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coiffier B., Thieblemont C., Van Den Neste E., Lepeu G., Plantier I., Castaigne S., Lefort S., Marit G., Macro M., Sebban C., et al. Long-term outcome of patients in the LNH-98.5 trial, the first randomized study comparing rituximab-CHOP to standard CHOP chemotherapy in DLBCL patients: A study by the Groupe d’Etudes des Lymphomes de l’Adulte. Blood. 2010;116:2040–2045. doi: 10.1182/blood-2010-03-276246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crump M., Neelapu S.S., Farooq U., Van Den Neste E., Kuruvilla J., Westin J., Link B.K., Hay A., Cerhan J.R., Zhu L., et al. Outcomes in refractory diffuse large B-cell lymphoma: Results from the international SCHOLAR-1 study. Blood. 2017;130:1800–1808. doi: 10.1182/blood-2017-03-769620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu Y., Barta S.K. Diffuse large B-cell lymphoma: 2019 update on diagnosis, risk stratification, and treatment. Am. J. Hematol. 2019;94:604–616. doi: 10.1002/ajh.25460. [DOI] [PubMed] [Google Scholar]
- 6.Leppa S., Jorgensen J., Tierens A., Meriranta L., Ostlie I., de Nully Brown P., Fagerli U.M., Larsen T.S., Mannisto S., Munksgaard L., et al. Patients with high-risk DLBCL benefit from dose-dense immunochemotherapy combined with early systemic CNS prophylaxis. Blood Adv. 2020;4:1906–1915. doi: 10.1182/bloodadvances.2020001518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oki Y., Noorani M., Lin P., Davis R.E., Neelapu S.S., Ma L., Ahmed M., Rodriguez M.A., Hagemeister F.B., Fowler N., et al. Double hit lymphoma: The MD Anderson Cancer Center clinical experience. Br. J. Haematol. 2014;166:891–901. doi: 10.1111/bjh.12982. [DOI] [PubMed] [Google Scholar]
- 8.Petrich A.M., Gandhi M., Jovanovic B., Castillo J.J., Rajguru S., Yang D.T., Shah K.A., Whyman J.D., Lansigan F., Hernandez-Ilizaliturri F.J., et al. Impact of induction regimen and stem cell transplantation on outcomes in double-hit lymphoma: A multicenter retrospective analysis. Blood. 2014;124:2354–2361. doi: 10.1182/blood-2014-05-578963. [DOI] [PubMed] [Google Scholar]
- 9.Sehn L.H., Berry B., Chhanabhai M., Fitzgerald C., Gill K., Hoskins P., Klasa R., Savage K.J., Shenkier T., Sutherland J., et al. The revised International Prognostic Index (R-IPI) is a better predictor of outcome than the standard IPI for patients with diffuse large B-cell lymphoma treated with R-CHOP. Blood. 2007;109:1857–1861. doi: 10.1182/blood-2006-08-038257. [DOI] [PubMed] [Google Scholar]
- 10.Cheson B.D., Fisher R.I., Barrington S.F., Cavalli F., Schwartz L.H., Zucca E., Lister T.A., Alliance A.L., Lymphoma G., Eastern Cooperative Oncology G., et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: The Lugano classification. J. Clin. Oncol. 2014;32:3059–3068. doi: 10.1200/JCO.2013.54.8800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pasqualucci L., Dalla-Favera R. Genetics of diffuse large B-cell lymphoma. Blood. 2018;131:2307–2319. doi: 10.1182/blood-2017-11-764332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hilton L.K., Tang J., Ben-Neriah S., Alcaide M., Jiang A., Grande B.M., Rushton C.K., Boyle M., Meissner B., Scott D.W., et al. The double-hit signature identifies double-hit diffuse large B-cell lymphoma with genetic events cryptic to FISH. Blood. 2019;134:1528–1532. doi: 10.1182/blood.2019002600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Savage K.J., Johnson N.A., Ben-Neriah S., Connors J.M., Sehn L.H., Farinha P., Horsman D.E., Gascoyne R.D. MYC gene rearrangements are associated with a poor prognosis in diffuse large B-cell lymphoma patients treated with R-CHOP chemotherapy. Blood. 2009;114:3533–3537. doi: 10.1182/blood-2009-05-220095. [DOI] [PubMed] [Google Scholar]
- 14.Scott D.W., King R.L., Staiger A.M., Ben-Neriah S., Jiang A., Horn H., Mottok A., Farinha P., Slack G.W., Ennishi D., et al. High-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements with diffuse large B-cell lymphoma morphology. Blood. 2018;131:2060–2064. doi: 10.1182/blood-2017-12-820605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu S., Xu-Monette Z.Y., Tzankov A., Green T., Wu L., Balasubramanyam A., Liu W.M., Visco C., Li Y., Miranda R.N., et al. MYC/BCL2 protein coexpression contributes to the inferior survival of activated B-cell subtype of diffuse large B-cell lymphoma and demonstrates high-risk gene expression signatures: A report from The International DLBCL Rituximab-CHOP Consortium Program. Blood. 2013;121:4021–4031. doi: 10.1182/blood-2012-10-460063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han B., Kim S., Koh J., Yim J., Lee C., Heo D.S., Kim T.M., Paik J.H., Jeon Y.K. Immunophenotypic Landscape and Prognosis of Diffuse Large B-Cell Lymphoma with MYC/BCL2 Double Expression: An Analysis of A Prospectively Immunoprofiled Cohort. Cancers. 2020;12:3305. doi: 10.3390/cancers12113305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riedell P.A., Smith S.M. Double hit and double expressors in lymphoma: Definition and treatment. Cancer. 2018;124:4622–4632. doi: 10.1002/cncr.31646. [DOI] [PubMed] [Google Scholar]
- 18.Landsburg D.J., Falkiewicz M.K., Maly J., Blum K.A., Howlett C., Feldman T., Mato A.R., Hill B.T., Li S., Medeiros L.J., et al. Outcomes of Patients with Double-Hit Lymphoma Who Achieve First Complete Remission. J. Clin. Oncol. 2017;35:2260–2267. doi: 10.1200/JCO.2017.72.2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pfreundschuh M., Ho A.D., Cavallin-Stahl E., Wolf M., Pettengell R., Vasova I., Belch A., Walewski J., Zinzani P.L., Mingrone W., et al. Prognostic significance of maximum tumour (bulk) diameter in young patients with good-prognosis diffuse large-B-cell lymphoma treated with CHOP-like chemotherapy with or without rituximab: An exploratory analysis of the MabThera International Trial Group (MInT) study. Lancet Oncol. 2008;9:435–444. doi: 10.1016/S1470-2045(08)70078-0. [DOI] [PubMed] [Google Scholar]
- 20.Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 21.Swerdlow S.H., Campo E., Pileri S.A., Harris N.L., Stein H., Siebert R., Advani R., Ghielmini M., Salles G.A., Zelenetz A.D., et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375–2390. doi: 10.1182/blood-2016-01-643569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hans C.P., Weisenburger D.D., Greiner T.C., Gascoyne R.D., Delabie J., Ott G., Muller-Hermelink H.K., Campo E., Braziel R.M., Jaffe E.S., et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103:275–282. doi: 10.1182/blood-2003-05-1545. [DOI] [PubMed] [Google Scholar]
- 23.Berendsen M.R., Stevens W.B.C., van den Brand M., van Krieken J.H., Scheijen B. Molecular Genetics of Relapsed Diffuse Large B-Cell Lymphoma: Insight into Mechanisms of Therapy Resistance. Cancers. 2020;12:3553. doi: 10.3390/cancers12123553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ott G., Rosenwald A., Campo E. Understanding MYC-driven aggressive B-cell lymphomas: Pathogenesis and classification. Blood. 2013;122:3884–3891. doi: 10.1182/blood-2013-05-498329. [DOI] [PubMed] [Google Scholar]
- 25.Klapproth K., Wirth T. Advances in the understanding of MYC-induced lymphomagenesis. Br. J. Haematol. 2010;149:484–497. doi: 10.1111/j.1365-2141.2010.08159.x. [DOI] [PubMed] [Google Scholar]
- 26.Hemann M.T., Bric A., Teruya-Feldstein J., Herbst A., Nilsson J.A., Cordon-Cardo C., Cleveland J.L., Tansey W.P., Lowe S.W. Evasion of the p53 tumour surveillance network by tumour-derived MYC mutants. Nature. 2005;436:807–811. doi: 10.1038/nature03845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Calado D.P., Sasaki Y., Godinho S.A., Pellerin A., Kochert K., Sleckman B.P., de Alboran I.M., Janz M., Rodig S., Rajewsky K. The cell-cycle regulator c-Myc is essential for the formation and maintenance of germinal centers. Nat. Immunol. 2012;13:1092–1100. doi: 10.1038/ni.2418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Green T.M., Young K.H., Visco C., Xu-Monette Z.Y., Orazi A., Go R.S., Nielsen O., Gadeberg O.V., Mourits-Andersen T., Frederiksen M., et al. Immunohistochemical double-hit score is a strong predictor of outcome in patients with diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J. Clin. Oncol. 2012;30:3460–3467. doi: 10.1200/JCO.2011.41.4342. [DOI] [PubMed] [Google Scholar]
- 29.Sewastianik T., Prochorec-Sobieszek M., Chapuy B., Juszczynski P. MYC deregulation in lymphoid tumors: Molecular mechanisms, clinical consequences and therapeutic implications. Biochim. Biophys. Acta. 2014;1846:457–467. doi: 10.1016/j.bbcan.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 30.Laude M.C., Lebras L., Sesques P., Ghesquieres H., Favre S., Bouabdallah K., Croizier C., Guieze R., Drieu La Rochelle L., Gyan E., et al. First-line treatment of double-hit and triple-hit lymphomas: Survival and tolerance data from a retrospective multicenter French study. Am. J. Hematol. 2021;96:302–311. doi: 10.1002/ajh.26068. [DOI] [PubMed] [Google Scholar]
- 31.Basci S., Yigenoglu T.N., Bakirtas M., Uncu Ulu B., Yaman S., Dal M.S., Kizil Cakar M., Altuntas F. The effect of bulky mass on prognosis in diffuse large-B-cell lymphoma: Still poor? Leuk. Res. 2021;102:106521. doi: 10.1016/j.leukres.2021.106521. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.